Neg blood type
O negative blood type - NHS Blood Donation
Your blood type is determined by genes inherited from your parents.
Whether your blood type is rare, common or somewhere in between, your donations are vital in helping save and improve lives.
You can register online to give blood.
How rare is O negative blood?
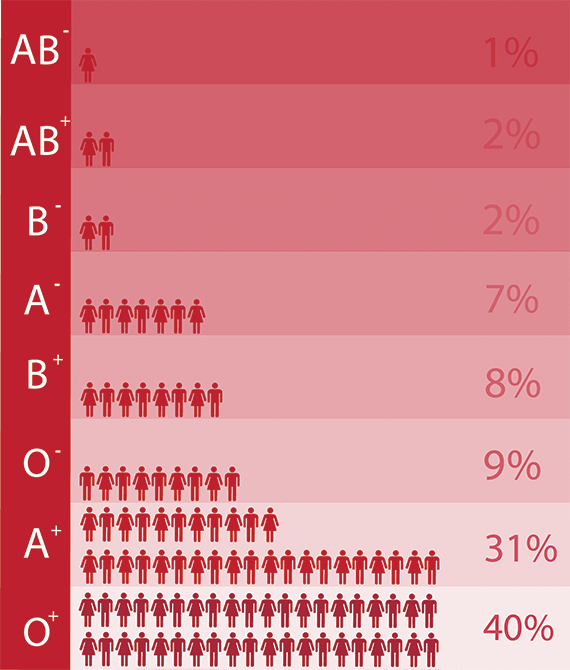
Around 1 in 7 people have O negative blood
Around 13% of our blood donors have O negative blood.
In comparison, 35% of donors have O positive blood.
Air ambulances and emergency response vehicles carry O negative supplies for emergencies. Collecting enough O negative blood is a constant challenge and we always need your donations.
Are you O negative?
As an O negative donor you are the lifeblood of the emergency services. You are a First Responder.
Find out more
Who can receive O negative blood?
Everyone can receive O negative red blood cells
O negative donors are often called ‘universal donors’ because anyone can receive the red blood cells from their donations.
Although about 8% of the population has O negative blood, it accounts for around 13% of hospital requests for red blood cells.
What blood can O negative people receive?
Only O negative blood
People with O negative blood can only receive red cell donations from O negative donors.
Why is O negative blood important?
It’s used in emergencies
