Painful uterus after birth
Relief of pain caused by uterine cramping or involution after giving birth
In this update, we include 28 studies (involving 2749 women). The evidence identified in this review comes from middle- to high-income countries. Generally the trials were at low risk of selection bias, performance bias and attrition bias, but some trials were at high risk of bias due to selective reporting and lack of blinding. Our GRADE certainty of evidence assessments ranged from moderate to very low certainty, with downgrading decisions based on study limitations, imprecision, and (for one comparison) indirectness.
Most studies reported our primary outcome of adequate pain relief as reported by the women. No studies reported data relating to neonatal adverse events, duration of hospital stay, or breastfeeding rates. Almost half of the included studies (11/28) excluded breastfeeding women from participating, making the evidence less generalisable to a broader group of women.
Non-steroidal anti-inflammatory drugs (NSAIDs) compared to placebo
NSAIDs are probably better than placebo for adequate pain relief as reported by the women (risk ratio (RR) 1. 66, 95% confidence interval (CI) 1.45 to 1.91; 11 studies, 946 women; moderate-certainty evidence). NSAIDs may reduce the need for additional pain relief compared to placebo (RR 0.15, 95% CI 0.07 to 0.33; 4 studies, 375 women; low-certainty evidence). There may be a similar risk of maternal adverse events (RR 1.05, 95% CI 0.78 to 1.41; 9 studies, 598 women; low-certainty evidence).
NSAIDs compared to opioids
NSAIDs are probably better than opioids for adequate pain relief as reported by the women (RR 1.33, 95% CI 1.13 to 1.57; 5 studies, 560 women; moderate-certainty evidence) and may reduce the risk of maternal adverse events (RR 0.62, 95% CI 0.43 to 0.89; 3 studies, 255 women; low-certainty evidence). NSAIDs may be better than opioids for the need for additional pain relief, but the wide CIs include the possibility that the two classes of drugs are similarly effective or that opioids are better (RR 0.37, 95% CI 0.12 to 1.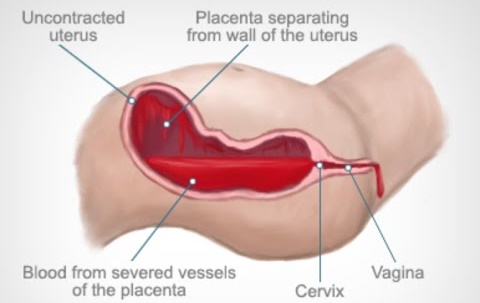 12; 2 studies, 232 women; low-certainty evidence).
12; 2 studies, 232 women; low-certainty evidence).
Opioids compared to placebo
Opioids may be better than placebo for adequate pain relief as reported by the women (RR 1.26, 95% CI 0.99 to 1.61; 5 studies, 299 women; low-certainty evidence). Opioids may reduce the need for additional pain relief compared to placebo (RR 0.48, 95% CI 0.28 to 0.82; 3 studies, 273 women; low-certainty evidence). Opioids may increase the risk of maternal adverse events compared with placebo, although the certainty of evidence is low (RR 1.59, 95% CI 0.99 to 2.55; 3 studies, 188 women; low-certainty evidence).
Paracetamol compared to placebo
Very low-certainty evidence means we are uncertain if paracetamol is better than placebo for adequate pain relief as reported by the women, the need for additional pain relief, or risk of maternal adverse events (2 studies, 123 women).
Paracetamol compared to NSAIDs
Very low-certainty evidence means we are uncertain if there are any differences between paracetamol and NSAIDs for adequate pain relief as reported by the women, or the risk of maternal adverse events.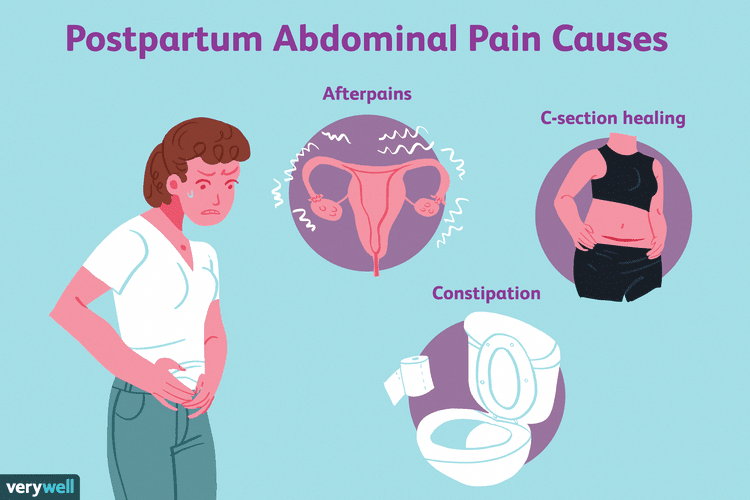 No data were reported about the need for additional pain relief comparing paracetamol and NSAIDs (2 studies, 112 women).
No data were reported about the need for additional pain relief comparing paracetamol and NSAIDs (2 studies, 112 women).
NSAIDs compared to herbal analgesia
We are uncertain if there are any differences between NSAIDs and herbal analgesia for adequate pain relief as reported by the women, the need for additional pain relief, or risk of maternal adverse events, because the certainty of evidence is very low (4 studies, 394 women).
Transcutaneous nerve stimulation (TENS) compared to no TENS
Very low-certainty evidence means we are uncertain if TENS is better than no TENS for adequate pain relief as reported by the women. No other data were reported comparing TENS with no TENS (1 study, 32 women).
Causes and How to Get Relief
Buckle up for another wild ride — here comes the postpartum stage.
As if being pregnant for 9 long months and giving birth wasn’t enough, you may experience a host of aches and pains after delivery that you didn’t quite expect.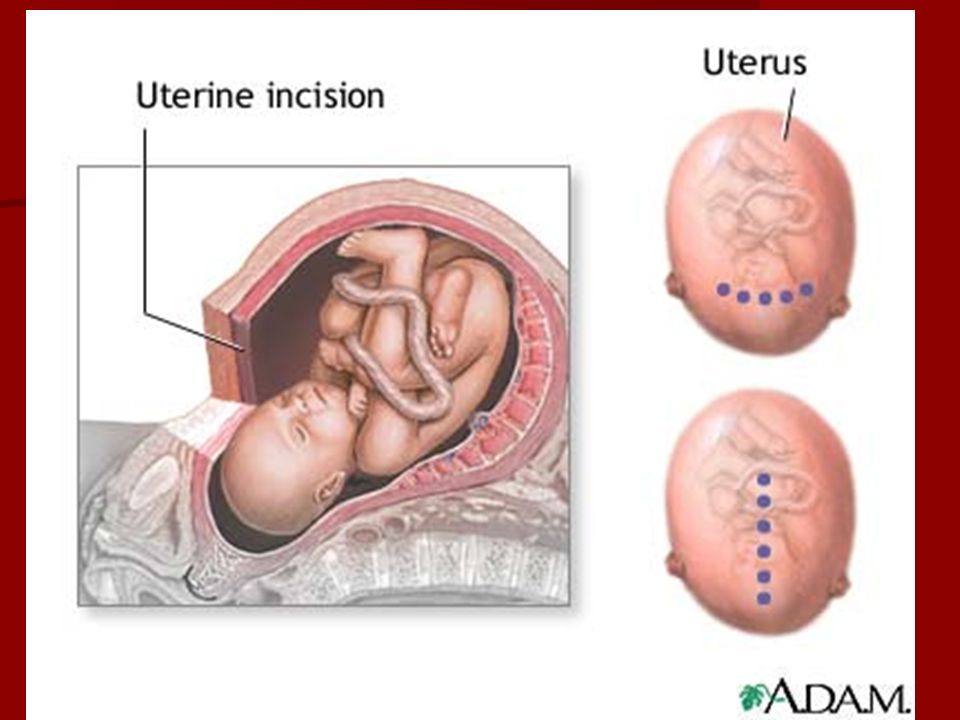 Even if you’re a seasoned parent, there are different situations and sensations you’ll have with each baby.
