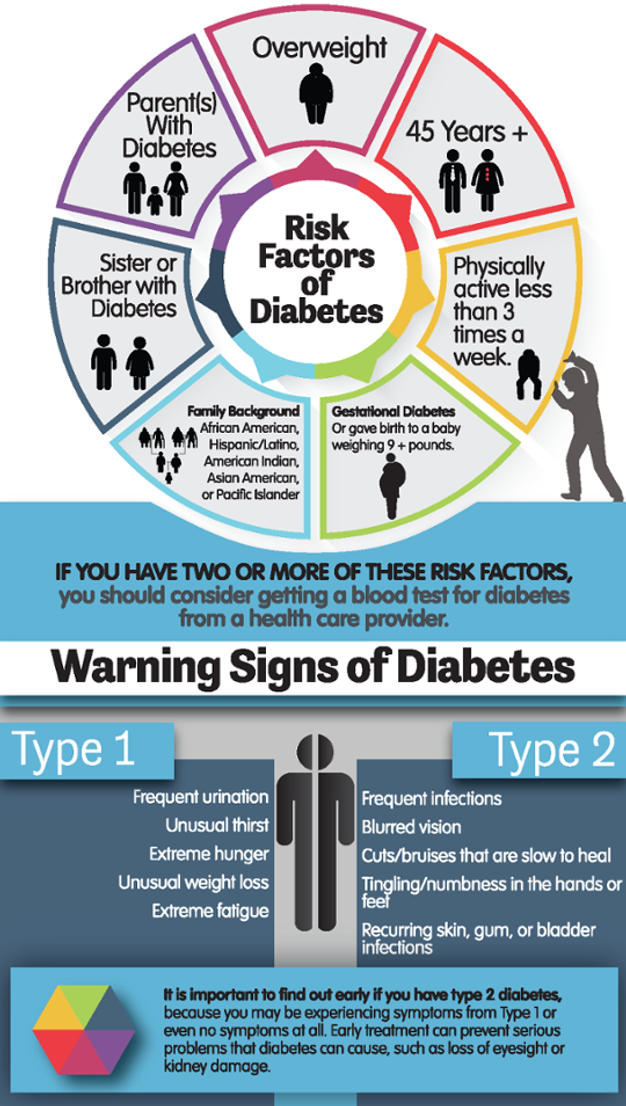
Signs of type 2 diabetes in kids
Type 2 diabetes in children - Symptoms and causes
Overview
Type 2 diabetes in children is a chronic disease that affects the way your child's body processes sugar (glucose) for fuel. Without treatment, the disorder causes sugar to build up in the bloodstream, which can lead to serious long-term consequences.
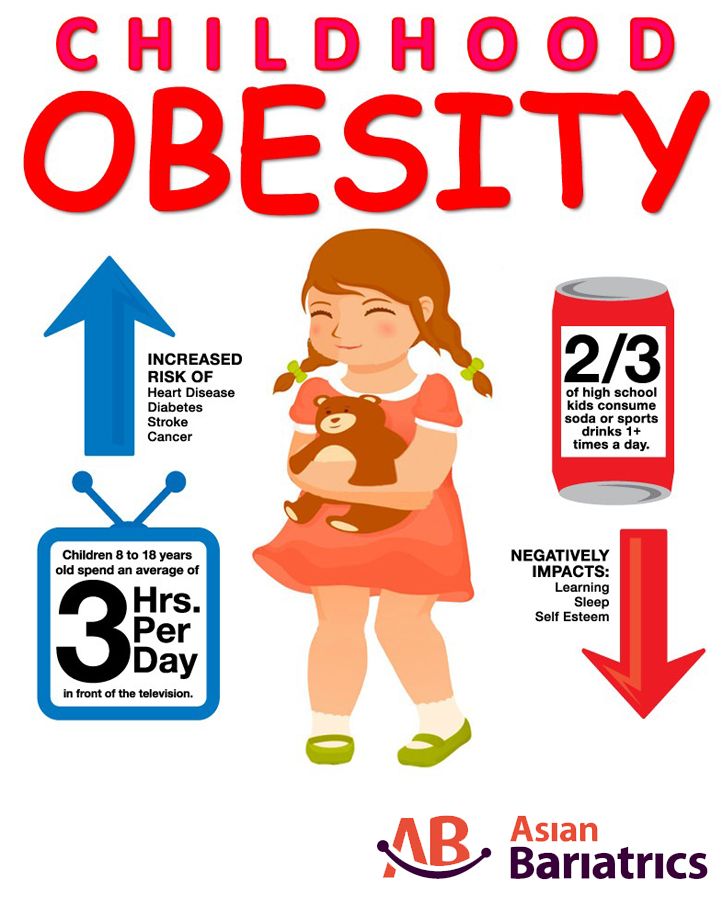
Type 2 diabetes occurs more commonly in adults. In fact, it used to be called adult-onset diabetes. But the increasing number of children with obesity has led to more cases of type 2 diabetes in younger people.
There's plenty you can do to help manage or prevent type 2 diabetes in your child. Encourage your child to eat healthy foods, get plenty of physical activity and maintain a healthy weight. If healthy eating and exercise aren't enough to control type 2 diabetes, oral medication or insulin treatment may be needed.
Products & Services
- Book: Mayo Clinic Guide to Raising a Healthy Child
- Book: The Essential Diabetes Book
Symptoms
Type 2 diabetes in children may develop so gradually that there are no noticeable symptoms. Sometimes, the disorder is diagnosed during a routine check-up.
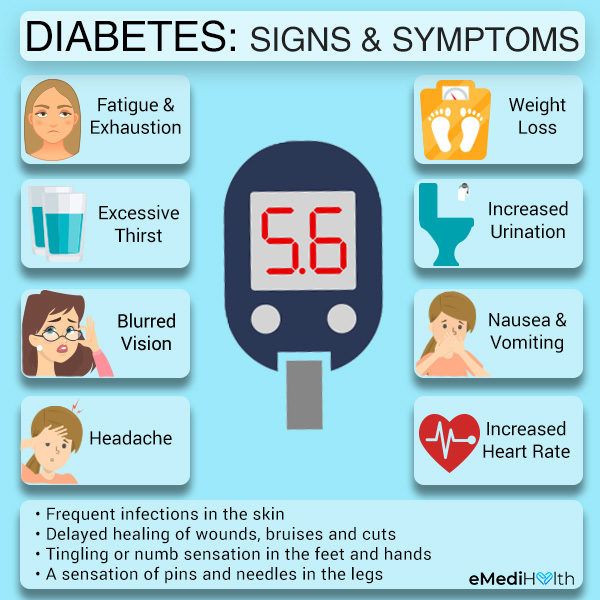
Some children might experience these signs and symptoms as a result of too much sugar in their bloodstreams:
- Increased thirst
- Frequent urination
- Increased hunger
- Fatigue
- Blurry vision
- Darkened areas of skin, most often around the neck or in the armpits and groin
- Unintended weight loss, although this is less common in children with type 2 diabetes than in children with type 1 diabetes
- Frequent infections
When to see a doctor
See your child's health care provider if you notice any of the signs or symptoms of type 2 diabetes. Undiagnosed, the disease can cause serious damage.
