Which hole does the baby come out of
Female Reproductive System (for Parents)
What Is Reproduction?
Reproduction is the process by which organisms make more organisms like themselves. But even though the reproductive system is essential to keeping a species alive, unlike other body systems, it's not essential to keeping an individual alive.
In the human reproductive process, two kinds of sex cells, or gametes (GAH-meetz), are involved. The male gamete, or sperm, and the female gamete, the egg or ovum, meet in the female's reproductive system. When sperm fertilizes (meets) an egg, this fertilized egg is called a zygote (ZYE-goat). The zygote goes through a process of becoming an embryo and developing into a fetus.
The male reproductive system and the female reproductive system both are needed for reproduction.
Humans, like other organisms, pass some characteristics of themselves to the next generation. We do this through our genes, the special carriers of human traits. The genes that parents pass along are what make their children similar to others in their family, but also what make each child unique. These genes come from the male's sperm and the female's egg.
What Is the Female Reproductive System?
The external part of the female reproductive organs is called the vulva, which means covering. Located between the legs, the vulva covers the opening to the vagina and other reproductive organs inside the body.
The fleshy area located just above the top of the vaginal opening is called the mons pubis. Two pairs of skin flaps called the labia (which means lips) surround the vaginal opening. The clitoris, a small sensory organ, is located toward the front of the vulva where the folds of the labia join. Between the labia are openings to the urethra (the canal that carries pee from the bladder to the outside of the body) and vagina. When girls become sexually mature, the outer labia and the mons pubis are covered by pubic hair.
A female's internal reproductive organs are the vagina, uterus, fallopian tubes, and ovaries.
The vagina is a muscular, hollow tube that extends from the vaginal opening to the uterus. Because it has muscular walls, the vagina can expand and contract. This ability to become wider or narrower allows the vagina to accommodate something as slim as a tampon and as wide as a baby. The vagina's muscular walls are lined with mucous membranes, which keep it protected and moist.
The vagina serves three purposes:
- It's where the penis is inserted during sexual intercourse.
- It's the pathway (the birth canal) through which a baby leaves a woman's body during childbirth.
- It's the route through which menstrual blood leaves the body during periods.
A very thin piece of skin-like tissue called the hymen partly covers the opening of the vagina. Hymens are often different from female to female. Most women find their hymens have stretched or torn after their first sexual experience, and the hymen may bleed a little (this usually causes little, if any, pain). Some women who have had sex don't have much of a change in their hymens, though. And some women's hymens have already stretched even before they have sex.
Some women who have had sex don't have much of a change in their hymens, though. And some women's hymens have already stretched even before they have sex.
The vagina connects with the uterus, or womb, at the cervix (which means neck). The cervix has strong, thick walls. The opening of the cervix is very small (no wider than a straw), which is why a tampon can never get lost inside a girl's body. During childbirth, the cervix can expand to allow a baby to pass.
The uterus is shaped like an upside-down pear, with a thick lining and muscular walls — in fact, the uterus contains some of the strongest muscles in the female body. These muscles are able to expand and contract to accommodate a growing fetus and then help push the baby out during labor. When a woman isn't pregnant, the uterus is only about 3 inches (7.5 centimeters) long and 2 inches (5 centimeters) wide.
At the upper corners of the uterus, the fallopian tubes connect the uterus to the ovaries. The ovaries are two oval-shaped organs that lie to the upper right and left of the uterus. They produce, store, and release eggs into the fallopian tubes in the process called ovulation (av-yoo-LAY-shun).
The ovaries are two oval-shaped organs that lie to the upper right and left of the uterus. They produce, store, and release eggs into the fallopian tubes in the process called ovulation (av-yoo-LAY-shun).
There are two fallopian (fuh-LO-pee-un) tubes, each attached to a side of the uterus. Within each tube is a tiny passageway no wider than a sewing needle. At the other end of each fallopian tube is a fringed area that looks like a funnel. This fringed area wraps around the ovary but doesn't completely attach to it. When an egg pops out of an ovary, it enters the fallopian tube. Once the egg is in the fallopian tube, tiny hairs in the tube's lining help push it down the narrow passageway toward the uterus.