Even if you’re a seasoned parent, there are different situations and sensations you’ll have with each baby.
Cramping is definitely a thing in the days and weeks after delivery. Often it has to do with your uterus returning to its normal state of being. Other times, though, it may be a reason for concern.
Here’s what you need to know about postpartum cramping, what causes it, and when you should contact your doctor.
Again, it’s normal to experience cramping in your lower abdomen after you give birth. After all, your uterus grows to many times its original size throughout pregnancy — all while its lining thickens and its blood vessels enlarge to support the placenta and your baby.
When your baby is born, your body begins the process of getting back to its starting point.
Afterpains
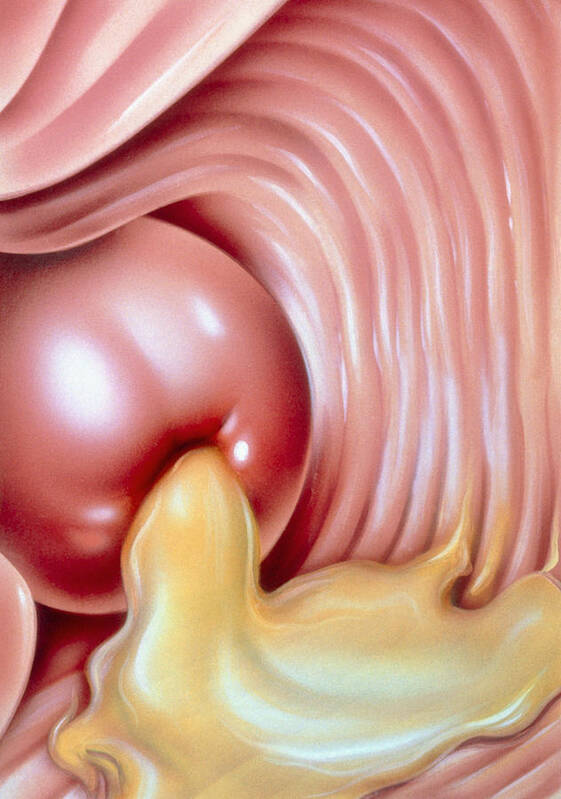
The most common reason you have cramping after your baby is born is that your uterus contracts to shrink back down to its original size. While it contracts, your body is also working to compress blood vessels in the uterus to prevent too much bleeding.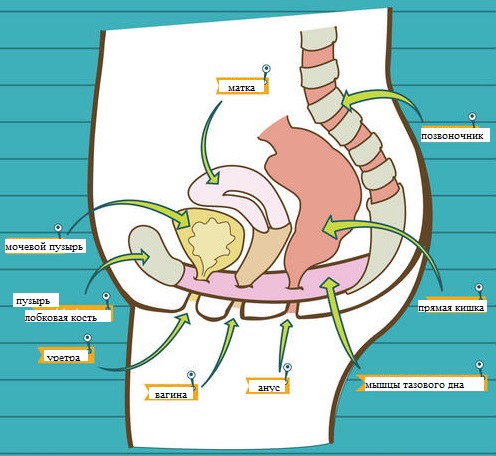
The contractions are like mini versions of labor contractions and they’re sometimes called “afterpains” because, well, you get these pains after you deliver your little one.
The cramps may feel a lot like menstrual cramps — from mild to possibly severe at times — and they tend to be more noticeable with second or third pregnancies.
Afterpains are generally most uncomfortable in the first few days after delivery. They tend to fade away after that, but you may find they’re more noticeable when you’re breastfeeding.
Cesarean delivery
Afterpains don’t only affect people who give birth vaginally. Your uterus also contracts this way after you have a C-section. So, the same rules apply to the uterus and its need to return to its pre-pregnancy size.
That said, it’s important to note that you may have additional discomfort in your lower abdomen after a cesarean delivery. After all, it’s major surgery! You may feel cramping and soreness as your incision and the surrounding tissues heal.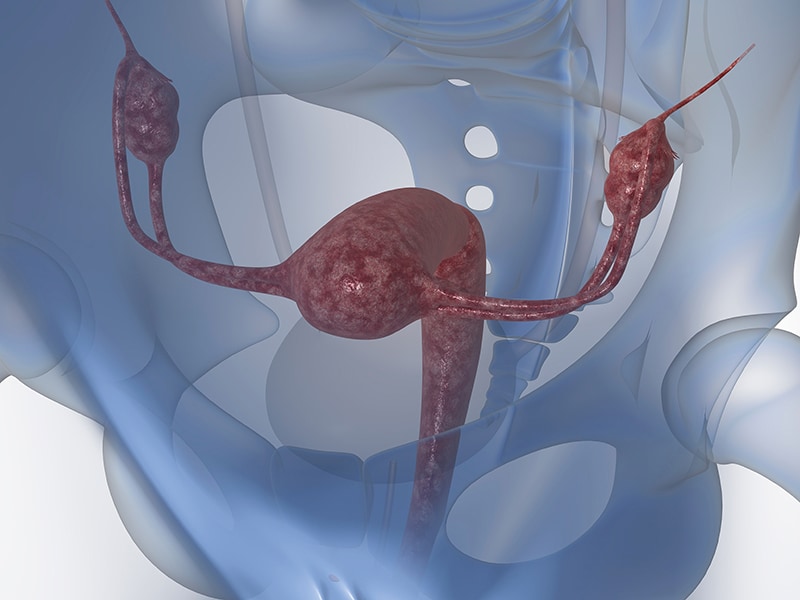
Constipation
That’s right — constipation. The thing nobody really talks about is pooping after delivery, but we went there.
You’ll likely have your first postpartum bowel movement within a few days of delivery. But you can also develop constipation, which may be caused by high progesterone levels in pregnancy, your diet (for example, low fiber intake), and lowered activity levels.
Constipation comes with cramping — and you may also just feel backed up or have some bloating and pressure.
This condition may be particularly likely if you’ve had a cesarean delivery. Why is this? Well, you may be spending some extra time in bed recovering after surgery. And certain pain medications may also slow down your digestive system and back you up, leading to cramping.
Infections and more
While less common, it’s possible to develop infections after giving birth. Some types of infections are more likely to develop than others. And it’s also important to note that you might feel pain and cramping that aren’t related to giving birth at all.
Possibilities include things like:
- Endometritis is inflammation of the uterine lining caused by infection. Other symptoms include fever, constipation, unusual vaginal discharge, and pelvic pain.
- Bacterial vaginosis is an infection caused by too much bad bacteria in the uterus. Other symptoms include a burning sensation when urinating, foul-smelling discharge, and itching/pain in the vulva.
- Urinary tract infection (UTI) impacts the ureters, bladder, urethra, and kidneys. Other symptoms include fever, painful or frequent urination, urgency to urinate, cloudy/bloody urine, and pelvic pain.
- Appendicitis is inflammation of the appendix. While completely unrelated to childbirth, researchers note that it’s possible to experience appendicitis (and other conditions) in the postpartum period, but that with everything else going on, diagnosis may be delayed. Other symptoms include low-grade fever, nausea/vomiting, abdominal pain that gets worse with movement, and diarrhea/constipation.
Afterpains may begin immediately after you give birth to your baby. They tend to peak in their intensity on days 2 and 3 after birth. Then they continue for the first week to 10 days after delivery, or until your uterus returns to its pre-pregnancy size.
Cesarean section discomfort is also more likely in the first few days after delivery. However, you’ll still likely experience general afterpains, which follow the timeline above.
