Sleeping disorder in infants
Sleep in Infants (2-12 Months)
What to expect
Infants sleep between 9 and 12 hours during the night and nap between 2 and 5 hours during the day. At 2 months, infants take between two and four naps each day, and at 12 months, they take either one or two naps. Expect factors such as illness or a change in routine to disrupt your baby’s sleep. Developmental milestones, including pulling to a standing and crawling, may also temporarily disrupt sleep.
By 6 months of age, most babies are physiologically capable of sleeping through the night and no longer require nighttime feedings. However, 25%-50% continue to awaken during the night. When it comes to waking during the night, the most important point to understand is that all babies wake briefly between four and six times. Babies who are able to soothe themselves back to sleep (“self-soothers”) awaken briefly and go right back to sleep. In contrast, “signalers” are those babies who awaken their parents and need help getting back to sleep. Many of these signalers have developed inappropriate sleep onset associations and thus have difficulty self-soothing. This is often the result of parents developing the habit of helping their baby to fall asleep by rocking, holding, or bringing the child into their own bed. Over time, babies may learn to rely on this kind of help from their parents in order to fall asleep. Although this may not be a problem at bedtime, it may lead to difficulties with your baby falling back to sleep on her own during the night.
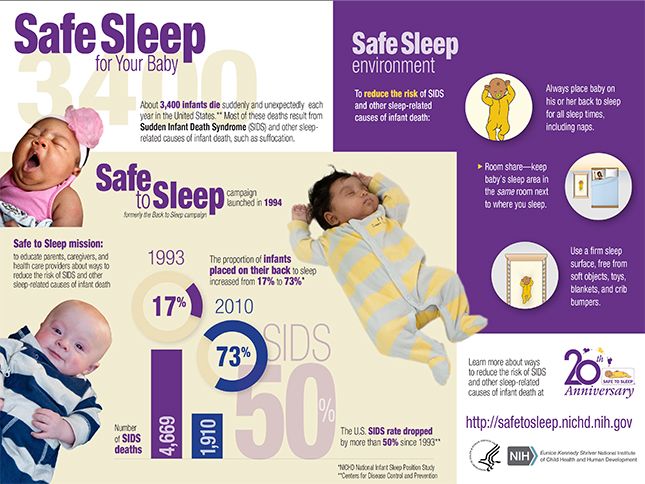
Safe Sleep Practices for Infants
-
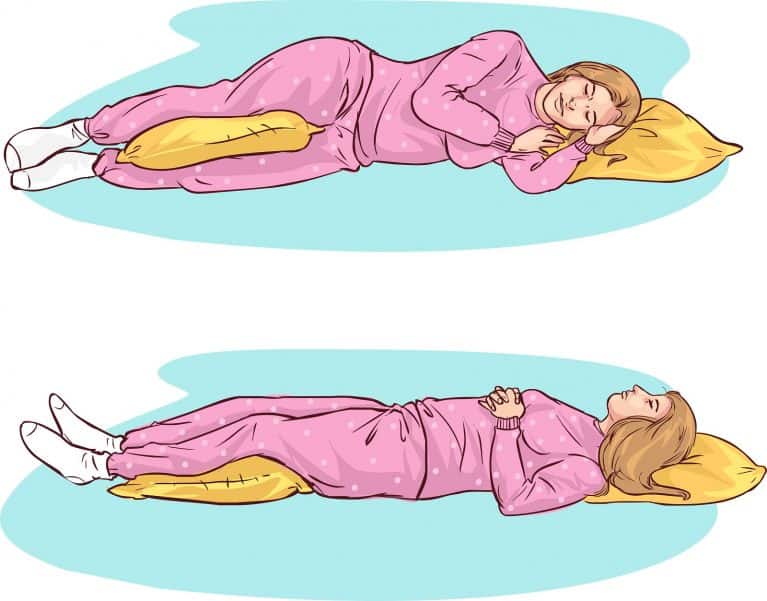
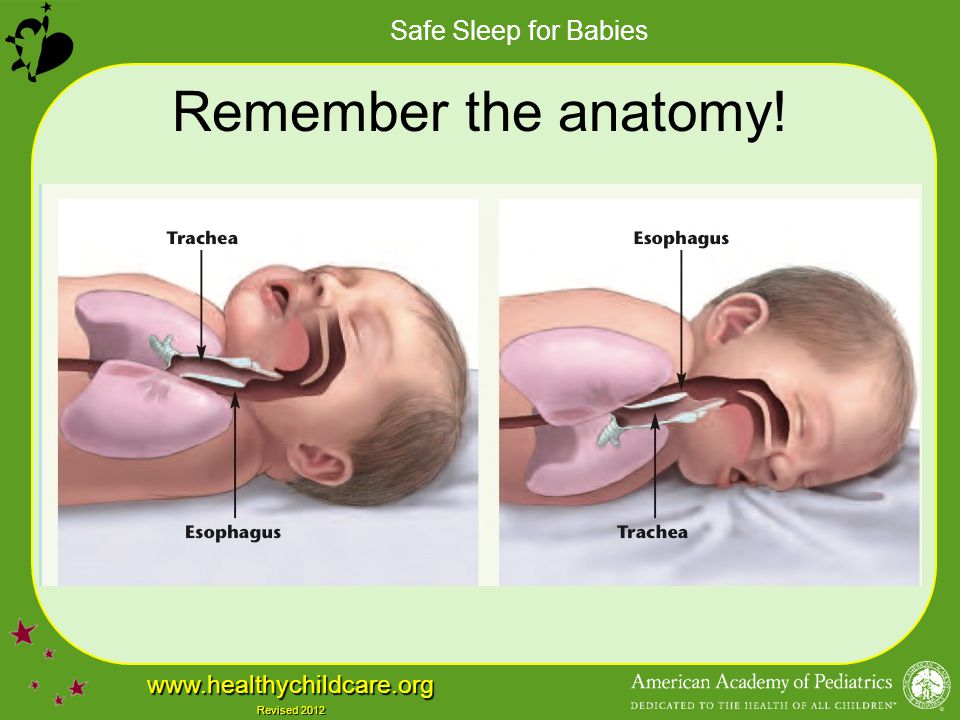
Practice the ABC’s of safe sleep: Babies should always sleep Alone, on their Backs, in a Crib. Place your baby on his or her back for every sleep, night time and nap time.
