Newborn head bones
Cranial sutures Information | Mount Sinai
Fontanelles; Sutures - cranial
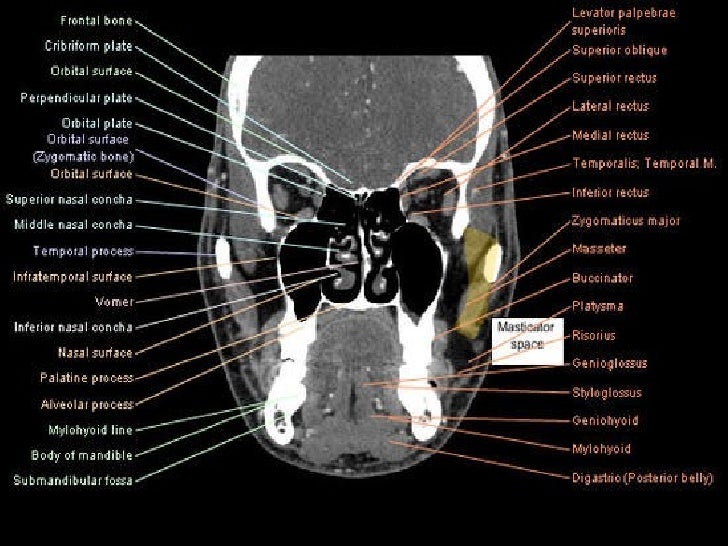
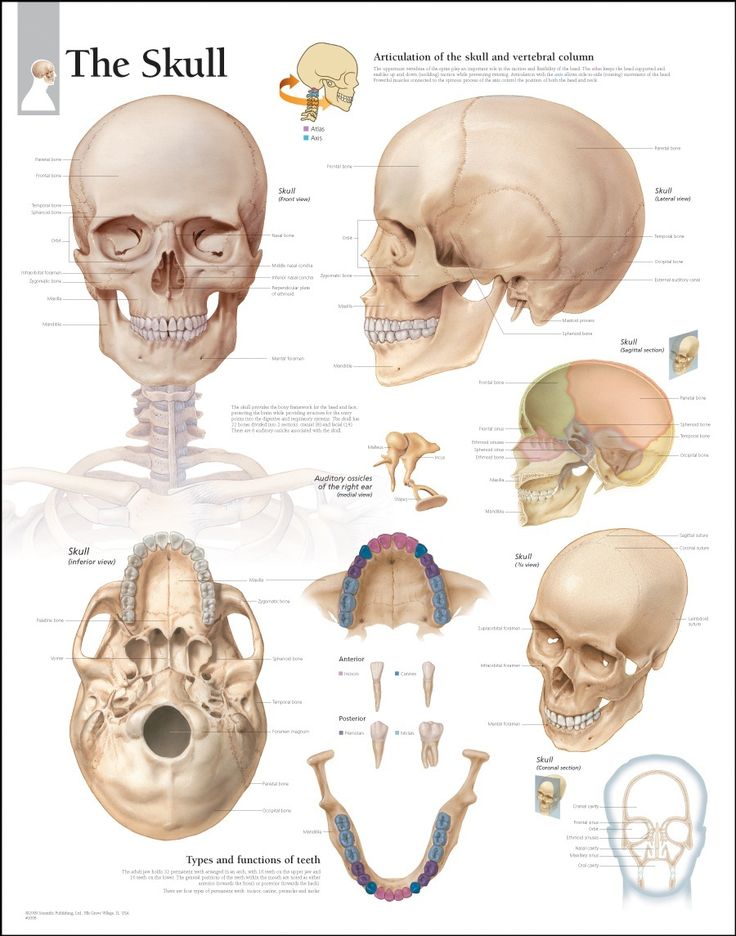
Cranial sutures are fibrous bands of tissue that connect the bones of the skull.
The sutures or anatomical lines where the bony plates of the skull join together can be easily felt in the newborn infant. The diamond shaped space on the top of the skull and the smaller space further to the back are often referred to as the soft spot in young infants.
Fontanelles are the soft spots on an infant's head where the bony plates that make up the skull have not yet come together. It is normal for infants to have these soft spots, which can be seen and felt on the top and back of the head. Fontanelles that are abnormally large may indicate a medical condition.
Information
An infant's skull is made up of 6 separate cranial (skull) bones:
- Frontal bone
- Occipital bone
- Two parietal bones
- Two temporal bones
These bones are held together by strong, fibrous, elastic tissues called sutures.
The spaces between the bones that remain open in babies and young children are called fontanelles. Sometimes, they are called soft spots. These spaces are a part of normal development. The cranial bones remain separate for about 12 to 18 months. They then grow together as part of normal growth. They stay connected throughout adulthood.
Two fontanelles usually are present on a newborn's skull:
- On the top of the middle head, just forward of center (anterior fontanelle)
- In the back of the middle of the head (posterior fontanelle)
The posterior fontanelle usually closes by age 1 or 2 months. It may already be closed at birth.
It may already be closed at birth.
The anterior fontanelle usually closes sometime between 9 months and 18 months.
