Signs of fetal compromise
Signs of Fetal Distress: What is Fetal Distress?
Understanding Complications Related to Fetal Distress
Fetal distress happens when a baby is not receiving an adequate amount of oxygen during pregnancy or labor. Typically, fetal distress can be detected through an abnormal fetal heart rate. While most pregnancies and childbirth happen without complications, it’s still critical for doctors and other medical providers to monitor the baby throughout every pregnancy stage to ensure that any potential complications are addressed immediately.
When fetal distress goes undetected, many problems can arise during pregnancy and labor. Here’s what you need to know.
What is Fetal Distress?
Fetal Distress is a medical condition which generally refers to “hypoxia” or low levels of oxygen in an unborn child. While it may occur before the onset of labor, it is more common during the delivery process. If fetal distress is not promptly corrected it can lead to injury to the unborn child, or worse.
Signs of Fetal Distress
Some common signs and symptoms of fetal distress include:
- Abnormal Heart Rates
- Decrease in Fetal Movement
- Maternal Cramping
- Abnormal Maternal Weight Gain
- Vaginal Bleeding
- Meconium in Amniotic Fluid
Each of these signs or symptoms may indicate fetal distress and should be monitored closely.
Abnormal Heart Rates
Babies who are progressing well in utero will have stable and robust heartbeats. Changes in heart rates and slower movement patterns or no movement at all can indicate a fetus may be in fetal distress. According to the National Center for Biotechnology Information (NCBI), a healthy fetal heart rate should be between 110 and 160 beats per minute (bpm). The following are heart rate abnormalities that can be associated with fetal distress:
- Fetal tachycardia is an abnormally fast heart rate and is identified by a heart rate higher than 160 to 180 bpm.

- Fetal bradycardia is an abnormally slow heart rate and is identified by a heart rate of less than 110 bpm.
- Variable decelerations happen when there is a sudden decrease in the fetal heart rate, and the decline is greater than or equal to 15 beats per minute and lasts for longer than 15 seconds — but less than 2 minutes from the onset to the return of the baseline rate.
- Late decelerations in a fetal heartbeat can happen through excessive uterine contractions or maternal hypotension, resulting in a decreased blood flow to the placenta. This is a cause for concern, and it can point to fetal acidemia. Fetal acidemia occurs when the blood becomes abnormally acidic.
Decrease in Fetal Movement
Medical professionals will monitor fetal movement to confirm a baby is progressing healthfully. Around 28 weeks of gestation, a baby will begin to establish movement patterns, including rest and stillness in the womb.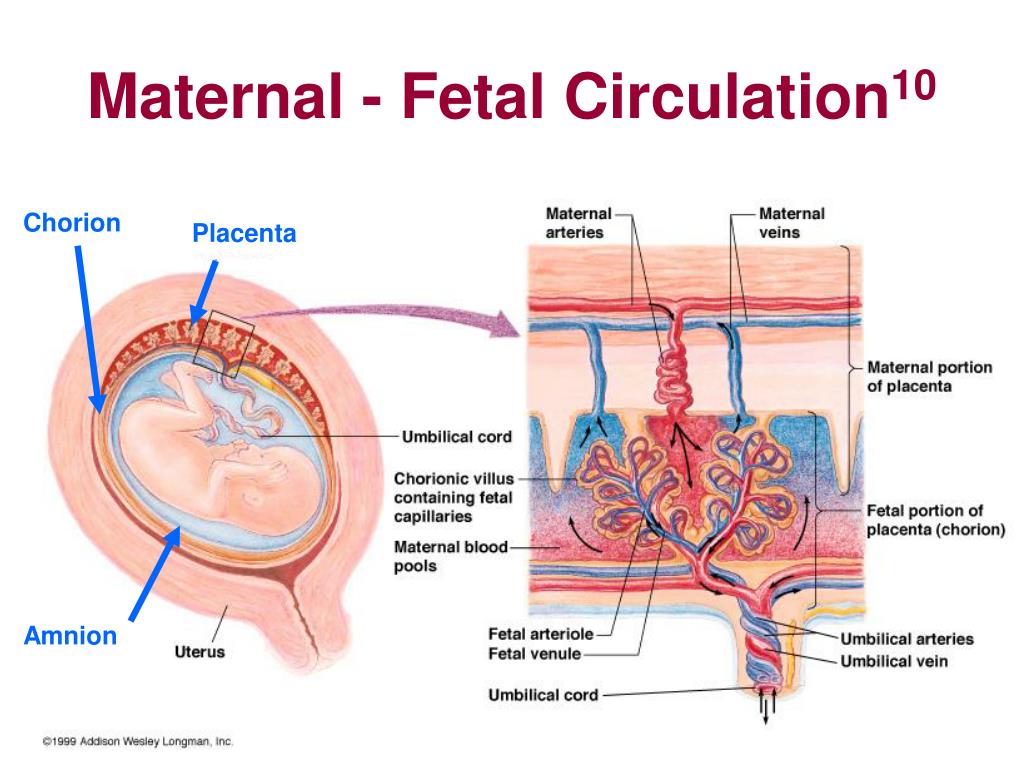 Doctors should ask expectant mothers if there are any noticeable changes in movement or movements that have stopped or decreased. Any decrease or abnormal change in movements can be a sign of fetal distress.
Doctors should ask expectant mothers if there are any noticeable changes in movement or movements that have stopped or decreased. Any decrease or abnormal change in movements can be a sign of fetal distress.
Maternal Cramping
It’s common for mothers to experience cramping as the fetus grows and the uterus expands. However, if intense cramping, along with severe back pain is happening, it could point to fetal distress and other complications. Report cramping to your doctor as soon as you begin feeling them so that they can be monitored.
Maternal Weight Gain
Healthy weight gain for expectant mothers should be between 25 and 40 pounds. It’s crucial for doctors and mothers to monitor weight gain, as excessive weight gain over 40 pounds could lead to fetal distress.
Vaginal Bleeding
When a pregnant mother is experiencing vaginal bleeding, it should be reported to medical professionals immediately. Vaginal bleeding could indicate the following problems related to fetal distress:
Placenta previa occurs when the placenta partially or completely covers the mother’s cervix (the lower part of the uterus).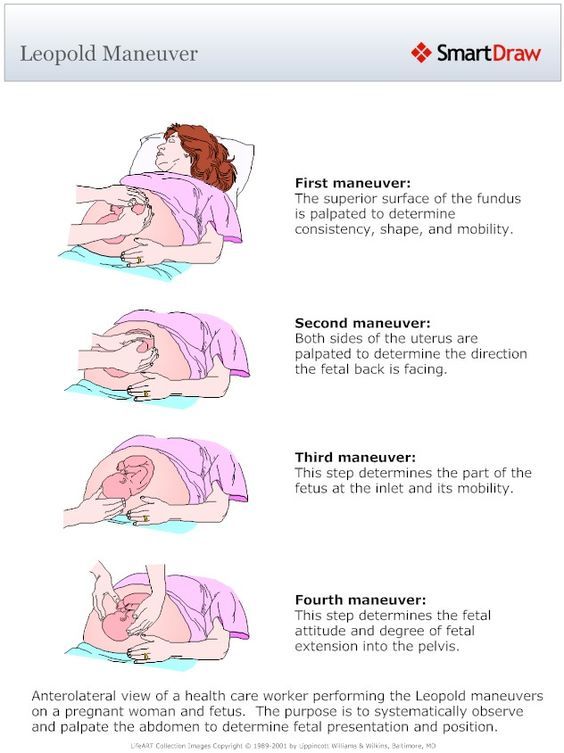 Placenta previa can cause heavy bleeding during pregnancy and delivery.
Placenta previa can cause heavy bleeding during pregnancy and delivery.
Vasa previa occurs when some of the fetal umbilical cord blood vessels run across or close to the cervix’s internal opening. Since the vessels are inside the amniotic membranes, they are unprotected by the umbilical cord or placenta, and as a result, the vessels can rupture as the membranes break. Although vasa previa is very rare, it can cause severe pregnancy complications.
Meconium in the Amniotic Fluid
Meconium, a thick, tar-like substance, can be found in a baby’s intestines during pregnancy. While it’s not usually released from your baby’s bowel until after birth, in some cases, a baby will have a bowel movement before birth, releasing the meconium into the amniotic fluid. If meconium is present, it could indicate fetal distress, and your doctors should look for additional signs of fetal distress.