-
Do not put your baby to sleep on his side or tummy.
-
Once your baby can roll from his back to tummy and tummy to back, your baby can stay in the sleep position that he assumes.
 But always place your baby to sleep on his back.
But always place your baby to sleep on his back. -
Place your baby on a firm mattress in a safety-approved crib with slats no greater than 2-3/8 inches apart.
-
Make sure your baby’s face and head stay uncovered and clear of blankets and other coverings during sleep. If a blanket is used make sure your baby is placed “feet-to-foot” (feet at the bottom of the crib, blanket no higher than chest-level, blanket tucked in around mattress) in the crib. Remove all pillows from the crib.
-
Create a “smoke-free-zone” around your baby.
-
Avoid overheating during sleep and maintain your baby’s bedroom at a temperature comfortable for an average adult.
-
Remove all mobiles and hanging crib toys by about the age of 5 months, when your baby begins to pull up in the crib.
-
Remove crib bumpers by about 12 months, when your baby can begin to climb
For additional safe sleep practices for infants including information and video on choking, making a safe home environment, resources, swaddling and tummy time, click here.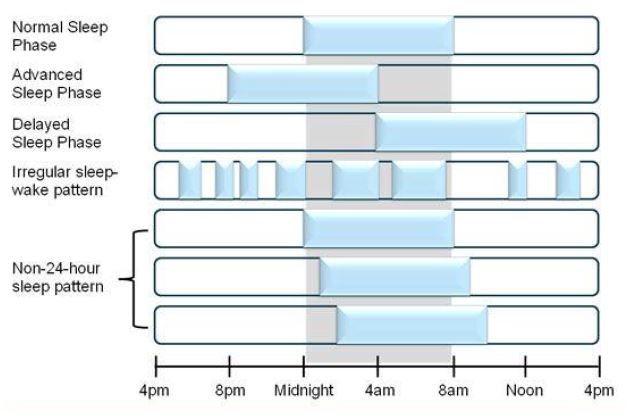
How to Help Your Infant Sleep Well
-
Learn your baby’s signs of being sleepy. Some babies fuss or cry when they are tired, whereas others rub their eyes, stare off into space, or pull on their ears. Your baby will fall asleep more easily and more quickly if you put her down the minute she lets you know that she is sleepy.
-
Decide on where your baby is going to sleep. Try to decide where your baby is going to sleep for the long run by 3 months of age as changes in sleeping arrangements will be harder on your baby as he gets older. For example, if your baby is sleeping in a bassinet, move him to a crib by 3 months. Always practice the ABC’s of safe sleep: Babies should always sleep Alone, on their Backs, in a Crib.
-
Develop a daily sleep schedule. Babies sleep best when they have consistent sleep times and wake times.
 Note that cutting back on naps to encourage nighttime sleep results in overtiredness and a worse night’s sleep.
Note that cutting back on naps to encourage nighttime sleep results in overtiredness and a worse night’s sleep. -
Encourage use of a security object. Once your baby is old enough (by 12 months), introduce a transitional/love object, such as a stuffed animal, a blanket, or a t-shirt that was worn by you (tie in a knot). Include it as part of your bedtime routine and whenever you are cuddling or comforting your baby. Don’t force your baby to accept the object, and realize that some babies never develop an attachment to a single item.
-
Develop a bedtime routine. Establish a consistent bedtime routine that includes calm and enjoyable activities that you can stick with as your baby gets older. Examples include a bath and bedtime stories. The activities occurring closest to “lights out” should occur in the room where your baby sleeps. Also, avoid making bedtime feedings part of the bedtime routine after 6 months.
-
Set up a consistent bedroom environment. Make sure your child’s bedroom environment is the same at bedtime as it is throughout the night (e.g. lighting). Also, babies sleep best in a room that is dark, cool, and quiet.
-
Put your baby to bed drowsy but awake. After your bedtime routine, put your baby to bed drowsy but awake, which will encourage her to fall asleep independently. This will teach your baby to soothe herself to sleep, so that she will be able to fall back to sleep on her own when she naturally awakens during the night.
-
Sleep when your baby sleeps. Parents need sleep also. Try to nap when your baby naps, and be sure to ask others for help so you can get some rest.