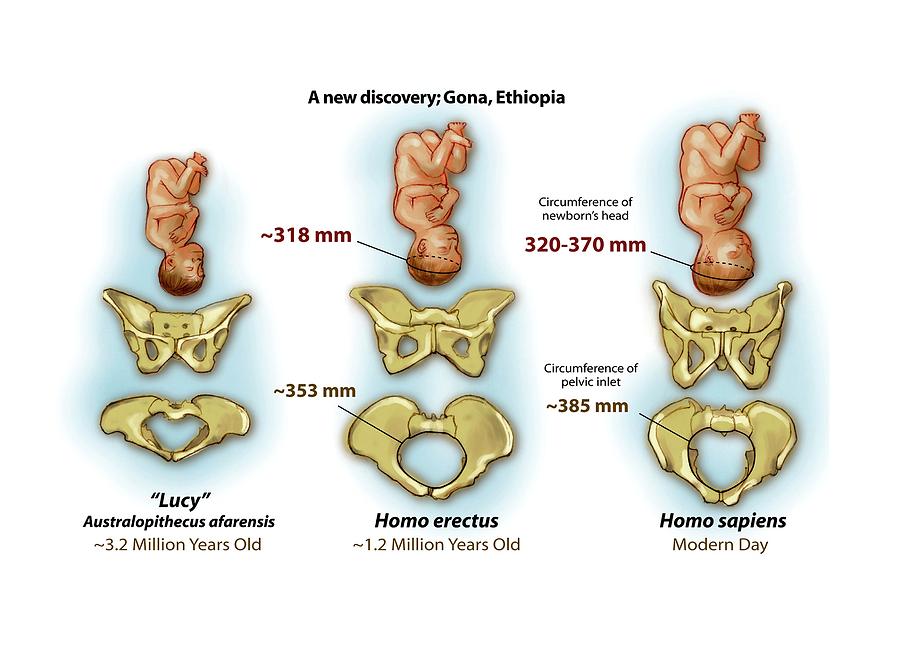
The sutures and fontanelles are needed for the infant's brain growth and development. During childbirth, the flexibility of the sutures allows the bones to overlap so the baby's head can pass through the birth canal without pressing on and damaging their brain.
During infancy and childhood, the sutures are flexible. This allows the brain to grow quickly and protects the brain from minor impacts to the head (such as when the infant is learning to hold his head up, roll over, and sit up). Without flexible sutures and fontanelles, the child's brain could not grow enough. The child would develop brain damage.
Feeling the cranial sutures and fontanelles is one way that health care providers follow the child's growth and development. They are able to assess the pressure inside the brain by feeling the tension of the fontanelles. The fontanelles should feel flat and firm. Bulging fontanelles may be a sign of increased pressure within the brain. In this case, providers may need to use imaging techniques to see the brain structure, such as CT scan or MRI scan. Surgery may be needed to relieve the increased pressure.
Bulging fontanelles may be a sign of increased pressure within the brain. In this case, providers may need to use imaging techniques to see the brain structure, such as CT scan or MRI scan. Surgery may be needed to relieve the increased pressure.
Sunken, depressed fontanelles are sometimes a sign of dehydration.
Goyal NK. The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Varma R, Williams SD. Neurology. In: Zitelli BJ, McIntire SC, Nowalk AJ, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 16.
Last reviewed on: 2/2/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA.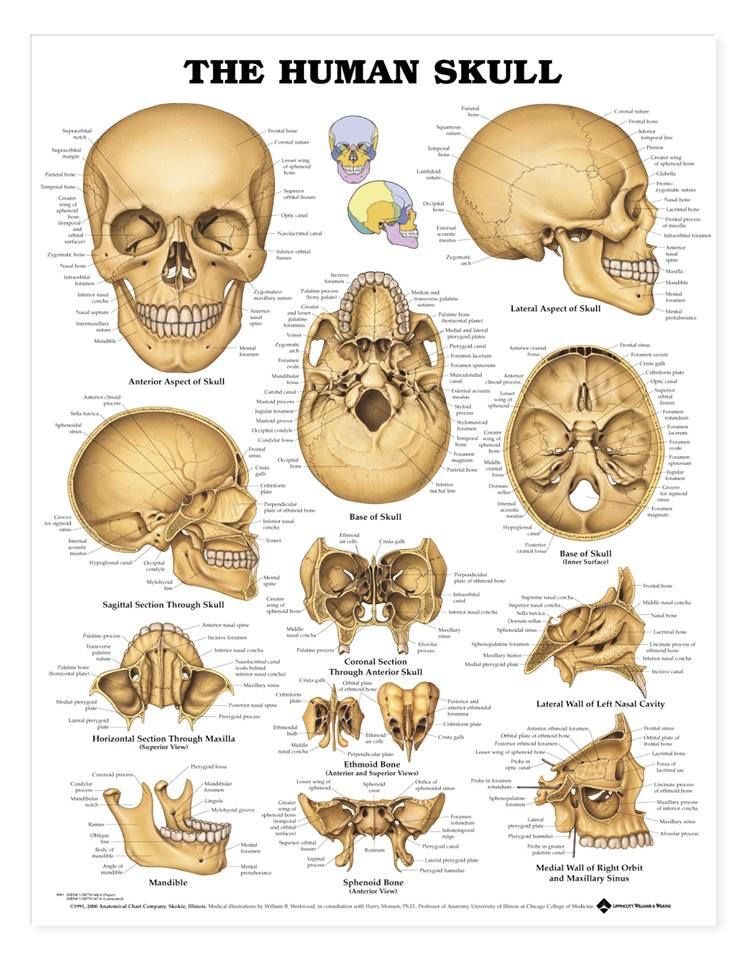 Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Facts about Craniosynostosis | CDC
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen.