O negative blood is often called the ‘universal blood type’ because people of any blood type can receive it.
This makes it vitally important in an emergency or when a patient’s blood type is unknown.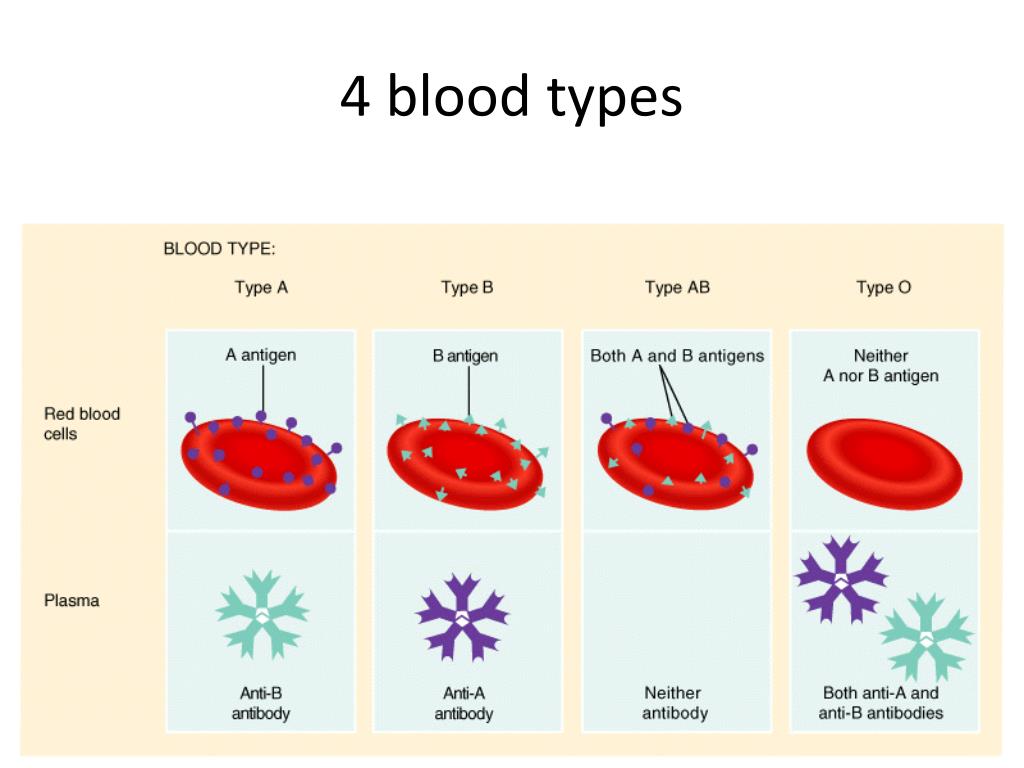
Coronavirus information
Register
Become a blood donor
Register
More information about the different blood types that provide a lifeline to all kinds of patients
Blood types O positive O negative A positive A negative B positive B negative AB positive AB negative Rare blood types Ro subtype
Blood type materials
Cards and fact sheets about different blood types to download and share
View materials
Blood Types Explained - A, B, AB and O
How Blood Type Is Determined And Why You Need To Know
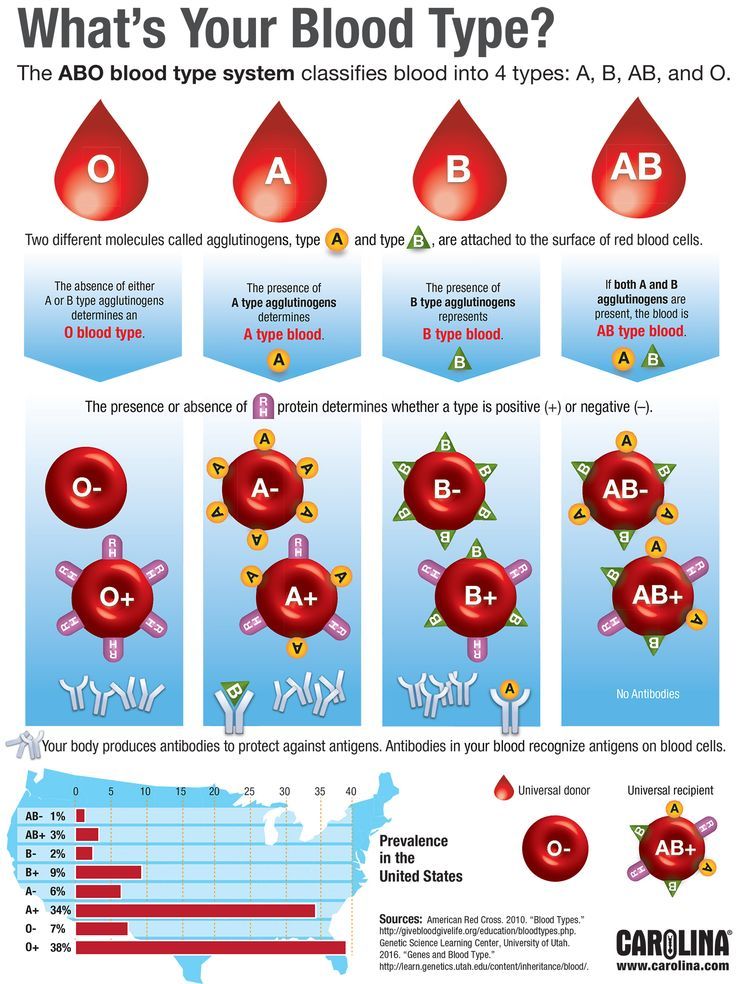
Blood types are determined by the presence or absence of certain antigens – substances that can trigger an immune response if they are foreign to the body.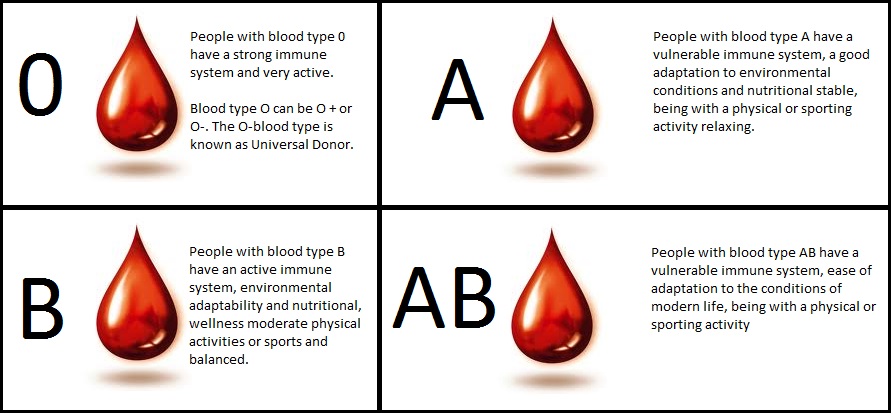 Since some antigens can trigger a patient's immune system to attack the transfused blood, safe blood transfusions depend on careful blood typing and cross-matching. Do you know what blood type is safe for you if you need a transfusion?
Since some antigens can trigger a patient's immune system to attack the transfused blood, safe blood transfusions depend on careful blood typing and cross-matching. Do you know what blood type is safe for you if you need a transfusion?
Discover what blood types are compatible with yours.
