Dairy sensitive baby
Milk allergy and lactose intolerance in babies and children
Milk allergy and lactose intolerance in babies and children | Pregnancy Birth and Baby beginning of content10-minute read
Listen
Call triple zero (000) and ask for an ambulance if your child has these symptoms: wheezing or difficulty breathing, throat swelling, they are pale and floppy or unconscious. They could be having a severe allergic reaction and may need urgent medical attention.
Key facts
- Some babies and children have a reaction when they drink cow’s milk or formula made from cow’s milk.
- Symptoms after drinking cow’s milk could be due to lactose intolerance or an allergy to milk.
- If your child has lactose intolerance, you will need to reduce the amount of milk and dairy products in their diet.
- If your child has a milk allergy, you will need to alter their diet to avoid milk and dairy products completely.
- Many young children grow out of both lactose intolerance and milk allergy, but be sure to speak to your doctor before removing or reintroducing milk into your child’s diet.
What is the difference between lactose intolerance and milk allergy?
Around 1 in 10 young children have a reaction when they drink cow's milk. This could be because they have a lactose intolerance or a milk allergy. Milk allergy is much more common than lactose intolerance in children under 5 years of age.
Lactose intolerance is a problem with the digestive system — it means your child doesn't have the enzyme needed to digest lactose, which is the sugar naturally present in milk.
Milk allergy, however, is a problem with the immune system, where the body reacts to the protein in milk. An allergy usually involves other parts of the body as well as the stomach and may cause symptoms such as a skin rash or swelling of the face.
Many young children grow out of their intolerance or allergy. But don’t start giving them milk until your doctor tells you it’s safe to do so.
How do I know if my child is lactose intolerant or has a milk allergy?
Your doctor can confirm whether your child is lactose intolerant or has a milk allergy by asking about your child’s symptoms and doing medical tests. Don’t remove milk or milk-based foods from your child’s diet unless your doctor has told you to.
Don’t use unproven tests such as Vega, kinesiology, Alcat or allergy elimination tests for children. A milk intolerance is very unlikely to be the cause of mucus or coughing.
What causes lactose intolerance?
Lactose is the sugar found in the milk produced by all mammals, including humans. Sometimes, people don’t produce enough of the enzyme lactase in their gut to break down the lactose.
Very few babies have true lactose intolerance, a rare genetic condition where they’re born without any lactase enzymes at all. (This is called primary lactose intolerance.) However, many people develop lactose intolerance later in life, after the age of 5 years. It is more common among Aboriginal and/or Torres Strait Islander people and people from Asia, Africa, the Middle East and some Mediterranean countries.
(This is called primary lactose intolerance.) However, many people develop lactose intolerance later in life, after the age of 5 years. It is more common among Aboriginal and/or Torres Strait Islander people and people from Asia, Africa, the Middle East and some Mediterranean countries.
Lactose intolerance is rare in babies and young children. However, they can become temporarily intolerant to milk if the lining of their gut is damaged by an illness such as gastroenteritis, or an allergy or intolerance to another food. This is called secondary lactose intolerance and will resolve once the gut heals, usually over a few months.
What are the symptoms of lactose intolerance?
The symptoms of lactose intolerance in babies and children are:
- liquid, frothy stools (poo), which may be green
- being irritable
- stomach aches
- bloating
- passing a lot of gas
- slow weight gain
- nappy rash
All of these symptoms are common in babies and don't necessarily mean they have lactose intolerance. But if your child has persistent diarrhoea or isn't putting on weight, see your doctor. Don't stop breastfeeding unless your doctor tells you to.
But if your child has persistent diarrhoea or isn't putting on weight, see your doctor. Don't stop breastfeeding unless your doctor tells you to.
How is lactose intolerance diagnosed?
Your doctor may suggest cutting out dairy from your child’s diet to see if their symptoms improve. This is known as an elimination diet.
Tests may also include a breath test to measure the hydrogen in your child’s breath, though this test may not be very helpful for young babies (under 3 months old).