Click here to view a larger image
Click here to view a larger image
What is Craniosynostosis?
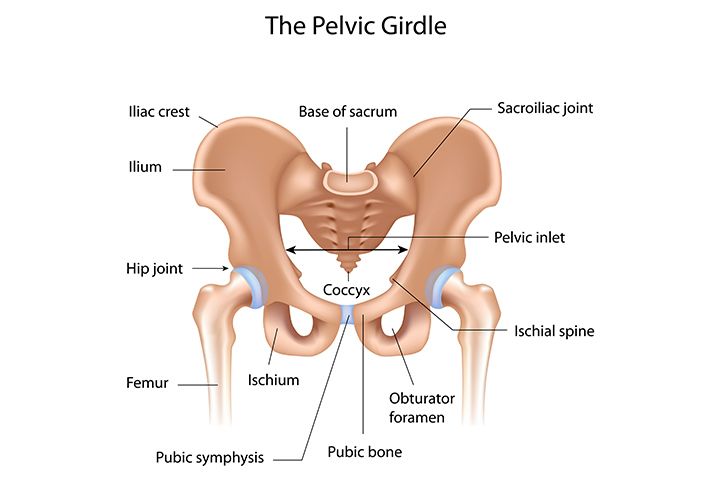
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen. The spaces between a typical baby’s skull bones are filled with flexible material and called sutures. These sutures allow the skull to grow as the baby’s brain grows. Around two years of age, a child’s skull bones begin to join together because the sutures become bone.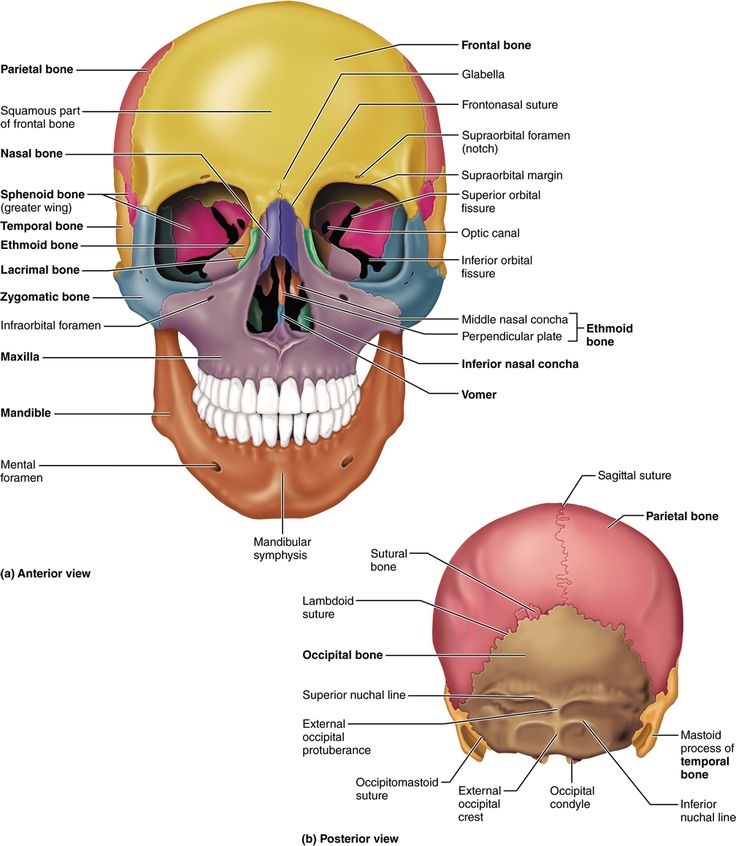 When this occurs, the suture is said to “close.” In a baby with craniosynostosis, one or more of the sutures closes too early. This can limit or slow the growth of the baby’s brain.
When this occurs, the suture is said to “close.” In a baby with craniosynostosis, one or more of the sutures closes too early. This can limit or slow the growth of the baby’s brain.
When a suture closes and the skull bones join together too soon, the baby’s head will stop growing in only that part of the skull. In the other parts of the skull where the sutures have not joined together, the baby’s head will continue to grow. When that happens, the skull will have an abnormal shape, although the brain inside the skull has grown to its usual size. Sometimes, though, more than one suture closes too early. In these instances, the brain might not have enough room to grow to its usual size. This can lead to a build-up of pressure inside the skull.
Types of Craniosynostosis
The types of craniosynostosis depend on what sutures join together early.
- Sagittal synostosis– The sagittal suture runs along the top of the head, from the baby’s soft spot near the front of the head to the back of the head.
 When this suture closes too early, the baby’s head will grow long and narrow (scaphocephaly). It is the most common type of craniosynostosis.
When this suture closes too early, the baby’s head will grow long and narrow (scaphocephaly). It is the most common type of craniosynostosis. - Coronal synostosis – The right and left coronal sutures run from each ear to the sagittal suture at the top of the head. When one of these sutures closes too early, the baby may have a flattened forehead on the side of the skull that closed early (anterior plagiocephaly). The baby’s eye socket on that side might also be raised up and his or her nose could be pulled toward that side. This is the second most common type of craniosynostosis.
- Bicoronal synostosis – This type of craniosynostosis occurs when the coronal sutures on both sides of the baby’s head close too early. In this case, the baby’s head will grow broad and short (brachycephaly).
- Lambdoid synostosis – The lambdoid suture runs along the backside of the head. If this suture closes too early, the baby’s head may be flattened on the back side (posterior plagiocephaly).
