Babies urine infection
Urinary Tract Infections (UTIs) in Infants & Children
What Are Urinary Tract Infections (UTIs)?
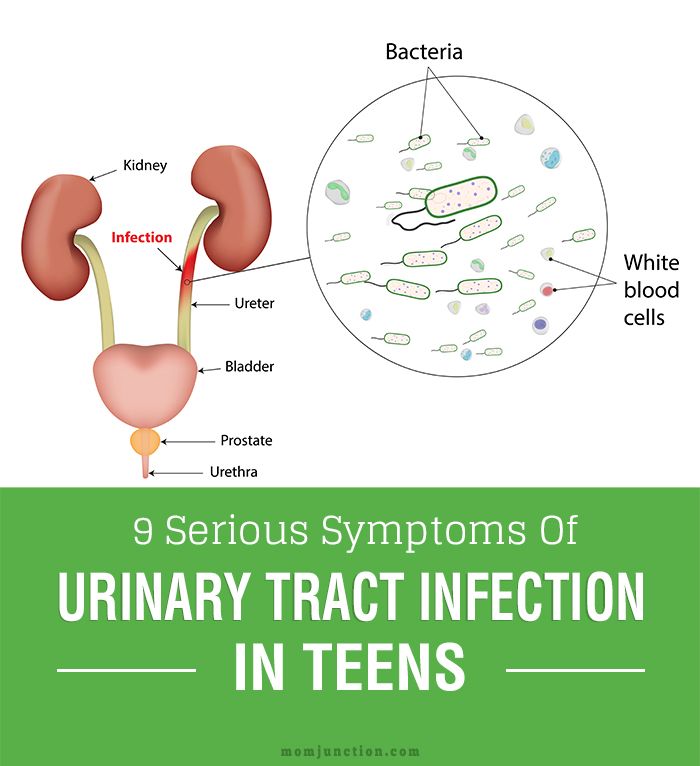
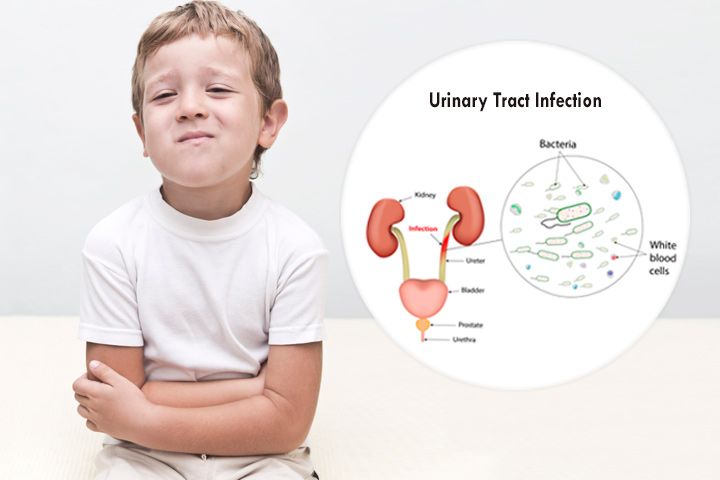
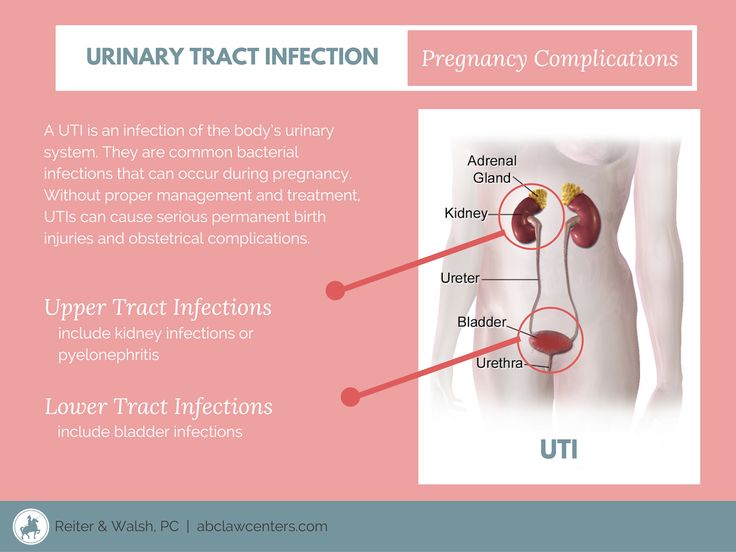
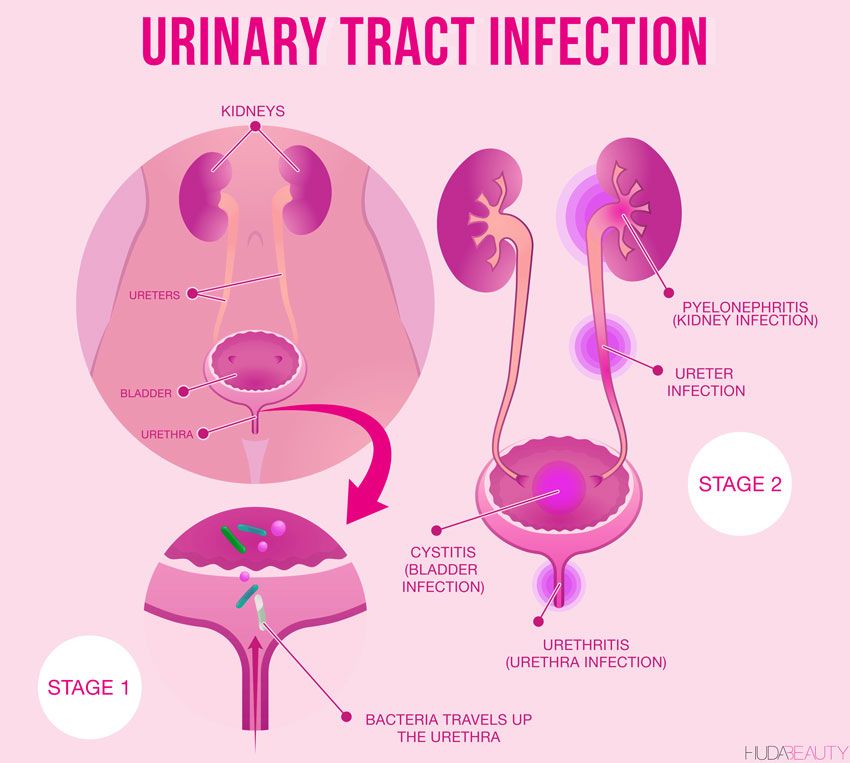
A urinary tract infection (UTI) happens when bacteria (germs) gets into the urinary tract. The most common place for a UTI to occur is in the bladder, but infections also occur in the urethra, ureters or kidneys. UTIs are easily treated but can cause problems if left alone.
What is the urinary tract and how do infections occur?
The urinary tract is the body’s drainage system for getting rid of urine (liquid waste). It includes the two kidneys, bladder (the organ where urine is stored), and two ureters and one urethra (tubes).
The blood in the body passes through the kidneys. The kidneys filter the liquid waste products (urine) out of the blood. This urine passes through the ureters and into the bladder. The urine leaves the bladder through the urethra, and passes out of the body through the opening (meatus).
Most UTIs in children occur because bacteria that are normally found in the bowel cause an infection in the urinary tract.
What causes UTIs?
These factors can increase your child’s chance of getting a UTI:
- Poor bathroom habits, such as not changing out of wet underwear or not wiping properly
- “Holding it,” instead of urinating frequently (in toilet trained kids)
- Frequent constipation or diarrhea
- Having some kind of blockage in the urinary tract that limits or stops urine flow
- Irritation in the “perineal” area (where urine comes out of the body). This can be caused by things such as bubble bath, bath soap or tight clothing.