-
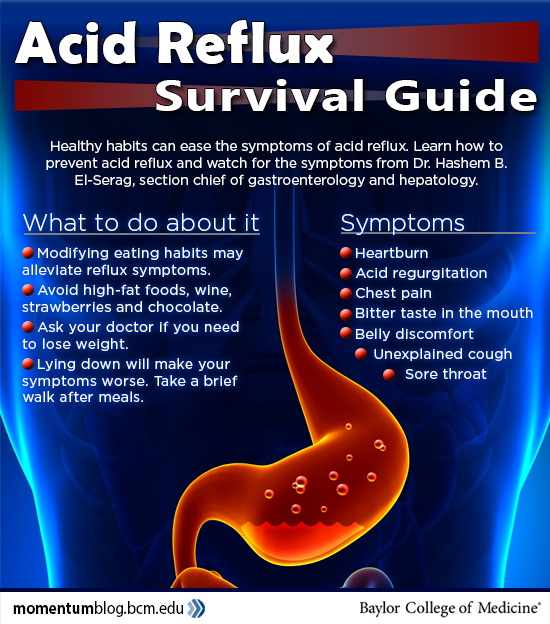
Contact your doctor if you are concerned. Babies who are extremely fussy or frequently difficult to console may have a medical problem, such as colic or reflux.
 Also, be sure to contact your doctor if your baby ever seems to have problems breathing.
Also, be sure to contact your doctor if your baby ever seems to have problems breathing.
Adapted from: Mindell JA & Owens JA (2003). A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. Philadelphia: Lippincott Williams & Wilkins.
Pediatric Sleep Disorders | OHSU
A good night’s sleep is essential for your child’s well-being. When sleep is disrupted, children may have health, behavior and development problems. At OHSU Doernbecher Children’s Hospital, doctors will give your child or teen the most effective treatment in a caring environment.
You’ll find:
- Experienced sleep specialists who do more than 700 sleep tests a year.
- A coordinated team of child specialists in:
- Sleep medicine
- Pulmonology (the respiratory system)
- Otolaryngology (ear, nose and throat)
- Neurology (the brain and nerves)
- Craniofacial surgery
- Sleep tests in a homelike setting where you can stay with your child.

- Sleep tests at Doernbecher for children on ventilators or who can’t be in a regular bed.
Understanding sleep disorders
What are sleep disorders?
Sleep disorders happen when your child has trouble falling asleep or staying asleep at night. Sleep can be disrupted because of blocked airways, low iron levels, neurological disorders or other causes. Left untreated, your child may have problems functioning or may develop health problems.
Why is sleep so important?
Children who don’t get enough sleep at night become fatigued and irritable. They may have problems with attention, learning, and behavior at home and at school. Poor sleep can also affect a child’s growth, blood sugar levels and immune system.
Types of sleep disorders
The most common are:
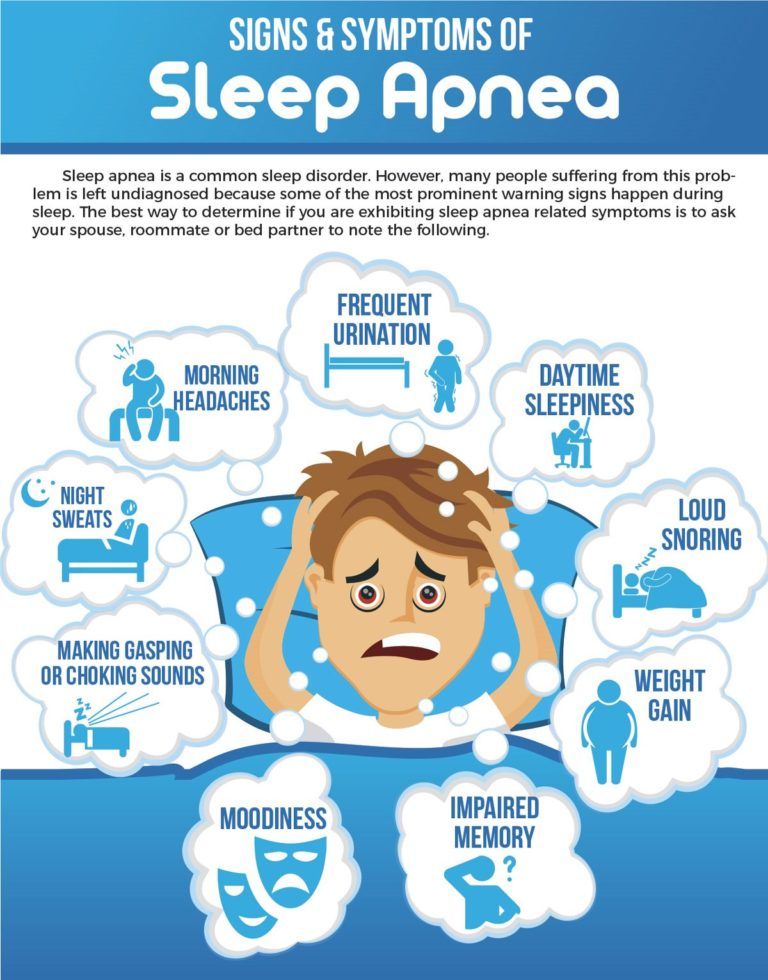
Sleep apnea: Up to 4% of children, typically ages 2 to 8, have sleep apnea. The two types are:
- Obstructive sleep apnea: The most common type occurs when soft tissue at the back of the throat blocks the upper airway.
 This cuts off oxygen for a few seconds until the child wakes up and breathes normally.
This cuts off oxygen for a few seconds until the child wakes up and breathes normally. - Central sleep apnea: This happens when the brain stops signaling a child to breathe, sometimes for a minute or longer. It’s usually linked to other conditions that involve the central nervous system (brain and spinal cord).