 This is one of the rarest types of craniosynostosis.
This is one of the rarest types of craniosynostosis. - Metopic synostosis – The metopic suture runs from the baby’s nose to the sagittal suture at the top of the head. If this suture closes too early, the top of the baby’s head shape may look triangular, meaning narrow in the front and broad in the back (trigonocephaly). This is one of the rarest types of craniosynostosis.
Other Problems
Many of the problems a baby can have depend on:
- Which sutures closed early
- When the sutures closed (was it before or after birth and at what age)
- Whether or not the brain has room to grow
Sometimes, if the condition is not treated, the build-up of pressure in the baby’s skull can lead to problems, such as blindness, seizures, or brain damage.
How Many Babies are Born with Craniosynostosis?
Researchers estimate that about 1 in every 2,500 babies is born with craniosynostosis in the United States.1
Causes and Risk Factors
The causes of craniosynostosis in most infants are unknown.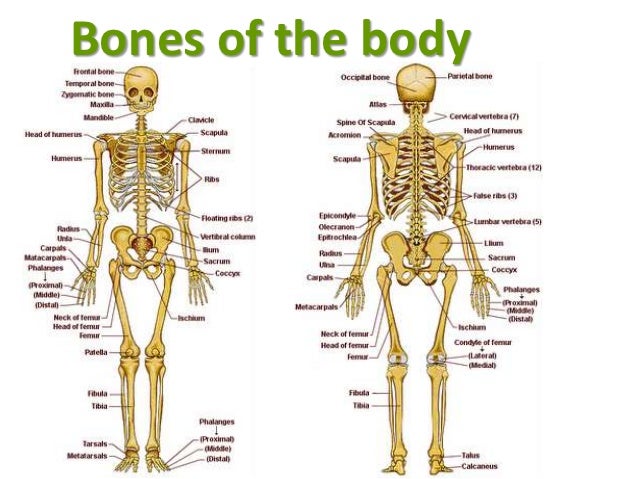 Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
CDC, like the many families of children with birth defects, wants to find out what causes these conditions. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011), to understand the causes of and risks for birth defects, such as craniosynostosis.
Recently, CDC reported on important findings from research studies about some factors that increase the chance of having a baby with craniosynostosis:
- Maternal thyroid disease ― Women with thyroid disease or who are treated for thyroid disease while they are pregnant have a higher chance of having an infant with craniosynostosis, compared to women who don’t have thyroid disease.
 2
2 - Certain medications ― Women who report using clomiphene citrate (a fertility medication) just before or early in pregnancy are more likely to have a baby with craniosynostosis, compared to women who didn’t take this medicine.3
CDC continues to study birth defects, such as craniosynostosis, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Craniosynostosis usually is diagnosed soon after a baby is born. Sometimes, it is diagnosed later in life.
Usually, the first sign of craniosynostosis is an abnormally shaped skull. Other signs may include:
- No “soft spot” on the baby’s skull
- A raised firm edge where the sutures closed early
- Slow growth or no growth in the baby’s head size over time
Doctors can identify craniosynostosis during a physical exam. A doctor will feel the baby’s head for hard edges along the sutures and unusual soft spots. The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
Treatments