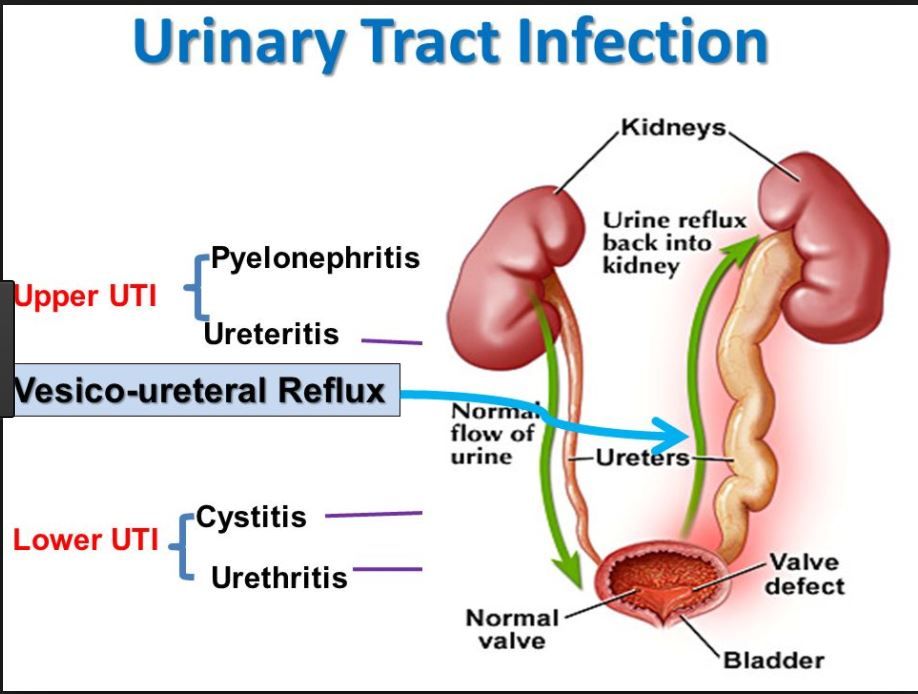
- A condition called vesicoureteral reflux (VUR), in which urine flows backward from the bladder and toward the kidneys
Learn about how to prevent a UTI.
Are UTIs common in children?
UTIs are the second most common type of infection in children (ear infections are the most common). They are more common in girls, although uncircumcised boys are at slightly higher risk than other male babies or older boys.
What are the signs and symptoms of a UTI?
There are two different kinds of UTIs. The most common is called cystitis. It occurs when the infection is in the urethra or bladder. A child who has cystitis may:
- Have a fever (this may be the only symptom in babies)
- Be fussy (common in babies)
- Vomit (common in babies or older children)
- Feel the need to use the bathroom often, yet only pass a very small amount of urine (more common in older children)
- Wet themselves, even after being successfully potty trained
- Have pain or burning with urination (more common in older children)
- Have lower belly or back pain
- Have blood in the urine
The less common type of UTI is called pyelonephritis, which is an infection that occurs in the kidneys. Pyelonephritis can sometimes be treated at home, but in some cases it can become serious and even life threatening. A child who has pyelonephritis may have:
- A fever greater than 101 degrees
- Flu-like symptoms such as shaking, chills, nausea, vomiting or achiness
- Pain in the belly, back, side or groin
- Pain or a burning feeling when urinating
- Urine that is cloudy, red, foul smelling or changes to a dark cola color
- Pus or blood in the urine
- Urgent or frequent urination
If your child experiences symptoms of cystitis or pyelonephritis, call your pediatrician.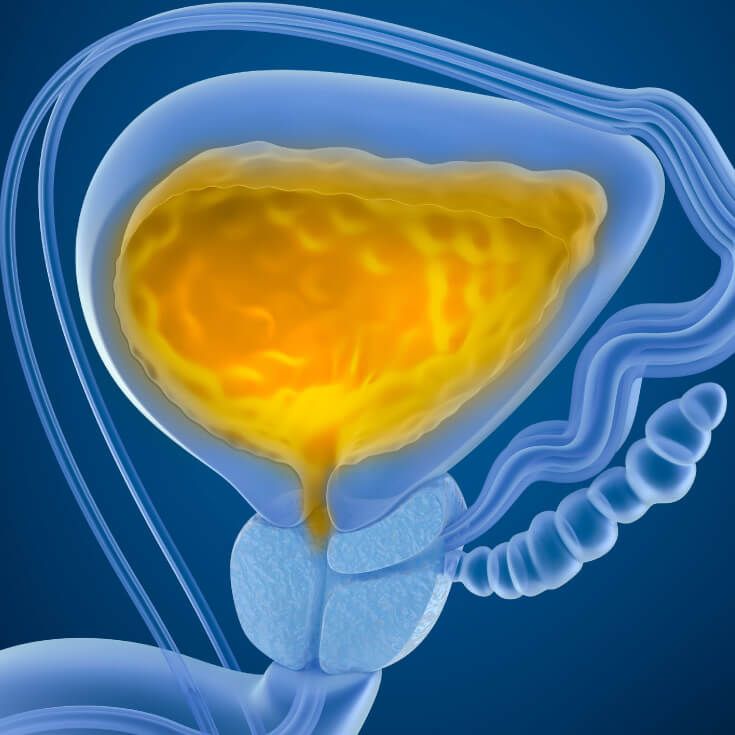
How is a child diagnosed with a UTI?
If the pediatrician thinks your child may have a UTI, they will:
- Ask about your child’s symptoms and health history
- Do a physical exam
- Run tests, including a urinalysis (a simple study of a urine sample) and/or urine culture (which detects specific bacteria in urine)
How do you treat UTIs?
