Placenta grade 1 means
Placenta praevia | Pregnancy Birth and Baby
Placenta praevia | Pregnancy Birth and Baby beginning of content4-minute read
Listen
The placenta develops at the same time as your baby and is attached to the lining of your uterus (womb) during pregnancy. It allows for oxygen and nutrients to pass from you to your baby as well as producing hormones that support your pregnancy.
The fertilised ovum (egg) implants into the lining of your uterus and the placenta grows from there. As your pregnancy progresses and your baby and placenta increase in size, your womb expands and this affects the placenta's position. The area where the placenta is usually attached stretches upwards, moving the placenta away from your cervix.
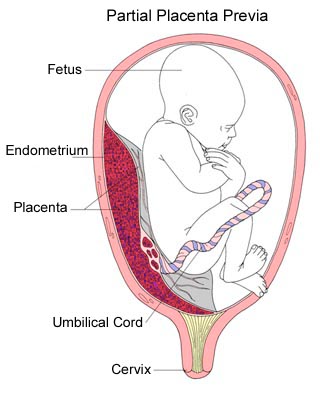
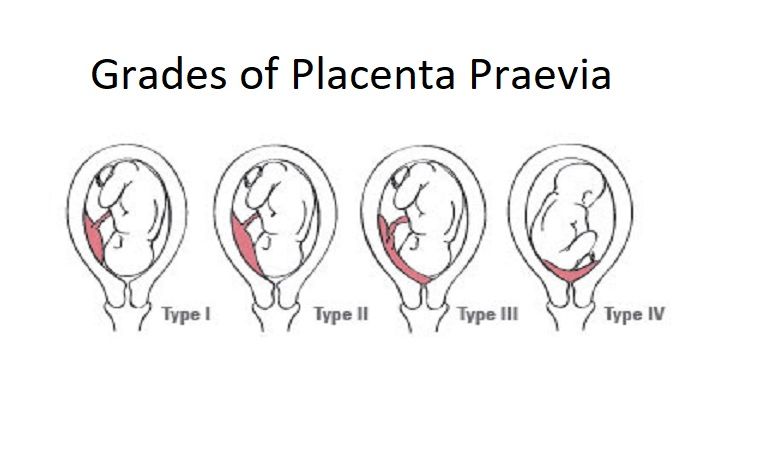
If the placenta stays low in your womb, near to or covering your cervix, it may block the baby's way out. This is called 'low-lying placenta' or 'placenta praevia'.
The position of your placenta will be recorded at your 18-22 week ultrasound scan. If your placenta is significantly low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again. For most women, the placenta will have moved into the upper part of the womb by this stage.
What causes placenta praevia?
There is no obvious cause for placenta praevia. It may be that there is a larger placenta area (such as, if you are having twins) or there could be scar tissue from a previous caesarean or curette. There are several factors that can increase your risk of placenta praevia, including having had a caesarean section in the past (especially if your last baby was born by caesarean), and older age in the mother.
There is nothing you can do to prevent placenta praevia.
Placenta praevia symptoms
Signs that the placenta could be low-lying include painless, bright red bleeding from the vagina (either spontaneously or after sex) any time after 20 weeks of pregnancy.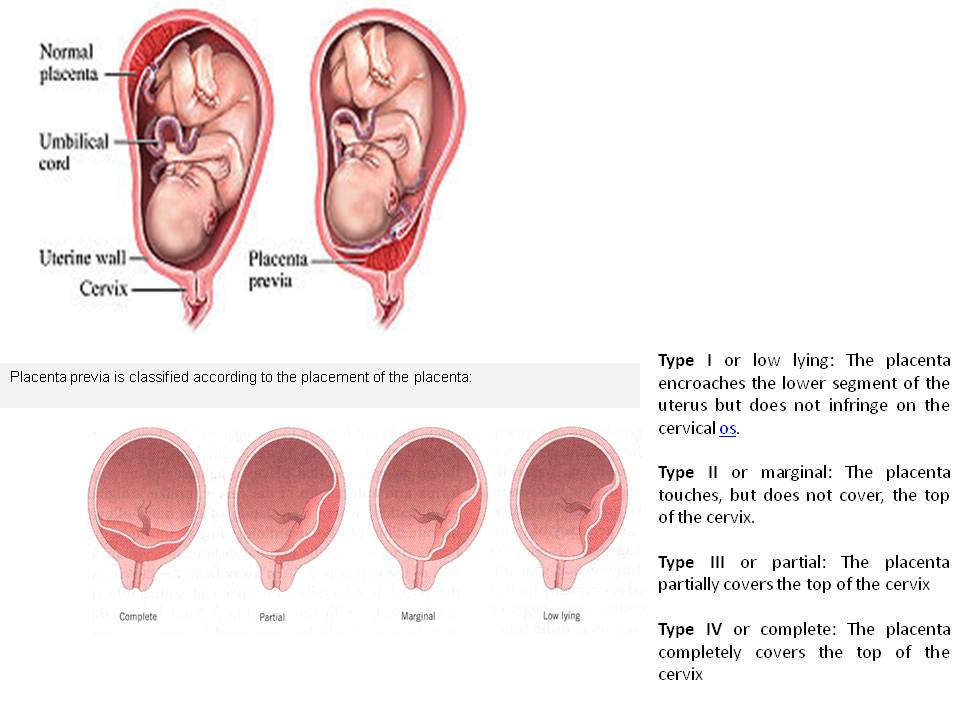 Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
You may also experience:
- cramping in your uterus with bleeding
- bleeding during labour
If you experience bleeding during your pregnancy, contact your midwife or doctor immediately.
Placenta praevia treatment
Placenta praevia is graded into 4 categories from minor to major. If you have grade 1 or 2 it may still be possible to have a vaginal birth, but grade 3 or 4 will require a caesarean section.
Any grade of placenta praevia will require you to live near or have easy access to the hospital in case you start bleeding. Heavy bleeding may mean you need to be admitted to hospital for the remainder of your pregnancy.
When you are in hospital, your blood will be taken to make sure an exact donor blood match is available in case you need a blood transfusion. You may also need to take iron tablets if you have anaemia (low blood haemoglobin level).
If you have bleeding during your pregnancy and have Rh negative blood, you will need an injection of Anti D so your baby is not affected by the bleeding.
Your baby may also be monitored with a cardiotocograph (CTG) to make sure they are not distressed. The CTG records your baby's heart rate and response to movements and contractions.
Being in hospital doesn't stop you from bleeding, but your baby can be delivered more quickly if needed. Your doctor or midwife will discuss any test results with you and what steps may be needed to ensure you and your baby's wellbeing.
As well as speaking to your doctor or midwife for advice, you can get help and information from:
- Pregnancy, Birth and Baby — call 1800 882 436 to speak to a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Australian Birth Trauma Association offers advice, resources and a peer-to-peer support service.
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.
- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AET).
Sources:
RANZCOG (Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management), Women's and Children's Health Network (Placenta praevia), March of Dimes (Placenta previa)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2019
Back To Top
Related pages
- Placenta complications in pregnancy
- About the placenta
Need more information?
