Pain relief during labor
Childbirth - pain relief options
Actions for this page
Summary
Read the full fact sheet- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
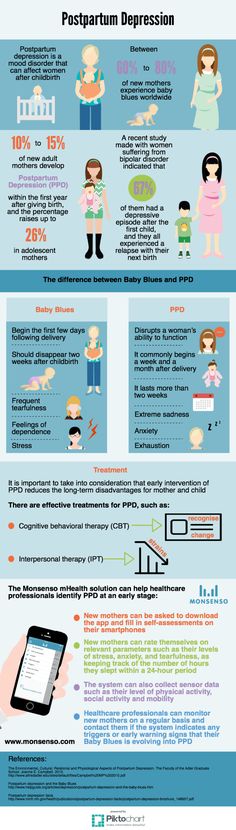
Labour and childbirth is usually a painful experience and women vary in their response to it. Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options. For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods. You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
Non-medical pain relief options for childbirth
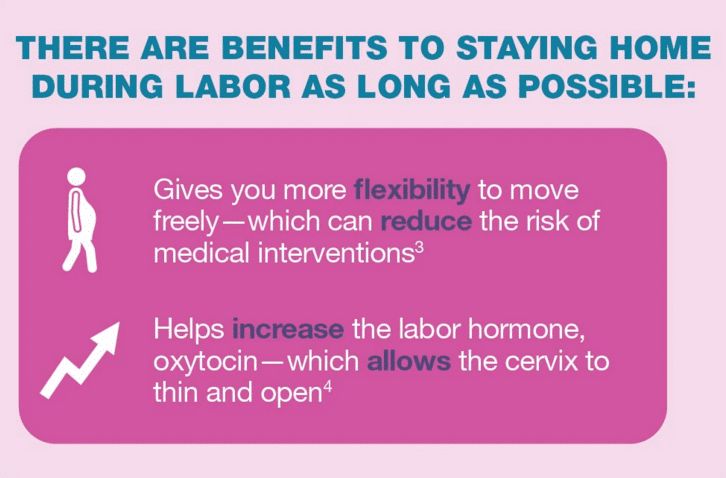
Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
- Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
- Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
- Breathing techniques may help you to ‘ride the waves’ of each contraction.
- Constant, close support from your partner (or a trusted friend or loved one) for the duration of labour can reduce anxiety.

- Using distractions like music can help to take your mind off the pain.
- Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
- Hypnosis, acupuncture and acupressure are areas in which there has been little research but these may be considered also.
Transcutaneous electrical nerve stimulation (TENS)
TENS is a technique in which nerves in the lower back are stimulated using a small hand-held device controlled by the woman. It has no known side effects for mother or baby and many women find it helpful either alone or in combination with other methods of pain relief.
Medical pain relief options for childbirth
The three main medical pain-relieving options for labour include:
- Nitrous oxide
- Pethidine
- Epidural anaesthesia.
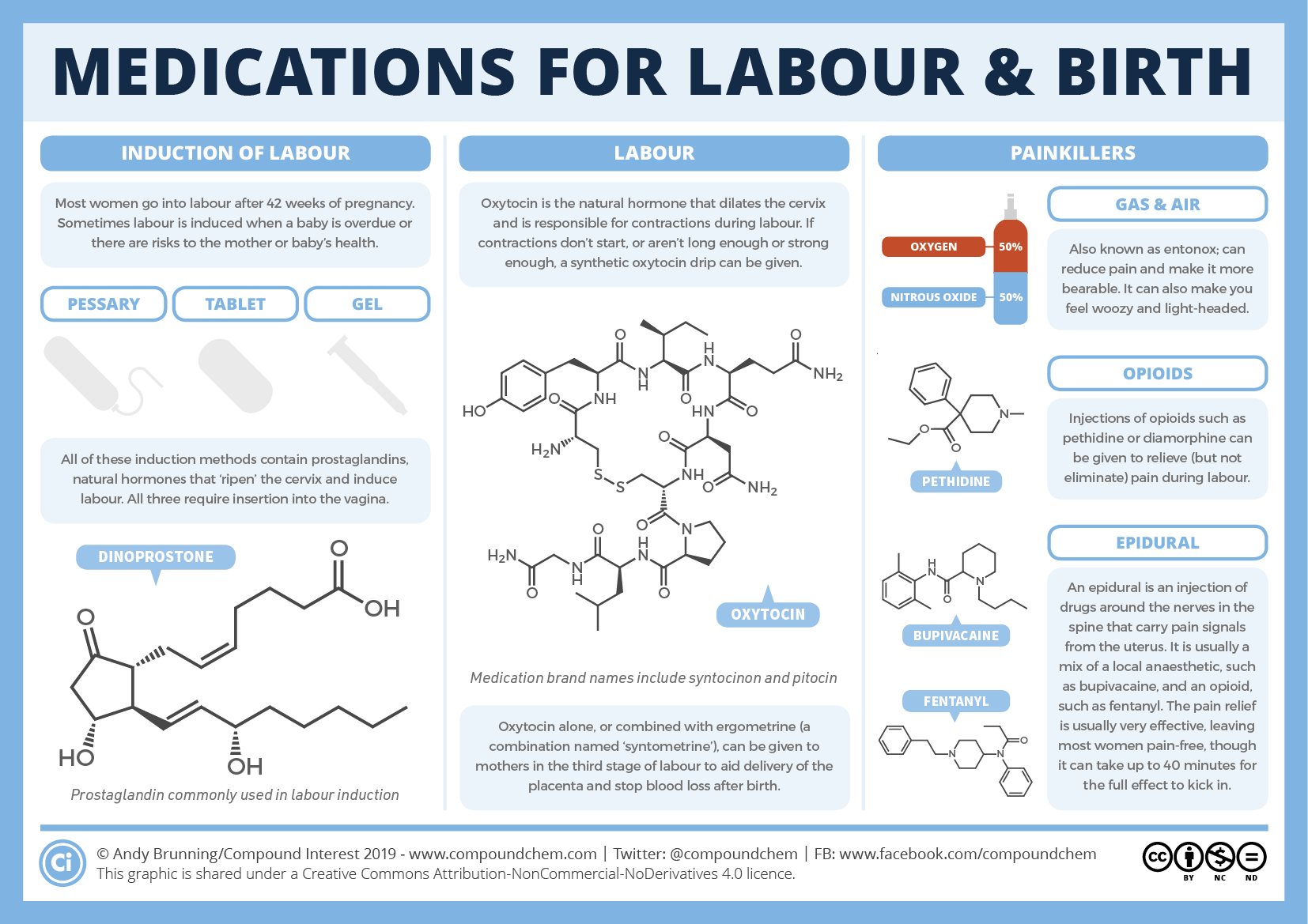
Nitrous oxide
Nitrous oxide, known as ‘laughing gas’, is mixed with oxygen and administered to the mother through a face mask or a tube held in the mouth. The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
Nitrous oxide doesn’t stop the pain entirely, but takes the ‘edge’ off the intensity of each contraction. Many women prefer nitrous oxide because it allows them direct control – you can hold the mask yourself and take deep breaths whenever you feel the need.
