Infant skin rashes on face
Rash on a baby's face: Pictures, causes, and treatments
In babies, most facial rashes are harmless and tend to clear up without treatment. Causes can include eczema, acne, and infection.
Sometimes, however, a rash on a baby’s face can indicate a more serious condition.
Being able to distinguish between different rashes can help a parent or caregiver know when to seek professional advice.
In this article, we describe common facial rashes in babies, treatments, and when to see a doctor.
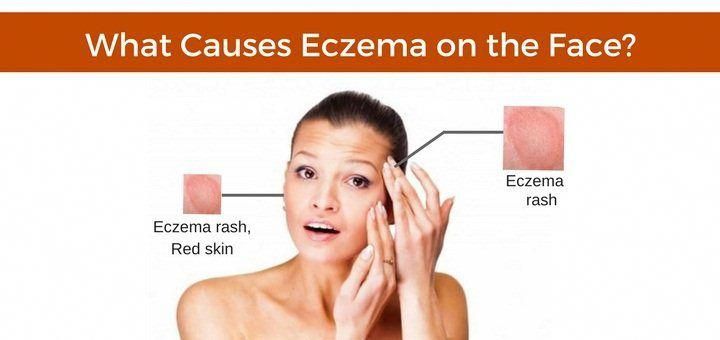
Eczema refers to a group of conditions that cause the skin to become rough, irritated, itchy, and inflamed.
These conditions are common in young children, often appearing between the ages of 6 months and 5 years. Many children grow out of their eczema.
According to the National Eczema Association in the United States, if eczema develops within the first 6 months of life, it tends to appear on the cheeks, chin, forehead, or scalp. The rash will be dry, red, and itchy.
Between the ages of 6 and 12 months, eczema may develop in other parts of the body. The elbows and knees are particularly susceptible when babies start to crawl.
Treatment
Although the exact cause of eczema is unknown, experts believe that both genetic and environmental factors can play a role.
Certain environmental triggers may over-activate the immune system, causing inflammation and skin irritation.
When trying to establish the cause of a child’s eczema, it may help to keep a diary of symptoms and potential triggers. By avoiding these triggers, it may be possible to prevent flare-ups of symptoms.
Below are some common triggers of eczema in babies:
- heat and sweating
- dry skin
- irritants, such as soaps, washing detergents, and cigarette smoke
- allergens, such as dust mites, pollen, and pet dander
- certain fabrics, such as wool and nylon
Treatments for eczema include:
- over-the-counter (OTC) moisturizers
- prescription creams and ointments, such as steroid creams
- immunosuppressant drugs
- phototherapy
A doctor can consult with a pediatric dermatologist and recommend a course of treatment. They can also advise about triggers and how to avoid them.
They can also advise about triggers and how to avoid them.
Check that over-the-counter treatments are suitable for infants.
Seborrheic dermatitis causes a rash to develop on areas of skin that contain many oil-producing glands.
In babies, the rash mainly appears on the scalp, and people commonly refer to it as cradle cap. However, cradle cap can also affect the cheeks, particularly around the eyes and nose.
The rash may have the following characteristics:
- redness and inflammation
- an oily or greasy appearance
- white or yellow scaly or crusty patches
Treatment
Cradle cap is generally harmless and usually disappears between 6 and 12 months of age.
If the child is not experiencing any discomfort, treatment may not be necessary.
