Folate supplementation pregnancy
Folic Acid | CDC
CDC urges all women of reproductive age to take 400 micrograms (mcg) of folic acid each day, in addition to consuming food with folate from a varied diet, to help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida).
About folic acid
Folic acid is a B vitamin. Our bodies use it to make new cells. Think about the skin, hair, and nails. These–and other parts of the body – make new cells each day. Folic acid is the synthetic (that is, not generally occurring naturally) form of folate used in supplements and in fortified foods such as rice, pasta, bread, and some breakfast cereals
Why folic acid is important before and during pregnancy
When the baby is developing early during pregnancy, folic acid helps form the neural tube. Folic acid is very important because it can help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida). The neural tube forms the early brain and spine.
Women of reproductive age need 400 mcg of folic acid every day
- All women of reproductive age should get 400 mcg of folic acid every day to get enough folic acid to help prevent some birth defects because
- About half of U.S. pregnancies are unplanned, and
- Major birth defects of the baby’s brain or spine occur very early in pregnancy (3-4 weeks after conception), before most women know they are pregnant.
- When taking folic acid, a higher dose than 400 mcg of folic acid each day is not necessarily better to prevent neural tube defects, unless a doctor recommends taking more due to other health conditions.
- When planning to become pregnant, women who have already had a pregnancy affected by a neural tube defect should consult with their healthcare provider. CDC recommends that these women consume 4,000 mcg of folic acid each day one month before becoming pregnant and through the first 3 months of pregnancy.

- When planning to become pregnant, women who have already had a pregnancy affected by a neural tube defect should consult with their healthcare provider. CDC recommends that these women consume 4,000 mcg of folic acid each day one month before becoming pregnant and through the first 3 months of pregnancy.
Learn more about CDC’s folic acid recommendations here.
Learn more about the recommended intake level of folic acid here.
When to start taking folic acid
Every woman of reproductive age needs to get folic acid every day, whether she is planning to get pregnant or not, to help make new cells.
Are folate and folic acid the same thing?
The terms “folate” and “folic acid” are often used interchangeably, even though they are different. Folate is a general term to describe many different types of vitamin B9.
Types of folate can include
- Dihydrofolate (DHF)
- Tetrahydrofolate (THF)
- 5, 10-methylenetetrahydrofolate (5, 10-Methylene-THF)
- 5-methyltetrahydrofolate (5-Methyl-THF or 5-MTHF)
Food fortification is a way to add vitamins or minerals, or both, to foods. Some rice, pasta, bread, and breakfast cereals are fortified with folic acid. These foods are labeled “enriched.” Folic acid is a specific type of folate that does not generally occur naturally.
Folic acid is the ideal form of folate to use for food fortification. It is more stable than types of natural food folate, which can easily be broken down by heat and light. Folic acid is better suited for food fortification because many fortified products, such as bread and pasta, are cooked.6
CDC recommends that women of reproductive age who could become pregnant consume at least 400 micrograms (mcg) of folic acid every day. However, it’s difficult to get 400 mcg of folic acid through diet alone. You can get 400 mcg of folic acid each day by taking a vitamin with folic acid in it, eating fortified foods, or a combination of the two, in addition to consuming a balanced diet rich in natural food folate.
How to get enough folic acid to prevent neural tube defects
In addition to eating foods with folate from a varied diet, women can get folic acid from
- Taking a vitamin that has folic acid in it:
- Most vitamins sold in the United States have the recommended daily amount of folic acid (400 mcg) that women need for the prevention of neural tube defects.
 Vitamins can be found at most local pharmacy, grocery, or discount stores.
Vitamins can be found at most local pharmacy, grocery, or discount stores.
- Most vitamins sold in the United States have the recommended daily amount of folic acid (400 mcg) that women need for the prevention of neural tube defects.
- Eating fortified foods:
- You can find folic acid in some breads, breakfast cereals, and corn masa flour.
- Getting a combination of the two: taking a vitamin that has folic acid in it and eating fortified foods.
If taking folic acid for reasons other than neural tube defect prevention, talk to your healthcare provider.
Learn more about where to find folic acid in the United States here.
More Information
For more information, visit the Frequently Asked Questions page.
You can also contact CDC-INFO in English or Spanish:
- 1-800-CDC-INFO (800-232-4636)
- TTY: 1-888-232-6348
- In English
- en español
Folic acid | March of Dimes
Taking folic acid before and during early pregnancy can help prevent neural tube defects in your baby.
Before pregnancy, take a vitamin supplement that has 400 micrograms of folic acid in it every day.
During pregnancy, take a prenatal vitamin that has 600 micrograms of folic acid in it every day.
Take a vitamin supplement with folic acid every day, even if you’re not trying to get pregnant.
You can get folic acid from food, too. Look for fortified foods to make sure you’re getting enough.
What is folic acid?
Folic acid is a vitamin that every cell in your body needs for healthy growth and development. If you take it before pregnancy and during early pregnancy, it can help protect your baby from birth defects of the brain and spine called neural tube defects. The neural tube is the part of a developing baby that becomes the brain and spinal cord. NTDs happen in the first month of pregnancy, before you may know that you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
NTDs affect about 3,000 pregnancies each year in the United States. If all women take 400 micrograms (also called mcg) of folic acid every day before getting pregnant and during early pregnancy, it may help prevent up to 7 in 10 (70 percent) NTDs. Because nearly half of all pregnancies in the United States are unplanned, all women who can get pregnant should take folic acid every day.
Because nearly half of all pregnancies in the United States are unplanned, all women who can get pregnant should take folic acid every day.
Some studies show that folic acid also may help prevent birth defects in a baby’s mouth called cleft lip and palate. A cleft lip is a birth defect in which a baby’s upper lip doesn’t form completely and has an opening in it.
How can you get enough folic acid?
There are several ways to get enough folic acid:
- Taking a vitamin that has folic acid in it
- Eating foods with folate from a varied diet
- Eating fortified foods
- Getting a combination of the two: taking a vitamin that has folic acid in it and eating fortified foods
How much folic acid do you need?
Here’s what you need to know about taking folic acid to prevent NTDs:
Most women
To help prevent NTDs in your baby, take a vitamin supplement with 400 mcg of folic acid every day before you get pregnant. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. Start taking 400 mcg of folic acid each day at least 1 month before pregnancy through the first 12 weeks of pregnancy. Your folic acid supplement can be:
A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. Start taking 400 mcg of folic acid each day at least 1 month before pregnancy through the first 12 weeks of pregnancy. Your folic acid supplement can be:
- A multivitamin. This is a pill that contains many vitamins and other nutrients that help your body stay healthy.
- A prenatal vitamin. This is a multivitamin made for pregnant women. Your health care provider may give you a prescription for prenatal vitamins, or you can get them over the counter without a prescription.
- A supplement that contains just folic acid
Take a vitamin supplement with 400 mcg of folic acid each day, even if you’re not trying to get pregnant.
During pregnancy, take a prenatal vitamin each day that has 600 mcg of folic acid in it. Folic acid only works to prevent NTDs before and during the first few weeks of pregnancy. Later in pregnancy, you need 600 mcg of folic acid each day to help your baby grow and develop.
Later in pregnancy, you need 600 mcg of folic acid each day to help your baby grow and develop.
Women at high risk for NTDs
If you’re at high risk for having a baby with an NTD, take 4,000 mcg of folic acid each day to help prevent an NTD. Start taking 4,000 mcg of folic acid 3 months before you get pregnant through 12 weeks of pregnancy. You’re at high risk if:
- You’ve had a baby with an NTD in the past.
- You or your partner has an NTD.
- Your partner has a child with an NTD.
Studies show that taking 4,000 mcg of folic acid before and during early pregnancy can help reduce your risk of having another baby with an NTD by about 70 percent. Ask your provider how to safely get this much folic acid. It’s not safe to take several multivitamins or prenatal vitamins because you can get too much of other nutrients, which may be harmful to your health. Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
How can you get folic acid from food?
You can get folic acid from food. Some foods are fortified with folic acid. Fortified means a food has folic acid added to it. Check the product label to see how much folic acid you get in each serving. Look for the word “fortified” or “enriched” on labels on foods like:
- Bread
- Breakfast cereal
- Cornmeal
- Flour
- Pasta
- Products made from a kind of flour called corn masa, like tortillas, tortilla chips, taco shells, tamales and pupusas
- White rice
Some fruits and vegetables are good sources of folic acid. When folic acid is found naturally in food it’s called folate. Foods that are good sources of folate are:
- Beans, like lentils, pinto beans and black beans
- Leafy green vegetables, like spinach and Romaine lettuce
- Asparagus
- Broccoli
- Peanuts (But don’t eat them if you have a peanut allergy.)
- Citrus fruits, like oranges and grapefruit
- Orange juice (100 percent juice is best.
 This means one serving of juice is equal to one serving of fruit.)
This means one serving of juice is equal to one serving of fruit.)