Cramping that’s caused by other conditions, like constipation or infection, will last for different amounts of time. And without treatment, the cramping may continue until you address the underlying cause.
So, if you’re in pain — don’t delay. Get checked out so you can feel better ASAP.
Your uterus does need to go through the work of contracting and shrinking after the birth of your baby. There’s no treatment that will stop it — nor would you want to stop it — but you can treat the cramping and pain you experience to make it a bit more comfortable.
- Pain medication. Over-the-counter (OTC) medications, like ibuprofen, can take the edge off. For particularly painful cramping, your doctor may also give you a prescription for a short course of pain meds that are a bit stronger.
- Movement. It may sound unappealing, but getting up and gently walking around as soon as you’re able may ease your afterpains. Bonus: Moving your body is also good for constipation.
- Relaxation. Try some deep breathing exercises when you get the pains. This may help you move through them and stay calm.
- Heat. Heating pads or hot water bottles may also provide some relief and are easy to find at big box stores and pharmacies. (Or you can make your own.)
- Other suggestions. Keep your bladder empty; if you’re breastfeeding, try to do so frequently; and remember that this, too, shall pass.
If you’re constipated, consider taking OTC stool softeners or laxatives to get things moving.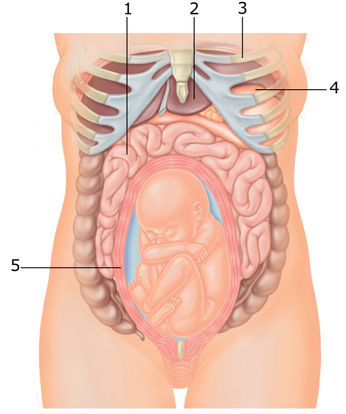 Your doctor or pharmacist can point you to specific ones that are OK to take while breastfeeding.
Your doctor or pharmacist can point you to specific ones that are OK to take while breastfeeding.
Lifestyle changes that may help include:
- engaging in light exercise (keyword light — like walking)
- eating a high fiber diet with lots of fresh fruits and vegetables
- drinking more water
How much more water do you need? Experts recommend that you drink 13 cups of fluids a day if you’re breastfeeding.
For infections, you’ll need to see a doctor and get a prescription for appropriate medications. Your doctor may also be able to suggest at-home methods to ease your discomfort, like taking OTC pain medications.
While cramping can be common, severe pain and other symptoms aren’t — and may be a sign of infection. Be sure to check in with your doctor if you experience any of the following warning signs.
- Fever. If you feel unwell, try taking your temperature. Any reading that’s 100.4°F (38°C) or higher may indicate an infection.

- Discharge. You’ll experience varying degrees of bleeding and discharge after delivery. But if the discharge is a strange color or smells foul, you may have an infection like endometritis or bacterial vaginosis.
- Bleeding. With cramping, you may experience increased bleeding and discharge. Bleeding is considered heavy if it soaks through more than one pad every 1 to 2 hours.
- Painful urination. Frequent or painful urination may be signs of a UTI or other infection. Without treatment, UTIs can lead to kidney infections or sepsis.
- Severe abdominal pain. While cramping can be strong at times, it shouldn’t last more than a few days or persist when you aren’t breastfeeding. If you’re in tremendous pain, you may have an infection.
- Redness around your incision. If you have pain, redness, discharge, or warmth around your incision after a C-section, the area may be infected.
The American College of Obstetricians and Gynecologists shares that you should reach out to your healthcare provider within the first 3 weeks of giving birth. That way, you can explain anything that you think might be off with your recovery.
From there, you should also schedule a full postpartum appointment no later than 12 weeks after your baby is born.
And remember: It’s also possible to have cramping or pain in your abdomen that’s caused by something not related to your pregnancy or delivery. When in doubt, get checked out.
There’s a lot going on in those early weeks after you have your baby — but self-care is super important.
Between all the diaper changes, feedings, and sleepless nights, try your best to find moments of peace and quiet for yourself as well. Tune in with your body and make note of anything that doesn’t feel quite right.
For most people, uterine cramping should subside within a week or so of delivery. If it continues or you have other concerns, don’t hesitate to contact your doctor.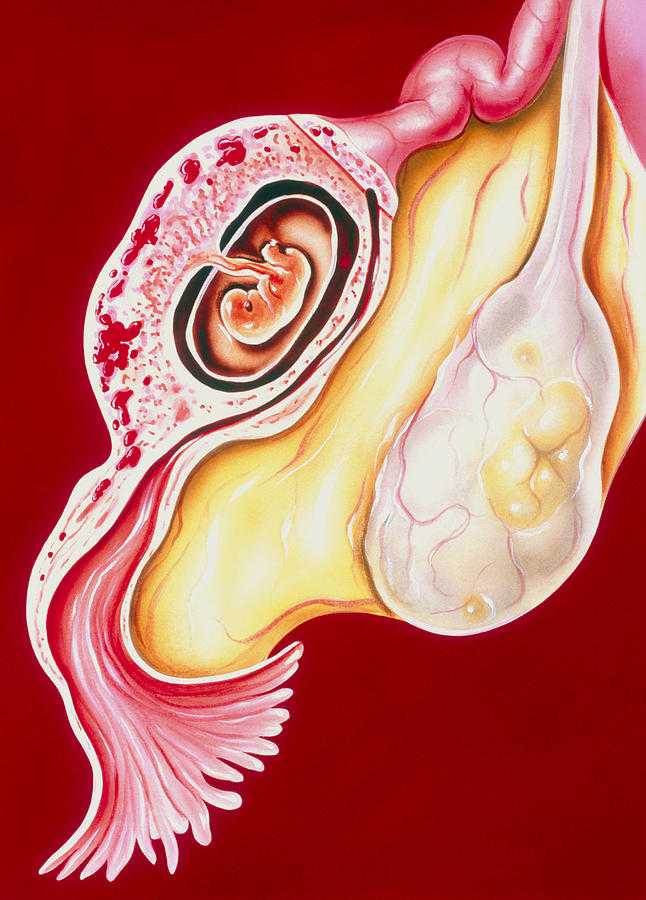
Recovery after childbirth
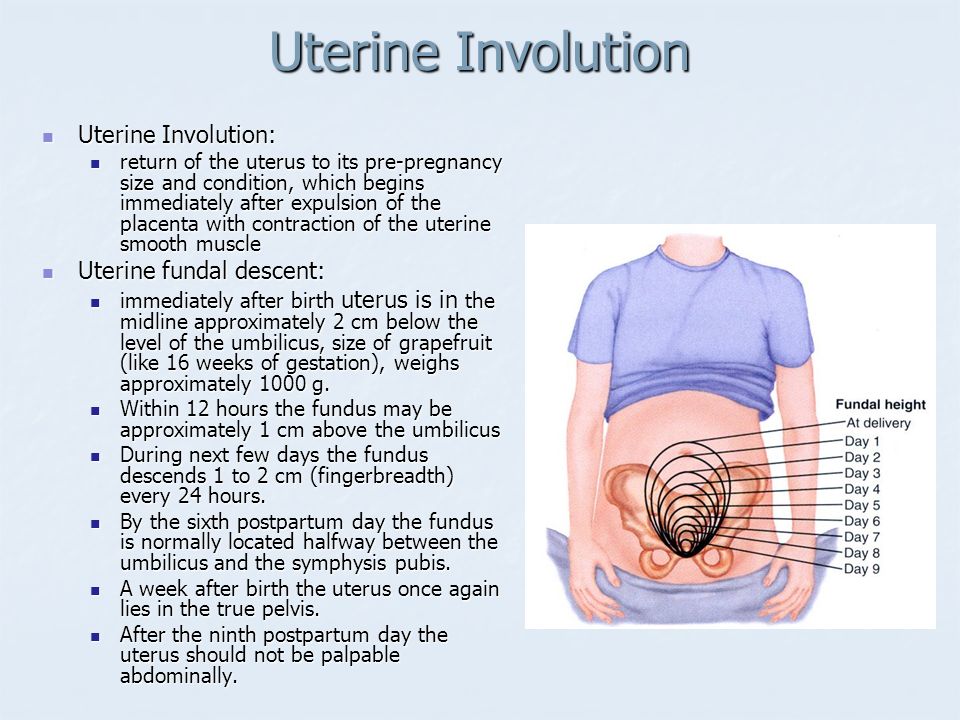
In most cases, the recovery of normal health is not rapid. The first sensation of incredible relief has passed, and now you notice that the stomach is still large, and even a little sore. To take its former size, the uterus must still be contracted for a long time and diligently. Its weight decreases from 1 kg to 50 g within 6-8 weeks.