How is lactose intolerance treated?
If the lactose intolerance is caused by a tummy upset, keep on breastfeeding. If your baby is formula fed, talk to your doctor or child and family health nurse before switching to low-lactose or lactose-free formula.
Older children will need to cut down on, but not eliminate, dairy foods from their diet. They can still have some cheeses, yogurt, calcium-fortified soy products, lactose-free milk, butter and cream. Your doctor or a dietitian will advise you on the best diet for your child.
Most of the time, young children will recover from lactose intolerance after a few weeks of having a low-lactose diet. Speak to your doctor or dietitian about how to slowly reintroduce milk and dairy products into your child’s diet.
What causes milk allergy?
Milk allergy occurs when your child's immune system reacts to the protein in milk. It is one of the most common food allergies in young children. Most children outgrow milk allergy by the time they reach school age.
What are the symptoms of cow’s milk allergy?
Reactions to milk can occur within minutes or several hours.
Rapid reactions include:
- hives (urticaria)
- swelling of the lips, face or eyes
- stomach pain
- vomiting or diarrhoea
- noisy breathing, wheezing or hoarseness
- a swollen tongue or throat
- change in consciousness or floppiness in babies or young children
Call triple zero (000) and ask for an ambulance if your child has these symptoms:
- wheezing or difficulty breathing
- throat swelling
- they are pale and floppy or unconscious
They could be having a severe allergic reaction (anaphylaxis) and may need urgent medical attention.
Delayed reactions include:
- an increase in eczema
- vomiting and/or diarrhoea that starts 2 to 24 hours after having milk
How is milk allergy diagnosed?
It is very important to see a doctor if your child has the symptoms of milk allergy. Your doctor will ask about your child’s symptoms. They may also refer your child for blood or skin allergy tests.
How is milk allergy treated?
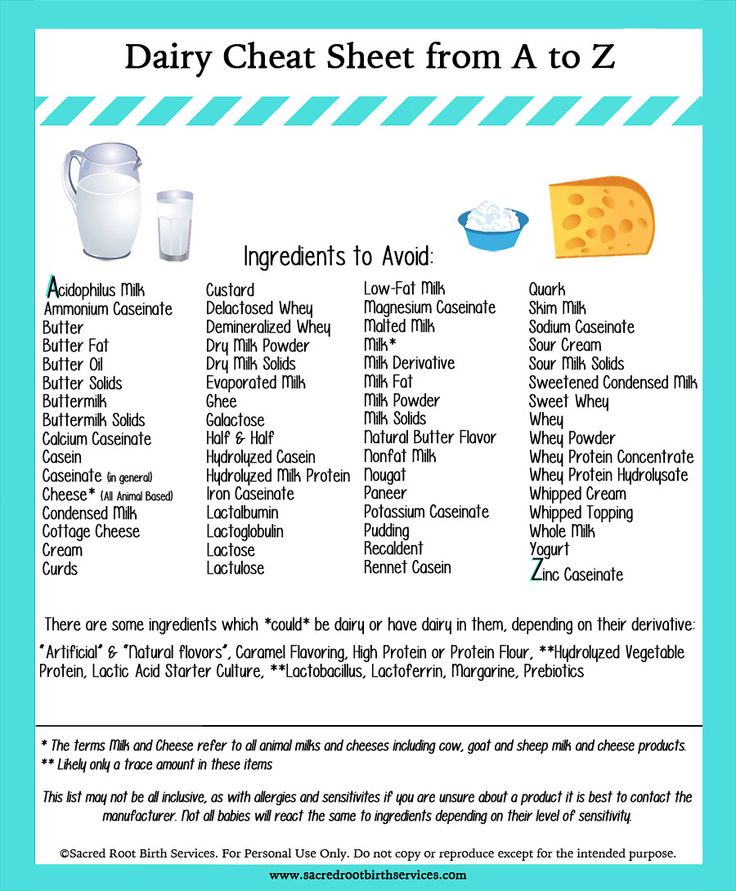
If your child is allergic to milk, you need to completely remove dairy products from their diet. Follow your doctor's or allergy specialist's advice and read food labels carefully. You may also need to avoid milk from other animals, such as goats. You should use coconut products with caution, as many coconut products (especially those from South East Asia) may be contaminated with cow’s milk.
