Placenta previa marginalis
Placenta Previa: Symptoms, Causes & Treatments
Overview
With placenta previa, the placenta covers all or part of the cervix.What is placenta previa?
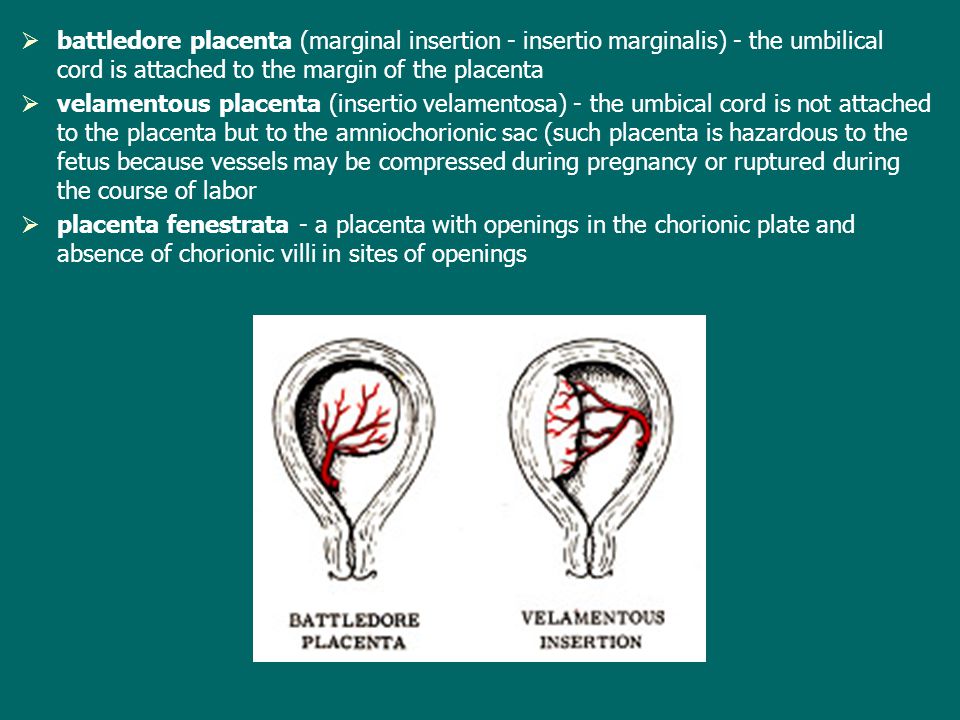
Placenta previa is a condition when the placenta blocks all or part of your cervix in the last months of pregnancy. The placenta develops in your uterus during pregnancy. It’s a sac-like organ that supplies oxygen and nutrients to the fetus through the umbilical cord.
The placenta stretches and grows through pregnancy. It’s common for it to be low in your uterus in early pregnancy. In the third trimester (weeks 28 to 40 of pregnancy), the placenta should move to the top of your uterus. This happens so your baby has a clear path to the vagina for delivery. Placenta previa occurs when the placenta doesn’t move to the top of your uterus. This means the placenta is blocking your baby’s exit from your vagina.
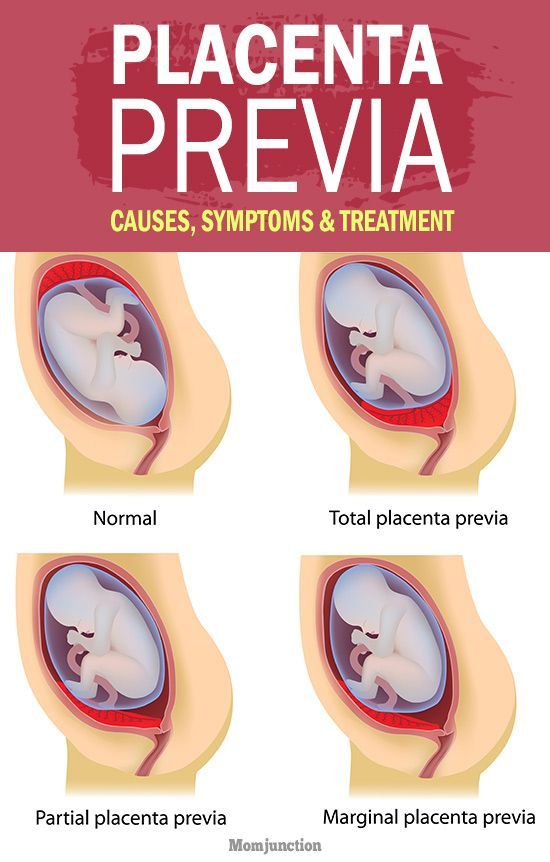
What are the types of placenta previa?
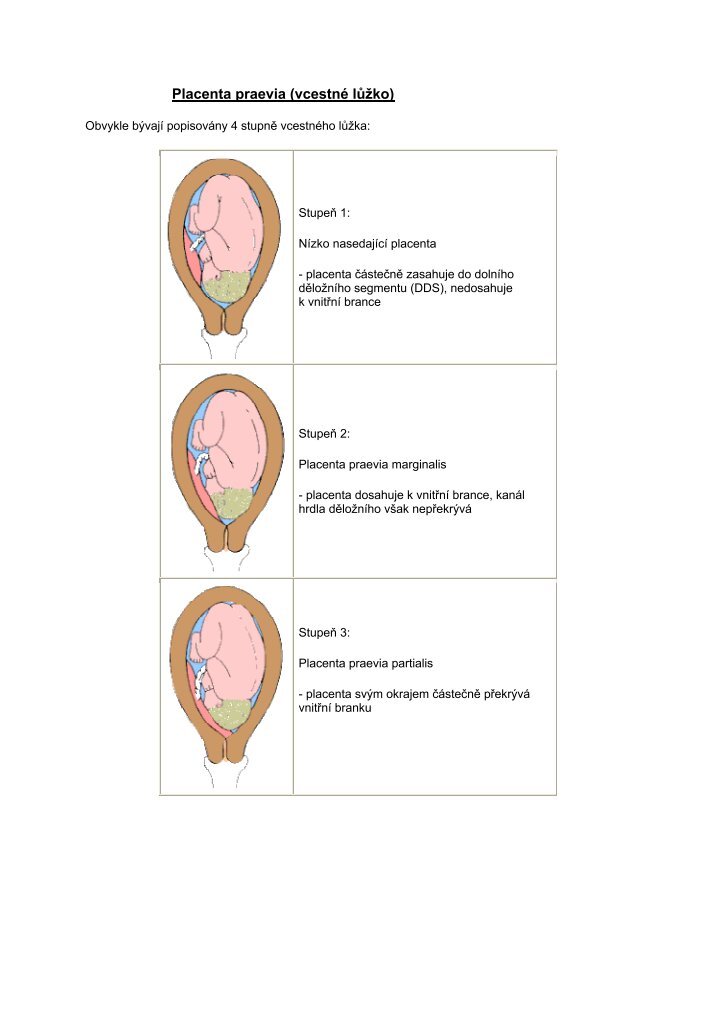
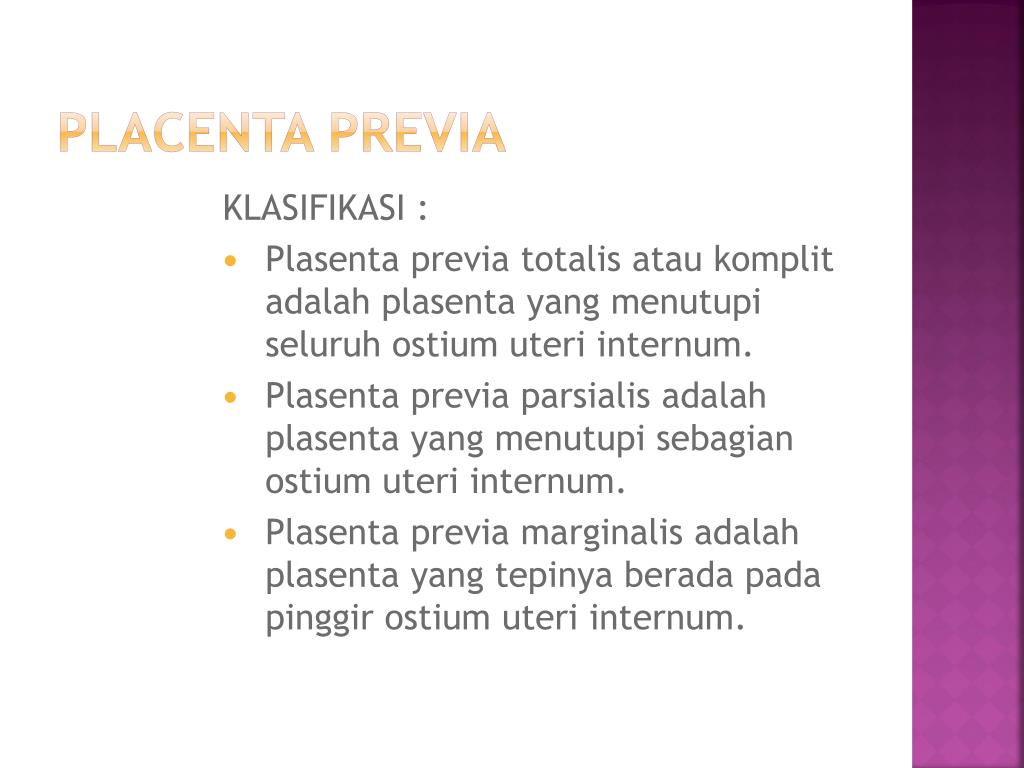
There are several types of placenta previa:
- Marginal placenta previa: The placenta is positioned at the edge of your cervix.