Nitrous oxide doesn’t interfere with contractions and it doesn’t linger in either the woman’s or the baby’s body.
Possible problems with using nitrous oxide include:
- Nausea and vomiting
- Confusion and disorientation
- Claustrophobic sensations from the face mask
- Lack of pain relief – in some cases, nitrous oxide doesn’t offer any pain relief at all (this applies to around one-third of women).
Pethidine
Pethidine is a strong pain reliever (related to morphine and heroin), usually injected directly into a muscle in the buttock. It may also be administered intravenously (directly into a vein). Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Possible problems with pethidine for the mother include:
- Giddiness and nausea
- Disorientation and altered perception
- Respiratory depression (reduced breathing)
- Lack of pain relief, in some cases.
Possible problems with pethidine for the baby include:
- The unborn baby is exposed to the drug via the umbilical cord and may experience respiratory depression at birth, particularly if several doses are given or the baby delivers soon after a pethidine injection. This effect can be reversed by an injection given to the baby.
- The baby’s sucking reflex may also be depressed, as well as other normal reflexes. Debate persists over the effects of pethidine on newborns.
Epidural anaesthesia
Epidural injections are the most effective pain relief available. They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Possible side effects and complications of epidural anaesthesia include:
- The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
- After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
- An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
- The lack of sensation in the lower body means that you will not be able to tell when you need to urinate.
 A urinary catheter will be inserted in most cases.
A urinary catheter will be inserted in most cases. - Epidurals can lengthen the second stage of labour.
- The likelihood of having a normal vaginal delivery is reduced.
- If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
- Around one per cent of women experience headache immediately following the procedure.
- Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
- Some women experience pain or tenderness where the epidural was injected.
- Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
- Very rare complications include infection, blood clots and difficulty breathing.
An epidural does not:
- Increase the length of the first stage of labour
- Increase the likelihood of a caesarean section
- Cause long-term backache.

Where to get help
- Your doctor
- Obstetrician
- Midwife
Things to remember
- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
- Continuous support for women during childbirth, 2007, Cochrane Database of Systematic Reviews, Issue 2. More information here.
- Using water for pain relief during labour, 2007, The Royal Women’s Hospital, Melbourne.
- Epidural information, 2013, The Royal Women’s Hospital, Melbourne.
- Pain relief during labour and birth, Women’s and Children’s Health Network, Department of Health, South Australian Government.
 More information here.
More information here. - Epidural anaesthesia – side effects, 2011, NHS Choices, UK. More information here.
- Epidural anaesthesia, NHS, UK. More information here.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 31-08-2014
Labor Pain: Signs, Symptoms & Management
Labor PainYou’re having a baby! You’re likely excited and no doubt nervous about several things — including the hard work and pain of labor and giving birth. Fortunately, there are many ways to ease labor pain and help you relax, including medications and breathing techniques.
There are many ways to ease labor pain and help you relax, including medications and breathing techniques.
Every woman’s pain during labor is different. Talking with your health care providers, including your anesthesiologist, will help you decide which pain management methods will help you have the best possible labor and delivery experience. You may decide to use no medication, or you might choose from different types and levels of medications. Depending on how your labor progresses, you may choose to change your pain management plan or use a combination of methods. Whatever you decide, your anesthesiologist is available to help you.
Talking with your health care providers, including your anesthesiologist, will help you decide which pain management methods will help you have the best possible labor and delivery experience. You may decide to use no medication, or you might choose from different types and levels of medications. Depending on how your labor progresses, you may choose to change your pain management plan or use a combination of methods. Whatever you decide, your anesthesiologist is available to help you.
Here are some of the most common options for managing labor pain:
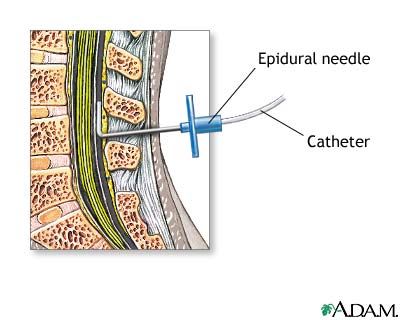
- Epidural: This is the most common type of pain relief used during labor. If you choose to have an epidural, an anesthesiologist will insert a needle and a tiny tube, called a catheter, in the lower part of your back. An epidural numbs only the lower part of your body below your belly button and allows you to be awake and alert throughout labor, as well as to feel pressure.
 You will be able to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work, and you can continue to receive it as needed. Epidurals are very safe; however, as with all medications and medical procedures, there are some potential side effects to be aware of.
You will be able to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work, and you can continue to receive it as needed. Epidurals are very safe; however, as with all medications and medical procedures, there are some potential side effects to be aware of. - Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate. To make this less likely, you will be given extra fluids through a tube in your arm (IV line) and may need to lie on your side. Sometimes, your anesthesiologist will give you a medication to maintain your lower blood pressure.
- Sore back – Your lower back may be sore where the needle was inserted to deliver the medication. This soreness should last no more than a few days.