The ovaries (OH-vuh-reez) are also part of the endocrine system because they produce female sex
hormonessuch as estrogen (ESS-truh-jun) and progesterone (pro-JESS-tuh-rone).
How Does the Female Reproductive System Work?
The female reproductive system enables a woman to:
- produce eggs (ova)
- have sexual intercourse
- protect and nourish a fertilized egg until it is fully developed
- give birth
Sexual reproduction couldn't happen without the sexual organs called the gonads. Most people think of the gonads as the male testicles. But both sexes have gonads: In females the gonads are the ovaries, which make female gametes (eggs). The male gonads make male gametes (sperm).
Most people think of the gonads as the male testicles. But both sexes have gonads: In females the gonads are the ovaries, which make female gametes (eggs). The male gonads make male gametes (sperm).
When a baby girl is born, her ovaries contain hundreds of thousands of eggs, which stay inactive until puberty begins. At puberty, the
pituitary gland (in the central part of the brain) starts making hormones that stimulate the ovaries to make female sex hormones, including estrogen. The secretion of these hormones causes a girl to develop into a sexually mature woman.
Toward the end of puberty, girls begin to release eggs as part of a monthly period called the menstrual cycle. About once a month, during ovulation, an ovary sends a tiny egg into one of the fallopian tubes.
Unless the egg is fertilized by a sperm while in the fallopian tube, the egg leaves the body about 2 weeks later through the uterus — this is menstruation. Blood and tissues from the inner lining of the uterus combine to form the menstrual flow, which in most girls lasts from 3 to 5 days. A girl's first period is called menarche (MEH-nar-kee).
A girl's first period is called menarche (MEH-nar-kee).
It's common for women and girls to have some discomfort in the days leading to their periods. Premenstrual syndrome (PMS) includes both physical and emotional symptoms that many girls and women get right before their periods, such as:
- acne
- bloating
- tiredness
- backaches
- sore breasts
- headaches
- constipation
- diarrhea
- food cravings
- depression
- irritability
- trouble concentrating or handling stress
PMS is usually at its worst during the 7 days before a girl's period starts and disappears after it begins.
Many girls also have belly cramps during the first few days of their periods caused by prostaglandins, chemicals in the body that make the smooth muscle in the uterus contract. These involuntary contractions can be dull or sharp and intense.
It can take up to 2 years from menarche for a girl's body to develop a regular menstrual cycle. During that time, her body is adjusting to the hormones puberty brings. On average, the monthly cycle for an adult woman is 28 days, but the range is from 23 to 35 days.
During that time, her body is adjusting to the hormones puberty brings. On average, the monthly cycle for an adult woman is 28 days, but the range is from 23 to 35 days.
What Happens If an Egg Is Fertilized?
If a female and male have sex within several days of the female's ovulation, fertilization can happen. When the male ejaculates (when semen leaves the penis), a small amount of semen is deposited into the vagina. Millions of sperm are in this small amount of semen, and they "swim" up from the vagina through the cervix and uterus to meet the egg in the fallopian tube. It takes only one sperm to fertilize the egg.
About 5 to 6 days after the sperm fertilizes the egg, the fertilized egg (zygote) has become a multicelled blastocyst. A blastocyst (BLAS-tuh-sist) is about the size of a pinhead, and it's a hollow ball of cells with fluid inside. The blastocyst burrows itself into the lining of the uterus, called the endometrium. The hormone estrogen causes the endometrium (en-doh-MEE-tree-um) to become thick and rich with blood. Progesterone, another hormone released by the ovaries, keeps the endometrium thick with blood so that the blastocyst can attach to the uterus and absorb nutrients from it. This process is called implantation.