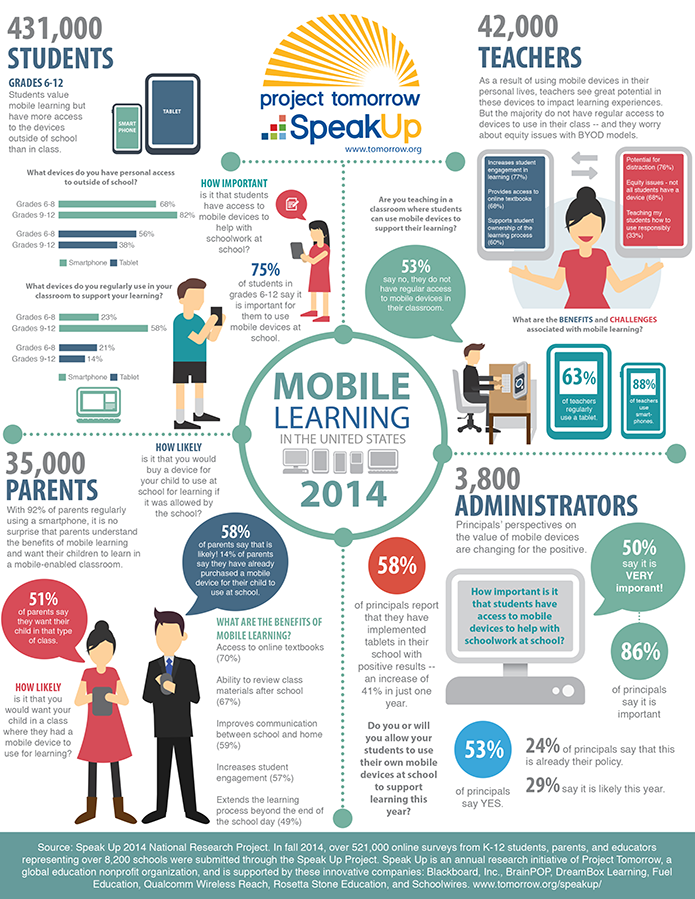
Diabetes screening is recommended for children who have started puberty or are at least 10 years old, who are overweight or obese, and who have at least one other risk factor for type 2 diabetes.
Request an appointment
Causes
The exact cause of type 2 diabetes is unknown.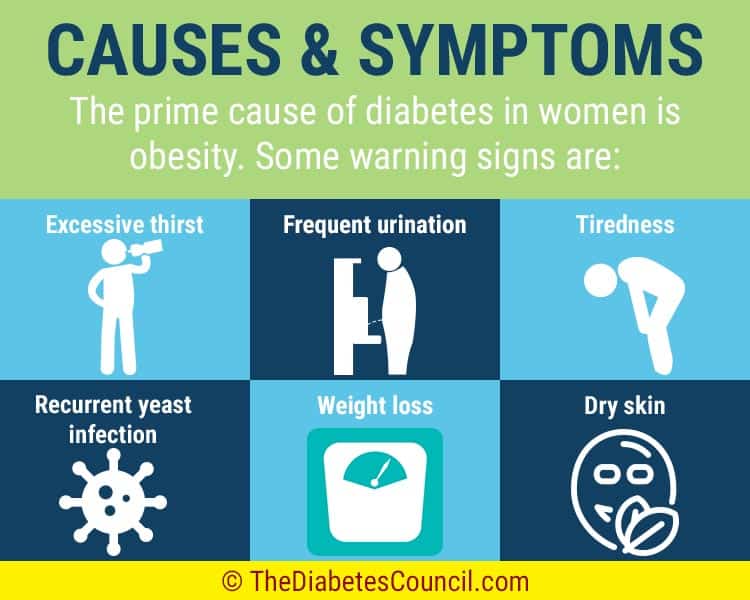 But family history and genetics appear to play an important role. What is clear is that children with type 2 diabetes can't process sugar (glucose) properly.
But family history and genetics appear to play an important role. What is clear is that children with type 2 diabetes can't process sugar (glucose) properly.
Most of the sugar in the body comes from food. When food is digested, sugar enters the bloodstream. Insulin allows sugar to enter the cells — and lowers the amount of sugar in the blood.
Insulin is produced by a gland located behind the stomach called the pancreas. The pancreas sends insulin to the blood when food is eaten. When the blood sugar level starts to drop, the pancreas slows down the secretion of insulin into the blood.
