Pile treatment in pregnancy
Dealing with hemorrhoids during pregnancy
Hemorrhoids can also result from constipation since pregnancy hormones cause your bowels slow down. When stool is hard, the extra straining to eliminate it can put pressure on veins in your rectal area, causing them to become inflamed and bulge. "On top of that, higher progesterone levels cause the walls of the veins to relax and allow them to swell more easily," says Dr. Harris.
If you had hemorrhoids before pregnancy, you're more likely to have them during pregnancy. They can also develop postpartum because of pushing during labor.
How can you prevent hemorrhoids during pregnancy?
Your body undergoes a lot of changes when you're expecting, and swelling veins can be one of them. Talk to other expectant moms during prenatal classes, share experiences or ask your instructor about natural remedies.
These steps may help you avoid hemorrhoids during pregnancy:
Avoid constipation
- Eat a high-fiber diet.
Choose from fresh avocados, beans, and other fruits and vegetables.
- Don't delay going to the bathroom when you feel the urge. Make sure you don't sit on the toilet longer than necessary because this puts pressure on your rectal area.
- If you're already constipated, ask your healthcare provider about a fiber supplement or stool softener.
- Choose a food-based prenatal vitamin. Synthetic vitamins, especially iron, can cause constipation. Food-based prenatal vitamins are more absorbable.
Keep moving
- Get regular (and safe) exercise right up to your due date — as long as your provider says it's OK.
- Do Kegel exercises. They increase circulation in the rectal area and strengthen the muscles around the anus.
- Don't sit or stand for long stretches of time. If your job involves sitting at a desk, get up and move around for a few minutes every hour or so.
Promote good habits
- Drink plenty of water and other fluids.
 If you aren't drinking enough, your body will reabsorb water through the colon, leaving dry stool that's hard to push out.
If you aren't drinking enough, your body will reabsorb water through the colon, leaving dry stool that's hard to push out. - Lie on your side when sleeping, reading or watching TV to take the pressure off your rectal veins.
- Try not to gain more than the recommended amount of weight because the more you gain, the more pressure on the rectum.
How can you treat symptoms during pregnancy?
If you experience symptoms, try one of these remedies:
- Cold therapy can help reduce swelling and bring temporary relief. Apply an ice pack (with a covering) to the affected area.
- Soak in warm water several times a day. If you don't have a bathtub, you can buy a sitz bath. After getting out of the tub, pat the area dry.
- If sitting is uncomfortable, get a donut-shaped pillow to ease the pressure.
- Apply witch hazel pads to the area and change the pads frequently. Witch hazel has a cooling effect and helps reduce swelling.
- Baking soda – used wet or dry – can be applied topically to help alleviate itching.

- Coconut oil can relieve pain and inflammation. So can pure aloe vera without added chemicals and fragrances, or arnica.
- Stay clean and use soft, unscented toilet tissue or unscented wipes to avoid more irritation in the affected area.
- Acupuncture can also help.
When should you see your healthcare provider?
Consult your provider if preventive efforts and home treatments don't help, or if you have severe pain or rectal bleeding. In some cases, you may need professional help shrink your hemorrhoids.
Also, always check with your provider before taking any medication for hemorrhoids while you're pregnant. There are a lot of hemorrhoid relief products available. Keep in mind that most of these products should be used for no more than a week to avoid such side effects as skin irritation or thinning.
For many women, hemorrhoid symptoms resolve after delivery. If they persist, surgical treatment might be recommended.
Pregnancy Hemorrhoids: Causes, Risks, Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.No one likes to talk about them, but hemorrhoids are a fact of life for many people, especially during pregnancy. Hemorrhoids are simply veins inside or outside of your anus that have become large and swollen.
Hemorrhoids are simply veins inside or outside of your anus that have become large and swollen.
Also called piles, they can look like varicose veins when outside your body. Hemorrhoids develop frequently during pregnancy, especially in the third trimester and during and shortly after childbirth.
You may have hemorrhoids only during pregnancy, or you may have them at other times of your life as well.