It’s hard to get all of the folic acid you need from food. Even if you eat foods that have folic acid in them, take your vitamin supplement each day, too.
How do you read a product label to see how much folic acid is in a vitamin supplement?
To find out if a vitamin supplement has folic acid in it, check the label (also called supplement facts). The label is usually on the back of the bottle. Look for the word “folate” on the label to see how much folic acid you’re getting. The label tells you this information:
- Serving size. This tells you how much of the product is in one serving. One multivitamin usually is one serving.
- Servings per container. This tells you how many servings are in a multivitamin bottle. For example, if two pills are one serving and the bottle has 30 multivitamins in it, that’s 15 servings.
- Nutrients, like vitamin D, folate and calcium, in each serving
- Daily value (also called DV) of one serving.
 DV is the amount of a nutrient in a serving. For example, if the DV of folic acid in a multivitamin is 50 percent, that multivitamin gives you 50 percent (half) of the folic acid you need each day.
DV is the amount of a nutrient in a serving. For example, if the DV of folic acid in a multivitamin is 50 percent, that multivitamin gives you 50 percent (half) of the folic acid you need each day.
Vitamin supplement labels now list “mcg DFE of folate,” which stands for dietary folate equivalent. It’s the amount of folate your body absorbs. If a serving has less than 400 mcg DFE of folate, you need more than one serving to get all the folic acid you need each day.
Labels on food products don’t always list the amount of folic acid in the product. Newer food labels that list folic acid will list mcg DFE of folate, just like for vitamin supplements.
If you have an MTHFR variant, can taking folic acid help prevent NTDs in your baby?
Yes. If you have an MTHFR variant, taking 400 mcg of folic acid every day before and during early pregnancy can help prevent NTDS in your baby.
MTHFR stands for methylenetetrahydrofolate reductase. It’s an enzyme (protein) that helps your body break down and use folate.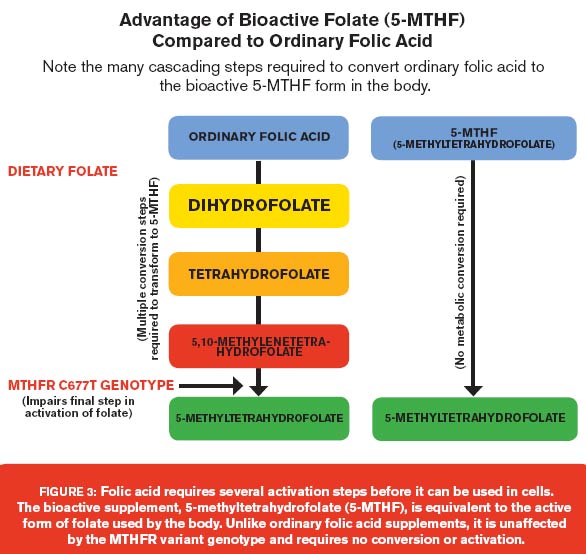 One MTHFR variant (called MTHFRTT or CT genotype) is a change in your body’s MTHFR gene that makes you use folate more slowly than usual. Genes are parts of your body’s cells that store instructions for how your body grows and works. They are inherited (passed from parents to children). MTHFR variants are inherited. If you know you have an MTHFR variant or you think it runs in your family, talk to your provider.
One MTHFR variant (called MTHFRTT or CT genotype) is a change in your body’s MTHFR gene that makes you use folate more slowly than usual. Genes are parts of your body’s cells that store instructions for how your body grows and works. They are inherited (passed from parents to children). MTHFR variants are inherited. If you know you have an MTHFR variant or you think it runs in your family, talk to your provider.
Your provider may want to test you for an MTHFR variant if you have high levels of a substance in your blood called homocysteine. Too much homocysteine in your blood can cause heart conditions, blood clots and stroke. You can find out your homocysteine levels with a blood test. If your level is high, you can have a genetic test to see if you have an MTHFR variant. A genetic test looks for changes in genes that can cause birth defects or other medical conditions.
You may have heard not to take folic acid if you have an MTHFR variant because it can increase your risk of pregnancy complications and your baby having health problems.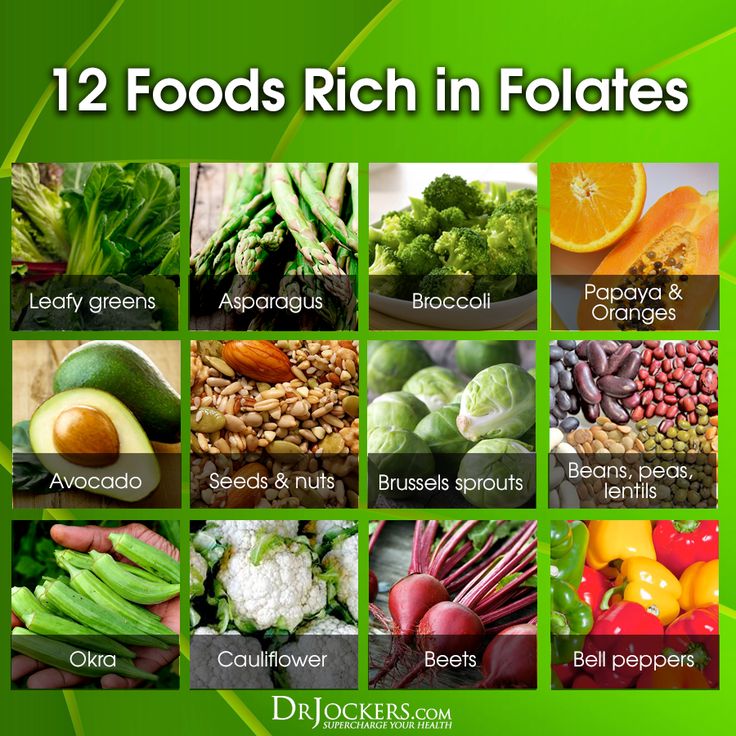 The Centers for Disease Control and Prevention (also called CDC) recommends that all women take 400 mcg of folic acid every day before and during early pregnancy. If you have an MTHFR variant, talk to your provider.
The Centers for Disease Control and Prevention (also called CDC) recommends that all women take 400 mcg of folic acid every day before and during early pregnancy. If you have an MTHFR variant, talk to your provider.
Additional versions of this article are available in: Arabic, Chinese Simplified, Hindi, and Urdu
Translated documents are courtesy of the employees of CooperSurgical Inc.
Folic Acid Health Action Sheet
More information
CDC
Show Your Love Preconception Health
Last reviewed: May 2020
Folic acid for pregnancy planning
Our services
Surrogate mothers are urgently needed.
Requirements: physical and mental health, presence of own children is obligatory, age up to 35 years. For all questions, please contact:
8(495)2235324, 8(926)0423057
home » About clinic » Folic acid when planning pregnancy
Any woman who plans to soon become pregnant and become a mother should consciously and carefully prepare for this new status. And if everyone knows about a healthy lifestyle, parting with bad habits and walking in the fresh air, then expectant mothers often ignore the intake of certain vitamins and medicines before pregnancy. One such remedy is folic acid.
And if everyone knows about a healthy lifestyle, parting with bad habits and walking in the fresh air, then expectant mothers often ignore the intake of certain vitamins and medicines before pregnancy. One such remedy is folic acid.
What is folic acid?
Folic acid is vitamin B9. Often you can hear the generalized name - folates, they are derivatives of this vitamin. We must understand that we get them from food, and folic acid tablets are a synthetic agent that is already converted into folates inside the body.
All derivatives of vitamin B9 play an important role in hematopoiesis, that is, the formation of new blood cells. Therefore, the lack of these substances leads to anemia - a condition in which there are not enough red blood cells, or they are irregular in shape and do not perform their functions. Folates have another very important feature: they stimulate the formation of nucleic acids (DNA and RNA), which are the basis of all body cells. Therefore, it is folic acid that is necessary for all rapidly dividing human tissues, including embryonic tissues.
Therefore, it is folic acid that is necessary for all rapidly dividing human tissues, including embryonic tissues.
The role of folic acid:
- participates in the formation of DNA in all cells, that is, the source of hereditary information;
- stimulates hematopoiesis;
- indirectly blocks the formation of cancer cells;
- restores muscle tissue;
- during pregnancy: plays a role in the laying and development of the nervous tissue of the embryo, participates in the formation of placental vessels.
Why do you need folate during pregnancy?
During pregnancy, especially in the early stages, the consumption of folate increases dramatically. All cells of the embryo are intensively dividing in order to eventually form full-fledged tissues. The nervous tissue of the future man is transformed especially quickly and difficultly. And it is she who requires a large amount of folic acid.
Folic acid deficiency during pregnancy can occur due to the following reasons:
- Insufficient intake of folate from food.
- Folate malabsorption (in chronic inflammatory diseases of the stomach and intestines).