The most common treatment for a UTI is antibiotics, which kill the germs that are causing the infection. The pediatrician also may recommend that your child take pain relief medicine as needed, and drink plenty of fluids.
UTIs can cause irritation and raw skin on your child’s private parts. If these symptoms do not improve after exposing the skin to air and creating a moisture barrier with petroleum jelly or, zinc oxide or lanolin, let your pediatrician know.
If my child is being treated for a UTI, what can I do to help?
- Give your child all the medicine the doctor prescribed for the infection.
 Do not stop the medicine, even if your child is feeling and acting better.
Do not stop the medicine, even if your child is feeling and acting better. - Give your child lots of fluids to drink so they continue to urinate regularly, every two to three hours for toilet trained children.
- Tell your doctor if your child’s fever, pain or other symptoms continue after taking the medicine for two days.
- If your child is in pain or has a fever, give medicine only as directed by the doctor. Do not give aspirin to children.
- Keep all follow-up appointments.
- Do not allow your child to sit in bathwater that contains bubble bath, shampoo or soap, as this can cause irritation. If your child takes a bath, have them sit in clear water until you’re ready to use these products. Once you are finished, rinse your child off and remove the products from the tub.
What if my child gets frequent UTIs?
Some children get UTIs more often than others. Be sure to tell your pediatrician if symptoms happen again after treatment, or if your child has three or more UTIs in a six-month period.
The pediatrician may recommend taking your child to a pediatric urology practice for an evaluation. Physicians and nurse practitioners at this type of practice specialize in treating children who have problems with their urinary system. These specialists may run additional tests to learn about the cause, and recommend a new treatment plan.
These additional tests may include:
- An ultrasound to view the kidneys, bladder and the tubes connecting them
- A voiding cystourethrogram (sis-toe-u-reeth-ro-gram), or VCUG. This X-ray shows how the bladder is working while the person is urinating.
Last Updated 07/2021
Reviewed By Nicole Inman, CNP
The Division of Urology treats a complete range of disorders affecting the urinary and genital tracts, from common concerns to rare and complex abnormalities.
Learn More
For more information or to request an appointment, contact the Division of Urology.
Contact Us
Urinary Tract Infections In Babies
AddictionAllergies & AsthmaAmbulatoryAudiologyAutismAwardsBC4TeensBehavioral HealthBehind the ScenesBurn CenterCancerCardiologyCenter for Healthy Weight and NutritionCenter for Injury Research and PolicyChild BehaviorChild DevelopmentColorectal and Pelvic ReconstructionCommunity EducationCommunity ResourcesCoronavirusDentistryDermatologyDiseases & ConditionsDiversity and InclusionEndocrinologyENTEpilepsyEverything MattersFertility and Reproductive Health ProgramFundraising EventsGastroenterologyGeneticsGynecologyHematologyHomecareHospiceHospital NewsInfants & NewbornsInfectious DiseaseKids & TeensLaboratory ServicesMake Safe HappenMarathonNeonatologyNephrologyNeurologyNeurosurgeryNew HospitalNICUNutrition & FitnessOccupational TherapyOphthalmologyOrthopedicsOur PatientsOur staffPalliative CareParentingPediatric NewsPharmacyPhysical Therapy - Sports and OrthopedicPlastic SurgeryPopulation HealthPregnancyPrimary CarePsychologyPulmonaryRadiologyReach Out and ReadRehabilitationResearchRheumatologySafety & PreventionSports MedicineSurgical ServicesThe Center for Family Safety and HealingTherapeutic RecreationTherapyTHRIVE ProgramToddlers & PreschoolersUrgent CareUrology
Aaron Barber, AT, ATC, PESAbbie Roth, MWCAbby Orkis, MSW, LSWAdam Ostendorf, MDAdriane Baylis, PhD, CCC-SLPAdrienne M. Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.
Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D. Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.
Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H. Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.
Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.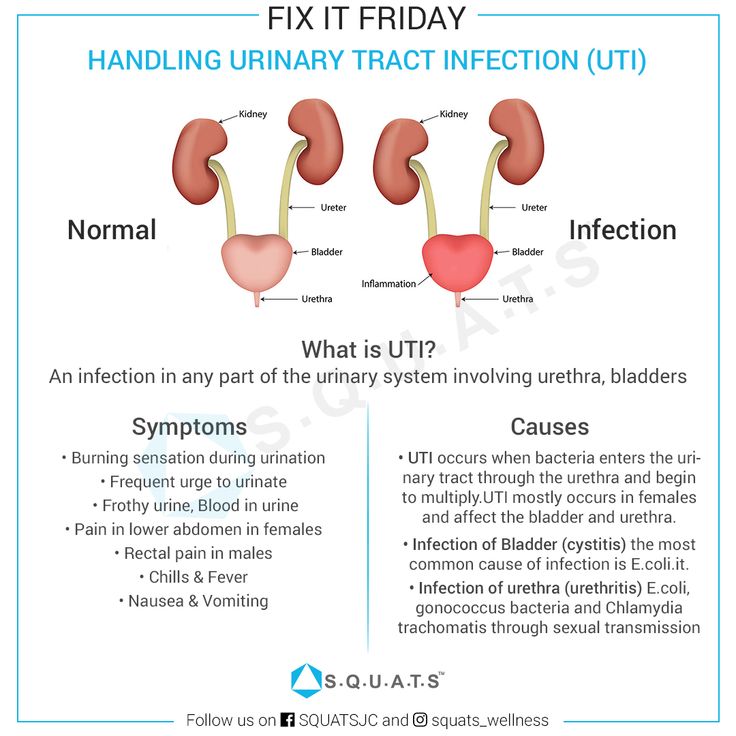 Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D.
Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M.
Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.
Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N. Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P.
Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.
Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I. Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C.
Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L.
Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Urinary tract infection in newborns.
Urinary tract infection in young children is no less common than viral respiratory infections. Vomiting and nausea, cramps in the abdomen are often attributed by parents to colic, malnutrition or intestinal infections. However, with such symptoms, it is recommended to consult a doctor. If this is a urinary tract infection, then its untimely diagnosis and treatment will lead to unpleasant consequences for the baby.
A urinary tract infection occurs when bacteria in the child's body begin to multiply rapidly in the urinary tract.
Most often this pathology is caused by microbes such as:
- Escherichia coli,
- Staphylococcus aureus,
- Pseudomonas aeruginosa,
- Klebsiella
These include:
- vesicoureteral reflux;
- narrowing of the ureters;
- malposition of the organs of the urinary system;
- horseshoe kidney and others
Another cause of infection is the presence of a microbial focus in the body. With an infectious-inflammatory pathology of other organs, the bacterial flora can enter the kidneys and urinary tract, causing inflammation there. Also, the bacterium can enter the baby's body from the mother during breastfeeding.
Genitourinary infection in infants presents with the same symptoms as in adults. The problem is that a newborn baby cannot complain.
Parents should keep a close eye on their child to detect symptoms of illness.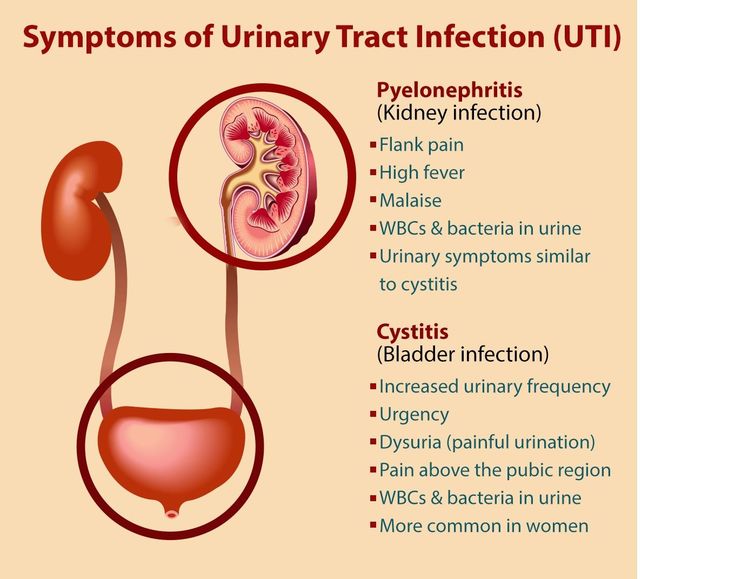
Initial symptoms include tearfulness, restlessness, poor sleep and loss of appetite.
In children under one year old, a urinary tract infection may be manifested by a decrease or increase from the age norm of urine excreted, a change in the color and saturation of urine (the child's urine may become bright yellow (with an increase in the concentration of urine, which is usually accompanied by a decrease in its quantity), red or brown (admixture of blood.) When bacteria appear, the urine does not change its color, but becomes cloudy and loses its transparency.0003
Edema may appear due to the characteristics of the baby's body, the appearance of an unpleasant smell from the diaper.