Insomnia: Your child has trouble falling asleep or staying asleep, or wakes too early. Causes can be poor sleeping habits, stress or anxiety. In the U.S., 45% of adolescents don’t get enough sleep, and some may suffer from insomnia, according to National Sleep Foundation.
Delayed phase sleep syndrome: This chronic disorder, common among teens, occurs when they go to bed two or more hours later than normal. This makes it hard to wake up the next morning.
Excessive sleepiness: This is unexplained sleepiness, with no other sleep disorder or related medical issue.
Periodic limb movement disorder: An urge to move or kick the legs repeatedly wakes the child. Scientists have linked this disorder to iron deficiency.
Scientists have linked this disorder to iron deficiency.
Parasomnia: This set of conditions is marked by abnormal movements during sleep. Doctors sometimes call it “things that go bump in the night.” Common types include:
- Nightmares: A child wakes from a frightening dream.
- Sleep terrors: A sleeping child sits up screaming, shouting or kicking. The child typically doesn’t respond to voices and has no memory of the event the next morning. These are also called night terrors.
- Sleep talking: A child talks during sleep.
- Sleepwalking: A child walks or makes other movements while partly awake.
Narcolepsy: This is a central nervous disorder in which the brain can’t properly regulate sleep and awake cycles. It’s uncommon in children. Children with narcolepsy have poor sleep, excessive sleepiness, sleep attacks and sudden loss of muscle control. They may also have cataplexy — sudden and uncontrollable muscle weakness that causes them to collapse.
They may also have cataplexy — sudden and uncontrollable muscle weakness that causes them to collapse.
Signs and symptoms of sleep disorders
If your child has any of these symptoms, see your child’s doctor. Your child may need to see a sleep specialist.
- Difficulty falling asleep
- Waking frequently
- Noisy, choppy breathing
- Tossing and turning all night
- Pauses in breathing while sleeping
- Gasping or snorting during sleep
- Nightmares
- Waking up screaming
- Sleep walking
- Restless legs
- Bedwetting
- Irritability
- Falling asleep in class
- Overweight
- Attention deficit hyperactivity disorder (ADHD)
Tests for sleep disorders
Your child’s doctor will gather his or her medical and sleep history to determine the best test. Tests include:
OHSU’s Dr. Derek Lam is an ear, nose and throat surgeon who specializes in sleep and aerodigestive disorders. He is the surgical director of our aerodigestive clinic.
He is the surgical director of our aerodigestive clinic. - Sleep study: A polysomnogram or PSG is an overnight study in our sleep lab to measure and record how your child is sleeping. The test is used to diagnose sleep apnea and other disorders. You can stay with your child through the night.
- Electroencephalogram (EEG): This test detects the brain’s electrical activity during sleep. It measures your child’s sleep stages and brief episodes of wakefulness.
- Multiple sleep latency test: This test is used for unexplained sleepiness and to diagnose narcolepsy. It measures brain activity and eye movement to see how quickly your child falls asleep during a series of naps.
- Actigraphy: The test is used to diagnose obstructive sleep apnea and insomnia. Your child wears a watch-like device with a sensor that measures sleep and awake patterns.
- Blood test: This can find iron deficiencies.
 Low iron levels have been linked to periodic limb movement disorder and restless legs syndrome.
Low iron levels have been linked to periodic limb movement disorder and restless legs syndrome.
Preparing for a sleep study
Sleep lab location:
The Residence Inn by Marriott at RiverPlace
2115 S.W. River Parkway, fifth floor
Portland, OR 97201
Treatments for sleep disorders
A range of specialists will confer about your child’s specific sleep disorder. Treatment will vary by diagnosis.
Sleep apnea
Surgery: Surgery to remove enlarged tonsils and adenoids is the first-line recommended treatment for children with obstructive sleep apnea. If a child has unusual facial anatomy, we may consider other options, such as craniofacial surgery.
Nonsurgical treatments: We’ll consider nonsurgical options if a child:
- Is not a good candidate for surgery
- Has central sleep apnea
- Has some remaining obstructive sleep apnea after surgery to remove the tonsils and adenoids
Nonsurgical options include:
- CPAP (continuous positive airway pressure): A CPAP machine improves breathing at night.
 The child wears a mask over the nose that’s connected by a hose to a machine that gently blows air. Your child’s doctor determines the correct air pressure to keep the airway open.
The child wears a mask over the nose that’s connected by a hose to a machine that gently blows air. Your child’s doctor determines the correct air pressure to keep the airway open. - BPAP (bilevel positive airway pressure): This machine, similar to a CPAP, helps some children exhale. It uses higher air pressure for inhaling and lower pressure for exhaling.
Medication: Nasal steroids and other medications may be prescribed to help open airways and ease your child’s breathing.
Insomnia
Medications: There are no FDA-approved medications specifically for children’s insomnia. Our doctors generally discourage using over-the-counter medicines for children with insomnia, but they can review all options with you.
Behavior therapy: Your child’s doctor will work with you to develop strategies and routines to help your child fall asleep and stay asleep. They include:
- Setting regular times for your child to go to bed and wake up every day.
- Limiting the amount of time in bed without sleeping.
- Restricting sugar.
- Avoiding caffeine.
- Reducing television time.
- Minimizing use of smartphones or video games before bed.
- Relaxation therapy, including deep breathing.
- Exercising regularly.
Environmental changes: Create signals, such as blackout curtains, to help a child fall asleep.