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.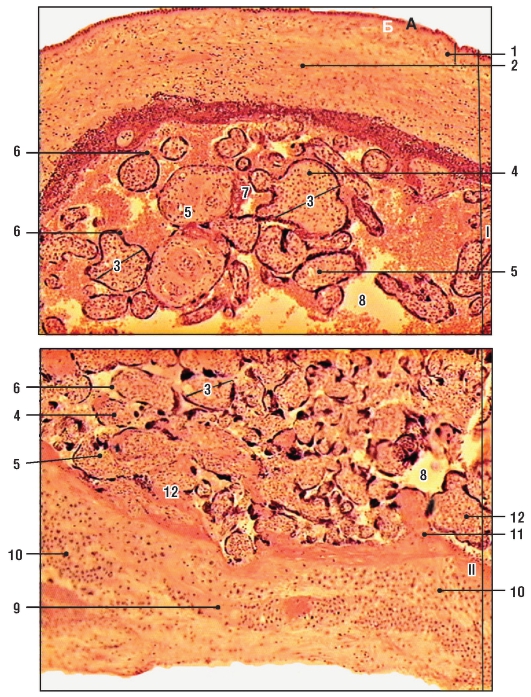
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Ageing or calcification of the placenta
In this article
- What does an 'ageing placenta' or 'calcification of the placenta' mean?
- How is the calcification or age of the placenta measured?
- How will an ageing or calcified placenta affect my delivery?
- Is it harmful to my baby if my placenta calcifies or ages too soon?
- Is there anything I can do to prevent early calcification or ageing of the placenta?
What does an 'ageing placenta' or 'calcification of the placenta' mean?
Placental calcification is the medical term for some of the changes that happen to the placenta, as pregnancy progresses.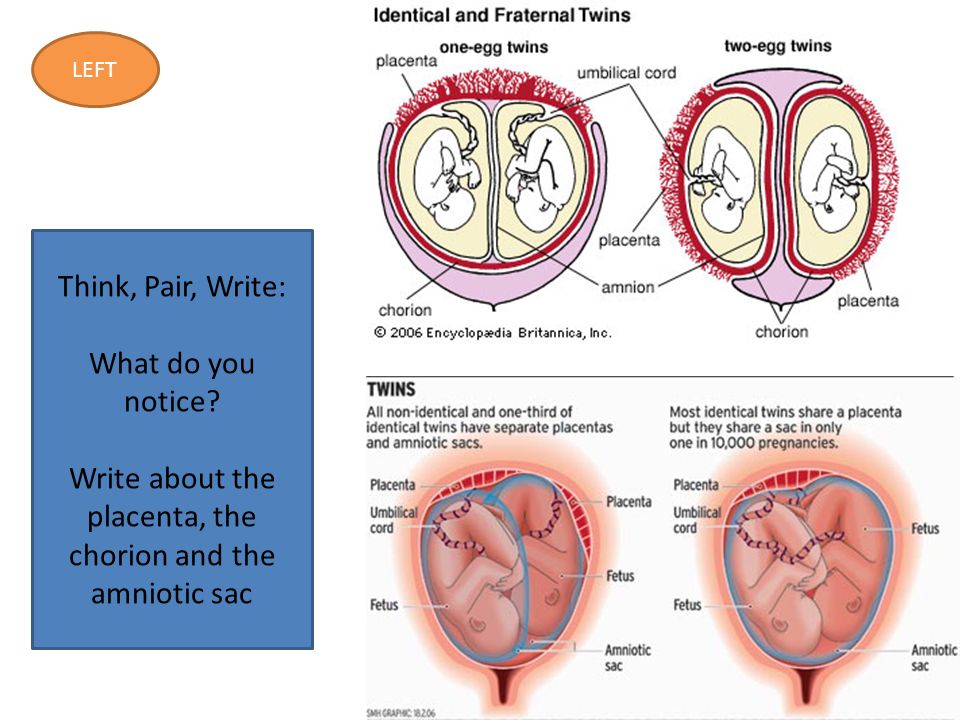
Many researchers regard placental calcification as a normal ageing process, rather than a change related to a disease or ailment.
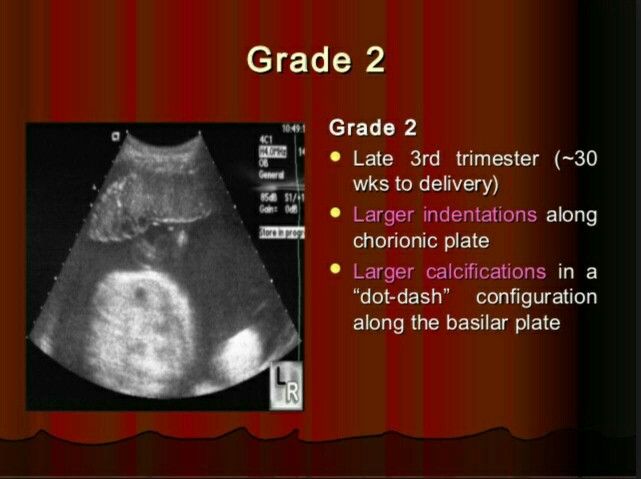
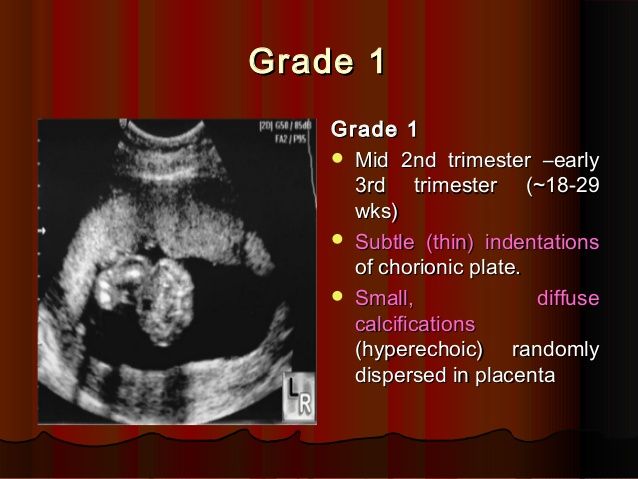
The placenta is usually described as going through four grades, from 0 (most immature) to III (most mature).
All placentas start at grade zero in early pregnancy. Changes can be seen from 12 weeks onwards. As pregnancy progresses, the placenta matures and calcifies.
It is classified into the following grades at different stages in pregnancy, at approximately the following times:
- Grade 0. Before 18 weeks of pregnancy.
- Grade I. Around 18 to 29 weeks of pregnancy.
- Grade II. Around 30 to 38 weeks of pregnancy.
- Grade III. Around 39 weeks of pregnancy. It is usually not seen before 38 weeks. A grade III placenta is known as a severely calcified placenta. At this stage, a formation of indentations or ring-like structures can be seen within the placenta.
How is the calcification or age of the placenta measured?
There is some uncertainty about whether changes in the placenta can be measured accurately as it can be difficult to grade the placenta objectively.
A lot depends on the interpretation of the ultrasound images by the ultrasound doctor. Some differences may also arise as it depends on how a doctor interprets the result.
How will an ageing or calcified placenta affect my delivery?
The effect of an ageing placenta on labour and delivery is difficult to say. Experts seem to have different opinions on the significance of a calcified placenta on delivery due to the lack of conclusive evidence.
Some placental changes during late pregnancy are considered a normal part of pregnancy and not thought to be of concern. However, in cases where changes occur earlier than expected, there is some disagreement regarding their significance.
