Milk let down when not feeding
Let-down reflex | Pregnancy Birth and Baby
Let-down reflex | Pregnancy Birth and Baby beginning of content3-minute read
Listen
The let-down reflex is an important part of breastfeeding that starts milk flowing when your baby feeds. Each woman feels it differently, and some may not feel it at all. It can be affected by stress, pain and tiredness but once feeding is established, it requires little or no thought.
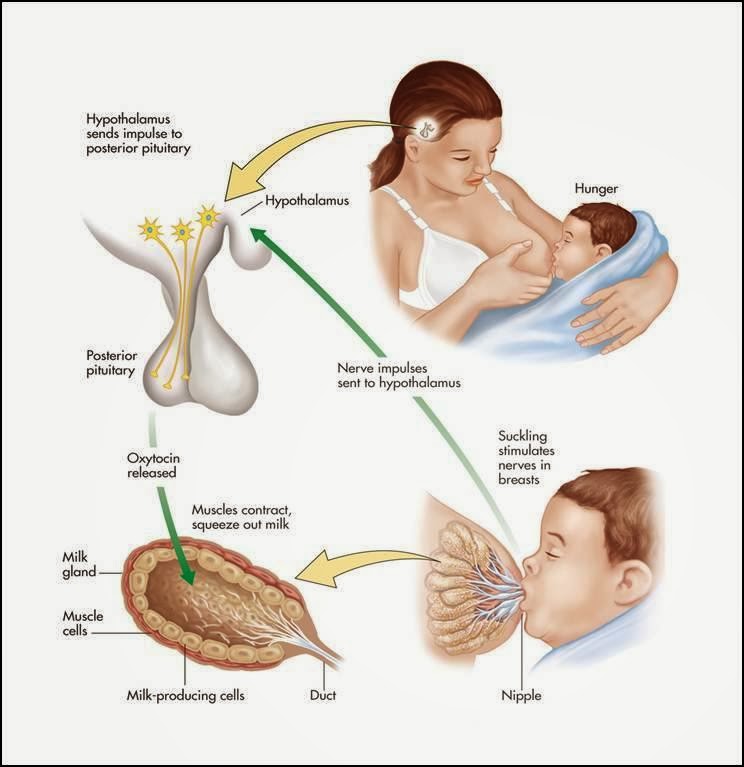
What is the let-down reflex?
The let-down reflex is what makes breastmilk flow. When your baby sucks at the breast, tiny nerves are stimulated. This causes two hormones – prolactin and oxytocin – to be released into your bloodstream. Prolactin helps make the milk, while oxytocin causes the breast to push out the milk. Milk is then released or let down through the nipple.
Some women feel the let-down reflex as a tingling sensation in the breasts or a feeling of fullness, although others don’t feel anything in the breast.
Most women notice a change in their baby’s sucking pattern as the milk begins to flow, from small, shallow sucks to stronger, slower sucks.
Some women also notice, while feeding or expressing from one breast, that milk drips from the other.
Your let-down reflex needs to be established and maintained to ensure a good supply of milk. This reflex requires no thought, unless you are having problems with breastfeeding.
When does it occur?
The let-down reflex occurs:
- in response to your baby sucking at the breast
- hearing, seeing or thinking about your baby
- using a breast pump, hand expressing or touching your breasts or nipples
- looking at a picture of your baby
- hearing your baby (or another baby) cry
The let-down reflex generally occurs 2 or 3 times a feed. Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
The let-down reflex can also occur with other stimulation of the breast, such as by your partner.
Strategies to encourage the reflex
The let-down reflex can be affected by stress, pain and tiredness. There are many things to try if you are experiencing difficulty.
- Ensure that your baby is correctly attached to the breast. A well-attached baby will drain a breast better.
- Feed or express in a familiar and comfortable environment.
- Try different methods to help you to relax: calming music, a warm shower or a warm washer on the breast, some slow deep breathing, or a neck and shoulder massage.
- Gently hand express and massage your breast before commencing the feed.
- Look at and think about your baby.