Delayed phase sleep syndrome
Medications/supplements: Melatonin supplements or medications may be prescribed for a short time and with behavior strategies.
Behavior therapy: Your child’s doctor will work with you to develop strategies including:
- Setting regular times for your child to go to bed and wake up every day.
- Restricting sugar and caffeine before bed.
- Setting a quiet time before bed with no smartphones, television or video games.
Bright light therapy: Exposure to a special light box early in the morning can readjust your child’s body clock.
Periodic limb movement disorder
Supplements: Iron supplements may be prescribed if your child has low iron levels.
Behavior therapy: Your doctor will work with you to develop strategies including:
- Setting regular times for your child to go to bed and wake up every day.
- Restricting sugar and caffeine before bed.
- Setting a quiet time before bed with no smartphones, television or video games.
- Increasing physical activity.
- Avoiding food or medication that may worsen the condition.
Restless legs syndrome
Supplements: Iron supplements may be prescribed if your child has low iron levels.
Behavior therapy: Your child’s doctor will work with you to develop strategies including:
- Setting regular times for your child to go to bed and wake up every day.
- Restricting sugar and caffeine before bed.
- Setting a quiet time before bed with no smartphones, television or video games.
- Increasing physical activity.
- Avoiding food or medication that may worsen the condition.
Parasomnias
Behavior therapy: Your child’s doctor will work with you to develop strategies including:
- Setting regular times for your child to go to bed and wake up every day.
- Restricting sugar and caffeine before bed.
- Setting a quiet time before bed with no smartphones, television or video games.
- Increasing physical activity.
- Avoiding food or medication that may worsen condition.
Parent counseling: Parents are guided on what they can do when their child has a parasomnia. For example, with night terrors, parents are advised to stay calm, to not try to wake the child, and to make sure the child can’t hurt him or herself.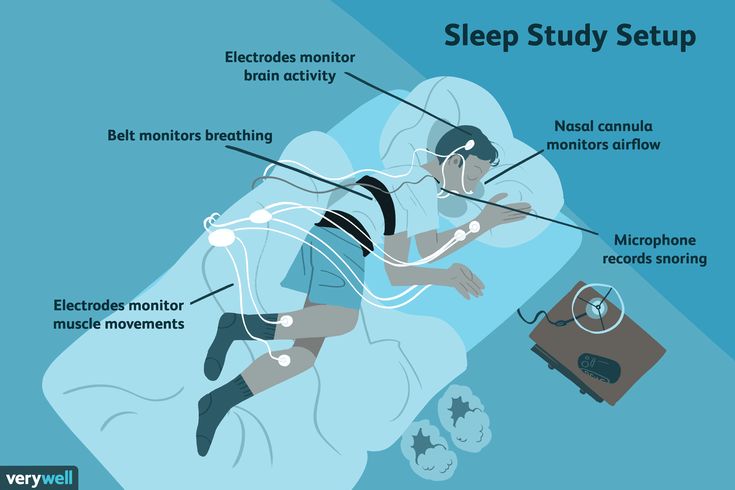
Narcolepsy
Medications: Alert medication such as modafinil in the morning can increase wakefulness. Antidepressants before bed can help a child sleep.
Behavior therapy: Your child’s doctor will work with you to develop strategies including:
- Scheduling nap times.
- Avoiding activities when not alert, such as swimming or driving.
- Exercising.
- Lifestyle counseling.
Learn more
OHSU Healthy Families blog
Other information
- Sleep in Middle and High School Students, Centers for Disease Control and Prevention
- Children and Bedtime Fears and Nightmares, National Sleep Foundation
- Baby Sleep Advice by Experts, Pediatric Sleep Council
- Pediatric Sleep-disordered Breathing, American Academy of Otolaryngology
For families
Call 503-346-0640 to:
- Request an appointment.

- Seek a second opinion.
- Ask questions.
Location
Parking is free for patients and their visitors.
Doernbecher Children’s Hospital
700 S.W. Campus Drive
Portland, OR 97239
Map and directions
Find other locations across Oregon and in southwest Washington.
Refer a patient
Story for children
causes, symptoms and treatment at the Family Doctor clinic in Moscow
Doctors
Clinic doctors
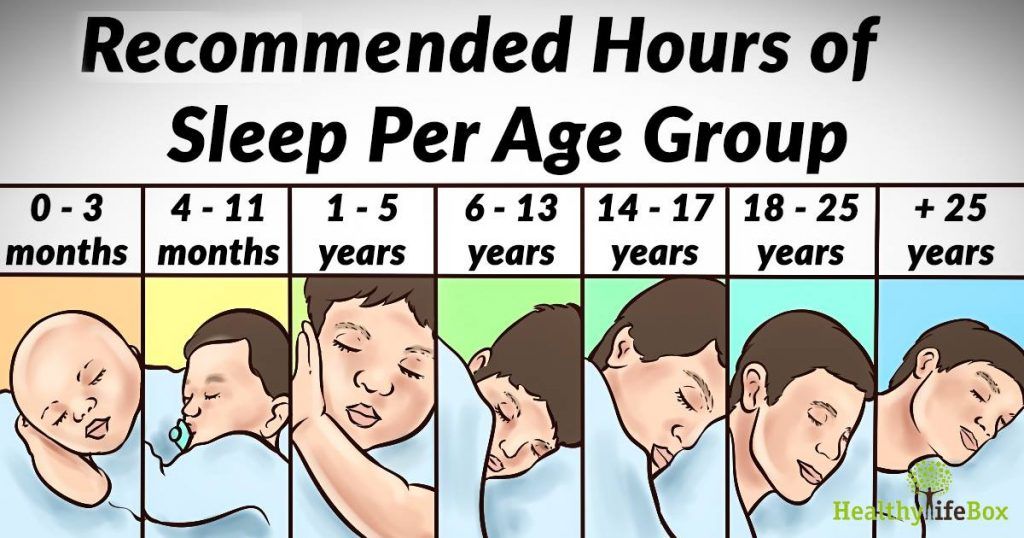
Sleep disorders in children (insomnia) are quite common, they are not considered a separate disease, 95% are due to somatic or mental pathology. Parents complain that the kids do not fall asleep well, sleep restlessly at night. Teenagers sometimes have sleep inversions, when daytime rest takes longer than nighttime. This is due to physiological reasons. In addition, sleepwalking, enuresis, grinding of teeth (bruxism) and other phenomena can disturb sleep. Normally, the duration and quality of sleep differ in children of different ages, which is reflected in Table 1.
