Pelvic back bone pain
This Overlooked Pelvis Problem Might Be Causing Your Lower Back Pain
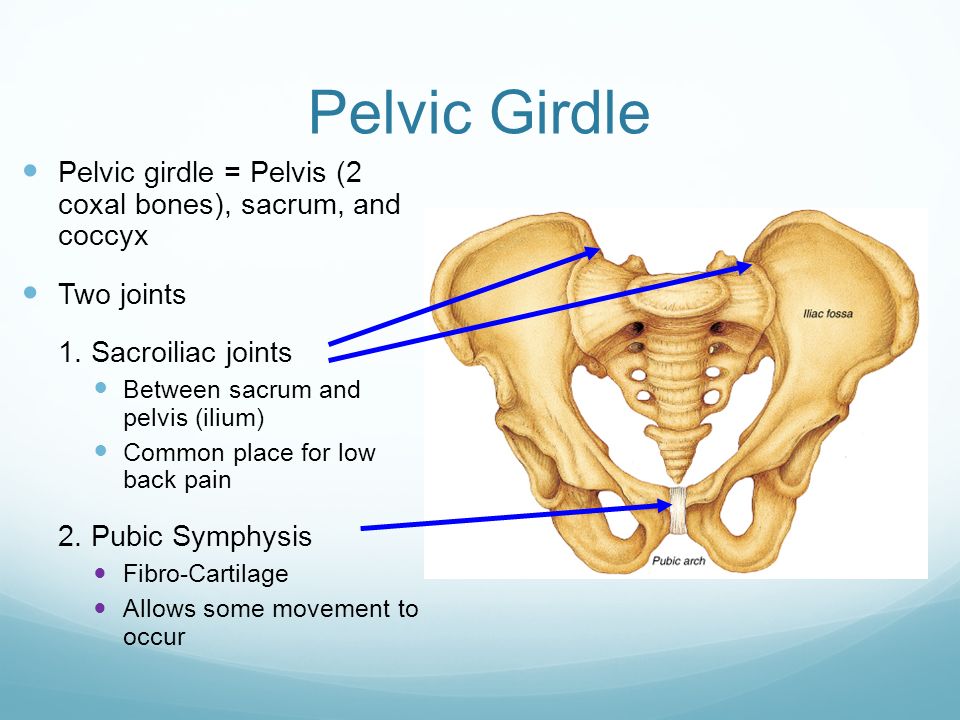
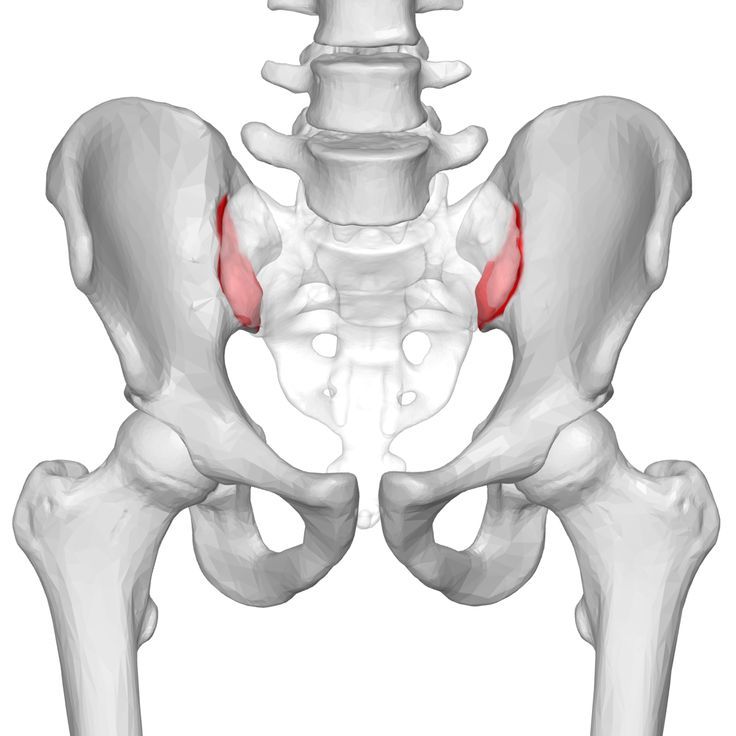
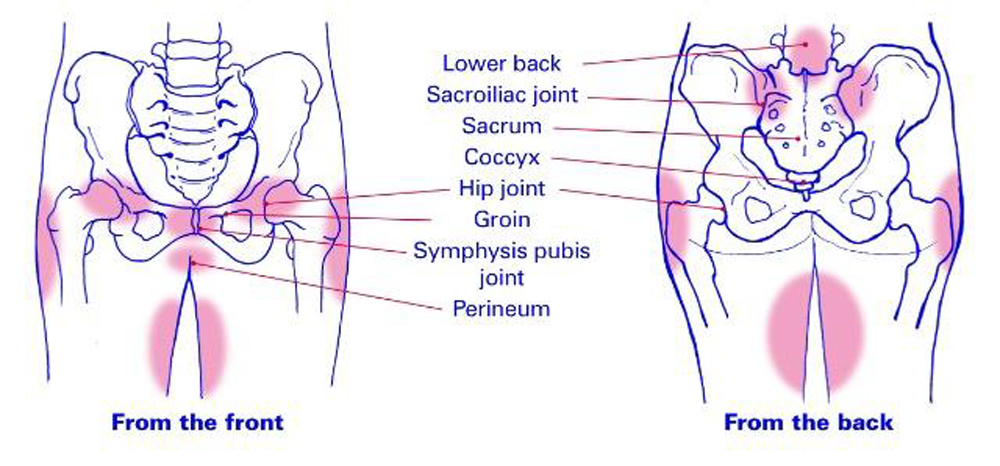
Deep in the back of your pelvis, you have a joint called the sacroiliac (SI) joint, which connects the bottom of your spine to your pelvis on each side. Problems with these joints are associated with up to 30% of lower back pain cases. 1 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359
The sacroiliac joint(s) can become a source of pain back and leg pain when there is either too much or too little movement in the joints. Inflammation of the sacroiliac joint (sacroiliitis) can also produce pelvic pain and stiffness. Watch Sacroiliac Joint Dysfunction Video
This blog highlights what you need to know about your SI joints and how they can contribute to lower back pain.
advertisement
What is a sacroiliac joint?
