What is fetal distress
Fetal distress | Pregnancy Birth and Baby
Fetal distress | Pregnancy Birth and Baby beginning of content7-minute read
Listen
Key facts
- Fetal distress is a sign that your baby is not well.
- Your doctor or midwife will monitor your baby’s heartbeat during pregnancy and labour to assess their wellbeing.
- If your baby shows signs of fetal distress, your midwife or doctor will act quickly to try and treat any underlying cause.
- You may need help to birth your baby quickly with an assisted (instrumental) delivery or caesarean section.
- Fetal distress can increase the risk of birth complications, especially if it isn’t treated quickly.
If you are pregnant and notice a decrease in your baby’s movements, seek urgent medical attention. This may be a sign that your baby is unwell.
What is fetal distress?
Fetal distress is a sign that your baby is not well. It happens when the baby isn’t receiving enough oxygen through the placenta.
Fetal distress can sometimes happen during pregnancy, but it’s more common during labour.
What causes fetal distress?
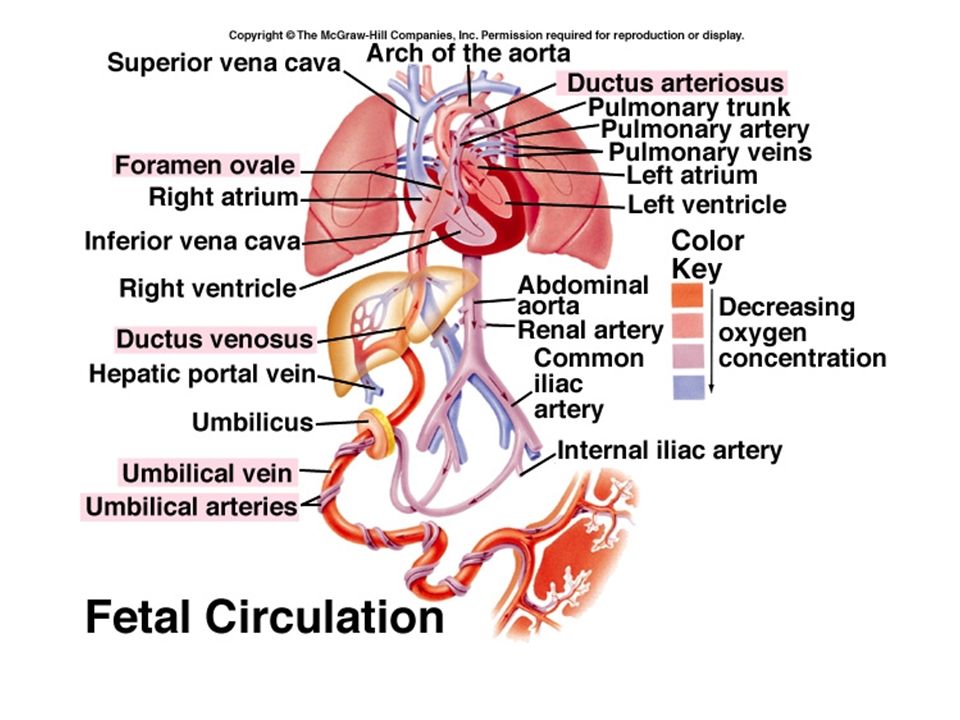
Fetal distress may occur when the baby doesn’t receive enough oxygen because of problems with the placenta (such as placental abruption or placental insufficiency) or problems with the umbilical cord (such as cord prolapse).
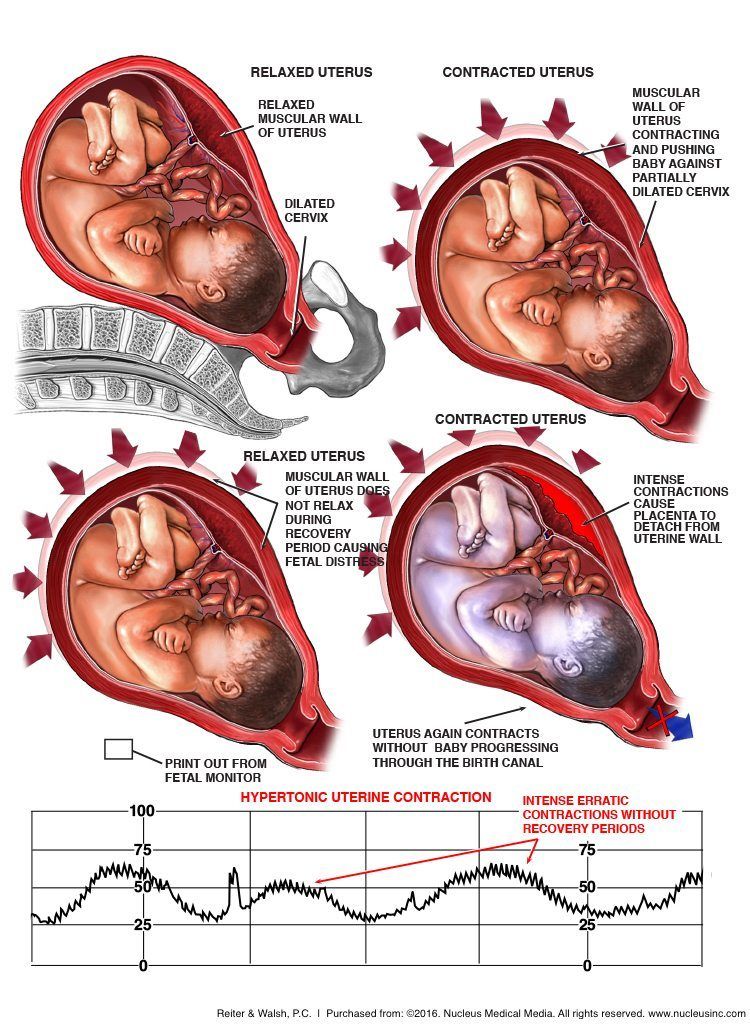
It is more common if you are overdue, have pregnancy complications or when there are other complications during labour. Sometimes it happens because the contractions are too strong or too close together.