In addition, sleepwalking, enuresis, grinding of teeth (bruxism) and other phenomena can disturb sleep. Normally, the duration and quality of sleep differ in children of different ages, which is reflected in Table 1.
Table 1. Features in children of different ages
| Age | Sleep features |
| 0-28 days | Rest time is evenly distributed throughout the day. |
| 1–12 months | Gradually, a continuous night sleep is formed, daytime episodes become shorter and shorter. |
| 1–3 years | The time of daytime rest decreases, gradually disappearing. |
| 4–9years | Reduced night time. |
| 9–14 years old | The need for rest increases with puberty. |
| 15 years and older | The cycle of wakefulness is close to that of adults. |
The quality of sleep in children also differs. So, up to 6 months, the phase of REM sleep predominates: the REM phase. At this time, people sleep very sensitively, rapid eye movements under closed eyelids are noted - the brain processes the information received.
After six months of the sleep phase, children resemble adults: the REM phase is observed approximately 1.5 hours after falling asleep. Further, the deep sleep phase (NREM) lasts until midnight, and after midnight NREM and REM alternate. Awakening occurs in the REM phase.
Reasons
Children's sleep disorders are caused by various causes. The main ones are summarized in Table 2.
Table 2. Causes of violations
| Cause | Features |
| Physiological | Do not let sleep: desire to eat, go to the toilet. |
| Psychological | Emotional excitement. |
| behavioral | In case of violation of the ritual of falling asleep. So, if the baby always falls asleep with a toy, then it will be difficult for him to fall asleep without a toy. |
| Pathological | Fear of deterioration at night prevents sleep. For example, a child suffering from bronchial asthma may be afraid of an asthma attack that usually occurs in the morning. |
| Pharmacological | Nootropics and some other drugs activate the brain, which can interfere with sleep. |
Causes of sleep disturbance in children in 80% of cases
- Emotional arousal.
- Activities in the evening: outdoor games, watching TV, Internet surfing.

- Overwork. Many lessons at school, extra classes, sports sections.
- Fear of the dark or being alone.
- Discomfort due to pain, hunger, illness.
- Eating caffeinated foods and carbonated sugary drinks in the evening.
Sleep disorders in neurotic disorders in children
Most neurogenic disorders are accompanied by a violation of falling asleep and night rest, which negatively affects the general condition of patients.
Table 3. Features of insomnia in neurogenic disorders
| Pathology | Features of insomnia |
| Down syndrome | Risk of apnea and bronchial obstruction. Children snore, fall asleep with difficulty, often sitting. |
| Angelman syndrome | All types of disorders, including enuresis and bruxism. |
| Prader-Willi syndrome | Difficulties in breathing are due to the small size of the nasopharynx, coupled with enlarged tonsils. The situation worsens in the presence of obesity. |
| Smith-Magnelis Syndrome | Decrease in total sleep time, violation of its quality. Nighttime awakenings for drinking or going to the toilet are common. |
| Ondine Syndrome | The sensitivity of the respiratory center to an increase in the concentration of carbon dioxide is impaired. Apnea during the NREM phase can be fatal. |
In children suffering from neurogenic diseases, insomnia worsens the quality of life, so it is necessary to pay attention to this, create conditions for a good night's rest, and contact a pediatric neurologist in a timely manner.
Symptoms of sleep disorders in children
Sleep disturbance. The child delays the moment when it is necessary to go to bed. She turns in bed, can cry, does not let her parents go for a long time, is afraid to be alone. Constantly getting up to drink, eat or go to the toilet.
Sleep problems in a child. Wakes up at night, tosses and turns, cries. Can't sleep.
As a result, the duration of night rest is significantly reduced. During the day, the child is drowsy, apathetic, constantly yawning. His emotional state is unstable, quickly moving from aggression to tearfulness. The eyes are red, the look is "glassy". Does not want to do anything, referring to fatigue. Wakes up with difficulty in the morning, does not want to go to kindergarten or school. Eating badly. Communication with people weighs him down, even with parents and friends.
You should consult a doctor if there are at least 2 sleepless nights during the week. Or if the child sleeps less than normal for a week or more.
Or if the child sleeps less than normal for a week or more.
Diagnosis
First of all, you need to contact a pediatrician. He will examine the child, determine his condition, exclude somatic diseases. To do this, he can appoint consultations of doctors of various specialties, laboratory and instrumental studies.