- Genetic disorders of the folate cycle. In rare cases, a woman's body lacks the necessary enzymes (MTHFR). As a result, folic acid is not converted to folates, and they do not perform the necessary functions. Intermediate metabolic products accumulate in the body, which can lead to cardiovascular diseases, tumor processes, infertility and miscarriage. In the presence of such a mutation, it is recommended to take folic acid derivatives, for example, Metafolin. It is absorbed faster and in greater volume.
- Taking certain anti-epilepsy drugs and hormonal drugs dramatically reduces blood folate levels:
- oral contraceptives;
- barbiturates, diphenylhydantoin;
- sulfa drugs (for example, biseptol), which inhibit the synthesis of vitamin B9 by the intestinal microflora;
- drinking alcohol also lowers their levels.

At what stage of pregnancy should I take folic acid supplements?
Folic acid intake to prevent fetal malformations should be started already at the stage of preparation for pregnancy, at least three months before the intended conception. That is why pregnancy should be planned. If conception occurred unexpectedly, then you need to start taking the drug as soon as it became known.
Reasons for taking folates at the stage of pregnancy planning:
- If a woman has an unbalanced diet, her folic acid level can be low, so it takes time to replenish her reserves. It usually takes three to four months.
- The neural tube of the fetus is laid at such an early stage that a woman may not even be aware of the pregnancy, especially with a long menstrual cycle.
- Folate deficiency can make pregnancy difficult.
Doctors of the Intime Family Planning Clinic give the following recommendations for taking folic acid: in most cases, three months before conception and throughout pregnancy, you need to take 400 micrograms of folic acid per day. In some cases, the dosage is advised to increase: up to 1 mg per day for epilepsy and diabetes; up to 4 mg per day if there have been children with neural tube defects in the past Increased doses of folates can only be prescribed by a doctor after a thorough examination. The dose of folic acid during pregnancy remains the same.
In some cases, the dosage is advised to increase: up to 1 mg per day for epilepsy and diabetes; up to 4 mg per day if there have been children with neural tube defects in the past Increased doses of folates can only be prescribed by a doctor after a thorough examination. The dose of folic acid during pregnancy remains the same.
We wish you an easy pregnancy and healthy babies!
×
Send a request for a free consultation
We provide the first free consultation for new patients. Just leave your contact details and we will contact you within a business day.
Your name
Your Phone
Choose a service Family PlanningIn vitro fertilizationMen's healthWomen's healthTests
By clicking on the button, you consent to the processing of personal data and agree to the privacy policy.
The use of folic acid in the process of preconception preparation and during pregnancy
Despite the fact that the health of the pregnant woman and her unborn child is one of the priorities of modern medicine, such pregnancy complications as preeclampsia, spontaneous miscarriage, preterm birth remain highly relevant due to its prevalence, the risk of adverse outcomes for women's health and perinatal losses [1, 2]. Infant mortality and morbidity in children, in turn, are caused not only by prematurity and / or fetal growth retardation as a result of impaired functions of the fetoplacental complex, but also by malformations that are observed in 3-5% of newborns and occupy, according to the World Health Organization (WHO) ), 20% in the structure of morbidity and disability, 15-20% in the structure of perinatal mortality [3, 4]. Malformations of newborns are not only a tragedy of the family, but also a significant social problem that significantly burdens the state, so preventing their occurrence is an important medical and social task [5].
Infant mortality and morbidity in children, in turn, are caused not only by prematurity and / or fetal growth retardation as a result of impaired functions of the fetoplacental complex, but also by malformations that are observed in 3-5% of newborns and occupy, according to the World Health Organization (WHO) ), 20% in the structure of morbidity and disability, 15-20% in the structure of perinatal mortality [3, 4]. Malformations of newborns are not only a tragedy of the family, but also a significant social problem that significantly burdens the state, so preventing their occurrence is an important medical and social task [5].
Studies of the causes of malformations have made it possible to assume a significant role of nutrient status in their formation and designate the provision of the mother's body with all the necessary vitamins, vitamin-like substances and minerals as the most important factor contributing to the physiological course of pregnancy and the normal development of the fetus [6, 7].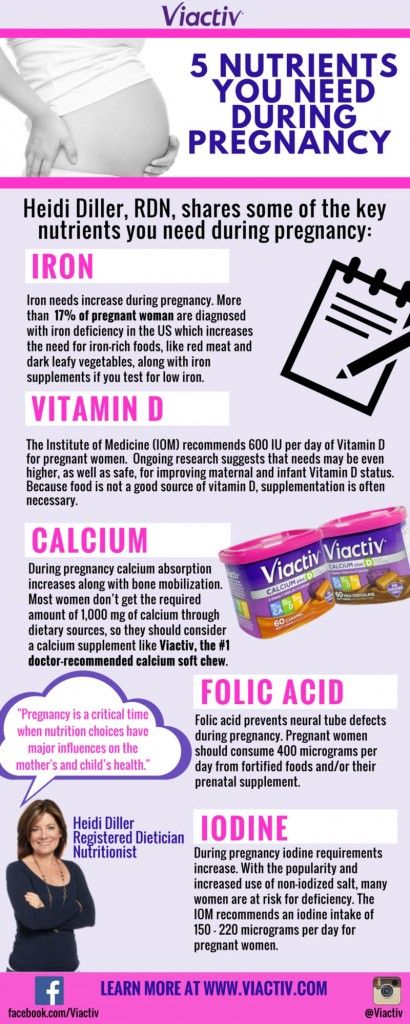 In recent years, special attention has been paid to folate deficiency as one of the leading causes of the development of various anomalies, primarily neural tube defects (NTDs).
In recent years, special attention has been paid to folate deficiency as one of the leading causes of the development of various anomalies, primarily neural tube defects (NTDs).
Folic acid derivatives - folates [8] acquired their name from the Latin " folia" - "leaf", as they were first obtained from spinach leaves. The reduced form of hydrated folic acid, tetrahydrofolate (THF), can attach methyl, methynyl, formin, and forminin groups at the 5th and/or 10th position, forming metabolites with varying degrees of biological activity and different uses. In the blood, 80% of folates circulate as methyltetrahydrofolate (MTHF), and enterohepatic circulation plays an important role in the short-term regulation of folate homeostasis, maintaining their level between meals. The supply of unmethylated polyglutamates in the liver and peripheral tissues ensures long-term maintenance of the level of folates in the blood, and the effective reabsorption of folates in the kidneys is included in folate homeostasis in cases of acute need. Thus, the body is protected from folate deficiency.
Thus, the body is protected from folate deficiency.
Indeed, folates are essential for the body to carry out vital functions, namely replication, repair and epigenetic regulation (methylation) of DNA, which is especially important for actively growing tissues, including hematopoiesis, the formation of placental tissue and new blood vessels in the uterus [9]. Folates are involved in the metabolism of purines, homocysteine, choline, histidine, they synthesize amino acids, nucleic acids, pyrimidines, essential phospholipids, neurotransmitters (serotonin, melatonin, adrenaline, dopamine), as well as cell receptors.
Tetrahydrofolate transfers hydroxymethyl, formyl groups and hydrocarbon radicals in the process of homocysteine, histidine, tryptophan and serine metabolism, synthesis of purine and pyrimidine bases, DNA biosynthesis [10, 11]. A genetically determined deficiency of dihydrofolate reductase (DHFR), which regenerates dihydrated folate into THF, increases cancer risk by disrupting cell growth and reproduction [12].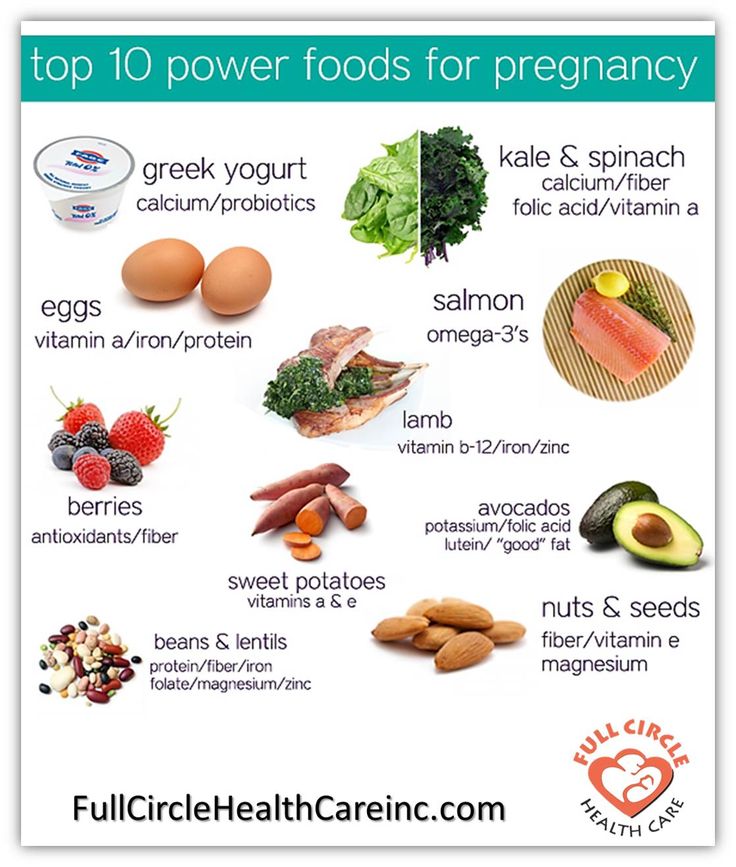
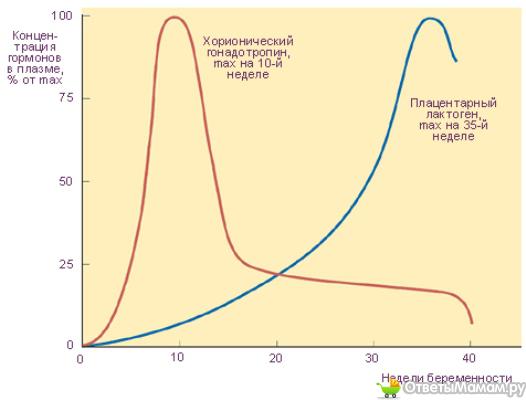
Remethylation of homocysteine to methionine is accompanied by the restoration of THF from the methyl form with the participation of vitamin B12, the deficiency of which leads to functional insufficiency of the folate cycle: the extraction of THF from MTHF becomes impossible, and with an increased level of MTHF, homocysteine accumulates. Another cause of folate deficiency with the outcome in hyperhomocysteinemia is the low activity of methylenetetrahydrofolate reductase (MTHFR), which converts 5`10`-methylenetetrahydrofolates into 5-MTH. It is a supplier of methyl groups in the homocysteine / methionine exchange. With gene polymorphism MTHFR MTHFR activity is reduced, the formation of 5-MTHF is reduced and the 5-MTHF methyl group is not enough for sufficient transformation of homocysteine into methionine. The degree of decrease in activity varies depending on the genotype. Thus, polymorphism MTHFR 677TT (homozygous genotype) reduces MTHFR activity by 70%, which leads to hyperhomocysteinemia.