When your child has type 2 diabetes, this process doesn't work as well. As a result, instead of fueling cells, sugar builds up in your child's bloodstream. This can happen because:
- The pancreas may not make enough insulin
- The cells become resistant to insulin and don't allow as much sugar in
Risk factors
Researchers don't fully understand why some children develop type 2 diabetes and others don't, even if they have similar risk factors.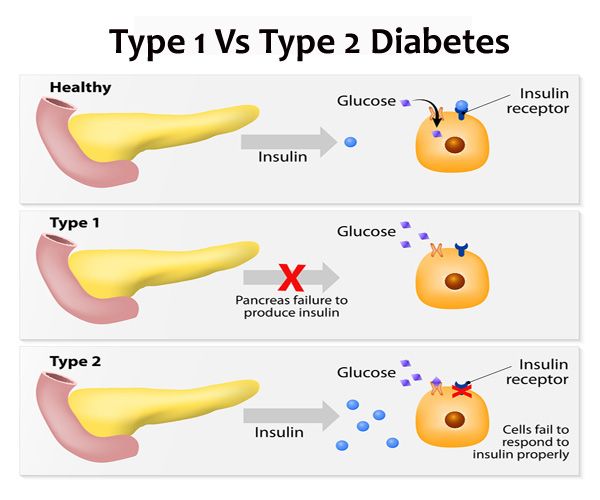 However, it's clear that certain factors increase the risk, including:
However, it's clear that certain factors increase the risk, including:
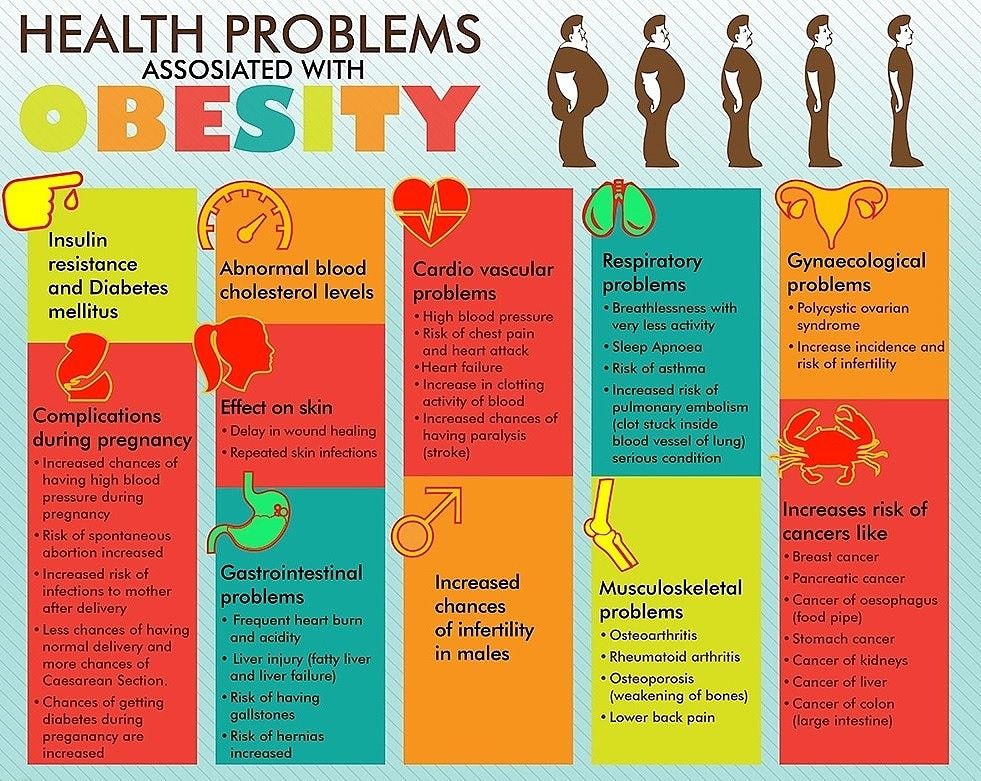
- Weight. Being overweight is a strong risk factor for type 2 diabetes in children. The more fatty tissue children have — especially inside and between the muscle and skin around the abdomen — the more resistant their bodies' cells become to insulin.
- Inactivity. The less active children are, the greater their risk of type 2 diabetes.
- Diet. Eating red meat and processed meat and drinking sugar-sweetened beverages is associated with a higher risk of type 2 diabetes.
- Family history. Children's risk of type 2 diabetes increases if they have a parent or sibling with the disease.
- Race or ethnicity. Although it's unclear why, certain people — including Black, Hispanic, American Indian and Asian American people — are more likely to develop type 2 diabetes.
- Age and sex.
 Many children develop type 2 diabetes in their early teens, but it may occur at any age. Adolescent girls are more likely to develop type 2 diabetes than are adolescent boys.
Many children develop type 2 diabetes in their early teens, but it may occur at any age. Adolescent girls are more likely to develop type 2 diabetes than are adolescent boys. - Maternal gestational diabetes. Children born to women who had gestational diabetes during pregnancy have a higher risk of developing type 2 diabetes.
- Low birth weight or preterm birth. Having a low birth weight is associated with a higher risk of developing type 2 diabetes. Babies born prematurely — before 39 to 42 weeks' gestation —have a greater risk of type 2 diabetes.
Type 2 diabetes in children is often associated with metabolic syndrome and polycystic ovarian syndrome.
Metabolic syndrome
When certain conditions occur with obesity, they are associated with insulin resistance and can increase the risk of diabetes — and heart disease and stroke. A combination of the following conditions is often called metabolic syndrome:
- High blood pressure
- Low levels of high-density lipoproteins (HDL), the "good" cholesterol
- High triglycerides
- High blood sugar levels
- Large waist size
Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) affects young females after puberty.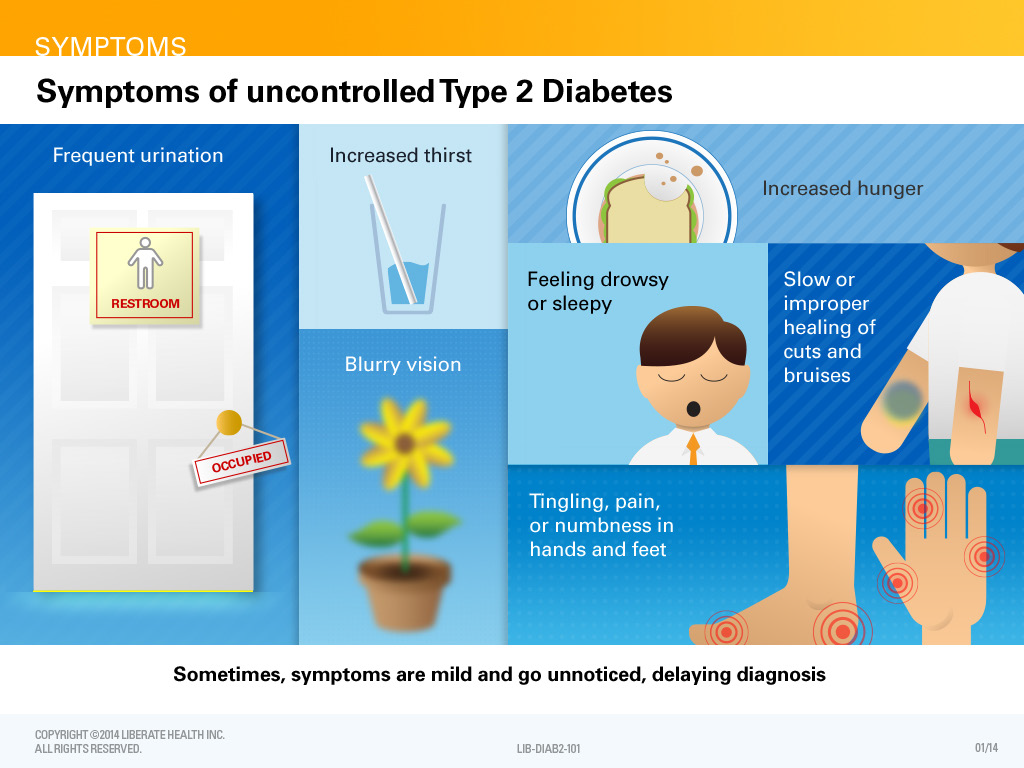 PCOS is caused by an imbalance of hormones, resulting in signs such as weight gain, irregular menstrual periods, and excess face and body hair. People with PCOS often have problems with metabolism that can result in insulin resistance and type 2 diabetes.