Since the contraction of the uterus occurs due to the work of the muscles, this is accompanied by pain sensations of varying intensity, reminiscent of light contractions. You may notice an increase in pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which contributes to uterine contractions.
For better uterine contraction, it is recommended to lie on your stomach after childbirth. If you feel good, try to move more and do gymnastics.
Another disturbing circumstance is pain in the perineum, which appears even if there were no tears and the doctor did not make an incision. This is due to the fact that the tissues have undergone a strong stretch during childbirth. Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks.
This is due to the fact that the tissues have undergone a strong stretch during childbirth. Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks.
Haemorrhoids often appear after childbirth. Careful hygiene and daily evening showers help reduce pain. Do not forget about the diet, include in your diet foods rich in fiber and with a slight laxative effect: seaweed, beets, baked apples, cauliflower, germinated cereals. Medications are usually not used because the inflammation usually goes away with time. If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures.
Constipation that occurred during pregnancy may also remind of itself in the postpartum period. They are, in particular, caused by the fear of damaging the seams in the perineum. However, such fear is unfounded. In addition, during a bowel movement, you can hold the area where the stitches are applied with a napkin, which will reduce the stretching of the tissues, and the bowel movement will be less painful. The chair usually does not happen immediately after childbirth, but after 2-3 days. To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle.
After childbirth, especially strong discharge from the uterus is observed on the first day, then it decreases. After 3 days, the discharge becomes muco-bloody. By the 5-6th week after birth, the discharge from the uterus stops altogether. During this period, hygiene must be carefully observed, because an infection that has entered the uterus can lead to endometritis (an inflammatory process of the uterine mucosa).
For 9 months, all the organs of the female body worked to ensure the child's proper development and good health. Now he was born and became quite "independent". However, the functions of a woman-mother did not end there. The main one - to provide the baby with food - is taken over by the mammary glands. In the body of a woman, hormonal changes continue, due to which significant changes occur in the mammary glands, and they begin to produce milk. In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended.
However, women often face the opposite problem - an excess amount of milk and difficulty in its outflow. This, in turn, leads to its stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the chest area. It may even increase body temperature. How to prevent such occurrences?
It may even increase body temperature. How to prevent such occurrences?
First of all, try to breastfeed your baby regularly, and in the first 3-4 days after birth, limit fluid intake to 800 ml per day. Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks is fraught with the development of mastopathy. Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation.
To prevent cracks in the nipples, it is necessary to apply the baby to each breast in turn in the first 2-3 days after childbirth. First, give the baby one for 5-7 minutes, then another for 5-7 minutes. To prevent cracks, there is a special cream that needs to be used between feedings, and before them, carefully wash off its remnants.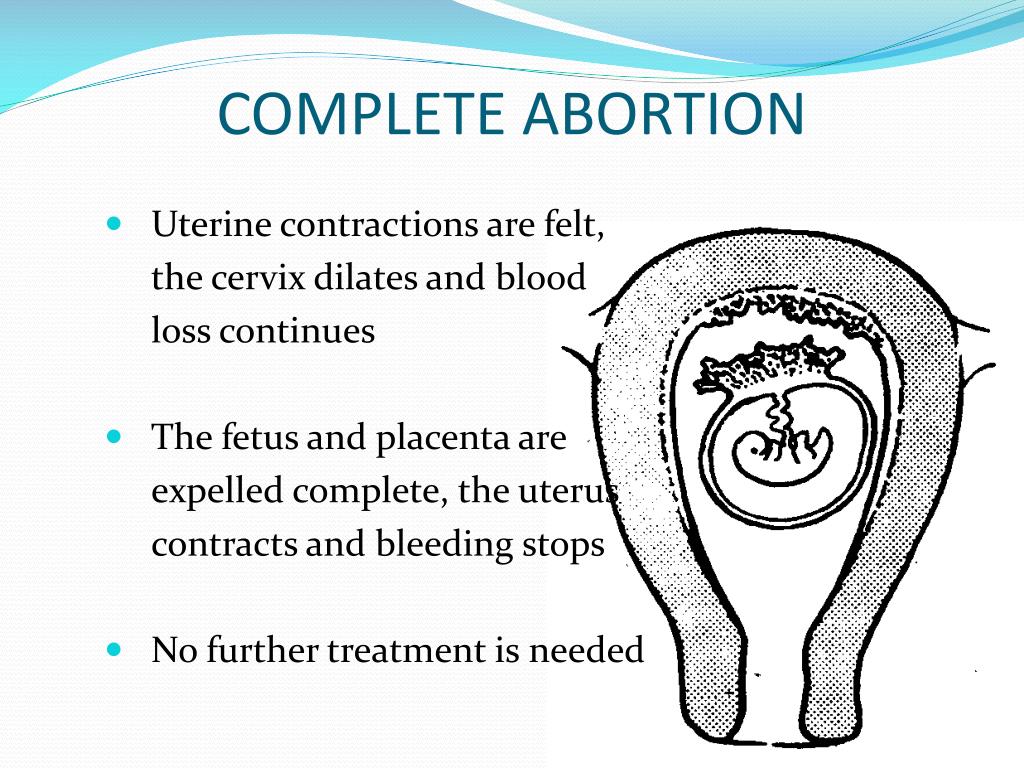
That's all the troubles that are easily forgotten and seem not so significant against the background of new worries. Now your attention will be constantly occupied by the baby. However, it is very important not to forget about yourself, maintain your health and restore your former beauty. Not everyone succeeds, which contributes to the development of postpartum depression.
Lochiometer
After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied. In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - a postpartum wound secret, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
The first 2-3 days after birth, lochia have a bloody character, then, from the 4th-5th day, they acquire a dark red and brownish hue, and after a week they become yellowish-white due to the high content of leukocytes.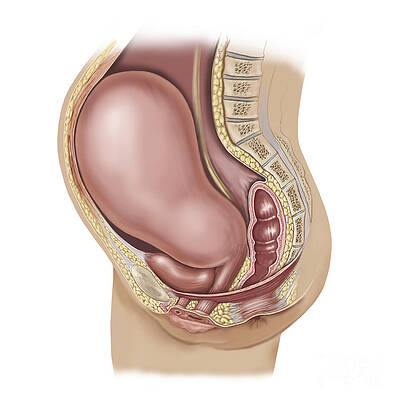 From the 10th day, the discharge becomes light, watery, serous-mucous consistency. Gradually, the number of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely.
From the 10th day, the discharge becomes light, watery, serous-mucous consistency. Gradually, the number of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely.
With a delay in the outflow of postpartum secretions, they speak of a lochiometer - stagnation of lochia in the uterine cavity. The danger of developing lochiometers lies in the high probability of infection of the contents of the uterus, since lymph, serum, blood, and tissue remnants serve as the best nutrient medium for the reproduction of microbial flora. Most often, against the background of lochiometers, endometritis develops.