The ability of the body to store folates and turn on the mechanism of renal reabsorption when necessary prevents the development of significant folate deficiency even in genetically predisposed individuals. But the combined effect of genetic and environmental factors can have adverse consequences, conventionally grouped into three groups: cancer risk due to deficiency of DHFR and other folate cycle enzymes [13], hyperhomocysteinemia associated with MTHFR deficiency [14], and cell developmental disorders due to deficiency folates.
Predisposition to folate deficiency is most relevant for pregnant women who have an increased, but not always met, need for folate due to gastrointestinal disorders (rarely) or alimentary deficiency (often). Inadequate folic acid intake during pregnancy carries a risk of hyperhomocysteinemia even in heterozygous genotypes of the MTHFR polymorphism. However, even in a genetically healthy woman, with a low intake of folic acid, the folate supply may not be enough for the growing needs of the fetus, and this will not only affect the course of pregnancy, but also directly affect the fetus.
A pregnant woman is the only source of nutrients for the fetus, therefore, rational nutrition determines not only her own health, but also the health of her unborn child, which must be taken care of in advance, using the body's ability to store vital substances, including folates, to create their strategic reserve in the liver and peripheral tissues. The only problem is that it is almost impossible to establish such a rational healthy diet in modern conditions.
Folates are found in leafy vegetables, green peas, citrus fruits, bread and cereals, animal liver, nutritional yeast, cheese, cottage cheese, but their bioavailability is low, and normal cooking conditions based on heat treatment lead to the destruction of 90% of folic acid. The typical "Western diet" high in meat, legumes and potatoes, and low in fruits is associated with reduced levels of folate, vitamin B6, vitamin B12. Folate deficiency is exacerbated by the use of hormonal contraceptives [15], hepatotoxic antibiotics, and alcohol. Large studies involving tens of thousands of people have shown that most adults consume less than the recommended folate intake. A study of the nutritional status of children and adolescents in several European and American countries revealed plasma folate levels below the recommended level in 96.3% of those examined [16].
Large studies involving tens of thousands of people have shown that most adults consume less than the recommended folate intake. A study of the nutritional status of children and adolescents in several European and American countries revealed plasma folate levels below the recommended level in 96.3% of those examined [16].
Manifestations of folate deficiency are far from always obvious, but no less dangerous. The lack of active folates leads to a slowdown in cell growth, and in adults, folic acid deficiency causes the greatest damage to rapidly renewing cell populations, primarily bone marrow tissues [17]. The consequence of deep hypovitaminosis B9 is megaloblastic anemia, a slowdown in the development of leukocyte growth and renewal of the lymphocyte population reduces resistance to infections and disrupts the immune response [18]. Megaloblastic anemia is rare, but folic acid deficiency, along with a lack of vitamins B12, B6 and C, can cause iron deficiency anemia by reducing iron absorption.
Less significant folic acid deficiency, without manifesting itself as anemia, can manifest itself with symptoms of mental disorders: mild depression, irritability, sleep disorders and cognitive dysfunction, which is explained by the ability of folates to interact with noradrenergic (α1 and α2) and serotonergic receptors (5-hydroxytryptamine - 5 -HT1A and 5-HT2A/2C). Folic acid deficiency is also associated with subclinical disorders of carbohydrate and fat metabolism, fatigue and maladjustment - the inability to endure physical and mental stress.
Hyperhomocysteinemia has an independent significance in the development of a number of pathological conditions and diseases, as well as several conditions beyond the scope of insufficient folic acid intake, among which low MTHFR activity is observed in individuals with MTHFR genotype polymorphism (usually in 677TT), low cystathion activity -β-synthase (the result of vitamin B6 deficiency), vitamin B12 deficiency. An increase in the level of homocysteine is significant in pathogenesis atherosclerosis, coronary heart disease, stroke, venous thrombosis, neurodegenerative diseases, osteoporotic fractures [19, 20]. Endothelial dysfunction that occurs with hyperhomocysteinemia is a factor in the pathogenesis of pregnancy complications that depend on microcirculation, starting with spontaneous miscarriage in the first trimester of pregnancy and ending with preeclampsia, placental abruption and antenatal fetal death [21, 22].
An increase in the level of homocysteine is significant in pathogenesis atherosclerosis, coronary heart disease, stroke, venous thrombosis, neurodegenerative diseases, osteoporotic fractures [19, 20]. Endothelial dysfunction that occurs with hyperhomocysteinemia is a factor in the pathogenesis of pregnancy complications that depend on microcirculation, starting with spontaneous miscarriage in the first trimester of pregnancy and ending with preeclampsia, placental abruption and antenatal fetal death [21, 22].
Multiple evidence of higher prevalence of homozygous and heterozygous genotypes MTHFR among women with complicated pregnancy. Genotypes MTHFR 677TT and 1298AC are associated with an increased risk of spontaneous abortion: the relative risk (RR) for the 677TT genotype compared to that of CC/TT is 5.0, 95% confidence interval (CI): 1.2–20.9; The RR for the 1298AC genotype compared to the AA genotype is 5.5, 95% CI: 1.1–26.6 [23]. The association of the MTHFR gene polymorphism with the risk of preterm birth is discussed. Folate metabolism disorders also affect the health of children: gene 9 polymorphism0105 MTHFR in the mother doubles the risk of developing autism [24], and the polymorphism of the gene encoding DHFR, DHFR (homozygous genotype — 3.78, 95% CI: 1.89–7.55) [25]. It is noteworthy that excessive, exceeding the daily requirement, consumption of folic acid by a woman carrying the DHFR 19bpdel genotype increases the oncological risk even with a normal genotype of the child.
Folate metabolism disorders also affect the health of children: gene 9 polymorphism0105 MTHFR in the mother doubles the risk of developing autism [24], and the polymorphism of the gene encoding DHFR, DHFR (homozygous genotype — 3.78, 95% CI: 1.89–7.55) [25]. It is noteworthy that excessive, exceeding the daily requirement, consumption of folic acid by a woman carrying the DHFR 19bpdel genotype increases the oncological risk even with a normal genotype of the child.