For mild symptoms, OTC medications, such as antifungal creams and medicated shampoos, may help to relieve discomfort and speed healing. However, talk to a doctor before using these products on an infant.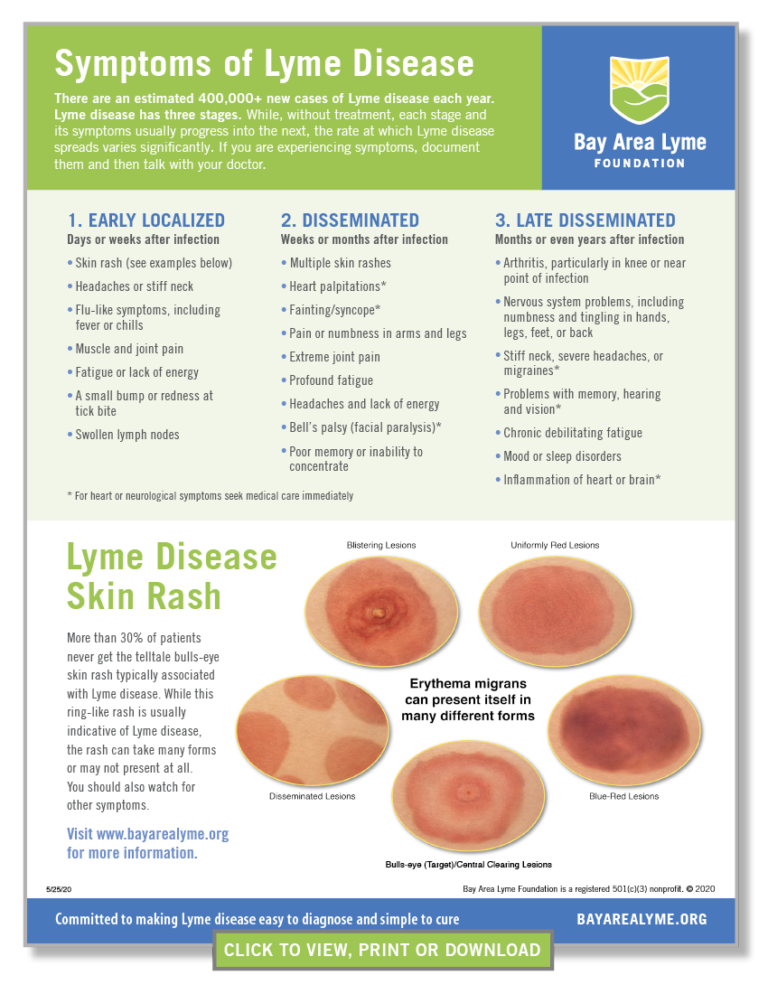
If the rash is scaly, applying mineral oil or petroleum jelly to the baby’s scalp 1 hour before using an anti-dandruff shampoo can help loosen and remove the scales.
For babies with more severe symptoms, a doctor may prescribe topical steroids to reduce inflammation.
Particularly severe cradle cap can increase the risk of infection. See a doctor immediately, if the baby’s skin:
- feels hot
- oozes fluid
- gives off an unpleasant odor
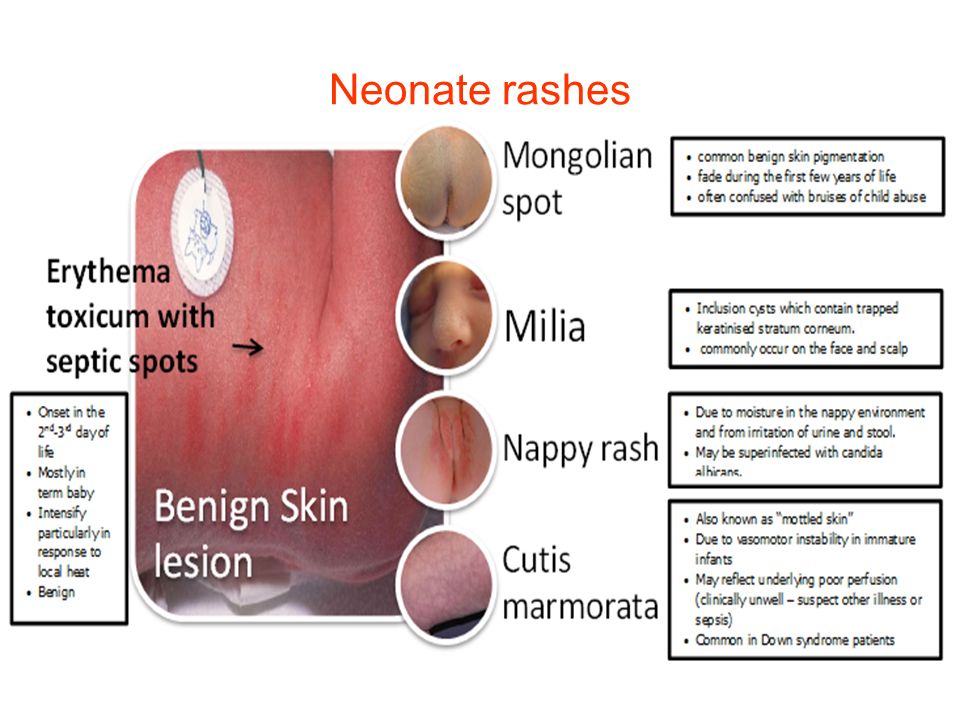
Around 40–50 percent of healthy newborns develop milia, which are tiny white or yellow bumps about 1–3 mm in size.