Many types of craniosynostosis require surgery. The surgical procedure is meant to relieve pressure on the brain, correct the craniosynostosis, and allow the brain to grow properly. When needed, a surgical procedure is usually performed during the first year of life. But, the timing of surgery depends on which sutures are closed and whether the baby has one of the genetic syndromes that can cause craniosynostosis.
Babies with very mild craniosynostosis might not need surgery. As the baby gets older and grows hair, the shape of the skull can become less noticeable. Sometimes, special medical helmets can be used to help mold the baby’s skull into a more regular shape.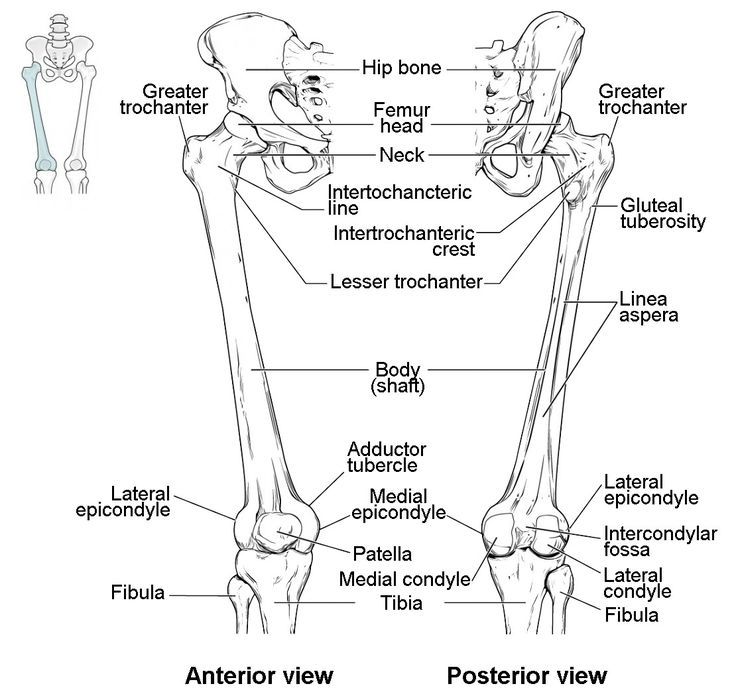
Each baby born with craniosynostosis is different, and the condition can range from mild to severe. Most babies with craniosynostosis are otherwise healthy. Some children, however, have developmental delays or intellectual disabilities, because either the craniosynostosis has kept the baby’s brain from growing and working normally, or because the baby has a genetic syndrome that caused both craniosynostosis and problems with how the brain works. A baby with craniosynostosis will need to see a healthcare provider regularly to make sure that the brain and skull are developing properly. Babies with craniosynostosis can often benefit from early intervention services to help with any developmental delays or intellectual problems. Some children with craniosynostosis may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups also can be useful for new families of babies with birth defects of the head and face, including craniosynostosis.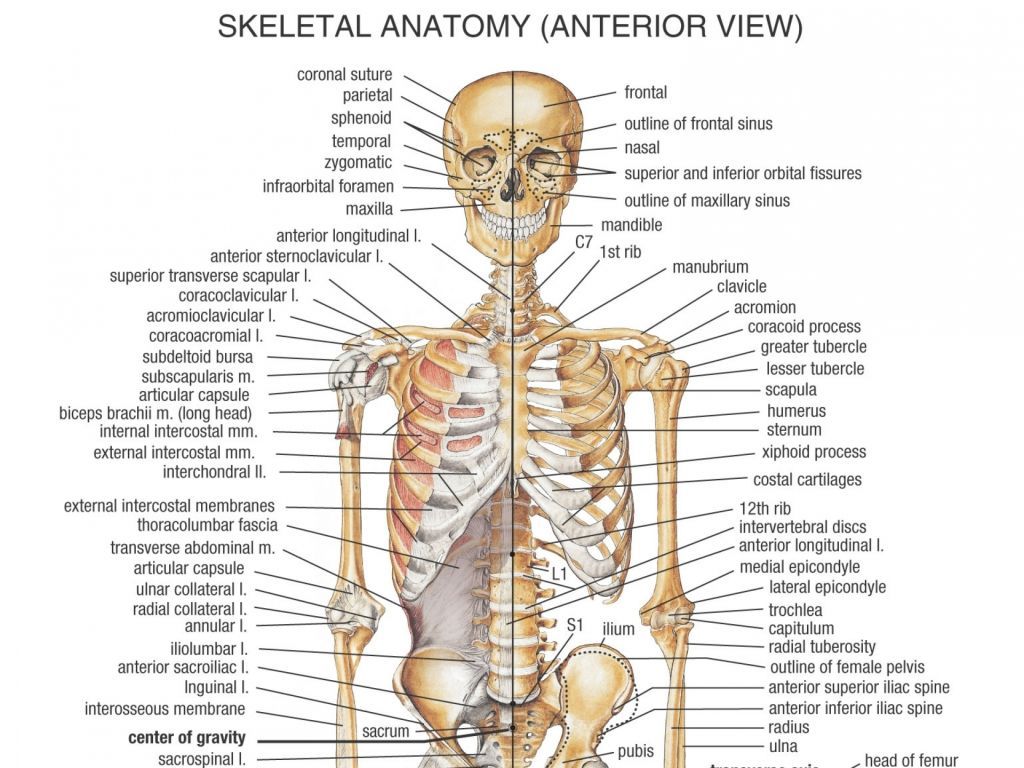
Other Resources
The views of these organizations are their own and do not reflect the official position of CDC.
- Children’s Craniofacial Association (CCA)
CCA addresses the medical, financial, psychosocial, emotional, and educational concerns relating to craniofacial conditions. - The National Craniofacial Association (FACES)
FACES is dedicated to assisting children and adults who have craniofacial disorders resulting from disease, accident, or birth.
References
- Boulet SL, Rasmussen SA, Honein MA. A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet Part A. 2008;146A:984–991.
- Rasmussen SA, Yazdy MM, Carmichael SL, Jamieson DJ, Canfield MA, Honein MA. Maternal thyroid disease as a risk factor for craniosynostosis. Obstet Gynecol. 2007;110:369-377.
- Reefhuis J, Honein MA, Schieve LA, Rasmussen SA, and the National Birth Defects Prevention Study. Use of clomiphene citrate and birth defects, National Birth Defects Prevention Study, 1997–2005.
 Hum Reprod. 2011;26:451–457.
Hum Reprod. 2011;26:451–457.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
Fontanelle in a newborn
Fontanelles are non-ossified areas between the bones of the skull. By the time of birth, the baby has 6 fontanelles:
- front (large) - has a diamond shape, its size is from 0.6 to 3.6 cm (average 2.1)
- back (small) - its dimensions are about 0.