Causes of the development of lochiometers
The development of lochiometers is due to mechanical obstacles to the outflow of secretions in the cervical canal or insufficient uterine contractility.
Mechanical obstruction may be due to kinking (hyperanteflexia) of the uterus or obstruction of the cervical canal by blood clots, remnants of the decidua, and flaking uterine tissue.
Insufficient contractile activity of the uterus in the postpartum period usually develops as a result of overstretching of the uterus (with a large fetus, polyhydramnios or multiple pregnancy), weak or discoordinated labor, spasm of the internal os, caesarean section.
The development of lochiometers is facilitated by prolonged bed rest and low activity after childbirth.
Symptoms of lochiometer
Lochiometer develops 5-7 days after birth, characterized by a marked decrease or cessation of postpartum discharge from the uterus. At the same time, there is an increase in the size of the uterus compared to the norm for the current postpartum day, its soreness on palpation. The general health and objective condition of a woman with a lochiometer does not suffer, body temperature is normal, tachycardia is absent.
When delaying timely therapeutic tactics in relation to lochiometers, fever appears (body temperature 38-40 ° C), chills, cramping pains, turbid discharge with an unpleasant odor, tachycardia. After 1-2 days, the temperature drops critically with the simultaneous appearance of liquid purulent lochial discharge.
Diagnosis lochiometers
Lochiometers are diagnosed by characteristic clinical signs. With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a densely elastic consistency, often - the closure of the internal pharynx, the bend of the uterus.
Clarifying lochiometer diagnostics includes ultrasound. during which the expansion of the uterine cavity is revealed, the presence of hyperechoic blood clots and liquid blood in it.
Treatment of lochiometers
Treatment of lochiometers consists in ensuring the free outflow of lochia, taking into account the cause that caused this condition.
When lochiometers are detected, the gynecologist prescribes injections of antispasmodics (papaverine, no-shpy) to relieve spasm of the uterine os. In the treatment of lochiometers, uterotonic (contracting the uterus) agents are used - oxytocin, methylergometrine.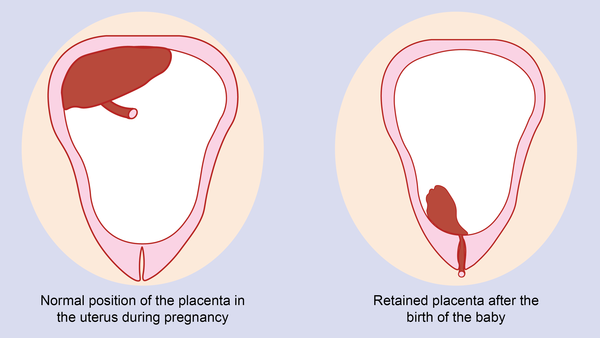 For a free outflow of secretions, the puerperal is recommended to lie on her stomach 2-3 times a day for 1-2 hours.
For a free outflow of secretions, the puerperal is recommended to lie on her stomach 2-3 times a day for 1-2 hours.
In case of hyperanteflexion of the uterus, the bend is eliminated during the bimanual examination; exercise therapy is prescribed. In the case of a lochiometer due to blockage of the cervical canal by clots, when viewed on a chair, digital dilatation of the cervical canal and careful removal of clots are performed.
Situations when the lochiometer is not allowed within 2-3 days are considered by clinical gynecology as an indication for instrumental removal of the contents of the uterus with a curette or vacuum apparatus under hysteroscopy control. For the prevention and treatment of postpartum infections against the background of lochiometers, antibiotics are prescribed, taking into account the results of a bacteriological smear.
Complications of lochiometers
If, after the elimination of lochiometers, uterine tenderness, its poor contraction, hyperthermia persist, one should think about the development of postpartum metroendometritis.
If the infection progresses, the condition of the puerperal may worsen due to the development of purulent-resorptive fever, manifested by intoxication, abdominal pain, purulent discharge with a putrid odor. Against this background, the transition of lochiometers to pyometra is noted.
Prevention and prognosis with lochiometer
To prevent the development of lochiometers, competent management of pregnancy and preparation of the woman for childbirth are required, as well as careful monitoring of the puerperal during the postpartum period: regular monitoring of uterine contractions (daily palpation determination of its sensitivity, consistency, fundus height), volume and nature of discharge .
In the postpartum period, a woman needs to monitor the timeliness of emptying the bladder and intestines, breastfeed the newborn on demand, perform postpartum exercises, and lie on her stomach.
After discharge from the maternity hospital, a young mother should also monitor her well-being and discharge from the genital tract.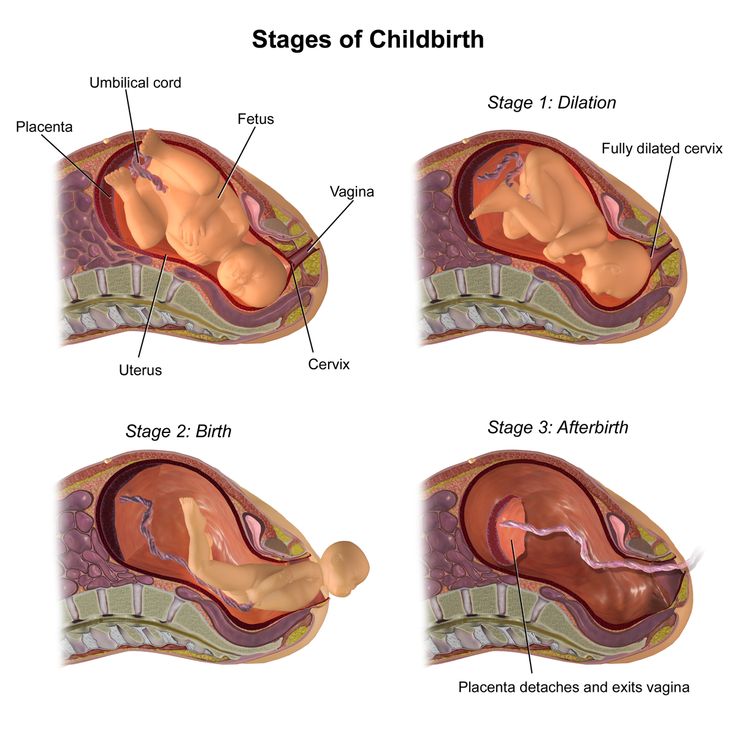 In the event of an increase in temperature, a delay in lochia, a change in their nature or smell, an immediate appeal to a gynecologist is necessary.
In the event of an increase in temperature, a delay in lochia, a change in their nature or smell, an immediate appeal to a gynecologist is necessary.
The prognosis for timely detection and elimination of lochiometers is favorable.