Your baby is more likely to experience fetal distress if:
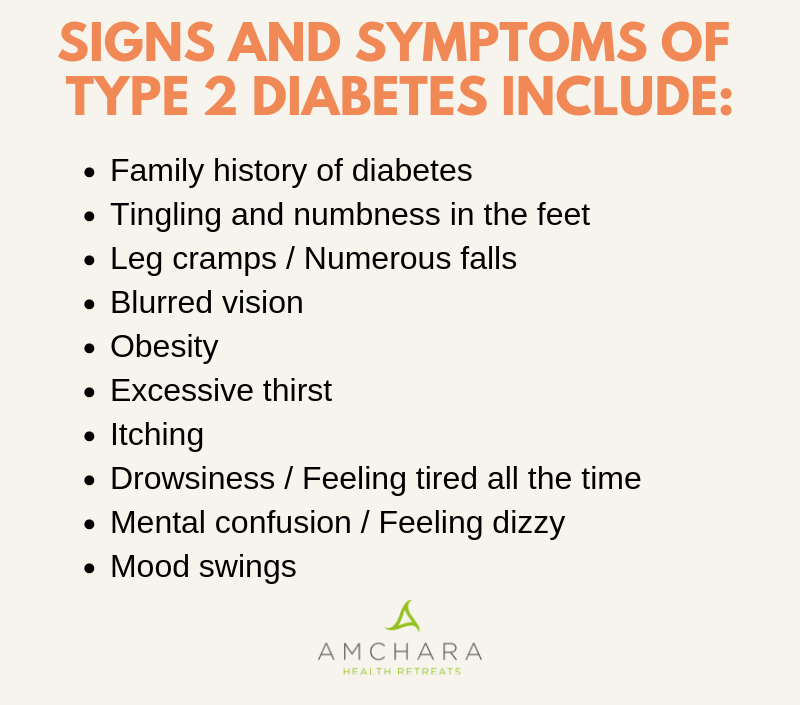
- you are obese
- you have high blood pressure in pregnancy or pre-eclampsia
- you have a chronic disease, such as diabetes, kidney disease or cholestasis(a condition that affects the liver in pregnancy)
- you have a multiple pregnancy
- your baby has fetal growth restriction
How is fetal distress diagnosed?
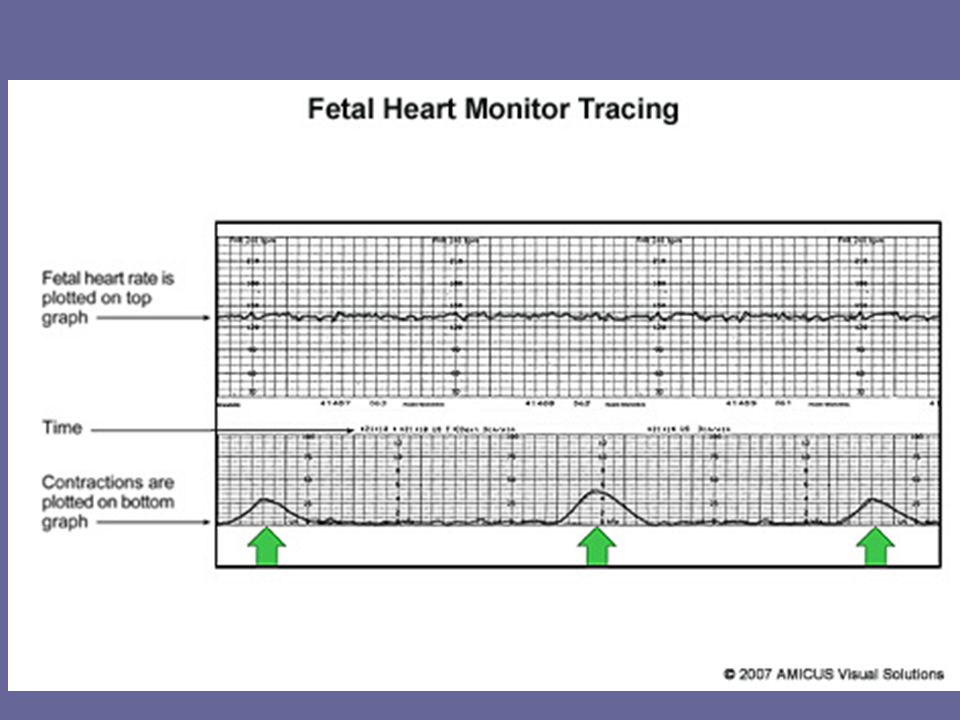
Fetal distress is diagnosed by monitoring the baby’s heart rate.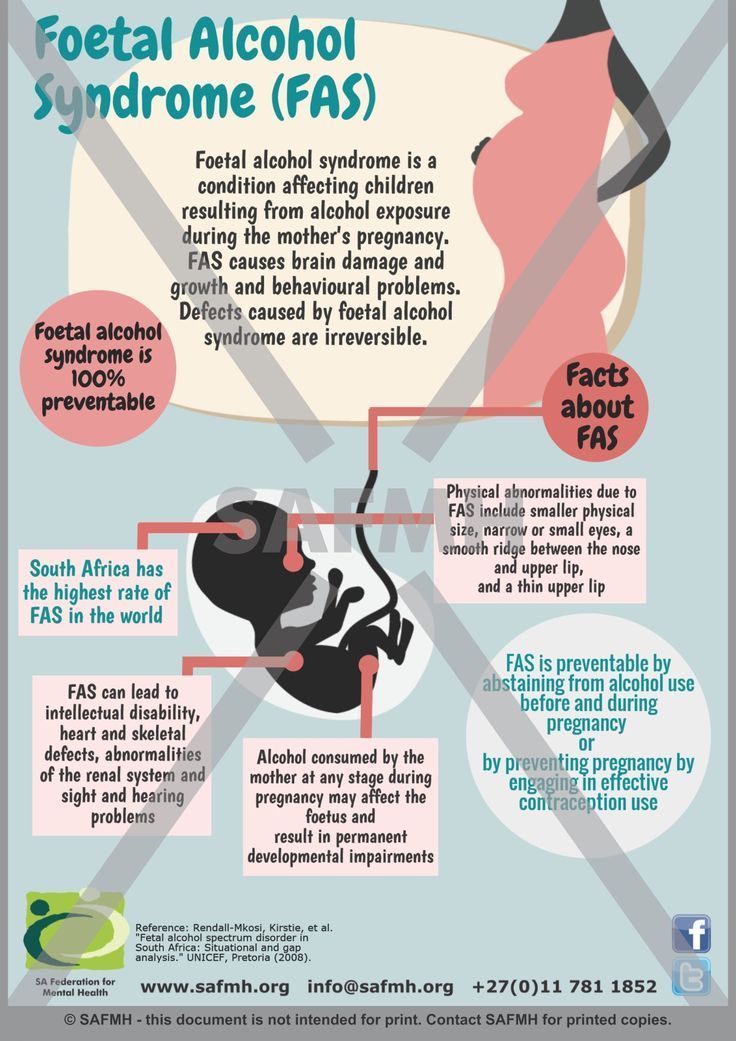 A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
Your doctor or midwife might pick up signs of fetal distress as they listen to your baby’s heart during pregnancy.
Your baby’s movements are a sign that your baby is well. A change in your baby’s movements may be a sign of fetal distress.
If you haven’t felt your baby move, or the pattern of moments has changed, contact your doctor or midwife immediately, as this may be a sign of fetal distress.
Another sign of possible fetal distress is meconium in the amniotic fluid. Let your doctor or midwife know right away if your notice your amniotic fluid is green or brown, since this could signal the presence of meconium (newborn poo, that your baby may pass while still in your uterus if they are distressed).
How is fetal distress managed?
