Period or miscarriage clots
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
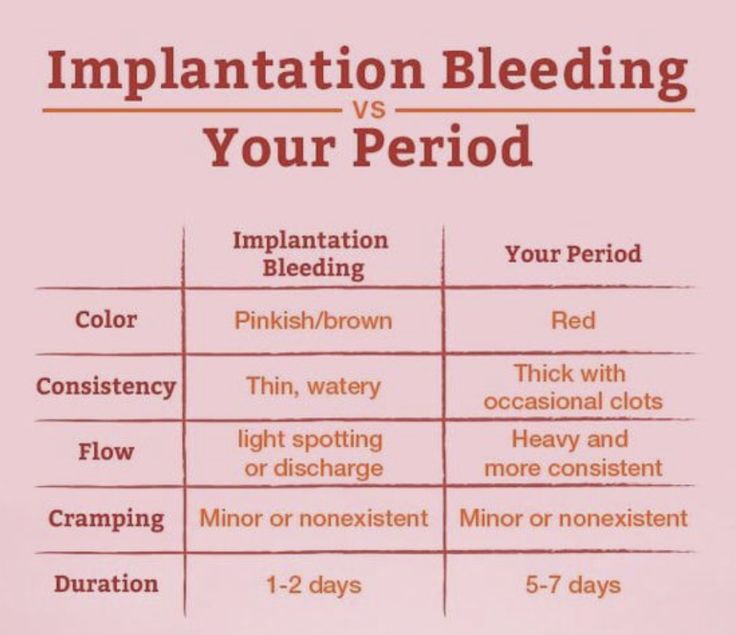
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
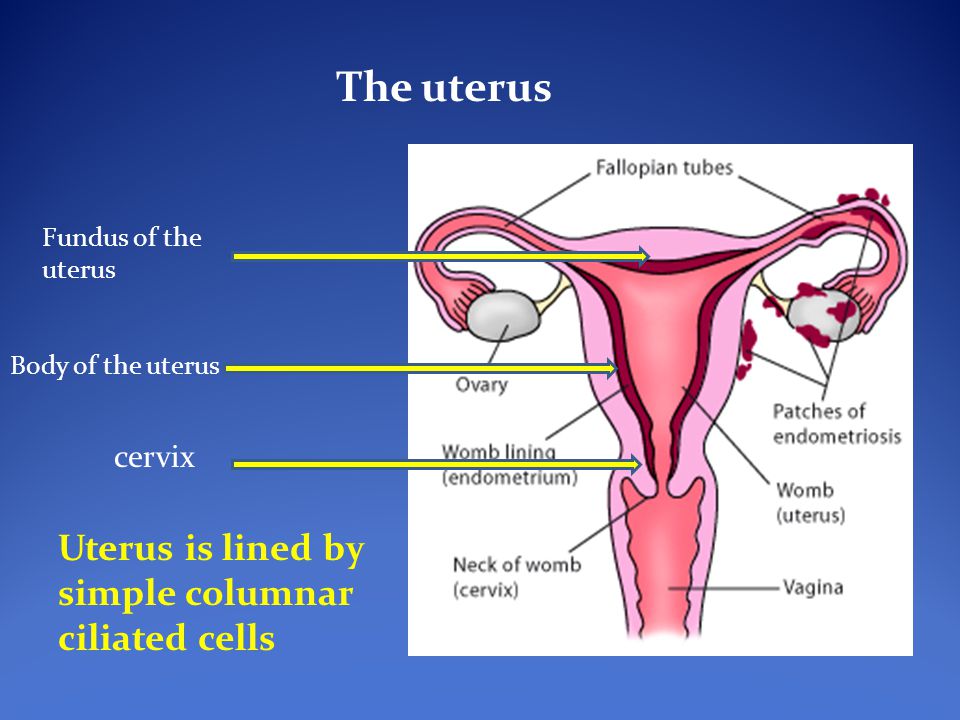
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
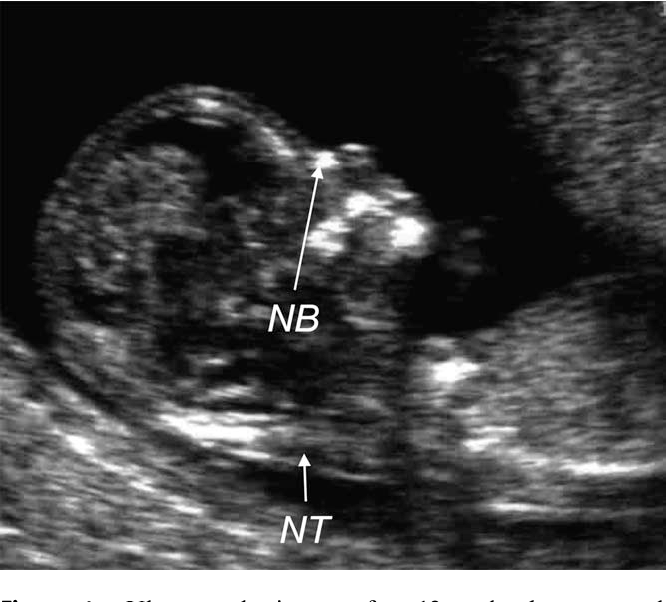
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress. If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining.