Dangerous (too low or too high) amniotic fluid levels can also point to fetal distress and should be monitored regularly.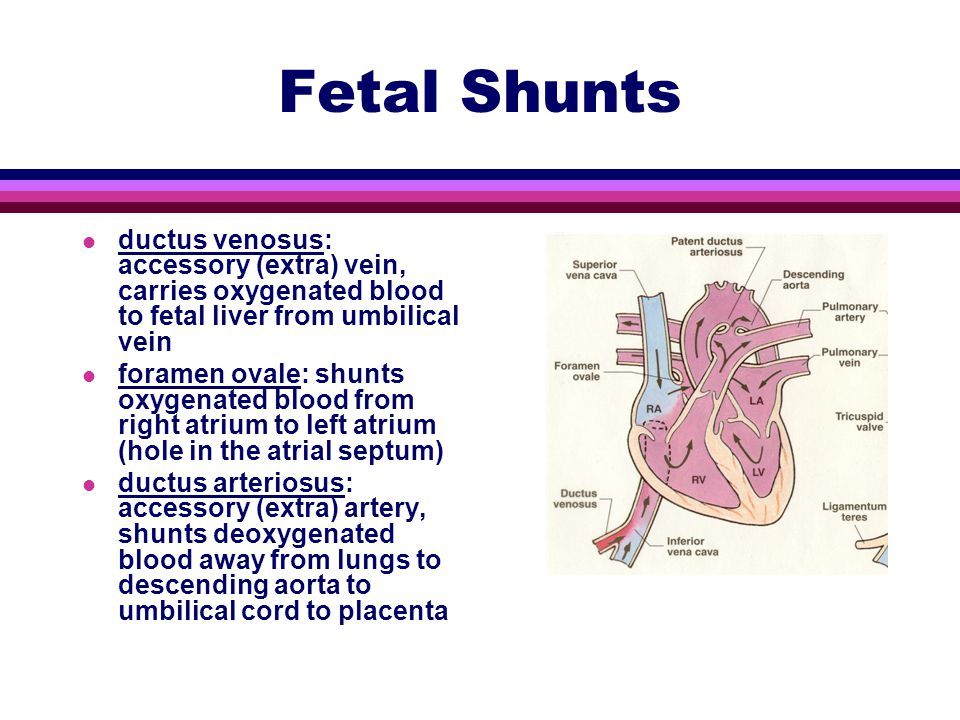
Common Causes of Fetal Distress
While Fetal Distress is thankfully not a common occurrence, there are a number of reasons it can occur.
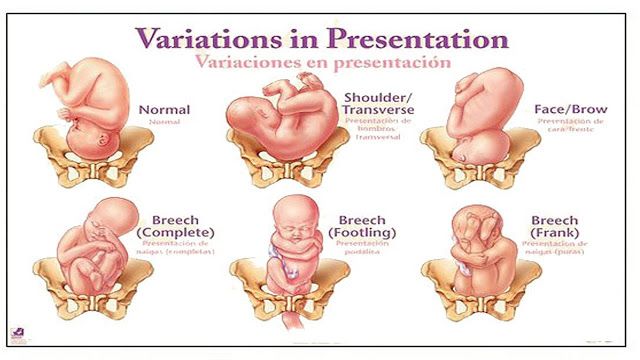
Mispositioning
The term mispositioning generally refers to when the unborn child is in a less than optimal delivery position which makes it difficult and sometimes even dangerous in the labor process. The baby being in the wrong position can occur naturally but it is important to correct the position to avoid complications such as fetal distress.
Improper Medical Tool Use
Although medical tools (i.e. forceps, vacuum extractors) may be of important use during the delivery, if used incorrectly they can lead to a whole host of complications, including but not limited to, fetal distress.
Tangled Umbilical Cord
Before the baby gets delivered, the umbilical cord can become wrapped around the unborn child’s neck or other body parts. If the tangle is not resolved and tightens it can lead to fetal distress, bodily injury or worse.
Poor Blood Circulation
Blood circulation is critical to the unborn child as that is the primary way they receive oxygen while inside their mother. There can be a number of causes for poor blood circulation such as health conditions of the mother (ie high blood pressure, asthma, diabetes) or it results from the stress of the pregnancy and labor itself on the mother’s body.
Placental Abruption
The placenta provides the unborn child with vital nutrients they need during their development. If the placenta ruptures or becomes detached from the wall of the uterus, fetal distress quickly occurs. This can be an extremely serious event should it occur. While acute trauma and the birth of a twin that results in fluid loss are recognized as possible causes of placenta abruption, in most instances the exact cause is not known.
Uterine Rupture
In this dangerous situation, if the uterus ruptures, severe internal bleeding can result. This complication requires immediate attention as both the mother and child’s life can potentially be in jeopardy.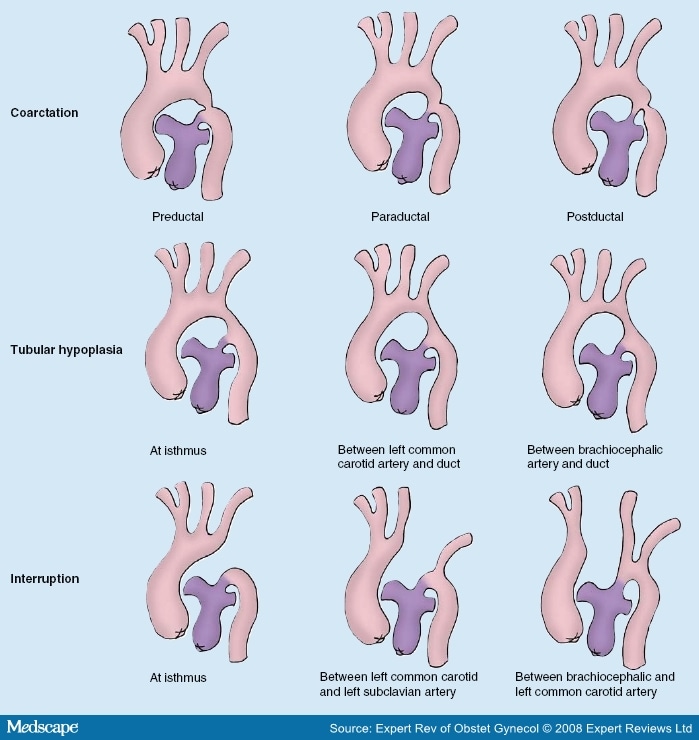
Mismanaging Fetal Distress Resulting in Birth Injury
Fetal distress is a complication that requires detection and proper intervention to prevent injury to the unborn child. If you believe that your child or loved one suffered an injury as a result of a medical provider failing to follow the standard of care during a fetal distress event, you may have a case for medical malpractice. Speak to one of our team of experienced birth injury attorneys to discuss your unique situation today.
The Long-Term Consequences of Fetal Distress
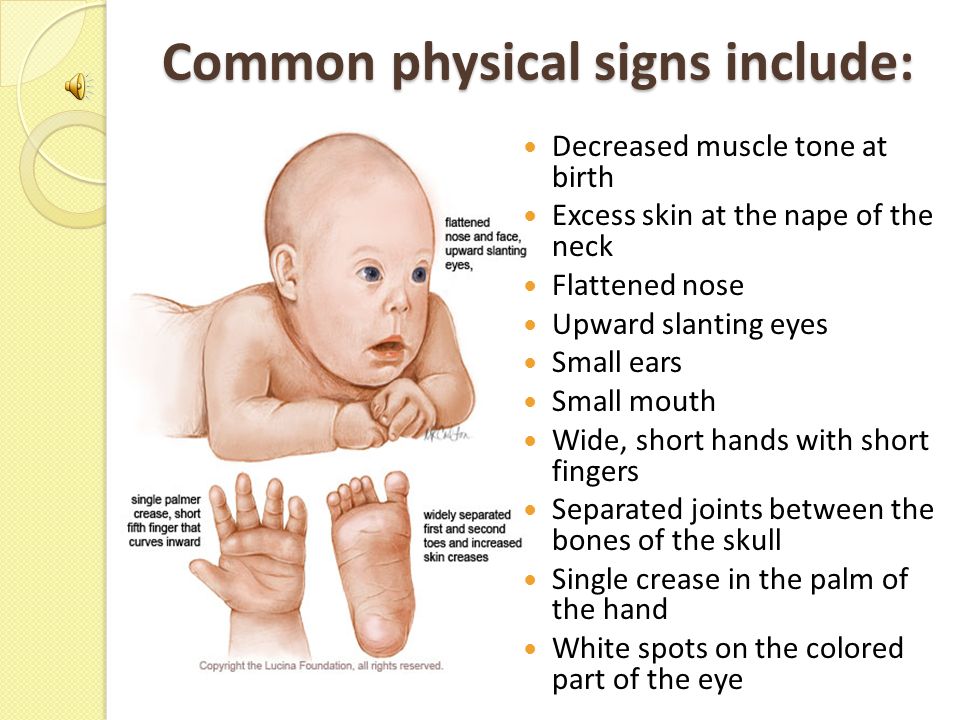
When a baby is delivered under fetal distress conditions, the consequences can be devastating, and the complications can pose life-long medical challenges. Some common conditions that can be linked to fetal distress are:
- Cerebral palsy
- Brain injuries
- Motor impairment
- Hearing and visual impairment
- Seizure disorders
- Mental health disabilities
While it can be challenging to detect disabilities in newborns, some symptoms may be present immediately, such as breathing difficulties and seizures as well as:
- Eating/feeding complications
- Failure to meet milestones such as sitting up and talking
- Lack of muscle tone or “floppy” arms and legs.