It’s touching your cervix, but not covering it. This type of placenta previa is more likely to resolve on its own before your baby’s due date.
- Partial placenta previa: The placenta partially covers your cervix.
- Complete or total placenta previa: The placenta is completely covering your cervix, blocking your vagina. This type of placenta previa is less likely to correct itself.
Each type of placenta previa can cause vaginal bleeding during pregnancy and labor. Due to the high risk of bleeding, most people will require a Caesarean (C-section) delivery.
How common is placenta previa?
Placenta previa occurs in about 1 in 200 pregnancies. Pregnancy care providers usually diagnose it in the second trimester during an ultrasound.
What is the difference between placenta previa and placental abruption?
In placenta previa, the placenta is covering all or part of your cervix. Even though the placenta is in a complicated position, it’s still attached to your uterus.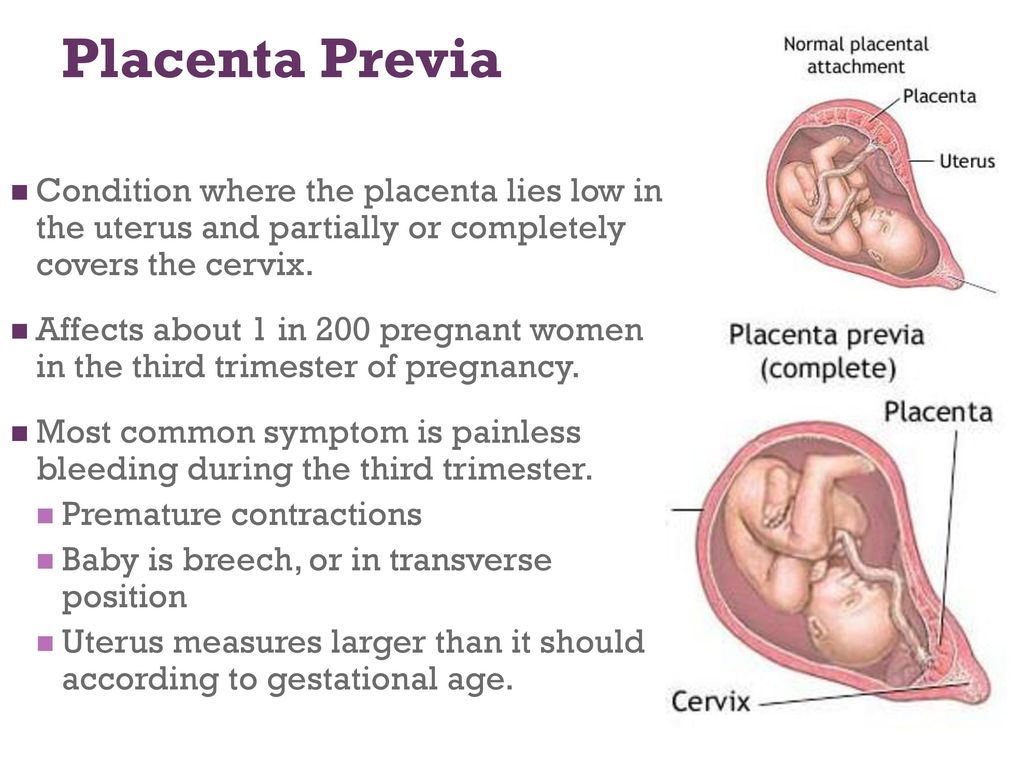 A placental abruption is when the placenta detaches from your uterus. Both conditions can cause vaginal bleeding during pregnancy and labor.
A placental abruption is when the placenta detaches from your uterus. Both conditions can cause vaginal bleeding during pregnancy and labor.
Is placenta previa the same as anterior placenta?
Placenta previa isn’t the same as anterior placenta. Your placenta can grow anywhere in your uterus. An anterior placement of the placenta means the placenta has implanted in the front of your body. Think of anterior placenta as a pillow between your baby and your stomach.
Symptoms and Causes
What are the symptoms of placenta previa?
The most common symptoms of placenta previa are:
- Bright red bleeding from your vagina. The bleeding often starts near the second half of pregnancy. It can also start, stop, then start again a few days later.
- Mild cramping or contractions in your abdomen, belly or back.
The amount of vaginal bleeding can vary and is often not accompanied by any pain.
What causes placenta previa?
There isn’t a known cause of placenta previa.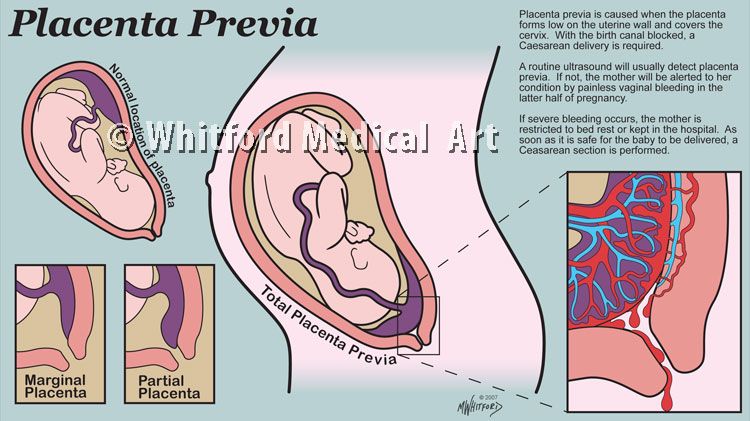 There are some factors that can increase your risk of developing placenta previa, including your medical history and certain lifestyle habits.