 This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development.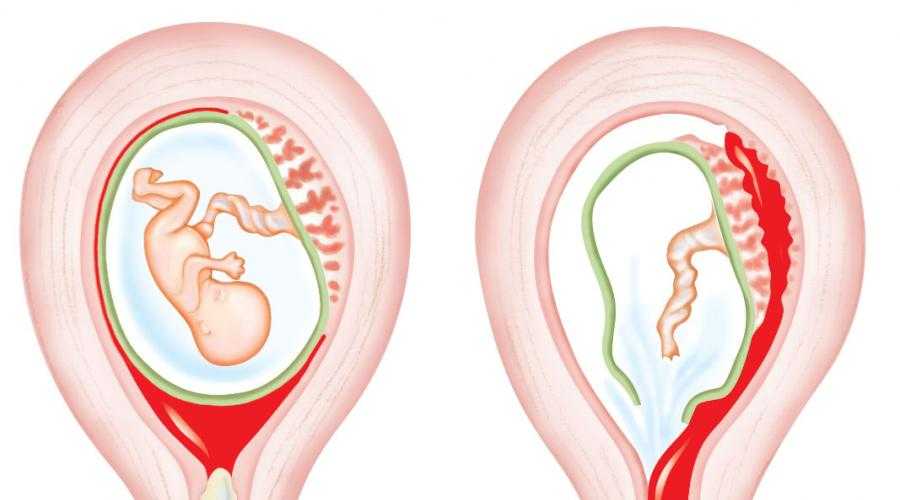 Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant.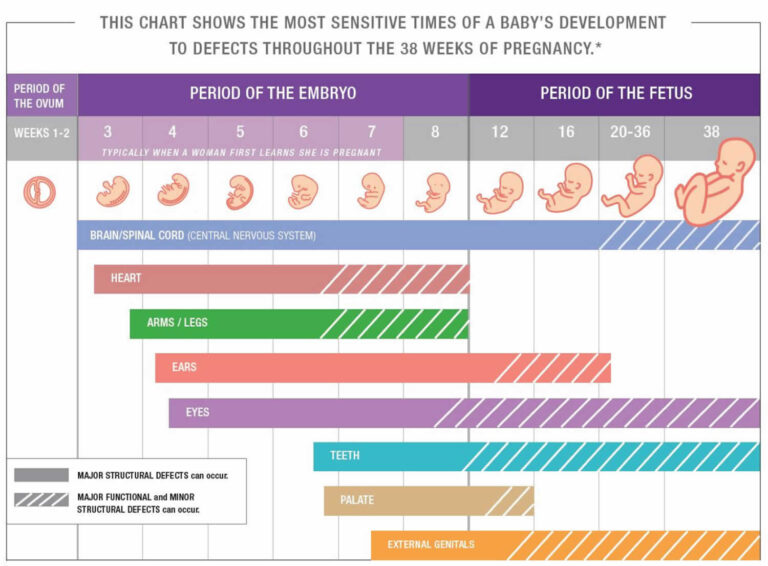 You can ovulate and become pregnant within two weeks of an early miscarriage.