- Muscle spasms
- Lack of attentiveness/alertness
- Showing preference to one side of the body
If you notice any of the signs above, talk to your pediatrician as soon as possible for a proper diagnosis.
Did Your Child Suffer a Birth Injury Due to Fetal Distress? We can Help
If your child suffered a birth injury due to improper monitoring of fetal distress, our Philadelphia birth injury attorneys at The Villari Firm, PLLC are here to help you seek justice. Our experienced attorneys work with leading experts, including doctors and other legal professionals, to investigate and prepare cases for our clients. We spare no expense to ensure we are armed with everything needed to help our clients receive the compensation they deserve.
Contact The Villari Firm, PLLC at (215) 372-8889 to schedule a free consultation today.
Fetal distress | Pregnancy Birth and Baby
Fetal distress | Pregnancy Birth and Baby beginning of content7-minute read
Listen
Key facts
- Fetal distress is a sign that your baby is not well.

- Your doctor or midwife will monitor your baby’s heartbeat during pregnancy and labour to assess their wellbeing.
- If your baby shows signs of fetal distress, your midwife or doctor will act quickly to try and treat any underlying cause.
- You may need help to birth your baby quickly with an assisted (instrumental) delivery or caesarean section.
- Fetal distress can increase the risk of birth complications, especially if it isn’t treated quickly.
If you are pregnant and notice a decrease in your baby’s movements, seek urgent medical attention. This may be a sign that your baby is unwell.
What is fetal distress?
Fetal distress is a sign that your baby is not well. It happens when the baby isn’t receiving enough oxygen through the placenta.
Fetal distress can sometimes happen during pregnancy, but it’s more common during labour.
What causes fetal distress?
Fetal distress may occur when the baby doesn’t receive enough oxygen because of problems with the placenta (such as placental abruption or placental insufficiency) or problems with the umbilical cord (such as cord prolapse).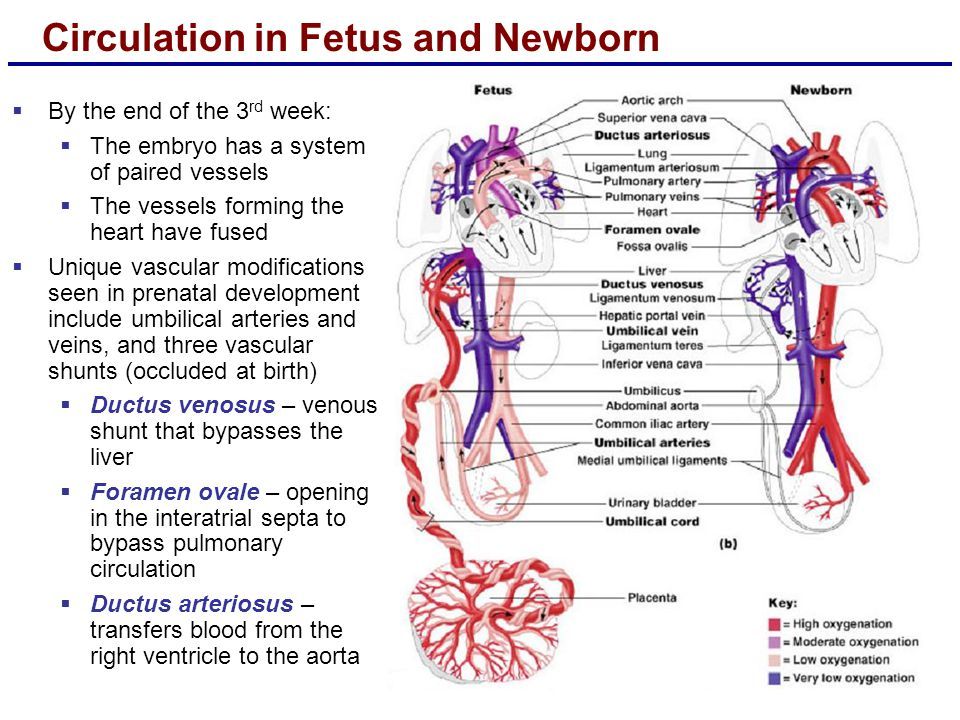
It is more common if you are overdue, have pregnancy complications or when there are other complications during labour. Sometimes it happens because the contractions are too strong or too close together.
Your baby is more likely to experience fetal distress if:
- you are obese
- you have high blood pressure in pregnancy or pre-eclampsia
- you have a chronic disease, such as diabetes, kidney disease or cholestasis(a condition that affects the liver in pregnancy)
- you have a multiple pregnancy
- your baby has fetal growth restriction
How is fetal distress diagnosed?
Fetal distress is diagnosed by monitoring the baby’s heart rate. A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
Your doctor or midwife might pick up signs of fetal distress as they listen to your baby’s heart during pregnancy.
Your baby’s movements are a sign that your baby is well. A change in your baby’s movements may be a sign of fetal distress.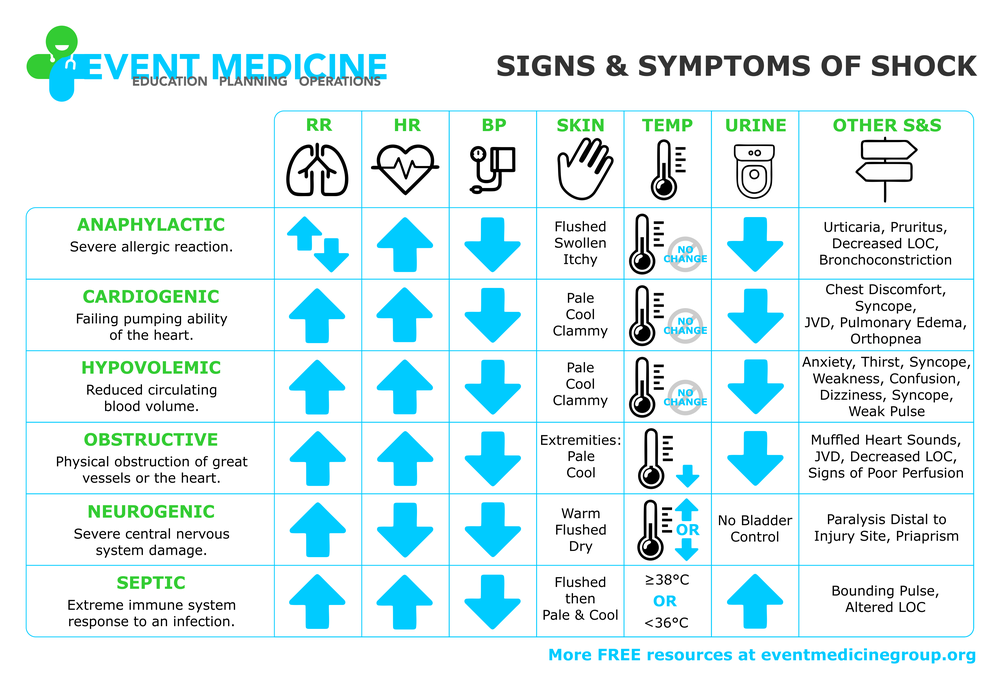
If you haven’t felt your baby move, or the pattern of moments has changed, contact your doctor or midwife immediately, as this may be a sign of fetal distress.