Milia result from blocked pores and typically develop on the face, often around the eye and nose. The bumps can appear in large numbers, and usually a roughly equal number form on each side of the face.
In babies, milia can also develop in the mouth. In this case, the medical name is Epstein pearls.
Treatment
Milia tends to clear up on their own within a few weeks, once the pores open up.
No treatment is usually necessary. Avoid using creams and ointments on the baby’s skin, as these can further clog the pores and lead to more milia.
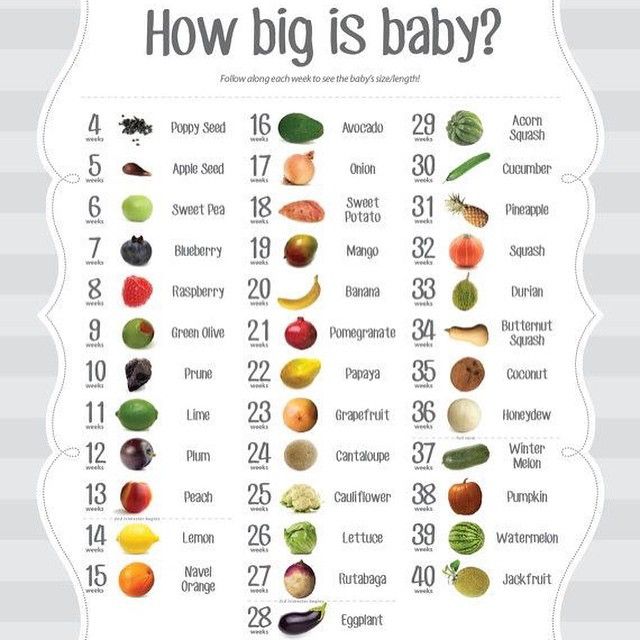
Newborn, or neonatal, acne causes small, red pimples to develop, usually around 2–6 weeks of age. However, some babies are born with them.
The medical term for acne that develops between 6 weeks and 6 months of age infantile acne, and we discuss this below.
Neonatal acne affects around 20 percent of newborns, according to the American Academy of Dermatology.
The pimples tend to develop on the baby’s cheeks and nose, but breakouts can also appear on the:
- forehead
- chin
- scalp
- neck
- chest
- upper back
Treatment
Generally, newborn acne is not a cause for concern. It is unlikely to cause scarring and tends to clear up without treatment after a few weeks or months.
Parents and caregivers should:
- gently wash the baby’s skin with lukewarm water
- avoid scrubbing affected areas
- avoid oily or greasy skincare products
- seek advice from the child’s doctor before using acne medicines or cleansing products
Infantile acne develops in babies older than 6 weeks. It typically appears between 3 and 6 months of age.
It typically appears between 3 and 6 months of age.
Infantile acne is less common than newborn acne. Symptoms can be more severe and may require treatment.
Before treating infantile acne, it is important to rule out other conditions, such as such as eczema and infections, which are more common in this age group.
Treatment
Infantile acne usually clears up within 6–12 months after it first appears.
After diagnosis, a dermatologist can advise about treating the acne and preventing scarring. If they suspect that the acne results from an underlying medical condition, they may consult a specialist.
A doctor can diagnose the cause of a rash.
Slapped cheek syndrome is a viral infection. Anyone can get it, but it most commonly develops in school-aged children.
Other names for the syndrome include fifth disease and erythema infectiosum. It results from infection with the B19 parvovirus.
The defining characteristic is a bright red rash on one or both cheeks. The rash is not usually painful. It typically appears within 4–14 days of infection.
The rash is not usually painful. It typically appears within 4–14 days of infection.