Some risks that are known to be associated with placental calcification at each stage of pregnancy are listed below.
Changes between 28 and 36 weeks
One study suggests that women in high-risk pregnancies who develop a calcified placenta between 28 and 34 weeks need closer monitoring.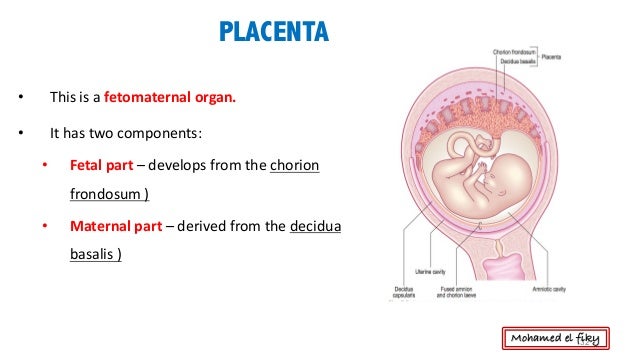 Some examples of high-risk pregnancies include pregnancies complicated by placenta praevia, diabetes, high blood pressure or severe anaemia.
Some examples of high-risk pregnancies include pregnancies complicated by placenta praevia, diabetes, high blood pressure or severe anaemia.
Calcification of placenta before 32 weeks of pregnancy is called an "early preterm placental calcification". It is known to be associated with a higher risk of pregnancy and birth complications, such as
- heavy bleeding after birth or postpartum haemorrhage
- placental abruption
- premature baby
- having a baby with a low Apgar score
- stillbirth
Changes from 36 weeks
One study has suggested that having a grade III placenta at 36 weeks is associated with an increased risk of pregnancy-related high blood pressure and having a low-birth-weight baby.
Hence, ultrasound scans that show placental calcification at 36 weeks may help in identifying high-risk pregnancies.
Changes from 37 to 42 weeks
A grade III calcified placenta from 37 weeks onwards is found in about 20 to 40 per cent of normal pregnancies.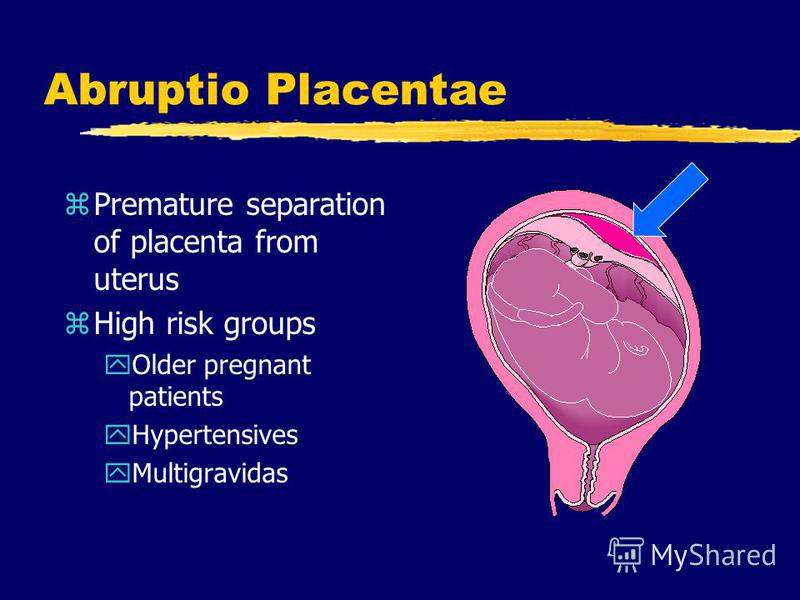 However, it is thought to of little clinical significance.
However, it is thought to of little clinical significance.
The effects of calcified placenta probably need to be evaluated on a case-to-case basis, depending on:
- how early the changes are seen
- how severe they are
- whether it is a high-risk pregnancy or not
- your doctor's opinion
Is it harmful to my baby if my placenta calcifies or ages too soon?
Preterm calcification of the placenta can be harmful to a baby in the womb, but it also depends on the grade and stage of pregnancy.
Some studies suggest that placental calcification before 32 weeks of pregnancy can result in low birth weight babies, babies with a low Apgar score and even stillbirth.
Some studies have shown that having a grade II placenta between 30 and 34 weeks can predict a low birth weight baby. But this is only among women who smoke during pregnancy.
Is there anything I can do to prevent early calcification or ageing of the placenta?
The exact causes of an ageing placenta are still not very clear, so it is difficult to say what would prevent it.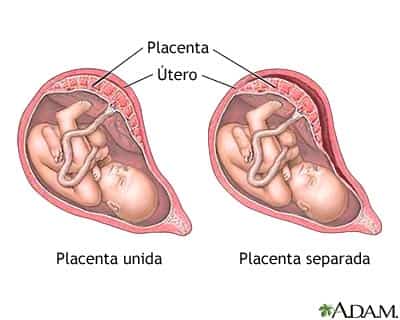 However, some research suggests that placental calcification is more likely in:
However, some research suggests that placental calcification is more likely in:
- younger women
- first-time pregnancies
- women who smoke during their pregnancy
Your doctor will be monitoring your health throughout your pregnancy. So, make sure you don’t miss any antenatal check-ups and your ultrasound scan appointments.
यह लेख हिंदी में पढ़ें!
Read more on:
- Scans to check the position of the placenta
- Low amniotic fluid (oligohydramnios)
- Dizziness in pregnancy
References
Abramowicz JS, Sheiner E. 2007. In utero imaging of the placenta: Importance for diseases of pregnancy. Placenta. 21(Suppl A):S14–S22.
Bricker L, Neilson JP, Dowswell T. Routine ultrasound in late pregnancy (after 24 weeks' gestation). Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD001451. DOI: 10.1002/14651858.CD001451. pub3.
pub3.
Chen KH, Chen LR, Lee YH. 2012. The role of preterm placental calcification in high-risk pregnancy as a predictor of poor uteroplacental blood flow and adverse pregnancy outcome. Ultrasound Med Biol. 38(6):1011-8. Online first 3 Apr.
Grannum PA, Berkowitz RL, Hobbins JC. 1979. The ultrasonic changes in the maturing placenta and their relation to fetal pulmonary maturity. American Journal of Obstetrics and Gynecology. 133:915–22.
Hill LM. Breckle R. Ragozzino MW. Wolfgram KR. O'Brien PC. Grade 3 placentation: incidence and neonatal outcome. Obstetrics & Gynecology. 61(6):728-32, 1983 Jun. Abstract. Full text available to Fellows, Members and Trainees.
Hills D. Irwin GA. Tuck S. 1984. Distribution of placental grade in high-risk gravidas. AJR. American Journal of Roentgenology. 143(5):1011-3.
Kazzi GM, Gross TL, et al. 1984. The relationship of placental grade, fetal lung maturity, and neonatal outcome in normal and complicated pregnancies. Am J Obstet Gynecol. ;148(1):54-8
;148(1):54-8
McKenna D, Tharmaratnam S, Mahsud S, 2005. Ultrasonic evidence of placental calcification at 36 weeks' gestation: maternal and fetal outcomes. Acta Obstet Gynecol Scand. 84(1):7-10.
Miller JM Jr, Brown HL, Kissling GA, Gabert HA. The relationship of placental grade to fetal size and growth at term. Am J Perinatol 1988; 5: 19–21.