- Headache – On rare occasions, the needle pierces the covering of the spinal cord, which can cause a headache that may last for a few days if left untreated.

Women sometimes ask if an epidural can slow labor or lead to a cesarean delivery, also known as a C-section. There is no evidence that it does either.
- Spinal block: This can be used alone or in combination with an epidural, which is referred to as a combined spinal epidural (CSE). For this, an anesthesiologist provides medication through a needle inserted in the lower back into the spinal canal. The relief from pain is immediate and lasts from an hour and a half to three hours. You will be numb from your abdomen to your legs and feel no pain. A spinal block can be used for vaginal childbirth as well as for a planned C-section.
- Analgesics: These pain medications are delivered through an IV line into a vein or injected into a muscle. Analgesics can include bothopioid and non-opioid medications and temporarily relieve pain but do not eliminate it.
- General anesthesia: This is the only type of pain medication used during labor that makes you lose consciousness.
 With general anesthesia, you will not be awake for the birth of your baby. It works quickly and is typically used only if you need an emergency C-section or have another urgent medical problem (such as bleeding).
With general anesthesia, you will not be awake for the birth of your baby. It works quickly and is typically used only if you need an emergency C-section or have another urgent medical problem (such as bleeding). - Additional and complementary pain management methods: There are also ways to help you cope with labor pain without medication, or in combination with medication:
- Massage – Have your partner massage your back or feet.
- Breathing – Deep, slow breaths and grunting are two examples of the many different ways to breathe through the pain of a contraction.
- Visualization –You may find it helpful to picture yourself somewhere enjoyable, such as on a beach or walking through a forest.
- Water – Soak in a tub or take a shower to soothe some tension.
Nitrous oxide – Often referred to as “laughing gas,” this option had not traditionally been used in the U. S. for labor and delivery, but is becoming more common. It may help reduce anxiety, but does not eliminate pain. Nitrous oxide may potentially affect your breathing, decrease awareness and cause nausea, vomiting, and dizziness. More research is needed to determine how effective nitrous oxide is, potential complications it could cause, in addition to any possible long-term side effects for you or baby.
S. for labor and delivery, but is becoming more common. It may help reduce anxiety, but does not eliminate pain. Nitrous oxide may potentially affect your breathing, decrease awareness and cause nausea, vomiting, and dizziness. More research is needed to determine how effective nitrous oxide is, potential complications it could cause, in addition to any possible long-term side effects for you or baby.
Thanks to the miracles of modern medicine, more women are giving birth in their late 30s and 40s. But older age and conditions such as diabetes, high blood pressure, and obesity increase the risk of complications for you and your baby. If you are an expectant mother, you should talk with your obstetrician and your anesthesiologist to develop a plan that ensures the safest possible pregnancy, childbirth, and recovery.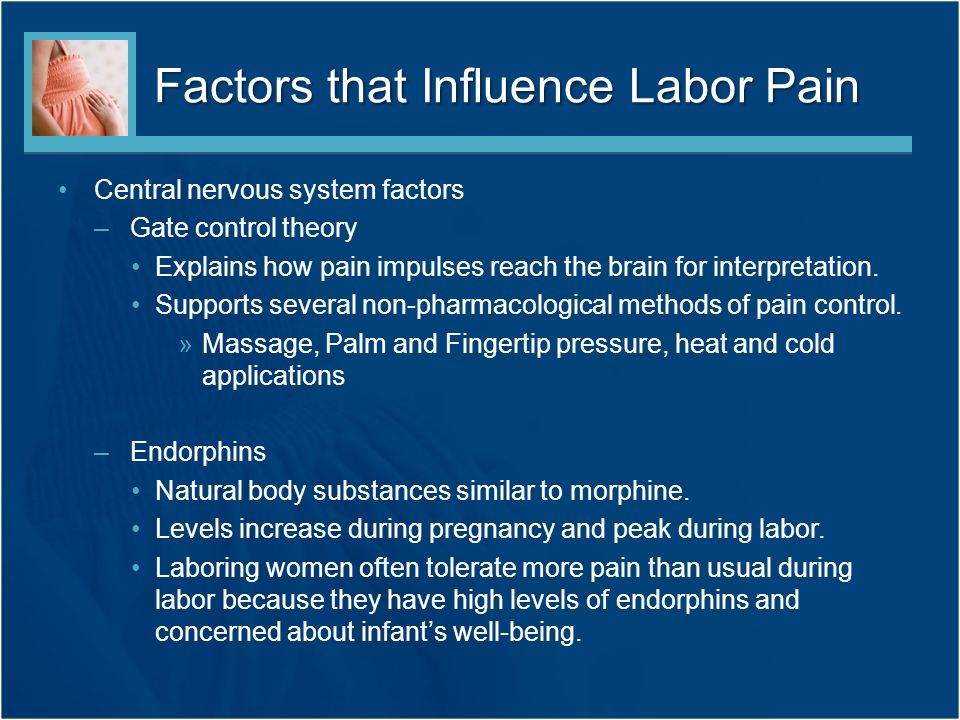
Share:
Here are some of the things you can do:
- Take care of yourself: If you are older, overweight, or have diabetes, high blood pressure, or other health conditions, work closely with your physicians to address your condition prior to labor and delivery so you understand all possible complications and have a plan. About halfway through your pregnancy, meet with your anesthesiologist, who will provide information to help keep you safe by developing an optimal labor, delivery, and recovery plan.
- Express your concerns: If you have had a bad experience with anesthesia or have any fears about childbirth, let your physicians know. Never brush off your concerns — if something doesn’t feel right, tell your obstetrician and anesthesiologist. Be sure to ask about other issues of possible concern, such as whether having a slipped disk or a lower back tattoo would prevent you from having an epidural.
- Ask about an emergency plan.
 Your physicians will always prioritize your safety as well as your baby’s. But it’s important to know your hospital has an emergency plan in place. Anesthesiologists have extensive critical care training and are experts in treating emergencies such as postpartum hemorrhage (bleeding) and preeclampsia (high blood pressure).