- If you are away from your baby, try looking at your baby’s photo.
- Always have a glass of water nearby.
Milk let-down can be quite forceful, particularly at the beginning of a feed. This fast flow of milk can upset your baby, but it might not mean you have oversupply. It can be managed through expressing before a feed, reclining slightly and burping your baby after the first few minutes. If you continue to have problems, seek advice.
How to deal with unexpected let-down
Until you and your baby fine-tune breastfeeding, many sensations and thoughts can trigger your let-down reflex. Leaking breasts can be embarrassing, but should stop once breastfeeding is fully established.
In the meantime you can feed regularly, apply firm pressure to your breasts when you feel the first sensation of let-down, use breast pads and wear clothing that disguises milk stains.
If you need help and advice:
- Pregnancy Birth and Baby on 1800 882 436
- your maternal child health nurse
- a lactation consultant (your maternity hospital might be able to help)
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australian Breastfeeding Association (Breastfeeding - naturally : the Australian Breastfeeding Association's guide to breastfeeding - from birth to weaning), Australian Breastfeeding Association (Let-down reflex)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Breastfeeding your baby
- How to increase breast milk supply
- Oversupply of breastmilk
Need more information?
Breastfeeding challenges - Ngala
Sometimes breastfeeding can be challenging
Read more on Ngala website
Breast refusal and baby biting breast | Raising Children Network
Breast refusal or baby biting breast are common breastfeeding issues. These issues might resolve themselves, or your child and family health nurse can help.
Read more on raisingchildren.net.au website
Breastfeeding - expressing breastmilk - Better Health Channel
Expressing breast milk by hand is a cheap and convenient method.
Read more on Better Health Channel website
Breast feeding your baby - MyDr.com.au
Breast milk has long been known as the ideal food for babies and infants. Major health organisations recommend that women breast feed their babies exclusively until they are 6 months old, and continue breast feeding, along with solids, until they are 12 months old or more. Breast milk has many benefits.
Read more on myDr website
Expressing and storing breast milk
This page includes information about expressing, storing, cleaning equipment, transporting and preparing expressed breastmilk for your baby.
Read more on WA Health website
Expressing breastmilk & storing breastmilk | Raising Children Network
You can express breastmilk by hand, or with a manual or an electric pump..jpg) Store expressed breastmilk in special bags or containers in the fridge or freezer.
Store expressed breastmilk in special bags or containers in the fridge or freezer.
Read more on raisingchildren.net.au website
Mastitis, blocked duct & breast abscess | Raising Children Network
If you think you have a blocked milk duct, you can treat it at home to start with. If you think you have mastitis or a breast abscess, see your GP as soon as possible.
Read more on raisingchildren.net.au website
Weaning at 6 Months | Tresillian
Babies start weaning when they begin consuming foods other than breastmilk. For advice on weaning check out Tresillian's tip page.
Read more on Tresillian website
Frequently asked questions about alcohol and pregnancy | FASD Hub
We've answered some common questions about alcohol use during pregnancy and breastfeeding, and about living with fetal alcohol spectrum disorder (FASD).
Read more on FASD Hub Australia website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What You Should Know About Your Let Down Reflex
Written by WebMD Editorial Contributors
In this Article
- How Does the Let Down Reflex Work?
- What Are Signs of a Good Let Down?
- Complications of the Let Down Reflex
When your baby first latches on to nurse, they don’t actually get much milk at first. Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
How Does the Let Down Reflex Work?
If milk came out of your breasts instantly when your baby latched on, you’d probably leak constantly. Instead, your breasts store the milk until it’s needed. Most often, your let down reflex is triggered by a particular suckling motion your baby makes to stimulate milk production.
The let down reflex is a physiological response to your baby’s sucking. They stimulate small nerves in the nipple, which causes prolactin and oxytocin to produce milk and let down milk, respectively. The reflex is often accompanied by a tingling sensation in the nipple, but not all women experience that.