There are a few ways that fetal distress may be managed. Your doctor will assess your situation and discuss with you the best management option in your situation.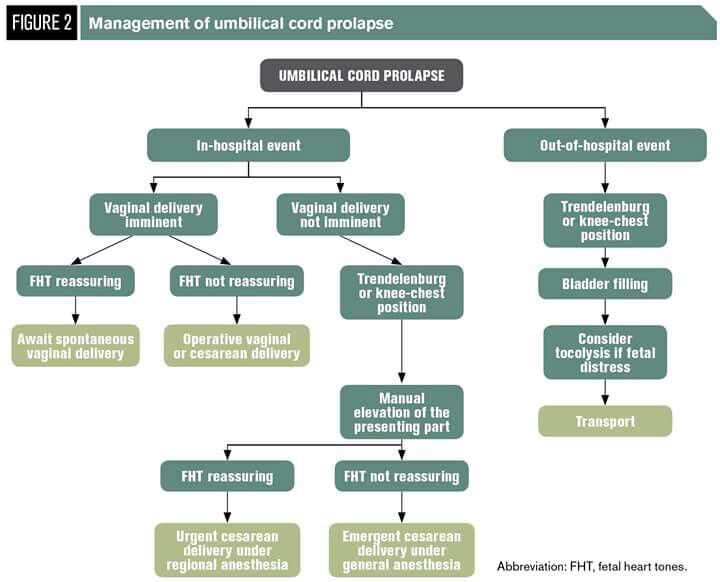
If you are not in labour
Depending on your situation, your doctor or midwife may recommend interventions such as medicines or intravenous fluids. If these interventions do not help, your doctor may recommend an emergency caesarean section so you birth your baby quickly.
If you are in labour
You will usually be given you oxygen and fluids. Sometimes changing position, such as turning onto your side, can reduce the baby’s distress.
You may be given medicine to slow down the contractions. If you had medicines to speed up labour, these may be stopped if there are signs of fetal distress.
Sometimes, a baby in fetal distress needs to be born quickly. Your doctor may recommend an assisted (or instrumental) birth or you might need to have an emergency caesarean.
Most of the time, there will be time to discuss your options with your doctor and/or midwife. However, in some emergency situations, your doctor or midwife will need to act quickly. If there are any medical interventions you object to, such as receiving a blood donation, it’s a good idea to make sure that your doctor and/or midwife are aware of this when you arrive at the hospital.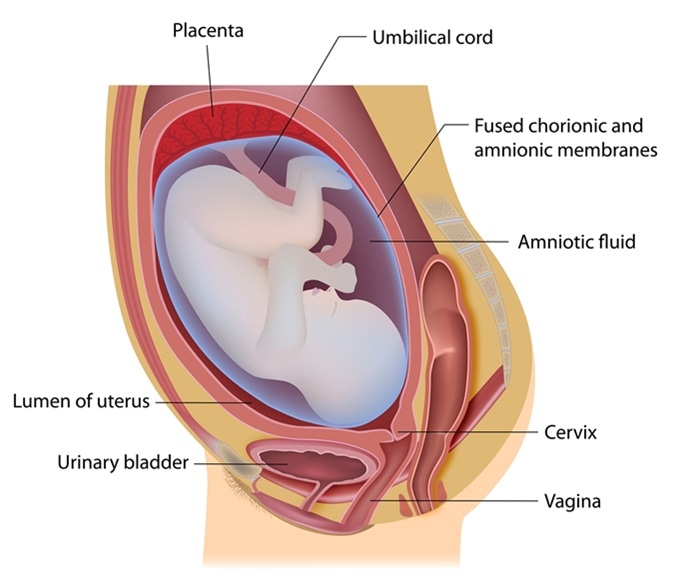
Does fetal distress have any lasting effects?
Babies who experience fetal distress are at greater risk of complications after birth. Prolonged lack of oxygen during pregnancy and birth can lead to serious complications for the baby, if it is not noticed and managed early. Complications may include brain injury, cerebral palsy and even stillbirth.
Fetal distress may require an assisted birth or caesarean section. While these interventions are safe, they are associated with their own set of risks and complications. Having fetal distress in one pregnancy doesn’t mean you will necessarily experience fetal distress in your next pregnancy. Every pregnancy is different. If you’re worried about future pregnancies, it can help to talk to your doctor or midwife so they can explain what happened before and during the birth.
Where can I find resources and support?
If your labour didn’t go to plan, you may experience difficult feelings about their birth experience.![]()
If you feel sad, disappointed or traumatised about what happened, it is important to talk to someone. There are lots of people and organisations who can help, including:
- your doctor
- PANDAon 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blueon 1300 22 4636
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australasian Birth Trauma Association (What is birth trauma?), King Edward Memorial Hospital (Fetal compromise (acute): Management if suspected), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Intrapartum fetal Surveillance Clinical Guideline)Learn more here about the development and quality assurance of healthdirect content.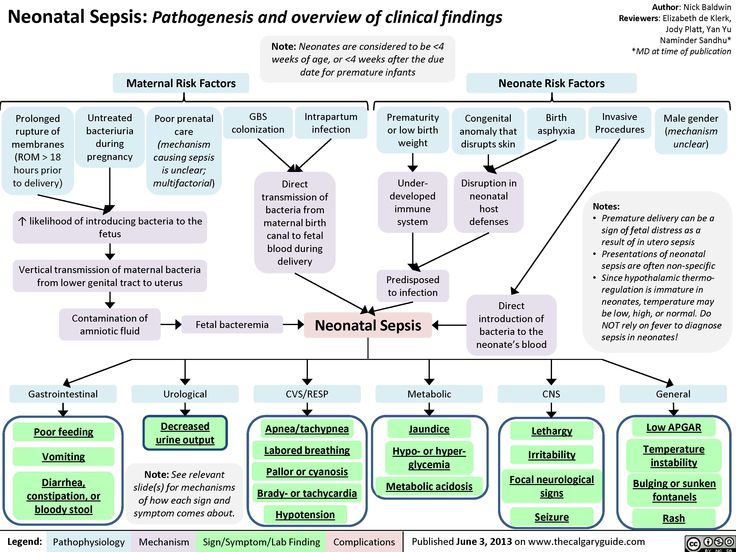
Last reviewed: July 2022
Back To Top
Related pages
- Baby movements during pregnancy
- Fetal heart rate monitoring
- Giving birth - stages of labour
- Induced labour
- Interventions during labour
- Labour complications
Need more information?
Fetal heart rate monitoring
During pregnancy and labour, your baby's heart rate is monitored to check for any signs of distress.