Another sign of possible fetal distress is meconium in the amniotic fluid. Let your doctor or midwife know right away if your notice your amniotic fluid is green or brown, since this could signal the presence of meconium (newborn poo, that your baby may pass while still in your uterus if they are distressed).
How is fetal distress managed?
There are a few ways that fetal distress may be managed. Your doctor will assess your situation and discuss with you the best management option in your situation.
If you are not in labour
Depending on your situation, your doctor or midwife may recommend interventions such as medicines or intravenous fluids. If these interventions do not help, your doctor may recommend an emergency caesarean section so you birth your baby quickly.
If you are in labour
You will usually be given you oxygen and fluids. Sometimes changing position, such as turning onto your side, can reduce the baby’s distress.
Sometimes changing position, such as turning onto your side, can reduce the baby’s distress.
You may be given medicine to slow down the contractions. If you had medicines to speed up labour, these may be stopped if there are signs of fetal distress.
Sometimes, a baby in fetal distress needs to be born quickly. Your doctor may recommend an assisted (or instrumental) birth or you might need to have an emergency caesarean.
Most of the time, there will be time to discuss your options with your doctor and/or midwife. However, in some emergency situations, your doctor or midwife will need to act quickly. If there are any medical interventions you object to, such as receiving a blood donation, it’s a good idea to make sure that your doctor and/or midwife are aware of this when you arrive at the hospital.
Does fetal distress have any lasting effects?
Babies who experience fetal distress are at greater risk of complications after birth. Prolonged lack of oxygen during pregnancy and birth can lead to serious complications for the baby, if it is not noticed and managed early.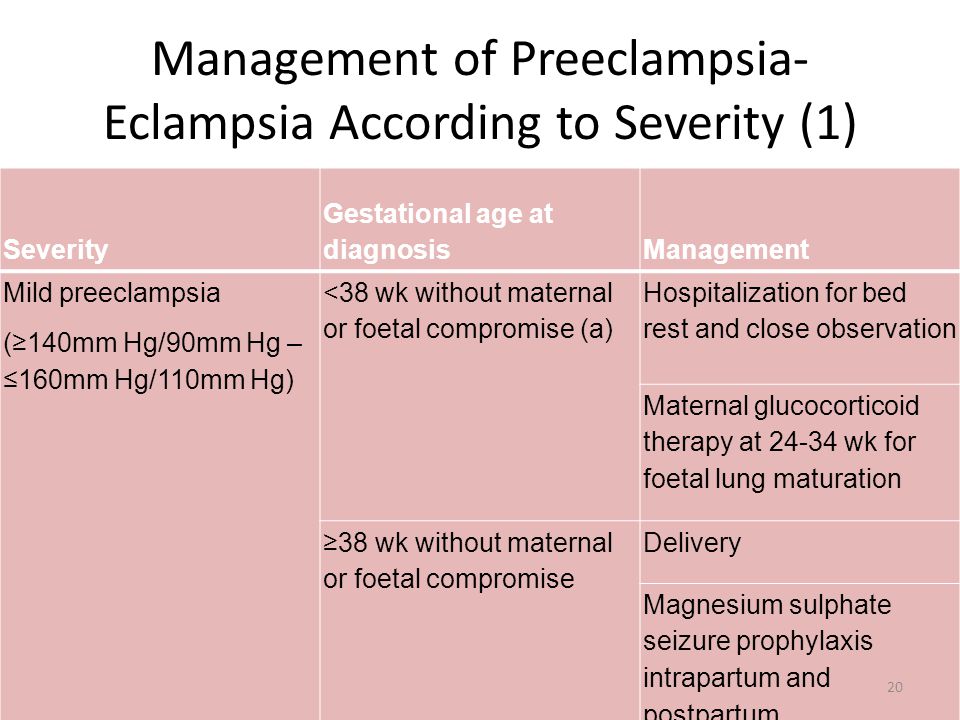 Complications may include brain injury, cerebral palsy and even stillbirth.
Complications may include brain injury, cerebral palsy and even stillbirth.
Fetal distress may require an assisted birth or caesarean section. While these interventions are safe, they are associated with their own set of risks and complications. Having fetal distress in one pregnancy doesn’t mean you will necessarily experience fetal distress in your next pregnancy. Every pregnancy is different. If you’re worried about future pregnancies, it can help to talk to your doctor or midwife so they can explain what happened before and during the birth.
Where can I find resources and support?
If your labour didn’t go to plan, you may experience difficult feelings about their birth experience.
If you feel sad, disappointed or traumatised about what happened, it is important to talk to someone. There are lots of people and organisations who can help, including:
- your doctor
- PANDAon 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blueon 1300 22 4636
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Australasian Birth Trauma Association (What is birth trauma?), King Edward Memorial Hospital (Fetal compromise (acute): Management if suspected), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Intrapartum fetal Surveillance Clinical Guideline)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Baby movements during pregnancy
- Fetal heart rate monitoring
- Giving birth - stages of labour
- Induced labour
- Interventions during labour
- Labour complications
Need more information?
Fetal heart rate monitoring
During pregnancy and labour, your baby's heart rate is monitored to check for any signs of distress.
Read more on Pregnancy, Birth & Baby website
Monitoring the Baby’s Heart Rate in Labour
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Pregnant women not to trust smartphone heart rate apps
Pregnant women are being urged not to rely on smartphone apps that claim to listen to your baby's heartbeat.
Read more on Pregnancy, Birth & Baby website
Baby movements during pregnancy
Every baby is unique and it is important for you to get to know your baby’s movement patterns.
Read more on Pregnancy, Birth & Baby website
Heart abnormality birth defects - Better Health Channel
Some congenital heart defects are mild and cause no significant disturbance to the way the heart functions.
Read more on Better Health Channel website
Ultrasound scans during pregnancy
Ultrasound scans will help you and your doctors monitor your baby’s health throughout your pregnancy. Find out more, including about why you might need one.
Read more on Pregnancy, Birth & Baby website
External cephalic version (ECV)
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour.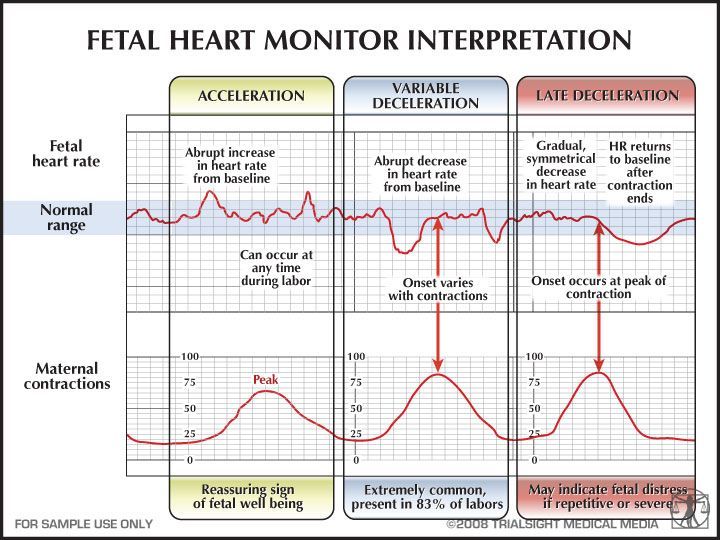 Find out what it means for you and your baby.
Find out what it means for you and your baby.
Read more on myDr website
Having a small baby
It's normal for parents to worry about their baby's birth weight and growth. Here’s what you need to know if you have been told your baby is likely to be small (less than 2.5kg at birth).
Read more on Pregnancy, Birth & Baby website
Baby due date - Better Health Channel
Pregnancy is calculated from the first day of your last period, not from the date of conception.