If you pay attention to your baby’s nursing patterns, at first their suckling will be faster and shallower to stimulate the release of milk. Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Other let down triggers. Since your brain is wired to care for a newborn, other things may trigger the let down reflex. If your baby cries, or if you hear any baby cry, your milk may let down in response. If you go too long without nursing and your breasts get too full, your let down reflex may trigger to relieve the pressure.
Strong emotions may also trigger a let down of milk. If you are feeling intensely stressed, angry, or sad, your body may take that as a sign that you need to nurse your baby or release milk to alleviate pressure.
If your milk is not letting down, you can physically stimulate the nipple to allow let down. Try gently rolling your hand down your breast toward the nipple, then massage gently. It can also help to relax and think about your baby.
What Are Signs of a Good Let Down?
Breastfeeding is wonderful for your baby, but it is often full of doubts and questions. Are you producing enough milk? Are you doing it right? This extends to the let down reflex, too. You may wonder if your let down is strong enough or too strong.
Here are signs of a healthy, functioning let down response:
Uterine cramps. You may notice that your uterus cramps during a let down in the days following birth. This is natural and nothing to be concerned about. As with menstrual cramps, for some the cramps are mild and barely noticeable, while for others the contractions can be more painful.
Change in sucking pattern. You may notice a change in your baby’s sucking pattern during a nursing session. Their suckle will go from being short and fast to long and slow once milk lets down. If they need more milk, their sucking may change again to encourage another let down.
Your feelings.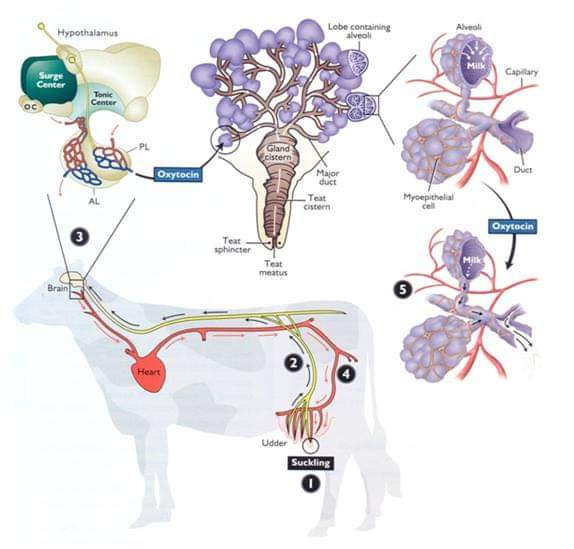 Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Complications of the Let Down Reflex
Oversupply milk ejection reflex. A powerful let down is often accompanied by an oversupply of milk, sometimes called oversupply milk ejection reflex (O-MER). When your let down happens, you may notice that your baby sputters, coughs, and even chokes on your milk. Your baby may bite down to slow the milk flow. You may leak when not nursing or notice that your baby has more frequent but short feedings if you have an oversupply.
If this happens, keep a bib or cloth handy to catch your milk when it first lets down so that your baby doesn’t choke. After a moment when the let down slows, you can try latching your baby again. You can also restrict your milk flow by squeezing your areola during breastfeeding.
Talk to your doctor about safe ways to decrease your oversupply so that your let down is less strong.
Dysphoric milk ejection reflex. In some women, breastfeeding can create a negative physiological response, leading to negative emotions like guilt, anxiety, depression, and sadness. It is usually an isolated response that occurs only when you first let down your milk and into the first few minutes of breastfeeding. This is called dysphoric milk ejection reflex (D-MER) and is different from postpartum depression.
There is still more research needed on the causes and effects of D-MER. Talk to your doctor if you are struggling with negative emotions during breastfeeding.
Weak let down. You may have a weak let down if your baby seems frustrated while nursing. They may not be getting enough milk, or they may not be getting milk as fast as they want it. Using a breast pump can supplement less successful nursing sessions.
When pumping, look at photos and videos of your baby to try and encourage a let down. And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
Article "Pumping - when and how?"
There are times in the life of mother and baby when breastfeeding is either impossible or difficult for some reason. For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
This can happen if the baby is born prematurely, and the very process of sucking the mother's breast turns out to be hard physical work for him - such an infant can also be offered expressed milk.