There are some factors that can increase your risk of developing placenta previa, including your medical history and certain lifestyle habits.
What are the risk factors for developing placenta previa?
There are several factors that increase your risk for placenta previa during pregnancy:
- You smoke cigarettes or use cocaine.
- You’re 35 or older.
- You’ve been pregnant several times before.
- You’re pregnant with twins, triplets or more.
- You’ve had surgery on your uterus, including a C-section or a D&C (dilation and curettage).
- You have a history of uterine fibroids.
What are possible complications of placenta previa?
If you have placenta previa, there are risks for both you and your baby. Complications from placenta previa include:
For you:
- Bleeding: Severe bleeding can occur during pregnancy, labor or delivery.
- Early birth: If you’re bleeding severely, your healthcare provider may perform an emergency C-section before your baby is full term (40 weeks).

- Blood loss: Anemia, low blood pressure, pale skin or shortness of breath are all side effects of losing too much blood.
- Placenta accreta: The placenta grows too deeply in the wall of your uterus. This can cause severe bleeding after delivery.
- Placental abruption: The placenta separates from your uterus before your baby is born. This decreases your baby’s supply of oxygen and nutrients.
For baby:
- Premature birth: If your bleeding is severe and you need an emergency C-section, your baby may be born too early.
- Low birth weight: Trouble staying warm and poor weight gain are potential side effects of low birth weight.
- Respiratory issues: Underdeveloped lungs could make breathing more difficult.
Can you have placenta previa without bleeding?
Yes, it’s possible to have placenta previa and not experience vaginal bleeding. You could have mild cramping or pain in your pelvic region or back. It’s best to discuss any bleeding or pelvic pain you have with your healthcare provider.
You could have mild cramping or pain in your pelvic region or back. It’s best to discuss any bleeding or pelvic pain you have with your healthcare provider.
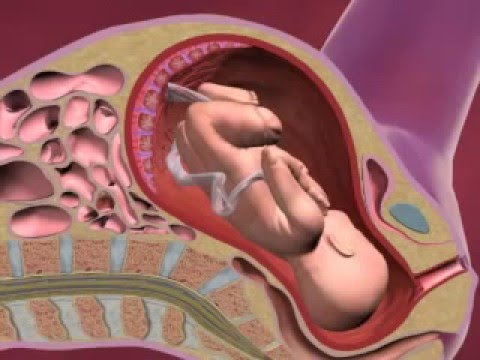
Why do you bleed when you have placenta previa?
There are two main reasons you bleed if you have placenta previa. They have to do with how your body prepares for labor.
- Your cervix is the opening from uterus to your vagina. As pregnancy progresses in the third trimester, your cervix thins (effaces) and spreads to prepare for birth. If your placenta is touching or covering your cervix, this thinning will cause you to bleed.
- During labor, your cervix opens (dilates) in order to allow the baby to exit your uterus and descend down your vagina. When your cervix opens, the blood vessels connecting the placenta to your uterus are torn and can cause bleeding.
Can placenta previa cause a miscarriage?
Miscarriage occurs when you experience a loss of pregnancy before 20 weeks. Pregnancy care providers don’t typically diagnose placenta previa until around or after the 20th week of pregnancy.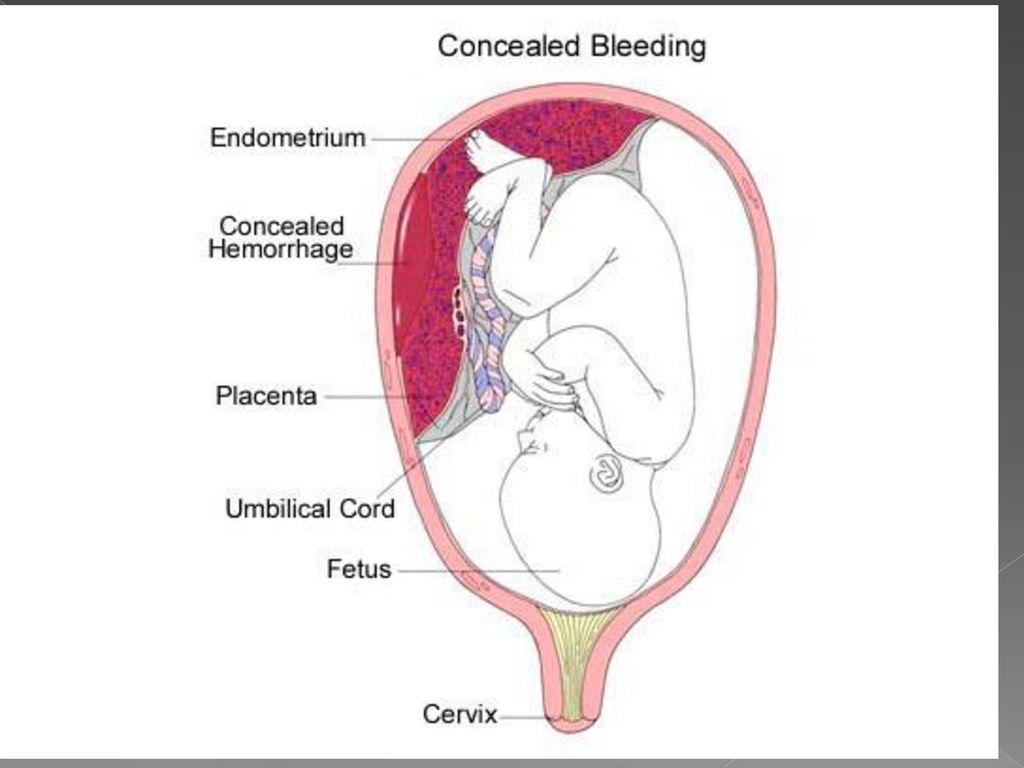 It’s uncommon that placenta previa would be the cause of a miscarriage.
It’s uncommon that placenta previa would be the cause of a miscarriage.
Diagnosis and Tests
How is placenta previa diagnosed?
Pregnancy care providers usually identify placenta previa in a routine ultrasound around 20 weeks of pregnancy. It’s sometimes found when a person experiences symptoms of placenta previa like vaginal bleeding. Your provider will recommend ultrasounds to monitor the placement of the placenta for the remainder of your pregnancy.
What tests are used to diagnose placenta previa?
Your healthcare provider will diagnose placenta previa using ultrasounds that show the inside of the female reproductive system:
- Vaginal ultrasound (or transvaginal ultrasound): Your provider places a wand-like device (a transducer) into your vagina to check the position of your baby, the placenta and your cervix.
- Abdominal ultrasound: Your provider places gel on your abdomen, then moves a handheld device (the transducer) around the outside of your belly.
 This can also show the position of your baby, the placenta and your cervix.
This can also show the position of your baby, the placenta and your cervix.
Both types of ultrasound show the images on a monitor or screen. Your pregnancy care provider will determine how much of your cervix is covered by the placenta and recommend treatment.
Management and Treatment
How is placenta previa treated?
The goal is to get you as close to your due date as possible. Delivering via C-section is often the safest treatment if bleeding continues. Treatment of placenta previa depends on:
- How severely you’re bleeding.
- The gestational age of your baby.
- The position of the placenta and your baby.
- The health of you and your baby.
If your provider finds placenta previa early in your second trimester, it can get better on its own. The position of the placenta can change as your uterus expands to accommodate the growing baby. There is often less of a chance that the placenta will move higher in your uterus if your provider diagnoses you with the condition later in pregnancy.