Complications after childbirth - causes and consequences
- Increased discharge
- Retention of part of the placenta in the uterine cavity
- Changes in the blood coagulation system
- Disorder of uterine muscle contraction
- Inflammatory process in the vagina or uterus
- Vaginal candidiasis (thrush)
- Postpartum endometritis
- Laktostasis and mastitis
- Postpartum pyelonephritis
- Venous thrombosis
- Discomfort in the area of postoperative sutures
- Urinary incontinence, feces, uterine prolapse
- Hemorrhoids
After giving birth, a woman often thinks that all worries and anxieties are behind her. But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
Labor ends after the third stage of labor, that is, after the birth of the placenta. Following this, the uterus immediately significantly decreases in size, becomes spherical, its cavity is filled with blood clots; the bottom of the uterus at this moment is located approximately in the middle between the womb and the navel. The early postpartum period lasts for 2 hours and during this time the woman is in the maternity ward. Then comes the late postpartum period. This period lasts 6-8 weeks. During this time, there is a reverse development (involution) of all organs and systems that have undergone changes due to pregnancy and childbirth. The exception is the mammary glands, whose function reaches its peak precisely in the postpartum period. The most pronounced involutional changes occur in the genital organs, especially in the uterus.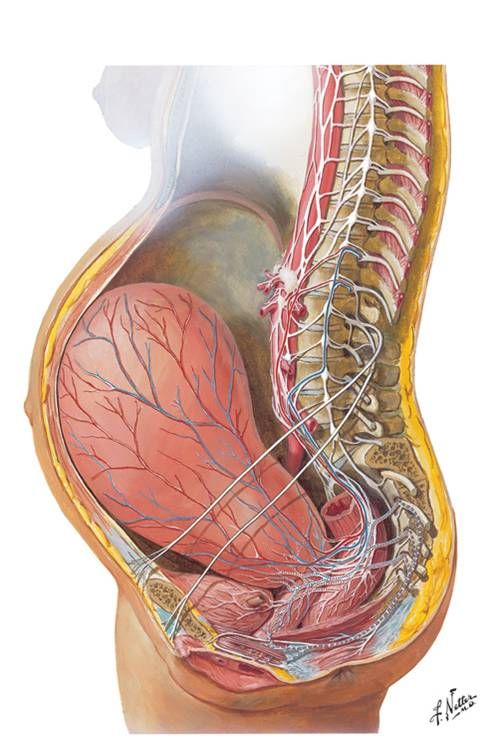 The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
What complications can occur after childbirth
You should consult a gynecologist in the following cases:
Increased amount of discharge
discharge does not stop for a long time, large blood clots appeared. When bleeding occurs, you need to contact an obstetrician-gynecologist, preferably at the maternity hospital where the birth took place.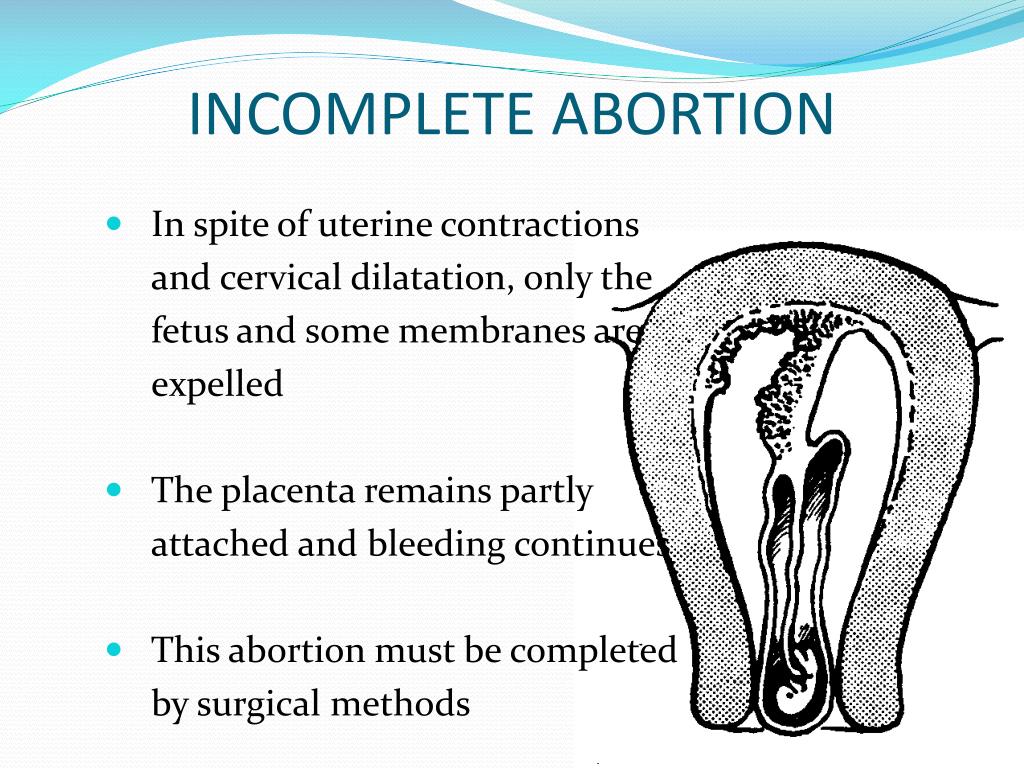 If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
Retention of part of the placenta in the uterine cavity
The most common cause of late postpartum hemorrhage (that is, those that occur later than 2 hours after birth) is the retention of a part of the placenta in the uterine cavity. The diagnosis in this case is confirmed by ultrasound. To remove the remnants of the placenta, the walls of the uterus are scraped under general intravenous anesthesia with mandatory subsequent antibiotic therapy to prevent infectious complications.
Changes in the blood coagulation system
In rare cases, the causes of bleeding may be changes in the blood coagulation system of a hereditary or acquired nature, blood diseases. In these cases, complex drug therapy is required.
Violation of contraction of the muscles of the uterus
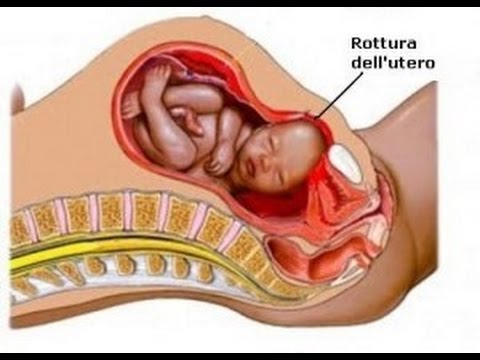
Possible development of bleeding associated with impaired contraction of the muscles of the uterus.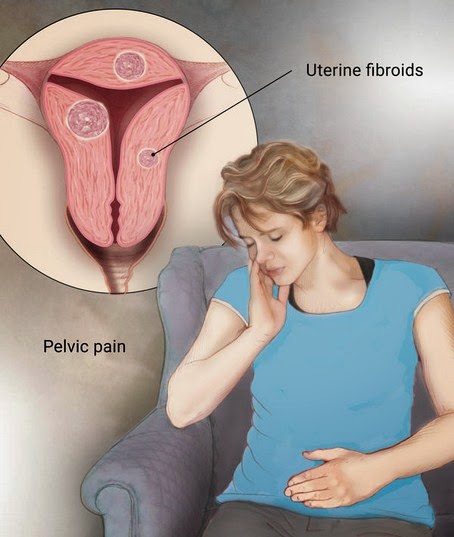 This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
A sharp, unexpected cessation of spotting should also alert the woman and requires urgent medical attention. In this case, the outflow of blood from the uterus may be disturbed, that is, lochia accumulate in the cavity and the so-called lochiometer develops. Blood clots are a good breeding ground for bacteria, so if the lochiometer is not treated in time, bacteria enter the uterine cavity and endometritis develops - inflammation of the uterine mucosa.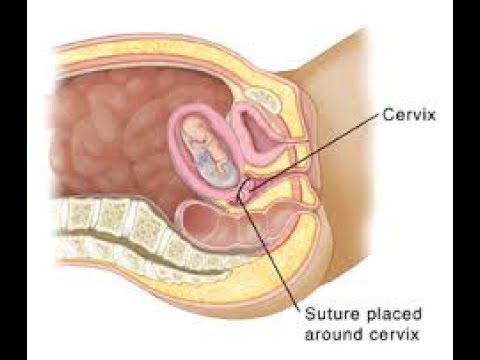 After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
Inflammatory process in the vagina or uterus
The discharge has acquired an unpleasant odor. This may indicate the development of an inflammatory process in the vagina or in the uterus. In the postpartum period, there was a significant increase in the composition of most groups of bacteria, including bacteroids, Escherichia coli, streptococci, staphylococci. Potentially, all of these species can be the cause of postpartum infectious diseases. A common problem for women after childbirth is the development of bacterial vaginosis. Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Vaginal candidiasis (thrush)
The appearance of curdled discharge, itching, burning in the genital area, redness indicates the development of vaginal candidiasis (thrush). The risk of this complication increases with antibiotics. Diagnosis is based on the detection of a large number of yeast-like fungi in a smear on the flora. For treatment, local preparations are used in the form of vaginal suppositories or tablets.