You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week.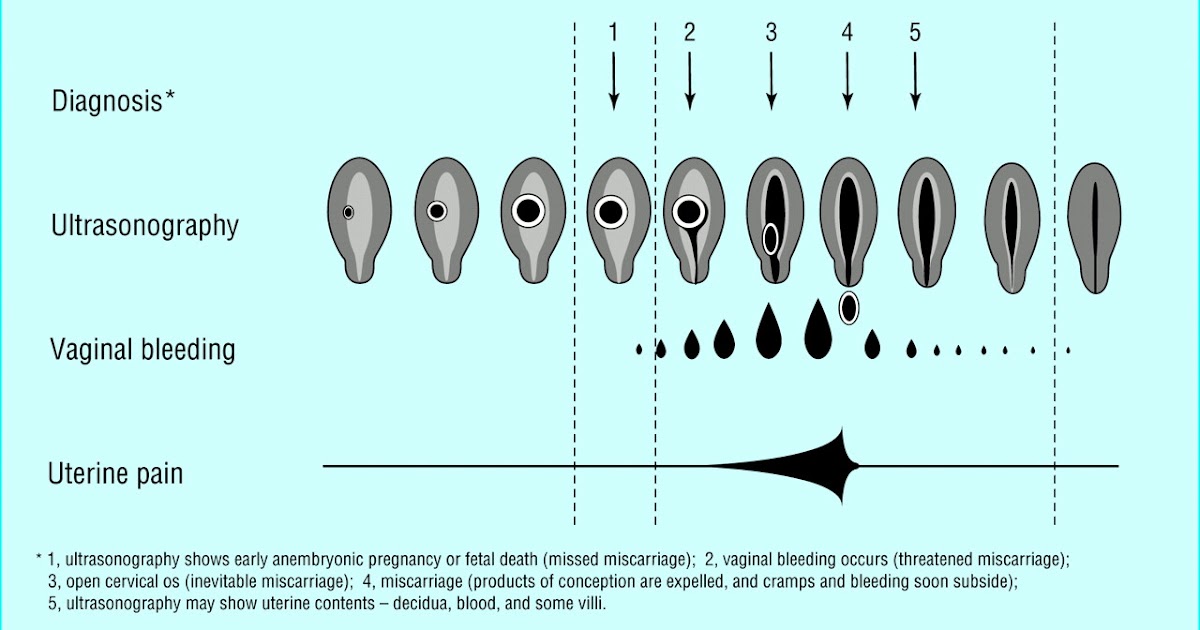 It will take about four to eight weeks for your regular period to return.
It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester.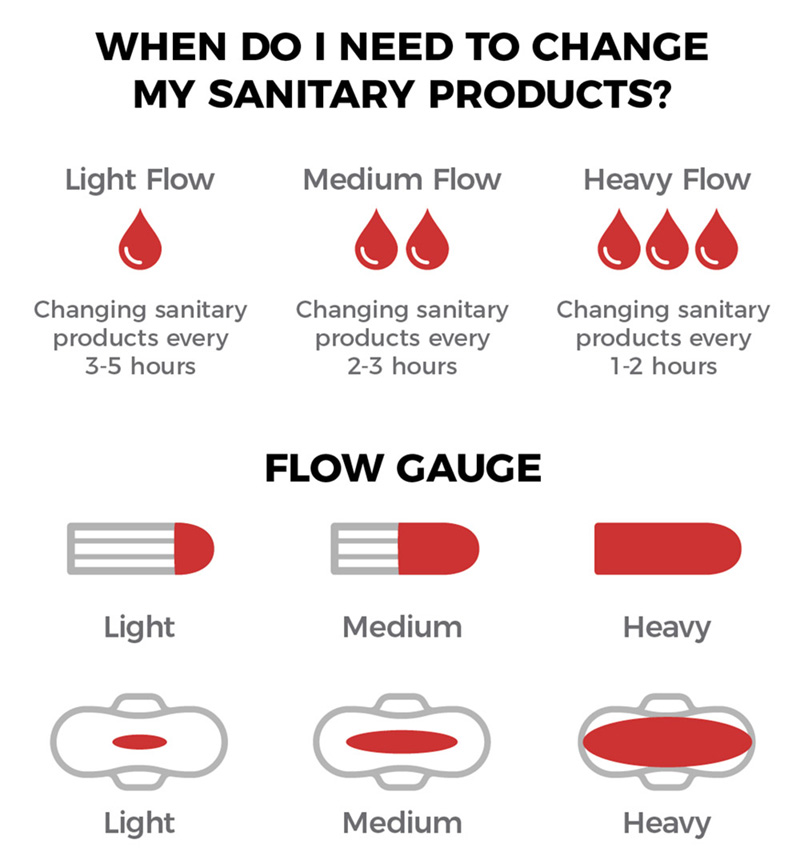 It happens in about 10 percent of known pregnancies.