Get our guide to find out.
Download Guide
There are four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells. In addition to the A and B antigens, there is a protein called the Rh factor, which can be either present (+) or absent (–), creating the 8 most common blood types (A+, A-, B+, B-, O+, O-, AB+, AB-).
",xd="",yd="
",zd="",Ad='
There are very specific ways in which blood types must be matched for a safe transfusion. The right blood transfusion can mean the difference between life and death. Use the interactive graphic below to learn more about matching blood types for transfusions.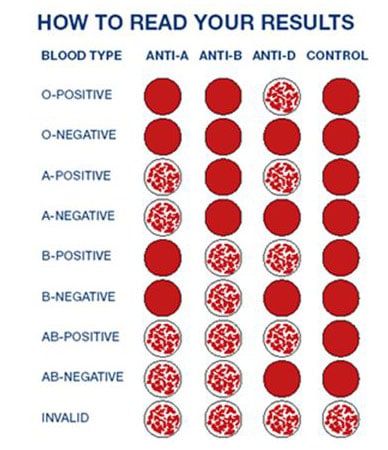
Also, Rh-negative blood is given to Rh-negative patients, and Rh-positive or Rh-negative blood may be given to Rh-positive patients. The rules for plasma are the reverse.
- The universal red cell donor has Type O negative blood.
- The universal plasma donor has Type AB blood.
There are more than 600 other known antigens, the presence or absence of which creates "rare blood types." Certain blood types are unique to specific ethnic or racial groups. That’s why an African-American blood donation may be the best hope for the needs of patients with sickle cell disease, many of whom are of African descent. Learn about blood and diversity.
Universal donors are those with an O negative blood type. Why? O negative blood can be used in transfusions for any blood type.