If the placenta is near or covering just part of the cervix and you’re not bleeding, your healthcare provider may recommend:
- Reducing strenuous activities like running, lifting and exercising.
- Bed rest at home.
- No sexual intercourse, tampons or douching.
- More frequent prenatal appointments and ultrasounds.
For moderate to severe cases of placenta previa or frequent bleeding, other treatments could include:
- Bed rest in the hospital.
- Medicine to prevent early labor.
- Steroid shots to help the baby's lungs develop faster.
- Blood transfusions if you experience heavy bleeding.
- An emergency C-section for heavy, uncontrolled bleeding.
Does placenta previa go away?
Placenta previa can go away on its own if it’s found in the second trimester. Going away on its own means the placenta shifts upwards to the top of your uterus. As your uterus expands in the third trimester, the placenta may still move. The later in the pregnancy it remains covering the cervix, the less likely it is to go away. Your healthcare provider will monitor the position of the placenta to see if the condition has resolved before delivery.
The later in the pregnancy it remains covering the cervix, the less likely it is to go away. Your healthcare provider will monitor the position of the placenta to see if the condition has resolved before delivery.
Prevention
Can I reduce my risk for placenta previa?
There is nothing you can do to prevent placenta previa and no surgical or medical procedure can correct it. There are certain risk factors for placenta previa that are within your control, like not smoking or using cocaine. Once your provider diagnoses the condition, there are ways to reduce the amount of vaginal bleeding.
Outlook / Prognosis
What can I expect if I have placenta previa?
Your treatment will be unique to your condition. Most people can expect:
- Frequent monitoring through the second and third trimester. Your provider does this to check the position of the placenta and watch for any changes in symptoms.
- Modified or restricted physical activities like exercise and sex.
- Blood tests post-delivery to check your blood counts.
Will my baby be born early if I have placenta previa?
Maybe. Your healthcare provider will consider the amount of bleeding, the position of the placenta and the baby’s gestational age before deciding if an early delivery is necessary. Around 36 weeks of pregnancy, the best option for the health of you and your baby could be an early delivery. Other times a person reaches full term or 40 weeks of pregnancy.
Can I still have a vaginal delivery with placenta previa?
If you have a marginal placenta previa (the placenta is close to your cervix, but not covering it), your healthcare provider may be able to deliver your baby vaginally. This carries a risk of bleeding and may be too dangerous. Your provider will discuss the safest way to deliver your baby.
Will I need a C-section if I’m diagnosed with placenta previa?
A C-section is usually the safest delivery option if you have placenta previa.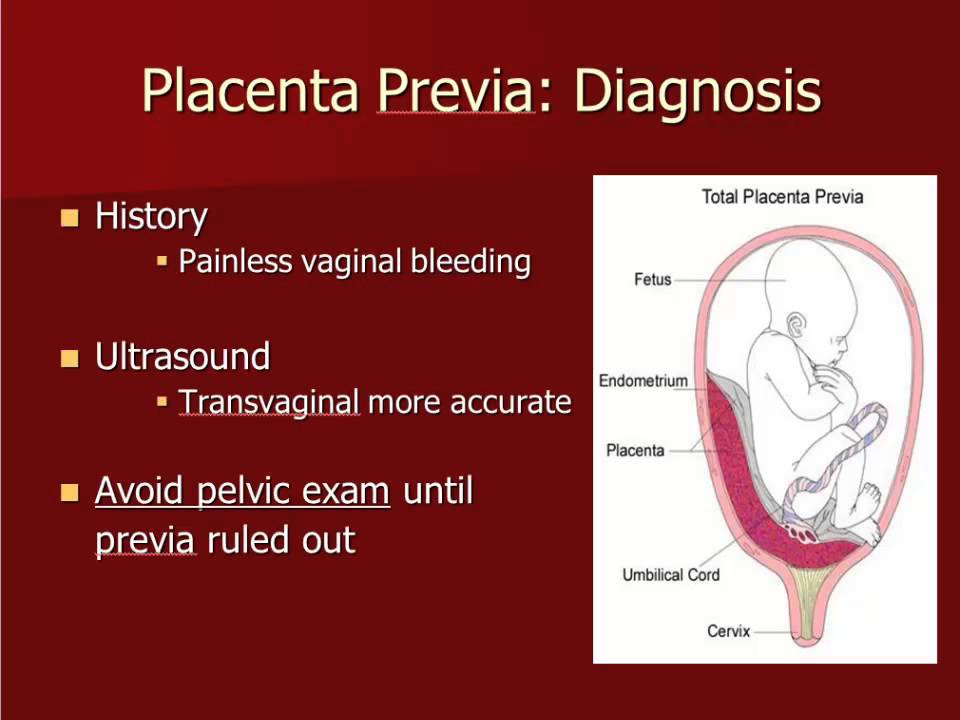 If the placenta covers even a part of your cervix, a vaginal delivery can cause severe bleeding. Your provider will typically schedule your C-section in advance, but if your bleeding is too severe at any time, you may need an emergency C-section.
If the placenta covers even a part of your cervix, a vaginal delivery can cause severe bleeding. Your provider will typically schedule your C-section in advance, but if your bleeding is too severe at any time, you may need an emergency C-section.
Can placenta previa cause birth defects?
It’s uncommon for placenta previa to cause birth defects. Your baby may be born premature if your healthcare provider feels it’s the safest time to deliver. Premature birth carries some complications such as low birth weight and respiratory problems.
Will I get placenta previa again?
If you’ve had placenta previa in a past pregnancy, your chances of having it again are around 2%. If you become pregnant, let your healthcare provider know so that they’re aware of your medical history.
Will placenta previa affect my fertility?
Placenta previa doesn’t impact your chances of getting pregnant again. You’ll have a small risk of getting placenta previa again if you become pregnant.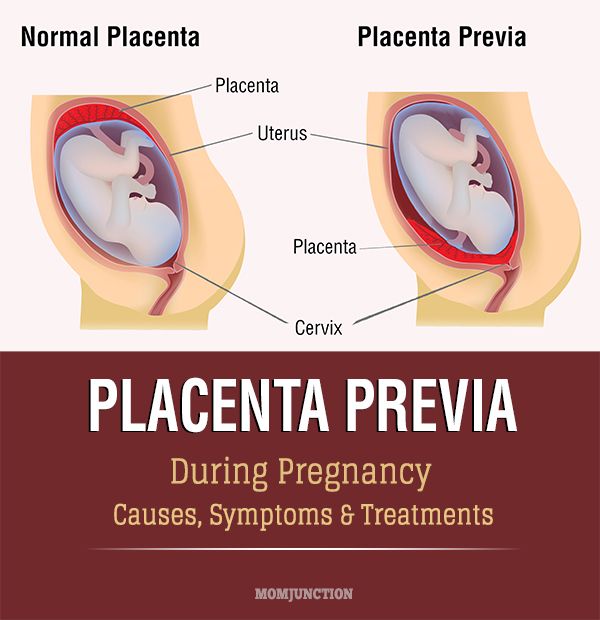
What questions should I ask my doctor?
Your healthcare provider should be able to answer your questions and prepare you for treatment of placenta previa. Here are some questions you might ask:
- Is the baby’s life in danger? Is mine?
- What are my treatment options?
- How will I know if my placenta previa goes away?
- Should I limit certain activities?
- Can the baby be born now?
- What are potential complications?
- Will I need additional ultrasounds or tests?
- What are the signs that I need to go to the hospital?
What questions will my doctor ask me?
- When did you first notice bleeding?