PCOS is caused by an imbalance of hormones, resulting in signs such as weight gain, irregular menstrual periods, and excess face and body hair. People with PCOS often have problems with metabolism that can result in insulin resistance and type 2 diabetes.
Complications
Type 2 diabetes can affect nearly every organ in your child's body, including the blood vessels, nerves, eyes and kidneys. The long-term complications of type 2 diabetes develop gradually over many years. Eventually, diabetes complications may be severe or even life-threatening.
Complications of type 2 diabetes are related to high blood sugar and include:
- High cholesterol
- Heart and blood vessel disease
- Stroke
- Nerve damage
- Kidney disease
- Eye disease, including blindness
Keeping your child's blood sugar level close to the standard range most of the time can dramatically reduce the risk of these complications. You can help your child prevent diabetes complications by:
You can help your child prevent diabetes complications by:
- Working with your child to maintain good blood sugar control as much as possible
- Teaching your child the importance of healthy eating and participating in regular physical activity
- Scheduling regular visits with your child's diabetes treatment team
Prevention
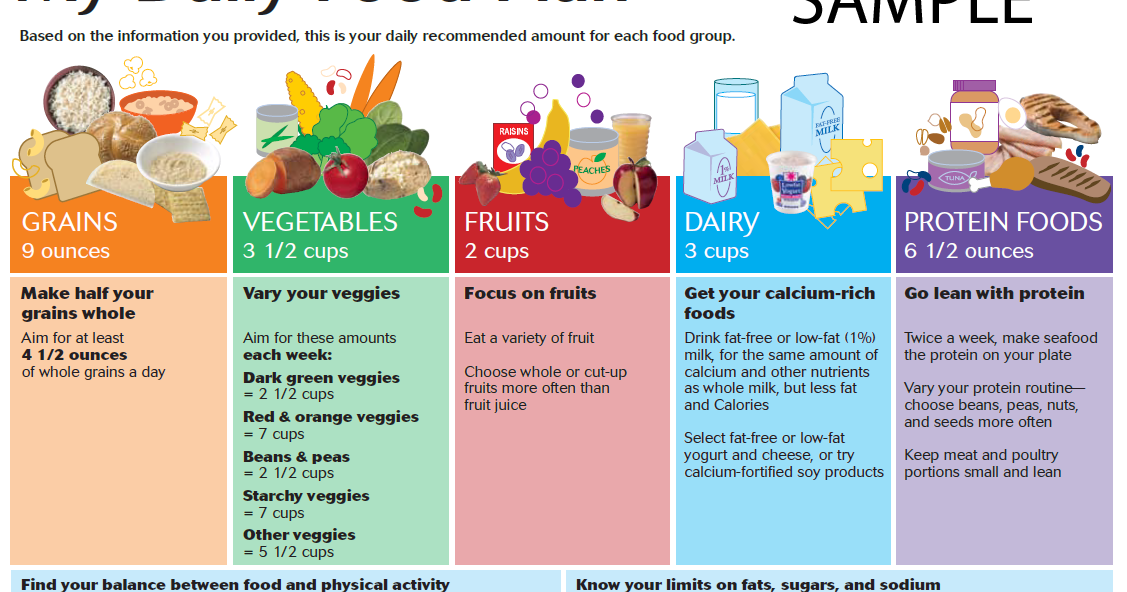
Healthy-lifestyle choices can help prevent type 2 diabetes in children. Encourage your child to:
- Eat healthy foods. Offer your child foods low in fat and calories. Focus on fruits, vegetables and whole grains. Strive for variety to prevent boredom.
- Get more physical activity. Encourage your child to become active. Sign up your child for a sports team or dance lessons.
Better yet, make it a family affair. The lifestyle choices that can help prevent type 2 diabetes in children can do the same for adults.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
What Is Type 2 Diabetes? (for Parents)
en español: ¿Qué es la diabetes tipo 2?
Reviewed by: Mary L.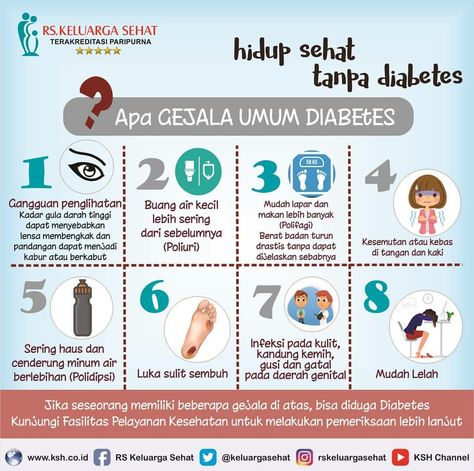 Gavin, MD
Gavin, MD
What Is Type 2 Diabetes?
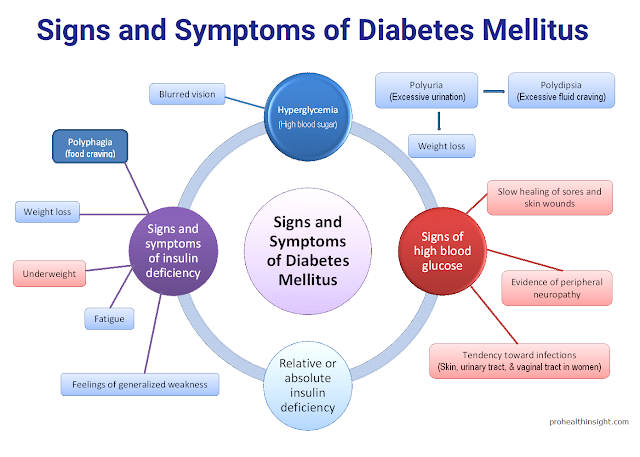
People who have type 2 diabetes have a hard time using glucose (sugar) from food for energy.
After we eat, carbohydrates in food break down into glucose. When glucose enters the bloodstream, blood sugar levels go up. When it does, the pancreas sends insulin into the blood. Insulin helps open cells throughout the body to let glucose in, giving the cells the energy they need.
In type 2 diabetes, the pancreas makes insulin, but the cells don’t respond to it as they should. This is called insulin resistance. When glucose can’t get into cells, the blood sugar level rises. Then the pancreas works harder to make even more insulin. At first, the extra insulin keeps sugars in the normal range. But over time, the pancreas can’t keep up, and the blood sugars stay high. When blood sugars stay high, the person may have type 2 diabetes.