The causes of your hemorrhoids may be unique to pregnancy. You can often treat or prevent hemorrhoids with home-based remedies and lifestyle adjustments.
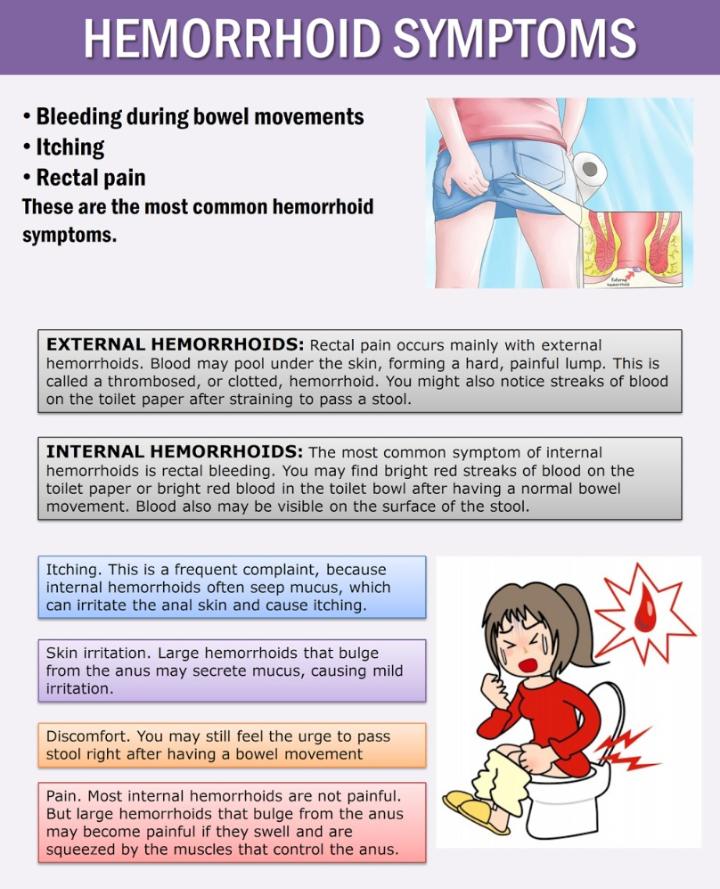
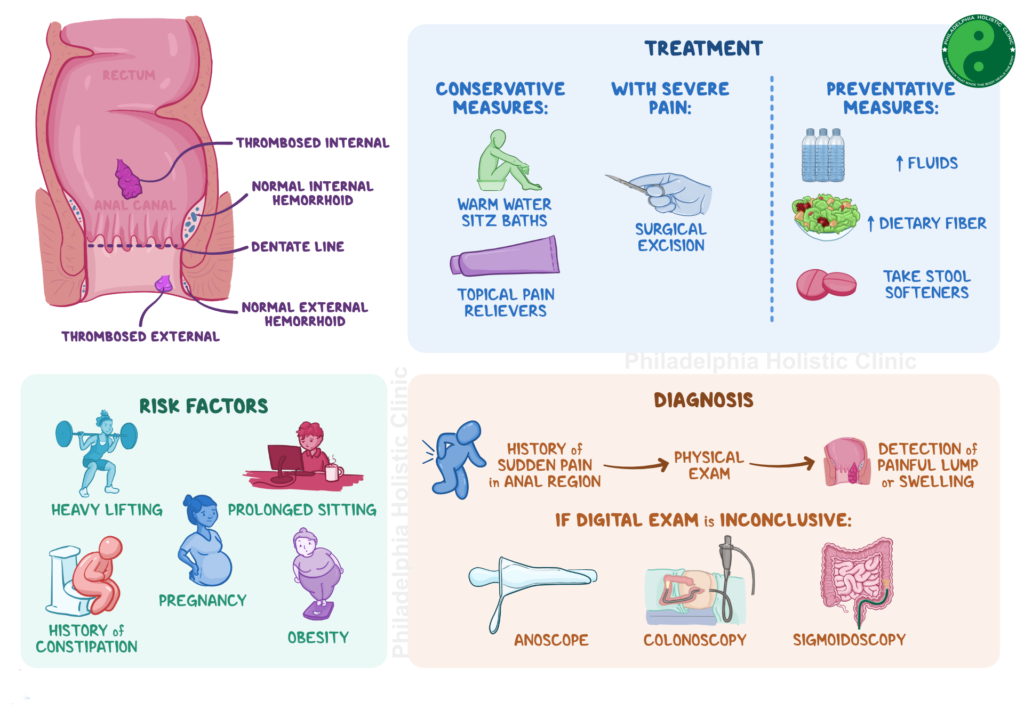
There are two types of hemorrhoids: internal hemorrhoids and external hemorrhoids. Each type of hemorrhoid can have different symptoms.