Watch out for other words used to describe milk on food labels, such as butter, buttermilk, cream, curd, ghee, milk, cheese, dairy, milk solids, whey, yoghurt, casein and caseinates.
If your baby is formula-fed, you can use extensively hydrolysed formula (EHF) or amino acid-based formula (AAF). If your baby is over 6 months old, you can also use soy protein formula (unless they are also allergic to soy). Do not use formula made from cow's milk, goat's milk, sheep's milk, HA or A2 milk or lactose-free formulas.
If your child is over the age of one, they can be given soy milk, or calcium-enriched rice, oat or nut milks. It is important to make sure they are getting enough calcium.
If your child is allergic to milk, you may be advised to carry an adrenaline autoinjector (EpiPen® and Anapen®). Severe allergic reactions can sometimes lead to anaphylaxis, which is an emergency and can even be fatal. An adrenaline autoinjector can be used to give first aid in the event of anaphylaxis.
Can I still breastfeed my baby if they are lactose intolerant?
If your baby is lactose intolerant, you can continue to breastfeed without changing your diet. Reducing the amount of dairy you consume will not reduce the amount of lactose in your breastmilk.
Can I still breastfeed my baby who has a milk allergy?
Breastmilk is best, including for babies who have a milk allergy. In some cases, your doctor may advise you to remove milk and dairy products from your own diet. In other cases, you may be able to eat your regular diet. Your doctor or allergy specialist will advise you.
You don’t need to deal with lactose intolerance and milk allergy by yourself. You can get help from:
- your doctor
- Pregnancy, Birth and Baby on 1800 882 436
- Australasian Society of Clinical Immunology and Allergy
- Australian Breastfeeding Association on 1800 686 268
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Children's Hospital Melbourne (Lactose intolerance), Australian Breastfeeding Association (Lactose intolerance and the breastfed baby), Australasian Society of Clinical Immunology and Allergy (Cow’s milk (dairy) allergy), Sydney Childrens Health Network (Cow’s milk (dairy) allergy and milk free diet), Australasian Society of Clinical Immunology and Allergy (Food Protein-Induced Enterocolitis Syndrome (FPIES) Frequently Asked Questions (FAQ)), Australasian Society of Clinical Immunology and Allergy (Guide for Milk Substitutes in Cow’s Milk Allergy), Royal Children’s Hospital Melbourne (Eczema; food allergies and other triggers), Royal Children's Hospital Melbourne (Cows milk allergy), Australasian Society of Clinical Immunology and Allergy (Cow’s Milk Protein (Dairy) Allergy - dietary food guide)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2022
Back To Top
Related pages
- Airborne allergies
- How to introduce allergy foods
Need more information?
Lactose intolerance - MyDr.com.au
Lactase deficient people do not have enough lactase, the enzyme that helps break down lactose and they suffer from lactose intolerance. The main symptoms of lactose intolerance are bloating and wind.
Read more on myDr website
Lactose intolerance - Better Health Channel
Symptoms of lactose intolerance include bloating, gas, abdominal pain and diarrhoea.
Read more on Better Health Channel website
ASCIA Guide for Milk Substitutes in Cow’s Milk Allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Guide for Milk Substitutes in Cow’s Milk Allergy
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy - Cow's milk allergy and milk free diet | Sydney Children's Hospitals Network
How common is cow’s milk allergy? Cow’s milk allergy is one of the most common food allergies in childhood affecting about 1-2% of preschool children
Read more on Sydney Children's Hospitals Network website
Cow's milk (dairy) allergy | Dietitians Australia
Cow's milk allergy is common in babies and children, and symptoms can range from mild to severe. Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Read more on Dietitians Australia website
Food allergy versus food intolerance - MyDr.com.au
A food allergy is an immune response triggered by eating specific foods that cause certain well known symptoms to develop.