- How heavy is the bleeding?
- Is bleeding constant or does it come and go?
- Do you have any pelvic pain?
- Have you had pregnancy complications before?
- Have you had uterine surgeries?
- Do you smoke or use cocaine?
- Is there someone to care for you if bed rest is required?
Living With
When should I see my healthcare provider?
Call your healthcare provider immediately if you’re bleeding, cramping or experiencing pelvic pain during your pregnancy, especially in the second half of pregnancy.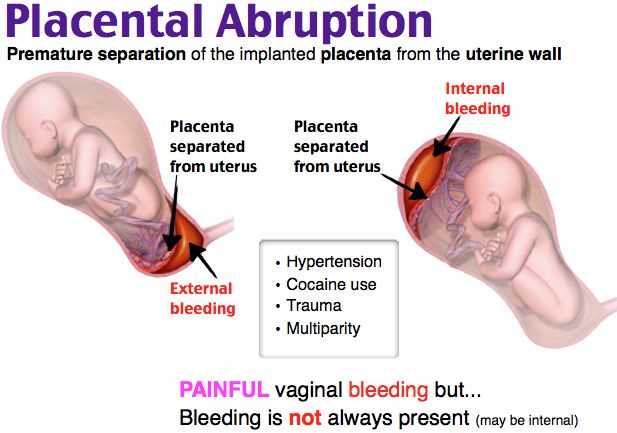
When should I go to the ER?
If you’re experiencing severe blood loss, you should seek emergency medical care immediately. Major blood loss carries several serious side effects to both you and your baby.
Can I exercise with placenta previa?
Your healthcare provider will likely advise you to limit certain activities like exercise, squatting, jumping and lifting. These activities could cause bleeding. It's best to discuss your day-to-day activities with your provider so they can suggest modifications as necessary.
Can I have sex if I have placenta previa?
Most healthcare providers will advise against having sexual intercourse if you have placenta previa. It’s best to avoid any activities that can trigger bleeding or contractions, like using tampons, douching or inserting anything into your vagina.
A note from Cleveland Clinic:
Placenta previa is a treatable condition where most people go on to deliver healthy babies. You’re likely to have a safe delivery if you follow the guidance of your pregnancy care provider. Don’t be afraid to speak up if you experience any bleeding or discomfort during your pregnancy.
Don’t be afraid to speak up if you experience any bleeding or discomfort during your pregnancy.
Marginal Placenta Previa • Sonosession
US image, exam type “Obstetrics”, preset “General”This patient returned for a follow up ultrasound exam (CPT 76815) for a low lying placenta identified on her 20 wk growth and anatomy scan. She is G3P2 and currently 30w3d.
When performing a follow up ultrasound exam, it is always important to begin with fetal presentation. As we reviewed in class, when you know the fetal lie then you know how to manipulate your probe to find what you are looking for. Here you can see that the baby is in a cephalic presentation.
The image above is a sagittal slice. Remember the notch is facing mom’s head and therefore the left side of the screen is superior (toward mom’s head) and the right side is inferior (toward mom’s feet).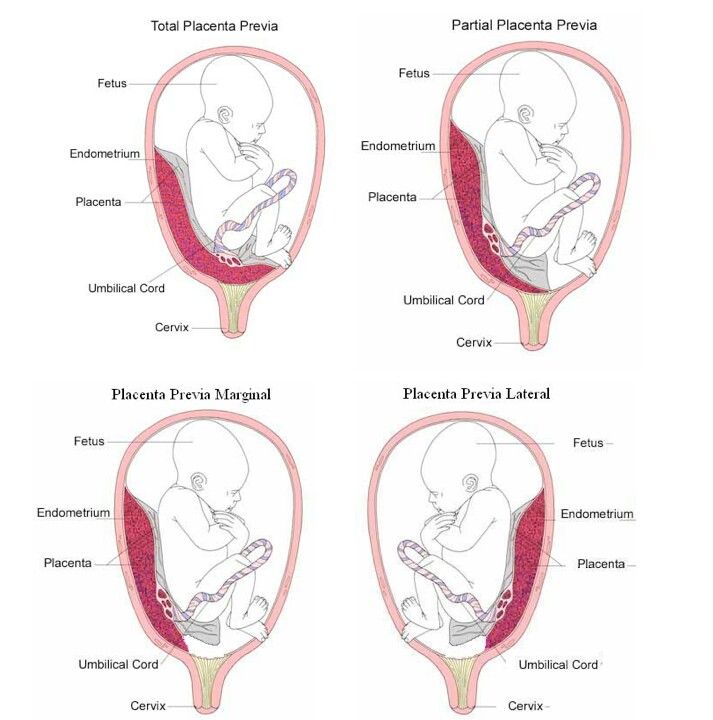
The next thing I do is look for a beating heart. Establishing viability is a requirement anytime you perform an ultrasound on a pregnant woman. Even if it is a limited exam for previa or checking the fluid, you must confirm fetal viability. You can confirm viability multiple ways. You can use m-mode, pulse wave Doppler, or cine clip. It isn’t required to get a fetal heart rate, just confirm that the fetus is alive. The practitioner used PW Doppler and did get a fetal heart rate of 146 bpm.
US image, pulse wave DopplerThese next two images are of the posterior placenta. The reason for this exam is to follow up the low lying placenta that was identified on the anatomy scan.
US image, posterior placenta image in longitudinal planeUS image, posterior placenta in transverse plane
When evaluating the placenta, it is important to image it in two planes. The transverse plane will identify location.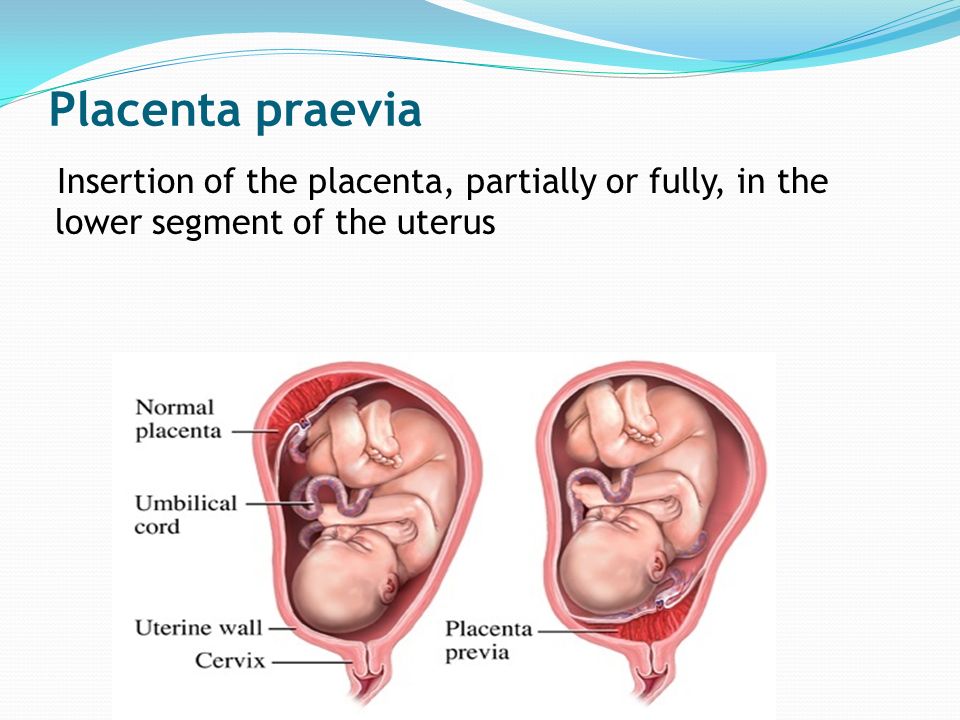 Note the image on the left. You can see that there is placenta above and below. That is because this placenta is posterior maternal right. The transverse plane will give you information on the location of the placenta within the uterus but the sagittal plane with tell you the location of the placenta in relation to the cervix.