Internal hemorrhoids
Internal hemorrhoids form inside your body, within the rectum. Because they are concealed in the rectum, they can be harder to diagnose. Some internal hemorrhoids can prolapse, meaning they extend outside of the anal opening.
Although internal hemorrhoids can cause bleeding, they typically don’t cause pain. This is because they are located in an area that doesn’t have nerve endings. However, if an internal hemorrhoid prolapses, it can be extremely painful.
This is because they are located in an area that doesn’t have nerve endings. However, if an internal hemorrhoid prolapses, it can be extremely painful.
External hemorrhoids
External hemorrhoids form outside of your body. They’re located near the anus and covered by skin. This skin is extra-sensitive and can become inflamed.
An external hemorrhoid can hurt if it becomes swollen or develops a blood clot.
If a blood clot forms in a hemorrhoid, it can cause sudden, severe pain. The pain often gets worse within the first 48 hours, then improves over several days.
The symptoms of hemorrhoids can vary depending on the type of hemorrhoids you have.
Common hemorrhoid symptoms
- bleeding (you may notice blood when you wipe after a bowel movement)
- painful bowel movements
- a raised area of skin near your anus
- itching
- burning
- swelling
Generally, you will experience these symptoms with external hemorrhoids. You may have no symptoms with internal hemorrhoids.
You may have no symptoms with internal hemorrhoids.
You may also develop a blood clot in an external hemorrhoid. This is known as a thrombosed hemorrhoid. They are generally hard, inflamed, and more painful.
It’s possible to push out an internal hemorrhoid when having a bowel movement. If this occurs, you may experience bleeding and discomfort.
Up to 50 percent of pregnant women develop hemorrhoids.
Causes
- increased blood volume, leading to larger veins
- pressure on veins near your anus from the baby and your growing uterus
- changing hormones
- constipation
You may be more susceptible to constipation during pregnancy than at other times of life. One 2014 study found that among 280 pregnant women, 45.7 percent experienced constipation.
This constipation may be due to:
- sitting for long periods of time
- changing hormones
- taking iron or other supplements
Your hemorrhoids may disappear completely after pregnancy and delivery without any treatment as your hormone levels, blood volume, and intra-abdominal pressure decrease after delivery.
The most common times hemorrhoids develop during pregnancy is in your third trimester and during and immediately after childbirth. You may develop hemorrhoids from childbirth if you experience extended straining during the second stage of labor.
You can try many home remedies and lifestyle modifications to reduce hemorrhoids.
It’s best not to ignore them, though. Untreated hemorrhoids may get worse with time and cause complications such as increased pain or, in rare cases, anemia from bleeding.
You may need to reach out to a healthcare professional to diagnose and treat your hemorrhoids. Since hemorrhoids are not the only cause of bleeding near your anus, it’s always a good idea to speak with a doctor if you notice new bleeding when you wipe or in your stool.
Home remedies for hemorrhoids
There are many steps you can take at home to relieve and prevent hemorrhoids. Here are some ideas.
- Use wipes or pads that contain witch hazel.
- Use gentle, flushable wipes when you have a bowel movement.