The negative consequences of folate deficiency and metabolic disorders include congenital malformations of the fetus: neural tube defects (anencephaly, cerebral hernia, spina bifida) [26], anomalies of the genitourinary tract, congenital heart defects, maxillofacial region ("cleft palate") [ 27]. Low dietary folic acid intake is associated with a 4-fold increased risk of limb defects (OR 3.9, 95% CI 1.08-13.78). Different variants of folate cycle disorders can lead to the formation of malformations, but, apparently, folic acid deficiency is more significant here than MTHFR deficiency.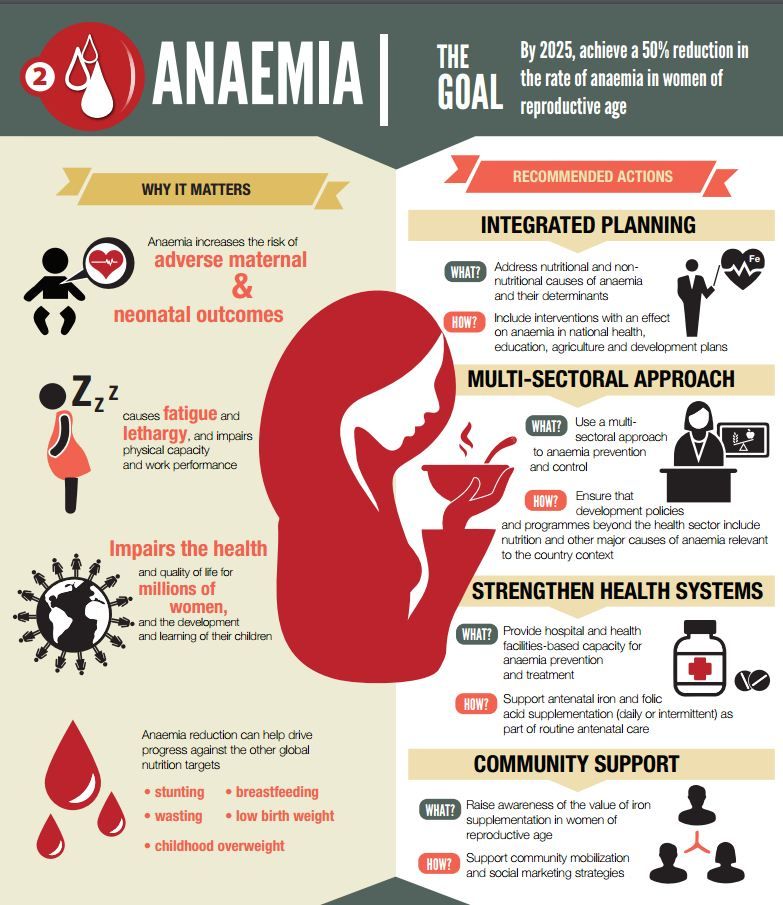 The possibility of a toxic effect of hyperhomocysteinemia on the fetus is not excluded [28], but in the experiment, injections of homocysteine into pregnant mice or its introduction into the culture of rat embryos had neither embryotoxic nor teratogenic effects, including did not cause NTD [29]. In the process of searching for the causes of the known teratogenic effect of valproic acid, a group of researchers found that valproate increases the expression of MTHFR [30] and, in an experiment on mice with low activity of the enzyme, increases the frequency of NTDs. High expression of MTHFR, therefore, is no less harmful than its insufficient activity. This phenomenon can be explained in terms of the multiple effects of endogenous folates. Unmethylated folates are required for the synthesis of thymidine and purine, and MTHFR converts them into 5-MTHF, which is used to methylate homocysteine to methionine [31]. Excessive MTHFR activity disrupts the balance of methylated and unmethylated folates, which damages the synthesis of thymidine and purine and does not provide an adequate level of nucleotides for DNA synthesis.
The possibility of a toxic effect of hyperhomocysteinemia on the fetus is not excluded [28], but in the experiment, injections of homocysteine into pregnant mice or its introduction into the culture of rat embryos had neither embryotoxic nor teratogenic effects, including did not cause NTD [29]. In the process of searching for the causes of the known teratogenic effect of valproic acid, a group of researchers found that valproate increases the expression of MTHFR [30] and, in an experiment on mice with low activity of the enzyme, increases the frequency of NTDs. High expression of MTHFR, therefore, is no less harmful than its insufficient activity. This phenomenon can be explained in terms of the multiple effects of endogenous folates. Unmethylated folates are required for the synthesis of thymidine and purine, and MTHFR converts them into 5-MTHF, which is used to methylate homocysteine to methionine [31]. Excessive MTHFR activity disrupts the balance of methylated and unmethylated folates, which damages the synthesis of thymidine and purine and does not provide an adequate level of nucleotides for DNA synthesis. Insufficient activity of the enzyme prevents the recovery of THF from 5-MTHF due to the lack of the latter and also creates a deficiency of unmethylated folates for participation in DNA synthesis. Despite the complexity of the interactions of the participants in the folate cycle, the fact that insufficient intake of folic acid, a substrate for the synthesis of endogenous folates, leads to impaired DNA synthesis and forms malformations, regardless of genotype 9 polymorphism, can be considered indisputable today.0105 MTHFR . The role of hyperhomocysteinemia in the development of NTDs is the subject of discussion, and any significant change in MTHFR activity and a shift in the ratio of methylated and unmethylated folates can lead to a violation of DNA synthesis, even with a normal intake of folic acid.
Insufficient activity of the enzyme prevents the recovery of THF from 5-MTHF due to the lack of the latter and also creates a deficiency of unmethylated folates for participation in DNA synthesis. Despite the complexity of the interactions of the participants in the folate cycle, the fact that insufficient intake of folic acid, a substrate for the synthesis of endogenous folates, leads to impaired DNA synthesis and forms malformations, regardless of genotype 9 polymorphism, can be considered indisputable today.0105 MTHFR . The role of hyperhomocysteinemia in the development of NTDs is the subject of discussion, and any significant change in MTHFR activity and a shift in the ratio of methylated and unmethylated folates can lead to a violation of DNA synthesis, even with a normal intake of folic acid.
The significance of folate in the normal course of pregnancy and fetal development and the role of folate deficiency in the formation of maternal and child morbidity and mortality determine the need to create an optimal folate status at the stage of preconception preparation and continue folic acid supplementation during pregnancy [32].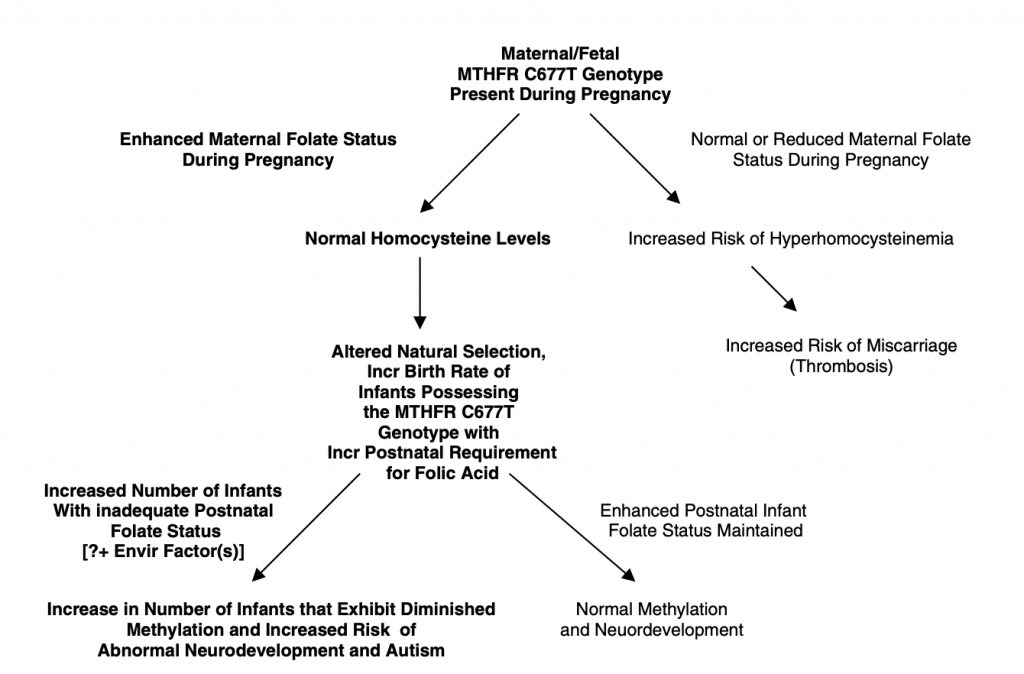 However, the introduction of programs to increase folate levels during conception through the promotion of a healthy diet or food fortification did not give the expected result in reducing the incidence of NTDs [33]. In contrast, folic acid supplementation in the form of drugs has proven to be effective in reducing the risk of NTDs [34] and other fetal anomalies [35]. In Northern Europe and Scandinavia, increased intake of synthetic folic acid by women during preconception led to a 16% reduction in NTDs [36]. Data from the Italian National Institute of Health confirm that taking 400 mcg/day of folic acid before and during pregnancy reduces the incidence of abnormal embryogenesis of the brain, heart, urinary system, cleft palate, limb defects, defects in large arteries, and omphalocele - umbilical hernia [37 ]. Folic acid supplementation reduces the risk of developing Down syndrome [38, 39], congenital heart defects, maxillofacial defects [40]. Experimental studies [41] indicate the properties of folic acid to prevent the development of congenital malformations in mice with a model of diabetes mellitus.