Note the image on the left. You can see that there is placenta above and below. That is because this placenta is posterior maternal right. The transverse plane will give you information on the location of the placenta within the uterus but the sagittal plane with tell you the location of the placenta in relation to the cervix.
You can see a longitudinal slice of the cervix and the posterior placenta adjacent to it. The cervical canal is visible as well.
When measuring the cervix transabdominally, remember to have the bladder as empty as possible. This may seem counterintuitive because a full bladder helps us see better. However, a full bladder can artificially elongate the cervix. Here you can see an empty bladder and a long closed cervix measuring 4.2 cm.
The most effective way to confirm a placenta previa is to look transvaginally. Below you will see images of a transvaginal approach.
Below you will see images of a transvaginal approach.
US image, transvaginal approach, cervix and placenta
Below you will see a measurement from the edge of the placenta to the internal os. The bright echos to the left of the screen are the fetal skull. You can see that the measurement from the tip of the placenta to the internal os is only 6 mm. Historically, there have been three defined types of previa: complete, marginal and partial. Currently, these have been consolidated into two definitions: complete and marginal. A complete previa completely covers the internal os. A marginal previa is defined by distance of less than 2 cm from the internal os but not covering it.
US image, measurement of the distance between the placental edge and internal cervical osIt is also critical to investigate for vasa previa. This dangerous condition can be identified with color Doppler. Place the color box over the internal os and make sure the gain is turn up enough to identify color.
In closing, the best time to look for placenta location is during the growth and anatomy scan. During this time there is plenty of room to fully evaluate the placenta. This exam will prompt you to either clear the placenta or schedule a follow up to evaluate if it is indeed covering the cervix or if it is low lying. A posterior placenta can be challenging to evaluate in the third trimester. A transvaginal approach is the method of choice when a complete or marginal previa are suspected.
Imaging of placenta previa | Blog RH
By Greg Marrinan
Review
Placenta previa (PP) occurs in 0.3-2.0% of all pregnancies. As the age of the mother increases, the risk of this condition increases.
Placenta previa is a condition in which placental tissue is abnormally close to the inside of the cervix. There are 4 generally recognized subtypes of PP:
- Complete or central, in which the placenta completely covers the internal os of the uterus;
- Incomplete or partial, in which the placenta partially covers the internal os of the uterus;
- Marginal, in which placental tissue adheres to, but does not cover, the internal os of the uterus;
- A low-lying placenta that is abnormally close to the internal uterine os but does not cover it at all.

The reported incidence of placenta previa in the second trimester is almost 10 times higher than during childbirth. The most likely theory of this phenomenon suggests that in the third trimester the lower segment of the uterus lengthens faster than the placenta increases. Thus, a placenta that appears marginal or low-lying at 20 weeks may be normal as the due date approaches. However, the results of most studies of this phenomenon indicate that a complete placenta previa in the second trimester rarely returns to its normal position at term.
Magnetic resonance imaging
Usually the placenta is relatively homogeneous. Its signal intensity on T1-weighted images is low and slightly higher than that of the myometrium. On T2-weighted images, the placental tissue has a high signal intensity and can be clearly distinguished from the adjacent fetus, uterus, and cervix. Sagittal images best demonstrate the position of the placenta in relation to the internal uterine os.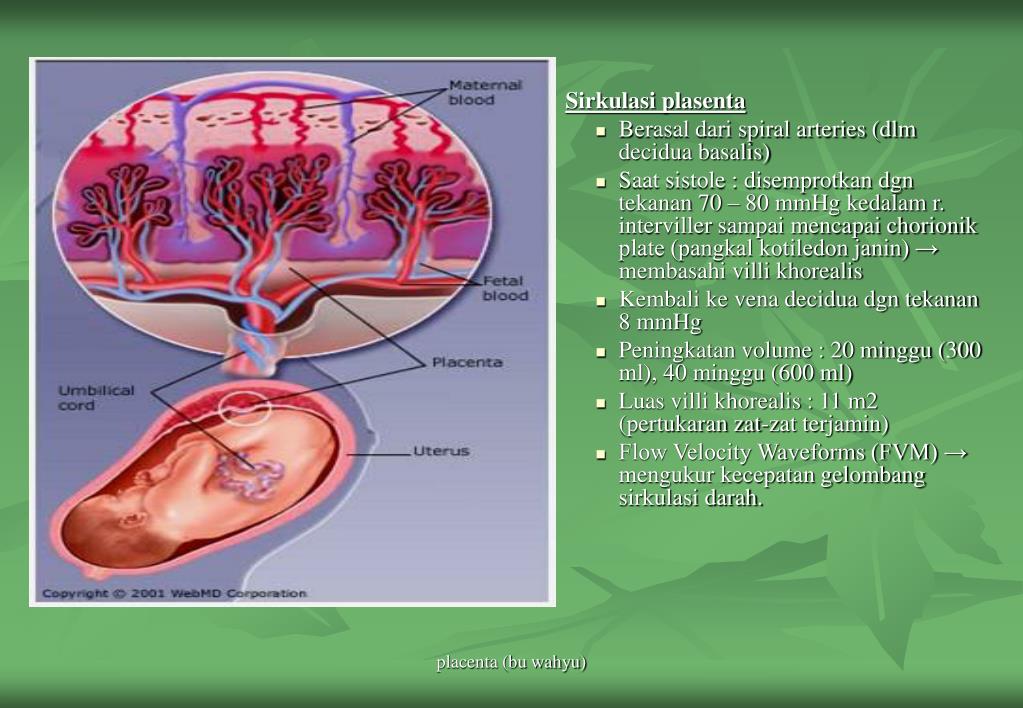 Sometimes endometrial veins can be seen at the edges of the placenta.
Sometimes endometrial veins can be seen at the edges of the placenta.
Normal physiological placental calcifications that occur during late pregnancy are usually not seen on MRI.
Placenta previa is diagnosed when placental tissue is found to cover all or part of the internal uterine os.
Figure 1 : Sagittal T2-weighted image (SSFSE) showing complete placenta previa at 28 weeks' gestation.
Diagnosis accuracy
No large prospective studies have been conducted to investigate the accuracy of MRI in the diagnosis of placenta previa. However, a series of images taken showed that the results are similar and perhaps slightly better than the results of ultrasound.
The author has not found any reported false negatives in the literature. False-positive results may be due to myometrial contraction in the lower uterine segment on imaging. Although the placental margin remains distinct from the contracted muscle and internal uterine os, the distance between the placental margin and the axis may decrease, leading to a false diagnosis of a low-lying placenta. In extreme cases, the edge of the placenta may come into contact with or even overlap part of the internal os of the uterus and thereby mimic placenta previa.
In extreme cases, the edge of the placenta may come into contact with or even overlap part of the internal os of the uterus and thereby mimic placenta previa.
Imaging markers
Failure to diagnose placenta previa can have serious consequences during the last trimesters and during labor. The relatively high frequency of placenta previa in the second trimester should not lead to the fact that the doctor cannot diagnose this condition. Whenever a diagnosis is suspected, further evaluation is recommended. In almost all cases, this evaluation includes a repeat ultrasound during the third trimester.