- Use a sitz bath or soak in clean warm water for 10 minutes at a time a few times a day.
- Take Epsom salt baths in warm water that’s not too hot.
- Hold an ice pack on the area for a few minutes several times a day.
- Move around frequently and try not to sit for too long to avoid extra pressure on your anus.
- Drink lots of water and eat foods high in fiber to help keep stools soft.
- Avoid straining while having a bowel movement or sitting on the toilet for long periods of time.
- Perform Kegel exercises to strengthen muscles.
You can shop for many of these items online:
- hemorrhoid pads
- flushable wipes
- sitz bath
- Epsom salt
- ice bags
You may want to speak with a doctor before treating hemorrhoids at home. This will ensure you get a proper diagnosis and understand the treatment options available to you.
Medical treatment for hemorrhoids
During pregnancy, always talk with your doctor before taking any medication, including those you apply to your skin (topical). This will ensure treatments do not pose a risk to your baby.
This will ensure treatments do not pose a risk to your baby.
Topical over-the-counter or prescription treatments may help hemorrhoids. These medications often include pain-relieving or anti-inflammatory ingredients.
Creams or ointments that contain hydrocortisone-pramoxine can be especially effective for reducing pain, inflammation, and itching caused by hemorrhoids. But these ingredients may not be safe for pregnancy. Make sure to discuss them with a doctor.
The doctor may also be able to recommend a safe laxative or a suppository to relieve constipation.
Some prescription oral treatments, like ruto-sides and hidrosmine, are available for treating hemorrhoids, but they may not be safe during pregnancy or if you’re breastfeeding or chestfeeding.
Other medical treatment options for hemorrhoids includes:
- Rubber band ligation. During banding, a small rubber band is placed around the base of a hemorrhoid. The band stops the flow of blood into the hemorrhoid and eventually the hemorrhoid will fall off.
 This usually takes 10 to 12 days. Scar tissue is formed during this process that helps prevent the hemorrhoid from recurring in that same location.
This usually takes 10 to 12 days. Scar tissue is formed during this process that helps prevent the hemorrhoid from recurring in that same location. - Sclerotherapy. A chemical solution is injected directly into the hemorrhoid. This causes it to shrink and to form scar tissue. It’s possible for a hemorrhoid to return after this treatment.
- Hemorrhoidectomy. A hemorrhoidectomy is a surgical procedure to remove hemorrhoids. It’s associated with several risks, including general anesthesia, risk of damage to the muscles of the anus, more pain, and a longer recovery time. As a result, this treatment is only recommended for severe hemorrhoids or when there are complications, such as multiple hemorrhoids or hemorrhoids that have prolapsed.
- Stapledhemorrhoidopexy. The hemorrhoidal tissue is placed back inside the anus and held in place using surgical staples.
Your doctor may suggest packing the site of the hemorrhoid with absorbent bandages to avoid excessive bleeding.
You can try to reduce hemorrhoids or prevent them from developing in several ways.
Prevention tips
- Eat a diet full of fiber-rich foods, like vegetables and fruits.
- Drink plenty of water to help keep your stools soft and your bowel movements regular.
- Avoid straining when using the toilet.
- Avoid sitting on the toilet for long periods of time.
- Pass a bowel movement as soon as you feel it coming — not holding it in or delaying.
- Move around as much as you can by exercising and avoid long periods of sitting.
- Talk with your doctor about adding a supplement to your diet that helps avoid constipation.
If you’re pregnant and think you have hemorrhoids, be sure to talk with your doctor about the symptoms you’re having.
Contact a doctor if you have:
- hemorrhoid symptoms that fail to improve after receiving treatment
- recurring hemorrhoids
- fever or chills
- pus oozing from your hemorrhoid
- severe bleeding or bleeding that won’t stop
- severe pain
Hemorrhoids during pregnancy are common. Seek medical treatment if you discover a hemorrhoid since they can get worse.
Seek medical treatment if you discover a hemorrhoid since they can get worse.