Progesterone, another hormone released by the ovaries, keeps the endometrium thick with blood so that the blastocyst can attach to the uterus and absorb nutrients from it. This process is called implantation.
As cells from the blastocyst take in nourishment, another stage of development begins. In the embryonic stage, the inner cells form a flattened circular shape called the embryonic disk, which will develop into a baby. The outer cells become thin membranes that form around the baby. The cells multiply thousands of times and move to new positions to eventually become the embryo (EM-bree-oh).
After about 8 weeks, the embryo is about the size of a raspberry, but almost all of its parts — the brain and nerves, the heart and blood, the stomach and intestines, and the muscles and skin — have formed.
During the fetal stage, which lasts from 9 weeks after fertilization to birth, development continues as cells multiply, move, and change. The fetus (FEE-tis) floats in amniotic (am-nee-AH-tik) fluid inside the amniotic sac. It gets oxygen and nourishment from the mother's blood via the placenta (pluh-SEN-tuh). This disk-like structure sticks to the inner lining of the uterus and connects to the fetus via the umbilical (um-BIL-ih-kul) cord. The amniotic fluid and membrane cushion the fetus against bumps and jolts to the mother's body.
It gets oxygen and nourishment from the mother's blood via the placenta (pluh-SEN-tuh). This disk-like structure sticks to the inner lining of the uterus and connects to the fetus via the umbilical (um-BIL-ih-kul) cord. The amniotic fluid and membrane cushion the fetus against bumps and jolts to the mother's body.
Pregnancy lasts an average of 280 days — about 9 months. When the baby is ready for birth, its head presses on the cervix, which begins to relax and widen to get ready for the baby to pass into and through the vagina. Mucus has formed a plug in the cervix, which now loosesn. It and amniotic fluid come out through the vagina when the mother's water breaks.
When the contractions of labor begin, the walls of the uterus contract as they are stimulated by the pituitary hormone oxytocin (ahk-see-TOE-sin). The contractions cause the cervix to widen and begin to open. After several hours of this widening, the cervix is dilated (opened) enough for the baby to come through. The baby is pushed out of the uterus, through the cervix, and along the birth canal. The baby's head usually comes first. The umbilical cord comes out with the baby. It's clamped and cut close to the navel after the baby is delivered.
The baby is pushed out of the uterus, through the cervix, and along the birth canal. The baby's head usually comes first. The umbilical cord comes out with the baby. It's clamped and cut close to the navel after the baby is delivered.
The last stage of the birth process involves the delivery of the placenta, which at that point is called the afterbirth. After it has separated from the inner lining of the uterus, contractions of the uterus push it out, along with its membranes and fluids.
Your baby in the birth canal Information | Mount Sinai
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Childbirth is really a series of four stages that culminate in the actual birth and short period thereafter. For more specific information regarding emergency delivery see the information on childbirth, emergency delivery.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Cephalic (head first) presentation is considered normal, but a breech (feet or buttocks first) delivery can be very difficult, even dangerous for the mother and the baby.
In a normal pregnancy, the baby is positioned head down in the uterus.
The term fetal presentation refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
FETAL LIE
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between his head and tailbone.
Your baby's spine is between his head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.

- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
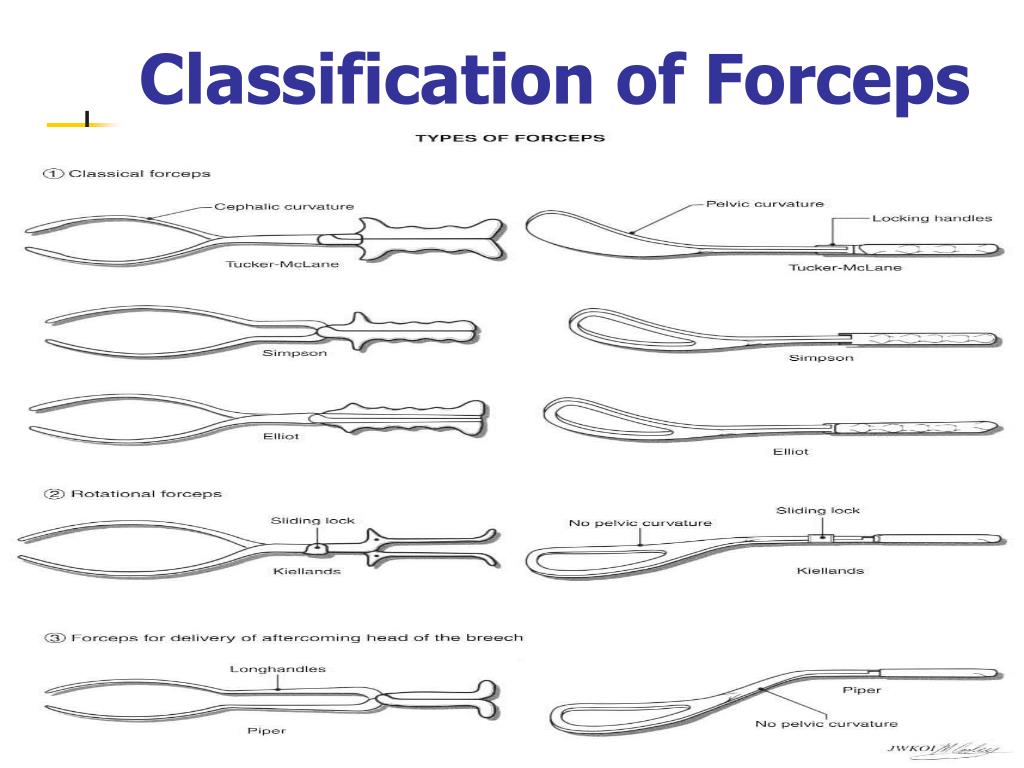
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
Engagement
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
Descent
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
Flexion
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
Extension
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back.
 It rotates under and around the pubic bone.
It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
Expulsion
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Last reviewed on: 12/3/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
What does the child feel during childbirth?
Children, unlike mothers, cannot share their birth stories…maybe it is not in vain that this is provided by nature?
PRESSURE for uterine contractions. The child is not endangered; during normal childbirth, it is protected by amniotic fluid. When passing through the birth canal, the anatomy (bone mobility) helps to compensate for pressure and prevent injuries to the child.
STRESS , in a good way. During childbirth, the mother's body produces a hormone that helps to cope with pain. It stimulates the production of the stress hormone in the baby, which mobilizes the body to “eliminate the threat” and prepares it for life outside the womb.
SON . The baby can maintain the sleep cycle it is used to in the womb and sleep up to 50 minutes every hour.
DISTRESS fetus. If the pregnancy did not go very smoothly, the condition of the child during childbirth may worsen. For example, oxygen delivery may decrease, and the heartbeat will worsen. Therefore, during childbirth, KTG . If so, the doctors take the necessary measures.
PAIN during the period of exile. With a normal birth, it is not very strong. If, for example, a child is born with a birth tumor, it is logical that he was not well. But the sensations experienced by the child are not comparable with the sensations of the mother. This is due to the fact that the pain receptors in the newborn are not yet fully developed.
MOOD mother. It is necessary to remain calm and positive not only during pregnancy, but also during childbirth. It has been proven that the baby's heartbeat slows down, and he calms down when he hears the mother's voice. No matter how the birth goes, the child understands that “something is wrong”, so it is important for him to hear his mother. There are also studies that prove the positive effect of mother's laughter on the child. Women in childbirth don't often laugh, but having a partner help create the right atmosphere would be great!
No matter how the birth goes, the child understands that “something is wrong”, so it is important for him to hear his mother. There are also studies that prove the positive effect of mother's laughter on the child. Women in childbirth don't often laugh, but having a partner help create the right atmosphere would be great!