Postpartum endometritis
Purulent discharge, lower abdominal pain, fever. These symptoms may indicate the development of a serious complication - postpartum endometritis (inflammation of the inner lining of the uterus).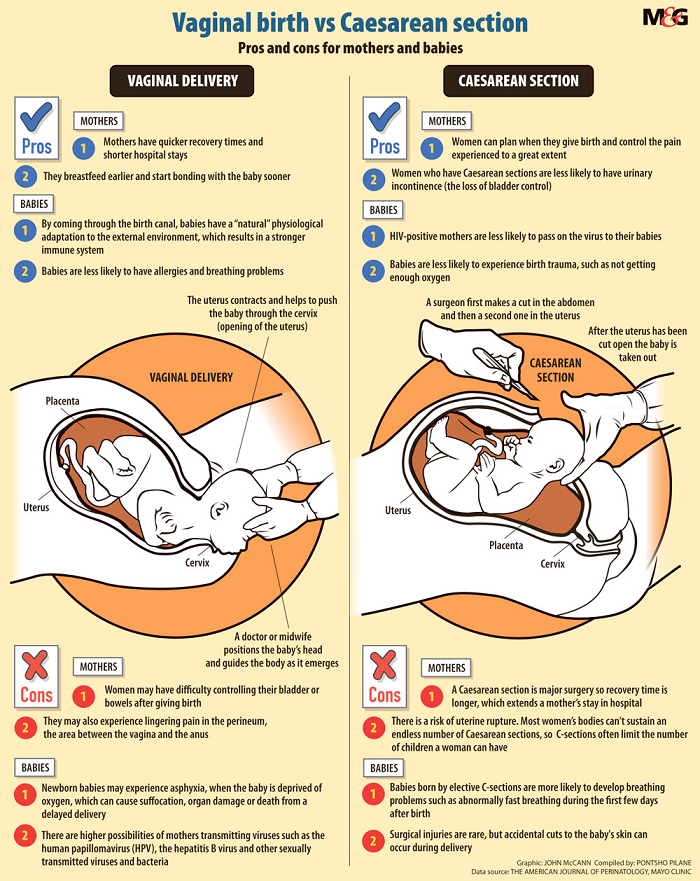 Most often, endometritis occurs in patients after cesarean section, manual examination of the postpartum uterus, manual separation of the placenta and removal of the placenta (if independent separation of the placenta is difficult due to a violation of the contractile function of the uterus), with a long anhydrous interval (more than 12 hours from the moment of amniotic fluid outflow to the birth of a baby), in women admitted to childbirth with inflammatory diseases of the genital tract (for example, against the background of sexually transmitted infections), in patients with a large number of abortions in the past. The classic form of endometritis occurs on days 1-5. Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill.
Most often, endometritis occurs in patients after cesarean section, manual examination of the postpartum uterus, manual separation of the placenta and removal of the placenta (if independent separation of the placenta is difficult due to a violation of the contractile function of the uterus), with a long anhydrous interval (more than 12 hours from the moment of amniotic fluid outflow to the birth of a baby), in women admitted to childbirth with inflammatory diseases of the genital tract (for example, against the background of sexually transmitted infections), in patients with a large number of abortions in the past. The classic form of endometritis occurs on days 1-5. Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill.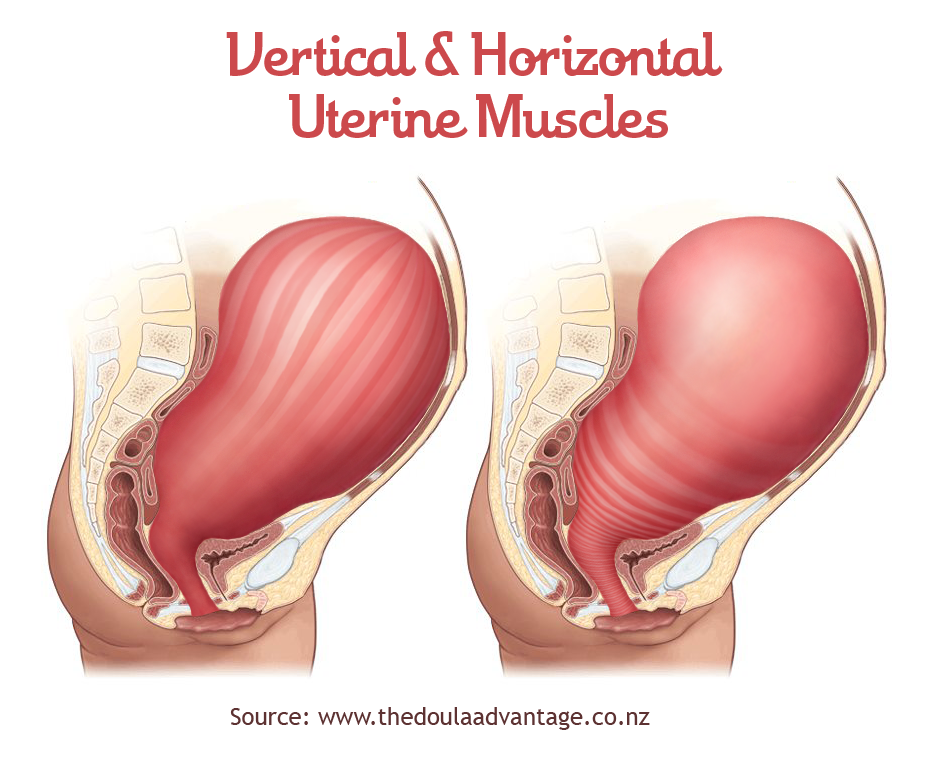 Endometritis after caesarean section always proceeds in a severe form.
Endometritis after caesarean section always proceeds in a severe form.
An ultrasound examination of the uterus and a complete blood count, which reveal signs of inflammation, help the doctor make a diagnosis. Treatment of endometritis should be started as early as possible. It is carried out in a hospital. Assign bed rest, with acute endometritis cold on the lower abdomen. Postpartum endomeritis is necessarily treated with antibiotics, along with them, agents that reduce the uterus are used. Currently, in many clinics and maternity hospitals, the uterine cavity is washed with cooled solutions of antiseptics. In severe cases, an intravenous infusion of saline solutions is required to improve blood circulation, relieve symptoms of intoxication.