Moran M, Ryan J, Higgins M, et al. 2011. Poor agreement between operators on grading of the placenta. J Obstet Gynaecol. 31(1):24-8.
Proud J, Grant AM. 1987. Third trimester placental grading by ultrasonography as a test of fetal wellbeing. BMJ 294: 1641–4.
Smith R, Maiti K, Aitken RJ. 2013. Unexplained antepartum stillbirth: a consequence of placental aging? Placenta. 34(4):310-3. Online first 26 Feb.
Szymanowski K, Chmaj-Wierzchowska K, Florek E,et al. 2007. Does calcification of placenta reveal only maternal cigarette smoking? Przegl Lek. 2007;64(10):879-81.
Walker MG, Hindmarsh PC, Geary M, et al. 2010. Sonographic Maturation of the Placenta at 30 to 34 Weeks Is Not Associated With Second Trimester Markers of Placental Insufficiency in Low-risk Pregnancies. J Obstet Gynaecol. 32(12):1134.– 39.
Sonographic Maturation of the Placenta at 30 to 34 Weeks Is Not Associated With Second Trimester Markers of Placental Insufficiency in Low-risk Pregnancies. J Obstet Gynaecol. 32(12):1134.– 39.
Yin TT, Loughna P, Ong SS, et al. 2009. No correlation between ultrasound placental grading at 31-34 weeks of gestation and a surrogate estimate of organ function at term obtained by stereological analysis. Placenta. 30(8):726-30. Online first 12 Jun.
Show references Hide references
Placental insufficiency - what is it and how to treat it
- Types and causes of placental insufficiency
- Diagnosis of placental insufficiency
- Treatment of placental insufficiency
Most women know that the placenta connects mother and baby during pregnancy and provides nutrients and oxygen to the baby.
Are there situations when the placenta ceases to perform its function correctly and fully? Is it possible to somehow prevent this?
What is the function of the placenta
So, the placenta is an important organ that is formed only during pregnancy. The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg, starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.
The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg, starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.
Inside the villi flows the blood of the baby, and outside they are bathed in the blood of the mother. Between the blood flow of mother and baby there is only one layer of cells, which plays the role of a barrier between the body of mother and child. Thanks to this membrane, the blood of the mother and fetus does not mix.
However, in recent years it has become known that fetal blood cells still penetrate the placental barrier into the mother's bloodstream, and thanks to this, it has become possible to conduct genetic analyzes and determine chromosomal abnormalities, Rh factor and fetal sex from the blood of a pregnant woman (non-invasive prenatal test) .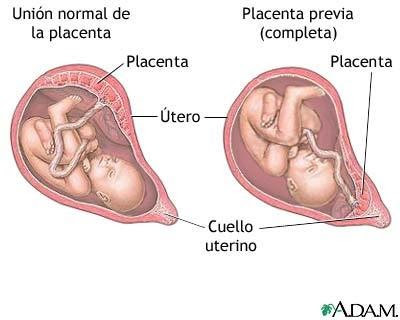
In the placenta, there is a constant exchange of substances between mother and child. Oxygen and nutrients are supplied from the mother's blood to the fetus, carbon dioxide and metabolic products from the fetus back to the mother, to be removed from the body.
The placental barrier performs an immunological function, as it allows some protective antibodies - blood cells that fight infectious agents, in addition, it is impervious to certain harmful substances, viruses and bacteria. Unfortunately, the placental barrier is easily overcome by drugs, alcohol, nicotine, components of many drugs and some viruses.
An important function of the placenta is the production of hormones and biologically active substances. First of all, these are hormones that are important for successful pregnancy, for example, chorionic gonadotropin, placental lactogen, estrogens, etc.
Unfortunately, things don't always go well. Due to a variety of reasons, deviations in the development and functioning of the placenta may occur at different stages of pregnancy.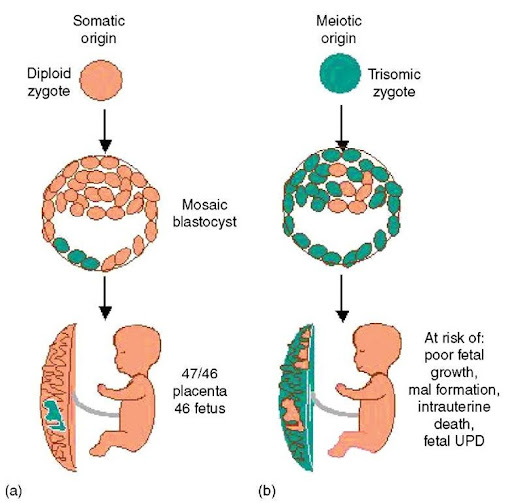 These changes never go unnoticed for mom and baby, and often have dire consequences.
These changes never go unnoticed for mom and baby, and often have dire consequences.
If the placenta ceases to perform its functions to the fullest, the so-called placental insufficiency develops. In fact, it consists in the deterioration of blood circulation in the mother-placenta-fetus system.
Types and causes of placental insufficiency
Doctors distinguish between acute and chronic placental insufficiency:
Acute placental insufficiency
This is a condition that requires urgent medical intervention. It is characterized by a rapid deterioration in placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or the death of certain areas of placental tissue, for example, during the formation of blood clots in the vessels. Abdominal trauma, antiphospholipid syndrome can serve as the cause of detachment.
Phospholipids are complex fats that are part of the membranes of all body cells. In some cases, the body's immune system produces a large number of antibodies to some of its own phospholipids and proteins that bind these lipids.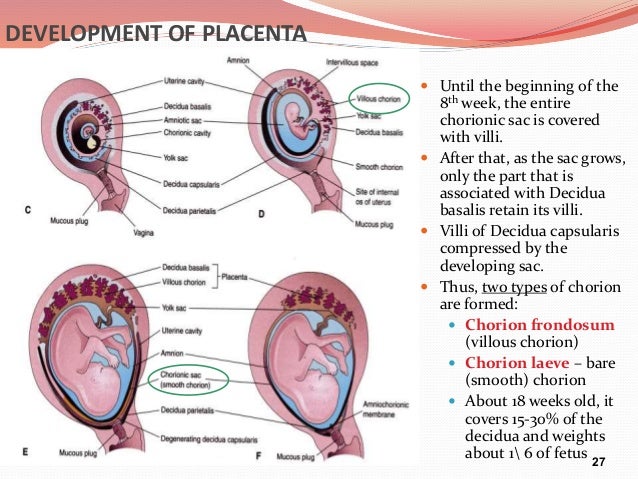 They are called antiphospholipid antibodies and, when interacting with the cells of the body, cause cell damage and activation of the blood coagulation system, which leads to thrombosis.
They are called antiphospholipid antibodies and, when interacting with the cells of the body, cause cell damage and activation of the blood coagulation system, which leads to thrombosis.
Antiphospholipid syndrome is the most common cause of thrombotic complications in pregnancy, including placental abruption and acute placental insufficiency.
A severe course of gestosis, a formidable complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine, can also cause placental abruption.
Acute placental insufficiency develops when more than 2/3 of the placental surface is detached.
In case of acute placental insufficiency, it is necessary to perform a caesarean section as soon as possible to save the life of the baby and mother.