Read more on Pregnancy, Birth & Baby website
Monitoring the Baby’s Heart Rate in Labour
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Baby movements during pregnancy
Every baby is unique and it is important for you to get to know your baby’s movement patterns.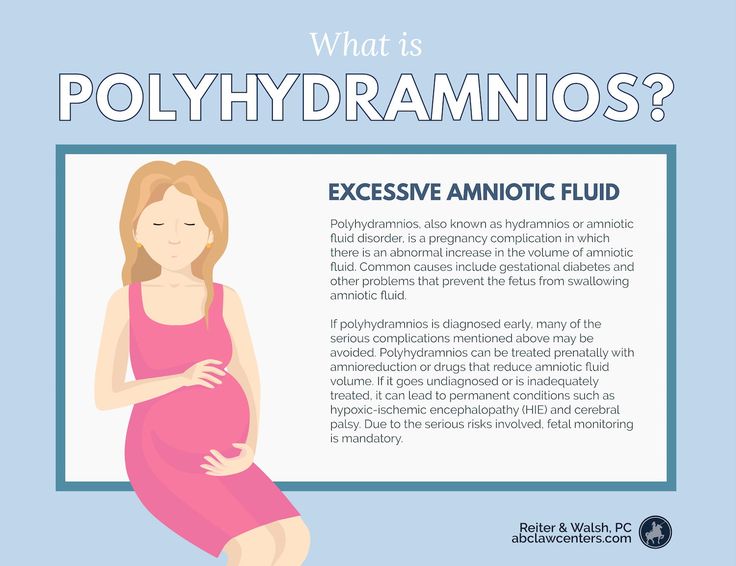
Read more on Pregnancy, Birth & Baby website
Heart abnormality birth defects - Better Health Channel
Some congenital heart defects are mild and cause no significant disturbance to the way the heart functions.
Read more on Better Health Channel website
Ultrasound scans during pregnancy
Ultrasound scans will help you and your doctors monitor your baby’s health throughout your pregnancy. Find out more, including about why you might need one.
Read more on Pregnancy, Birth & Baby website
External cephalic version (ECV)
ECV is a procedure to try to move your baby from a breech position to a head-down position.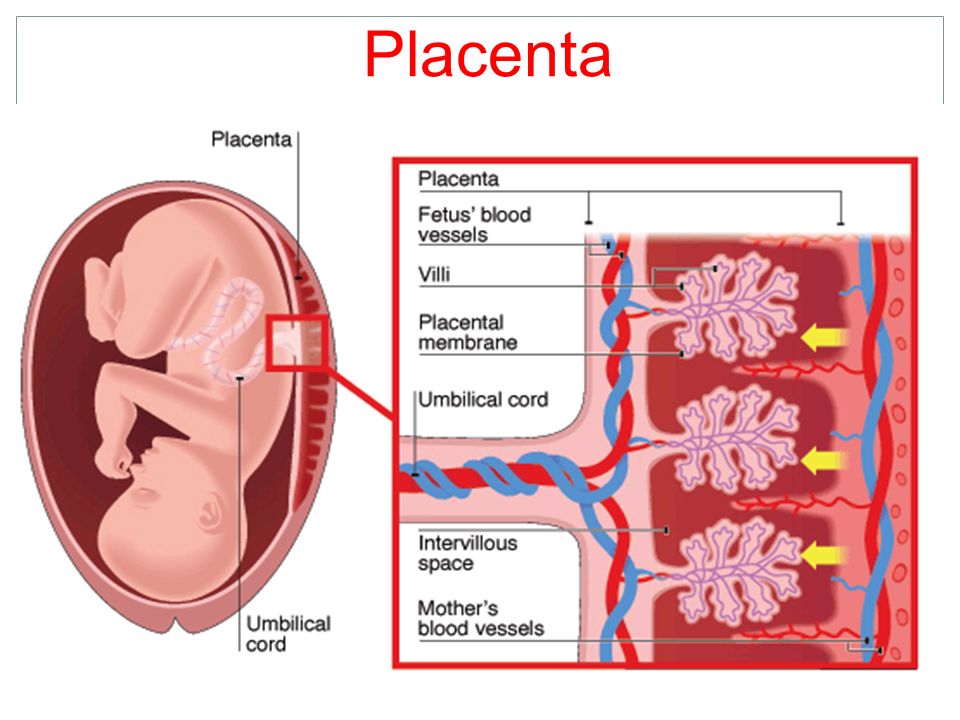 This is performed by a trained doctor.
This is performed by a trained doctor.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
Having a small baby
It's normal for parents to worry about their baby's birth weight and growth. Here’s what you need to know if you have been told your baby is likely to be small (less than 2.5kg at birth).
Read more on Pregnancy, Birth & Baby website
Baby due date - Better Health Channel
Pregnancy is calculated from the first day of your last period, not from the date of conception.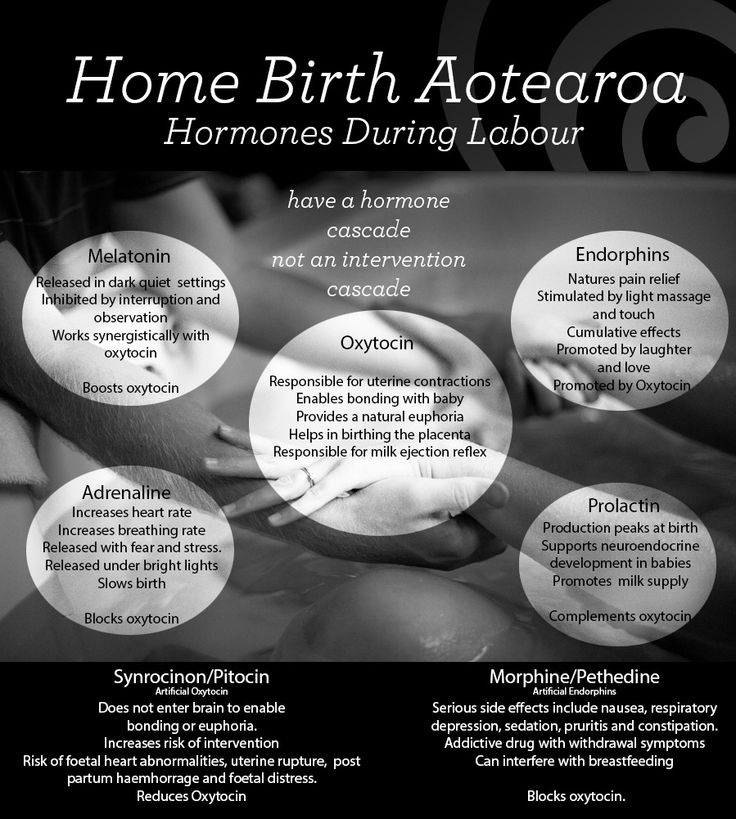
Read more on Better Health Channel website
Placental insufficiency
Find out about placental insufficiency - when the placenta does not work properly, and your baby doesn't get the oxygen and nutrients they need.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.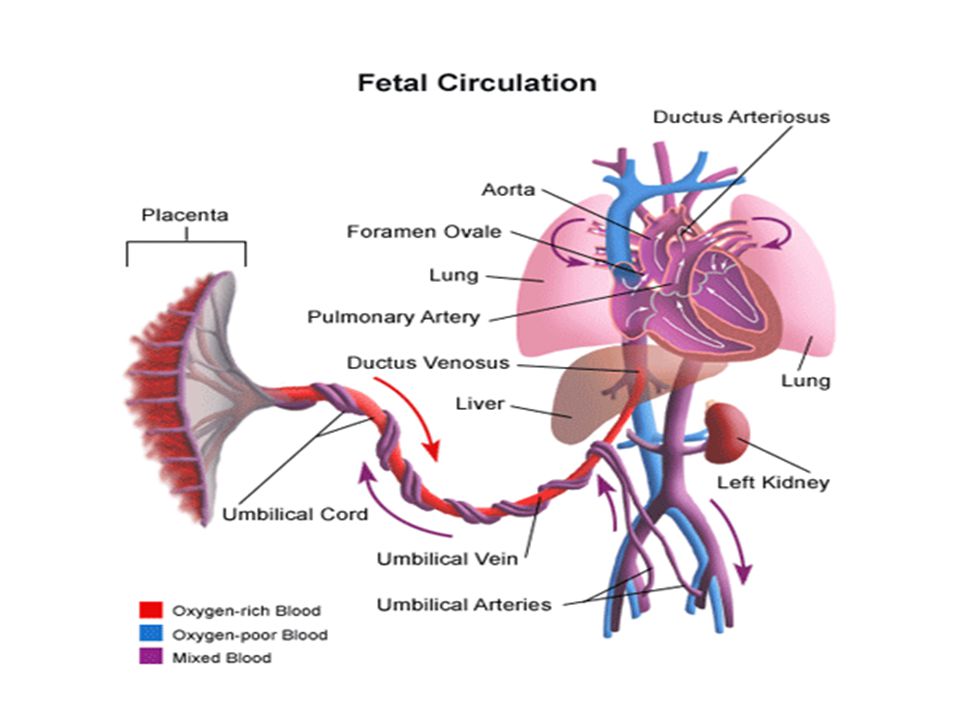 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fetal Distress - Women's Health Issues
By
Julie S. Moldenhauer
Moldenhauer
, MD, Children's Hospital of Philadelphia
Full review/revision Jul 2021 | Modified Sep 2022
VIEW PROFESSIONAL VERSION
GET THE QUICK FACTS
Fetal distress refers to signs before and during childbirth indicating that the fetus is not well.
Fetal distress is an uncommon complication of labor. It typically occurs when the fetus has not been receiving enough oxygen.