In case of untimely treatment, there is a very high risk of spreading the inflammatory process to the entire uterus, small pelvis, the development of sepsis (the appearance of infectious agents in the blood), up to the death of the patient.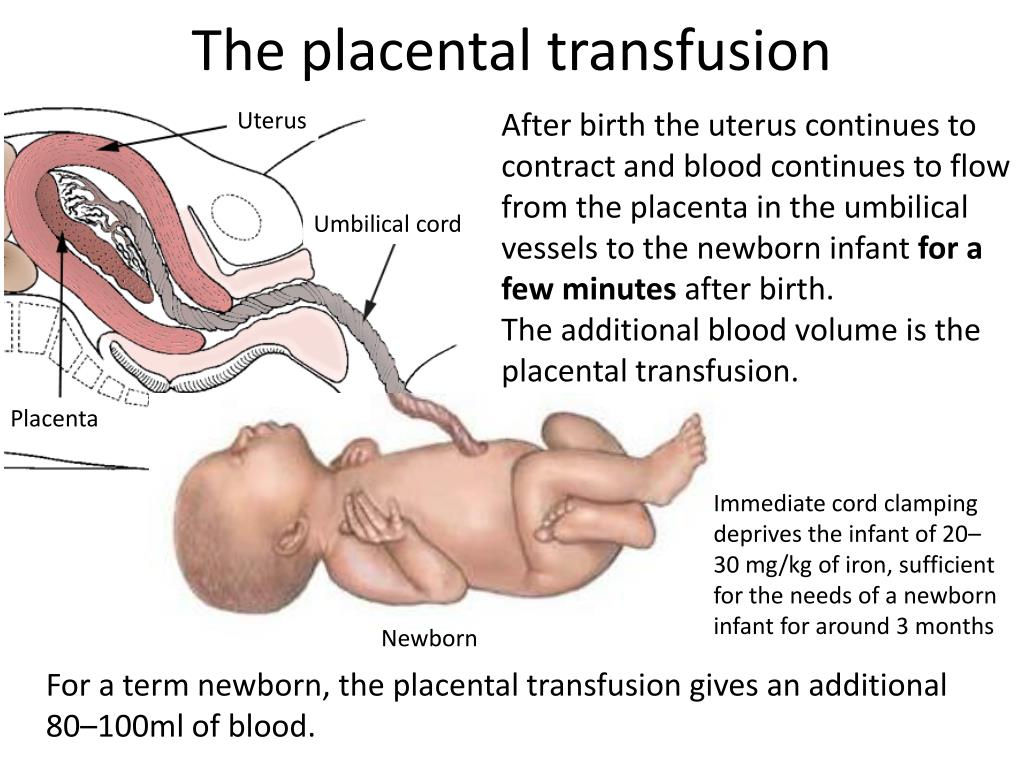
Laktostasis and mastitis
In the postpartum period, there may be pain in the mammary glands, a feeling of fullness, an increase in body temperature. When these symptoms appear, you should definitely consult a doctor - an obstetrician-gynecologist in a antenatal clinic or a surgeon.
Possible causes of pain in the mammary glands and the accompanying fever are lactostasis and mastitis.
Laktostasis (stagnation of milk in the gland), due to blockage of the excretory ducts. Most often, this condition develops when the baby is not properly attached to the chest, violation of the feeding regimen. Laktostasis often affects primiparous women. With the stagnation of milk, the mammary gland increases in volume, its dense enlarged lobules are determined. Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin. Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin. Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
To eliminate lactostasis, pumping, local anti-inflammatory ointments, and physiotherapy are used. Mastitis is treated with antibiotics. In some cases, lactation suppression and surgical treatment are required.
Mastitis is treated with antibiotics. In some cases, lactation suppression and surgical treatment are required.
Postpartum pyelonephritis
Fever, pain in the back or side, painful urination. These symptoms may indicate the development of postpartum pyelonephritis, that is, inflammation of the kidneys. Critical periods for the development of postpartum pyelonephritis, doctors consider 4-6 and 12-14 days of the postpartum period. The development of the disease is associated with infection in the urinary tract from the genital tract. Most often, the disease develops in puerperas, in the urine of which a small amount of bacteria was found during pregnancy. An ultrasound examination of the kidneys and bladder and a urine test help the doctor make the diagnosis.
Treatment of pyelonephritis is mandatory with antibiotics.
Venous thrombosis
Pain in the legs, swelling, redness on the legs along the vein, increased pain when walking - these are symptoms of a serious pathology - venous thrombosis (formation of blood clots in the veins) and require an urgent visit to a surgeon or phlebologist. The most dangerous periods for the occurrence of thrombosis are considered 5-6 days after childbirth or cesarean section, less often thrombosis occurs 2-3 weeks after childbirth. The causes of thrombosis are changes in the blood coagulation system that occur during pregnancy and after childbirth. Physiologically, in the postpartum period, the activation of the coagulation system occurs. As the body tries to stop bleeding. At the same time, the tone of the vessels of the small pelvis and lower extremities is reduced, the veins have not yet had time to adapt to work in new conditions. These conditions trigger the mechanisms of thrombus formation. An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
The most dangerous periods for the occurrence of thrombosis are considered 5-6 days after childbirth or cesarean section, less often thrombosis occurs 2-3 weeks after childbirth. The causes of thrombosis are changes in the blood coagulation system that occur during pregnancy and after childbirth. Physiologically, in the postpartum period, the activation of the coagulation system occurs. As the body tries to stop bleeding. At the same time, the tone of the vessels of the small pelvis and lower extremities is reduced, the veins have not yet had time to adapt to work in new conditions. These conditions trigger the mechanisms of thrombus formation. An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
The risk of developing venous thrombosis is especially high in women with various pathologies of the blood coagulation system, which are detected even before pregnancy or during childbearing.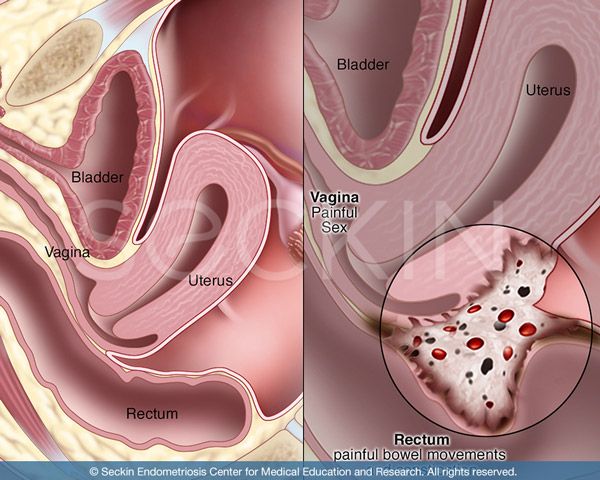 There is a high probability of thromboembolic complications and in the presence of diseases of the cardiovascular system, overweight. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of varicose veins of the lower extremities. The risk of thrombus formation is increased in women who have undergone a caesarean section. An ultrasound examination of the veins, with Dopplerography, that is, an assessment of blood flow in the vessels, helps the doctor in making a diagnosis. For the treatment of venous thrombosis, medications are used, wearing compression stockings.
There is a high probability of thromboembolic complications and in the presence of diseases of the cardiovascular system, overweight. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of varicose veins of the lower extremities. The risk of thrombus formation is increased in women who have undergone a caesarean section. An ultrasound examination of the veins, with Dopplerography, that is, an assessment of blood flow in the vessels, helps the doctor in making a diagnosis. For the treatment of venous thrombosis, medications are used, wearing compression stockings.
A severe complication of venous thrombosis is the separation of part of the thrombus and its movement along the vascular bed. In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur.
In severe cases, the work of the heart is disrupted and death can occur.
Unpleasant sensations in the area of postoperative sutures
Unpleasant sensations in the area of postoperative sutures after caesarean section or in the area of sutures on the perineum may disturb. Normally, after suturing vaginal tears, there may be slight pain for 1-2 days, but they quickly pass. Pain in the postoperative wound after cesarean section may be disturbing for 2 weeks, gradually decreasing. Feeling of heaviness, fullness, pain in the area of the postoperative wound may indicate the accumulation of hematoma (blood) in the area of the sutures. This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
Urinary incontinence, feces, uterine prolapse
Violation of the physiological functions of the pelvic organs of varying degrees (bladder, rectum), which may appear as in the postpartum period - urinary incontinence, feces, uterine prolapse. The problem of genital prolapse occurs when the pelvic floor muscles have lost the ability to contract so much that individual organs or parts of them do not fall into the projection of the supporting apparatus. The most common cause of pelvic organ prolapse is trauma to the pelvic floor muscles during childbirth.
Hemorrhoids
Quite often, after childbirth, women are worried about the appearance of hemorrhoids - varicose veins of the rectum. The predisposing factor in this case is a significant increase in intra-abdominal pressure during pregnancy and during childbirth. In the case of hemorrhoids, formations appear in the anus, which can be painless, but most often - painful, bleeding and itchy.