Chronic placental insufficiency
Chronic placental insufficiency is much more common in pregnant women. In this case, there is a violation of the formation and maturation of the placenta, the uteroplacental and fetal-placental blood flow decreases, gas exchange and metabolism in the placenta are limited, and the synthesis of placental hormones decreases. All these changes determine the insufficient supply of oxygen and nutrients to the baby, cause a delay in the growth and development of the fetus.
All these changes determine the insufficient supply of oxygen and nutrients to the baby, cause a delay in the growth and development of the fetus.
The most common causes of placental insufficiency are previous abortions, especially surgical abortion during the first pregnancy, smoking, while the number and strength of cigarettes smoked do not matter, since tobacco smoke, not nicotine, has a negative effect on the formation of defective placental vessels.
The risk group for the development of placental insufficiency also includes women with chronic diseases such as arterial hypertension, iron deficiency anemia, pyelonephritis, diabetes, thyroid disease.
In recent years, there has been a significant increase in placental insufficiency caused by bacteria, viruses, fungi. The reason for this can be both an acute infection suffered by the expectant mother during pregnancy, and the activation of a chronic infectious process in the body of a pregnant woman.
Of no small importance in the formation of chronic placental insufficiency is the pathology of the uterus: endometriosis, malformations of the uterus (saddle-shaped, bicornuate). Doctors also consider uterine fibroids to be a risk factor. Of course, a number of drugs have an adverse effect on the formation of the placenta and the development of the fetus. Currently, a list of drugs that are not approved for use during pregnancy has been defined.
Doctors also consider uterine fibroids to be a risk factor. Of course, a number of drugs have an adverse effect on the formation of the placenta and the development of the fetus. Currently, a list of drugs that are not approved for use during pregnancy has been defined.
Also of great importance in the development of placental insufficiency is thrombophilia - an increased tendency of the body to form blood clots - blood clots in the vessels.
In some cases, placental insufficiency may be due to the presence of chromosomal abnormalities in the fetus, in particular in Down syndrome (the presence of an additional chromosome 21 in the fetus) or Edwards syndrome (an additional chromosome 18 in the fetus), placental dysfunction is diagnosed already in the early stages of pregnancy.
It should be noted that among the complications of pregnancy, most often leading to the development of chronic placental insufficiency, a significant factor is preeclampsia (or late preeclampsia) - a complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine.
Regardless of the factors contributing to the development of placental insufficiency, it is based on circulatory disorders in the uterine-placental complex, leading to disruption of all functions of the placenta. Consequently, the symptoms of chronic placental insufficiency will be due to a lack of oxygen and nutrients to the fetus.
This is, first of all, intrauterine fetal growth retardation - a lag in the size of the fetus and a slowdown in its growth. Often there is a change in the motor activity of the fetus. At first there may be some increase in movements, and then a decrease. Violation of the protective function of the placenta leads to intrauterine infection of the fetus under the action of pathogenic (pathogenic) microorganisms penetrating the placenta. The fetus, the development of which occurs in conditions of placental insufficiency, is much more at risk of trauma during childbirth, they have a violation of adaptation to extrauterine life, increased morbidity in the first year of life.
According to the time of occurrence, doctors divide placental insufficiency into early and late.
Early (or primary) placental insufficiency
Develops before 16 weeks of gestation. It occurs already at the stage of placenta formation and is associated with diseases of a pregnant woman that are present before pregnancy, for example, with uterine pathology, chronic arterial hypertension, and endocrinological diseases. In this case, the formation of defective vessels in the placenta occurs.
Late (or secondary) placental insufficiency
Occurs after 16 weeks of pregnancy and is most often associated with diseases that have already occurred during pregnancy. Most often, these are iron deficiency anemia (that is, a decrease in the concentration of hemoglobin and iron in the blood), gestational diabetes mellitus (that is, a violation of the absorption of glucose by the body that occurred during pregnancy), past viral and bacterial infections.
It is important to subdivide placental insufficiency into compensated and decompensated forms.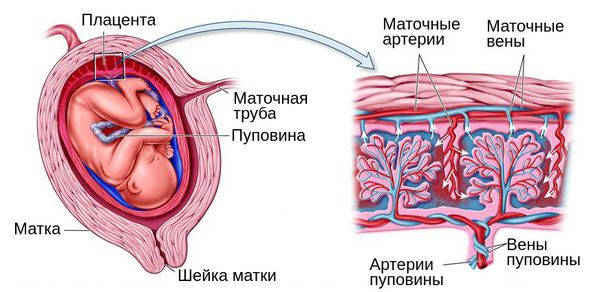
Compensated placental insufficiency
It develops, for example, with the threat of abortion and mild forms of late preeclampsia, if these complications are successfully amenable to medical correction.
Decompensated placental insufficiency
Causes the development of fetal growth retardation, chronic intrauterine hypoxia, up to fetal death.
Diagnosis of placental insufficiency
It is almost impossible to treat an already developed placental insufficiency, so doctors actively seek to identify pregnant women at risk of developing placental dysfunction. If placental insufficiency is detected in the 3rd trimester of pregnancy, there is no effective treatment, unfortunately. Therefore, all methods of identifying in the early stages of pregnancy those women whose formation of the placenta has been disturbed are being very actively used.
First of all, when registering for pregnancy, the most significant risk factors are identified - smoking, abortions, aggravated heredity (low birth weight, tendency to thrombosis), the presence of chronic diseases of the heart, blood vessels, diabetes mellitus.
Preventive measures against the development of placental insufficiency are especially relevant and necessary until 16-17 weeks of pregnancy, when the formation of placental structures occurs.
Significant assistance in assessing the risk of developing placental insufficiency is provided by prenatal screening, which is carried out at 11-14 weeks of pregnancy. It is carried out to detect Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most relevant is to conduct a comprehensive early screening of a pregnant woman to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation. Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic within the framework of compulsory medical insurance, but is available to everyone in prenatal diagnostic centers.