Your physicians will always prioritize your safety as well as your baby’s. But it’s important to know your hospital has an emergency plan in place. Anesthesiologists have extensive critical care training and are experts in treating emergencies such as postpartum hemorrhage (bleeding) and preeclampsia (high blood pressure). - Know experts are working to improve care. Anesthesiologists are leading the way to develop protocols that improve safety during and after childbirth. Efforts include:
- “Safety bundles” and best practices for managing common causes of maternal death, including postpartum hemorrhage and high blood pressure, which can lead to preeclampsia and, if not treated, to seizures, coma, brain damage, blood clots, and death.
- Early warning systems that trigger an immediate evaluation if a mother’s health declines rapidly.
- Refinement of labor and delivery pain management techniques, including epidurals and spinal anesthesia, which has led to significant reductions in maternal deaths.

- Multi-disciplinary review committees at the state level to examine maternal deaths and identify the causes, determine preventability, and implement prevention efforts.
- Plan your pain management: Untreated post-delivery pain (after vaginal as well as C-section birth) can lead to post-traumatic stress disorder in some women, so don’t downplay your pain. Ask your obstetrician to reach out to your anesthesiologist if you have questions about how to manage pain after birth. Ask whether opioids are an option or should be avoided.
Anesthesiologists are committed to patient safety and high-quality care, and have the necessary knowledge to understand and treat the entire human body.
Childbirth pain relief
Since ancient times, people have perceived pain during childbirth as an evil, attributed it to punishment coming from supernatural forces. To appease these forces, amulets were used or special rituals were performed. Already in the Middle Ages, decoctions of herbs, poppy heads or alcohol were tried to anesthetize childbirth.
Already in the Middle Ages, decoctions of herbs, poppy heads or alcohol were tried to anesthetize childbirth.
However, the use of these drinks brought only minor relief, accompanied by serious adverse events, primarily drowsiness. In 1847, the English professor Simpson first used ether anesthesia to anesthetize childbirth.
Physiological basis of labor pain. Typically, contractions are accompanied by pain of varying severity. Many factors affect the pain in childbirth, their intensity, truly painless childbirth are rare.
Pain during contractions due to:
- 1. Cervical dilatation.
- 2. Contraction of the uterus and tension of the uterine ligaments
- 3. Irritation of the peritoneum, the inner surface of the sacrum due to mechanical compression of this area during the passage of the fetus.
- 4. Pelvic floor muscle resistance.
- 5. Accumulation of products of tissue metabolism, formed during prolonged uterine contraction and temporary violation of the blood supply to the uterus.
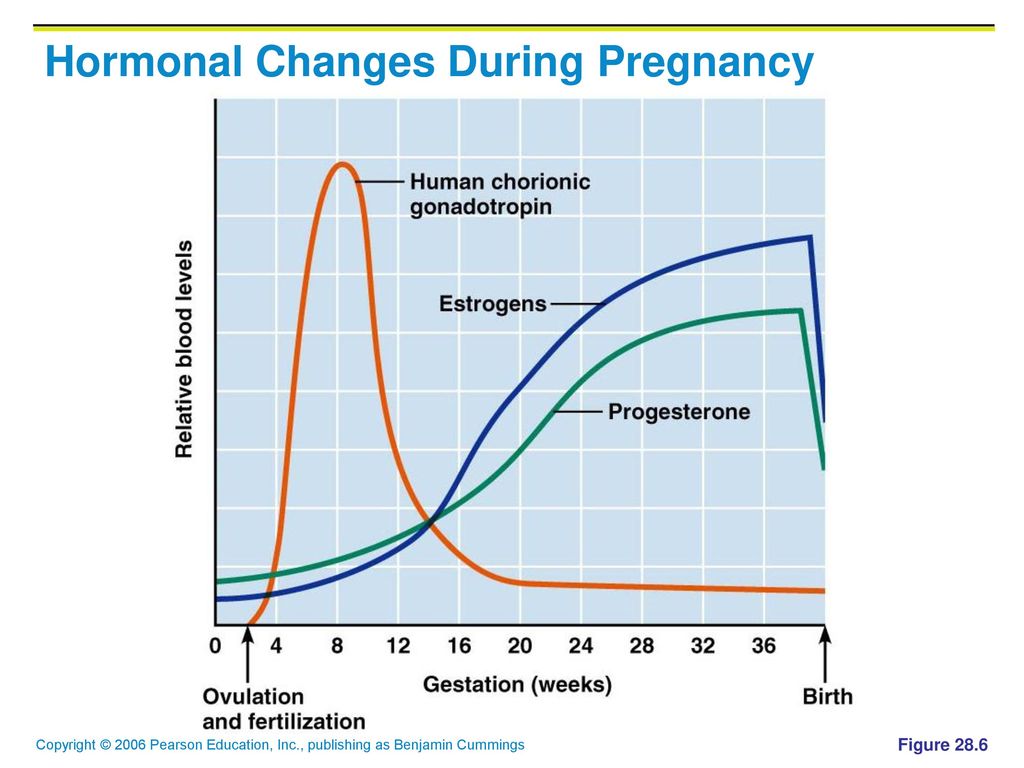
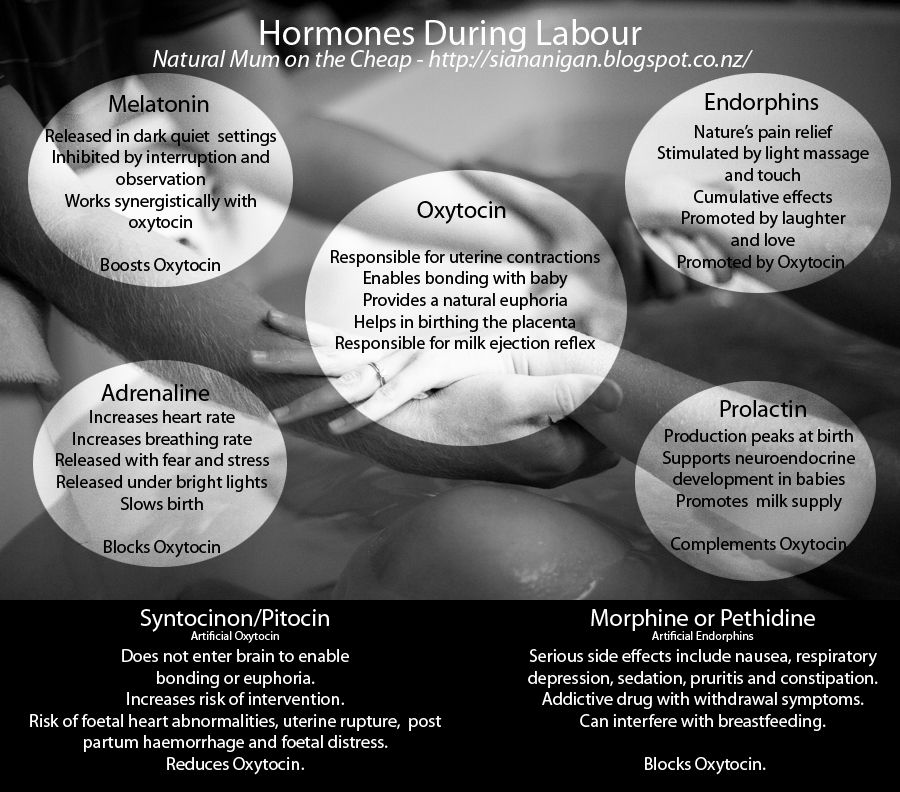