Why Do Some People Get Type 2 Diabetes?
No one knows for sure why some people get type 2 diabetes, but it’s likely a combination of genes and the environment. Many kids who get it have someone in their family who has it too.
Many kids who get it have someone in their family who has it too.
Type 2 diabetes happens more often in children:
- who are overweight. When a person has extra weight, sugar in the blood doesn’t get into the cells as well as it should. But people don’t have to be overweight to get type 2 diabetes.
- during puberty. Many kids and teens are diagnosed with type 2 diabetes around puberty. As growth hormone levels normally rise during puberty, insulin does not work as well.
- with polycystic ovary syndrome (PCOS). Girls and women with PCOS have insulin resistance and are more likely to get type 2 diabetes.
- whose mothers had diabetes during pregnancy. Babies are exposed to more sugar in the womb when their mother has diabetes. This along with genetic factors increase the chance of getting type 2 diabetes later in life.
What Are the Signs & Symptoms of Type 2 Diabetes?
Many people with insulin resistance have dark patches on their skin, especially in skin folds like those around the neck or in the armpits.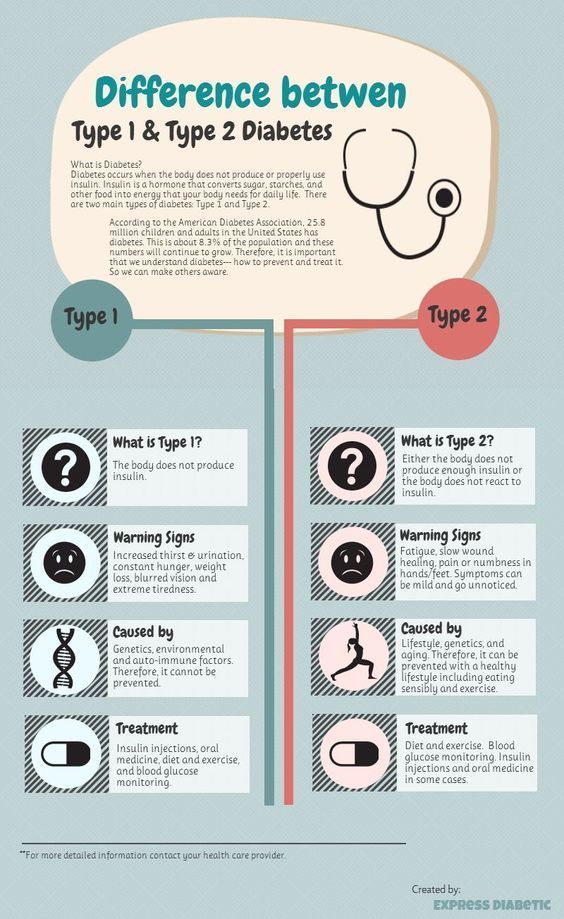 This is called acanthosis nigricans, or simply acanthosis, and it’s often an early sign that a person may develop type 2 diabetes.
This is called acanthosis nigricans, or simply acanthosis, and it’s often an early sign that a person may develop type 2 diabetes.
Type 2 diabetes can show up in different ways. Some kids have symptoms, but others don’t. Kids with diabetes symptoms may:
- need to pee a lot
- be thirstier and drink more than usual
- feel tired often
- have blurry vision
How Is Type 2 Diabetes Diagnosed?
Doctors may check for diabetes if a child has symptoms or risk factors, like being overweight and having acanthosis. Different kinds of blood tests can check for diabetes, including:
- HbA1c. This test shows a person's average blood sugar levels over the past few months. It’s also called a glycosylated hemoglobin or hemoglobin A1c test. HbA1c of 6.5% or higher means the person may have diabetes.
- fasting glucose. To get this test, a person first stops eating for at least 8 hours.
 A blood sugar reading of 126 mg/dL or higher means they might have diabetes.
A blood sugar reading of 126 mg/dL or higher means they might have diabetes. - random glucose. This test can be taken at any time. A blood sugar level of 200 mg/dL or higher means a person may have diabetes.
- glucose tolerance test. To get this test, a person first stops eating or drinking for at least 8 hours. Then, they drink a sugary liquid and their blood sugar is checked 1 and 2 hours later. A blood sugar of 200mg/dL or higher at 2 hours means they might have diabetes.
The doctor uses the results from one or more of these tests to tell if the child has diabetes. The doctor can order other tests to find out if it is type 1 diabetes or type 2 diabetes.
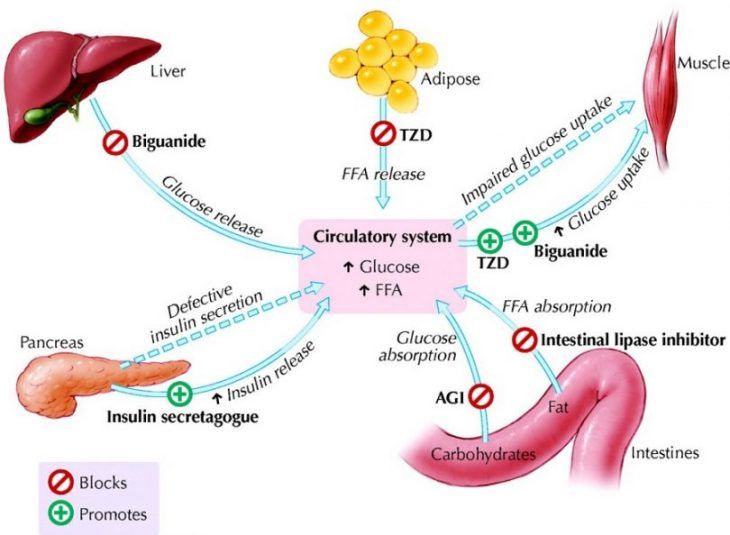
How Is Type 2 Diabetes Treated?
Kids and teens with type 2 diabetes often go to a pediatric endocrinologist for treatment. This kind of doctor treats problems affecting hormones, like diabetes. They also may see a dietitian, diabetes educator, or weight management specialist.
The goal of treatment for type 2 diabetes is to keep blood sugar levels in a healthy range. Treatment usually includes:
- eating a healthy, balanced diet
- getting regular physical activity
- checking blood sugar levels regularly
- losing weight, if recommended
- taking anti-diabetes pills or getting insulin (by injection or with a pump). If blood sugars remain high, the doctor may add another medicine.
What Problems Can Happen With Type 2 Diabetes?