The cheek rash often disappears in a few days, but another rash may develop on areas such as the chest, arms, and legs. This rash usually lasts for 7–10 days, but it may come and go.
The rash on the body is usually blotchy and light in color. It can be itchy, but it is not typically painful.
Slapped cheek syndrome can also cause the following symptoms:
- a fever of 38°C or higher
- a headache
- a runny nose
- a sore throat
Children can initially pass the infection to other children, but it usually stops being contagious once the rash appears.
Treatment
The symptoms of slapped cheek syndrome are usually mild, and the underlying infection typically clears up without treatment.
OTC medications, such as acetaminophen and ibuprofen, can help relieve any discomfort. However, speak to a doctor before giving these drugs to babies or young children.
Never give a child aspirin, as it may increase the risk of a serious condition called Reye’s syndrome.
Most rashes on babies’ faces are harmless. They usually clear up on their own.
However, a rash in this area can indicate an infection or an underlying health condition.
See a doctor if the rash is severe, or if the baby has:
- fluid-filled blisters
- a fever
- a loss of appetite
- red streaks extending from the rash
- tiny red or purple spots that do not fade when someone applies pressure
- swollen lymph nodes
- lethargy
- a cough
Facial rashes are common in babies and young children. The many possible causes include eczema, acne, and infection.
Most rashes clear up without treatment. However, see a doctor if a rash is severe or persistent, or if it accompanies other symptoms.
Read the article in Spanish.
Slapped cheek syndrome - NHS
Slapped cheek syndrome (also called fifth disease) is common in children and should get better on its own within 3 weeks. It's rarer in adults, but can be more serious.
It's rarer in adults, but can be more serious.
Check if it's slapped cheek syndrome
The first sign of slapped cheek syndrome is usually feeling unwell for a few days.
Symptoms may include:
- a high temperature
- a runny nose and sore throat
- a headache
Credit:
SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/550792/view
A few days later, a spotty rash may appear on the chest, arms and legs. The rash can be raised and itchy. It may be harder to see on brown and black skin.Credit:
John Kaprielian/SCIENCE PHOTO LIBRARY https://www. sciencephoto.com/media/618192/view
sciencephoto.com/media/618192/view
How long it lasts
The cheek rash usually fades within 2 weeks.
The body rash also fades within 2 weeks, but sometimes lasts for up to a month, especially if you're exercising, hot, anxious or stressed.
Adults might also have joint pain and stiffness. This can happen in children too, but it's rare. Joint pain can continue for many weeks, even after the other symptoms have gone.
If you're not sure your child has slapped cheek syndrome
Look at other rashes in babies and children.
Things you can do yourself
You do not usually need to see a GP for slapped cheek syndrome.
There are some things you can do to ease the symptoms.
Do
-
rest
-
drink plenty of fluids to avoid dehydration – babies should continue their normal feeds
-
take paracetamol or ibuprofen for a high temperature, headaches or joint pain
-
use moisturiser on itchy skin
-
speak to a pharmacist about itchy skin – they can recommend the best antihistamine for children
Important
Tell your midwife or a GP if you're pregnant or have a weakened immune system and have been near someone with slapped cheek syndrome.
Non-urgent advice: See a GP if:
you think you have slapped cheek syndrome and:
- you're pregnant – there's a very small risk of miscarriage or other complications
- you have a blood disorder, such as sickle cell disease or thalassaemia – there's a risk of severe anaemia
- you have a weakened immune system – for example, because of chemotherapy or diabetes
Ask for an urgent appointment if you have:
- very pale skin
- shortness of breath
- extreme tiredness
- fainting
These can be signs of severe anaemia and you might be sent to hospital for a blood transfusion.
How slapped cheek syndrome is spread
It's hard to avoid spreading slapped cheek syndrome because most people do not know they have it until they get the rash.
You can only spread it to other people before the rash appears.
Slapped cheek syndrome is caused by a virus (parvovirus B19). The virus spreads to other people, surfaces or objects by coughing or sneezing near them.
To reduce the risk of spreading the virus:
- wash your hands often with water and soap
- use tissues to trap germs when you cough or sneeze
- bin used tissues as quickly as possible
Information:
You do not have to stay off work or school after the rash appears.