The appearance of restlessness and crying when urinating, which indicates the presence of pain and cramps in the baby. Often, mothers note that the child strains when urinating. In this case, an intermittent stream of urine is recorded.
The rise in temperature to high numbers, if it does not go away after taking antipyretics and persists for several days, this is a reason to suspect an infection.
Infection of the genitourinary system in infants is detected by laboratory analysis of urine, urine culture, blood test, b / x blood test.
In case of inflammation, blood and urine tests show an increase in the number of leukocytes. With bakposev, it is possible to identify which bacterium caused the infection, and determine the individual sensitivity of the microbe to the antibiotic.
As noted above, the cause of infection in infants may be a congenital malformation of the genitourinary organs.
If this pathology is suspected, the following examinations should be performed:
- ultrasound examination of the urinary system organs;
- voiding cystography;
- retrograde radiography of the kidneys;
- CT or MRI of the kidneys.
The basis for the treatment of urinary tract infection is antibiotic therapy. A broad-spectrum antibiotic or a drug based on sensitivity is prescribed. The antibiotic is taken orally or injected intravenously.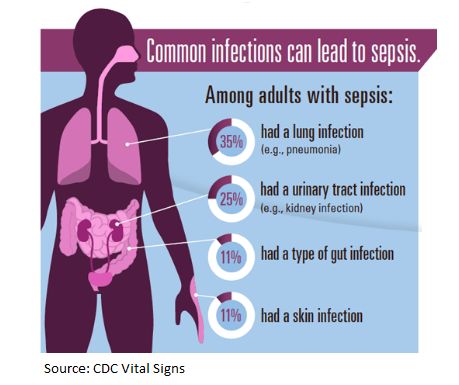
It is important that if an infection is detected, the infant must be hospitalized for the duration of treatment.
In addition to antibiotics, anti-inflammatory drugs and antipyretics are used. Moreover, many medicines are produced in a convenient form of application, for example, in candles.
Herbal uroseptics are often prescribed, which do not have a toxic effect and contribute to the recovery of the child. In no case should you start treatment on your own or cancel medications without a doctor's prescription. This will lead to the fact that the disease will go into a latent stage and will periodically worsen, again and again causing unpleasant symptoms. In addition, many drugs are contraindicated for children and their uncontrolled use will bring irreparable harm to the child.
Infection in infants with malformations will constantly recur despite good treatment. Therefore, the only way out is to carry out an operational correction of the defect. It should be noted that the operation is possible only after the acute inflammatory process is eliminated.
Prevention of urinary tract infections in infants.
In order to rule out an illness in a child, the following points should be followed:
- Carefully monitor the hygiene of the child's urinary organs.
- avoid hypothermia of the baby;
- monitor the rationality of nutrition.
Every year about 1400 children are treated in the Department of Prematurity and Pathology of Newborns. Of these, with urinary tract infection 65-70, with various congenital malformations of the kidneys and urinary system 28-30 children. All children undergo a complex of examinations and treatment according to the developed standards. All children are discharged with improvement and recovery and are subsequently observed by nephrologists and urologists in the regional children's clinic.
Infection of the genitourinary system is not such a terrible diagnosis. With a complete examination and high-quality, adequately selected therapy, the child will recover without any residual effects.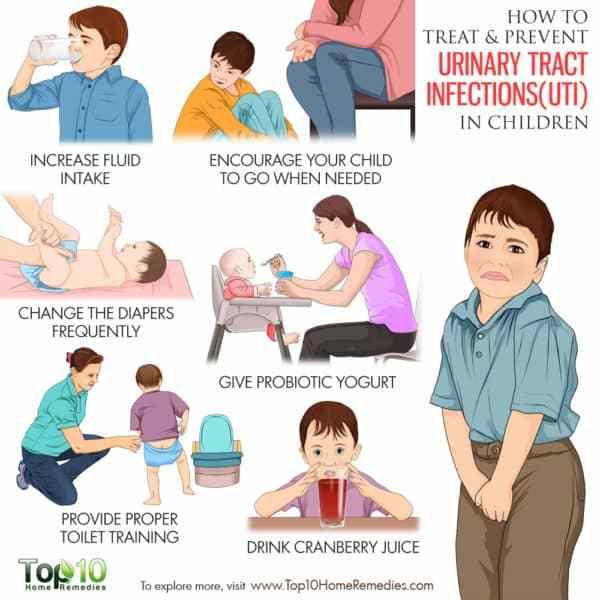
Urinary tract infections (UTIs) in children
According to statistics, urinary tract infections (UTIs) rank second after acute respiratory infections. Children under 3 years of age are especially susceptible to them. Moreover, in almost half of the cases, the inflammatory process starts asymptomatically, which is why parents do not have the opportunity to see a doctor in time. How to suspect an infection in a timely manner? How to prevent the development of complications? And how to treat the disease?