Not having the right amount of sugar in the blood can lead to:
- hyperglycemia. This is when blood sugars are too high. Kids with hyperglycemia may be extra thirsty and pee more than usual. If high blood sugars aren’t treated, kids can get very sick and have health issues later in life, like heart and kidney problems.
- diabetic ketoacidosis (DKA). This serious condition needs treatment right away. When there’s not enough insulin in the body to let the glucose into the cells, the body starts to break down fat instead of sugar.
 Symptoms of DKA can include nausea, vomiting, belly pain, fast breathing, and in severe cases, unconsciousness. DKA happens more often in people with type 1 diabetes, but it can sometimes happen to kids with type 2 diabetes.
Symptoms of DKA can include nausea, vomiting, belly pain, fast breathing, and in severe cases, unconsciousness. DKA happens more often in people with type 1 diabetes, but it can sometimes happen to kids with type 2 diabetes. - hyperglycemic hyperosmolar state (HHS). Like DKA, this is a serious condition that needs treatment right away. People with HHS have severe dehydration and very high blood sugars.
- hypoglycemia. This is when blood sugars are too low. It can sometimes happen when people with type 2 diabetes are treated with insulin. If a person with diabetes gets more insulin than they need, their blood sugar level can drop too low. Symptoms can include headache, weakness, shakiness, anxiety, and sweating.
How Can Parents Help?
It can take time for your child and your family to adjust to living with type 2 diabetes. The care team will teach you and your child everything you need to know about staying healthy.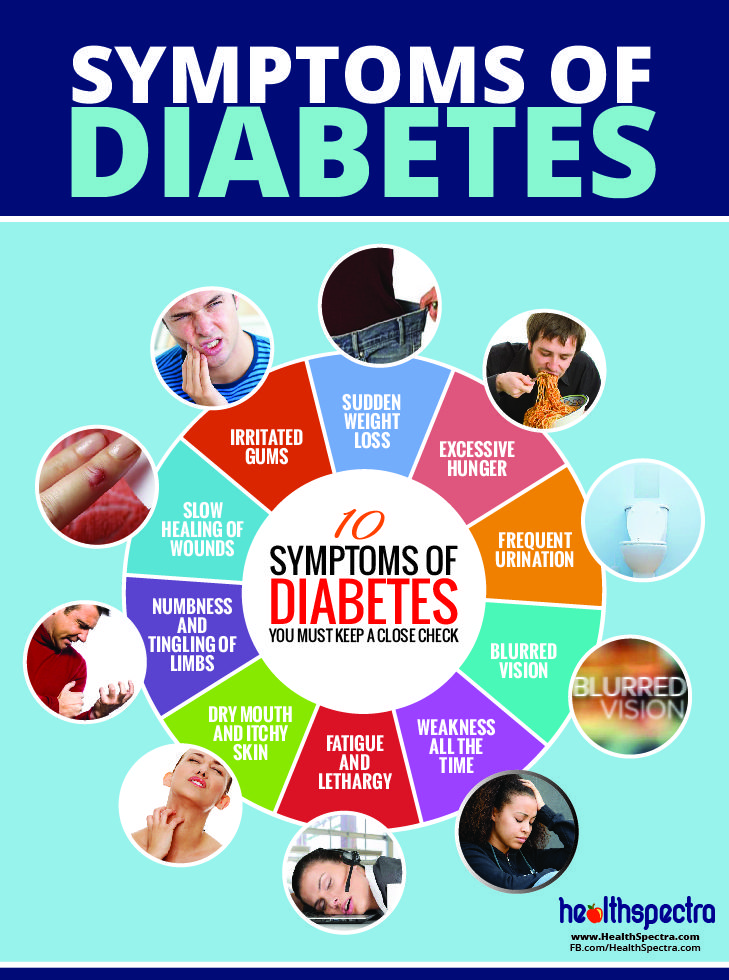 Taking your child to all their medical visits and following the diabetes care plan will help keep you on track.
Taking your child to all their medical visits and following the diabetes care plan will help keep you on track.
When your child has type 2 diabetes, it may feel like a lot at times, but you're not alone. The diabetes care team is there for you and your child. Go to them with questions and concerns, or when you need support.
Reviewed by: Mary L. Gavin, MD
Date reviewed: February 2022
Share:
/content/kidshealth/misc/medicalcodes/parents/articles/type2
Childhood diabetes | Prevention | GBUZ "City Polyclinic No.
 6 of Novorossiysk" MH KK
6 of Novorossiysk" MH KK Diabetes in children: causes, symptoms and signs, diagnosis, treatment.
) in the blood. Diabetes mellitus ranks first among all endocrine diseases in children. Diabetes mellitus in children is relatively acute and without appropriate treatment, as a rule, acquires a severe, progressive course. This development of diabetes in children is due to the intensive growth of the child's body and, accordingly, increased metabolism
Diagnosis of diabetes in children is based on identifying the symptoms of the disease and determining the concentration of glucose and insulin in the blood. Treatment of diabetes mellitus in children includes diet, dosed exercise, treatment with insulin preparations.
Forms of diabetes in children. There are two main types of diabetes mellitus:
- Insulin-dependent diabetes (type 1 diabetes).
- Non-insulin dependent diabetes (type 2 diabetes).

While type 2 diabetes mellitus predominates among adults, type 1 diabetes mellitus (insulin-dependent) predominates among children.
Type 1 diabetes mellitus is characterized by very low levels of insulin in the blood, as a result of which the diabetic child is dependent on insulin treatment.