The strength of the pain sensation depends on the individual characteristics of the threshold of pain sensitivity, the emotional mood of the woman and her attitude to the birth of the child. It is important not to be afraid of childbirth and labor pain. Nature has taken care to supply the woman with the painkillers she needs for childbirth. Among the hormones produced during childbirth, a woman's body secretes a large number of hormones of joy and pleasure - endorphins. These hormones help a woman to relax, relieve pain, give a feeling of emotional uplift. However, the mechanism for the production of these hormones is very fragile. If a woman experiences fear during childbirth, then a reflex suppression of the production of endorphins occurs and a significant amount of adrenaline (a stress hormone produced in the adrenal glands) is released into the blood. In response to the release of adrenaline, convulsive muscle tension occurs (as an adaptive form of response to fear), which leads to squeezing of muscle vessels and impaired blood supply to the muscles. Violation of the blood supply and muscle tension irritates the receptors of the uterus, which we feel as pain.
Violation of the blood supply and muscle tension irritates the receptors of the uterus, which we feel as pain.
Effect of pain on the course of labor.
The uterus has a complex system of receptors. There is a relationship between painful stimulation of the uterine receptors and the accumulation of the hormone of labor (oxytocin) in the pituitary gland. The facts of reflex influences of various painful stimuli on the motor function of the uterus have been established.
Feelings during childbirth largely depend on the mental state of the woman. If all the attention of a woman in labor is concentrated only on pain sensations, a violation of homeostatic mechanisms may occur, a violation of normal labor activity. Pain, fear and excitement during childbirth stimulate that part of the nerve fibers that irritate the circular fibers of the uterine muscle, thereby resisting the pushing forces of the longitudinal fibers of the uterus and disrupt the opening of the cervix. Two powerful muscles begin to oppose each other, this brings the muscles of the uterus into great tension. The tension is of an average level and is perceived as pain. Overvoltage causes a violation of the blood supply to the child through the placenta. If this phenomenon is short-term, then the condition of the fetus does not suffer, since much less oxygen saturation of the blood is necessary for its life support than for an adult. But if this situation persists for a long time, then due to the lack of oxygen, irreversible damage to the tissues and organs of the fetus, primarily its brain, as the organ most dependent on oxygen, can occur.
Two powerful muscles begin to oppose each other, this brings the muscles of the uterus into great tension. The tension is of an average level and is perceived as pain. Overvoltage causes a violation of the blood supply to the child through the placenta. If this phenomenon is short-term, then the condition of the fetus does not suffer, since much less oxygen saturation of the blood is necessary for its life support than for an adult. But if this situation persists for a long time, then due to the lack of oxygen, irreversible damage to the tissues and organs of the fetus, primarily its brain, as the organ most dependent on oxygen, can occur.
The main task of pain relief in childbirth is an attempt to break this vicious circle and not bring the muscles of the uterus to overexertion. Many women prepared for childbirth manage to cope with this task on their own, without resorting to medication due to psychological stability and various psychotherapeutic techniques (relaxation, breathing, massage, water procedures).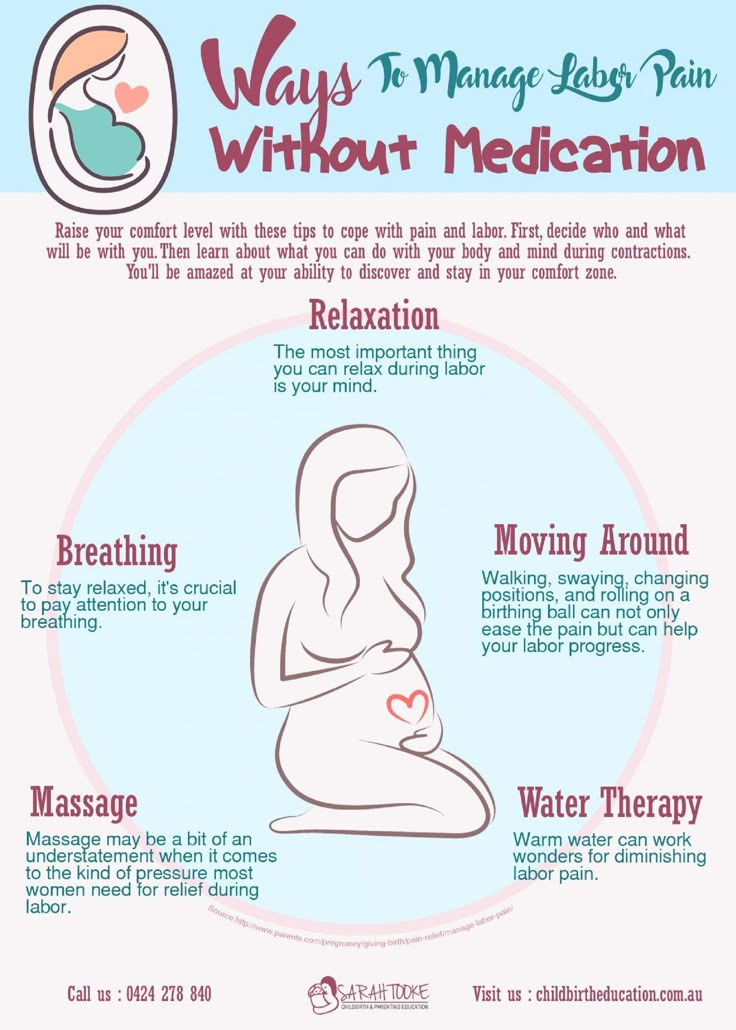 Other women simply need to provide appropriate medical attention, reducing the feeling of pain or blunting the nervous system's response to pain. If this is not done on time, then the overstressing of the uterus muscles can lead to negative consequences for the mother and fetus.