Fetal distress may occur when
The pregnancy lasts too long (postmaturity Postterm Pregnancy and Postmaturity A postterm pregnancy is one that lasts 42 weeks or more. In postmaturity, the placenta can no longer maintain a healthy environment for the fetus because the pregnancy has lasted too long.
 On... read more ).
On... read more ).Other complications of pregnancy or labor (such as difficult or rapid labor) occur.
Usually, doctors identify fetal distress based on an abnormal heart rate pattern in the fetus. Throughout labor, the fetus’s heart rate is monitored. It is usually monitored continuously with electronic fetal heart monitoring Fetal monitoring Labor is a series of rhythmic, progressive contractions of the uterus that gradually move the fetus through the lower part of the uterus (cervix) and birth canal (vagina) to the outside world... read more . Or a handheld Doppler ultrasound device may be used to check the heart rate every 15 minutes during early labor and after each contraction during late labor.
If a significant abnormality in the heart rate is detected, it can usually be corrected by the following:
Giving the woman oxygen
Increasing the amount of fluids given intravenously to the woman
Turning the woman on one side or the other
Did You Know.
 ..
..Contractions that are too strong and/or too close together may cause fetal distress. If oxytocin Induction of Labor was used to stimulate contractions, it is stopped immediately. The woman may be repositioned and given analgesics. If no drug was used to stimulate contractions, the woman may be given a drug that can slow labor (such as terbutaline, given by injection) to stop or slow the contractions.
If these measures to correct the fetus's heart rate or control contractions are not effective, the baby is delivered as quickly as possible by a vacuum extractor Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum. It is inserted... read more , forceps Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum.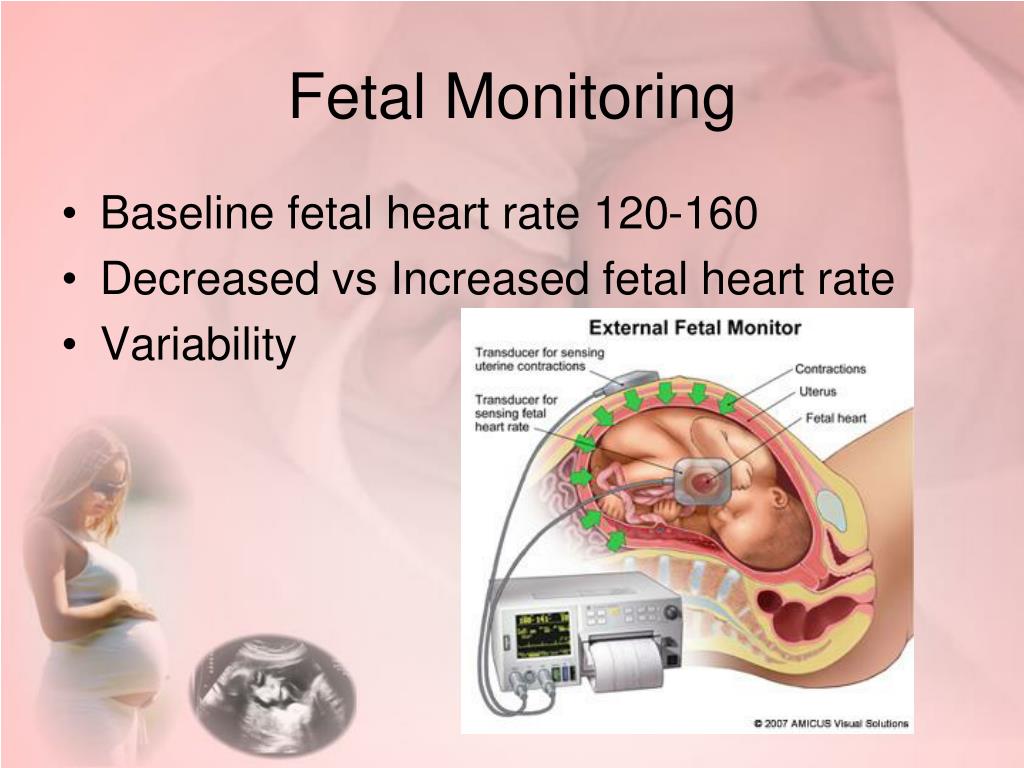 It is inserted... read more , or cesarean delivery Cesarean Delivery Cesarean delivery is surgical delivery of a baby by incision through a woman’s abdomen and uterus. In the United States, up to 30% of deliveries are cesarean. Doctors use a cesarean delivery... read more .