Features of the development of diabetes in children
A child's pancreas (an organ that produces the hormone insulin) is very small. By the age of 10, the mass of the child's pancreas doubles, reaching a size of 12 cm and a weight of just over 50 g. The production of insulin by the pancreas is one of its most important functions, which is finally formed by the fifth year of a child's life. It is from this age and up to about 11 years that children are especially susceptible to diabetes. All metabolic processes in a child's body proceed much faster than in an adult. Carbohydrate metabolism (assimilation of sugars) is no exception. Accordingly, a child needs to consume 10 g of carbohydrates per 1 kg of weight per day.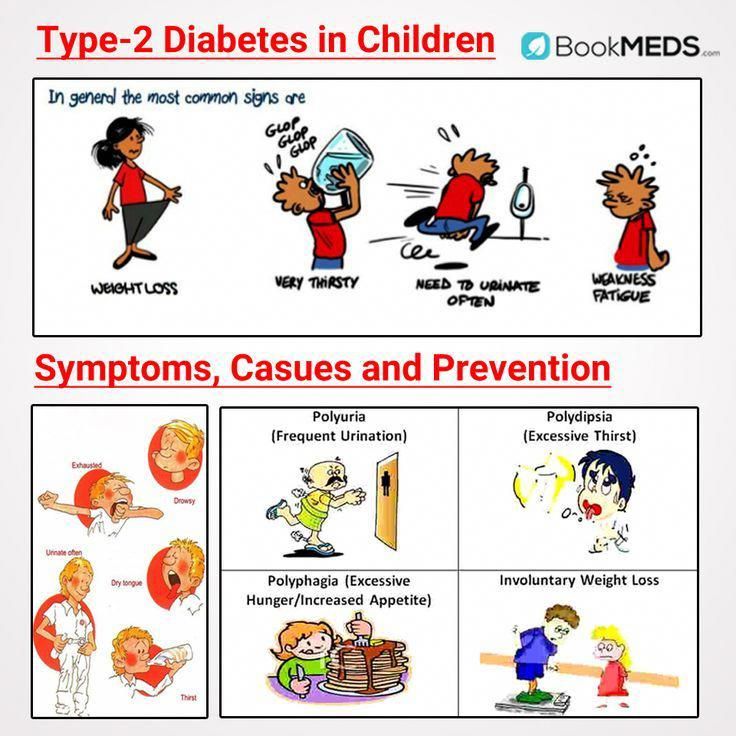 Therefore, all children are very fond of sweets - this is a natural need of their body. The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
Therefore, all children are very fond of sweets - this is a natural need of their body. The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
In general, the risk of developing diabetes is higher in premature, underdeveloped children, or adolescents during puberty. Also, the risk of developing diabetes is higher in children subject to significant physical exertion (for example, in pupils of sports schools).
The main cause of diabetes in children is a viral infection that destroys insulin-producing cells in the pancreas. Among childhood infections, many can cause the development of diabetes (mumps, rubella, measles, etc.). In this regard, one of the most important measures to prevent the development of diabetes in children is the timely vaccination of the child.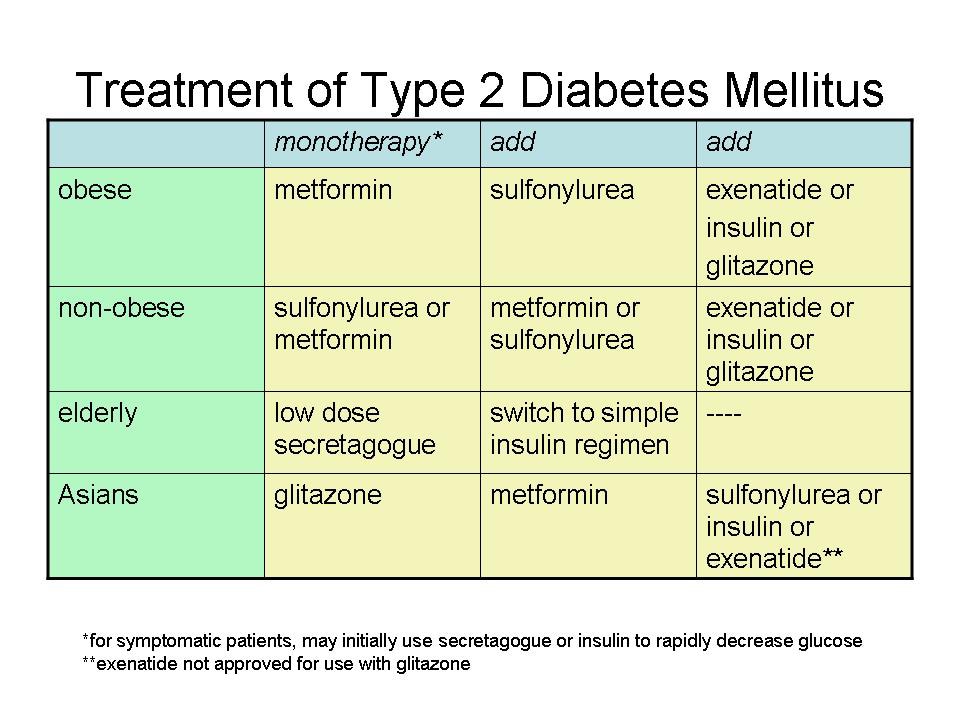
The course of diabetes mellitus in children also depends on the age of the child at which the disease began. The younger the child with diabetes, the more severe it is and the greater the risk of various complications. As a rule, once having arisen, diabetes in a child never goes away. A child with diabetes will need supportive care throughout his life.
Risk factors for diabetes in children
There are a number of risk factors that contribute to the development of diabetes in children. The presence of one or more risk factors greatly increases a child's chances of developing diabetes. Risk factors for diabetes in children:
- children born to diabetic mothers
- both parents of the child have diabetes mellitus
- frequent acute viral diseases
- birth weight exceeded 4.5 kg
- other metabolic disorders (hypothyroidism, obesity)
- immunosuppression
Symptoms of diabetes in children are almost the same as in adults:
- thirst
- weight loss
- excessive urine output (more than 2-3 liters per day)
- severe infections
- fatigue, inability to concentrate
Parents do not always notice these symptoms, which makes it difficult to detect diabetes in children.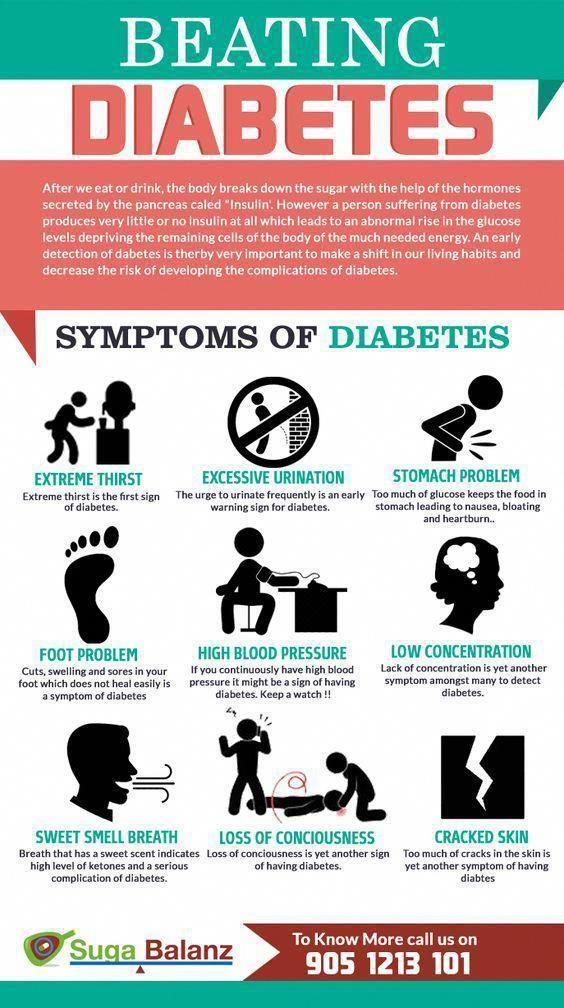 Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Treatment of diabetes in children.