The same applies to the situation when the baby is ill and feeling unwell prevents him from fully sucking, as he is too weak to make the efforts necessary to "extract" breast milk. In this case, it should be expressed for 2 reasons: firstly, to provide the child with complete and optimal nutrition for him, and secondly, to maintain lactation.
Situations are different, so it is important to understand why pumping is necessary, how to do it correctly and what are the conditions for storing breast milk.
When and why to express?
Pumping is the process by which a nursing mother manually or with the help of a breast pump extracts milk from her breast.
This is not a mandatory procedure for everyone, and it does not need to be carried out after each feeding, since the milk in the female breast is formed exactly as much as is needed to saturate the baby at a certain age. Those. how much milk the baby ate in one feeding - so much will appear in the breast by the next.
But if, after applying, you also express the rest of the milk, then by the upcoming feeding it will be produced more than the child can eat - and this often leads to stagnation of milk (lactostasis).
Milk should be expressed when:
-
Having to bottle feed or supplement a baby for one reason or another.
 If at the same time the pediatrician did not forbid the baby to eat breast milk, then the mother needs to feed the baby expressed.
If at the same time the pediatrician did not forbid the baby to eat breast milk, then the mother needs to feed the baby expressed. -
The baby is left without a mother for a long time. There are times when a woman needs to go away, and she cannot take the child with her. In this case, you can leave a supply of milk for several hours, after decanting it.
-
Mom is sick. It happens that during lactation a woman becomes seriously ill and is forced to take medications that penetrate into breast milk, which is strictly forbidden to give to a child. Medicines contained in milk, once in the child's body, can have an adverse effect on it. To prevent this from happening, the pediatrician will help you choose the milk formula that you need to feed the baby during the mother’s illness. Pumping in such a situation will help a woman maintain lactation until recovery.
-
Mom goes to work. A mother's return to work before the end of lactation can put her before a choice: transfer the baby to formula milk or feed it with expressed milk.
 Recently, more and more parents are choosing the latter option, since breast milk is much healthier than artificial nutrition.
Recently, more and more parents are choosing the latter option, since breast milk is much healthier than artificial nutrition. -
Injured nipples. With improper care and attachment of the child to the breast, cracks may appear on the nipples. Feeding in this condition of the nipples becomes very painful for the mother, and then the baby should be briefly transferred to expressed milk from a bottle. This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast.
-
There is a risk of lactostasis. A child, especially in the first days after birth, is not always able to suck out all the milk. To avoid lactostasis, mom needs to express excess milk. If this is not done in a timely manner, stagnation of milk can lead to inflammation of the mammary gland - mastitis. However, you must follow all the rules of pumping and do not resort to it after each feeding: this will only increase the flow of milk.
-
Not enough milk is produced. Pumping will help normalize lactation, as it leads to an increase in the production of milk in the breast, which can be useful during a lactation crisis.
5 pumping inhibitions
In order not to harm herself and not leave the baby without breast milk, the mother must know and be sure to follow the basic rules of pumping:
-
Do not express more than 3 times a day if pumping is combined with breastfeeding because this will lead to excess milk production. If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day).
-
Do not express immediately after feeding, as this may lead to hyperlactation, ie. increased milk production.
-
Do not express "to the last drop". The main indicator by the end of pumping should be a feeling of relief in the chest.
 The female body regards the emptying of the breast without a trace as an increased need for milk by the child - and begins to produce more milk, which the baby cannot eat, therefore, there will be a threat of milk stagnation.
The female body regards the emptying of the breast without a trace as an increased need for milk by the child - and begins to produce more milk, which the baby cannot eat, therefore, there will be a threat of milk stagnation. -
Do not express during the night, as this may also lead to the formation of excess milk. The main hormone responsible for milk production - prolactin - has a daily rhythm of formation, most of all it is produced at night, in response to the baby sucking or pumping.