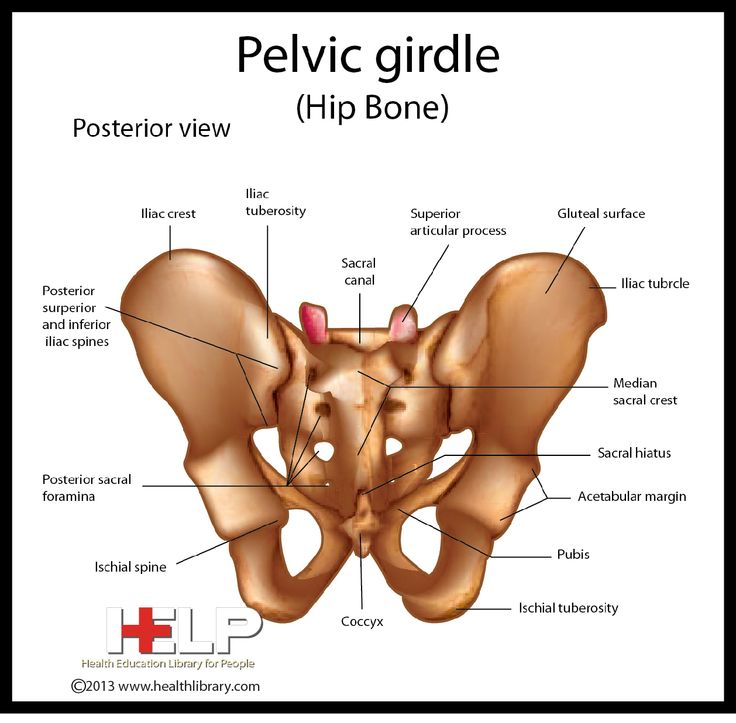
The SI joint is where the base of your spine (sacrum) connects to the butterfly-shaped group of bones in your pelvis. 1 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359
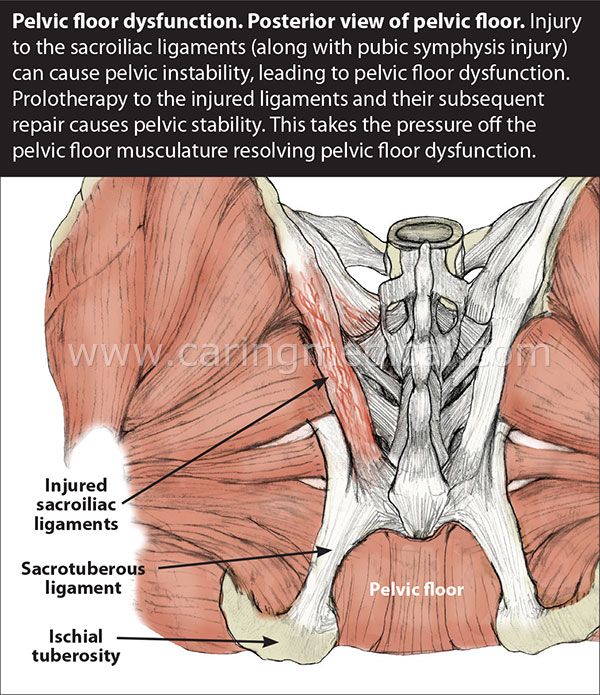
- The joint surfaces are covered with cartilage, held together by a fibrous capsule, and surrounded by synovial fluid (lubricating joint fluid). 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148
- Several ligaments surround the joint, providing strength and limiting its mobility. 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148
You have one of these joints on each side. 1 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV.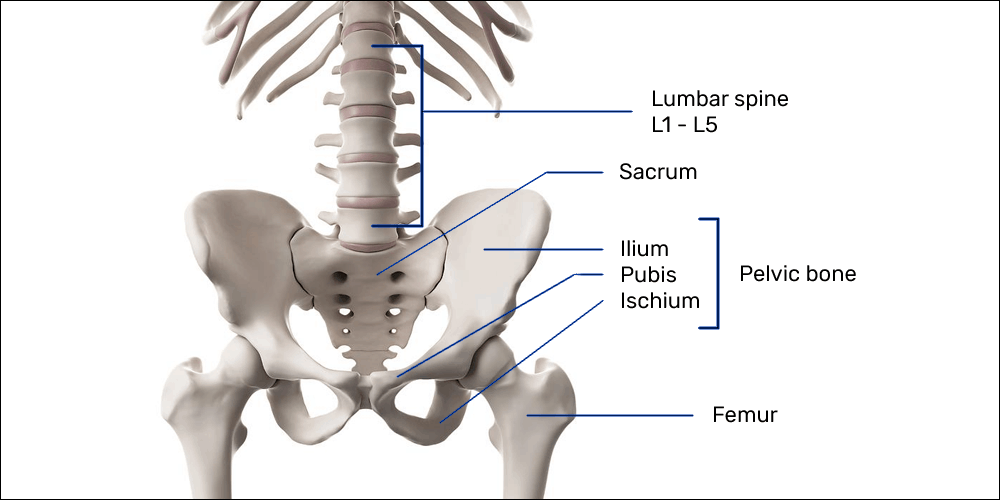 Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359
Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359
What does the sacroiliac joint do?
The SI joints support the weight of your upper body. They act as shock absorbers during the transfer of loads from the trunk of your body into your pelvis and legs. They also support your range of motion when you bend or twist at your hips. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
These joints are sturdy, have minimal mobility, and can withstand tremendous pressure. 1 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359 , 3 Raj MA, Varacallo M.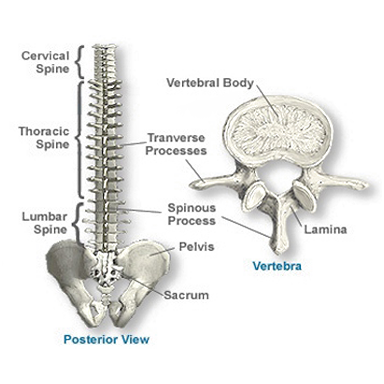 Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
How does the sacroiliac joint become painful?
SI joint pain occurs when there is malalignment or abnormal motion, such as too much or too little motion within the joint(s). 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
These painful conditions may develop gradually over time or from an inciting event:
- External trauma. High energy impacts, such as from a motor vehicle accident or a fall, may fracture or cause malalignment of the SI joint. Traumatic injuries may also overstretch (strain) the joint’s ligaments, causing pain. 2 Cohen SP, Chen Y, Neufeld NJ.
 Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148 , 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148 , 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ - Repetitive stress. Stressing the joint over time, such as daily jogging or weight lifting, may cause the SI joint and/or its surrounding ligaments to become painful. 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148 , 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.
 Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ , 4 Thawrani DP, Agabegi SS, Asghar F. Diagnosing Sacroiliac Joint Pain. Journal of the American Academy of Orthopaedic Surgeons. 2019;27(3):85-93. doi:10.5435/jaaos-d-17-00132
Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ , 4 Thawrani DP, Agabegi SS, Asghar F. Diagnosing Sacroiliac Joint Pain. Journal of the American Academy of Orthopaedic Surgeons. 2019;27(3):85-93. doi:10.5435/jaaos-d-17-00132 - Arthritis. Degenerative arthritis (osteoarthritis) or inflammatory arthritis (reactive or psoriatic arthritis) of the SI joint may cause lower back pain. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
- Pregnancy. The SI joint’s ligaments become relaxed and loose during pregnancy, making the joint more mobile than usual. Increased body weight and added pressure in the abdomen and lower back increase loads on the SI joints and may cause lower back pain in up to 90% of pregnant women.
 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148 , 5 Filipec M, Jadanec M, Kostovic-Srzentic M, van der Vaart H, Matijevic R. Incidence, pain, and mobility assessment of pregnant women with sacroiliac dysfunction. International Journal of Gynecology & Obstetrics. 2018;142(3):283-287. doi:10.1002/ijgo.12560
2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148 , 5 Filipec M, Jadanec M, Kostovic-Srzentic M, van der Vaart H, Matijevic R. Incidence, pain, and mobility assessment of pregnant women with sacroiliac dysfunction. International Journal of Gynecology & Obstetrics. 2018;142(3):283-287. doi:10.1002/ijgo.12560
Less common causes of SI joint pain include:
- Infections 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
- Scoliosis (abnormal sideways curvature of the spine) 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain.
 [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
[Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ - Discrepancy in leg length 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
- Ankylosing spondylitis (chronic, multisystem inflammatory disorder primarily involving the sacroiliac joints and the skeleton)
Carrying excessive weight and/or leading a sedentary lifestyle are contributing factors to SI joint pain. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
What does sacroiliac joint pain feel like?
Problems with your SI joint can be experienced with a wide range of symptoms, for example:
- A sharp, stabbing, and/or shooting pain may be felt directly over your affected joint – on the right or left side of the back of your hip.
 Alternatively, you may feel more of a persistent, dull ache in that area. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
Alternatively, you may feel more of a persistent, dull ache in that area. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ - The pain is usually localized to the lower back and/or over the buttock. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ , 6 Polly DW, Cher D. Ignoring the sacroiliac joint in chronic low back pain is costly [published correction appears in Clinicoecon Outcomes Res. 2016;8:349]. Clinicoecon Outcomes Res. 2016;8:23–31. Published 2016 Jan 21. doi:10.2147/CEOR.S97345 The pain may also extend down the back of your thigh, but typically does not extend below the knee.
.jpg) 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ - Certain positions or activities may cause your pain to flare up, such as going from standing to sitting, climbing stairs, or lying on the affected side. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
In addition to lower back pain, problems in the SI joint may mimic radicular (spinal nerve-root related) pain, 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.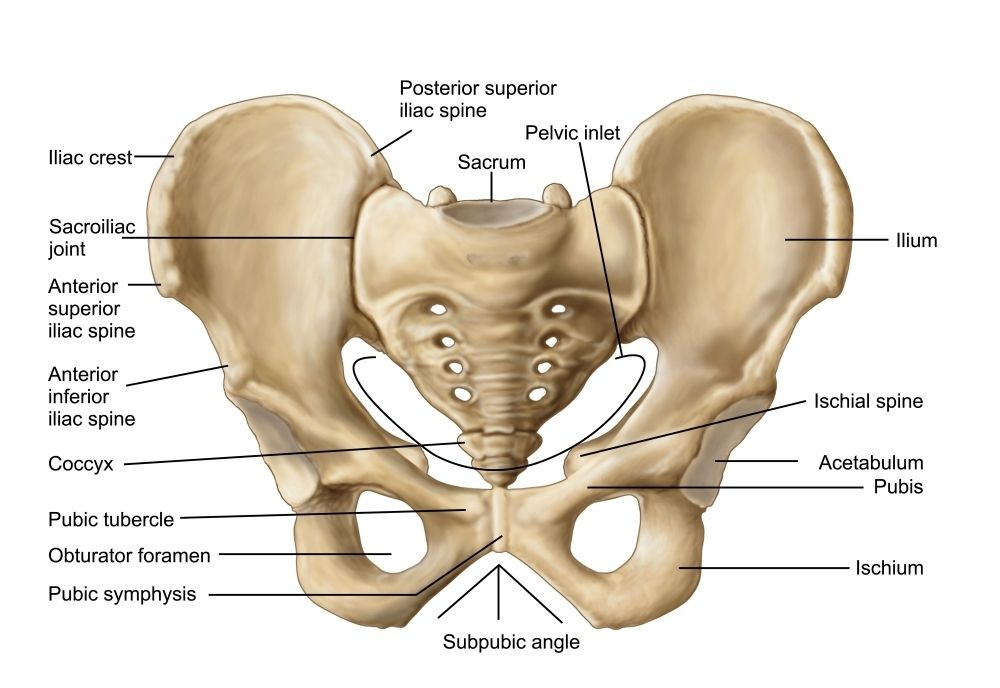 ncbi.nlm.nih.gov/books/NBK470299/ commonly referred to as sciatica.
ncbi.nlm.nih.gov/books/NBK470299/ commonly referred to as sciatica.