It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.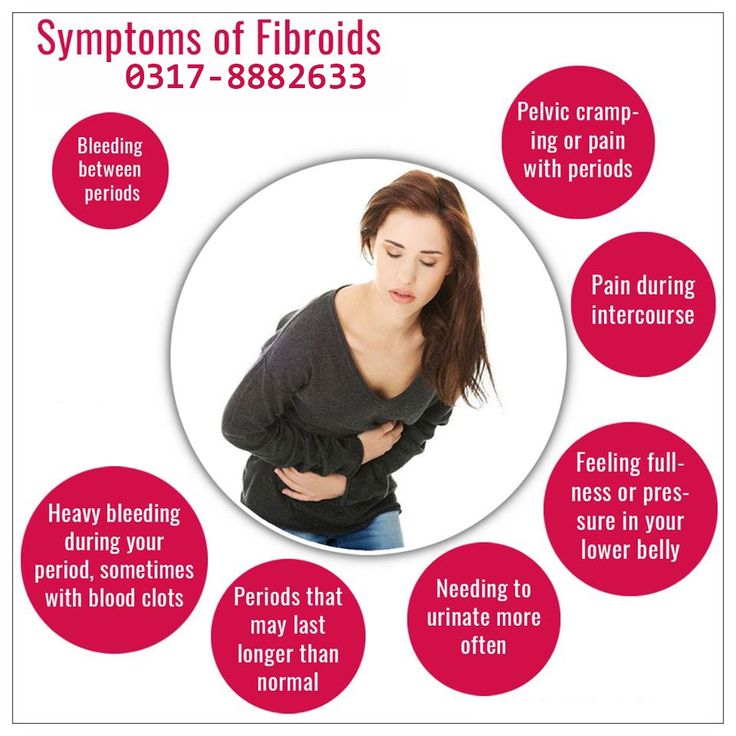
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress. If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.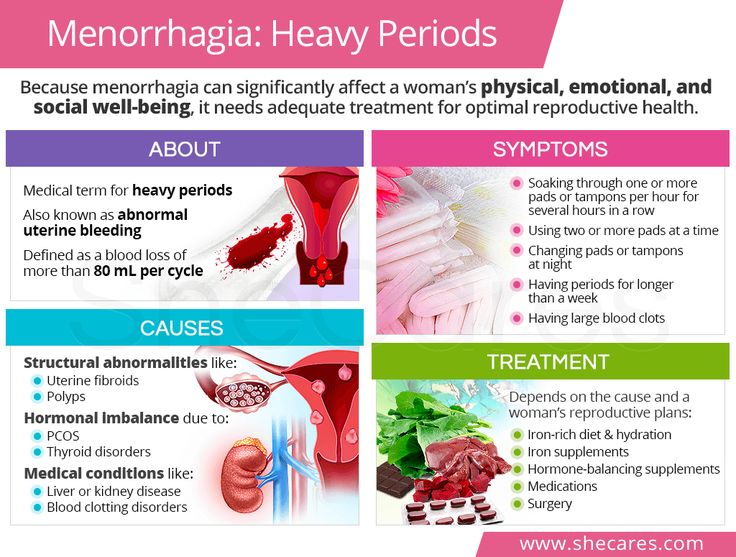
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining.