However, the introduction of programs to increase folate levels during conception through the promotion of a healthy diet or food fortification did not give the expected result in reducing the incidence of NTDs [33]. In contrast, folic acid supplementation in the form of drugs has proven to be effective in reducing the risk of NTDs [34] and other fetal anomalies [35]. In Northern Europe and Scandinavia, increased intake of synthetic folic acid by women during preconception led to a 16% reduction in NTDs [36]. Data from the Italian National Institute of Health confirm that taking 400 mcg/day of folic acid before and during pregnancy reduces the incidence of abnormal embryogenesis of the brain, heart, urinary system, cleft palate, limb defects, defects in large arteries, and omphalocele - umbilical hernia [37 ]. Folic acid supplementation reduces the risk of developing Down syndrome [38, 39], congenital heart defects, maxillofacial defects [40]. Experimental studies [41] indicate the properties of folic acid to prevent the development of congenital malformations in mice with a model of diabetes mellitus. A number of studies [42] have shown that folic acid supplementation has a beneficial effect on the course of pregnancy and fetal weight and height. In patients with polymorphism of the MTHFR genotype, the administration of folic acid preparations together with vitamins B6 and B12 reduces the level of homocysteine and prevents the development of complications associated with hyperhomocysteinemia [43].
A number of studies [42] have shown that folic acid supplementation has a beneficial effect on the course of pregnancy and fetal weight and height. In patients with polymorphism of the MTHFR genotype, the administration of folic acid preparations together with vitamins B6 and B12 reduces the level of homocysteine and prevents the development of complications associated with hyperhomocysteinemia [43].
An important factor in the effectiveness and safety of taking folic acid is its dosing. According to the guidelines set by the German Nutrition Society, the optimal intake for pregnant women is 600 micrograms of folate equivalents per day. The need for additional intake of folic acid, not counting folates obtained from food, is emphasized, at a minimum dose of 400 mcg / day for all pregnant women. These recommendations are consistent with the opinions of other European and American experts. A joint analysis of the results of folic acid supplementation conducted by German, Swiss and Austrian specialists confirmed that the minimum effective dose is a daily dose of 400 μg [44].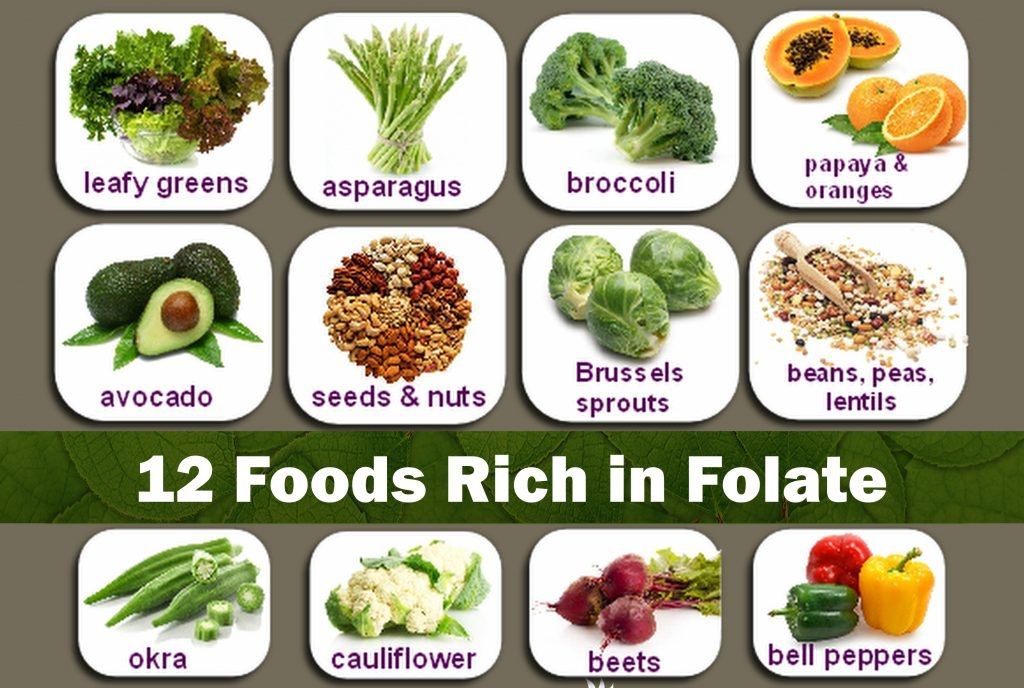 The upper limit of the dose of folic acid for the purpose of prevention should not reach 1000 mcg / day. The use of high doses of the vitamin (from 1000 to 5000 mcg/day) has the same result in reducing the risk of NTD by 50-80% as taking 400-800 mcg/day [45]. But an excess of folic acid, including with a genetically determined insufficient activity of folate cycle enzymes, can have negative consequences, blocking the action and creating an imbalance of different forms of folate, disrupting DNA stability and leading to undesirable outcomes, just like folate deficiency [32]. The health of the children of women who had elevated folate levels due to high doses of folic acid may suffer due to the development of obesity [46], as well as from rare but dangerous complications of excess folate intake in the presence of genotype 9 polymorphism0105 DHFR [12]. Thus, an effective and safe prophylactic daily dose of folic acid is a dose in the range of 400-800 mcg, and it should be taken at the stage of preparation for pregnancy.
The upper limit of the dose of folic acid for the purpose of prevention should not reach 1000 mcg / day. The use of high doses of the vitamin (from 1000 to 5000 mcg/day) has the same result in reducing the risk of NTD by 50-80% as taking 400-800 mcg/day [45]. But an excess of folic acid, including with a genetically determined insufficient activity of folate cycle enzymes, can have negative consequences, blocking the action and creating an imbalance of different forms of folate, disrupting DNA stability and leading to undesirable outcomes, just like folate deficiency [32]. The health of the children of women who had elevated folate levels due to high doses of folic acid may suffer due to the development of obesity [46], as well as from rare but dangerous complications of excess folate intake in the presence of genotype 9 polymorphism0105 DHFR [12]. Thus, an effective and safe prophylactic daily dose of folic acid is a dose in the range of 400-800 mcg, and it should be taken at the stage of preparation for pregnancy.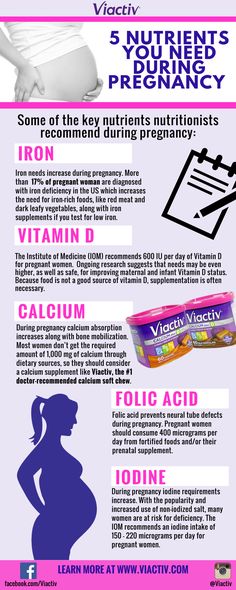 Increasing the dose to the therapeutic level of 1000-5000 mg is justified only if there is a confirmed genetic predisposition to folate cycle disorders due to severe MTHFR deficiency.
Increasing the dose to the therapeutic level of 1000-5000 mg is justified only if there is a confirmed genetic predisposition to folate cycle disorders due to severe MTHFR deficiency.
Women who did not take folic acid before conception are at risk of developing NTD, since the formation of the neural tube is completed by the 28th day of intrauterine development, and even the early start of folic acid intake due to the delay in menstruation does not allow one to hope for an initial folate deficiency to achieve their optimal level in such a limited time frame. This problem can be overcome in different ways. For example, the original approach of American researchers [47] suggests the use of 7.5 mg of folate (6L-5-MTHF) every 24 hours (5 doses in total) followed by switching to 800 mcg for 2 weeks and further intake of standard vitamin-mineral complexes containing 800 micrograms of folic acid. This method has been successfully tested only with a confirmed decrease in plasma folates of less than 25 nmol/L. Having no information about homozygous polymorphism MTHFR and/or the ability to determine 5-MTHF levels should be kept within the recommended prophylactic dose range. However, this range is relatively wide, and the question of what dose of folic acid is the most appropriate often arises in clinical practice. Undoubtedly, with long-term folic acid intake outside of pregnancy, its deficiency is unlikely. But, when prescribing vitamins to a pregnant woman for the first time, it must be remembered that a daily intake of 400 μg of folic acid brings the initially low level of 5-MTHF to an optimal value for a long time, on average, about 14 weeks, and in some cases it does not allow reaching normal concentration of folate in blood erythrocytes [48]. During pregnancy, this is unacceptable. 800 mcg folic acid increases plasma folate levels by 67% more than at the 400 mcg dose [49] and restores the optimal concentration of 5-MTHF in erythrocytes, on average for 4 weeks, therefore, this dose is much more acceptable.