-
Do not express on the first day after the arrival of milk. Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace. If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Substances that signal that milk is being produced in excess appear in the filled breast after about 1 day. If you express all the milk accumulated in the chest earlier than in a day, then it will be produced in the same amount.
If you express all the milk accumulated in the chest earlier than in a day, then it will be produced in the same amount.
Hand Expression Technique
There are two ways to express - manually and with a breast pump. Usually, each mother chooses the most convenient option for her. It is better to do it manually at home, when a woman has enough time, since the whole process will take some time. Breast pumps will help a working mother, which greatly facilitate the pumping process.
Rules for hand pumping
It is best to express milk 10-15 minutes after the end of feeding the baby. Wash your hands thoroughly beforehand. If you use any breast cream, wipe the skin and nipples with a cotton swab or pad soaked in breast milk. Prepare a wide-mouth milk container by first washing it under running water and then sterilizing it (by boiling, in a steam sterilizer or in a dishwasher).
Sit comfortably, keeping your back straight, because pumping can take some time, and an uncomfortable position can cause back pain.
Gently grasp the chest: the little finger is under the chest at the ribs, the remaining fingers are positioned so as to support the chest from below. The thumb lies on top, about 3-4 cm from the nipple. In this case, the thumb and forefinger are located opposite each other, forming the letter "C".
Use your thumb and forefinger to gently press down on your chest and hold this position for a few seconds. In no case do not bring your fingers together, they should remain in the same position, the letter "C".
Repeat pressing, moving the palm in a circle - this way you will use all the ducts of the mammary gland.
Be patient, milk may not come out immediately, but only after a while. If you are pumping for the first time, check with your doctor or lactation consultant beforehand to show you how to proceed.
Manual pumping errors
Do not squeeze the nipple: this way you will only hurt yourself and injure the breast, and you will not express milk fully.
Do not press the palm too tightly against the skin, moving the hand across the chest so that there is no irritation and microtrauma.
Do not give up at the first unsuccessful attempts, be patient.
Breast pumps
Breast pumps make pumping much easier, because they are designed to fit all the anatomical features of the female breast.
Which one to choose? Breast pumps are divided into mechanical and electrical. In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
Mom usually chooses a breast pump model according to her taste and financial capabilities. It should be borne in mind that devices powered by batteries lose power faster than devices powered by the mains.
Many women are confused by the fact that electric breast pumps are loud enough. To date, there are a large number of silent devices, which is recommended to pay attention to when buying. The most effective are electric breast pumps that express both breasts at the same time and have the option of adjusting the thrust force and suction speed.
When choosing a breast pump, pay attention to the presence of the “boil and sterilize” marking. There must be the possibility of such heat treatment of parts of the apparatus. If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
Rules for expressing with a breast pump
Before pumping for the first time, carefully read the instructions for the device. Check that it is properly assembled.
Sterilize the funnel and sump (boil or use a sterilizer).
Position the funnel so that the nipple is in the center of the funnel.
The draw should be the lowest, especially at first, until the breast is accustomed to expressing with a breast pump. Each breast must be pumped until a feeling of relief, add 2 minutes to this time. On average, the process will take about 15 minutes.
Pumping, like manual pumping, should be carried out some time after feeding.
Basic mistakes when expressing with a breast pump
Incorrect position of the funnel of the breast pump can cause pain to the woman. Remember: the nipple should be located strictly in the center of the funnel of the device.
Very long pumping. Do not exceed the time required to collect milk, this can lead to hyperlactation (production of excess milk).
Very strong traction. If your breast pump has a selectable thrust function, you should use the smallest one so as not to hurt your breasts.
Care of the breast pump. A breast pump, like any machine, needs proper care. It must not be clogged so as not to contaminate the milk.
Each model has a care instruction, which you should definitely read before using the device.
When washing, always disassemble the pump completely, removing even the smallest parts. This will prevent stagnation of milk residues in them.
Before each use, sterilize all parts of the machine that come into contact with milk. This can be done with a sterilizer.