Care should be taken not to confuse a more serious situation such as placental abruption or placenta ingrowth with placenta previa because the treatment of these conditions is different. In addition, the doctor must avoid errors in the search. The possibility of one of these diagnoses complicating placenta previa should be ruled out.
The time required to organize and conduct an adequate examination may limit its usefulness, especially in the setting of acute maternal bleeding.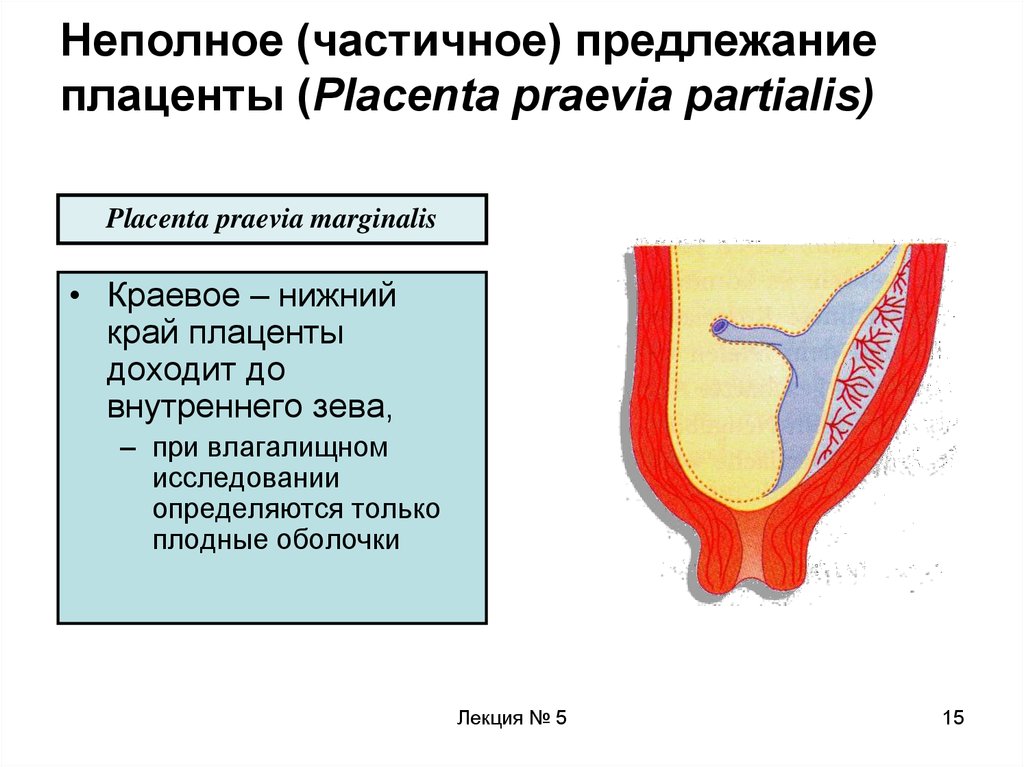
At present, the use of MRI to diagnose placenta previa should be limited to a few specific cases, and MRI should be used only after ultrasound has not provided adequate information.
Ultrasound diagnostics
If the internal uterine os can be visualized and if the placental tissue does not overlap it, placenta previa is ruled out. However, an attempt must be made to determine the lowest edge of the placenta and determine the distance between it and the internal axis. When the fetal head obscures the posterior placenta, or when the inferior border of the placenta is not visualized by transabdominal imaging, a transvaginal or transrectal approach is almost always adequate to reveal its position.
Figure 2 : Longitudinal transabdominal sonogram showing complete symmetrical placenta previa.
Figure 3 : Ultrasound shows an asymmetric complete placenta previa.
Figure 4 : Longitudinal sonogram of the same patient shows that her findings are not due to an overdistended bladder, but to true placenta previa.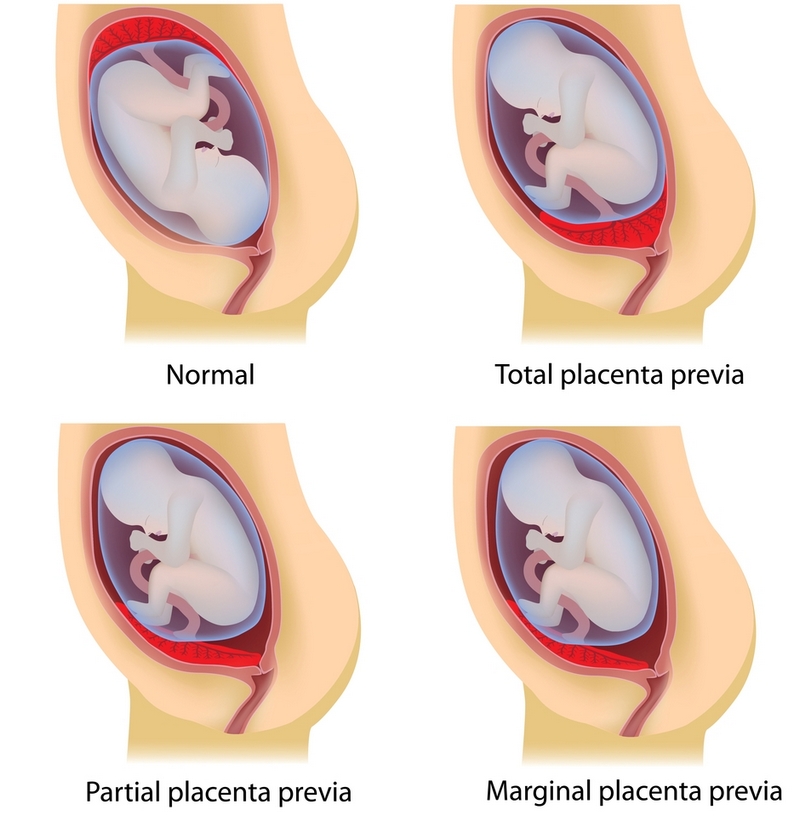
Although diagnostic criteria may vary from institution to institution, any of the following results exclude placenta previa:
- direct superposition of fetal presenting and cervix with no space for inserted tissue;
- presence of amniotic fluid between the presenting part of the fetus and the cervix, without the presence of placental tissue;
- Distance greater than 2 cm between the lower part of the placenta and the inside of the uterine os on direct visualization.
The conditions most commonly misdiagnosed as placenta previa are bladder overfilling and myometrial contraction. Excessive expansion of the mother's bladder creates pressure on the anterior part of the lower uterine segment, compressing it against the posterior wall and causing the cervix to lengthen. Thus, a normal placenta may underlie the internal os. The cervix should be no longer than 3-3.5 cm during the third trimester. If the cervix is greater than 3.5 cm, or if a dilated cervix is suspected, further imaging should be performed after the patient has emptied the bladder.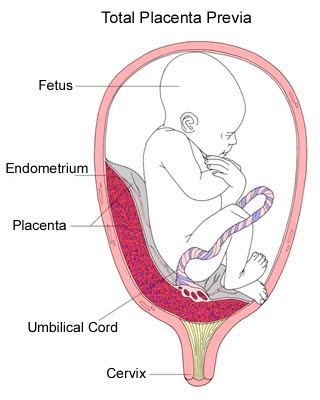 Because transvaginal imaging is performed when the patient's bladder is empty, this trap should very rarely occur.
Because transvaginal imaging is performed when the patient's bladder is empty, this trap should very rarely occur.