Definition
- Urinary tract infection (UTI) is a group of inflammatory diseases of the urinary system that develop when an infectious agent enters the body.
- Bacteriuria is the presence of bacteria in urine from the bladder. Asymptomatic bacteriuria is called, detected during a dispensary or targeted examination in a child without any complaints and clinical symptoms of a disease of the urinary system.
- Acute pyelonephritis is an inflammatory disease of the kidney caused by a bacterial infection.
- Acute cystitis is an inflammatory disease of the bladder of bacterial origin.
- Chronic pyelonephritis - kidney damage, manifested by fibrosis and deformity of the pelvicalyceal system, as a result of repeated attacks of UTI infection. As a rule, it occurs against the background of anatomical anomalies of the urinary tract or obstruction.
- Vesicoureteral reflux (VUR) is a retrograde flow of urine from the bladder into the ureter.
- Reflux nephropathy - focal or diffuse sclerosis of the renal parenchyma, the primary cause of which is vesicoureteral reflux, leading to intrarenal reflux, repeated attacks of pyelonephritis and sclerosis of the renal tissue.
- Urosepsis is a generalized nonspecific infectious disease that develops as a result of the penetration of various microorganisms and their toxins from the organs of the urinary system into the bloodstream.
Prevalence
In infants and young children, UTI is the most common severe bacterial infection, occurring in 10–15% of hospitalized febrile patients of this age. Before the age of 3 months, UTI is more common in boys, at an older age - in girls. At primary school age - in 7.8% of girls and 1.6% of boys. With age after the first episode of UTI, the relative risk of recurrence increases.
Recurrence rate:
in girls:
- 30% within one year of the first episode;
- 50% within 5 years of first episode;
in boys:
- 15–20% within one year of the first episode.
Some important facts about the disease
Most urinary tract infections in children are caused by bacteria such as E. coli, Enterococcus, Proteus and Klebsiella.
Among the numerous factors that cause the development of infection, the biological properties of microorganisms that colonize the urinary tract, and urodynamic disorders (vesicoureteral reflux, urinary tract obstruction, neurogenic bladder dysfunction) are of priority importance.
The most common route of infection is ascending. The reservoir of uropathogenic bacteria is the rectum, perineum, lower urinary tract.
The anatomical features of the female urinary tract (short wide urethra, proximity to the anorectal region) cause a high incidence and recurrence of urinary tract infections in girls and girls.
Diagnosis
In adults, urinary tract infections are usually accompanied by unpleasant symptoms (frequent and painful urination, acute pain in the lower abdomen, etc.), but in the case of children, all these signs of an inflammatory process UTIs are often absent, except for high fever. In fact, the fever itself in a child in the absence of any other visible symptoms of the disease often signals precisely the onset of inflammation in the urinary tract (in this case, a general analysis of the child's urine should be performed).
There are situations when a urinary tract infection in children manifests itself in the following signs:
- Child complains of soreness or burning sensation during "going to the toilet";
- The child complains of pain in the lower abdomen;
- Urine takes on an uncharacteristic color, density, or odor;
- Urinary incontinence (especially at night) over 7-8 years of age;
- Constant thirst;
- The general condition and behavior of the child may change - the baby becomes lethargic, capricious, whiny, loses appetite, etc.
A urinalysis can be used to refute or confirm the presence of a UTI with these symptoms. As a diagnostic method, it is recommended to conduct a clinical analysis of urine with a count of the number of leukocytes, erythrocytes and the determination of nitrates.