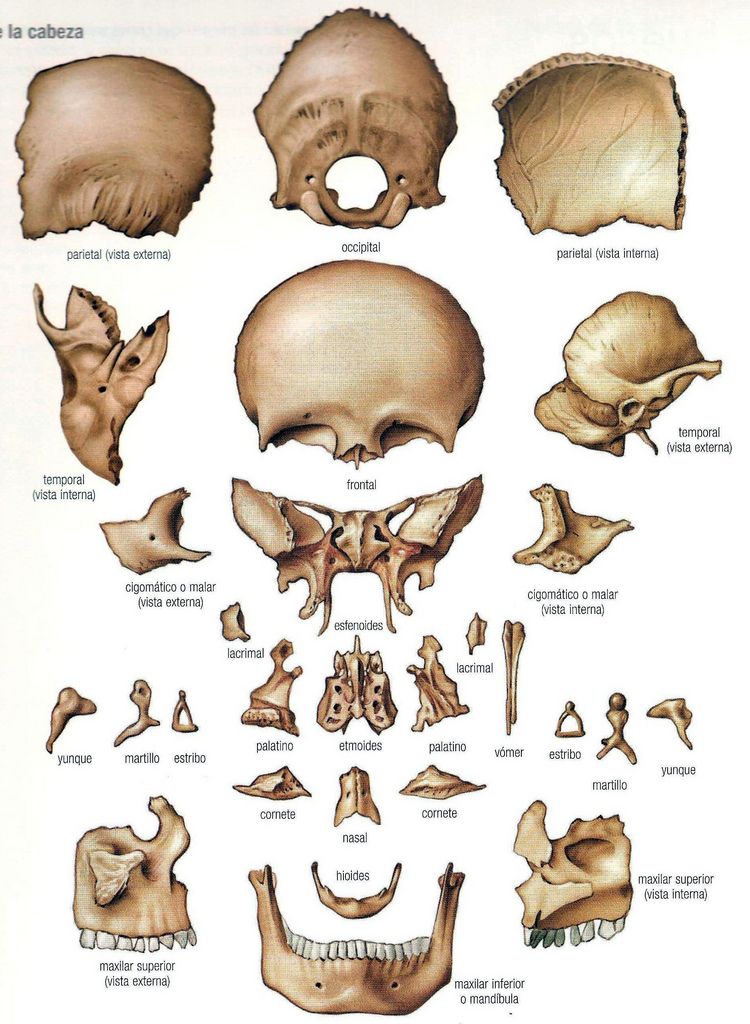 5 cm
5 cm - paired lateral: wedge and mastoid
The size of the fontanelles is determined by a large number of factors: gestational age, hereditary predisposition, metabolic state, the presence of diseases, and other components.
What are fontanelles for?
They allow the movement of the bones of the skull and the reshaping of the head for safe passage through the birth canal.
Mothers who have given birth naturally remember what a strange head shape the baby had after birth, and how it became normal after 3-5 days.
Nature designed it so that the bones of the skull during childbirth would not damage the brain, and the baby would not get stuck in the birth canal at birth.
What about skull growth?
It may be surprising, but the brain does not grow behind the bones of the skull, but the cranium increases due to the active growth of the brain. This process is especially active in the first two years of a child's life.
At the same time, the growth of the skull does not occur due to an increase in fontanelles, but due to the growth of each individual bone and the elongation of the sutures (the boundaries of the connection of the bones). If the suture between the frontal bones closes at an average of 2 years, then the remaining sutures remain open until the age of 18-20, until the end of brain growth.
Everything is individual, and the speed of closing the fontanelles depends on the characteristics of the baby. The norm is the closure of a large fontanel at 3 months. This fact must be compared with monthly increases in head circumference.
Normal indicators of fontanel closure:
- large - 3 to 24 months (average 13.8)
- small - up to 2 months
- lateral in full-term babies at birth are mostly closed.
Important nuances:
- Vitamin D supplementation and maternal diet have no effect on fontanel closure rate
- the speed of closing the large fontanel is determined by the individual characteristics of the child
- if the fontanelles close early, you need to monitor monthly increases in head circumference
- early closure of fontanelles with a slowdown in the growth of head circumference requires careful examination by a pediatrician to rule out microcephaly
Fontanelles are an important indicator of the rate of brain growth.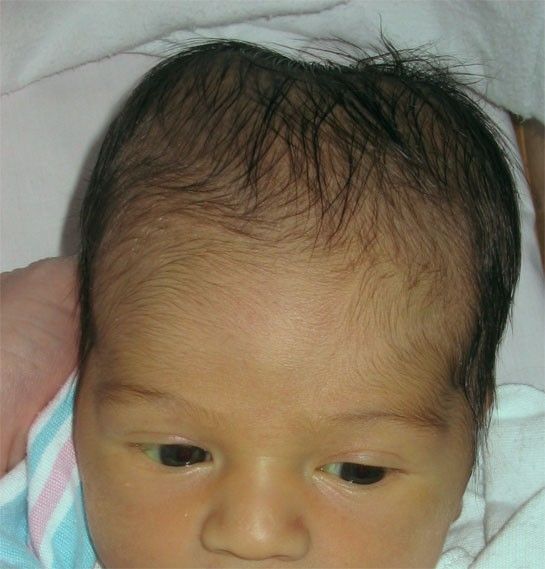 Therefore, the time of their closure requires supervision by a pediatrician or pediatric neurologist.
Therefore, the time of their closure requires supervision by a pediatrician or pediatric neurologist.
More articles
Water consumption and skin
ASIT and birch allergy
Frequent acute respiratory viral infections
Ophthalmologist's visitSee all articles The disease is cured by:
Children's osteopath
Article content
- Causes of
- Types of plagiocephaly in children
- Signs of disease
- Diagnostics of plagiocephaly in children
Plagiocephaly is an abnormally shaped skull, or flat head syndrome, in infants. Its signs are detected to some extent in every fifth child, and only every tenth of them needs specific treatment. Deformation becomes distinct noticeable by 2 months (sometimes earlier). Treatment started on time is usually effective.
Causes
- Postpartum - permanent position with emphasis on the bones of the skull (mainly lying on the back) or premature fusion of the sutures of the skull.
- Intrauterine - in most cases caused by the anatomical position during gestation - with twin pregnancy and / or pressing the fetus to the mother's ribs, large fetus or uterine abnormalities, premature prolapse during childbirth.