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.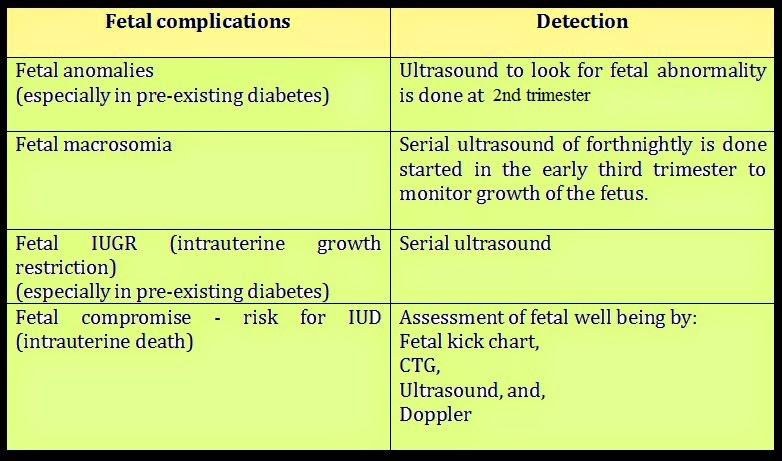
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.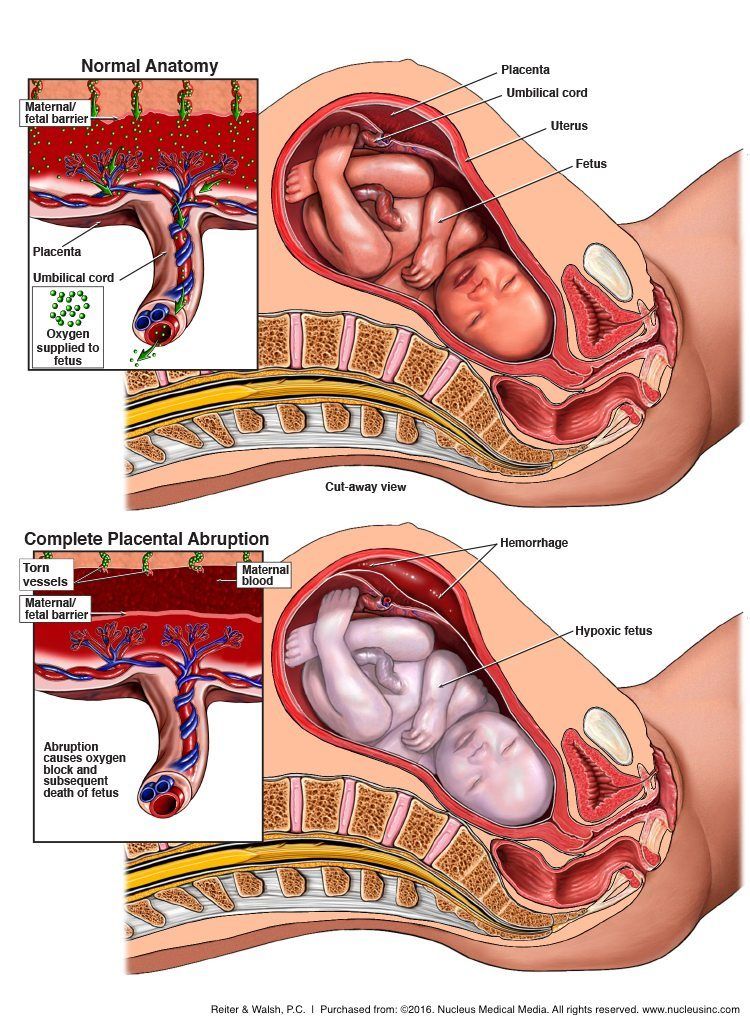
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
CTG during pregnancy: what it is and what it is for
Services and prices
CTG: (Multiple pregnancy)
2000 ₽
CTG: (Fetal cardiotocography)
1600 ₽
Cardiotocography (CTG) is a functional diagnostic method based on recording the fetal heart rate and uterine contractility during pregnancy and childbirth.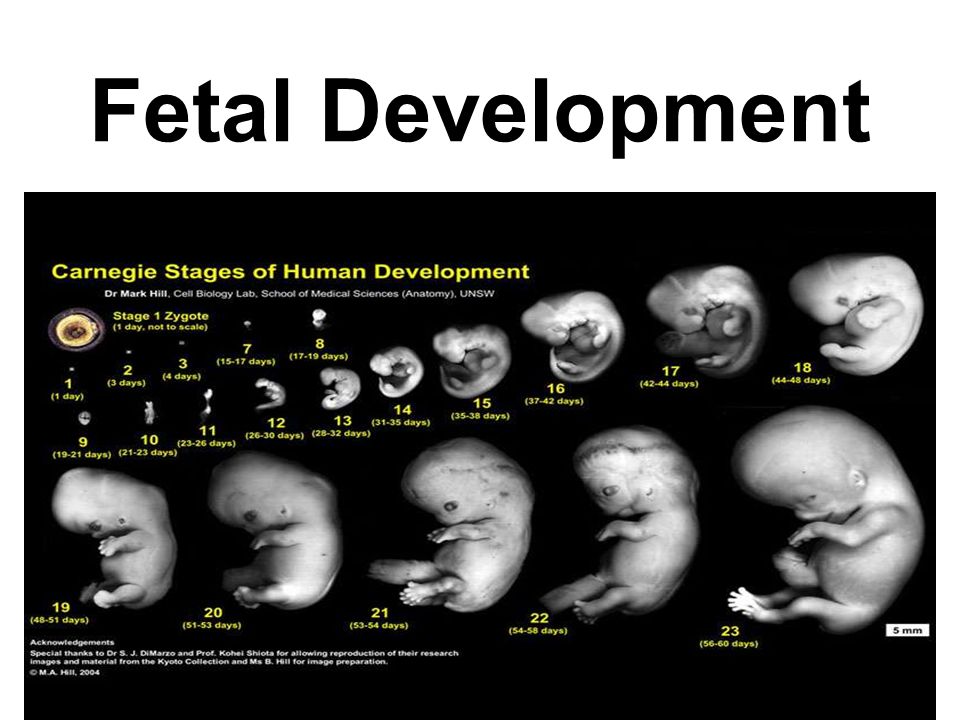 Cardiotocography is based on the Doppler effect and the principle of ultrasound. An ultrasonic wave is emitted from the transducer, which is reflected from the pulsating fetal heart, changes frequency and is sent back. The electronic system of the monitor registers and converts the signal. This recording is called a cardiotocogram.
Cardiotocography is based on the Doppler effect and the principle of ultrasound. An ultrasonic wave is emitted from the transducer, which is reflected from the pulsating fetal heart, changes frequency and is sent back. The electronic system of the monitor registers and converts the signal. This recording is called a cardiotocogram.
Two sensors are fixed on the belly of the pregnant woman. For better contact with the skin of the anterior abdominal wall, a special hypoallergenic gel is applied. At the point of best audibility of heart beats (usually around the navel), a heart rate sensor is applied, which records the fetal heartbeat. If the patient is pregnant with twins, then two sensors are used at once or measurements are taken in turn. The load cell registers the contractile activity of the uterus and the motor activity of the fetus.
Sometimes the baby's movements are recorded by an additional sensor. During the study, the device makes loud sounds, which should not be frightened.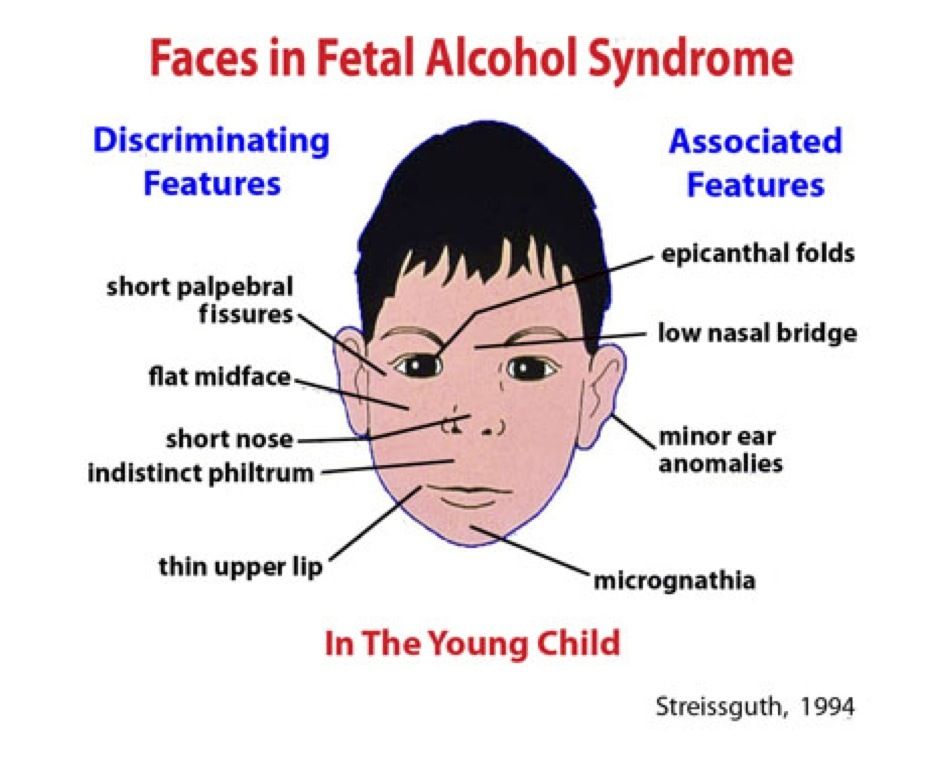 This is the baby's heartbeat. The fetus may change its position during the study, resulting in an incorrect recording. However, thanks to the sound component of the procedure, the doctor can control the correct location of the sensors and rearrange them in time after the child.