Other women simply need to provide appropriate medical attention, reducing the feeling of pain or blunting the nervous system's response to pain. If this is not done on time, then the overstressing of the uterus muscles can lead to negative consequences for the mother and fetus.
Medications used for labor pain relief must meet the following requirements:
- Have a fairly strong and fast-acting analgesic effect.
- Suppress negative emotions, a sense of fear, while not disturbing the consciousness of the woman in labor for a long period.
- Do not have a negative effect on the body of the mother and fetus, slightly penetrate the placenta and into the brain of the fetus.
- Do not adversely affect labor, the woman's ability to participate in childbirth and the postpartum period.
- Do not cause drug dependence at the required course of drug administration.
- Be available for use in any maternity facility.
The following groups of medicines are used to relieve childbirth:
1. Antispasmodics - drugs that reduce the tone and contractile activity of smooth muscles and blood vessels. Back in 1923, Academician A.P. Nikolaev suggested using an antispasmodic for pain relief during childbirth. The following drugs are usually used: DROTAVERIN (NO-SHPA), PAPAVERIN, BUSCOPAN. Appointment of antispasmodics shown:
Antispasmodics - drugs that reduce the tone and contractile activity of smooth muscles and blood vessels. Back in 1923, Academician A.P. Nikolaev suggested using an antispasmodic for pain relief during childbirth. The following drugs are usually used: DROTAVERIN (NO-SHPA), PAPAVERIN, BUSCOPAN. Appointment of antispasmodics shown:
- women in childbirth who have not undergone sufficient psychoprophylactic training, showing signs of weakness, imbalance of the nervous system, too young and old women. In such cases, antispasmodics are used at the beginning of the active phase of the first stage of labor (at 2-3 cm of cervical dilatation) in order to prevent labor pains and only partially to eliminate them. It is important to wait for regular steady contractions, otherwise this process of childbirth may stop.
- for women in labor, as an independent analgesic for already developed pains, or in combination with other drugs, when the cervix is dilated by 4 cm or more.
In case of developed labor activity, antispasmodics do not affect the strength and frequency of contractions, do not disturb the consciousness of the woman in labor and her ability to act. Antispasmodics well help to cope with the opening of the cervix, relieve spasm of smooth muscles, reduce the duration of the first stage of labor. They do not have a negative effect on the fetus. Of the side effects, there is a drop in blood pressure, nausea, dizziness, weakness. However, these drugs have an analgesic effect is not pronounced.
2. Non-narcotic analgesics: ANALGIN, TRAMAL, TRAMADOL. The use of drugs of this group, despite the good analgesic effect, in childbirth has some limitations.
In particular, analgin, when prescribed at the very beginning of labor, can weaken uterine contractions and lead to the development of weakness in labor. This is due to the fact that analgin suppresses the production of prostaglandins, which accumulate in the wall of the uterus in order to ensure the proper functioning of the muscles of the uterus during childbirth. At the same time, when labor activity is expressed, analgin does not affect uterine contractility. In addition, analgin affects blood clotting, which can increase blood loss during childbirth. And the use of a combination of analgesics with antispasmodics shortens the duration of the first stage of labor. Contraindications for the use of analgin in childbirth are impaired renal or hepatic function, blood diseases, bronchial asthma.
At the same time, when labor activity is expressed, analgin does not affect uterine contractility. In addition, analgin affects blood clotting, which can increase blood loss during childbirth. And the use of a combination of analgesics with antispasmodics shortens the duration of the first stage of labor. Contraindications for the use of analgin in childbirth are impaired renal or hepatic function, blood diseases, bronchial asthma.
In addition to pain relief, tramadol has a sedative effect, which is useful in case of a pronounced emotional component of labor pain. However, the sedative effect of tramadol allows it to be attributed to an intermediate position between analgesics and drugs. Respiratory depression in parturient women with the use of tramadol, as a rule, does not occur, rarely causes short-term dizziness, blurred vision, impaired perception, nausea, vomiting and itching. It is forbidden to use these drugs in late toxicosis of pregnancy (preeclampsia). However, the use of these drugs is limited, since with repeated injections they affect the nervous system of the fetus, cause a slowdown in the breathing of the newborn, and disrupt his heart rhythm. Premature newborns are especially sensitive to these drugs.
Premature newborns are especially sensitive to these drugs.
3. Sedatives - sedatives that relieve irritability, nervousness, and stress. These include DIAZEPAM, HEXENAL, THIOPENTAL, DROPERIDOL Hexenal and thiopental are used in childbirth as components of drug anesthesia to relieve agitation, as well as to reduce nausea and vomiting. Side effects of these drugs include hypotension and respiratory depression. They quickly penetrate the placental barrier, but at low doses do not cause severe depression in mature full-term newborns. During childbirth, these drugs are rarely prescribed. The main indication for their use is to obtain a rapid sedative and anticonvulsant effect in pregnant women with severe forms of preeclampsia.