See Sacroiliac Joint Dysfunction Symptoms and Causes
How is sacroiliac joint pain treated?
Infographic:See Stretches ForSciatica Pain Relief Infographic
See Stretches ForSciatica Pain Relief Infographic
The treatment of SI joint pain usually involves a multidisciplinary approach and may include a primary care provider, a physical therapist, and an orthopedic surgeon, among others. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
SI joint pain treatments typically include 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12].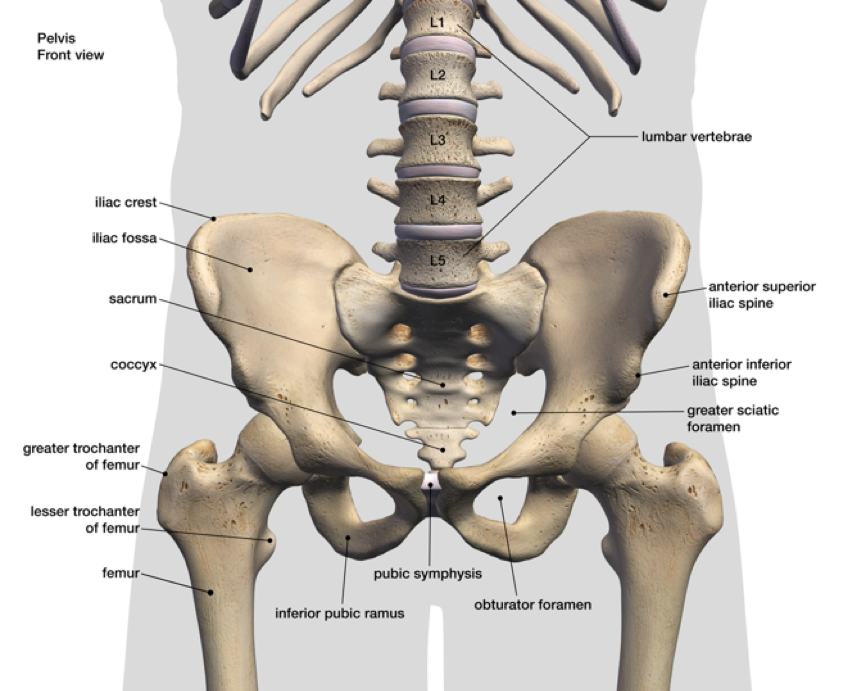 In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ :
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/ :
- Medication. Treatment is usually started with pain-relieving medications, such as NSAIDs to reduce the pain.
See Medications for Back Pain and Neck Pain
- Ice therapy. The intermittent use of an ice pack placed over your rear pelvis may provide relief from acute SI joint pain.
- Physical therapy. A guided physical therapy program is important to strengthen the pelvic muscles and regain function in the lower back.
See Physical Therapy for Low Back Pain Relief
- Manual manipulation. Manipulative therapies, such as from chiropractic treatments may help increase the mobility of the SI joint, providing pain relief.
See Chiropractic Procedures for the Sacroiliac Joint
- Posture correction. The use of supported posture while sitting, standing, walking, and lifting is important to prevent recurrences.
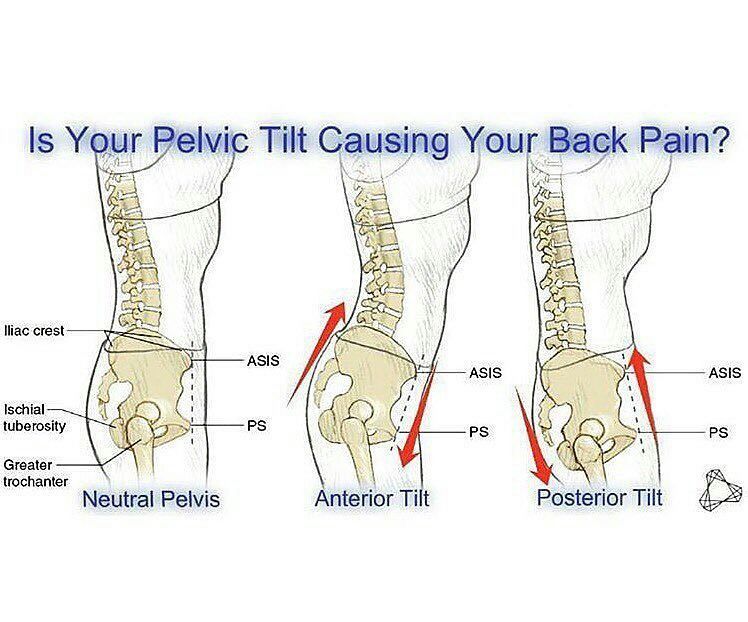
See Good Posture Helps Reduce Back Pain
advertisement
If the pain is severe, assistive devices, such as walkers may be used. Sacroiliac belts may be worn temporarily for short periods in case of pelvic instability. Minimally invasive treatments, such as radiofrequency ablation (creating heat lesions on nerves to stop them from transmitting pain) may be considered in severe SI joint dysfunction. Rarely, SI fusion surgery may be recommended. 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
If you suspect your SI joint(s) to be a cause of your lower back pain, consult your doctor for a medical examination. A doctor can conduct specific clinical tests, rule out serious underlying conditions, such as tumors or infections, and formulate an effective treatment plan for your SI joint pain.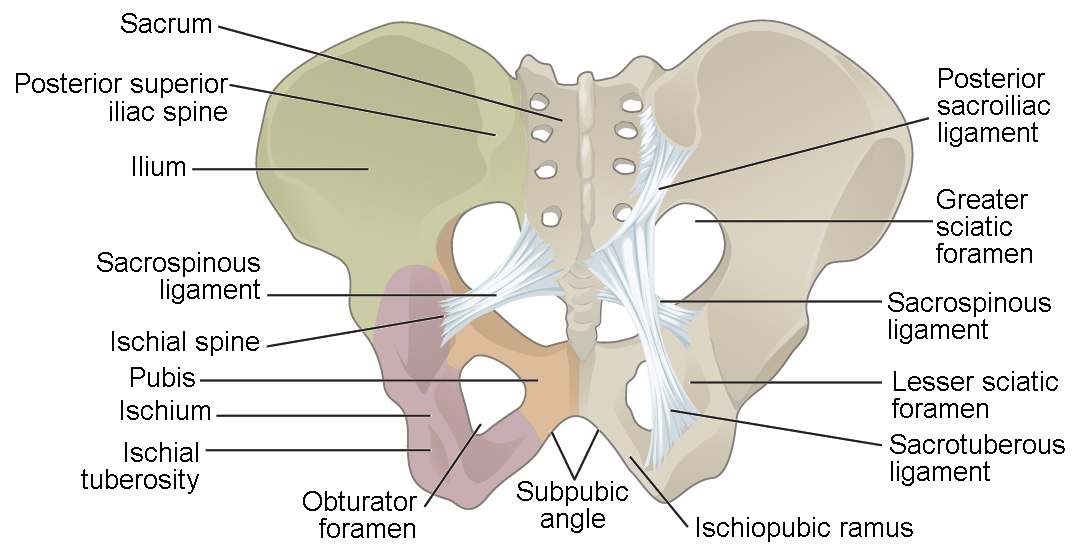
See Accurate Diagnosis of Sacroiliac Joint Dysfunction
Learn more:
Treatment Options for Sacroiliac Joint Dysfunction
Slideshow: Sacroiliac Joint Exercises for Sciatic Pain Relief
- 1 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clinical Spine Surgery. 2016;29(2):42-48. doi:10.1097/bsd.0000000000000359
- 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Review of Neurotherapeutics. 2013;13(1):99-116. doi:10.1586/ern.12.148
- 3 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. [Updated 2019 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
- 4 Thawrani DP, Agabegi SS, Asghar F.