It is inserted... read more , or cesarean delivery Cesarean Delivery Cesarean delivery is surgical delivery of a baby by incision through a woman’s abdomen and uterus. In the United States, up to 30% of deliveries are cesarean. Doctors use a cesarean delivery... read more .
| Generic Name | Select Brand Names |
|---|---|
oxytocin |
Pitocin |
terbutaline |
Brethaire, Brethine |
VIEW PROFESSIONAL VERSION
Copyright © 2023 Merck & Co.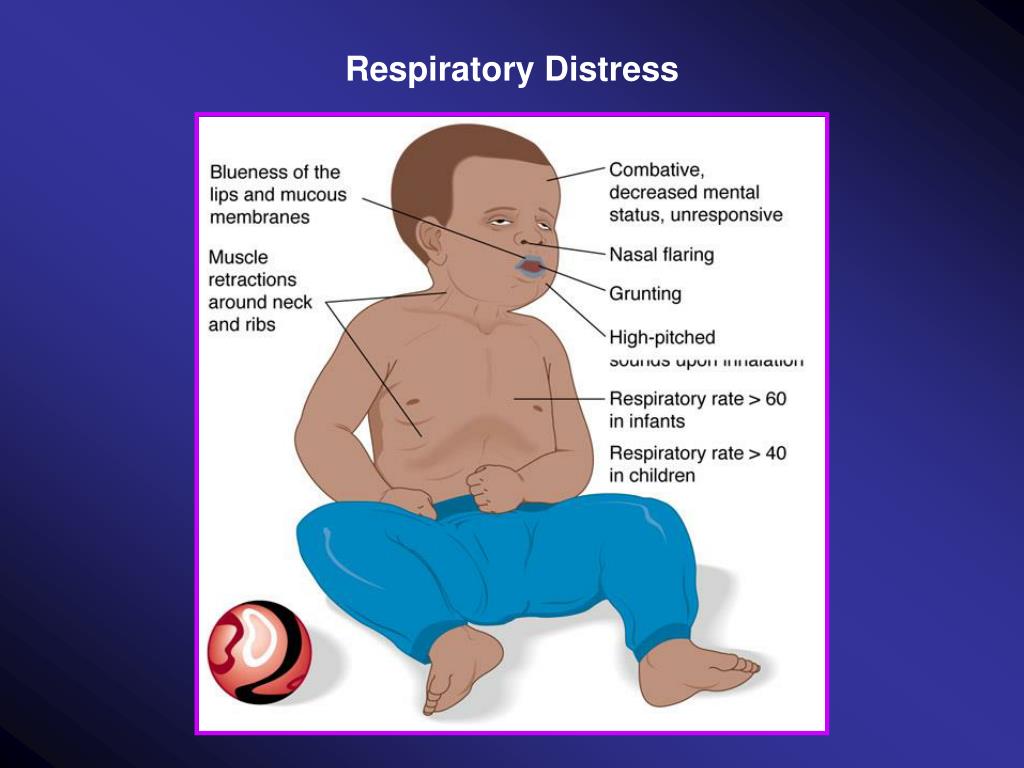 , Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
, Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Fetal distress - all you need to know about fetal distress
Sometimes at the last moment of pregnancy, unpleasant things happen that can be very sad. Fetal distress is one such complication that, if not addressed, can lead to problems for both the mother and the baby.
Fetal distress
Fetal distress is subdivided into intrauterine and birth distress. Distress is usually determined by monitoring the child's heart rate. The presence of meconium (the baby's first stool) may also indicate that the fetus is unwell in the womb.
Often referred to as hypoxia or threatened asphyxia, fetal distress occurs when an infant does not receive enough oxygen in the womb or during labor.
What causes fetal distress?
The reason why your unborn baby faces the problem of lack of oxygen can be different.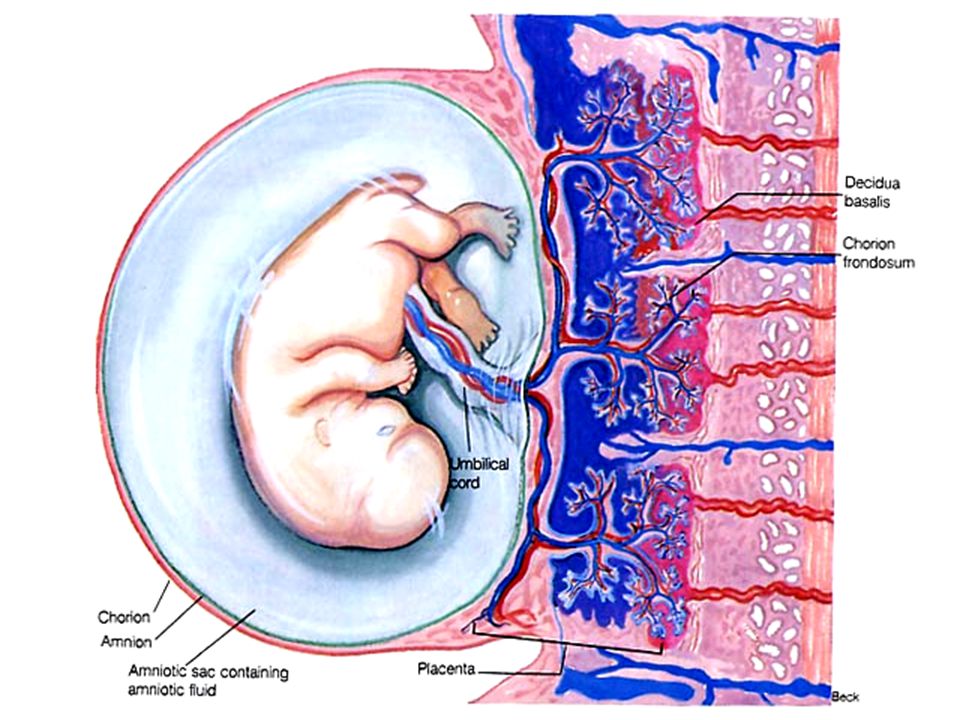 These could be umbilical cord problems, fetal abnormalities, the stress of childbirth, or reactions to certain medications. This can happen due to abnormal fetal development, problems with the placenta, or even multiple births.
These could be umbilical cord problems, fetal abnormalities, the stress of childbirth, or reactions to certain medications. This can happen due to abnormal fetal development, problems with the placenta, or even multiple births.
Fetal monitoring during labor
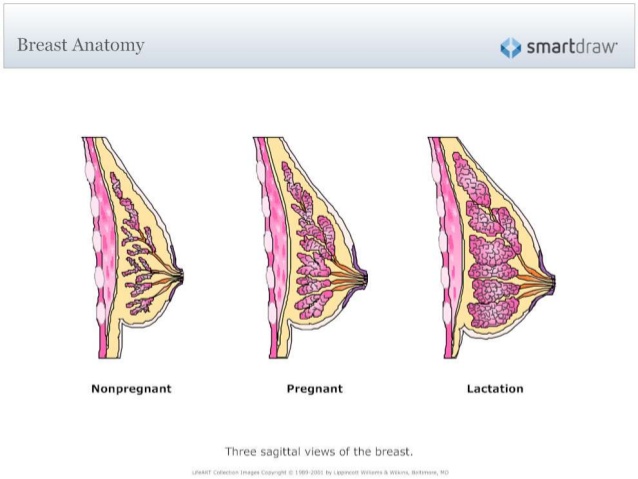
When a pregnant woman gives birth, the baby is constantly monitored. One of the most common methods for monitoring a baby is the use of an electronic fetal monitor (EFM). In this technique, two straps are wrapped around the abdomen, one measures the baby's heart rate, and the other assesses contractions or uterine activity. Monitors are also used to determine if the baby is having problems with each contraction.