The doctor will ask about the living conditions, habits, daily routine and the load on the child. If necessary, he will refer you to a pediatric neurologist or psychotherapist to clarify the diagnosis and treatment.
Sleep disorders in children. Treatment
First of all, parents need to restore the daily routine, create a ritual of going to bed. The end time for preschoolers is at 20–21 o'clock, for schoolchildren – 21–22 o'clock.
In the evening, the room needs to be ventilated, it is optimal to maintain the temperature in it at about 21 about C. If the air is dry, use a humidifier.
The bed should be comfortable. It is better to choose an anatomical mattress and pillow, lay sheets without folds. Do not allow food in bed so that there are no crumbs. Use a duvet according to the season. Parents report that children sleep better under heavy blankets.
It is better to choose an anatomical mattress and pillow, lay sheets without folds. Do not allow food in bed so that there are no crumbs. Use a duvet according to the season. Parents report that children sleep better under heavy blankets.
Improves falling asleep evening walk. The brain is saturated with oxygen, the nervous system calms down.
2 hours before the end of the day, exclude the use of gadgets, watching TV, active games. You can play calm games, draw, read.
The last snack is 1.5–2 hours before going to bed, otherwise the active work of the intestines will prevent you from falling asleep.
Before lights out, you can arrange a warm relaxing bath, soothing herbal tea.
If these measures are not enough, the doctor may additionally prescribe: physiotherapy, psychotherapy, physiotherapy exercises, massage. If there is no effect, drug therapy is used.
Complications
Sleep disorders in children negatively affect the functioning of the body. The fact is that it is in sleep that some hormones are produced, in particular somatotropin, which affect the growth and development of a person. If the situation is not brought back to normal, physical and mental development is disturbed, and sometimes mental deviations develop.
The fact is that it is in sleep that some hormones are produced, in particular somatotropin, which affect the growth and development of a person. If the situation is not brought back to normal, physical and mental development is disturbed, and sometimes mental deviations develop.
Table 4. Types of insomnia
| Title | Features |
| Dyssomnias | Violations of the duration and quality of sleep, difficulty falling asleep. |
| parasomnia | Sleepwalking, enuresis, grinding of teeth. |
| Hypersomnia | Difficulty waking up, daytime sleepiness. |
To get a consultation with a child and adolescent psychotherapist, contact the Family Doctor clinic by calling the unified contact center in Moscow +7 (495) 775 75 66, use the online appointment service for a doctor or contact the clinic reception.
Popular questions
What to do about insomnia in children under one year old?
Parents need to accustom their child from birth to sleep with normal household noise. The baby does not need a separate room for falling asleep, he can sleep anywhere when he gets tired. If you immediately create special conditions, for example, absolute silence, then in the future the baby will wake up from any noise, which greatly complicates the life of parents.
If a baby has insomnia, you need to exclude its objective causes: find out what is bothering you. Perhaps he experiences discomfort from new clothes, the smell of washing powder, colic, teething. By eliminating the cause of anxiety, you can return the child to a restful sleep. If this does not work, contact your pediatrician or pediatric neurologist.
How to normalize a teenager's sleep?
Due to the uneven development of brain structures in the puberty period, sleep disorders are observed in almost all adolescents. The matter is complicated by adherence to gadgets, endless scrolling through social networks. Therefore, you need to start by building a daily routine and limiting surfing the Internet before bedtime. If you cannot reach an agreement, sign up for a consultation with a psychotherapist.
The matter is complicated by adherence to gadgets, endless scrolling through social networks. Therefore, you need to start by building a daily routine and limiting surfing the Internet before bedtime. If you cannot reach an agreement, sign up for a consultation with a psychotherapist.
How many hours does a child need to sleep?
Table 5. Norms
| Age | Duration of sleep | 2 months | 12-18 |
| 1–3 years | 11-16 |
| 4–6 years old | 9-14 |
| 7–17 years | 7-11 9000 |
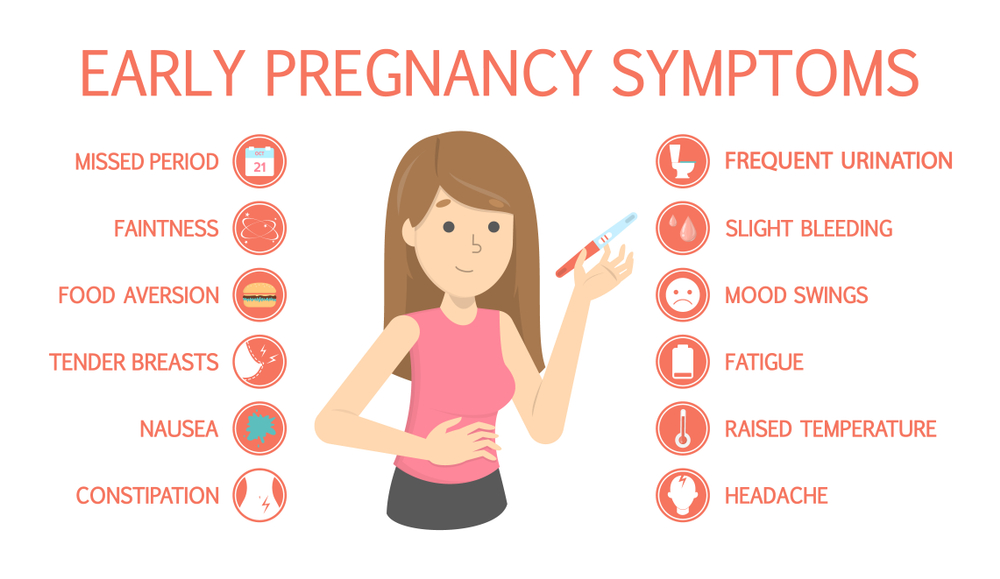
| Sleep disorders in children under one year old The happiness of being parents can be overshadowed by the stubborn unwillingness of the baby to sleep peacefully, which cannot but affect his mood. The child becomes moody and whiny. Yes, and the mother will be nervous and irritable. In this case, you should pull yourself together, because the bond between mother and child is very strong. Causes of insomnia A child's sleep disorder may be due to physiological or psychological causes. Physiological factors include: 1. Feeling of hunger. It happens that the mother's milk is not enough to saturate the baby. In this case, you can not do without complementary foods with a milk mixture. The psychological factor will be a disorder of the nervous system. If a child shudders for no reason or cries out in a dream, it is necessary to contact a neurologist or a somnologist. Only these specialists accurately diagnose the cause of the sleep disorder and correct it. Sometimes there is no apparent reason for a baby's insomnia. In this case, it is also necessary to involve a doctor in solving the problem. Ways to normalize sleep In addition to the methods discussed earlier, you can help normalize the process of falling asleep in the following universal ways: |

 They are especially active at the age of 2–6 years.