Having no information about homozygous polymorphism MTHFR and/or the ability to determine 5-MTHF levels should be kept within the recommended prophylactic dose range. However, this range is relatively wide, and the question of what dose of folic acid is the most appropriate often arises in clinical practice. Undoubtedly, with long-term folic acid intake outside of pregnancy, its deficiency is unlikely. But, when prescribing vitamins to a pregnant woman for the first time, it must be remembered that a daily intake of 400 μg of folic acid brings the initially low level of 5-MTHF to an optimal value for a long time, on average, about 14 weeks, and in some cases it does not allow reaching normal concentration of folate in blood erythrocytes [48]. During pregnancy, this is unacceptable. 800 mcg folic acid increases plasma folate levels by 67% more than at the 400 mcg dose [49] and restores the optimal concentration of 5-MTHF in erythrocytes, on average for 4 weeks, therefore, this dose is much more acceptable.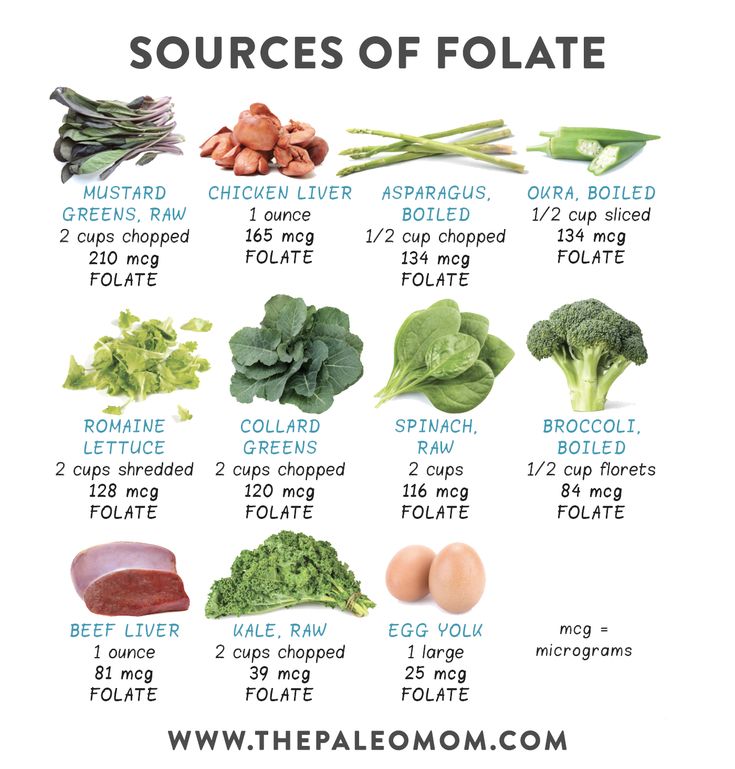 Studies of the pharmacodynamics of folic acid allowed German and Swiss researchers [48] to bring to the attention of the medical community the question of the need to increase the preventive supplementation of folic acid to pregnant women up to 800 mcg.
Studies of the pharmacodynamics of folic acid allowed German and Swiss researchers [48] to bring to the attention of the medical community the question of the need to increase the preventive supplementation of folic acid to pregnant women up to 800 mcg.
Folates are actively used as monopreparations, as part of vitamin complexes and even oral contraceptives [50] in two forms. Synthetic folic acid, a proven method of folate supplementation, once ingested, undergoes a series of enzymatic reactions resulting in both depot and active forms. The intake of synthetic folic acid has a direct relationship with an increase in the level of folate in blood plasma and erythrocytes, and an inverse relationship with the level of homocysteine [51]. The main studies of efficacy and safety were carried out on synthetic folic acid, its toxic effects are not described. AT 9In the 0s of the 20th century, another form of vitamin B9 was patented - levomefolate (left-handed isomer of 5-MTHF, L-methylfolate) calcium. The calcium compound 5-MTHF provides sufficient and independent of the polymorphism of the genes encoding MTHFR activity, the presence of folates in tissues. Levomefolate does not require enzymatic transformations, and its advantage is the ability to compensate for MTHFR deficiency in women with polymorphisms of the MTHFR gene [52]. But ideas about the effectiveness and safety of levomefolate are based only on data on folic acid, which is methodologically not quite correct. Until more information is received, the use of levomefolate as part of vitamin complexes and contraceptives is more justified in women with confirmed MTHFR deficiency. Currently, European experts recommend taking synthetic folic acid at the stage of preconception and during pregnancy [44], and the FDA reminds that calcium levomefolate and folic acid are not equivalent substances, and obliges manufacturers to indicate which folate contains a dietary supplement or drug . A randomized, double-blind, placebo-controlled clinical trial was conducted in Europe comparing the effects of methylfolate ([6S]-5-methyltetrahydrofolate) and folic acid on plasma and red blood cell folate concentrations over 24 weeks in women of childbearing age (18- 49years).
The calcium compound 5-MTHF provides sufficient and independent of the polymorphism of the genes encoding MTHFR activity, the presence of folates in tissues. Levomefolate does not require enzymatic transformations, and its advantage is the ability to compensate for MTHFR deficiency in women with polymorphisms of the MTHFR gene [52]. But ideas about the effectiveness and safety of levomefolate are based only on data on folic acid, which is methodologically not quite correct. Until more information is received, the use of levomefolate as part of vitamin complexes and contraceptives is more justified in women with confirmed MTHFR deficiency. Currently, European experts recommend taking synthetic folic acid at the stage of preconception and during pregnancy [44], and the FDA reminds that calcium levomefolate and folic acid are not equivalent substances, and obliges manufacturers to indicate which folate contains a dietary supplement or drug . A randomized, double-blind, placebo-controlled clinical trial was conducted in Europe comparing the effects of methylfolate ([6S]-5-methyltetrahydrofolate) and folic acid on plasma and red blood cell folate concentrations over 24 weeks in women of childbearing age (18- 49years). [68]
[68]
Women ( n = 104) were selected and randomly divided into groups:
1. Folic acid 100 mg/day (31 women)
2. Receiving methylfolate (MTHF) at 113 mg/day (38 women)
3. Placebo (28 women).
Studies show that methylfolate (MTHF) and folic acid increase blood folate concentrations at similar levels (see table).
Results of study
Folic acid, when taken before and during pregnancy, has been shown to reduce the risk of developing neural tube defects (NTDs). There is no data on whether MTHF (methylfolate) reduces the risk of developing NTDs.
Adequate replacement of folic acid deficiency, taking into account all the features of folate metabolism, does not guarantee complete prevention of NTD. The reason for this is the multifactorial nature of the disease [53], as well as the inclusion of a large number of vitamins, micro- and macroelements in the mechanism of the formation of fetal malformations. The same can be said about the nutrient background of pregnancy complications.
The same can be said about the nutrient background of pregnancy complications.
Folate metabolism and DNA methylation processes are equally affected by deficiency of each of vitamins B6, B9 or B12, therefore, the level of any of the B vitamins before conception is important for genetic health and prevention of fetal nervous system dysmorphism during pregnancy. Vitamin B12 deficiency in pregnant women increases the risk of fetal birth defects, primarily NTDs [54-56] , , as well as malformations of the cardiovascular system [57, 58]. A vitamin B6 level in the upper half of the normal range gives a higher chance of becoming pregnant (OR - 1.4; 95% CI: 1.1-1.9) and less chance of losing a pregnancy (OR - 0.7; 95% CI: 0 ,4-1,1) in comparison with the low normal concentration of vitamin B6 [59]. The relationship between the level of pyridoxine and the risk of pregnancy complications is not surprising: vitamin B6 acts as a cofactor for the enzyme cystathion-β-synthase, which is involved in the metabolism of homocysteine and eliminates its excess.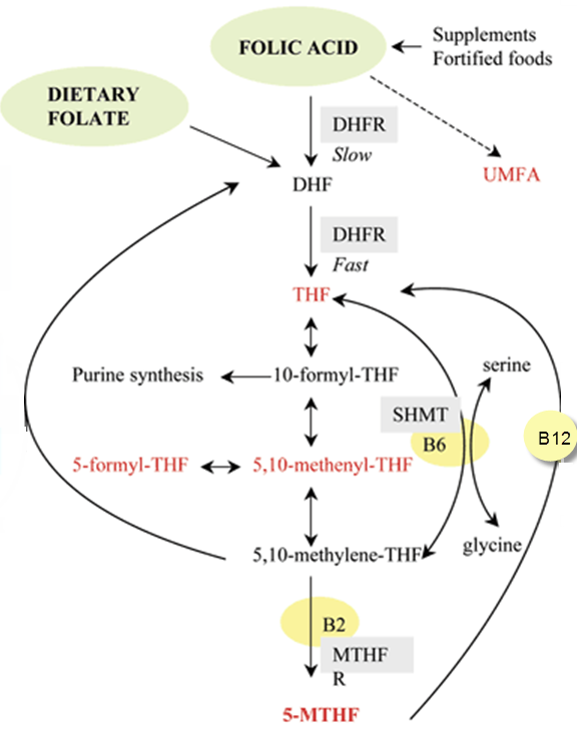
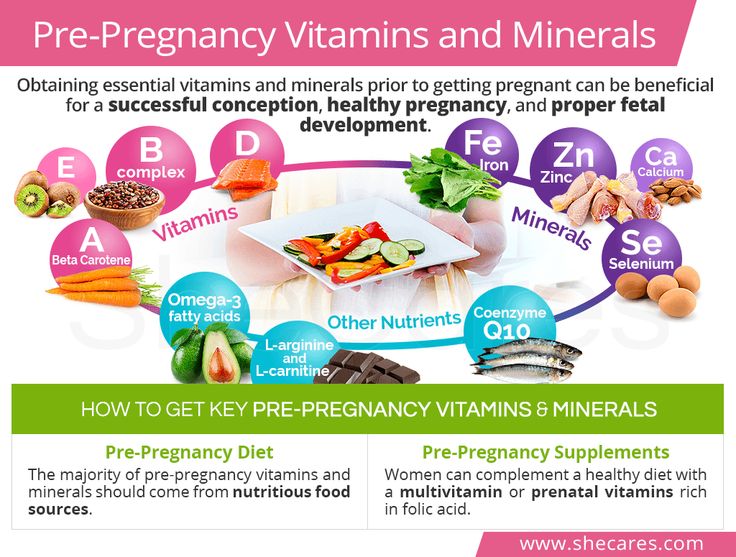
Vitamin B Complex needs to be supplemented with other vitamins and minerals. The formation of cleft palate and lip is 2 times more common with low intake of riboflavin, magnesium, calcium, vitamin B12 and zinc [60]. Heart defects occur with a low intake of riboflavin and nicotinamide and a high content of saturated fat in the diet [61]. The role of retinoic acid in the development of the heart and blood vessels is known, and its deficiency, as well as its excess, negatively affects the cardiovascular system [62], and vitamin A hypovitaminosis in the experiment is associated with laryngeal malformation [63].