There are many home treatments you can try, but you may need medical treatment as well. Talk with your doctor about any treatment, including over-the-counter creams, to be sure it won’t affect your pregnancy.
After childbirth, your hemorrhoids may clear up on their own without any treatment.
Treatment of hemorrhoids during pregnancy and after childbirth
Pregnancy and childbirth are often provoking factors for the development of hemorrhoids. Hemorrhoids (from Latin - bleeding) - a disease that occurs as a result of overflow of blood in the venous plexuses located in the anus. It is these dilated, altered veins that are called hemorrhoids.
Hemorrhoids overflow with blood due to a sedentary lifestyle, improper, irrational and irregular nutrition, as well as due to excess weight. Of great importance in the occurrence of hemorrhoids is heredity.
Congestion of blood in the veins of the small pelvis is facilitated by the use of drugs, such as oral contraceptives, antibiotics, laxatives. Of course, the abuse of alcohol and smoking has a negative impact on the state of health in the field of proctology. Some sports: equestrian, cycling, auto and motor sports, rowing, weight lifting - all this can provoke hemorrhoids.
Of course, the abuse of alcohol and smoking has a negative impact on the state of health in the field of proctology. Some sports: equestrian, cycling, auto and motor sports, rowing, weight lifting - all this can provoke hemorrhoids.
Pregnancy and childbirth also contribute to the development of hemorrhoids. Pregnancy changes a lot in a woman's life, the load on the female body increases by 2 times, and can provoke the development of hemorrhoids, and childbirth can aggravate it. According to statistics, women who have given birth suffer from hemorrhoids 5 times more often than those who have not given birth. During pregnancy and during childbirth, the enlarged uterus presses on the pelvic floor, due to which the venous plexuses fill with blood.
Also constipation, which very often accompanies pregnancy, worsens the situation. The number of pregnancies and childbirth, as well as the age of the pregnant woman affect the risk of developing hemorrhoids.
Hemorrhoids: what to do?
Unfortunately, hemorrhoids occur quite often in pregnant women. The only correct decision, if there are doubts about health in this delicate area, is to go to the doctor and start treatment. After all, hemorrhoids in a pregnant woman can disrupt the normal course of pregnancy in the later stages, as well as affect the course of childbirth and the postpartum period.
The only correct decision, if there are doubts about health in this delicate area, is to go to the doctor and start treatment. After all, hemorrhoids in a pregnant woman can disrupt the normal course of pregnancy in the later stages, as well as affect the course of childbirth and the postpartum period.
Fear and hope for "maybe" often lead to the fact that hemorrhoids pass the first stage, the health of a pregnant woman worsens, the disease progresses. Running hemorrhoids can cause anemia (a decrease in the amount of hemoglobin), diseases of the musculoskeletal system (for example, arthritis), the genitourinary system, and skin.
Manifestations of hemorrhoids resemble some other diseases of the rectum, and even oncological diseases.
According to the severity of painful manifestations, 3 degrees of severity of acute hemorrhoids in pregnant women are distinguished:
- I degree. There are small, painful nodes in the anus, accompanied by itching and burning in the anus, discharge that is not purulent.
 All these manifestations periodically pass.
All these manifestations periodically pass. - II degree. Hemorrhoids are enlarged. Pain in the anus is increasing.
- III degree. Swelling and redness growing. Large cyanotic-purple internal hemorrhoids protrude from the anus. If hemorrhoids are not treated at this stage, then the necrosis of the nodes may begin with the appearance of black areas on them. Complications of this stage can be paraproctitis (inflammation of the tissues around the rectum), infringement of a thrombosed internal node.
The effect of pregnancy and childbirth on hemorrhoids
As a rule, childbirth provokes a sharp exacerbation of hemorrhoids, even if during pregnancy this disease did not become exacerbated.
It's all about the very mechanism of labor activity: when the baby's head passes through the small pelvis, the maternal organs and tissues located in this area are squeezed, and first of all, the venous plexuses.