 This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.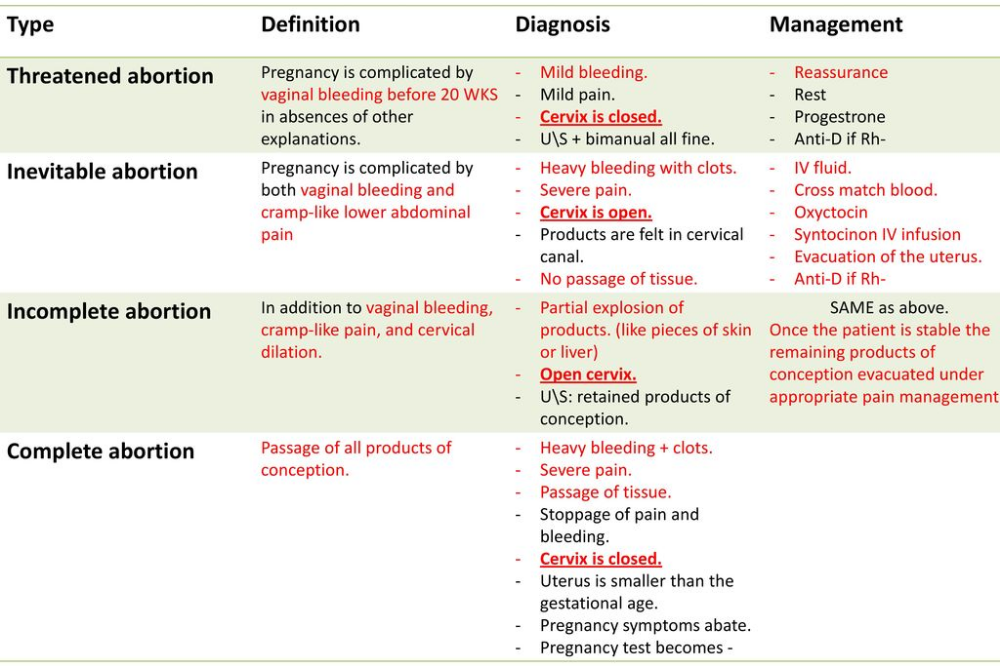
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week. It will take about four to eight weeks for your regular period to return.
It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
How to identify a miscarriage: early signs
15-20% of pregnant women experience early pregnancy loss. It is important to know the earliest symptoms of a miscarriage in order to have time to seek help and, possibly, save the pregnancy.
It is important to know the earliest symptoms of a miscarriage in order to have time to seek help and, possibly, save the pregnancy.
Vera Ermakova
According to a study published in 2015 in the American Journal of Obstetrics and Gynecology, 41% of women who experienced a miscarriage felt guilty about what happened. Meanwhile, according to the American College of Obstetricians and Gynecologists (ACOG), at least half of miscarriages (pregnancy losses before 20 weeks) are due to chromosomal abnormalities that cannot be prevented. Nevertheless, given that up to 20% of pregnancies end in miscarriages, it is worth knowing its early signs in order to consult a doctor in time. nine0003
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
Very heavy bleeding
Not all bleeding that a pregnant woman may experience is indicative of a miscarriage: for example, small spots of blood may appear when a fertilized egg is implanted in the uterus.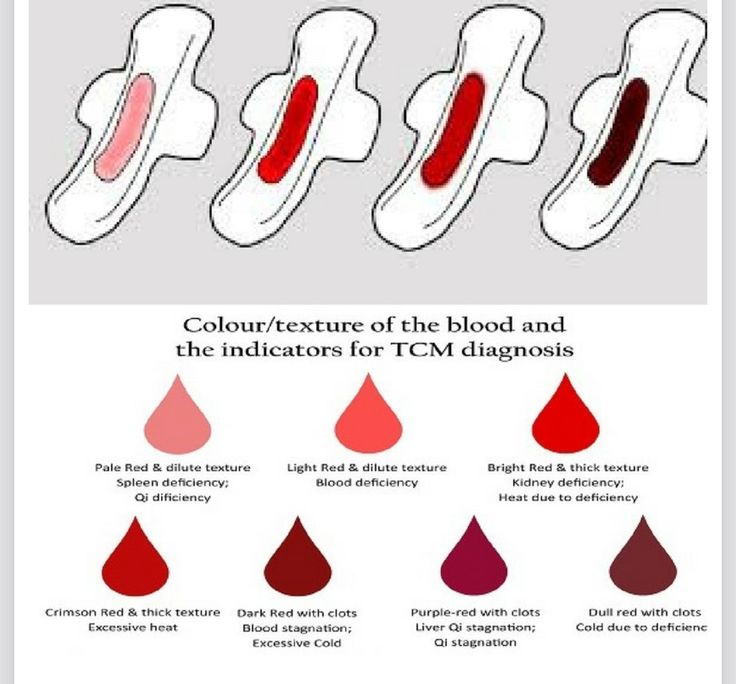 In addition, the developing placenta can also cause bleeding. But if the color of the discharge is bright red and they themselves are very intense, you should consult a doctor - this can be a dangerous sign. nine0003
In addition, the developing placenta can also cause bleeding. But if the color of the discharge is bright red and they themselves are very intense, you should consult a doctor - this can be a dangerous sign. nine0003
Pink discharge and tissue clots
Not only blood: it is worth paying attention to any discharge that you may encounter during pregnancy. Light pink vaginal fluid, which is also accompanied by the release of clots, is a very alarming symptom.