For monitoring, doctors may also use a device that is applied to the baby's scalp.
What should be the ideal fetal heart rate?
The results of the electronic fetal monitor are shown on the monitor in diagrammatic form.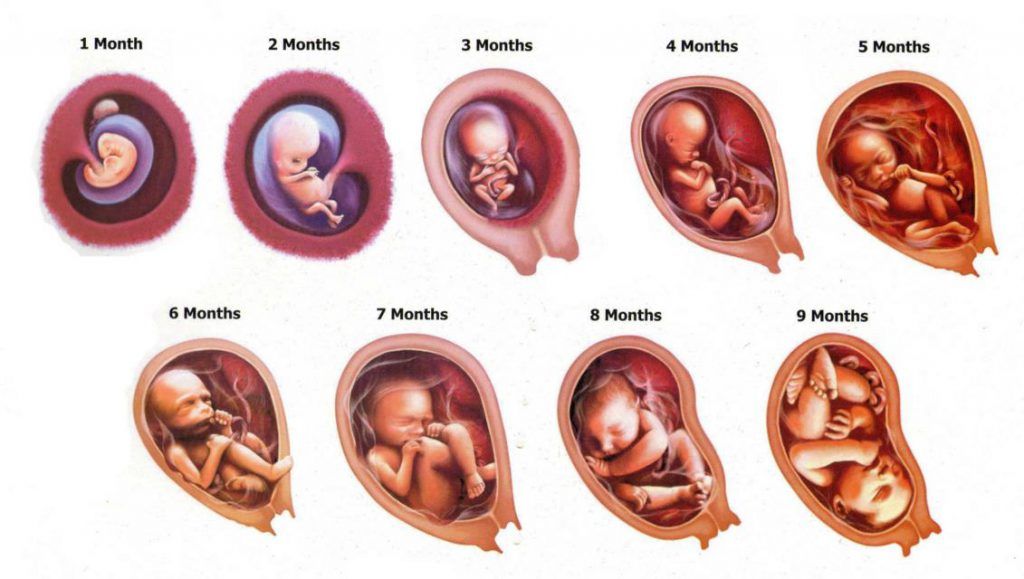 The doctor and nurses constantly monitor the numbers on the graphs and check if the heart rate is within adequate parameters. The ideal range should be between 110 and 160 beats per minute.
The doctor and nurses constantly monitor the numbers on the graphs and check if the heart rate is within adequate parameters. The ideal range should be between 110 and 160 beats per minute.
A temperature that is too high may indicate that the child is unwell or has a fever. While too low a temperature "speaks" of a lack of oxygen. Monitoring divides indications into 2 categories: accelerated heartbeat and slow heartbeat.
Rapid heartbeat
This means a short-term increase in heart rate, say 15 beats per minute, which can last 15 seconds or more. Accelerated, quite normal, it indicates an abundance of oxygen. For most babies, the heartbeat can speed up several times during the entire birth process.
If the doctor has any suspicions that the fetus is deteriorating, he may cause an increase in the fetal heart rate. Suspicion may arise from:
- Gently touching the mother's abdomen
- As a result of pressing the child's head, with a finger, through the cervix
Slow heart rate
Slow refers to temporary drops in heart rate.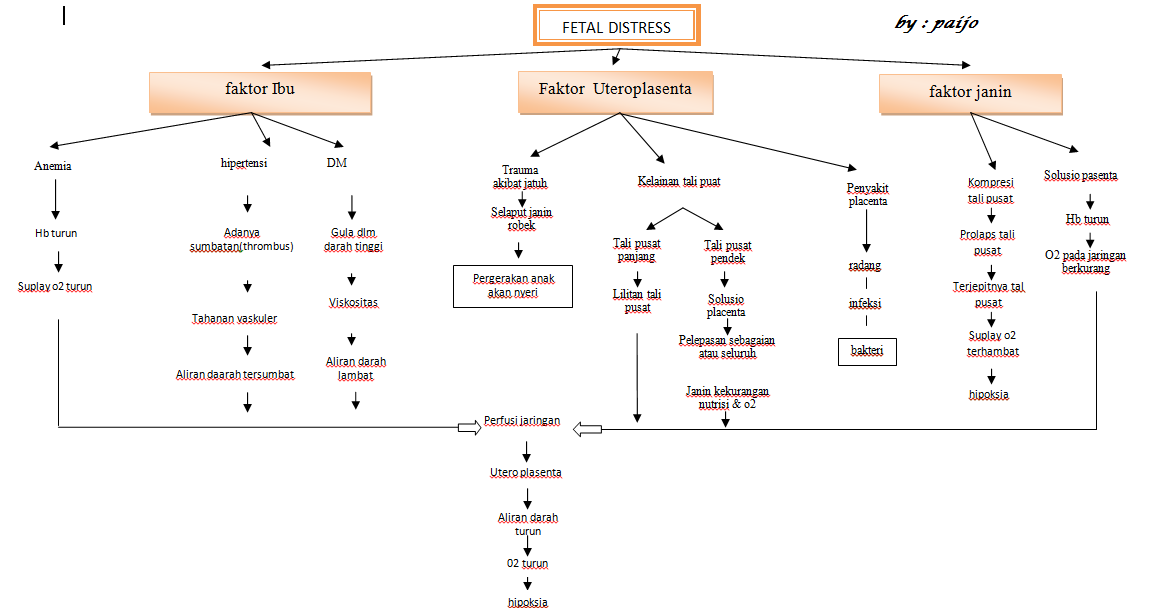 It can be divided into three types:
It can be divided into three types:
1. Early Deceleration
This is usually normal and nothing to worry about. Early deceleration occurs when the baby's head contracts. It mostly happens in the later stages of labor as the baby descends through the birth canal. Sometimes this happens during childbirth when the baby is premature or in a state of breech presentation.
2. Late Deceleration
They only happen when contractions are at their peak. Typically, late slows are smooth and shallow dips in heart rate that reflect the contraction that causes them. As long as the baby's heart rate shows an accelerated rhythm, late slowdowns are not a cause for concern. Late decelerations can also be a sign that the baby is not getting the amount of oxygen it needs.