Since the diagnosis of a suspected urinary tract infection is based on the result of a child's urine test, it is very important to collect the material for this analysis correctly and submit it on time. To collect tests, you need to use special sterile containers that are sold in a pharmacy. To collect urine from newborns and infants, convenient devices have been invented - special urinals that save parents from having to “squeeze out” diapers or guard near the baby, spread out on oilcloth ... These devices are completely safe, they are hermetically glued to the child’s genitals, do not cause the baby has no discomfort and is simply removed. No more than 1.5 hours should elapse between the moment of urine collection and its entry into the laboratory.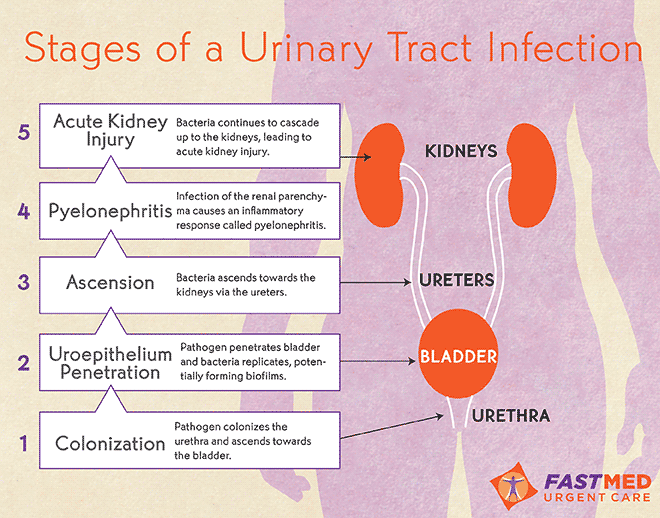 In other words, you can not collect urine from a child before bedtime, then put it in the refrigerator, and in the morning take such material to the laboratory - this analysis will not be reliable.
In other words, you can not collect urine from a child before bedtime, then put it in the refrigerator, and in the morning take such material to the laboratory - this analysis will not be reliable.
To avoid problems with urine collection, refuse to use special devices for collecting urine, a portable urine analyzer allows you to “wet” the test strip both directly in the urine stream and in any place where the child has urinated.
There are situations when it is difficult to quickly pass a urine test (late time of day, remoteness of the laboratory, etc.). In these cases, having a portable urine analyzer at home can be indispensable.
The diagnosis of UTI is not made without confirmation by laboratory tests of urine (general analysis of urine for an infectious process in the urinary tract indicates an abnormally large number of leukocytes). Sometimes a child is also assigned an ultrasound or x-ray study of the structural features of the urinary system, a consultation with a pediatric gynecologist or andrologist.
Treatment
If the diagnosis of UTI is confirmed, the doctor prescribes antibiotic therapy. The basis of effective treatment of any urinary tract infection in children and adults is the use of age-appropriate and medical situation-appropriate antibiotics. Already after 24-48 hours after the start of taking the drugs, the child's well-being will noticeably improve, but it is important for parents to remember that for a true recovery it is necessary to endure a full course of antibiotic therapy, which averages 7-14 days.
Indications for hospitalization in a specialized hospital for children with urinary tract infection:
- Young children (less than 2 years old).
- Presence of symptoms of intoxication.
- Inability to perform oral rehydration if there are signs of dehydration.
- Bacteremia and sepsis.
- Recurrent course of UTI to exclude its secondary nature and selection of adequate anti-relapse treatment.
The length of stay in the hospital for a UTI is 10–14 days.
Given the young age of many patients, the inability to find out the child's complaints, the absence of specific symptoms, in some cases it is difficult for parents to decide what caused the child's body temperature to rise - teething, banal SARS or urinary infection requiring hospitalization in a hospital. An express urinalysis can help in solving such a difficult issue. In these cases, the presence of a portable urine analyzer at home can become indispensable, with the help of the device you can quickly send the results of the analysis to your pediatrician, and the doctor will help you understand the difficult situation and make the right decision.
Prevention
- Regular bladder and bowel movements.
- Adequate fluid intake.
- Hygiene of the external genital organs.
Indications for preventive treatment:
- presence of vesicoureteral reflux grade 2–5;
- recurrence of UTI infection;
- severe anomalies in the development of UTI before surgical correction.

The duration of prophylaxis is selected individually: usually at least 6 months.
It is convenient to track the need for initiation of prophylactic treatment and its effectiveness by monitoring a complete urinalysis. In these cases, a portable urine analyzer is indispensable.
Case management and rehabilitation
- If UTIs recur (more than 2 in girls, more than 1 in boys), testing to rule out VUR is recommended.
- In the first 3 months of observation in acute pyelonephritis and after exacerbation of chronic pyelonephritis, a clinical urinalysis is performed 1 time in 10 days, within 1-3 years - monthly, then - 1 time in 3 months. The presence of a portable urine analyzer at home allows you to take an analysis avoiding contact with infectious patients (in clinics and laboratories).
- Urine culture is performed when leukocyturia appears and / or with unmotivated temperature rises without catarrhal phenomena.