 Diagnosing Sacroiliac Joint Pain. Journal of the American Academy of Orthopaedic Surgeons. 2019;27(3):85-93. doi:10.5435/jaaos-d-17-00132
Diagnosing Sacroiliac Joint Pain. Journal of the American Academy of Orthopaedic Surgeons. 2019;27(3):85-93. doi:10.5435/jaaos-d-17-00132 - 5 Filipec M, Jadanec M, Kostovic-Srzentic M, van der Vaart H, Matijevic R. Incidence, pain, and mobility assessment of pregnant women with sacroiliac dysfunction. International Journal of Gynecology & Obstetrics. 2018;142(3):283-287. doi:10.1002/ijgo.12560
- 6 Polly DW, Cher D. Ignoring the sacroiliac joint in chronic low back pain is costly [published correction appears in Clinicoecon Outcomes Res. 2016;8:349]. Clinicoecon Outcomes Res. 2016;8:23–31. Published 2016 Jan 21. doi:10.2147/CEOR.S97345
advertisement
Editor’s Top Picks
-
Surgical Treatment for Sacroiliac Joint Pain
-
Sacroiliac (SI) Joint Exercises for Sciatic Pain
-
Sacroiliac Joint Steroid Injection Video
-
Chiropractic Adjustment of the Sacroiliac Joint Video
-
Sacroiliac Joint Dysfunction Video
-
Sacroiliac Joint Block Video
Low back, Pelvic & Sacroiliac joint
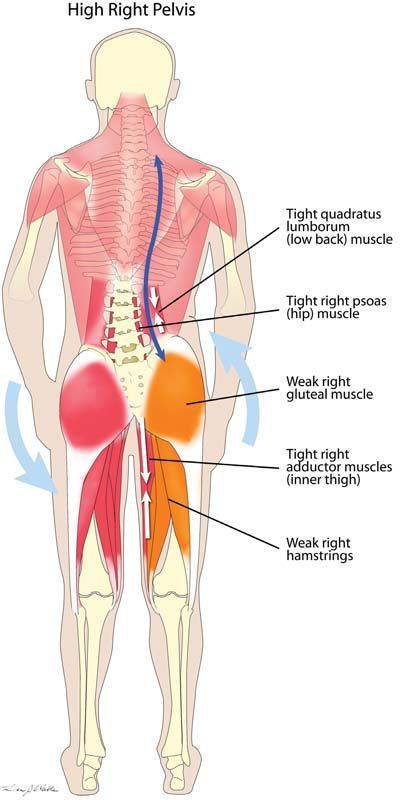
Luckily, the majority of people will get better quickly with the right treatment and muscle retraining.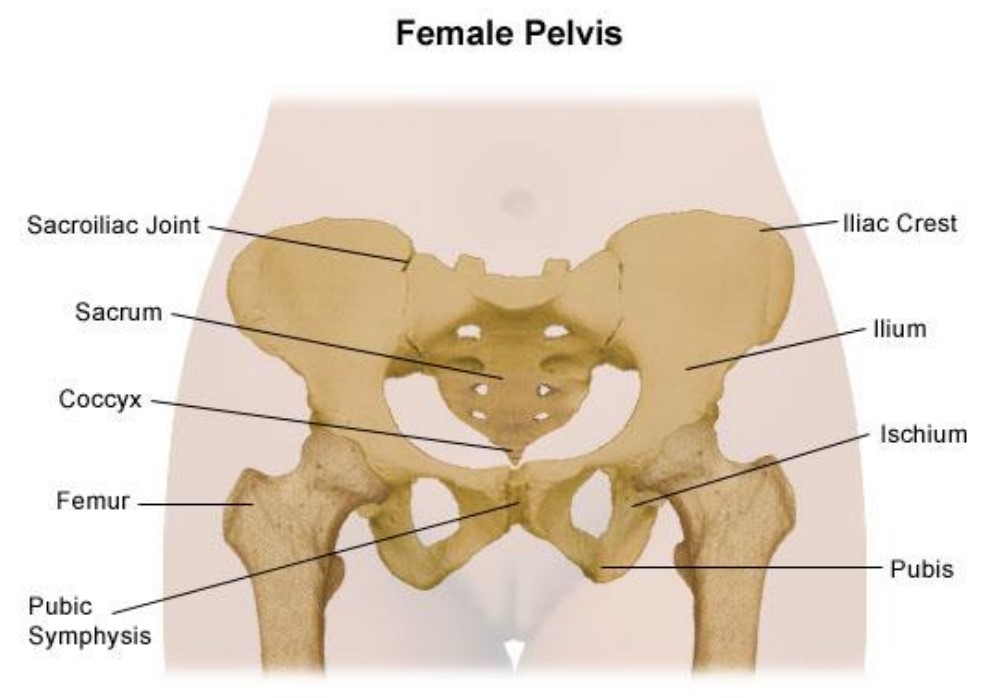 It is therefore important to find practitioners who have a depth of knowledge in assessing the lumbar spine and pelvis as well as surrounding muscles and nerves, and who know how to treat the many different types of back pain. A thorough initial examination allows us to determine what the main sources of your pain and disability are, and this allows us to direct treatment appropriately. 85% of people will suffer low back pain at some stage in their lives.
It is therefore important to find practitioners who have a depth of knowledge in assessing the lumbar spine and pelvis as well as surrounding muscles and nerves, and who know how to treat the many different types of back pain. A thorough initial examination allows us to determine what the main sources of your pain and disability are, and this allows us to direct treatment appropriately. 85% of people will suffer low back pain at some stage in their lives.
The team at Sydney Spine and Pelvis are at the forefront of providing professional education, treatment and rehabilitation for pelvic injuries and back pain.
Low back pain has many sources:
- There is the person who has just hurt their back acutely from an incorrect lift or a sporting injury. Often the pain is muscular or due to a facet joint strain
- There is the person who has had a disc or nerve root injury and is struggling to sit or get their pants on, and can’t get their muscles to hold them up
- Sciatic nerve and pudendal nerve irritation can cause buttock and leg pain that limits walking and activity
- There is the person who has had grumbling back pain for many years.
 Over time they realize their back pain is making them do less at home, work, and play. They notice they have less strength but any time they try to exercise their back pain gets worse.
Over time they realize their back pain is making them do less at home, work, and play. They notice they have less strength but any time they try to exercise their back pain gets worse. - There is the person who gets back ache from sitting and standing too long, and has pain every night when they go to bed or get out of bed in the morning
- There is the person who feels there back is weak, and knows their posture is poor but does not know how to improve it.