This is the baby's heartbeat. The fetus may change its position during the study, resulting in an incorrect recording. However, thanks to the sound component of the procedure, the doctor can control the correct location of the sensors and rearrange them in time after the child.
Cardiotocography, together with the results of other studies, allows you to recognize serious disorders, including fetoplacental insufficiency, intrauterine fetal hypoxia, various anomalies in the development of the fetal cardiovascular system, indirect signs of intrauterine infections, the threat of premature birth.
When and how often is the examination done?
The study is carried out no earlier than 32 weeks. It is by this time that the nervous and cardiovascular systems reach a certain maturity. By 8 months, a myocardial reflex is formed - the relationship between cardiac activity and motor activity of the fetus. At the same time, the activity-rest cycle is established. Rhythmic changes of sleep and wakefulness of the fetus follow each other during the entire remaining period of pregnancy.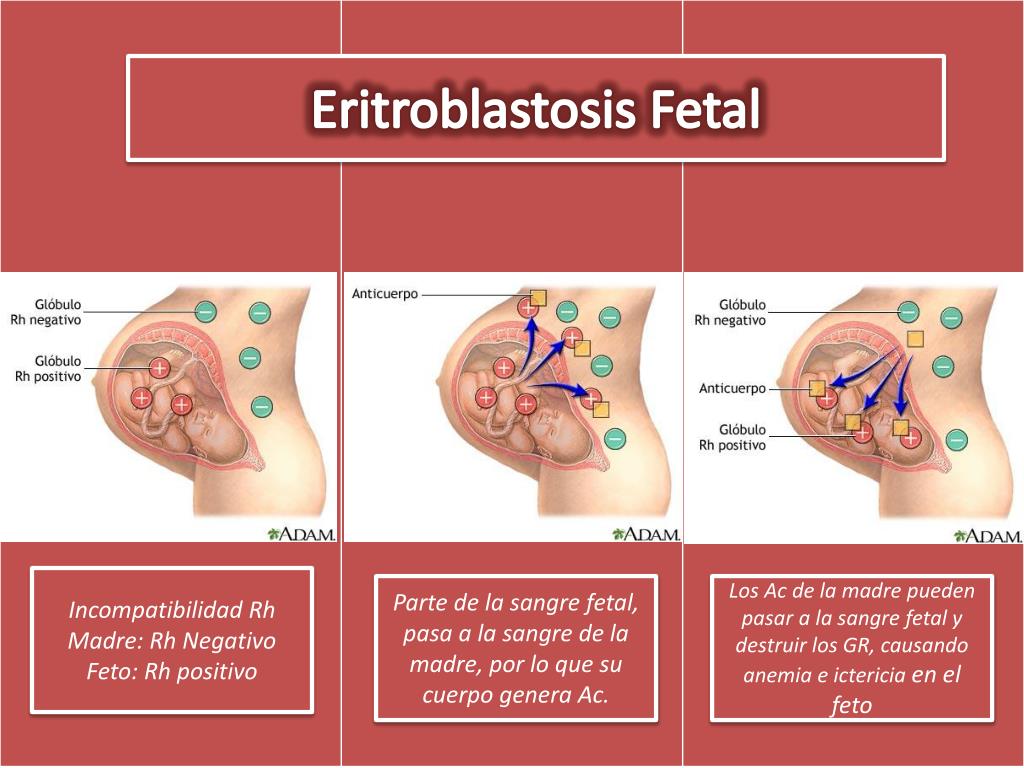
Cardiotocography must be performed 2 times during the 3rd semester. However, the frequency of the study is determined by the doctor based on the mother's history, pregnancy history, results of other examinations and risk factors.
Indications for examination
The purpose of cardiotocography is timely diagnosis and detection of fetal disorders. Based on the data of a number of functional diagnostic studies, such as ultrasound, CTG, dopplerometry, anamnesis, the obstetrician-gynecologist chooses the tactics of pregnancy management, treatment, the optimal term and method of delivery.
Indications for additional cardiotocography may include:
- Rh conflict
- Preeclampsia in the second half of pregnancy
- Maternal diseases
- Postterm pregnancy
- History of preterm birth
- Fetal growth retardation
- Pathologies of pregnancy and fetal abnormalities detected by ultrasound
- Oligohydramnios or polyhydramnios
- Multiple pregnancy
- Aggravated obstetric and gynecological history (abortions, miscarriages, premature births preceding this pregnancy)
- Change in the nature of fetal movements (complaints about a decrease or increase in the number of fetal movements per day)
Preparation for the procedure
The study does not require special preparation.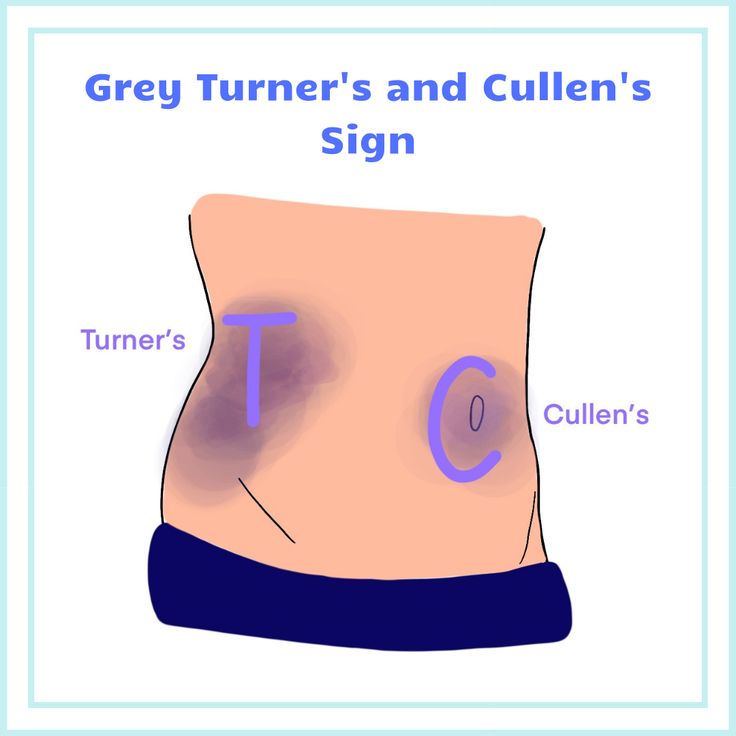 However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, it is recommended that a pregnant woman sleep well and relax. On the day of the study, it is worth taking care of a light meal 1-2 hours in advance. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including the phone, will have to be turned off, as the technique interferes with the recording.
However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, it is recommended that a pregnant woman sleep well and relax. On the day of the study, it is worth taking care of a light meal 1-2 hours in advance. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including the phone, will have to be turned off, as the technique interferes with the recording.
How long does Cardiotocography take?