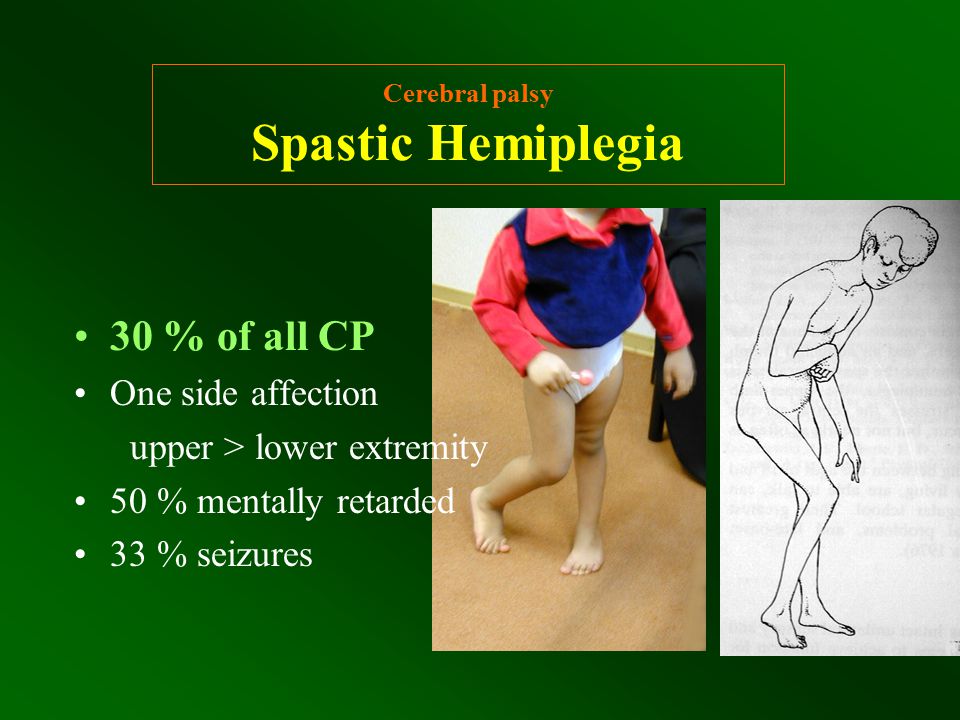
- Pathological conditions - torticollis, or torticollis - shortening of the muscles of the neck on one side, other neuromuscular diseases.
Previously, the disease was diagnosed less frequently - due to the fact that pediatricians recommended laying newborns on their side. To date, it has been proven that this position increases the risk of sudden infant death syndrome in a dream, therefore, since 1992, it has been recommended to lay children on their backs during sleep, which becomes a frequent cause of deformation of the skull bones that have not yet been fully formed.
Types of plagiocephaly in children
According to etiological types, plagiocephaly is distinguished:
- Positional - acquired, caused by mechanical deformations - intrauterine or perinatal. Occurs in the vast majority of cases. Source:
https://www.ncbi.nlm.nih.gov/pubmed/25382999
Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R
Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging
// Pediatric Child Health. 2014 Oct;19(8):423-7 - Deformation - due to congenital diseases - progressive deformity due to early fusion of the cranial bones. It occurs extremely rarely - in 1 out of 2,000 patients. Source:
https://www.ncbi.nlm.nih.gov/pubmed/30151193
Renz-Polster H, De Bock
Deformational plagiocephaly: The case for an evolutionary mismatch
// Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.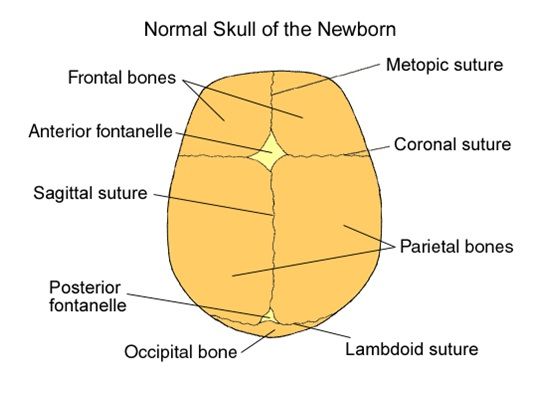 1093/emph/eoy019. eCollection 2018
1093/emph/eoy019. eCollection 2018
According to localization, it happens:
- frontal;
- occipital;
- side.
Signs of disease
Atypical skull shape - flattened in the occipital region. Rarely - elongated in the frontal direction or squeezed from the sides. Characteristic frontal or temporal bulges, protrusions of the parietal region are possible.