Treatment needs to be specific depending on your symptoms. Disc injuries with or without nerve root irritation can occur at any level in the spine. In its mildest form, a small broad based disc bulge is a normal part of aging and many of us will have this degenerative change without it causing pain. However, an acute focal disc bulge may cause inflammation that puts pressure onto the nerve root and this is often associated with referred pain, altered sensation, and difficulty weight bearing
Acute phase: Initially it is important to try to ease inflammation and pain, and to fully assess how the nerve is being affected.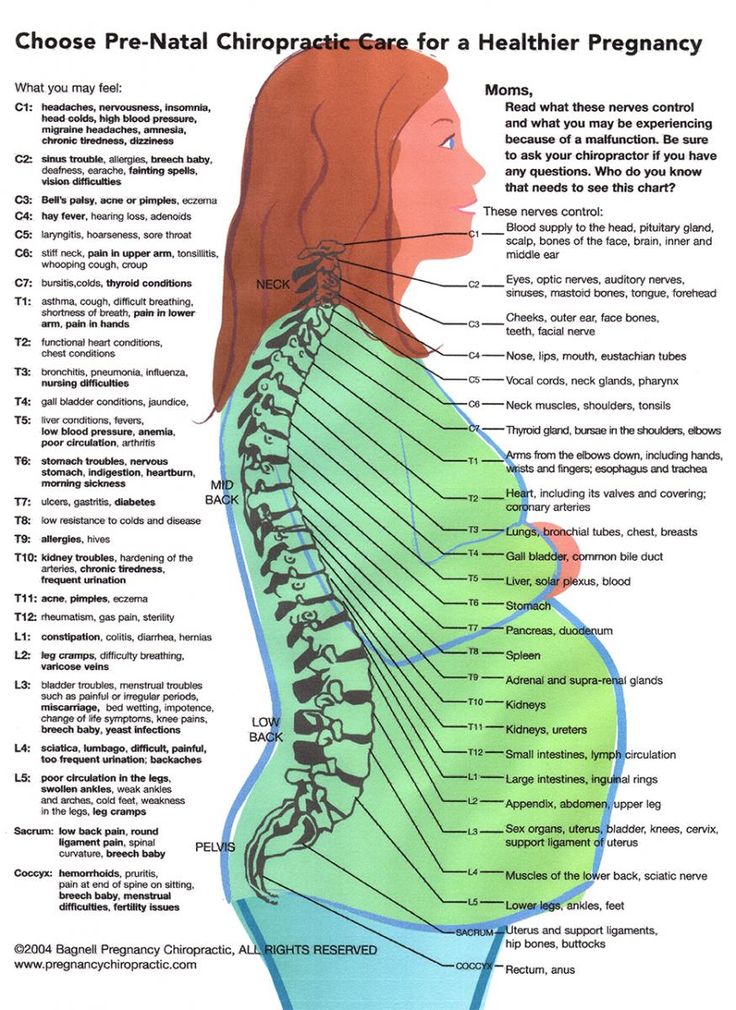
Ongoing back or leg pain related to an old disc injury: There can be many reasons for ongoing symptoms that may linger long after the disc has healed or micro-discectomy surgery has repaired the protruded disc material. At this stage physiotherapy treatment should combine manual therapy to release over active muscles and improve nerve mobility, core and lumbo-pelvic muscle retraining to restore strength and endurance, and posture retraining to decrease any ongoing irritation of the nerve tissue and minimize the chance of re-injury
Physiotherapy post Lumbar micro-diecectomy +/- Lmainectomy
As stated above, treatment post surgery needs to be specific to ensure good healing and improvoemnt of neural tissue irritation. Here is our Sydney Spine & Pelvis Post- operation protocol that will help patients understand what they should and shouldn't do in the weeks post surgery Lumbar_Micro_discectomy_post_op_protocol_FINAL.pdf
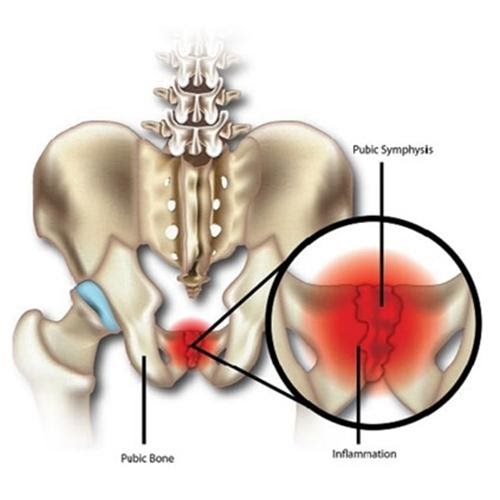
2. Pelvic dysfunction and Sacroiliac joint injuries
Pelvic dysfunction and Sacroiliac joint injuries
Pelvic pain is often less understood than low back pain, and yet research shows that up to 30% of low back pain is related to dysfunction and pain coming from the sacroiliac joints, the pubic symphysis or tissues that attach onto the pelvis. Pelvic dysfunction often occurs after a fall onto the bottom or knee, a lifting injury, or may be related to pregnancy and labour. The symptoms of pelvic pain are varied, from pain with sitting and rising from sitting, pain in the pelvic and buttock region with walking or standing on one leg, groin pain or even altered control of bladder function. Both the sacroiliac joints and the pubic symphysis can be involved, and can decrease the effectiveness of core muscle activation so that your ability to cope with normal daily activities is dramatically reduced. The team at Sydney Spine and Pelvis are experts at assessing and treating pelvic dysfunction with a combination of manual therapy, muscle and nerve release techniques, and specific exercise rehabilitation to facilitate lumbo-pelvic muscle control.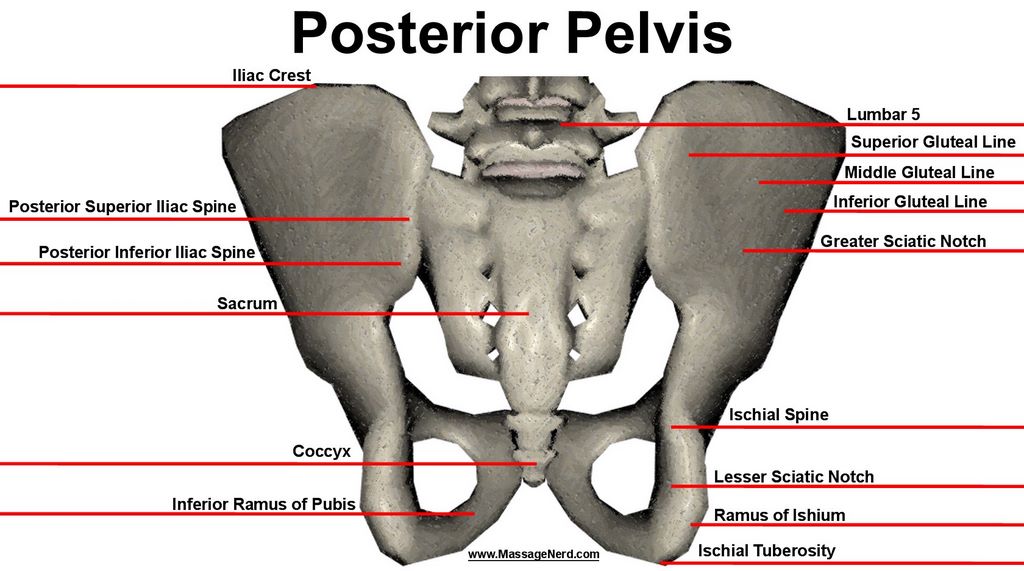
Low back pain can have many sources, but not all of these are easily picked up on x-rays or scans. As we have stated before, 85% of the western world will have back pain at some stage in their life. Often this relates to a muscle sprain or tight back muscles that are limiting the way the joints in the spine move. Poor posture and poor activation of your core muscles can leave your back feeling weak or unsupported.
The facet joints are 2 small joints at every level of the spine that allow a small sliding movement to occur every time you move your back. Repeated loading into extension can create a stress reaction, or stress fracture at the facet joints, and this is often an issue in sports such as cricket (bowling), gymnastics and tennis.
Degenerative changes (or arthritis) at the facet joints is a normal part of ageing and commonly occurs in the neck and low back. These degenerative changes can be shown on scans and are often asymptomatic (not painful).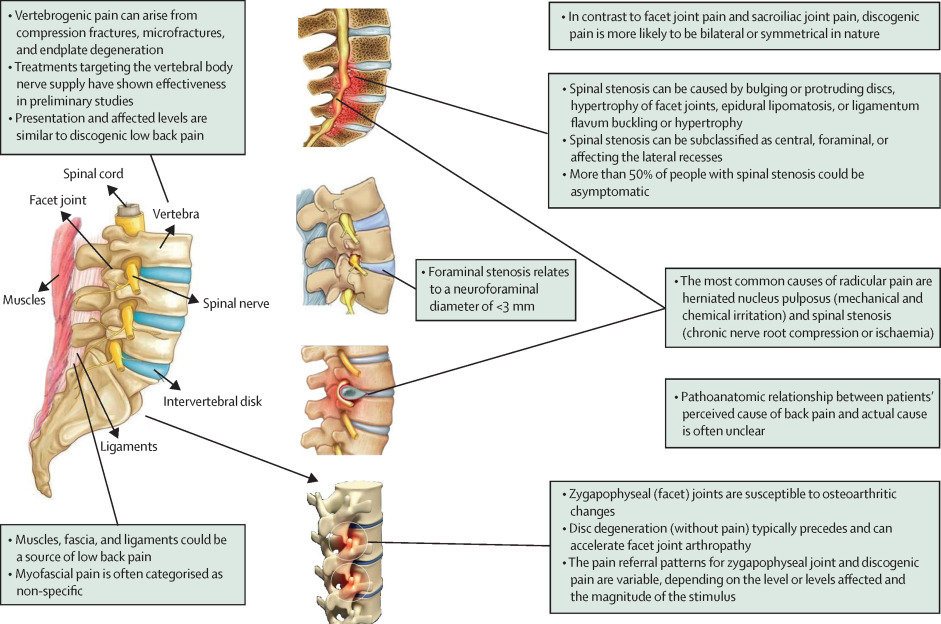 However, they can also become acutely inflamed and cause pain with movement. Treatment needs to be specific to ease the pressure on the irritated joint, decrease the inflammation and to re-activate the right muscles to support the joint during activity.
However, they can also become acutely inflamed and cause pain with movement. Treatment needs to be specific to ease the pressure on the irritated joint, decrease the inflammation and to re-activate the right muscles to support the joint during activity.
- 3RD(1998), 4TH (2001), 5th (2004) and 6th (2007) World Congress for Low Back & Pelvic Pain Dr Barb Hungerford has been researching the effects of pelvic injuries for the past decade and has presented her results at conferences such as
- Australian Physiotherapy Association Conference 2006, 2011
- Australian Pilates Method Association Conference 2006
- World Congress for Physical Therapy 2004
The Physiotherapists at Sydney Spine and Pelvis Centre are experts in assessment, treatment and rehabilitation for low back pain, pubic pain, pelvic or sacroiliac symptoms, sciatica and referred leg pain.
 We take an hour for our initial assessment in order to fully assess your problem and determine the best way we can help, whether that is specific manual therapy techniques, muscle retraining or exercise therapy. If you require further information about the treatment we provide or specific exercise rehabilitation please call us on 9719.9114, Monday to Friday from 8am to 6pm.