Type O is routinely in short supply and in high demand by hospitals – both because it is the most common blood type and because type O negative blood is the universal blood type needed for emergency transfusions and for immune deficient infants.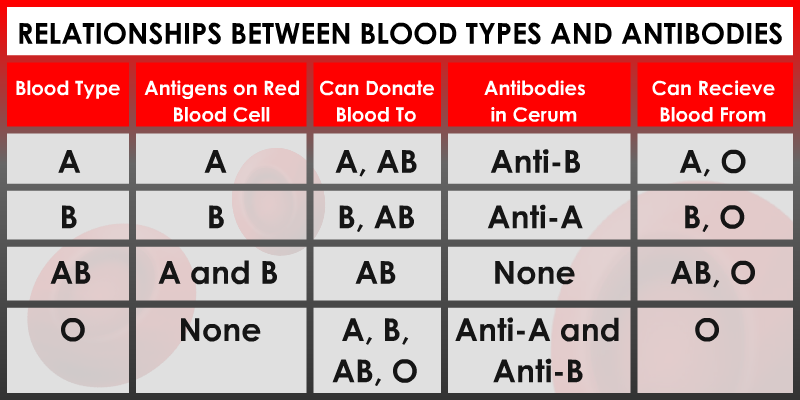
Approximately 45 percent of Caucasians are type O (positive or negative), but 51 percent of African-Americans and 57 percent of Hispanics are type O. Minority and diverse populations, therefore, play a critical role in meeting the constant need for blood.
Types O negative and O positive are in high demand. Only 7% of the population are O negative. However, the need for O negative blood is the highest because it is used most often during emergencies. The need for O+ is high because it is the most frequently occurring blood type (37% of the population).
The universal red cell donor has Type O negative blood. The universal plasma donor has Type AB blood. For more about plasma donation, visit the plasma donation facts.
Nearly 16 million blood components are transfused each year in the U.S."
What is your blood type? Donate and find out.
Schedule Your Appointment
There are more than 600 other known antigens, the presence or absence of which creates "rare blood types.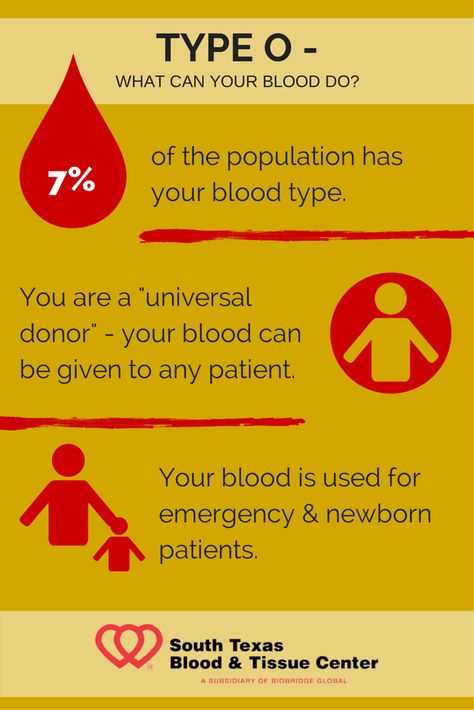 " Your blood type is considered rare if you lack antigens that 99% of the people are positive for. If you somehow lack an antigen that 99.99% are positive for, your blood type is extremely rare.
" Your blood type is considered rare if you lack antigens that 99% of the people are positive for. If you somehow lack an antigen that 99.99% are positive for, your blood type is extremely rare.
It’s inherited. Like eye color, blood type is passed genetically from your parents. Whether your blood group is type A, B, AB or O is based on the blood types of your mother and father.
View all child parent pairings
* Note: If you have questions about paternity testing or about blood group inheritance, your primary care physician should be able to provide you with an appropriate referral. Testing difficulties can cause exceptions to the above patterns. ABO blood typing is not sufficient to prove or disprove paternity or maternity.
Make Your Appointment
About Blood Types - Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood type and your Rh (rhesus factor).
A person's blood group is determined by antigens found on his red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion.
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB. It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is present on the surface of erythrocytes
- group B - only antigen B is present on the surface of erythrocytes
- group AB - both A and B antigens are present on the surface of erythrocytes
- group O - on the surface of erythrocytes there is neither antigen A nor antigen B.