Milk defrosting
Never thaw or heat breast milk in a microwave oven. When heated in the microwave, the milk warms up unevenly, while feeding the baby can burn. Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
To defrost breast milk, place it on the refrigerator shelf, and when it becomes liquid, heat it up. To do this, lower the milk bottle into hot water or put it under hot water. Also, special heaters can be used to warm milk.
If you have questions or don't know how to express, it's worth talking to a specialist. The doctor will not only tell, but also show how to do it correctly, give recommendations on the pumping schedule and advise which method is better to choose.
Remember that milk is undoubtedly a valuable food for the baby, but feeding with expressed milk should be used in exceptional cases.
At the School of Moms, our doctors talk in detail not only about how and when to express milk correctly, but also about how to properly attach a baby to the breast, how to avoid common problems with breastfeeding, such as lactostasis, as well as the rules for self-examination mammary glands.
Transitional milk | Stages of breast milk production
During the first couple of weeks after birth, the composition of breast milk changes dramatically. Learn about the amazing properties of this transitional milk.
Share this information
A newborn changes literally every day, and the same can be said about breast milk. With the advent of milk, the breast can increase to an impressive size, and changes occur not only on the outside, but also inside. During the first week, the milk-producing cells and the connections between them are rebuilt and prepare the breast for the upcoming feeding. 1 From now until about the end of the second week, they will produce so-called transitional milk. 2
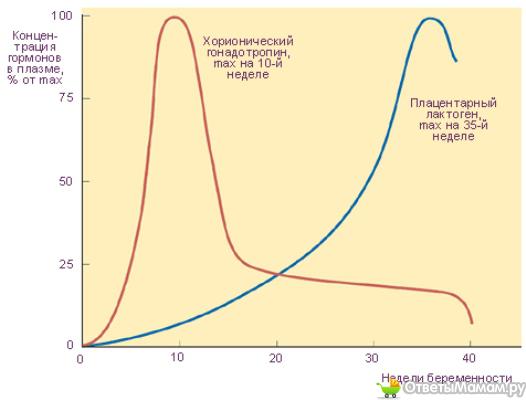
“After delivery of the placenta, levels of progesterone, the pregnancy hormone, begin to decline rapidly,” explains Professor Peter Hartmann of the University of Western Australia, a leading authority on the composition of breast milk. “As progesterone levels decrease, milk synthesis increases and the composition is approaching the norm, although a couple more weeks are needed for the full maturation of the milk.
Breastmilk stages: intermediate phase
If colostrum is the baby's very first food and mature milk is its main food for a long time, then transitional milk is a kind of bridge between them.
They should be considered as three different stages of milk production, not three types of milk. The main components remain unchanged throughout breastfeeding, only their quantity changes depending on the circumstances. During the transition period, the composition of milk undergoes the most significant changes, and this happens every day in accordance with the changing needs of the child.
Milk changes because it contains bioactive components, including cells, hormones and beneficial bacteria. The transition to mature milk does not happen all at once: the composition changes gradually and in strict accordance with the developmental needs of the baby. 3.4
“The amount of milk produced by the mother is the main influence on the composition of milk,” says Professor Hartman. “The composition of milk at low and higher levels of production is different.”
Transitional milk: increase
As your child grows, he needs more food and a different ratio of nutrients. The amount of milk produced during this period also increases significantly. You can produce 600-700 ml per day, 5 which is quite an impressive amount compared to the small amount of colostrum produced in the early days.
"The composition of milk in all mammals varies according to the needs of the young"
Your breasts are now in “boost” mode: your body is learning to produce the amount of milk your baby needs. The breast becomes more mature, as does the milk. Compared to colostrum, transitional milk contains more fat and lactose, a natural sugar that gives your baby energy. 2
“The level of lactose rises sharply in the first two or three days after birth,” says Prof. Hartmann, “Fat composition also changes: the content of medium-chain fatty acids C10 and C12 increases. They are an easily digestible source of energy and have antiviral properties. In addition, sodium and chloride levels are greatly reduced during this period, so that the milk has a very low salt content.”