Hemorrhoids increase, acquire a denser consistency. During contractions, and especially attempts, the nodes may bulge, turn red or even turn blue. In other words, the very mechanism of childbirth leads to a complication of hemorrhoids, provokes the prolapse of internal nodes and even their rupture.
Prevention and treatment of hemorrhoids during pregnancy and after childbirth
First, a pregnant woman needs to get rid of constipation and improve bowel function without prolonged straining.
This requires a diet rich in fruits and vegetables. Any alcoholic drinks, salty, spicy, spicy, pickled, peppery dishes are strictly prohibited. Do not eat fatty foods, fatty meats, high-calorie dairy products and buns, you need to limit the use of onions, mustard, black bread, legumes, unripe fruits and berries. It is recommended to eat broccoli, corn, carrots, ripe apples, beets, cauliflower, potatoes, raisins, prunes, dried apricots and honey, cereals, especially barley or oatmeal.
Physiotherapy exercises are indicated for pregnant women in order to prevent hemorrhoids.
It is important to avoid hypothermia during pregnancy.
It is necessary to observe the hygiene of the anus, especially after each emptying.
Proctologists distinguish three groups of pregnant women with hemorrhoids:
- The first group - - is women in a position with asymptomatic hemorrhoids. For them, preventive measures are recommended - diet, physiotherapy exercises, walks, an anus water toilet after defecation, laxative herbs, laxatives.
- The second group - - these are women who have constipation, bleeding, pain during defecation, anal itching, that is, patients with the first or second stage of the development of the disease. As a rule, for sick women at these stages of hemorrhoids, proctologists recommend treatment with suppositories and ointments, warm sitz baths with a weak solution of potassium permanganate, herbal infusions, and drugs taken orally.

- The third group - - these are pregnant women with an advanced form of hemorrhoids, with prolapse of internal nodes and frequent exacerbations of the disease, that is, those who are subject to hospitalization and surgical treatment.
Pregnant women with these complications of hemorrhoids should be treated surgically (they undergo hemorrhoidectomy - excision of the nodes) or minimally invasive methods of treatment (minor or bloodless operations). The minimally invasive methods used in Only Clinic include sclerotherapy - the introduction of special sclerosing drugs into the node, “blinding” the walls of the node; ligation - the node is pinched with a special latex ring, which causes rejection in 7-10 days, the death of the node; infrared photocoagulation and laser coagulation (exposure to a laser or high temperature on the base of the hemorrhoid at 3-5 points; in this case, a burn occurs, which subsequently causes necrosis of the node with its subsequent falling off; the process also takes 7-10 days).
If the condition of the pregnant woman allows, then the proctologists of the Only Clinic try to postpone all these interventions for the period when the woman recovers from childbirth.
A set of exercises for hemorrhoids for pregnant women. Recommendations of doctors-proctologists of Only Clinic:
Starting position (s.p.) - standing, stretch your arms in front of you, feet shoulder-width apart. Turn the body to the right, without taking your feet off the floor, and take your right hand as far back as possible - inhale. Return to starting position - exhale, turn to the left. Repeat 5 times on each side.
- I.p. - standing, hands raised in front of you, fingers clasped into the castle. Perform body turns to the right and left, moving your arms as far back as possible. Repeat the exercise 5 times in each direction.
- I.p. - sitting on the floor, resting his hands behind. Bend your knees, while moving the heels can not be torn off the floor.
 Slowly extend your legs. Repeat 5 times.
Slowly extend your legs. Repeat 5 times. - I.p. - sitting, spread your legs to the sides as much as possible, while the legs should be firmly pressed to the floor, do not bend your knees if possible. Lean forward and touch your right and left feet alternately with your hands as far as possible, then straighten up. Repeat the slopes 5-7 times (recommended for the first and second trimester only).
- I.p. - sitting in the same way as in the previous exercise, but perform tilts to the sides; the opposite hand is on the belt. Repeat 5 times in each direction (recommended for the first and second trimester only).