During myometrial contraction, two situations can occur that mimic placenta previa: first, the uterine wall can thicken and mimic placental tissue. Second, the lower uterine segment can shorten and bring the lower edge of the placenta into contact with the inside of the cervix, creating a condition that mimics placenta previa. To avoid this trap, contraction should be assumed if the myometrium is thicker than 1.5 cm. The results of a repeat imaging done 30 minutes later should be sufficient to rule out this condition.
DO YOU CARE THE ULTRASONIC MACHINE CORRECTLY?
Download the care manual now
Diagnosis accuracy
With a qualified operator, ultrasounds are more than 95% accurate. Transvaginal evaluation of the placenta has a 1% false positive rate and 2% false negative rate.
Transabdominal ultrasound is the test of choice for confirming placenta previa. The overall accuracy of ultrasound in assessing placenta previa is 93-98%. Transrectal studies have a negative predictive value of almost 100% for this diagnosis.
The overall accuracy of ultrasound in assessing placenta previa is 93-98%. Transrectal studies have a negative predictive value of almost 100% for this diagnosis.
Imaging markers
Caution should be exercised when diagnosing placenta previa in the second trimester. The condition is reported to occur 10 to 100 times more often than during the first trimester.
The likelihood of congenital anomalies and transverse positioning of the fetus is somewhat higher in patients with placenta previa than in others. Particular attention should be paid to documenting such results.
The main limitation of ultrasound in the diagnosis of placenta previa is related to gestational age at diagnosis.
Placenta previa - frwiki.wiki
This article is about human pregnancy. For other viviparous animals, see Pregnancy.
Previa is an abnormal location of the placenta may be responsible for severe bleeding during the third trimester of pregnancy.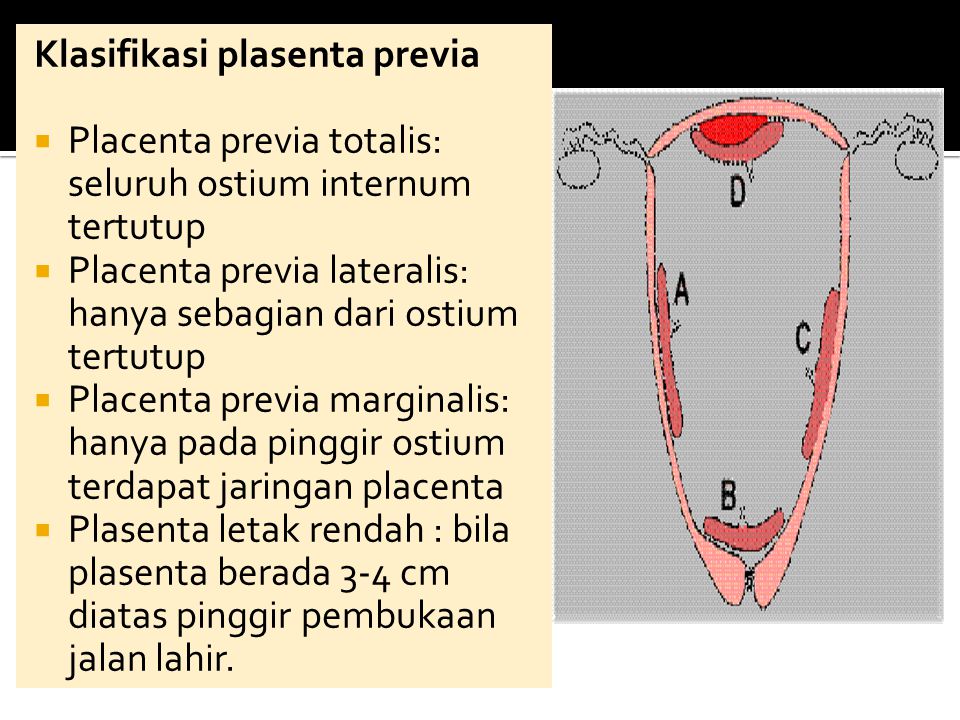 The placenta usually inserts into the top of the uterus, when it doesn't, it's called previa. Then it is located on the lower segment and can be lateral, marginal (when it is on the same level with its border with the opening of the cervix), partially covering or covering, when it is completely located above the uterus, the internal opening of the neck.
The placenta usually inserts into the top of the uterus, when it doesn't, it's called previa. Then it is located on the lower segment and can be lateral, marginal (when it is on the same level with its border with the opening of the cervix), partially covering or covering, when it is completely located above the uterus, the internal opening of the neck.
Placenta previa is promoted by malformations of the uterus, submucosal fibroids, a history of intrauterine manipulations (curettage, aspiration, abortion), scarring of the uterus (particularly by caesarean section), multiple pregnancies, advanced age of the mother, smoking, personal history of placenta previa.
Summary
- 1 Circumstances of discovery
- 2 Diagnostics
- 2.1 Differential diagnosis
- 2.1.1 Bleeding during pregnancy
- 2.1.2 Bleeding during childbirth
- 2.1 Differential diagnosis
- 3 Support
- 4 See also
- 4.1 Related articles
Circumstances of discovery
- This anatomical situation may be silent for a long time and only be detected during ultrasound, or it may manifest as metrorrhagia during pregnancy or even childbirth.
- The typical clinical picture of placenta previa is bleeding red blood, sometimes very profuse, occurring in the third trimester of pregnancy. This bleeding is painless.
- On palpation of the abdomen, the uterus is at least flexible and relaxes well between contractions. The general condition of the mother and especially blood pressure depends on the amount of blood lost.
Diagnostic
- Ultrasound will make the diagnosis first by the abdominal cavity and then by the vaginal route: this confirms the diagnosis, shows the exact position of the placenta. The distance between the inferior insertion of the placenta and the internal opening of the cervix allows the diagnosis to be made. Sometimes the placenta completely covers the internal opening of the cervix.
- Routine studies of fetal well-being will assess the effect of this bleeding on the fetus:
- fetal heart rate;
- Manning's score.
- Fetal participation in these hemorrhages was searched using the Kleihauer test.
Differential Diagnosis
Bleeding during pregnancy
- Uterine rupture
- Basal decidual hematoma or retro-placental hematoma
- Marginal decidual hematoma
- Circumvallate placenta
Bleeding during childbirth
- Uterine rupture
- Basal decidual hematoma or retro-placental hematoma
- Benckiser hemorrhage
Supported
Management mainly depends on the condition of the mother, gestational age, type of placenta, and condition of the baby.
- In the event of massive haemorrhage and/or fetal distress, emergency removal by caesarean section is necessary, with resuscitation of the mother if necessary.
- With moderate symptoms, the patient is admitted to the pathological pregnancy unit and placed on strict rest. In pregnancies up to 34 weeks, intravenous corticosteroids are suggested to accelerate fetal lung maturation (avoiding some neonatal complications, including hyaline membrane disease).
- In the case of very prematurity, blood transfusion maintains hemoglobin levels at 10 grams per deciliter and allows time for corticosteroid therapy to take effect.
- If the mother is Rh negative, anti-D gamma globulin should be given within 72 hours to prevent alloimmunization. Finally, some teams suggest tocolysis.
- At the end of these measures, if the placenta does not close, it is enough to wait for spontaneous delivery (under strict medical supervision). In the case of an overlying placenta, a caesarean section is necessary (the lower method is not possible), without the need for urgency, however, when maternal and fetal tolerance allows.
- The presence of placenta previa on a cesarean scar can lead to placental fusion. This is a situation with a high risk of bleeding during a caesarean section, sometimes requiring after conservative surgical attempts to remove the woman's uterus to stop the bleeding, this is called a hemostatic hysterectomy.
Learn more