We take an hour for our initial assessment in order to fully assess your problem and determine the best way we can help, whether that is specific manual therapy techniques, muscle retraining or exercise therapy. If you require further information about the treatment we provide or specific exercise rehabilitation please call us on 9719.9114, Monday to Friday from 8am to 6pm.Article "Chronic pelvic pain in women"
The problem of chronic pelvic pain in women of reproductive age occupies a special place in gynecology. Almost half of the patients who turn to the specialists of the EMC Department of Gynecology and Oncogynecology have complaints of chronic pelvic pain - discomfort for a long time in the lower abdomen, in the area below the navel. Long-term, despite the fact that conventional painkillers are ineffective, pelvic pain changes the psyche, the behavior of women, reduces the ability to work and quality of life.
Pain may be constant or intermittent, even paroxysmal, may be cyclical or not at all related to the menstrual cycle.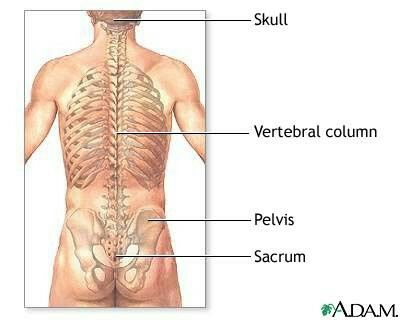 Pain impulses arising in the genitals and surrounding tissues as a result of irritation of nerve endings are transmitted to the central nervous system, which in most women is accompanied by general weakness, irritability, anxiety, excitability, emotional lability, attention disorders, memory loss, sleep disturbances.
Pain impulses arising in the genitals and surrounding tissues as a result of irritation of nerve endings are transmitted to the central nervous system, which in most women is accompanied by general weakness, irritability, anxiety, excitability, emotional lability, attention disorders, memory loss, sleep disturbances.
Chronic pelvic pain is characterized by:
-
persistent pain in the lower abdomen and lower back of varying intensity and character (pulling, dull, burning, etc.), prone to irradiation, lasting more than 6 months;
-
periodic exacerbations - pain crises arising in connection with cooling, overwork, stress, etc.;
-
psycho-emotional disorders, manifested by insomnia, irritability, disability, anxiety and depression, decreased sexual function up to a complete lack of interest and sexual response;
-
no or little effect of conventional pain and antispasmodic therapy.
In some cases, it is not possible to identify its causes even with in-depth examination - this is the so-called "inexplicable" pain.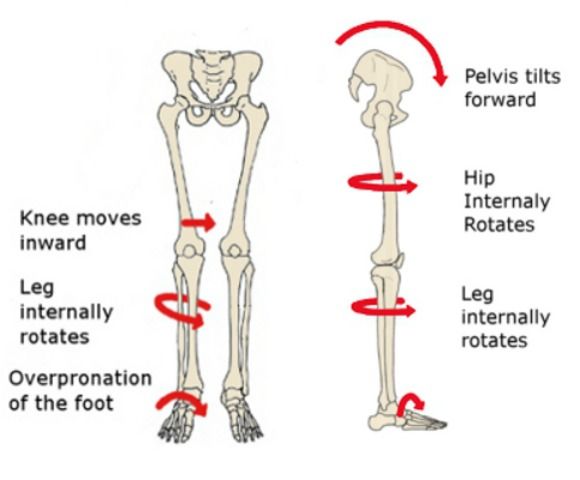 For such patients, the “triangle” route - gynecologist-urologist-neurologist - becomes familiar, and pain and fear force them to turn to an oncologist. Often, for years, these patients have been treated for "inflammation of the uterus and appendages" with large doses of antibacterial drugs, and such irrational treatment aggravates the situation even more.
For such patients, the “triangle” route - gynecologist-urologist-neurologist - becomes familiar, and pain and fear force them to turn to an oncologist. Often, for years, these patients have been treated for "inflammation of the uterus and appendages" with large doses of antibacterial drugs, and such irrational treatment aggravates the situation even more.
Pain is one of the most common symptoms in many gynecological diseases. External genital endometriosis, adhesions in the pelvic cavity, chronic inflammatory diseases of the internal genital organs, internal endometriosis of the uterine body, Allen-Masters syndrome, genital tuberculosis, uterine fibroids, benign and malignant ovarian tumors, malignant neoplasms of the body and cervix, developmental anomalies genital organs with a violation of the outflow of menstrual blood - this is not a complete list of diseases and conditions that may be accompanied by chronic pelvic pain.
The most common misconceptions about chronic pelvic pain
Chronic pelvic pain in women can only be caused by gynecological diseases
coccygeal articulation, primary tumors of the pelvic bones, metastases to the pelvic bones and spine, bone forms of tuberculosis, pathology of the symphysis), retroperitoneal neoplasms, diseases of the peripheral nervous system (plexitis), diseases of the gastrointestinal tract (chronic colitis, irritable bowel syndrome, nonspecific ulcerative colitis, proctitis, adhesive disease), diseases of the urinary system (chronic cystitis, urolithiasis, pelvic location of the kidney, prolapse of the kidney), vascular disease (varicose veins of the small pelvis). The causes of chronic pain syndrome can also be mental illness (abdominal epileptic seizures, depressive syndrome, schizophrenia).
Pain is usually caused by one factor, eliminating which, you can get rid of pain
In fact, in most gynecological diseases, the origin of pain is caused by several irritants at once, and it is often impossible to single out the leading factor. With uterine fibroids, pain can be caused by an increase in this organ, a violation of its blood supply and contractility of the uterine muscle, deformation of the uterine cavity by nodes, compression of the enlarged uterus or individual nodes of neighboring organs - the intestines, urinary tract, nerve plexuses, blood vessels.
In tumors and cysts of the ovaries, the tissues and ligaments of the ovaries are stretched (up to torsion), the maturation of follicles is disturbed, micro-ruptures with inflammation and the formation of adhesions are possible, compression of adjacent organs by cysts
a functioning uterus with aplasia of the cervix or vagina, a rudimentary uterine horn, a closed cavity of a bicornuate or doubled uterus) and other conditions accompanied by a violation of the outflow of menstrual blood (intrauterine synechia, stenosis of the cervical canal or cicatricial changes in the vagina). In these cases, the onset of pain is due to the expansion of closed cavities with blood and irritation of the peritoneum with almost constant hemoperitoneum, inflammation, and adhesions. Incorrect positions of the internal genital organs (bends of the uterus, prolapse, prolapse) also cause pelvic pain.
In these cases, the onset of pain is due to the expansion of closed cavities with blood and irritation of the peritoneum with almost constant hemoperitoneum, inflammation, and adhesions. Incorrect positions of the internal genital organs (bends of the uterus, prolapse, prolapse) also cause pelvic pain.
As a rule, most patients have a combined gynecological pathology, and each of the diseases can cause pain. External endometriosis often accompanies any other gynecological disease, and uterine fibroids are combined with internal endometriosis of the uterine body. Often there is a prolapse of the uterus, affected by fibroids or adenomyosis. The presence of a combined gynecological and extragenital pathology (hernias, diseases of the gastrointestinal tract, urinary tract, osteochondrosis of the spine) can significantly complicate the determination of the true cause of pain.
Periodic pain in women is normal
This myth has been around since the 19th century.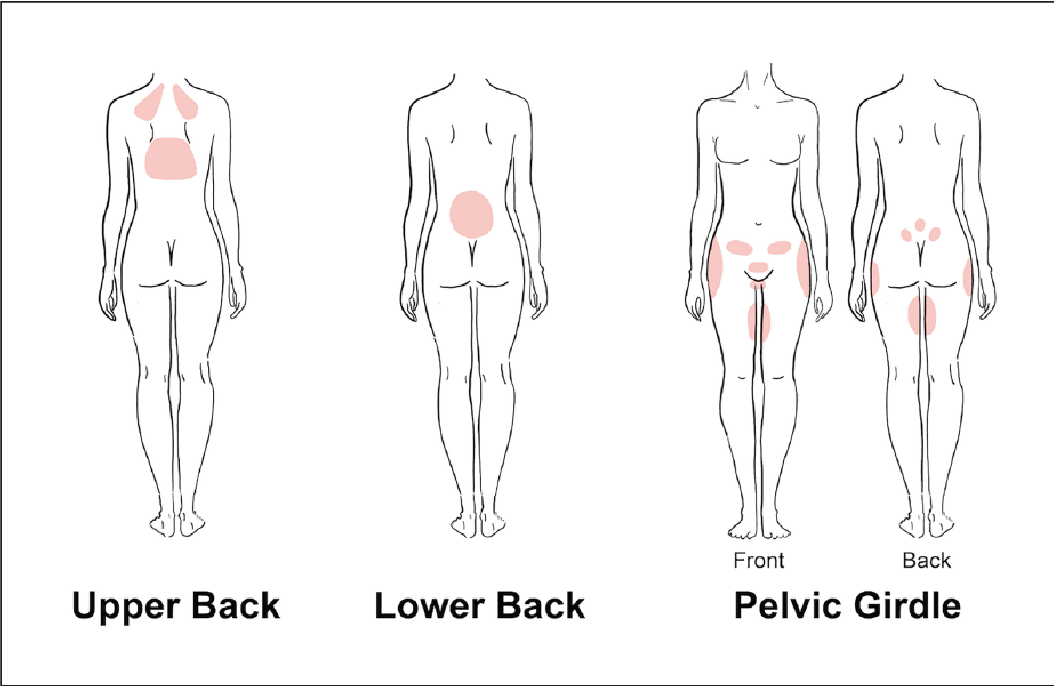 Doctors then explained menstrual pain by the instability and delicacy of the physiology of women and believed that pain during menstruation is the norm, which is very characteristic of the female body. Another "cause" of pain in women during menstruation is, according to some, a low pain threshold.