Determination of proteins produced by the placenta
First of all, the PAPP-A protein is determined, it is also a marker of chromosomal abnormalities of the fetus.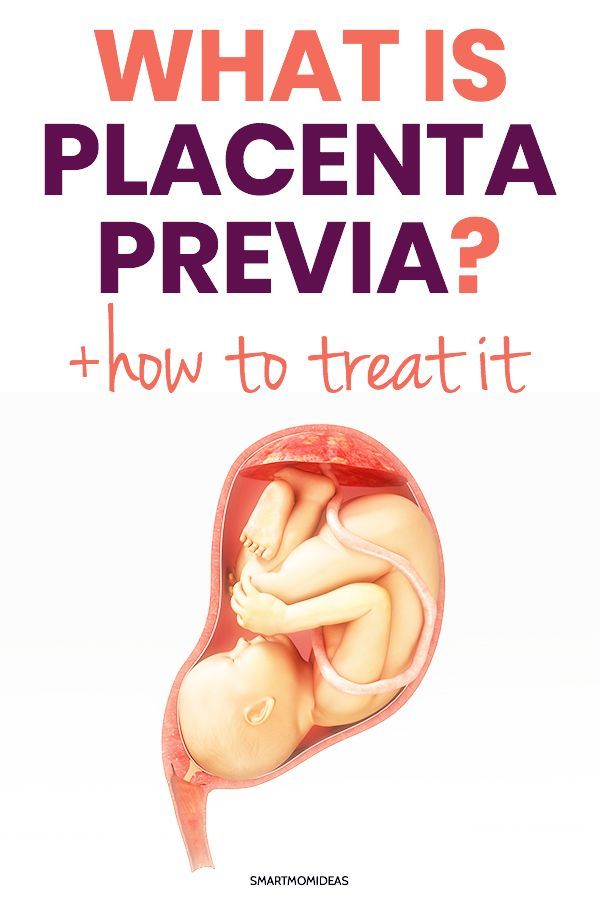 A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of gestation occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of gestation occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
The second placental hormone that helps in assessing the risk of placental insufficiency is PIGF (placental growth factor). Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not as widely used as PAPP-A, but many laboratories have already included this protein in 1st trimester prenatal screening. It is extremely important when screening the 1st trimester to measure blood flow in the vessels of the uterus. It has been unambiguously proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and lead to a decrease in the nutrition of the baby and the supply of oxygen, that is, to the development of placental insufficiency and fetal growth retardation.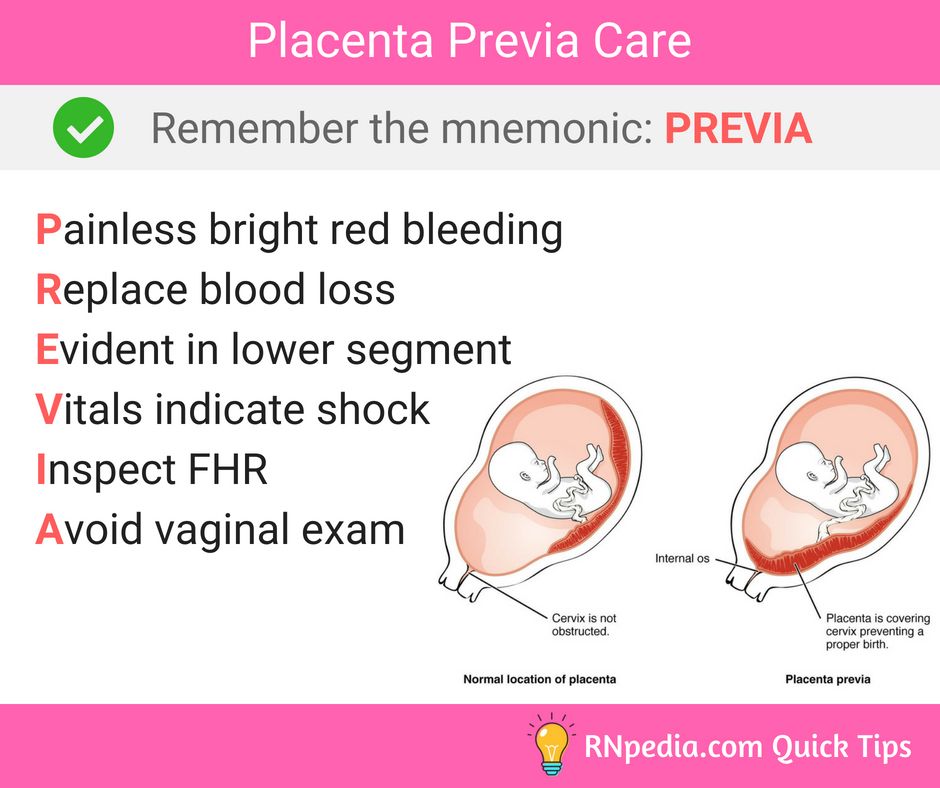 With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
The next mandatory screening ultrasound is at 20-21 weeks of gestation. In this case, measurements of the fetus must be carried out in order to assess whether there is a lag in growth. After all, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each period of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta. During ultrasound, dopplerometry of the uterine vessels is also performed to detect early changes that precede the clinical manifestations of placental insufficiency.
In patients belonging to the high-risk group, in addition to ultrasound and dopplerometry, daily monitoring of blood pressure fluctuations is also carried out, the amount of protein in the urine sample collected per day is determined, and the indicators of the blood coagulation system are evaluated.
The third ultrasound is performed for all expectant mothers at 30-34 weeks of pregnancy. The doctor measures the circumference of the head and abdomen of the crumbs, the length of the bones of his arms and legs, and calculates the estimated weight of the fetus. These measurements allow the doctor to make sure that the baby is developing normally. The structure of the placenta is also important, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that it ceases to have enough oxygen and nutrients and the development of the child is disturbed. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
Doppler
Doppler of the placental and umbilical cord vessels (method of studying blood flow velocities in these vessels) also allows you to assess the well-being of the baby. The doctor examines the blood flow in the arteries of the uterus, umbilical cord, heart and brain of the child.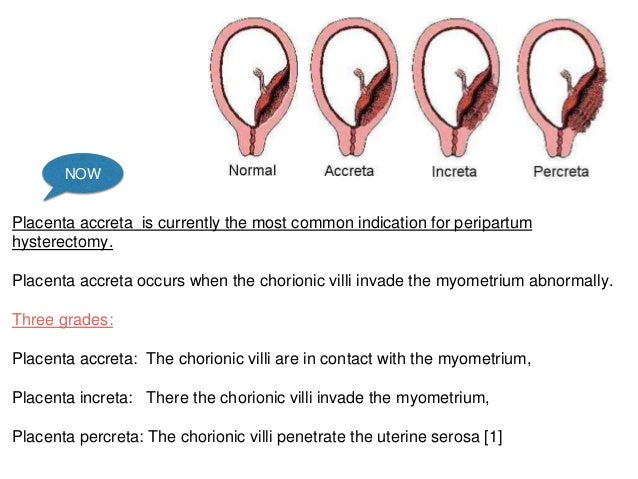 This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of preeclampsia in the mother. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of preeclampsia in the mother. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
A well-timed examination makes it possible to identify the initial stages of blood supply deficiency. In such cases, treatment can prevent formidable complications, such as hypoxia and intrauterine growth retardation of the baby. Dopperometry is carried out at 20-21 weeks and at 30-32 weeks of pregnancy, if there are changes, control is carried out at least every two weeks.
Cardiotocography
This is an important method for assessing the condition of the fetus. CTG is performed at a gestational age of 33 weeks or more, since only at this stage of the intrauterine development of the baby is a complete regulation of the activity of the cardiovascular system of the fetus established by the centers of the spinal cord and brain.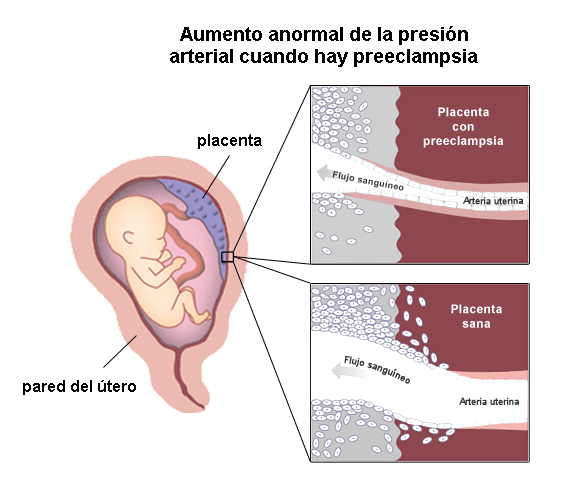 Recording of fetal heartbeats is carried out for 20-40 minutes, and if necessary, the study can be extended up to 1.5 hours.