Pain and cramps
The cramps and cramps that many women experience during their premenstrual period or during their period are unpleasant, but in most cases they are not dangerous. But if you experience these sensations during pregnancy, you should consult a doctor as soon as possible. Cramps, pains and spasms can signal not only a miscarriage, but also an ectopic pregnancy, a deadly condition. nine0003
Lower back pain
During pregnancy, even if it is normal, the pressure on the back and especially on the lumbar increases. Therefore, almost all pregnant women feel pain in this area and discomfort in this area, from slight to very strong. But since pain and cramps in the lumbar region can also warn of a miscarriage (and especially if they are accompanied by bleeding or abdominal pain), you should definitely tell your doctor about them.
Therefore, almost all pregnant women feel pain in this area and discomfort in this area, from slight to very strong. But since pain and cramps in the lumbar region can also warn of a miscarriage (and especially if they are accompanied by bleeding or abdominal pain), you should definitely tell your doctor about them.
Absence of fetal heartbeat
Sometimes a miscarriage is not accompanied by any "external" symptoms, and in these cases, the absence of a heartbeat in the fetus is the only manifestation. However, the disappearance of toxicosis and other signs accompanying the first trimester of pregnancy can also be considered an indirect symptom.
By the way: Miscarriage: 7 dangerous myths that have nothing to do with the truth
Pieces of meat during menstruation is an egg or a miscarriage? nine0001
#1
#2
9000 #3
#4
#5
You can't see an egg with the naked eye, no matter how hard you try.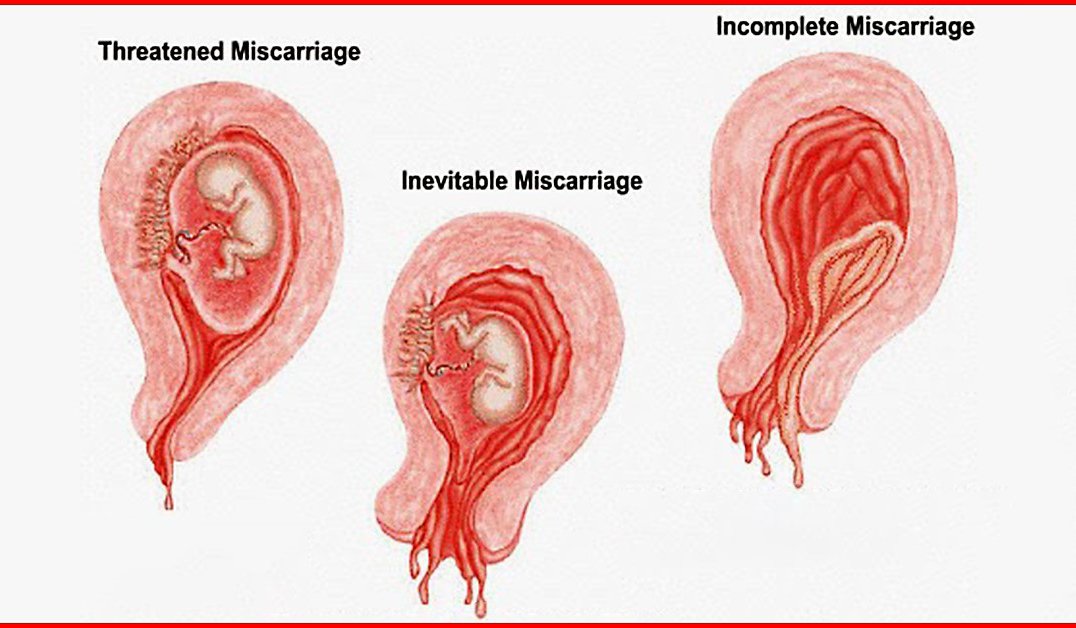
#6
Guest
is a piece of endometrium
#8
Your "piece of meat" is simply the largest endometrial clot. The egg itself is transparent and negligible for you to notice.