Doctors then explained menstrual pain by the instability and delicacy of the physiology of women and believed that pain during menstruation is the norm, which is very characteristic of the female body. Another "cause" of pain in women during menstruation is, according to some, a low pain threshold.
In fact, many women and girls experience pain during their periods. However, severe pain that disrupts the habitual lifestyle and level of activity cannot be the norm, and usually they are based on some kind of disease, for example, endometriosis, a hormone-dependent disease in which the lining of the uterus (endometrium) grows in other parts of the body. This is the third most common gynecological disease after uterine fibroids and various inflammatory processes in the genitals.
Therefore, every woman with severe pain during menstruation should be fully examined to identify their cause.
Early identification of the causes of pain determines the success of treatment.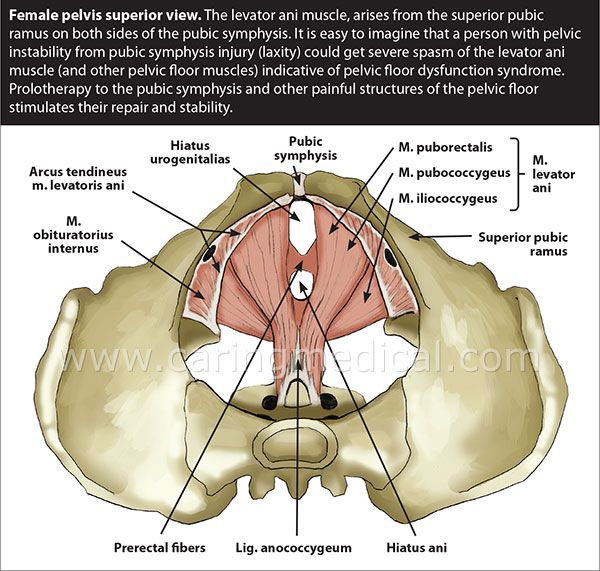 To establish the possible causes of pelvic pain, we work as a team with doctors of other specialties - general surgeons, oncologists, urologists, neurologists, psychologists.
To establish the possible causes of pelvic pain, we work as a team with doctors of other specialties - general surgeons, oncologists, urologists, neurologists, psychologists.
For the treatment of chronic pelvic pain, EMC gynecologists-surgeons use an approach based on reducing the invasiveness of surgical intervention, avoiding excessive radicalism, and expectant management in certain diseases of the genital area.
Laparoscopy and hysteroscopy provide us with unique diagnostic and therapeutic opportunities, which allow us to identify and eliminate possible causes of pain that are not diagnosed by other examination methods: endometriosis of the pelvic peritoneum, adhesions, anatomical disorders - hernia, peritoneal defects (Allen-Masters syndrome).
From the patient’s point of view, laparoscopic intervention, unlike laparotomy, is not perceived as a “big and difficult” operation, and the absence of intense and prolonged postoperative pain associated with the surgical wound of the anterior abdominal wall eliminates the aggravation of the initial pain due to layering on them operating rooms.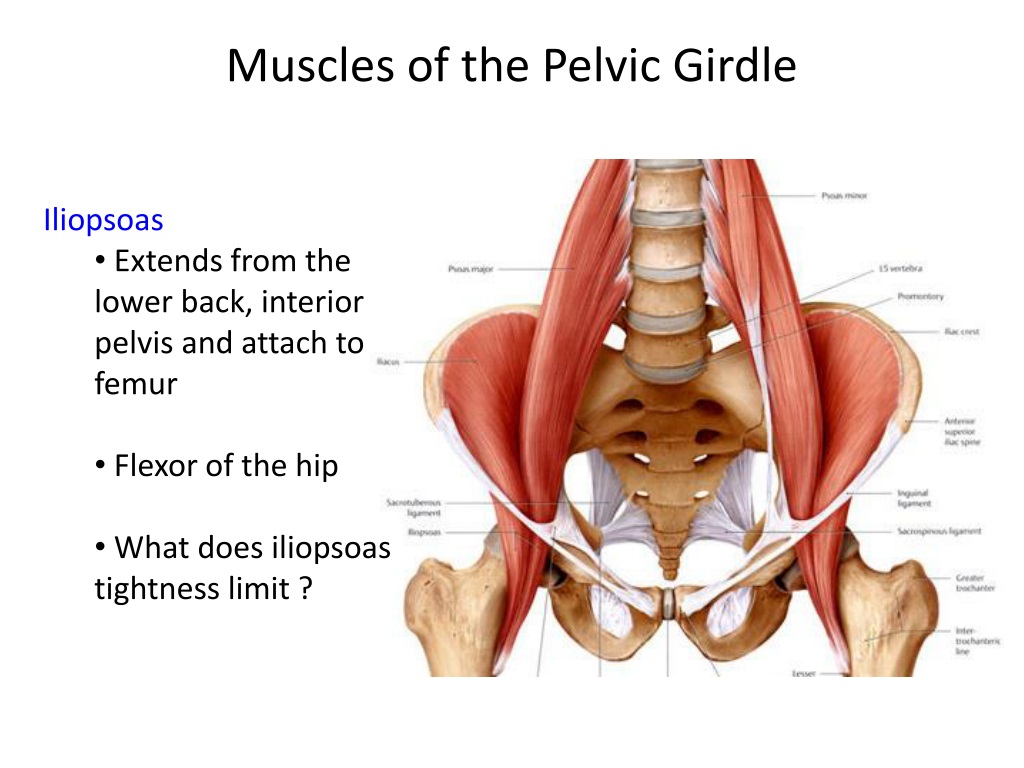 And, finally, early activation and return to physical activity, the almost absence of cosmetic defects also contribute to a quick recovery.
And, finally, early activation and return to physical activity, the almost absence of cosmetic defects also contribute to a quick recovery.
The volume of surgical intervention is chosen by EMC gynecologists depending on the age of the patient, her plans for childbearing, the severity of the detected pathology, the severity of pain. In young women, organ-preserving surgeries are performed, warning patients about the likelihood of recurrence of diseases such as endometriosis and uterine fibroids. Patients of older age groups with adenomyosis, multiple uterine fibroids, accompanied by severe pain, bleeding and leading to anemia, tumor growth and its significant size, dysfunction of neighboring organs, are shown radical operations in the volume of removal of the uterus, which we perform by laparoscopy or from a vaginal access .
In case of prolapse and prolapse of the pelvic organs accompanied by pelvic pain, EMC gynecologists use surgical correction technologies that are fundamentally different from each other, depending on the age of the patient, to effectively eliminate gynecological pathology and restore the disturbed pelvic anatomy.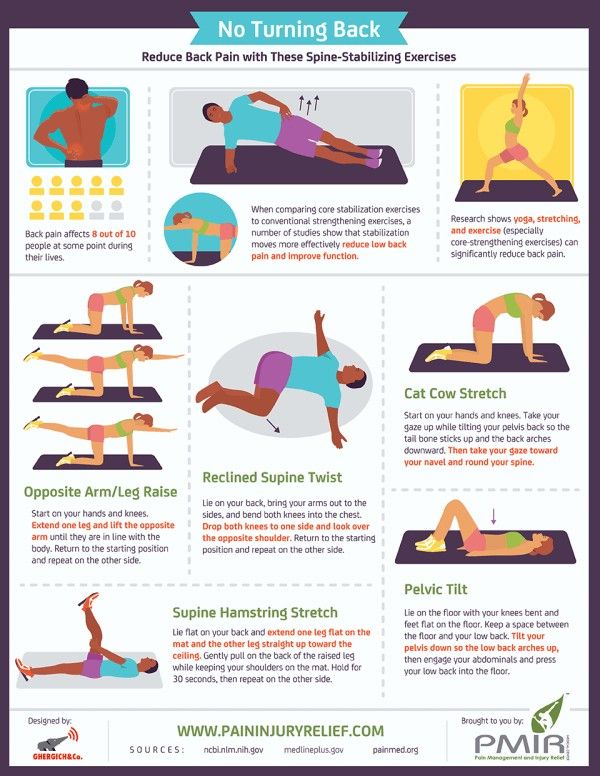 For pelvic varicose veins, we perform laparoscopic ovarian vein ligation, which is highly effective for pelvic pain due to congestion in the pelvic veins, without adversely affecting ovarian function.