Recording of fetal heartbeats is carried out for 20-40 minutes, and if necessary, the study can be extended up to 1.5 hours.
The device registers and records the baby's heart rate. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach. For example, with a decrease in the concentration of oxygen in the blood of the fetus, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks 1 time in 10-14 days, sometimes more often. Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant in the presence of signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby's heart activity and these data are transmitted via the Internet to the attending physician.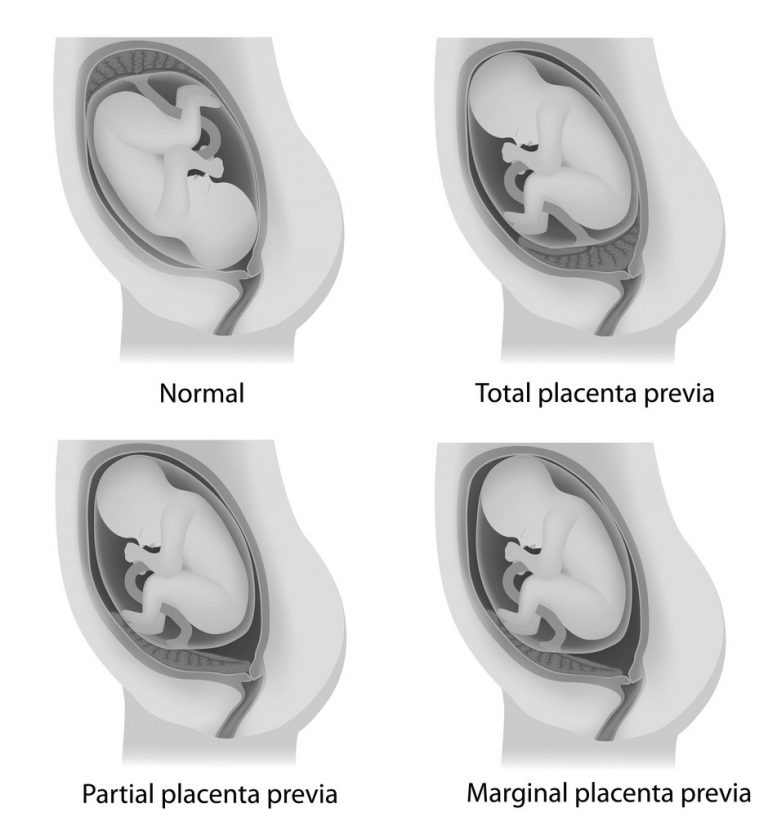
Treatment of placental insufficiency
There are currently no specific treatments for placental insufficiency because there are no drugs that selectively improve uteroplacental blood flow. That is why all measures to combat placental insufficiency are aimed at prevention. If the patient is at high risk for the development of placental insufficiency, from early pregnancy she is prescribed drugs whose effectiveness is well proven and which prevent the early development of severe placental dysfunction.
If during the additional methods of assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the flow of blood and oxygen through the placenta and mandatory control examinations against the background of ongoing therapy. If the changes are serious and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, then in such cases an emergency delivery is performed.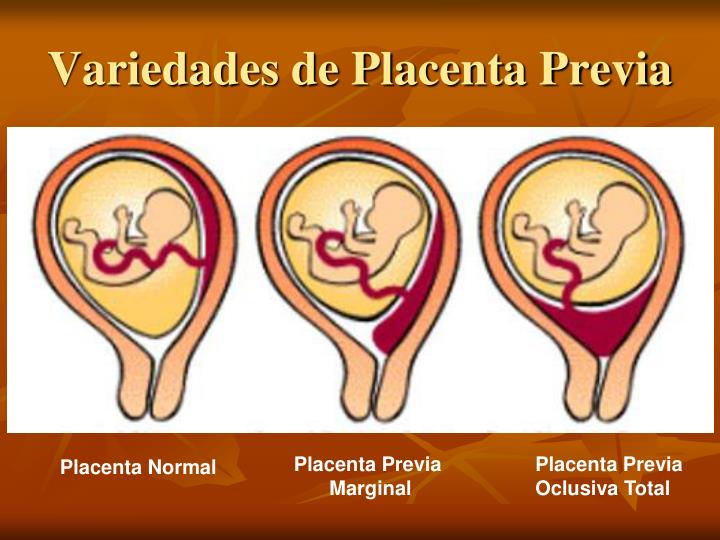
Screening for the detection of congenital diseases of the fetus during pregnancy
Category: Reminders for the population .
Pregnancy screening is a whole range of studies that allows parents and doctors to get the most complete information about the health of an unborn baby. Screening reveals many congenital and physical characteristics. How and when is pregnancy screening done?
What is pregnancy screening and why is it done
Screening during pregnancy is a complex of examinations, which includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to start treating genetic diseases as early as possible and, if not completely cure them, then at least stop the symptoms as much as possible. If the doctor notices any abnormalities during the examination, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth.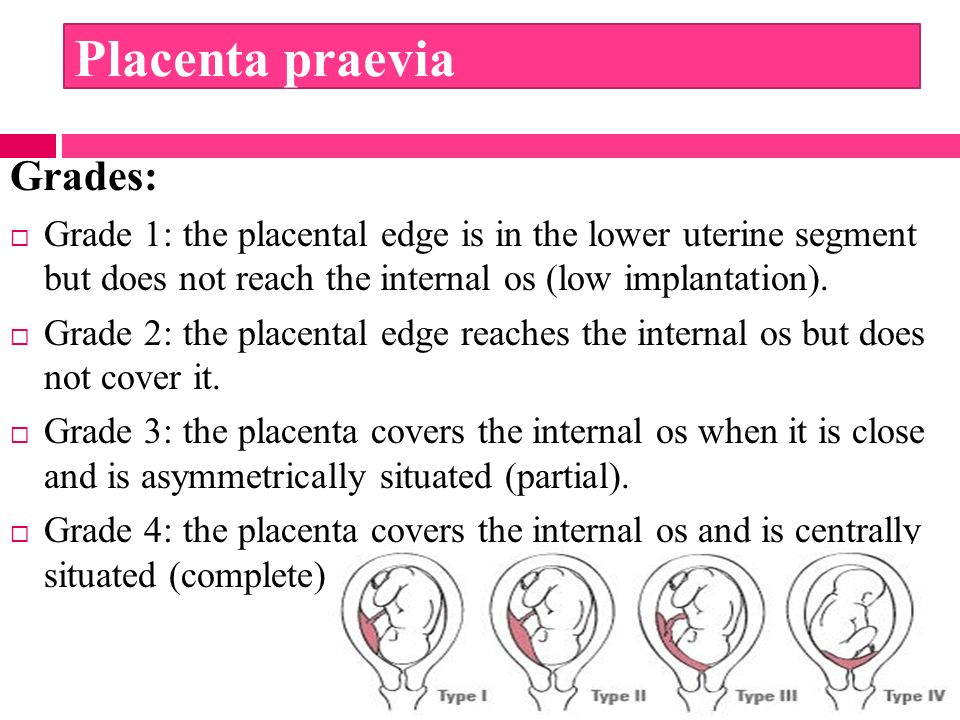 If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
Pregnancy screening is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not give a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman's compliance with the rules for preparing for the examination, and other factors.