Read more on myDr website
Cow’s milk allergy - Better Health Channel
Milk allergy symptoms range from mild to a life-threatening severe allergic reaction. Avoid food containing milk only under strict medical supervision
Read more on Better Health Channel website
Cow`s milk (dairy) allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Cow's milk is a common cause of food allergy in infants. In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Food intolerances: children & teenagers | Raising Children Network
Food intolerance symptoms in children and teens include bloating, diarrhoea and stomach pain. If you think your child has food intolerance, talk to your GP.
Read more on raisingchildren.net.au website
Food intolerance - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Around 1 in 20 infants and 1 in 100 adults are allergic to food. Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
causes, symptoms, treatment in children and adults
- What is milk allergy
- Causes of milk allergy
- Who is at risk
- Milk allergy: symptoms
- How lactose allergy manifests itself
- Milk allergy in children
- Is it possible to be allergic to goat milk
- Diagnostics of milk allergy
- Allergy to milk: treatment
What is allergy to milk
Allergy to milk - hypersensitivity of human immunity to the components of dairy products. An allergic reaction occurs when drinking fresh cow or goat milk, as well as secondary products based on them (sour cream, kefir, butter, cream, etc.). There are two forms of pathology: an allergy to milk protein (casein) and an allergy to lactose (a carbohydrate, also called milk sugar). The mechanism of the occurrence of a protein allergic reaction lies in the work of the immune system. The body's defenses mistakenly perceive the components of dairy products as a threat. In the blood, the production of immunoglobulin is activated, which provokes inflammatory processes.
An allergic reaction occurs when drinking fresh cow or goat milk, as well as secondary products based on them (sour cream, kefir, butter, cream, etc.). There are two forms of pathology: an allergy to milk protein (casein) and an allergy to lactose (a carbohydrate, also called milk sugar). The mechanism of the occurrence of a protein allergic reaction lies in the work of the immune system. The body's defenses mistakenly perceive the components of dairy products as a threat. In the blood, the production of immunoglobulin is activated, which provokes inflammatory processes.
Call for advice - consult a doctor
(067) 446-11-79
Allergy to lactose is associated with the functioning of the gastrointestinal tract. In a healthy person, an enzyme is produced in the digestive organs that promotes the absorption of milk disaccharides. In the absence or insufficient production of this enzyme, lactose intolerance develops. In the literal sense, such a reaction cannot be called allergic, since it occurs exclusively at the level of the digestive organs and does not provoke the production of histamine.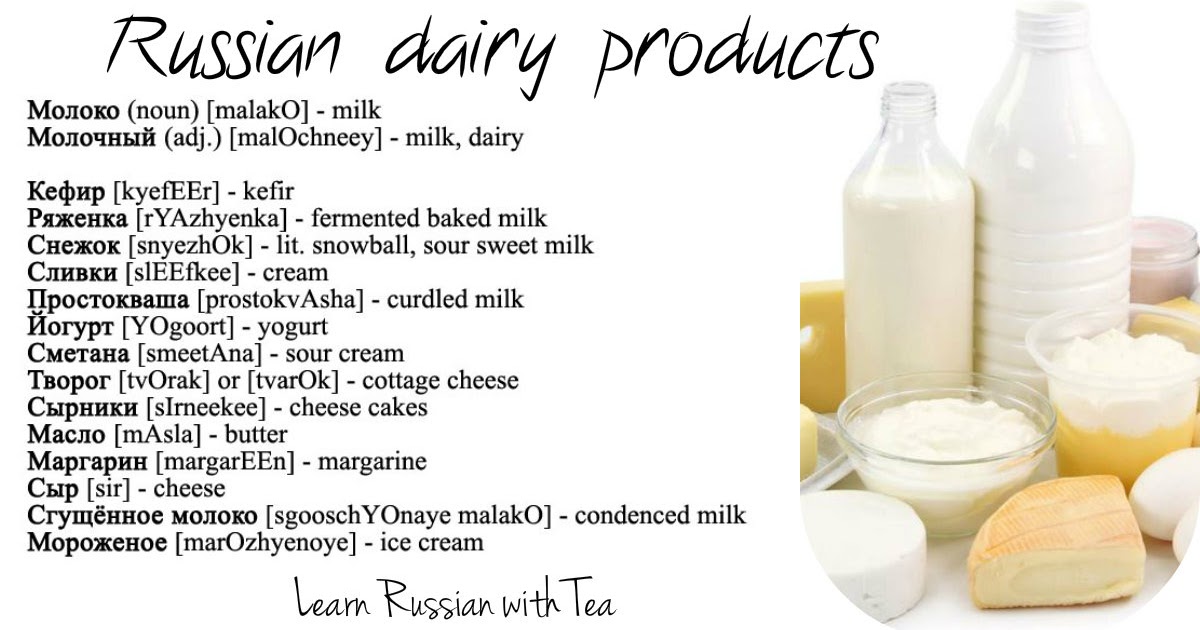 Many doctors believe that lactose allergy from milk is a very real diagnosis.