Let the school or teacher know if your child has slapped cheek syndrome.
Page last reviewed: 18 February 2021
Next review due: 18 February 2024
Red pimples on the face of a newborn: symptoms, causes and treatment
Allergic rash in a newborn
An allergy in a baby is an unfavorable immune response of a child's body to a potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberry;
- nuts.
The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.
Neonatal acne
Neonatal acne may appear in the first weeks of a child's life on the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the cause of the appearance of acne is increased production of sebum , which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
It is assumed that the cause of the appearance of acne is increased production of sebum , which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
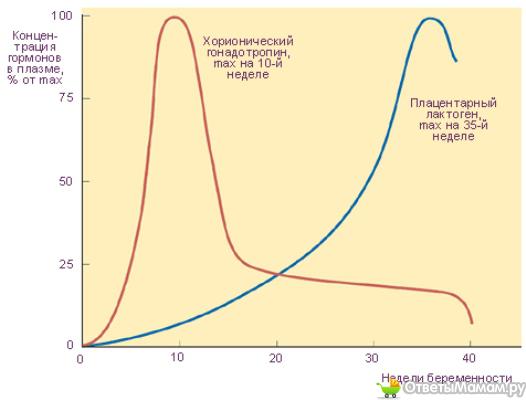
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system. The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Miliaria
Miliaria is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small blisters with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Miliaria itself is not dangerous to the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection. In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn.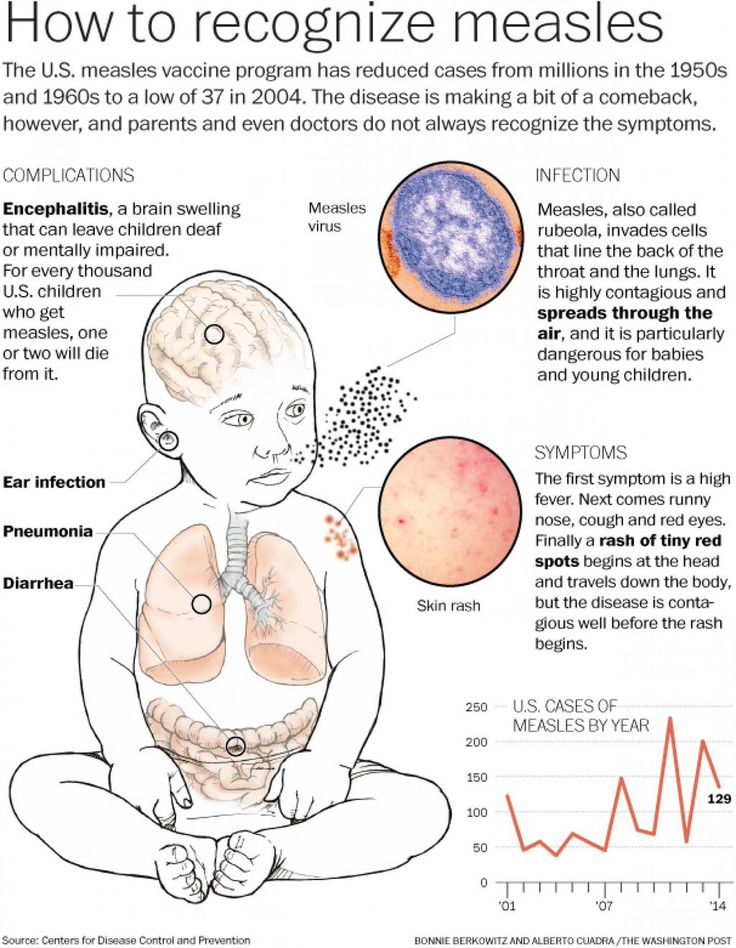 These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
In fact, the disease is caused by a high content of maternal hormones in the blood or a change in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only take care of proper care , but diligently remove the crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns.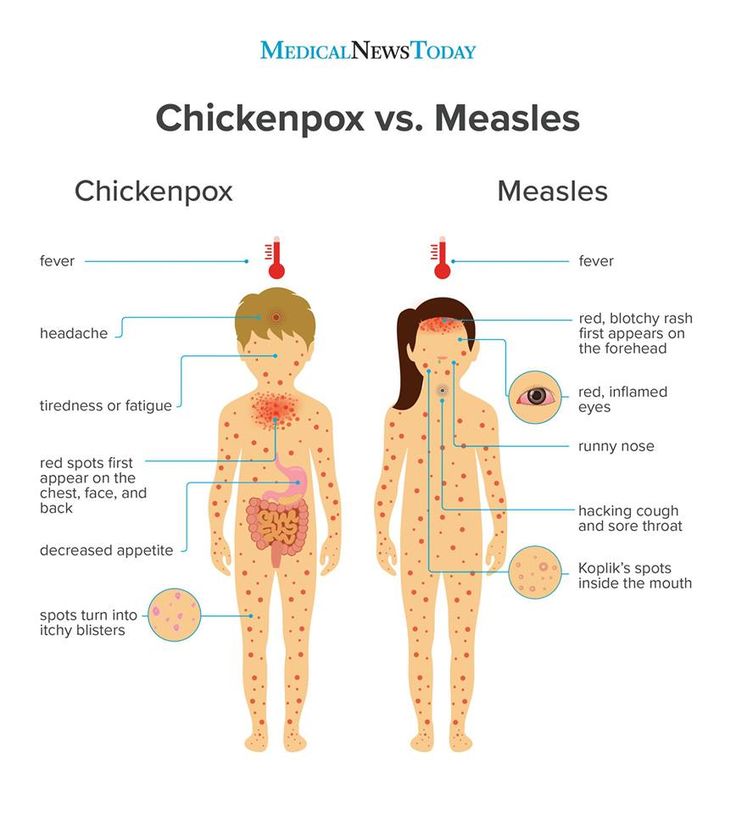 He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Milk crust cream which helps to completely remove milk crusts in an average of 7 days [5.3].
Atopic dermatitis
Atopic dermatitis is an allergic disease that is accompanied by chronic inflammation of the skin. Causes of an uncontrolled allergic reaction in infants are:
- food allergens - animal protein, soy products, certain types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.

Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.
 1]
1] - Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper zone in infants. Rash appears as a result of prolonged body contact with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious). The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