3. Variable Deceleration
Variable decelerations are sudden dips in the fetal heart rate that can lead to serious consequences.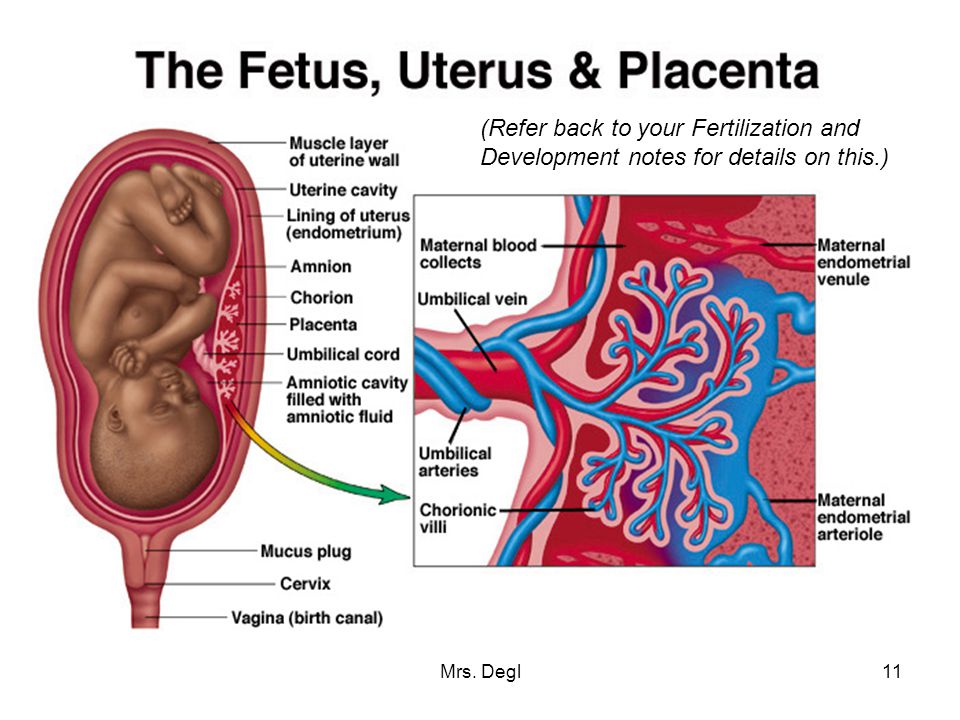 These slowdowns mostly occur during childbirth when the umbilical cord temporarily contracts, indicating a decrease in blood flow. Such variable changes in heart rate can be unsafe.
These slowdowns mostly occur during childbirth when the umbilical cord temporarily contracts, indicating a decrease in blood flow. Such variable changes in heart rate can be unsafe.
What to expect from a medical team?
In principle, the procedure for monitoring a child's heart rate is often painless. However, there are several risks associated with difficult birth situations that result in the medical team doing the following:
- Oxygen supply to mother
- Instillation of fluid into the amniotic sac to thicken the meconium (Amnioinfusion is the infusion of Ringer's solution or normal saline into the amniotic sac using a catheter.)
- Instrumentation (forceps/vacuum)
- Caesarean section
Before giving birth, be sure to consult with your doctor, ask him all the necessary and interesting questions. Get your medical card. And go to birth!!!
And remember, vigilance is the Key to a successful birth of your baby!!!
Fetal distress
The term "fetal distress" appeared in obstetric practice relatively recently.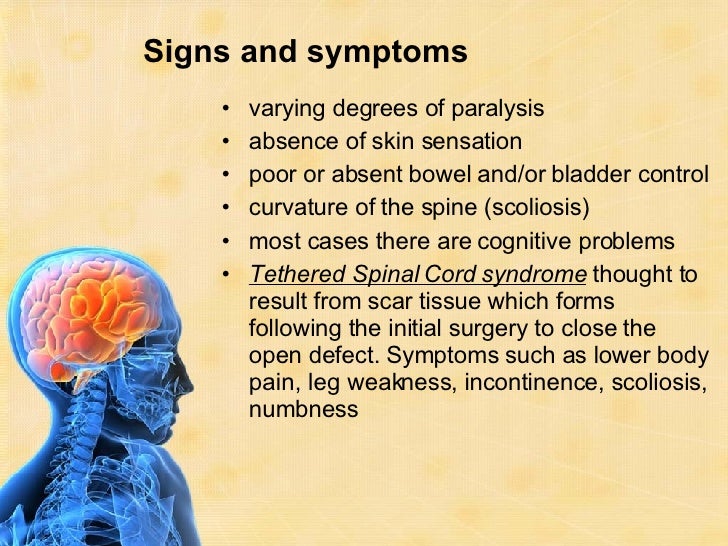 Fetal distress syndrome is spoken about in the presence of any changes in the functional state of the fetus, including acute and chronic intrauterine fetal hypoxia, and the threat of fetal asphyxia.
Fetal distress syndrome is spoken about in the presence of any changes in the functional state of the fetus, including acute and chronic intrauterine fetal hypoxia, and the threat of fetal asphyxia.
Fetal distress is most often manifested as hypoxia, which is a pathological physiological process. There are no symptoms that directly indicate that the child develops hypoxia. The baby's heartbeat does not directly indicate a lack of oxygen, the heart rate can also change reflexively.
If a pregnant woman has a suspicion of fetal distress, then she undergoes ultrasound, CTG, and other studies that evaluate the biophysical profile of the fetus.
Signs of distress also include tachycardia or a slow heartbeat, a decrease in the number of movements of the child, special reactions to contractions.
Types of fetal distress
According to the time of occurrence, fetal distress is divided into those that occur:
- during pregnancy;
- during childbirth.
Symptoms of distress can develop at any stage of pregnancy. The earlier the distress syndrome occurs, the worse it is for the fetus. In terms of prognosis, distress after 30 weeks of gestation is the safest, since an emergency caesarean section is possible.
If fetal distress occurs already in early pregnancy (eg, due to retrochorial hematoma), then this may well lead to malformations in the child, developmental disorders or miscarriage.
Antenatal fetal distress in the 2nd trimester can cause intrauterine growth retardation and subsequently lead to miscarriage, pregnancy failure, or premature birth.
Fetal distress during childbirth, especially in their second stage, is a serious obstetric problem, since it leads to an emergency caesarean section. In the event that the fetus in the uterus is already too low and fixed in the exit from the small pelvis, it is too late to resort to surgery. In this case, obstetricians speed up labor with vacuum extraction, perineotomy, and other methods that reduce the second stage of labor.
According to the severity of fetal suffering, distress is divided into:
- Distress in the stage of compensation - chronic distress, accompanied by hypoxia, developmental delay, lasts for several weeks.
- Distress in the stage of subcompensation - the presence of hypoxia, help is needed in the coming days.
- Distress in the stage of decompensation - the onset of intrauterine asphyxia, immediate assistance is required.
Sequelae of fetal distress
With timely intervention, the effects of distress are minimized. Otherwise, the child may die or be born in severe asphyxia, which cannot but affect his health in the future.
Related articles:
| Low placenta previa Low placenta previa - an unfavorable position in which the placenta is too close to the uterine os. But there is good news - with an increase in the gestational age, the placenta can migrate and rise to an acceptable height in the uterus before delivery. |