Many doctors believe that lactose allergy from milk is a very real diagnosis.
Causes of milk allergy
A pathological condition caused by an irritant affecting the body, in particular the immune system. With casein allergy, casein enters the bloodstream - the strongest allergen that causes acute inflammatory processes. Among adults and children, the most common allergy is cow's milk protein. However, most people with this diagnosis do not completely refuse dairy products. In particular, sheep and goat milk with allergies are much better tolerated by the body, since they contain much less casein.
Allergists identify a number of causes that cause allergic reactions to dairy products.
- Congenital pathologies associated with gene mutations. Violations are observed even in the period of intrauterine development and are often detected during prenatal diagnosis. Children with a similar disease from an early age are allergic to cow's milk and mother's milk.

- Prematurity of the child. Children who were born earlier than expected are characterized by weak immunity and a tendency to various diseases. Even during the period of breastfeeding, premature babies develop symptoms of lactose intolerance, which enters the body along with mother's milk. Later, an allergy develops to goat's milk, although it contains much less protein than cow's milk.
- Old age. After 30-40 years, the activity of cells producing enzymes decreases. Quite often, this affects the production of the lactase enzyme, which is responsible for the absorption of lactose. Acquired milk allergy in adults is usually associated with just such an etiology. A person suffers from digestive problems after eating dairy products, taking the symptoms that have arisen for a slight indigestion, which makes it difficult to diagnose the disease.
- Past infectious diseases of the gastrointestinal tract and chronic inflammatory pathologies of the digestive organs. Any pathology of the stomach and intestines disrupts their normal functioning.
 If during the progression of the disease the processes of production of the lactase enzyme were disrupted, an allergy to lactose develops. In adults, a similar etiology of allergy to dairy products is much more common, although cases of enzyme deficiency in children are not uncommon.
If during the progression of the disease the processes of production of the lactase enzyme were disrupted, an allergy to lactose develops. In adults, a similar etiology of allergy to dairy products is much more common, although cases of enzyme deficiency in children are not uncommon.
Who is at risk
As a rule, milk allergy begins in the fetus while still in the womb or in early childhood. The risk of developing pathology is highest under the influence of the following factors.
- The predominance of dairy products in the diet of a pregnant woman. If the expectant mother constantly consumes dairy products, cow's milk protein regularly enters her blood. Allergies are triggered by an excess amount of protein compounds that act as allergens. The pathological condition at the gene level is transmitted to the fetus and develops during the first few years after birth.
- Heredity. The risk of the disease increases if parents suffer from congenital allergic reactions to milk components.
 Lactose allergy in infants is hereditary in about 70% of cases, casein intolerance at the gene level occurs with the same frequency.