EFFECTS OF DRUGS . Much that enters the mother's body crosses the placental barrier. With general anesthesia, the child may fall asleep or even stop breathing. Therefore, the preferred method of pain relief is epidural anesthesia. The absorption of its components is minimal, so we can say that it practically does not enter the bloodstream of the fetus and does not have a systemic effect on its body.
FIRST BREATH . The crying of a baby after birth speaks of the health of his lungs. During the first breath, the lungs begin to expand, and this mechanism is accompanied by a cry. At the same time, the first breath and cry allow you to clear the lungs of amniotic fluid.
SENSOR OVERLOAD . After giving birth, everything around becomes colder, noisier and brighter.
TEMPERATURE CHANGE . Amniotic fluid facilitates the transition from uterine temperature to ambient temperature, and the physiology of the newborn compensates for temperature changes. Moreover, in rodboxes we maintain a comfortable temperature for mother and child, and we put newborns on special heated tables.
CONTACT WITH MOM . It is proved that the first hour after childbirth plays a fundamental role in the further development of the baby. Therefore, the procedures for weighing, washing, etc. are postponed in favor of the soonest establishment of skin-to-skin contact. Mom is the only person a child knows in this world, and their quick separation can be traumatic for the child. The child calms down, lying on the mother's chest and hearing her voice immediately after birth. In the future, the moments when his mother takes care of him, breastfeeds are very important for him. It is imperative to talk with the child, then he will understand that the voice that accompanied him 9months, still with him.
It is imperative to talk with the child, then he will understand that the voice that accompanied him 9months, still with him.
A child's attachment to his mother develops in the womb. The child not only hears the voice, but even feels the mother's smell. After the child is born, attachment grows, growing into love.
Diastasis of the rectus abdominis muscles - symptoms, signs, degrees, causes and treatment in men and women in Moscow in the "SM-Clinic"
This disease is treated by the Surgeon
Book online Request a call
- What is diastasis rectus abdominis?
- About disease
- Species
- Symptoms of diastasis recti
- Causes of diastasis recti
- Diagnostics of diastasis of the rectus abdominis muscles
- Expert opinion
- Treatment of diastasis recti
- Surgical treatment of diastasis recti
- Prophylaxis
- Rehabilitation after surgery
- Questions and Answers
- Sources
About the disease
The disease is based on stretching and expansion of the white line of the abdomen - a tendon that is located between the rectus muscles, connects and holds them. This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.
This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.
Due to an increase in intra-abdominal pressure or a violation of the properties of the connective fibers, the structure of the tendon changes, it weakens, becomes thinner and stretches. The trigger mechanism is prolonged pressure on the abdominal wall associated with pregnancy or visceral obesity. An aggravating factor is the loosening of the white line against the background of collagenopathy, the effects of relaxin, the immaturity of cellular structures, etc.
As a result, the white line becomes thinner and stretched. Normally, its dimensions are restored with a gradual decrease in the abdomen or as the properties of the connective tissue normalize. Thus, physiological diastasis is eliminated during the neonatal period or in women after childbirth.
If abdominal training is started early in the postpartum period, this leads to a contraction of the rectus muscles and a simultaneous increase in intra-abdominal pressure, and the white line is fixed in a stretched position and does not hold the internal organs well. As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
Species
Depending on the magnitude of the stretching of the tendon ligament, there are 3 degrees of diastasis of the rectus abdominis muscles:
- first - the muscles move away from each other by 2.5-5 cm;
- second - ligaments diverge by 5-8 cm;
- third - the line is stretched more than 8 cm.
According to the localization of the place of maximum stretching, supra-umbilical, sub-umbilical and mixed forms of diastasis are distinguished.
According to the degree of involvement of other muscles of the anterior abdominal wall, the pathology is classified into types:
- A - classical divergence of muscles after natural childbirth;
- B - relaxation of the lower lateral parts of the muscles;
- C - the expansion affects the region of the ribs and the xiphoid process;
- D - diastasis is combined with a curvature of the waistline.