Treatment of diabetes in a child includes: exercise, diet, medication.
Exercise for children with diabetes
Exercise increases the sensitivity of body tissues to insulin and lowers blood sugar levels. In this regard, dosed physical activity is an important part of the treatment of children with diabetes. It should be emphasized that only dosed physical activity is useful in diabetes, while uncontrolled physical activity in patients with diabetes mellitus contributes to the development of hypoglycemic conditions.
Proper exercise management in diabetic children necessarily includes the use of additional carbohydrates before, during and after exercise in accordance with the recommendations given by your doctor, as well as periodic monitoring of blood glucose levels.
It is important to measure blood glucose before, during and after exercise in order to correctly dose insulin with a short or intermediate duration of action.
Nutrition of a sick child plays an important role in the treatment of diabetes mellitus. The nutrition of a child with diabetes should meet all the requirements that are currently imposed on the nutrition of a healthy child: the diet should be as balanced as possible in all the most important ingredients (proteins, fats, carbohydrates and vitamins). Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
In diabetes mellitus, they limit the use of such foods and dishes as bakery products made from wheat flour, potatoes, cereals (semolina, rice). Porridge is given to the child no more than once a day, using coarse grinding cereals (buckwheat, oatmeal, corn) for their preparation.
Rice, semolina and pasta should be used in limited quantities. The consumption of bread should not exceed 100g per day. Vegetables (everything except potatoes) can be offered to the child without restrictions. Moreover, dishes from various vegetables should make up a significant part of the daily diet of children.
Fruits and berries – unsweetened varieties of apples, black currants, cherries, etc. – are also widely included in the diet for diabetes. Occasionally, you can give your child citrus fruits (oranges, tangerines), strawberries, wild strawberries, raspberries. A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
Fatty, spicy and salty sauces, sweet sauces are excluded from the menu. If the child does not have liver diseases associated with diabetes, it is allowed to add a small amount of onion to food as a seasoning.
It is necessary to feed a child with diabetes 6 times a day and more often. The greatest satisfaction for the child, as a rule, brings his usual food. In view of this, when compiling a diet, the features of the family nutrition stereotype should be taken into account: the hours and volume of each meal, the child's eating habits. The composition of the child's diet should be agreed with the doctor observing the child.
Drug treatment of diabetes in children.
Almost all children with diabetes receive insulin. Thanks to the introduction of long-acting insulin preparations into medical practice, as a rule, one injection of insulin per day is sufficient.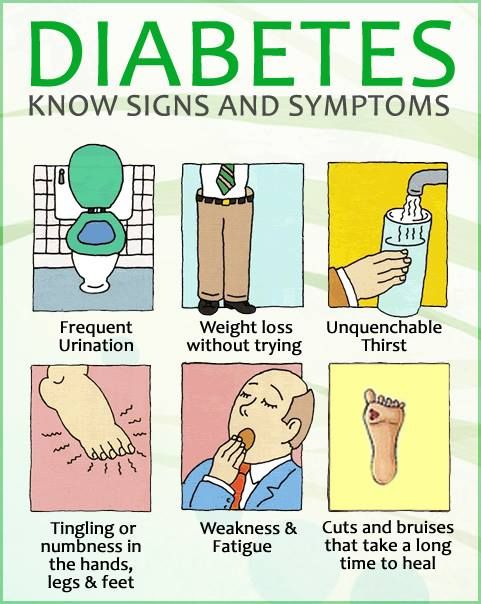
The choice of insulin preparation, its dosage and administration schedule are also determined by the attending physician. Tablets for diabetes (Maninil, Glipizide, etc.) are quite effective in treating diabetes in adults, but very rarely give good results in children. They are used in mild forms of the disease or prescribed as an adjuvant to reduce the number of injections or the dose of insulin.
Children and adolescents who are regularly treated, adhere to the diet exactly, develop well physically and mentally.
Properly selected and organized therapy with insulin preparations and constant monitoring of the child's condition greatly alleviate the course of the disease and allow children with diabetes to lead a full life.
Material taken from the site: Cherepovets City Maternity Hospital
Diabetes mellitus in children and adolescents
Category: Useful information.
Type 1 diabetes mellitus (insulin-dependent) predominates among children. Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age.
Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age.
What contributes to the development of diabetes in children?
- genetic predisposition.
- Early refusal of breastfeeding, improper introduction of complementary foods,
- Overweight.
- Infectious diseases transferred in early childhood.
- Stress.
The symptoms of diabetes mellitus in children are almost the same as in adults: severe thirst, bedwetting appears, the child loses weight, fatigue, poor performance at school, skin infections (boils, barley) often recur, and vaginal candidiasis in girls.
Diabetes in children of the first year of life is rare, but it still happens sometimes. An infant cannot complain. If the baby is in a diaper, then parents are unlikely to notice that he has begun to excrete much more urine.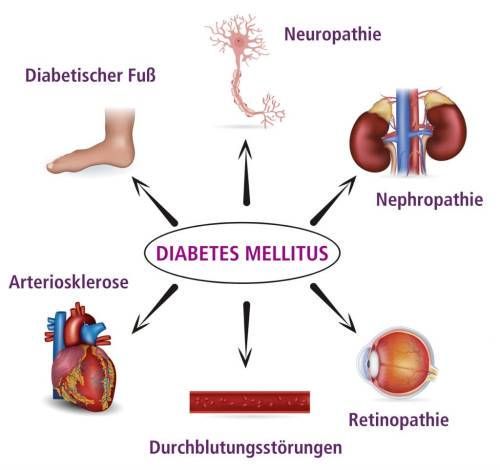 Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
The diagnosis is usually quickly confirmed by detecting an increase in blood glucose (greater than 11.1 mmol/L). If ketone bodies are detected in the blood or urine, urgent therapy is indicated. Waiting the next day to confirm hyperglycemia can be life-threatening. Children with diabetes need lifelong hormone replacement therapy. Diabetes never goes away. A child with diabetes will need maintenance treatment with insulin for the rest of his life.
Prevention of diabetes.
- Control of blood glucose levels, if among close relatives there are patients with diabetes mellitus.
- Breastfeeding up to 12 months, timely introduction of complementary foods.