If the asymmetry of the head is caused by congenital anomalies, then without treatment, the pathology progresses. Over time, it can cause negative consequences in a child - increased intracranial pressure and the symptoms caused by it . Source:
E.V. Mammadov
Plagiocephaly. II. Synostotic, deformation and compensatory
// Children's surgery, 2003, No. 5, p. 45-50
Diagnosis of plagiocephaly in a child
In accordance with modern recommendations, the diagnosis is made on the basis of a clinical examination.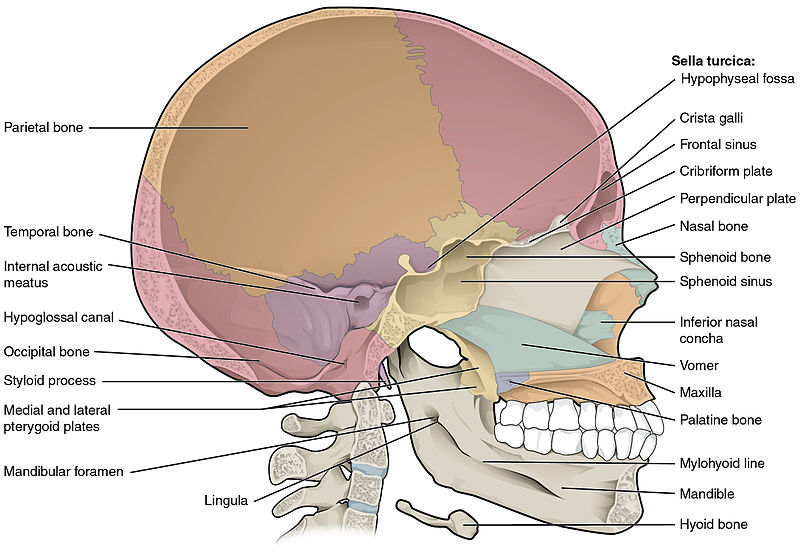 For differential diagnosis - identifying the cause of the pathology - ultrasound, radiography or CT of the skull are optionally prescribed.
For differential diagnosis - identifying the cause of the pathology - ultrasound, radiography or CT of the skull are optionally prescribed.
Methods of treatment
The main treatment for positional plagiocephaly in infants is the reposition method : multiple changes in body position during the day. The child should lie on his back as little as possible when he is awake. Minimize wearing in a sling and carrier, transport in a car seat. An effective technique is to change the position of the child relative to the light source (stimulates turning over).
Children over 7 weeks of age also need exercise therapy. It is aimed at:
- stimulation of motor development and correction of positional preferences;
- stretching of the neck muscles with torticollis - an increase in the range of motion in the cervical spine.
Includes laying out the child on the stomach during wakefulness under the supervision of adults.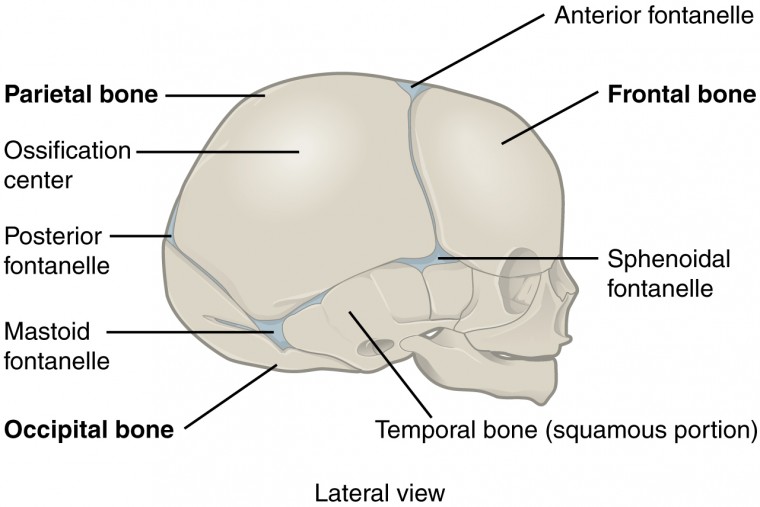
With moderate and severe deformities, as well as with the ineffectiveness of conservative treatment, orthotics are indicated - helmet therapy. The orthosis is made according to individual measurements in an orthopedic workshop. The child wears it 23 hours a day until it heals or needs to change the size of the helmet.
Conservative treatment and orthotics last for several months. The bones of the skull gradually assume a physiological position, while no damage is done to the brain, and neurological diseases do not develop.
If the deformity is due to a congenital anomaly, surgery is indicated. As a rule, it is done at the age of ~7-9 years. The use of orthopedic pillows for newborns is contraindicated, as they sometimes cause infant death.
Sources:
- https://www.ncbi.nlm.nih.gov/pubmed/25382999 Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging // Paediatr child health.
 2014 Oct;19(8):423-7.
2014 Oct;19(8):423-7. - https://www.ncbi.nlm.nih.gov/pubmed/30151193 Renz-Polster H, De Bock. Deformational plagiocephaly: The case for an evolutionary mismatch // Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2018.
- E.V. Mammadov. Plagiocephaly. II. Synostotic, deformation and compensatory // Children's surgery, 2003, No. 5, pp. 45-50.
The information in this article is provided for reference only and does not replace the advice of a qualified professional. Do not self-medicate! At the first signs of the disease, you should consult a doctor.
All pediatric osteopaths
- All doctors
- Malaya Balkanskaya, 23
- Udarnikov, 19k1
Make an appointment
Registration through the site is preliminary.
Our employee will contact you to confirm the appointment with a specialist.
Set time
Time9:009:3010:0010:3011:0011:3012:0012:3013:0013:3014:0014:3015:0015:3016:0016:3017:0017:3018:0018:3019:0019:3020: 0020:3021:0021:30
Specify specialist
Specialist-I don’t know-a pediatrician, allergists of the Gastroenter gynecologist of the dermatologist Immunology, Cardiology Logo-Pedious Neurological Department of the Oncology, Orthraded Orthraded Pulmonology Dermon, Uribid, Rhubate Department of the Rheumen Dermon, Uztoditsky Endo-Dermon, Uztodetsky Endo-Dermon, Uribided EndoD.