Diazepam has no analgesic effect, so it is prescribed in combination with narcotic or non-narcotic analgesics. Diazepam is able to accelerate the opening of the cervix, helps to relieve anxiety in a number of women in labor. However, it easily penetrates into the blood of the fetus, therefore, it causes respiratory failure, a decrease in blood pressure and body temperature, and sometimes signs of neurological depression in newborns.
Droperidol causes a state of neurolepsy (calmness, indifference and aloofness), has a strong antiemetic effect. In obstetric practice has received significant distribution. However, one should be aware of the side effects of droperidol: it causes incoordination and weakness in the mother, respiratory depression and pressure drop in the newborn. With high blood pressure in a woman in labor, droperidol is combined with analgesics.
4. Narcotic analgesics: PROMEDOL, FENTANIL, OMNOPON, GHB
The mechanism of action of these drugs is based on interaction with opiate receptors. They are believed to be safe for both mother and child. They act soothingly, relaxes, while maintaining consciousness. They have an analgesic, antispasmodic effect, promote the opening of the cervix, contribute to the correction of uncoordinated uterine contractions.
However, all narcotic drugs have a number of disadvantages, the main of which is that in high doses they depress breathing and cause drug dependence, state of stupor, nausea, vomiting, constipation, depression, lowering blood pressure.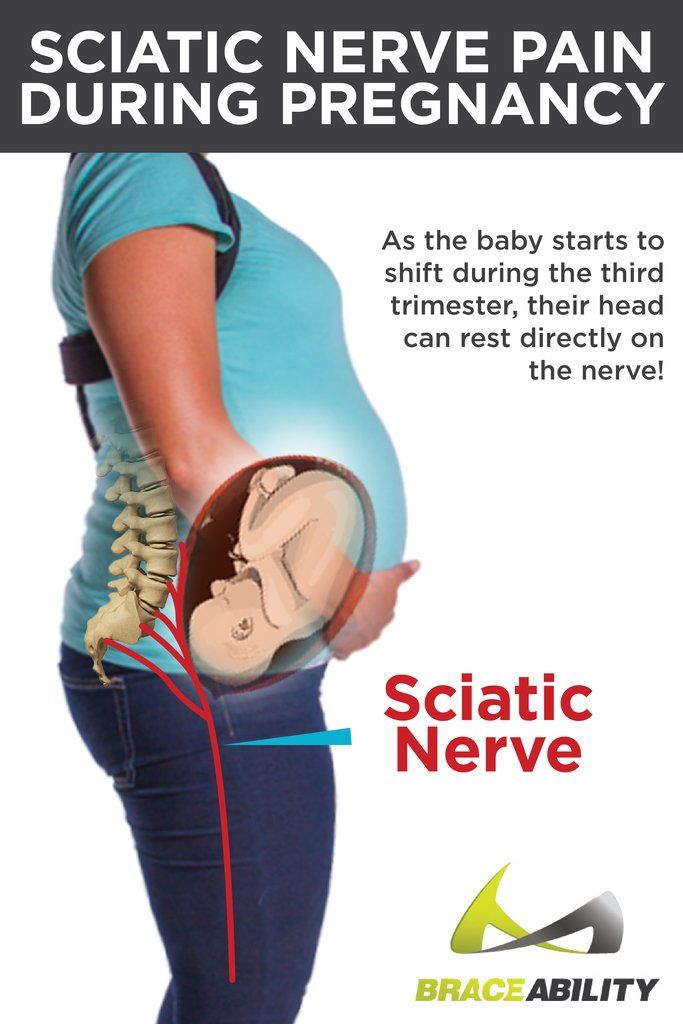 The drugs easily cross the placenta, and the more time passes from the moment the drug is administered, the higher its concentration in the blood of the newborn. The maximum concentration of promedol in the blood plasma of a newborn was noted 2-3 hours after its administration to the mother. If the birth occurs at this time, then the drug causes temporary respiratory depression of the child.
The drugs easily cross the placenta, and the more time passes from the moment the drug is administered, the higher its concentration in the blood of the newborn. The maximum concentration of promedol in the blood plasma of a newborn was noted 2-3 hours after its administration to the mother. If the birth occurs at this time, then the drug causes temporary respiratory depression of the child.
Sodium oxybutyrate (GHB) is used when a woman in labor needs to rest. As a rule, when the drug is administered, sleep occurs after 10-15 minutes and lasts 2-5 hours. Ether is not currently used for labor pain relief, since it significantly weakens labor activity, can increase blood pressure, and adversely affect the fetus.
Inhalation anesthesia of childbirth by inhalation of painkillers is still widely used in obstetric practice. Inhalation anesthetics are used in the active phase of labor with the opening of the cervix by at least 3-4 cm and in the presence of severe pain in contractions.
Nitrous oxide is the primary inhalant used for both obstetric and labor pain relief. The advantage of nitrous oxide is safety for the mother and fetus, the rapid onset of action and its rapid end, as well as the absence of a negative effect on contractile activity, and a pungent odor. They give nitrous oxide through a special apparatus using a mask. The woman in labor is introduced to the technique of using the mask and she herself applies the mask and inhales nitrous oxide with oxygen as needed. When inhaling it, a woman feels dizzy or nauseous. The action of the gas is manifested in half a minute, so at the beginning of the contraction, you need to take a few deep breaths
Trilene is a clear liquid with a pungent odor. It has an analgesic effect even in small concentrations and with the preservation of consciousness. Does not suppress labor activity. It is a well-administered fast-acting agent - after the cessation of inhalation, it quickly ceases to have an effect on the body. The downside is the bad smell.
The downside is the bad smell.
6. Epidural anesthesia during childbirth and caesarean section
Epidural analgesia is performed by blocking pain impulses from the uterus along the nerve pathways entering the spinal cord at a certain level by injecting a local anesthetic into the space around the spinal cord membrane.