Symptoms of diastasis of the rectus abdominis muscles
Manifestations of BPMD increase as the pathology progresses. In women, a vivid clinical picture manifests itself abruptly (shortly after childbirth), while in men the disease develops gradually.
At the onset of the disease, there may be no symptoms at all. The patient then notices a characteristic rounded vertical protrusion in the center of the abdomen. With deliberate tension of the press, the inner edges of the rectus muscles and the groove between them are clearly visible. Due to muscle dysfunction, pain in the spine, lower back, fatigue, and posture disorders are possible.
With the progression of the pathology, manifestations of dysfunction of the gastrointestinal tract join:
- heartburn;
- belching;
- flatulence;
- abdominal pain;
- constipation.
In the third stage of diastasis, patients are faced with the formation of hernias, which are formed due to structural defects in the white line. Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Causes of diastasis recti
Increase the risk of developing diastasis pathology of the connective tissue and increased pressure in the abdominal cavity. In different categories of patients, the causes of the development of PMSD are different.
Divergence of muscles in children is due to the failure of the musculature and tendons. After 2-12 months after birth, the muscles come into tone, the ligaments and tendons are strengthened - the process resolves itself. In premature babies and infants with intrauterine developmental pathologies, this may take longer. With Down syndrome, there is a risk of maintaining diastasis for life.
Pregnancy is the provocateur of diastasis of the rectus abdominis muscles in women. The growing uterus puts considerable pressure on the linea alba, stretching it. Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
In men, BMD is often provoked by obesity, physical activity and hereditary collagenopathies. The risk of diastasis increases with a tendency to constipation, as well as with chronic respiratory diseases accompanied by coughing.
Treatment of pathology by conservative methods is possible with a small diastasis. At the later stages of development, the pathological divergence of muscles is eliminated with the help of abdominal plastic surgery.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health.
You can find out more about the disease, prices for treatment and sign up for a consultation with a specialist by phone:
+7 (495) 292-39-72
Request a call back Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical recommendations
2
A comprehensive assessment of the nature of the disease and treatment forecast
3
Modern diagnostic equipment and own laboratory
4
High level of service and weighted pricing policy
Diagnosis of diastasis of the rectus abdominis muscles
Identification of BPMD is not difficult, since the disease has characteristic clinical manifestations. With signs of diastasis, you should contact the surgeon.
With signs of diastasis, you should contact the surgeon.
An increase in the space between the rectus muscles is determined during palpation of the abdomen. To conduct the test, the patient is asked to lie on his back, legs slightly bent at the knees, and then tighten the abdominal muscles, raising his head and shoulder blades. In patients with obesity, the doctor is not always able to fully explore the width of the white line.
The exact size of the stretch is determined by ultrasound. This diagnostic method also allows you to detect complications (hernia, displacement of internal organs). In order to differentiate the symptoms of diastasis and manifestations of chronic diseases of the gastrointestinal tract or the genitourinary system, consultations of specialized specialists are prescribed.
Expert opinion
Surgeons warn that diastasis rectus abdominis is asymptomatic for a long time. Therefore, in the presence of predisposing factors (recent pregnancy and childbirth, chronic constipation, obesity) or non-specific complaints, you should independently feel the white line of the abdomen in the navel. If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
Egiev Valery Nikolaevich, surgeon, oncologist, doctor of medical sciences, professor, head of the Department of Surgery and Oncology, FPC MR MI RUDN University
Treatment of diastasis recti
Functional diastasis in newborns and puerperas does not require treatment. Doctors use expectant tactics, recommend adhering to the principles of rational nutrition, doing massages, and doing gymnastics. The observation period can last up to 12 months. If after this time the problem persists, the surgeon decides on an operative method of correction.
Conservative treatment
Patients are prescribed a diet to prevent constipation and excessive gas formation, as well as to gradually reduce weight. In the postpartum period, incl. after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
Surgical treatment of diastasis of the rectus abdominis muscles
In case of complicated and uncomplicated diastasis of the rectus abdominis muscles of the 2-3rd degree, surgical treatment is indicated. It is possible to use the following techniques of the operation:
- Tension plasty using own tissues. It involves stitching the edges of the muscles with the removal of excess connective tissue.