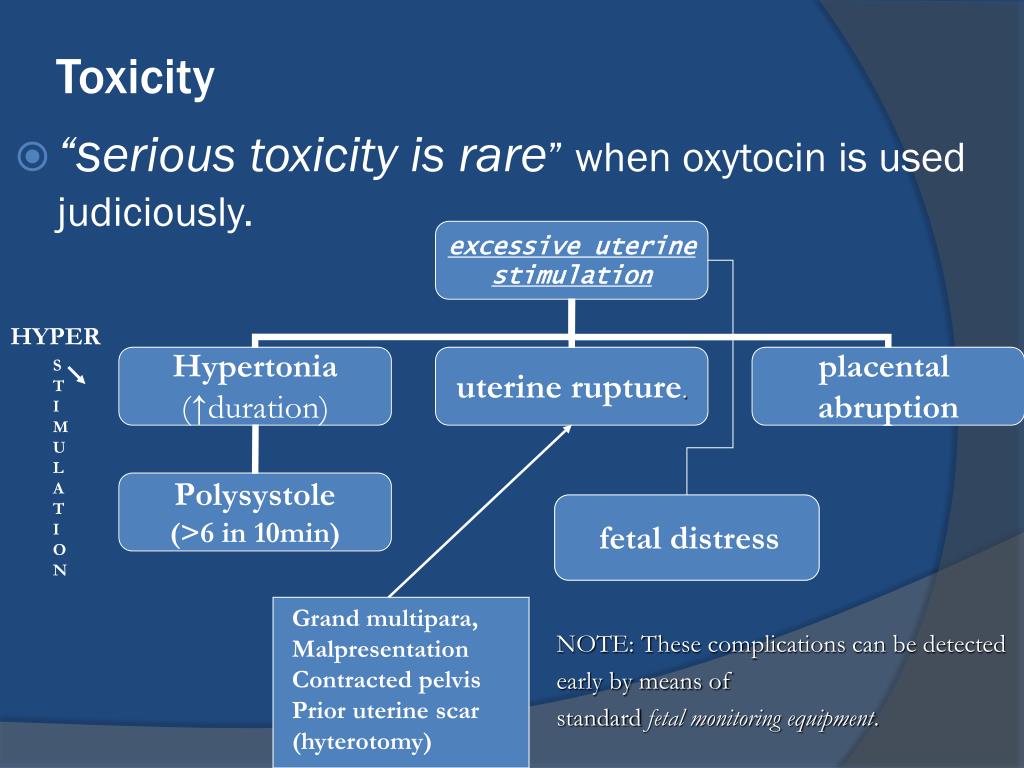
If a person has blood type A, B or 0, then in his blood plasma there are also antibodies that destroy those antigens that the person himself does not have. Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group. Therefore, the carrier of the AB blood group can be called universal patient.
A carrier of blood type 0 with a negative Rh factor, in turn, is called a universal donor, , since his red blood cells are suitable for all patients.
Rhesus (Rh ) accessory
Rh factor (Rh) can be positive (+) and negative (-). It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative.
It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative.
If a person is Rh negative, contact with Rh positive blood (for example, during pregnancy or blood transfusion) may form antibodies. These antibodies can cause pregnancy problems in an Rh-negative woman if she is carrying an Rh-positive baby.
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. According to the Kell system, donor blood is also examined.
How is the blood type determined?