The use of multivitamin supplements in combination with minerals is more effective than folic acid alone in reducing the risk of having children with malformations. One of the numerous studies showed that a complex of B vitamins (folic acid, vitamins B1, B2, B6 and B12), vitamin E and minerals (calcium, iron, magnesium and zinc) reduced the risk of congenital diaphragmatic hernia [64]. The use of antioxidant vitamins (vitamins C and E) contributed to a decrease in the frequency of NTDs in children of women with diabetes [65]. In a case-control study, the intake of vitamin-mineral complexes by pregnant women completely eliminated the risk of developing tetralogy of Fallot and disposition of large vessels in children [66].
The use of antioxidant vitamins (vitamins C and E) contributed to a decrease in the frequency of NTDs in children of women with diabetes [65]. In a case-control study, the intake of vitamin-mineral complexes by pregnant women completely eliminated the risk of developing tetralogy of Fallot and disposition of large vessels in children [66].
The use of multivitamin complexes, to a greater extent than taking folic acid alone, reduces the risk of pregnancy complications, which is natural, given the role of a number of vitamins, especially the B complex and antioxidants (ascorbic acid and tocopherol), in the prevention of preeclampsia [67]. Folic acid supplementation in a comparative study of 280,197 singleton pregnancies reduced the risk of premature detachment of a normally located placenta by 19%, and the use of a complex of vitamins with folic acid by 28% [68].
An absolutely necessary factor for the normal course of pregnancy is a sufficient level of magnesium [69, 70], which ensures the functioning of the nervous tissue, including the autonomic regulation of the cardiovascular system [71], and is an important component of the formation, accumulation and utilization of energy [72].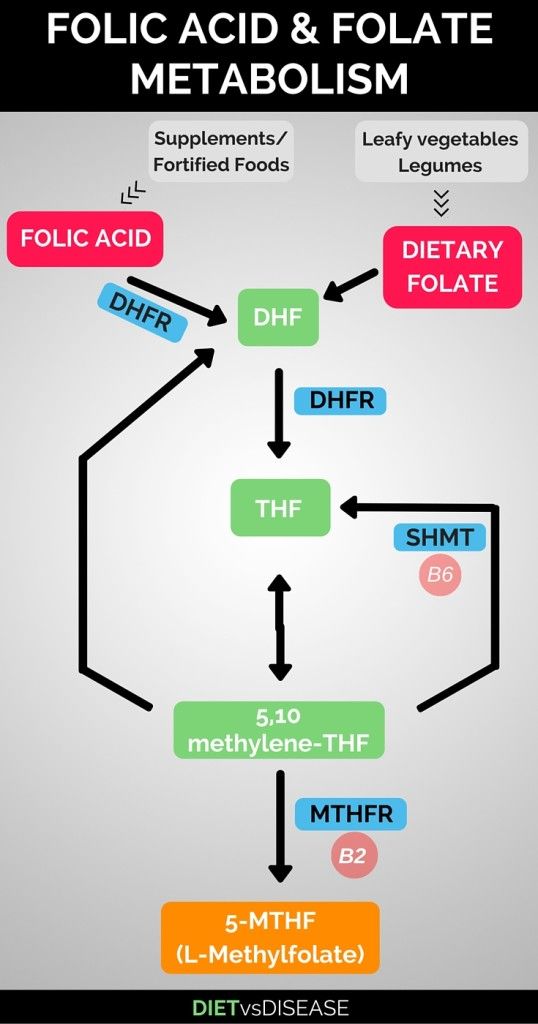 At the same time, the prevalence of magnesium deficiency is high, and especially in developed countries [73]. The high content of magnesium in food is by no means a guarantee of its intake into the body, since this macronutrient is well absorbed only from fresh vegetables, fruits, herbs and nuts, and during the processing and preparation of products, despite maintaining its high concentration, the percentage of magnesium absorption drops significantly [70]. Magnesium deficiency results in heart rhythm disturbances, pathological changes in the blood coagulation system, disorders of fat and carbohydrate metabolism, psychovegetative disorders, reduced immunity, increased risk of bronchospastic conditions, osteoporosis, and the formation of oxalate kidney stones [74]. During pregnancy, the daily requirement for magnesium increases by 2-3 times, which can lead to the development of a clinically pronounced macronutrient deficiency. Among its symptoms are weakness, fatigue and other manifestations of asthenia, anxiety, insomnia, night cramps in the calf muscles.
At the same time, the prevalence of magnesium deficiency is high, and especially in developed countries [73]. The high content of magnesium in food is by no means a guarantee of its intake into the body, since this macronutrient is well absorbed only from fresh vegetables, fruits, herbs and nuts, and during the processing and preparation of products, despite maintaining its high concentration, the percentage of magnesium absorption drops significantly [70]. Magnesium deficiency results in heart rhythm disturbances, pathological changes in the blood coagulation system, disorders of fat and carbohydrate metabolism, psychovegetative disorders, reduced immunity, increased risk of bronchospastic conditions, osteoporosis, and the formation of oxalate kidney stones [74]. During pregnancy, the daily requirement for magnesium increases by 2-3 times, which can lead to the development of a clinically pronounced macronutrient deficiency. Among its symptoms are weakness, fatigue and other manifestations of asthenia, anxiety, insomnia, night cramps in the calf muscles. A lack of magnesium in a woman's body leads to an increase in the tone of the myometrium, the threat of termination of pregnancy, increases the risk of preeclampsia, placental insufficiency and fetal growth retardation syndrome. Against the background of hypomagnesemia, the process of placental calcification accelerates. Magnesium deficiency in pregnant women may develop disorders of glucose metabolism, vascular disorders, electrolyte metabolism disorders [75].
A lack of magnesium in a woman's body leads to an increase in the tone of the myometrium, the threat of termination of pregnancy, increases the risk of preeclampsia, placental insufficiency and fetal growth retardation syndrome. Against the background of hypomagnesemia, the process of placental calcification accelerates. Magnesium deficiency in pregnant women may develop disorders of glucose metabolism, vascular disorders, electrolyte metabolism disorders [75].
Such a frequent complication of pregnancy as anemia, in the vast majority of cases, is associated with iron deficiency. Anemia in pregnancy increases the risk of fetal growth retardation, abnormal placentation, and other complications. Therefore, iron supplementation at a dose of 60 mg, according to WHO recommendations, is a necessary preventive measure, and the most justified way to take iron should be recognized as its combined use with folic acid and vitamin B12, i.e. as part of a vitamin-mineral complex.
Thus, the use of complex products containing vitamins and minerals necessary for the normal course of pregnancy is the optimal solution to the problem of maintaining the health of mothers and the birth of healthy children.
The drug, vitamin-mineral complex Vitrum Prenatal Forte has been tested in clinical trials for high efficiency and safety for pregnant women. The preparation contains sufficient amounts of B vitamins, including folic acid, vitamin C, E, iodine, magnesium, iron, etc. (13 vitamins and 10 minerals), corresponding to the physiological needs of pregnant women. The huge evidence base for the benefits of vitamins makes it possible not to raise the question of whether or not to prescribe well-studied drug complexes to a woman planning and carrying a pregnancy. This is the norm for managing patients in many countries of the world, including those with advanced medical care, such as Germany, France, Switzerland, etc.
Russia cannot be classified as a country with a favorable micronutrient status among the population. The Vitamin and Mineral Metabolism Laboratory of the Institute of Nutrition of the Russian Academy of Sciences reports a widespread vitamin deficiency among pregnant women in all regions of our country.