First pregnancy screening
The first screening during pregnancy is carried out between the 11th and 13th weeks. It makes no sense to undergo this examination earlier - before the 11th week of pregnancy, many indicators are practically indeterminate.
The study includes two medical tests - an ultrasound and a blood test.
ultrasound
With the help of ultrasound, the doctor determines the exact gestational age, evaluates the baby's physique, its dimensions (head circumference, limb length, height), the work of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus.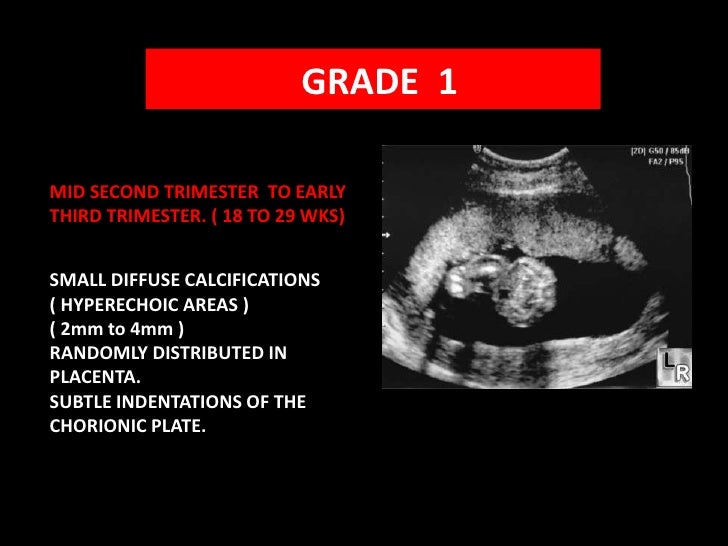 For each of these parameters, there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy, these rates are:
For each of these parameters, there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy, these rates are:
- KTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the tailbone) is 43–65 mm. If this figure is more than normal, then the child will be large. A downward deviation indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case, the heart will not be auscultated). However, this may also be due to a banal mistake in determining the timing of pregnancy.
- BDP (biparietal size, that is, the distance from the temple to the temple) - 17-24 mm. A high BDP means a large fetus, but only on the condition that all other indicators say the same. Otherwise, we can talk about a herniated brain or hydrocephalus. Low BDP indicates slow brain development.
- TVP (collar space thickness) - 1.
 6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research.
6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research.
The length of the nasal bone is 2–4.2 mm. Too small a nose bone can indicate pathology or simply that the baby's nose will be snub-nosed. HR (heart rate) - 140-160 beats per minute. A small (up to 40 beats per minute) deviation in one direction or another is considered a variant of the norm.
The size of the chorion, amnion and yolk sac. The chorion is the outer shell of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion previa. This is a potentially dangerous situation, fraught with miscarriage, and in this case, bed rest is recommended for the pregnant woman.
The amnion is the inner membrane that holds the amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of a fetus's life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies.
Cervix. Normally, its length by the time of the first screening is 35–40 mm. A shorter cervix means a risk of preterm labor.
Ultrasound is performed in two ways - transabdominal, in which the sensor of the ultrasound machine is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but it is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdomen does not allow the fetus and uterus to be examined in detail.
It is necessary to properly prepare for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that the bladder is full at the time of the examination - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With transvaginal ultrasound, the degree of fullness of the bladder does not matter, however, before the examination, it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is carried out. Therefore, expectant mothers suffering from flatulence are advised the day before the examination to take remedies for flatulence and not eat anything that produces gas.
Blood test
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU / ml is considered the norm. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes in the mother. Reduced hCG is typical of miscarriage, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome).
- PAPP-A is an A-plasma protein. The content rate for a period of 11–13 weeks is 0.79–6.01 mU / l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- A high PAPP-A is a sign of multiple pregnancies, large fetuses, or a low placenta.
In order for the blood test to give the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal.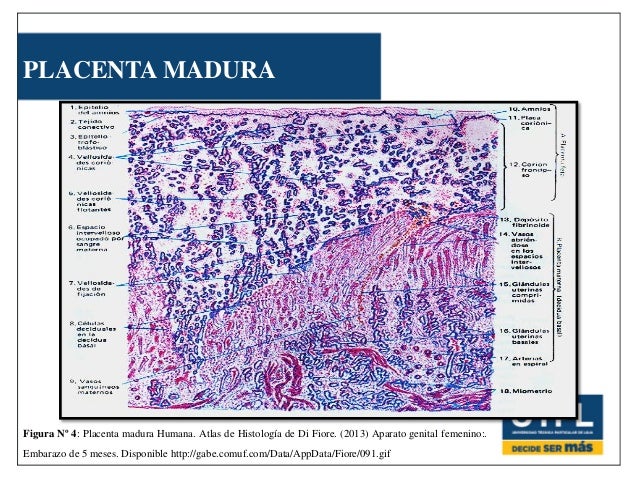 2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
Second pregnancy screening
The second screening during pregnancy is carried out at 16-20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood test.
ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate main indicators of the norm for a period of 16-20 weeks:
- BPR - 26–56 mm.
- DBK (length of the femur) - 13-38 mm.
- DPC (length of the humerus) - 13-36 mm.
- OG (head circumference) - 112-186 mm.
IAF (amniotic fluid index, that is, the volume of amniotic fluid) - 73-230 mm. Oligohydramnios can adversely affect the condition of the child's bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such localization, detachment of the placenta is possible.
Umbilical cord. One of the most important parameters is the place of attachment of the umbilical cord. Marginal, split or sheath attachment is fraught with fetal hypoxia and difficulties during childbirth, often it becomes an indication for caesarean section. The umbilical cord is fed through 2 arteries and 1 vein, although sometimes only one artery is available. This can cause fetal hypoxia, heart disease, disorders in the child’s cardiovascular system, and cause a baby’s low body weight. However, if all other analyzes and examinations do not show deviations from the norm, you should not worry.
Cervix. The length of the cervix at this time should be 40–45 mm. A short cervix means a threatened miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the peculiarities of the position of the fetus or the excess weight of the expectant mother, and by edema or hypertonicity of the uterus.
Blood test
As during the first screening, during the second, a blood test for b-hCG is taken, the level of free estriol and AFP is also checked. Here are the norms for their content at the 16th-20th weeks of pregnancy:
- b-hCG - 4.67-5-27 ng / ml.
- Free estriol is a hormone whose level can be used to judge the state of the placenta. The norm is 1.17–3.8 ng / ml. Elevated estriol is characteristic of multiple pregnancy or a large fetus. Reduced - for threatened miscarriage, placental insufficiency, anencephaly and Down's syndrome.
- AFP is a protein that is produced in the gastrointestinal tract of the fetus.
 Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Third pregnancy screening
The third screening during pregnancy is carried out at the 30th-43rd week. Based on the results of this screening, the doctor decides on the need for a caesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes dopplerography is prescribed - a study of the work of blood vessels. Here are the approximate norms for a given gestational age:
ultrasound
- BPR — 67–91 mm
- DBK - 47-71 mm
- WPC - 44-63 mm
- exhaust gas - 238-336 mm
- IAG — 82- 278 mm
The thickness of the placenta is 23.