9 indicated for non-drug treatment of pathology0006 air baths [7], bathing in decoction of string and celandine [8] and meticulous hygiene procedures. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, restores and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
______________________________________________________________________________________
References:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Herani M.I., Ando I. Acne in infancy and acne genetics // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3. Zanko NI Efficiency of new technologies for skin care in young children: Ph.D. dis. ... cand. honey. Sciences, M., 2000
Zanko NI Efficiency of new technologies for skin care in young children: Ph.D. dis. ... cand. honey. Sciences, M., 2000
4. Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis.
N Engle Gee Med. 360(4):387-96 (2009 January).
5. Results of the study 1035 F4.
5.1 Test results 1016F10.01.02
5.2 Test results 1008F4.01.16
5.3 Results of the study 1042F3.01.24
6. Thompson M., Hanifin J. Effective treatment of atopic dermatitis in children alleviates problems associated with food allergies
// GM Akad Dermatol.2005; 53: S214-S219.
7. Galliamova Yu.A. Diaper dermatitis and skin trauma in children. Attending doctor. – 2013; 9:42-6.
8. Zverkova F.A. Skin diseases in young children. SPb.: Sotis, 1994.
9. Tamrazova OB, Zaslavsky DV Diseases of the sebaceous glands in infants. Medical advice. 2019; 2:152-160.
10. Atopic-prone skin: latest discoveries (Laboratoire Expansion Center for Development and Research)
11. Inhibits the synthesis of inflammatory mediators. “A study of the activity of sunflower oil distillate on inflammatory mediators. June 2010»
“A study of the activity of sunflower oil distillate on inflammatory mediators. June 2010»
Rashes in babies | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
The rash peaks at the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with pityriasis scales, which can form a crust (“cap”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin in 1st to 2nd week of life or later, resolves spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a number of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
As a rule, removal of the damaging agent and short-term use of anti-inflammatory creams leads to a quick recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of age.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, coarse fabrics, detergent residues on clothing, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc. ). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.