 To date, it is not used due to the high risk of recurrence.
To date, it is not used due to the high risk of recurrence. - Tension-free repair with a mesh prosthesis. It implies the introduction of an endoprosthesis under the site of stretching.
- Tension plasty with prosthesis installation. It involves the removal of excess connective tissue, suturing the edges of the muscles and strengthening the zone with a polypropylene mesh.
- Combined technology. Includes muscle suturing, mesh strengthening, removal of excess adipose tissue and stretched skin.
Prevention
To reduce the risk of developing diastasis rectus abdominis, you should keep your body in shape - engage in regular exercise, train your muscles. However, do not overdo it: lifting weights can, on the contrary, become the main cause of muscle divergence.
It is also important to eat a complete and balanced diet - a lack of nutrients will lead to a decrease in the elasticity of the connective tissue.
It is necessary to control your weight - body mass index should not exceed 26 kg/m3. Obesity, especially of the abdominal type, is an important risk factor for BLV.
Obesity, especially of the abdominal type, is an important risk factor for BLV.
Prevention and timely treatment of chronic lung diseases accompanied by cough, pathologies of the digestive system, occurring with constipation, will reduce the possibility of increasing intra-abdominal pressure and, as a result, the likelihood of diastasis.
Rehabilitation after surgery
After surgery, the patient is under inpatient observation, receiving analgesic and antibiotic therapy. Full recovery lasts 1-3 months. During this period, the patient is prescribed a diet to normalize defecation, it is recommended to avoid significant physical exertion, weight lifting. To prevent excess tension, it is necessary to wear a bandage.
Questions and answers
A surgeon deals with the treatment of pathology.
In the stronger sex, obesity and connective tissue dysplasia are considered to be the main cause of BMD. Sharp weight loss or weight gain, excessive passion for power loads are capable of provoking muscle divergence. If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
There is no need to rush in this matter. Just the desire to quickly get in shape is the main reason for the progression of diastasis in women. Physical activity can be resumed 1-2 months after delivery. You can start with hiking or yoga. Abdominal exercises can be performed soon after the white line is reduced to 2 cm. It is advisable to pay attention to the diet. A smooth decrease in weight and volume of visceral fat will ensure gradual and timely muscle contraction. Sharp weight loss, on the contrary, can increase diastasis.
You can lie on a hard surface on your back, tense your abs. With gentle movements of the fingers, you should begin to probe the stomach in the middle in the navel. With a normal width of the white line and with diastasis, a depression will be found - this is the median ligament. If its width is equal to or greater than the width of two fingers, you should contact the surgeon. Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Pathogenesis and treatment of ventral hernias and diastasis of the rectus abdominis muscles: Abstract of the thesis / Zagirov U.Z. - 1995.
Comparative aspects of methods for eliminating diastasis of the rectus abdominis muscles / Topchiev MA, Bondarev VA, Elderov S.Sh.// Astrakhan medical journal. - 2010.
Jessen M. L., Öberg S., Rosenberg J. Treatment Options for Abdominal Rectus Diastasis // Front Surg. - 2019. - No. 6. - R. 65
>
Diseases referred by the Surgeon
Appendicitis Ascites Atheroma femoral hernia Crohn's disease Bursitis Hernia Hernia of the white line of the abdomen hiatal hernia Cholelithiasis Keratoma salivary gland cyst Lipoma Bowel obstruction Oleogranuloma kidney tumor Acute pancreatitis Inguinal hernia Peritonitis Barrett's esophagus Polycystic kidney disease Postoperative hernia Umbilical hernia Heel spur Stomach cancer Reflux esophagitis (GERD) Thyroiditis Furuncle (boil) Furunculosis Cholecystitis Peptic ulcer of the stomach and duodenum
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, 57, pp.