Lactose allergy in infants is hereditary in about 70% of cases, casein intolerance at the gene level occurs with the same frequency. - Worm infestations. Getting into the cavity of the digestive organs, parasites interfere with the production of enzymes and destroy intestinal immunity. In this case, the allergy to cow's milk proteins is acquired. The disease is most often diagnosed in children of primary school age, which is associated with non-compliance with hygiene rules.
- Late breastfeeding. In order for the intestines of the newborn to start, doctors recommend starting feeding within 2 hours after birth. Colostrum, which is produced by the mammary glands of a woman in the first days of feeding, contains immunoglobulins that lay the foundation for the child's immunity and protect his body from pathogenic bacteria. If the feeding did not take place on time, the baby develops intestinal dysbacteriosis, the consequence of which in the future is often an allergy to milk.

- Poor diet leading to hypovitaminosis. Vitamins of groups A, C and E play an important role in the functioning of the human immune system. Their deficiency leads to instability and abnormal sensitivity of the immune system to exogenous and endogenous stimuli. In children who are breastfed, milk allergy caused by hypovitaminosis does not occur, as they receive a full complex of vitamins with mother's milk.
Milk allergy: symptoms
Symptoms of an allergic reaction occur after drinking not only fresh milk, but also fermented milk products. Acute allergies appear within 1-2 hours after eating a small amount of allergenic food. In severe cases, symptoms appear within 10-20 minutes. The development of manifestations of chronic allergies takes up to a day, while the clinical picture is often mild. Pathology can also develop in a healthy person if milk predominates in his diet. With allergies of this nature, you should limit the amount of dairy products in the diet. The clinical picture of an allergic reaction to milk is quite extensive, it is individual for each person. Allergy to milk is characterized by such symptoms.
The clinical picture of an allergic reaction to milk is quite extensive, it is individual for each person. Allergy to milk is characterized by such symptoms.
- Violation of the gastrointestinal tract. The patient complains of heartburn, a feeling of heaviness in the abdomen, diarrhea, increased flatulence. There may also be stomach cramps, combined with vomiting.
- Respiratory reactions. After drinking milk, the patient develops shortness of breath, sneezing and dry cough begins. With severe allergies, swelling and spasm of the upper respiratory tract occurs.
- Skin inflammatory processes. A weak allergic reaction is characterized by urticaria, itching of the affected areas of the body, moderate swelling of the skin. If a critical amount of allergens enters the bloodstream, Quincke's edema develops.
When signs of allergy appear, the patient must be given first aid. If the victim is in serious condition, it is recommended to call an ambulance. Milk allergy is treated on an outpatient basis, in the absence of therapy, anaphylactic shock may develop, which quickly leads to the death of the patient. The main signs of anaphylactic shock: drop in blood pressure to a critical level, slow heartbeat, pale skin, cold sweat, dizziness.
Milk allergy is treated on an outpatient basis, in the absence of therapy, anaphylactic shock may develop, which quickly leads to the death of the patient. The main signs of anaphylactic shock: drop in blood pressure to a critical level, slow heartbeat, pale skin, cold sweat, dizziness.
How lactose allergy manifests itself
Lactose intolerance is a false form of allergy to dairy products. The mechanism of the development of the disease is not associated with the effect of allergens on blood cells. The pathological process occurs in the gastrointestinal tract, so its manifestations affect only the digestive organs. Flatulence (bloating), intestinal colic, diarrhea are signs that characterize lactose allergy. Symptoms also include belching, nausea, and vomiting. With chronic allergies, patients often develop a subconscious aversion to milk and products based on it.