Performed by an experienced anesthesiologist. The time to start epidural analgesia is determined by the obstetrician and anesthesiologist, depending on the needs of the woman in labor and the child during childbirth. It is usually performed with established regular labor and at least 3-4 cm dilatation of the cervix.
Epidural lumbar anesthesia is performed in the lower back with the mother sitting or lying on her side. After treating the skin in the area of the lumbar spine, the anesthesiologist makes a puncture between the vertebrae and enters the epidural space of the spine. First, a trial dose of anesthetic is administered, then, if there are no side effects, a catheter is inserted and the desired dose is given. Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg. The catheter is attached to the back, if it is necessary to increase the dose, subsequent injections will no longer require a second puncture, but are made through the catheter.
Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg. The catheter is attached to the back, if it is necessary to increase the dose, subsequent injections will no longer require a second puncture, but are made through the catheter.
Pain relief usually develops 10-20 minutes after the epidural and can be continued until the end of labor and is usually very effective. Epidural anesthesia is safe for mother and child. Of the side effects, there is a decrease in blood pressure, back pain, weakness in the legs, headaches. More severe complications are a toxic reaction to local anesthetics, respiratory arrest, and neurological disorders. They are extremely rare.
Sometimes the use of epidural anesthesia leads to a weakening of labor. At the same time, a woman cannot effectively push, and thus the percentage of surgical interventions (obstetrical forceps) increases.
Contraindications to the use of epidural anesthesia are: violation of blood clotting, infected wounds, scars and tumors at the puncture site, bleeding, diseases of the nervous system and spine.
Epidural anesthesia can be safely used for caesarean section. If an epidural catheter is already in place at the time of delivery and it becomes necessary to perform a caesarean section, it is usually sufficient to inject an additional dose of anesthetic through the same catheter. A higher concentration of the drug can cause a feeling of "numbness" in the abdominal cavity, sufficient for surgery
7. General anesthesia.
Indications for the use of general anesthesia in childbirth are emergency situations, such as a sharp deterioration in the condition of the child and maternal bleeding. This anesthesia can be started immediately and causes a rapid loss of consciousness, allowing for an immediate caesarean section. In these cases, general anesthesia is relatively safe for the child.
The use of any painkillers during childbirth is carried out only by obstetrician-gynecologists and anesthesiologists-resuscitators. Nurses, anesthetists and midwives follow the doctor's orders, monitor the condition of the woman in labor and note possible side effects that require a change in treatment.
Childbirth pain relief - childbirth pain relief methods (Anesthesia, anesthesia)
Childbirth is a natural process. Each of its stages is carefully thought out by nature. Only one "but" - the birth of a new life is invariably accompanied by pain.
But let's make a reservation: every woman gives birth differently, and even the first, second, third and subsequent births in one woman can differ significantly from each other. Different and pain threshold. Someone gives birth easily and it seems that they don’t care about everything, someone endures “from and to”, no matter what, others prefer to level these sensations as much as possible. Fortunately, modern medicine allows you to do this.
Pain relief during childbirth can be conditionally divided into non-drug and drug-based. And, if all possible measures of physiological anesthesia are used in almost 100% of cases, medical anesthesia for childbirth is a debatable topic. Therefore, the decision to use medical methods of anesthesia, as a rule, is made by the woman in labor. The doctor - an obstetrician-gynecologist and an anesthesiologist - act as consultants in this process: they will prompt, explain, direct and advise.
The doctor - an obstetrician-gynecologist and an anesthesiologist - act as consultants in this process: they will prompt, explain, direct and advise.
You can make a decision on the use of medical methods long beforehand, having firmly decided: "I can handle it myself", tune in accordingly. However, you can change your mind already in childbirth, the main thing is to make a final decision in time.
Non-drug methods
Maternity hospital "Medgard" stands for the free behavior of childbirth. This means that during the entire first stage of labor, the expectant mother does not lie, chained to the bed with sensors and devices, but can do what her body tells her, what relieves pain. Our body is a single system that allows, when exposed to certain parts of it, to achieve the desired effect of smoothing pain. Walking, massaging the lower back, using a fitball, singing, special breathing, and taking a bath or shower. Many mothers also note that pleasant conversations with a midwife and a doctor allow you to relax and not concentrate on sensations. Practice shows: during childbirth, the body knows how to move and what position to take to relieve pain. The wireless CTG device, which our delivery room is equipped with, contributes to this freedom of behavior, depriving the expectant mother of the need to lie down on the couch even for 10-15 minutes at 2-3 hours.
Practice shows: during childbirth, the body knows how to move and what position to take to relieve pain. The wireless CTG device, which our delivery room is equipped with, contributes to this freedom of behavior, depriving the expectant mother of the need to lie down on the couch even for 10-15 minutes at 2-3 hours.
Epidural
It is used at the request of the patient and for a number of medical indications. The essence of the method is the introduction of special drugs that block pain signals transmitted from the spinal cord to the brain. Anesthesia is carried out when opening from 3 to 6 centimeters and only in the case of a normal labor activity.
The anesthesiologist makes a puncture at the level of the lumbar spine and injects an anesthetic into the epidural space. Within a few minutes, the drug begins to act. An important point - with a reduction in pain in the lower abdomen and lower back, sensitivity in the legs is preserved. This method is considered safe for a woman and a child, at the same time, it allows you to reduce the manifestations of pain, relax and save strength for attempts.
Pain relief for caesarean section
There are two main types of anesthesia used for a caesarean section: spinal anesthesia and anesthesia.
Spinal anesthesia differs from epidural anesthesia primarily by the complete blockage of sensation and movement in the lower torso. At the same time, the expectant mother is conscious and takes a full part in the birth of the child, without feeling the ongoing manipulations. So already a few seconds after the birth of the Baby, the mother can say her first "I love" and kiss the baby on the top of her head. This method of pain relief can also be used when an emergency caesarean section is indicated.
Anesthesia or medication sleep involves a complete "shutdown" from the process. In this case, after treatment, the baby is transferred to the children's ward and transferred to the mother after her full recovery from anesthesia.
The use of epidural anesthesia during childbirth is a common phenomenon in international delivery practice.