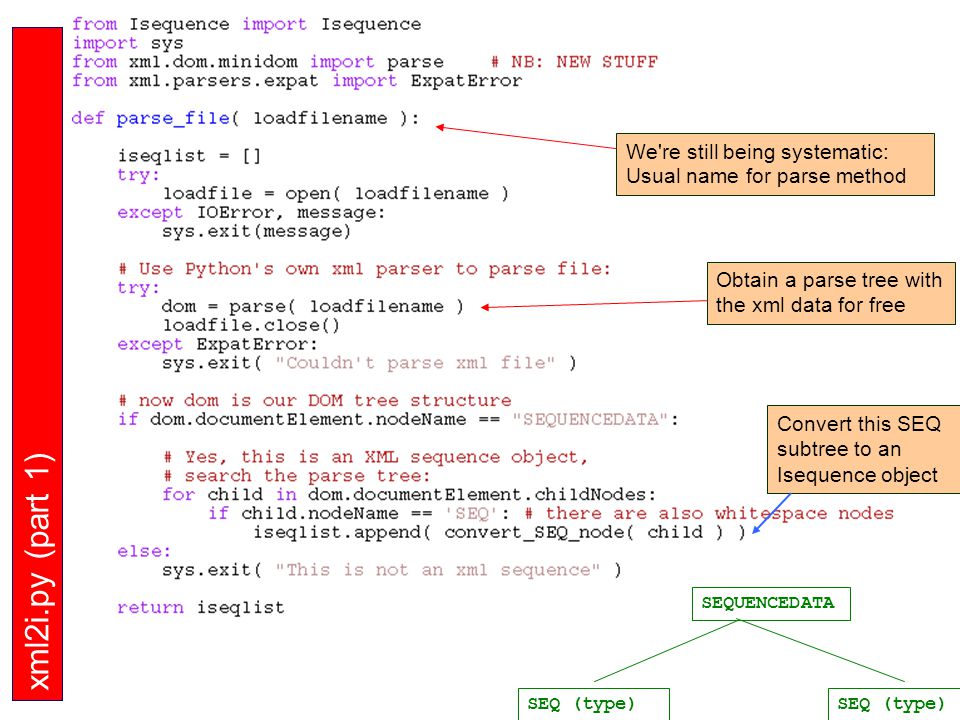
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent to the other, and the anti-D test reagent to the third, i.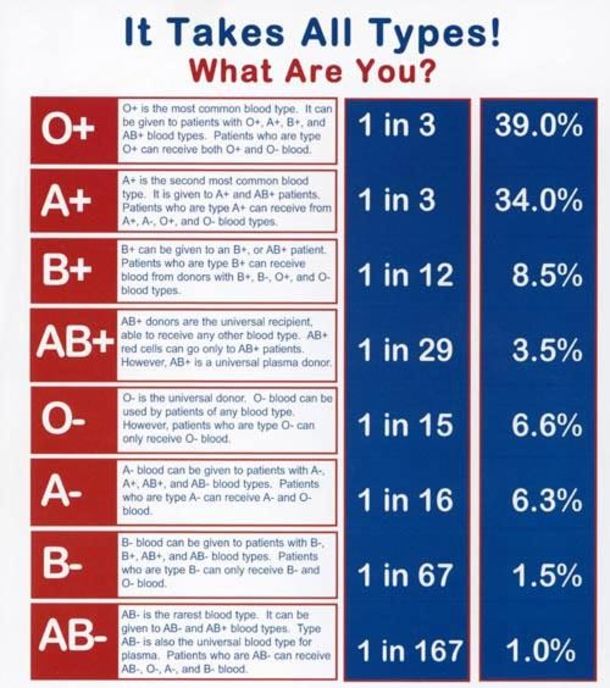 e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive.
e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive.
Donor and recipient blood group compatibility is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Inheritance of blood groups
A person inherits from his father and from his mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
- Most of our genes exist in two copies
- Each parent gives (based on a random selection) one of these copies to their children
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| ABO system | System Rh | |||||||||||||||||||||||||||||||||||||||||||
In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance consists of two parts, six different combinations can occur: Given that the hereditary substance consists of two parts, six different combinations can occur:
The stronger part appears, both equally or a combination. In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows:
Example: The mother has a combination of A0 genes in hereditary substance, and her blood type is A (at the same time, she is a carrier of the blood type 0 gene, and there is a possibility that she will pass it on to her child).
| In the Rh system, things are somewhat simpler, since there are only two options: the D antigen is either present (Rh positive) or absent (Rh negative). A positive Rh factor dominates a negative one.