They are especially active at the age of 2–6 years.  For one, 6 hours will be enough, and for another, 11 is not enough.
For one, 6 hours will be enough, and for another, 11 is not enough. 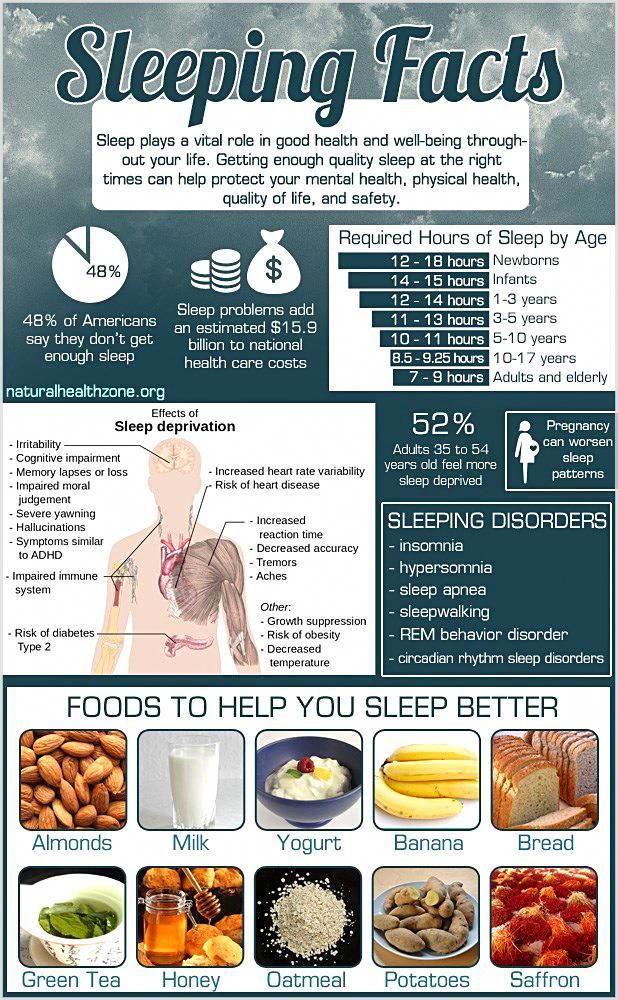
 If he is hot, the skin turns red, even droplets of sweat are visible. Cool hands, feet and nose mean that the baby is cold.
If he is hot, the skin turns red, even droplets of sweat are visible. Cool hands, feet and nose mean that the baby is cold. 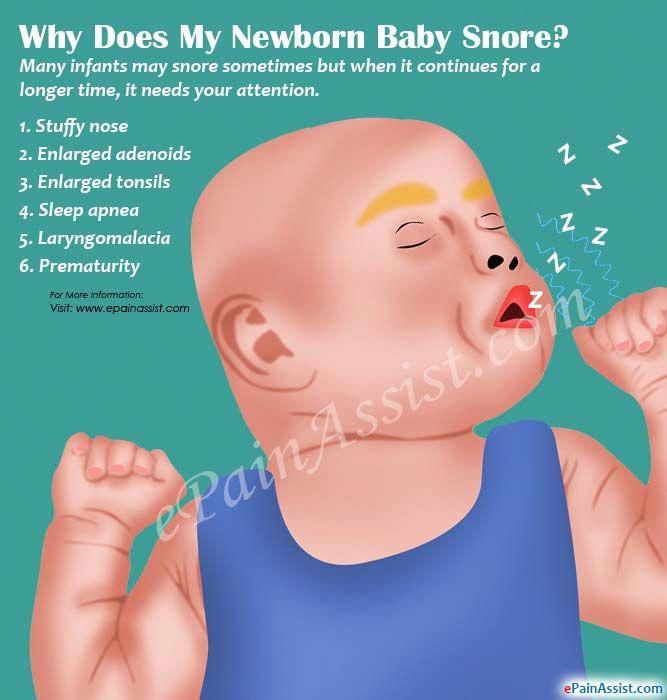 They disturb the child up to 4-5 months.
They disturb the child up to 4-5 months.