The procedure lasts from 30 to 60 minutes, depending on the activity of the baby. After 32 weeks, the fetus is characterized by the presence of periods of sleep and wakefulness. The active state lasts 50-60 minutes, while the calm state lasts 20-30 minutes. When evaluating cardiotocography, the period of wakefulness of the fetus is the leading one.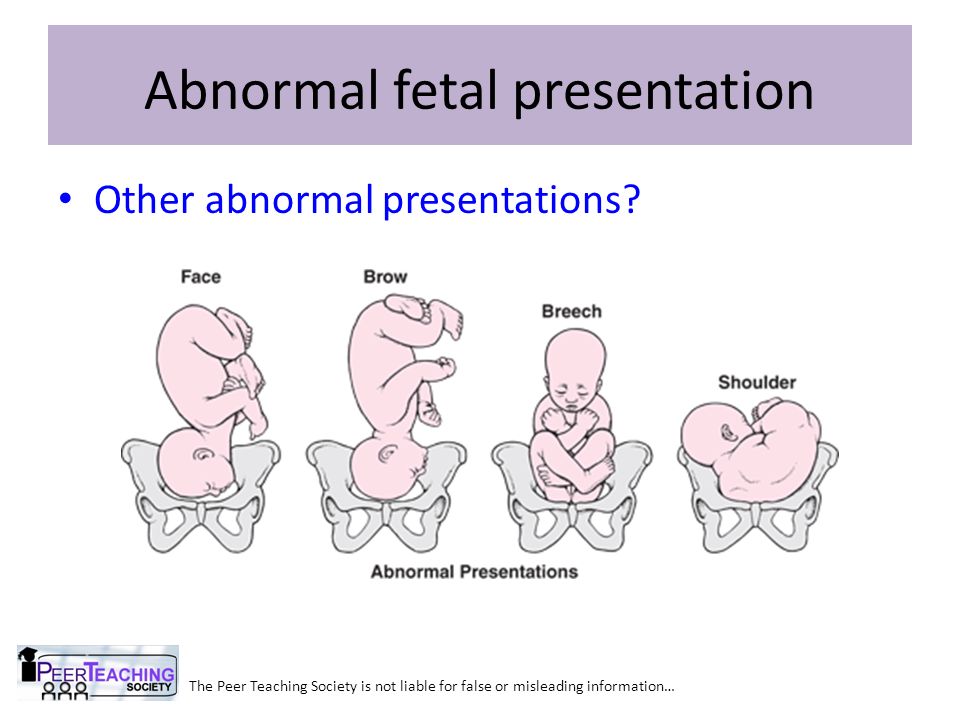 Therefore, the duration of the study may vary.
Therefore, the duration of the study may vary.
Indicators
When analyzing CTG, a number of indicators are taken into account.
- Basal rhythm.
The cardiac sensor records the heart rate, and the cardiotocograph calculates the average fetal heart rate, which remains unchanged for 10 minutes or more. This indicator is called the basal rhythm. Normally, the fetal heart rate is subject to slight changes.
- Rhythm variability.
Rhythm variability is spoken of by the number and amplitude of deviations from the basal rhythm.
- Acceleration periods.
Acceleration is a period of increase in the fetal heart rate by 15 or more beats per minute for 15 seconds or more compared to the basal rhythm.
- Deceleration periods.
Deceleration is an episode of slowing heart rate by 15 heart beats per minute or more lasting 15 seconds or more. Decelerations usually occur in response to uterine contractions or fetal movements.

- basal rhythm within 110-150 bpm
- heart rate variability amplitude - 5-25 bpm
- decelerations absent or sporadic, shallow and very short
- 2 or more accelerations are recorded during 10 minutes of recording. If this type of CTG is detected in a short study period, the recording may not be continued.
- 9-12 - the condition of the fetus is satisfactory
- 6-8 - the fetus is in a state of hypoxia, but there is no threat of death in the next day
- 0-5 - severe hypoxia, threat of intrauterine death
- 1-2 - signs of initial disturbances
- 2-3 - severe violations
- >3 - critical condition.
WHO recommendations The criteria for a normal cardiotocogram are the following:
If your CTG indicators do not match the WHO criteria, then this does not indicate pathology. Cardiotocography is a method that is very sensitive to external influences. The correct interpretation of the results of the examination is possible only by a specialist in conjunction with other data.
Interpretation of results
CTG decoding should be done only by a specialist. This is a difficult process that requires knowledge and experience. Cardiotocogram consists of two types of graphs - tachogram and hysterogram. The tachogram reflects the change in the heart rate of the fetus. Time is measured horizontally, and the number of beats per minute is measured vertically. Thus, the graph deviates downwards with a decrease in heart rate, and upwards with an increase. When measuring the motor activity of the fetus, the indicators are displayed under the tachogram. On the second graph, usually located in the lower part of the cardiotocogram, the force of uterine contraction is displayed.
The tachogram reflects the change in the heart rate of the fetus. Time is measured horizontally, and the number of beats per minute is measured vertically. Thus, the graph deviates downwards with a decrease in heart rate, and upwards with an increase. When measuring the motor activity of the fetus, the indicators are displayed under the tachogram. On the second graph, usually located in the lower part of the cardiotocogram, the force of uterine contraction is displayed.
Initially, a visual interpretation of CTG is performed. However, to reduce the subjectivity of the assessment, it is customary to use rating scales. There are two methods: the Gauthier scale and mathematical analysis.
Gautier's ten-point scale is a questionnaire where the doctor is asked to evaluate the basal rhythm, variability, the number of accelerations, decelerations, and fetal movement. Each of the indicators is rated from 0 to 2 points.
Based on the total scores, a conclusion and recommendations for further observation are formed.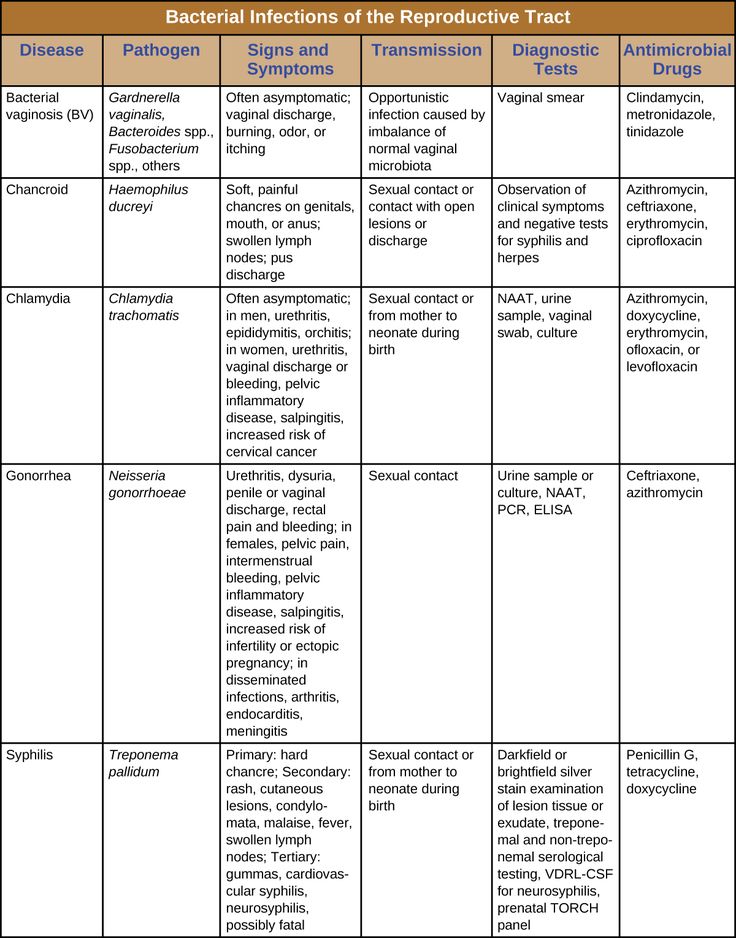 This scale has many modifications.
This scale has many modifications.
The second method of evaluation is mathematical. When interpreting computer-processed data, a fetal condition indicator (PSP) is used.
Scores above 2 indicate a dangerous condition that requires hospitalization in a maternity hospital.
The CTG method, like any other, has its drawbacks and errors. In some cases, fetal oxygen consumption may decrease, regardless of the presence of pathology. For example, compression of the umbilical cord by the fetus causes a short-term disruption of blood flow. In this case, cardiotocography will register fetal hypoxia. However, these changes are temporary and if the position of the fetus changes, the blood flow will be restored. Therefore, the conclusion is not a diagnosis, and only a doctor should evaluate and interpret the indicators of the cardiotocogram.