Example: if the mother has Rh positive blood, and there is a hidden negative version, that is, the allele (+/-), and the father has exactly the same combination, and they both pass the negative allele, then two Rh-positive parents can have a child with a negative Rh factor.
| |||||||||||||||||||||||||||||||||||||||||||
Geneticist spoke about the importance of the blood Rh factor for health | Science news | Izvestia
The blood Rh factor matters when it comes to people's resistance to severe infections, the rate of aging and other important factors. On Wednesday, August 18, Irina Zhegulina, a leading geneticist, head of the educational direction of the Atlas biomedical holding, told Izvestiya.
Rh blood status, according to the specialist, is inherited from parents separately from the blood group. So, if a person has inherited the dominant Rh antigen D from one or both parents, then he is Rh-positive (85% of people are Rh-positive). If a person has not inherited the Rh antigen D from either parent, then he is Rh-negative (15% of such people).
“Over the past ten years, several studies have shown that Rh-positive and Rh-negative people differ in their resistance to severe parasitic infections, the rate of aging, fatigue and nicotine addiction. The results of another study, conducted mainly on a young population, show that diarrhea, thyroiditis, anemia, panic attacks were more common in people with RhD-negative status, ”said Zhegulina.
The results of another study, conducted mainly on a young population, show that diarrhea, thyroiditis, anemia, panic attacks were more common in people with RhD-negative status, ”said Zhegulina.
She also added that people with a negative Rh factor tolerate toxoplasmosis more easily. In addition, they may be more resistant to other viruses or parasites that science has not yet discovered, the doctor suggested.
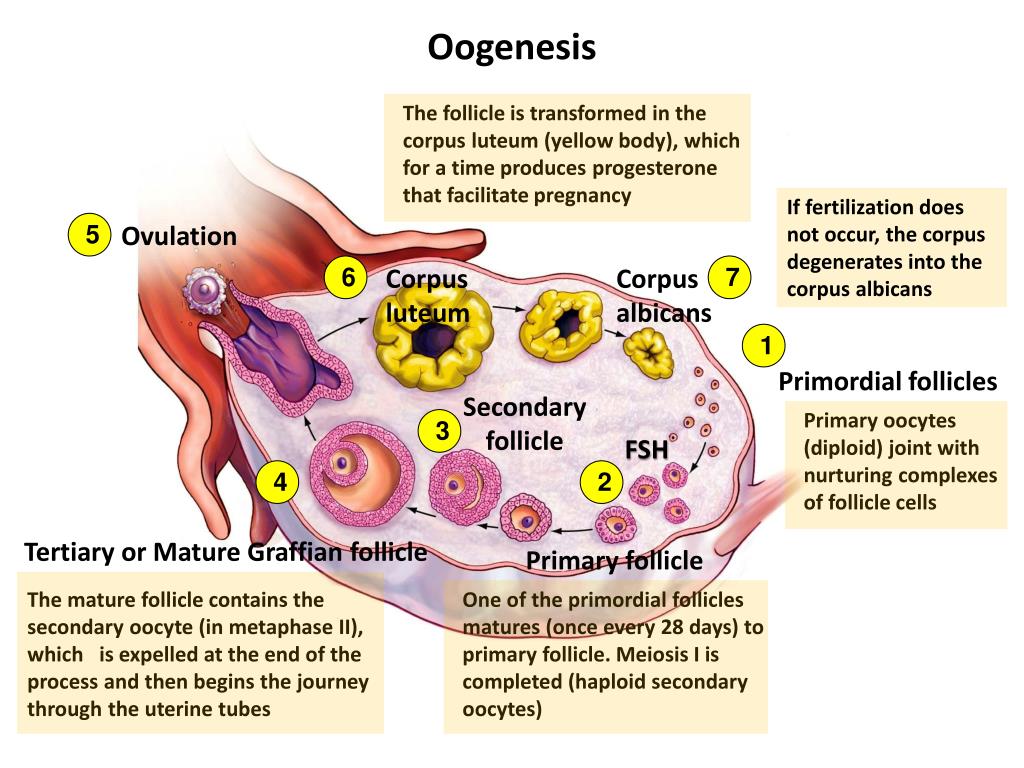
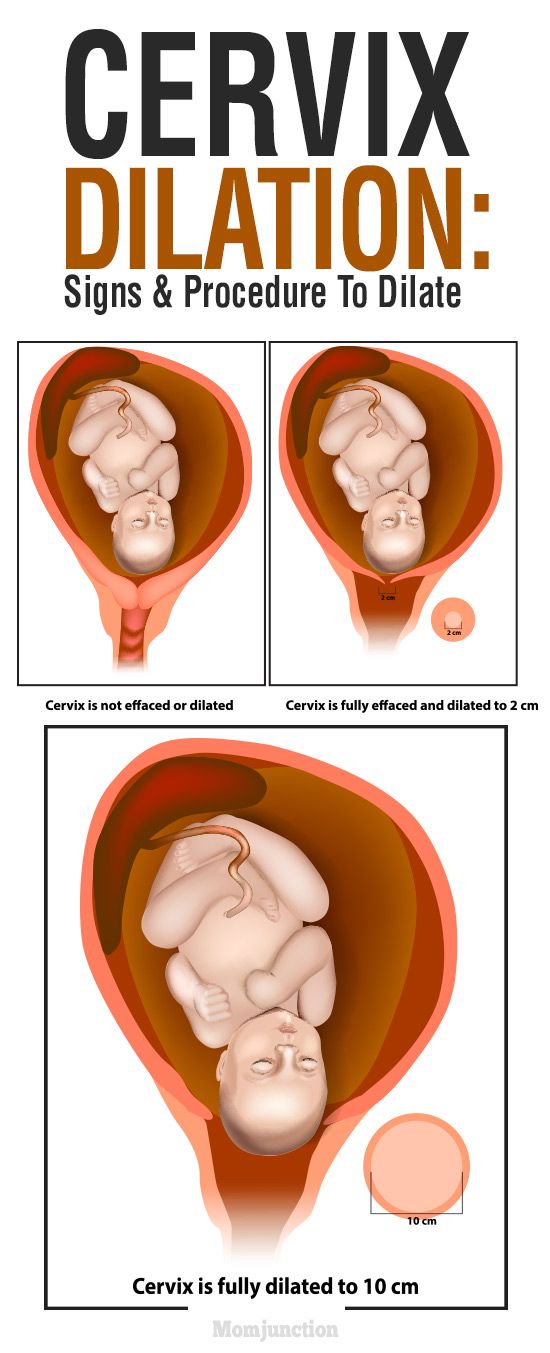