#9,0003
#10
#13
Epo Samurai
Gostnet, nifiga! it's the author's liver falling out. nine0003
Ahhahaaa))))))))))))))
#14
#15
#16
#18
#20,0003
#21
#22
Guest
Actually, blood clots are similar to pieces
#23
Miloskaya
I can’t straighten the monthly current, and there is already such traffic, there is already such traffic.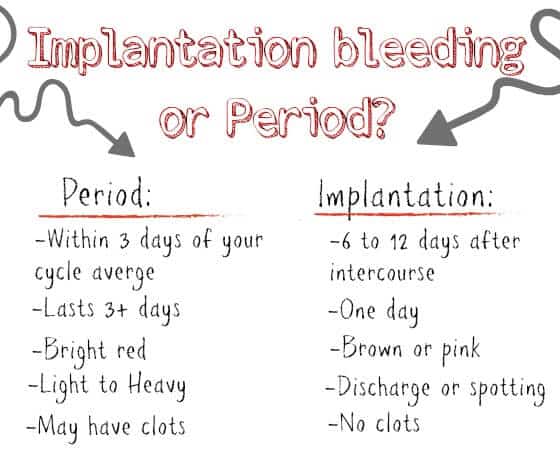 that she expects miscarriages every month.
that she expects miscarriages every month.
#24
Guest
The endometrium does not come out in pieces, donate blood for clotting for hemostasis and d_dimers, most likely you have a tendency to form thrombi. Not a good sign, fraught with endometriosis. nine0003
#25
KitKat
Endometrium is.... What kind of people have gone... they don't know shit about their body...
#26
Guest
why doesn't it come out in pieces? Well, not in pieces, of course, but formations up to 2cm. Is it a lot?
#27
Audrey
Guest
why doesn't it come out in pieces? Well, not in pieces of course, but formations up to 2cm.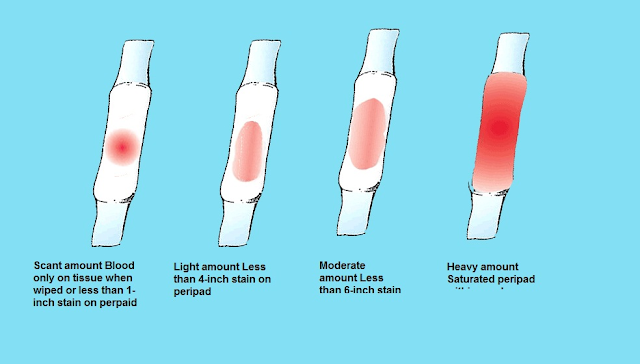 Is it a lot? nine0003
Is it a lot? nine0003
It always happens to me, even before pregnancy I asked the gynecologist when I wanted to get pregnant, then my period came with a delay, I thought it was a miscarriage, so she told me everything in detail! so it's ok! I have 1-2 pieces. such, it happens that they are very tiny or not
Woman.ru experts
-
Osipova Ksenia Andreevna
Psychologist
13 answers
nine0228 -
Maria Sinyapkina
Sexologist
71 answers
-
Maxim Sorokin
Practicing psychologist
846 responses
nine0228 -
Ivanova Svetlana
Coach
57 answers
-
Anna Antonchik
Female psychologist
122 answers
nine0228 -
Vladimir Titarenko
Fitness nutritionist
47 answers
-
Kremenetskaya Maria
Speech therapist - defectologist
17 answers
nine0228 -
Nikitina Anna Viktorovna
Specialist of Oriental practitioners
32 answers
-
Maria Burlakova
Psychologist
284 answers
nine0228 -
Tatyana Klimkova
Psychologist
80 answers
#28
Marquise
This is the endometrium, which grows by the beginning of menstruation and is rejected every month under the influence of hormones. The endometrium is rejected in the form of clots, the vessels at the site of its separation are exposed and bleed - this is the so-called. "period". nine0003
The endometrium is rejected in the form of clots, the vessels at the site of its separation are exposed and bleed - this is the so-called. "period". nine0003
You can't see an egg with the naked eye, no matter how hard you try.
#29
Anna
This is the endometrium. Nutrient "soil" for a fertilized egg, which covers the inner surface of the uterus during ovulation. If the egg is not fertilized, then this "soil" is rejected by the uterus and comes out in the form of bleeding. In the next cycle, the process is repeated. Your "piece of meat" is simply the largest endometrial clot. The egg itself is transparent and negligible for you to notice. nine0003
#30
Audrey
KitKat
The endometrium is.... What the hell are people. .. they don't know shit about their body...