- I.p. - lying on your back, arms along the body. Pull the legs bent at the knees to the stomach and return to the starting position (recommended only for the first and second trimester). Repeat 7-10 times.
- I.p. - lying on the right side, the right arm is bent at the elbow and lies under the head. Bend the left leg at the knee and press it to the stomach, you can help yourself with your left hand.
 Repeat 7-10 times. Then repeat the exercise, lying on your left side (recommended only for the first and second trimester).
Repeat 7-10 times. Then repeat the exercise, lying on your left side (recommended only for the first and second trimester). - I.p. - Sitting on a chair. Extend the right arm to the side, lift the left leg, bent at the knee, forward and to the left, trying to bring it to the lateral surface of the abdomen, helping yourself with your left hand - exhale. Return to starting position - inhale. Repeat for both legs 5 times. Recommended for third trimester.
Careful attitude to one's health, timely access to a doctor, examination, correct diagnosis and timely treatment will help to avoid or minimize hemorrhoidal problems.
Treatment of hemorrhoids during pregnancy | Articles of the medical center "SM-Clinic"
Hemorrhoids - a disease associated with inflammation and pathological expansion of the hemorrhoidal veins that form nodes around the rectum. This is a very common disease, its cause is usually venous blood stagnation in the lower body and legs.
The development of hemorrhoids takes place gradually - in the initial stage, there is heaviness and itching in the anus, pain, constipation, later - bleeding, sagging and prolapse of elastic hemorrhoids.
Factors that cause hemorrhoids are a sedentary lifestyle, unhealthy diet, obesity, alcohol abuse, cirrhosis of the liver of life.
This disease often accompanies pregnancy - about half of women who are expecting a child suffer from it. The main reasons for pregnant women are the pressure of the growing uterus on the lower abdomen, which compresses the veins, and constipation due to low intestinal motility.
In healthy women, hemorrhoids can develop in the second half of pregnancy, but if there is a hereditary predisposition, or the symptoms of hemorrhoids were manifested before pregnancy, then hemorrhoids can develop at an earlier date - already from the 12th week.
Symptoms of hemorrhoids during pregnancy
Hemorrhoids during pregnancy can occur in two forms:
- acute;
- chronic.

The acute form is characterized by the sudden formation of a blood clot in the veins of the rectum, which causes burning pain, especially after the defecation process. Dense external nodes are formed, the diameter of which can reach 2-3 cm, the skin under them swells and turns red.
After 5-10 days, the acute form becomes chronic - the nodes soften and swell only when straining. The process is accompanied by discomfort in the anus and itching.
Blood appears in the fecal masses, sometimes in fairly large quantities, hemorrhoids can fall out of the anus, self-adjusting after some time. There may be no pain, there may be a feeling of incomplete emptying of the intestine, discomfort, bloating. Walking and sitting become painful.
Treatment of hemorrhoids during pregnancy
The main methods of treatment of non-acute hemorrhoids during pregnancy are strict adherence to diet and hygiene rules. The diet prescribed by a dietitian should help avoid constipation and regulate bowel movements - dried fruits, nuts, cereals, and sour-milk products are recommended for this. Spicy foods, rich products, strong tea should be excluded.
Spicy foods, rich products, strong tea should be excluded.
For hygiene procedures, it is recommended to use wet toilet paper, wash the anus after defecation. If external nodes occur, you can take baths with a weak solution of chamomile or potassium permanganate.
To reduce blood stasis, it is necessary to perform preventive gymnastics - its main exercises should be aimed at stimulating the muscles of the pelvis, anus and legs. In addition, it is necessary to adjust the daily routine - to take walks, combining them with moderate rest and sleep.
If these measures do not bring the desired result, it is possible to use medicines - suppositories, ointments, creams. However, it is worth remembering that any drug treatment must be agreed with the gynecologist - during pregnancy, self-medication and the use of drugs without a prescription is unacceptable.
If conservative treatment is ineffective, surgery may be required, but usually during gestation it is performed only in extreme cases, with careful monitoring of the proctologist and surgeon.