The Rh factor plays an important role during pregnancy. The geneticist explained that if a pregnant woman is Rh positive, it will not cause any health problems - regardless of whether the fetus is Rh negative or positive. At the same time, about half of all pregnant women with a negative Rh factor have a fetus with a negative Rh factor. That shouldn't be a problem either, because their blood is "compatible," Zhegulina clarifies.
“But if an Rh negative woman is expecting an Rh positive baby, the mother's blood can produce anti-D antibodies against the baby's Rh factor. This can happen if some of the baby's blood mixes with the mother's - for example, after minor injuries to the placenta or umbilical cord during childbirth. And it can happen during pregnancy, either without any external influence, or as a result of testing - such as amniotic fluid analysis, ”the specialist added.
This can happen if some of the baby's blood mixes with the mother's - for example, after minor injuries to the placenta or umbilical cord during childbirth. And it can happen during pregnancy, either without any external influence, or as a result of testing - such as amniotic fluid analysis, ”the specialist added.
Anti-D antibodies usually do not harm the baby if this is the woman's first pregnancy. However, in subsequent pregnancies, these antibodies can adversely affect the development of an Rh-positive baby, causing hemolytic disease of the newborn. In this case, the mother is given injections of anti-D immunoglobulin to stop the production of antibodies and reduce the risk of complications for the child, the doctor concluded.
On August 10, Dmitry Zlobin, a doctor at the SberHealth online medical service, told Izvestia about the importance of blood type for health. According to him, this indicator can influence the risks of developing diabetes or the tendency to infection.
 The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type.
The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type.