Effect of the procedure on the fetus
Cardiotocography is a study based on the action of ultrasonic waves, the safety of which has been proven by numerous studies and is beyond doubt. The procedure has no contraindications. If necessary, monitoring of indicators using CTG can be carried out several times a day or continuously, as during childbirth.
Back to the list of articles
How to detect blood flow disorders during pregnancy
- Home
- How to recognize the disease
- Pregnancy and childbirth
- Blood flow disorder during pregnancy
More about the doctor
How to determine the violation of blood flow during pregnancy?
Blood flow disorders during pregnancy is a symptomatic complex that develops against the background of a dysfunction of the placenta, which is fraught with irreversible consequences for the fetus. The danger is that there may be no signs on the part of the mother. Against the background of this pathology, there is a risk of the formation of defects, hypoxia, developmental delay and even death of the fetus. Diagnosis of obstetric pathology is performed using KGT, ultrasound and doplerometry. Therapy is carried out within the framework of a hospital with the use of drugs that can normalize the hemodynamics of blood vessels in the placenta.
The danger is that there may be no signs on the part of the mother. Against the background of this pathology, there is a risk of the formation of defects, hypoxia, developmental delay and even death of the fetus. Diagnosis of obstetric pathology is performed using KGT, ultrasound and doplerometry. Therapy is carried out within the framework of a hospital with the use of drugs that can normalize the hemodynamics of blood vessels in the placenta.
The main causes of pathology
The placenta is an incredibly important, but temporary organ that unites the circulatory systems of the mother and fetus. The main purpose of the placenta is to provide protection, nutrition for the crumbs, and excretion of waste products. This organ interacts with the vascular system of the fetus and mother, so it is customary to distinguish two forms of blood flow:
- fetal-placental;
- uteroplacental.
There are several reasons that cause blood flow problems.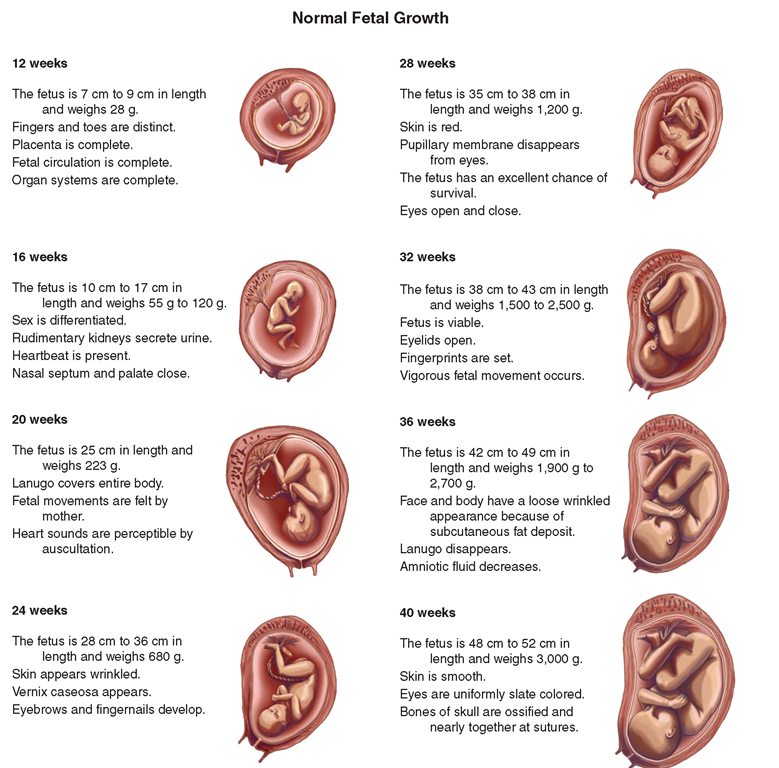 At risk are women who:
At risk are women who:
- suffer from chronic diseases;
- started early sexual activity;
- the presence of abortions, miscarriage, history of miscarriage;
- several sexual partners;
- abuse of alcohol, smoking and drugs.
Classification of placental insufficiency
There is a wide range of varieties of placental insufficiency, some of them are purely conditional.
Types of insufficiency by mechanism, formation time:
- Primary - manifests itself before the sixteenth week, has a close relationship with impaired placentation and implantation.
- Secondary - formed against the background of the formed placenta under the influence of exogenous factors after 16 weeks.
Clinical types of insufficiency:
- acute;
- chronic;
- compensated;
- decompensated.
Main signs of the disorder
Symptoms depend on the severity of the anomaly. As for the mother, the clinical picture may not always appear. Often, a woman develops preeclampsia, there is a threat of miscarriage and premature birth, pain in the groin and abdomen appears. In some cases, mucus appears with blood from the genital tract, conditionally pathogenic flora is activated, and colpitis occurs. Such complications can provoke infection of the fetus.
Impaired blood flow is more pronounced on the part of the baby. Many patients can independently suspect the symptoms of hypoxia. During the examination, the doctor is able to detect a rare or too frequent heartbeat of the baby, which signals placental insufficiency. Nutritional deficiencies can cause early placental abruption. This condition worsens the well-being of the mother and child, there is a threat to life.
Methods of diagnosis
Diagnosis begins with anamnesis, where it is possible to identify fetal, maternal and placental risk factors.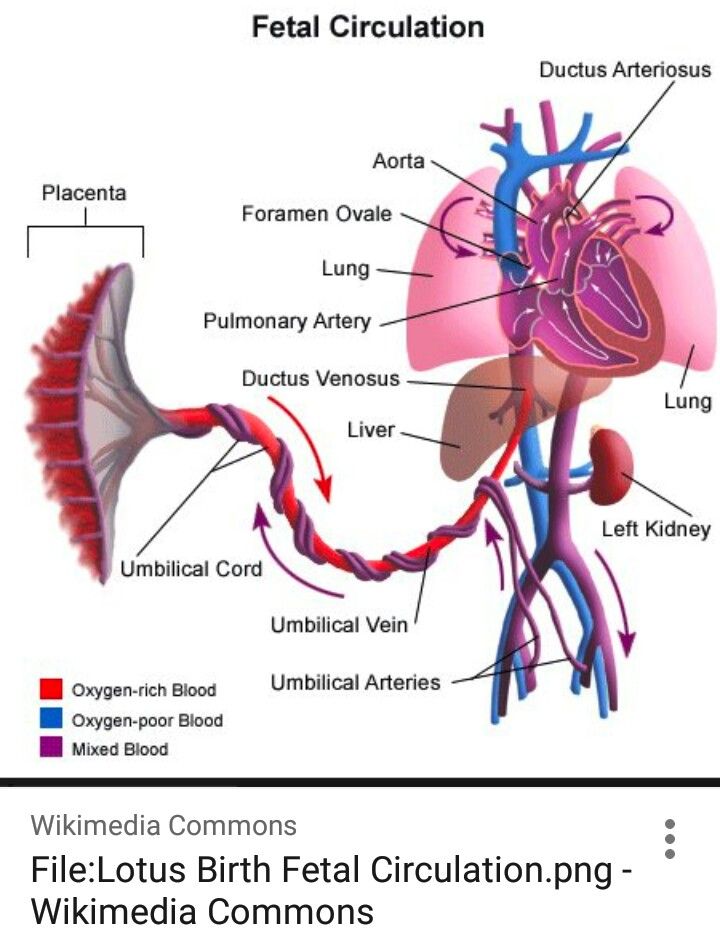 Closer attention should be paid to the presence of signs of abortion and preeclampsia.
Closer attention should be paid to the presence of signs of abortion and preeclampsia.
At physical examination it is worth considering:
- weight, height of the pregnant woman;
- uterine tone;
- number of fetal movements;
- presence of discharge with blood from the genital tract;
- abdominal circumference;
- the nature of the heartbeat.
Laboratory tests assess the hormonal function of the placenta:
- urinary excretion of estriol;
- detection of PL and oxytocinase in blood serum;
- determination of placental, total alkaline phosphatase in blood serum.
In addition to the above methods, diagnostics is carried out according to extragenital and obstetric diseases, against which placental insufficiency syndrome could form.
In the course of diagnostics, one cannot do without instrumental methods; KGT and ultrasound, Doppler and ultrasonic fetometry are actively used.