.. they don't know shit about their body...
#31
Invented stories
-
I am infuriated with my children and grandchildren ...
966 answers
-
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000
The man immediately warned that all the property was registered to the children
789 answers
-
Such a salary - I don’t want to work
544 answers
-
Long lie 23.
How to destroy?
817 answers
-
Husband left, 2 months of depression... How will you cope if you are left all alone?
181 responses
9038
#32
She also told me that I was so meticulous, went for an ultrasound ahead of time, and found out that I was pregnant, and if I hadn’t, I wouldn’t have paid attention to these clots. He says that many women do not even know that during menstruation they have a spontaneous miscarriage for a short time.
He says that many women do not even know that during menstruation they have a spontaneous miscarriage for a short time.
So an ultrasound or hcg will give you a concrete answer.
Not very competently, but she told me as best she could.
#33
Guest
Author, I had a delay, went for an ultrasound, they said I was pregnant, the period was 2 weeks. And suddenly menstruation begins with huge clots. I arrive at the hospital, the doctor says she is no longer pregnant, everything came out in these clots. And she also told me that I was so meticulous, I went for an ultrasound ahead of time, and found out that I was pregnant, and if I hadn’t gone, I wouldn’t have paid attention to these clots. He says that many women do not even know that during menstruation they have a spontaneous miscarriage for a short time. So an ultrasound or hCG will give you a specific answer.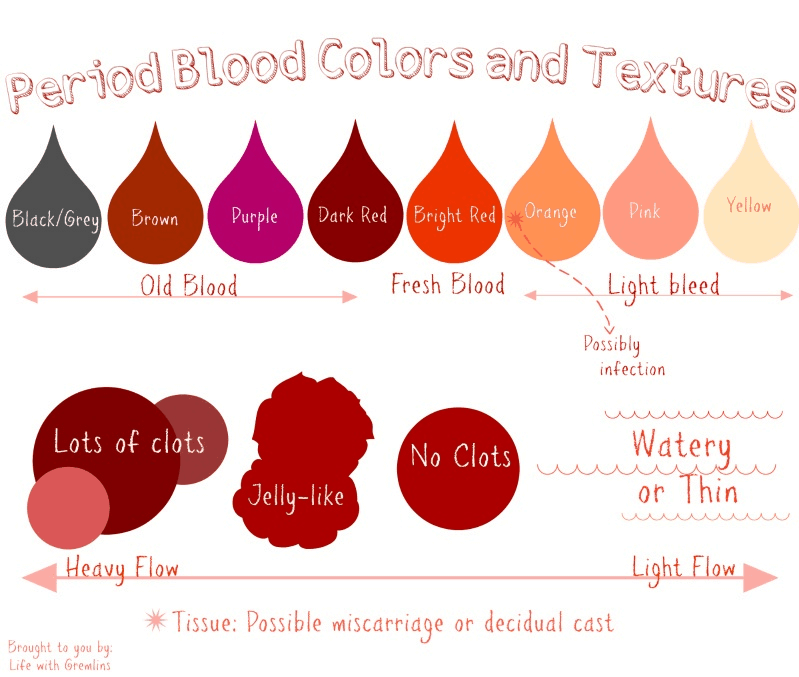 Not very well, but as she could tell. nine0003
Not very well, but as she could tell. nine0003
#34
#35
#36
was very frightened. Has anyone experienced this?
So far, there is no way to go to the doctor. I am in another city ..
#38
#39
#40
#41
Natalie
Girls, tell me please, I'm 3 weeks pregnant, but my periods started to clot she said that most likely a miscarriage and an ultrasound should be done and advised to do a test. The test is positive, but she hasn’t done an ultrasound yet. What could it be?
The test is positive, but she hasn’t done an ultrasound yet. What could it be?
#42
New topics
-
Monthly go 17 days
3 answers
-
For the treatment of dysplasia, the doctor prescribed this drug
No answers
-
?
15 answers
-
Normal questions for a gynecologist? Understandable? Not many questions?
5 answers
#43
#44
I also have
#45
#46
#47
9000 #48
2222 Nu here and think what it was.