Protein: correct ratio
The protein content of breast milk also does not remain unchanged. There are two types of proteins in human milk: casein and whey. Under the influence of acid in the child's stomach, casein turns into a solid mass (cottage cheese) and gives a feeling of satiety for a longer time. It also has antimicrobial properties. Whey, on the other hand, is rich in antibodies and remains liquid, so it is easily absorbed, which is especially important for newborns. As the child's gastrointestinal tract strengthens, the ratio of casein to whey in milk gradually changes. If in colostrum it is about 90:10, then after a month it reaches 60:40, and after a year of breastfeeding, the balance is set at 50:50. 6
This ratio of proteins is ideal for humans, as our body grows relatively slowly and the brain is constantly growing and becoming more complex. In addition, it promotes the supply of all the essential amino acids that a child needs for the healthy development of the brain, eyes and other organs.
The amount of whey protein in human milk is significantly higher than that of other mammals. In cow's milk, the ratio of whey and casein is the opposite: 20:80 (therefore, it is not suitable for feeding children under one year old). 7
“Milk is designed to perform a specific task,” continues Professor Hartmann, “Some components are present in any milk, such as proteins and fats, but if you look at which proteins and which fats, it becomes clear which animal belongs to milk. The composition of milk in all mammals varies depending on the needs of the young.
Changing the protective properties of transitional milk
Although your baby is still very young, already in the first couple of weeks he begins to develop his own immune system, and now he needs your direct protection a little less.
The concentration of protective enzymes and antibodies in breast milk changes accordingly. The content of some substances, in particular lactoferrin (protective enzyme) and secretory immunoglobulin A (antibody), decreases, while other substances, such as the antibacterial enzyme lysozyme, on the contrary, increase. 8
“The protein content of milk decreases around this time,” says Prof. Hartmann, “The synthesis of protective proteins occurs at the same rate, but they are more diluted due to increased milk production.”
The concentration of minerals such as zinc, copper and magnesium, which support the development of the child's immune system, also decreases as the immune system strengthens. 9
When breast milk becomes fully mature
During the transition period, the composition of breast milk changes significantly. By the end of the first month, it becomes fully mature. This means that the child will be able to eat them further as they grow. The composition of milk will no longer change much, no matter how long you continue breastfeeding - a few months, a year or more.
Would you like to know more? Read our free e-book Surprising Breast Milk Facts or article on mature milk.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. 2 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74. 3 Munblit D et al. Colostrum and mature human milk of women from London, Moscow, and Verona: determinants of immune composition. Nutrients. 2016; 8(11): 695. - Moonblit, D. et al., "Colostrum and mature breast milk from women in London, Moscow, and Verona: major factors in immune composition. 4 Pons SM et al. Triacylglycerol composition in colostrum, transitional and mature human milk. Eur J Clin Nutr . 2000;54(12):878-882. — Pons SM, "Triacylglycerol in colostrum, transitional and mature human milk". Yur J Klin Nutr. 2000;54(12):878-882. 5 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr . 1988;48(6):1375-1386. - Neville M.S. et al., "Female Lactation Study: Milk Quantity in Lactating Women at the Beginning and Peak of Lactation." Am F Clean Nutr. 1988;48(6):1375-1386. 6 Kunz C, Lönnerdal B. Re-evaluation of the whey protein/casein ratio of human milk. 7 Martin CR et al. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8(5). - Martin S.R. et al., Review of Infant Feeding Issues: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5). 8 Lönnerdal B et al. Longitudinal evolution of true protein, amino acids and bioactive proteins in breast milk: a developmental perspective. J Nutr Biochem. 2017;41:1-11. - Lönnerdahl B. et al., "Longitudinal evolution of true proteins, amino acids and biologically active proteins of human milk: a development perspective." G Nutr Biochem. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." F Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
" Nutrients. 2016; 8(11): 695.
Acta Paediatr. 1992;81(2):107-112. Kunz S, Lonnerdal W. Act Pediatr.1992;81(2):107-112. - Kuntz S., Lönnerdahl B., "New Evaluation of Whey Protein/Casein in Breast Milk". Akta Pediatr. 1992;81(2):107-112.