For pelvic varicose veins, we perform laparoscopic ovarian vein ligation, which is highly effective for pelvic pain due to congestion in the pelvic veins, without adversely affecting ovarian function.
The efficiency of surgical interventions performed by specialists of the EMC Department of Gynecology and Oncogynecology varies from 60 to 95%, which indicates the effectiveness of the treatment and the high level of training of specialists, whose experience allows them to take on even the most complex cases.
EMC Clinic of Gynecology and Oncogynecology works in accordance with evidence-based medicine protocols practiced in the USA and Western Europe. The EMC clinic is one of the few in Moscow whose level of medical services meets international standards.
The doctors of the Clinic work under the guidance of Vladimir Nosov, an experienced surgeon-gynecologist and obstetrician-gynecologist, certified by the US National Commission (Board Certified) in obstetrics-gynecology and oncogynecology, and also certified in Russia in obstetrics-gynecology and oncology.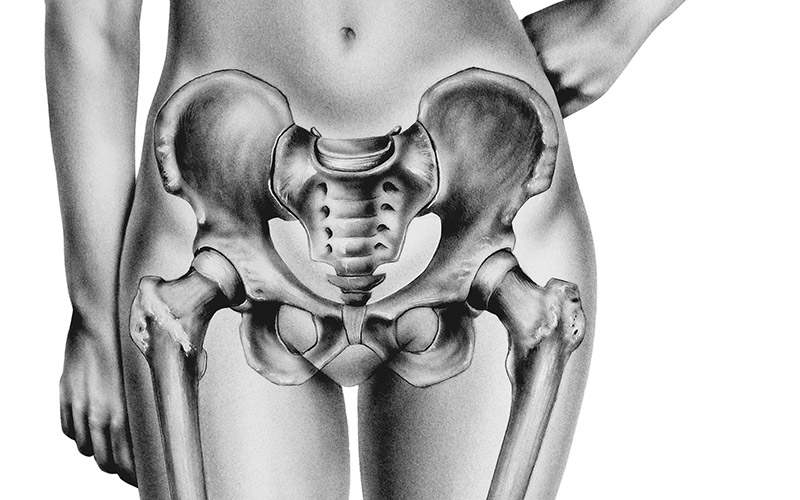
Pelvic pain - causes, examination and treatment | Symptoms
Menstrual cramps
Symptoms: Sharp or crampy pains that begin a few days before or during menstruation, are most intense within about 24 hours after the onset of menstruation and subside after 2 to 3 days, often accompanied by headache, nausea, constipation, diarrhea, or frequent urination. urination.
Endometriosis
Signs: Sharp or crampy pain that occurs before and during the first days of menstruation, often pain during intercourse and / or bowel movements. It can eventually lead to pain that is not related to the menstrual cycle.
Pain in the middle of the menstrual cycle
Signs: Severe, sharp pain that starts suddenly; can occur on either side, but only on one side each time, occurs at the same time during the menstrual cycle, usually in the middle of the cycle between periods (when the egg is released), most intense at the beginning, but then decreases over 1–2 days, there is often slight bleeding.
Pelvic inflammatory disease
Signs: Aching pain in the pelvic area, which can be felt on one or both sides. Usually a vaginal discharge that is sometimes foul-smelling and can become pus-like and yellow-green in color as the infection progresses. Sometimes pain during urination and/or intercourse, fever or chills, nausea or vomiting.
Rupture of an ovarian cyst
Signs: Pain that starts suddenly is initially limited to one area in the lower abdomen. Sometimes dizziness, fainting, slight vaginal bleeding, nausea, or vomiting occur.
Ectopic pregnancy
Signs: Persistent (not spasmodic) pain that starts suddenly, is initially limited to one area in the lower abdomen. Often slight vaginal bleeding, sometimes dizziness, fainting, fast heartbeat, or dangerously low blood pressure (shock) caused by severe internal bleeding.
Sudden degeneration fibromas in uterus
Symptoms: Sudden pain.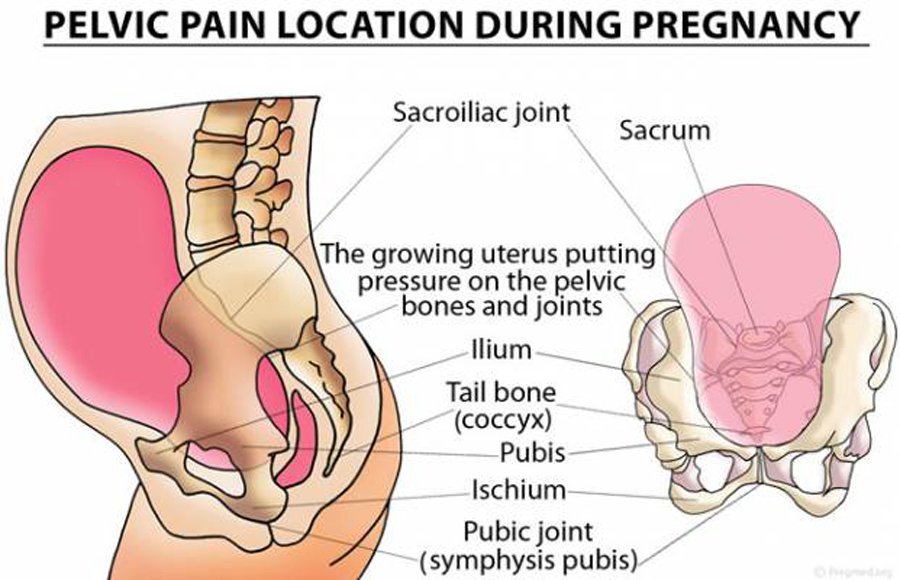 It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
Torsion (twisting) of the ovarian adnexa
Signs: Severe pain that starts suddenly, occurs on one side, grows rapidly. As well as intermittent pain that comes and goes (when the ovary twists and unwinds). Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries.
Ovarian cancer / Endometrial cancer
Signs: Gradually increasing pain. Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Spikes
Signs: Pain in the pelvic area, which gradually increases, often becomes chronic. As well as pain during intercourse. No vaginal bleeding or discharge. Sometimes nausea and vomiting (suggesting intestinal blockage).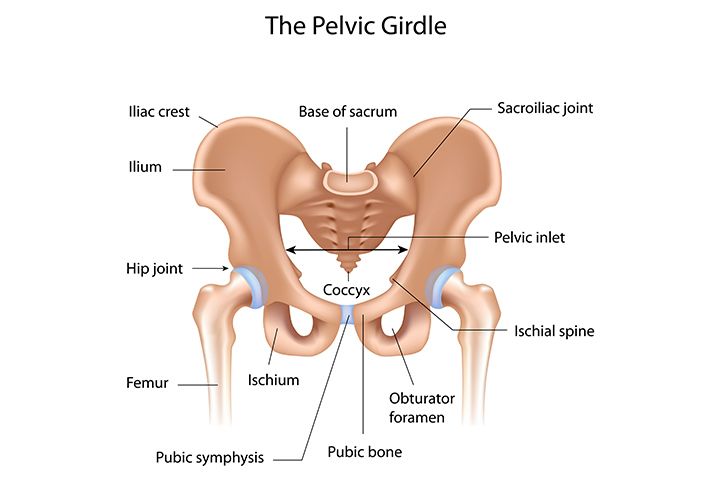 In women who have had abdominal surgery or in women with a pelvic infection.
In women who have had abdominal surgery or in women with a pelvic infection.
Miscarriage
Signs: Spasmodic pain in the pelvis or back, accompanied by vaginal bleeding. Other signs of early pregnancy such as breast tenderness, nausea, and missed periods.
Appendicitis
Signs: Pain that usually occurs in the lower right side of the abdomen. Loss of appetite and usually nausea and vomiting. Often fever.
Bladder infection
Signs: Pain just above the pubic bone. Sometimes an urgent need to urinate, more frequent urination, or burning when urinating.
Diverticulitis
Signs: Pain or tenderness in the left lower abdomen, fever.
Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)
Signs: Cramping pain in the abdomen, diarrhea, in ulcerative colitis often with blood in the stool, loss of appetite and weight loss.
Stones in the urinary tract
Signs: Excruciating intermittent pain in the lower abdomen, side or lower back, depending on the location of the stone, nausea and vomiting, blood in the urine.