Milk allergy in children
Dairy allergy in children is common. If the disease is not caused by a hereditary predisposition, the baby manages to cope with it by the age of 4-5 years. Sometimes the symptoms of the disease disappear after breastfeeding is completed. The causes of the pathology lie in the mother's diet (a woman consumes too much dairy products), in a lack of intestinal enzymes or intrauterine anomalies. Among babies under the age of one year, the most common allergy is cow's milk. In children, the symptoms of a food allergy are almost the same as the symptoms that occur in adults. So, in small allergies, the following signs of the disease are noted:
Sometimes the symptoms of the disease disappear after breastfeeding is completed. The causes of the pathology lie in the mother's diet (a woman consumes too much dairy products), in a lack of intestinal enzymes or intrauterine anomalies. Among babies under the age of one year, the most common allergy is cow's milk. In children, the symptoms of a food allergy are almost the same as the symptoms that occur in adults. So, in small allergies, the following signs of the disease are noted:
- increased flatulence;
- colic;
- loose stools;
- appearance of red spots on the cheeks, limbs, abdomen;
- skin rash with severe itching;
- fever;
- vomiting.
To eliminate allergy symptoms in a child, it is recommended that a nursing mother switch to hypoallergenic foods. Babies who are bottle-fed should be transferred to hydrolyzate mixtures. Pediatricians also recommend giving goat's milk to children with allergies. In composition, it is close to cow's, but contains fewer allergens.
Is it possible to be allergic to goat's milk? Allergies are triggered by the complex protein casein, which is part of the nutrient fluid. This protein makes up approximately 80% of cow's milk, and much less in goat's milk. With mild allergic reactions, doctors even recommend introducing goat's milk into the diet. Of course, the product does not help with allergies, but it allows you to abandon strict diets and enjoy a varied diet. However, this does not mean that goat's milk and allergies are incompatible things. For people with congenital lactose intolerance or an acute allergy to casein, the product is categorically contraindicated. Under such circumstances, goat's milk can provoke a severe inflammatory process.
Diagnosis of milk allergy
Today, pharmaceutical companies are actively promoting anti-allergy products, so the vast majority of people prefer not to visit a doctor. Such negligence causes addiction to drugs, and often provokes complications. The symptomatology of the pathology is so extensive that it is almost impossible to diagnose the disease without the participation of an experienced doctor. Some people are unaware that they may be allergic to milk, so they mistake signs of an allergic reaction for a cold or indigestion.
Some people are unaware that they may be allergic to milk, so they mistake signs of an allergic reaction for a cold or indigestion.
An allergist, an allergist-immunologist, and a pediatrician are responsible for diagnosing the disease. Milk allergy is determined by clinical manifestations, data on the patient's diet and laboratory results. The doctor interviews the patient, examines his outpatient card and conducts an examination. To determine the type of allergic reaction and prescribe the correct treatment, the doctor performs laboratory diagnostics. Research is aimed at identifying the allergen. Two main methods are used for this:
- skin allergy tests;
- immunogram.
Skin tests are prescribed for adults and children from 3 years of age with a mild allergic reaction. The allergen is injected with a needle under the skin or applied to the wrist. The result is evaluated within a day. If after a specified period of time the skin turns red or becomes covered with a rash, the patient is diagnosed with an allergy to milk.
Immunogram involves taking the patient's venous blood and then sending the sample to the laboratory. Under artificial conditions, the alleged allergen is injected into a test tube with blood. Monitoring of processes occurring at the cellular level is carried out using reagents and a microscope.
False or lactose allergy is diagnosed in a slightly different way. Since it is not associated with the production of histamine, skin tests and an immunogram are ineffective in this case. A patient with signs of lactose intolerance is advised to consult an allergist or gastroenterologist. After the examination, the doctor will prescribe the following procedures to the patient:
- coprogram (stool analysis) for the presence of lactic acid;
- urine and blood tests to determine the level of galactose;
- genetic blood test;
- endoscopy.
Milk allergy: treatment
Therapy is prescribed taking into account the causes of the allergic reaction. Allergy to milk protein is corrected by the patient following the following recommendations:
Allergy to milk protein is corrected by the patient following the following recommendations:
- a strict diet that excludes milk and dairy products;
- taking antihistamines, enterosorbents;
- use of hydrocortisone ointments and vasoconstrictor nasal/eye drops.
Congenital chronic milk allergy is eliminated with specific immunotherapy. The patient is given a kind of vaccination in the form of a subcutaneous injection of a small dose of casein. The body produces antigens that can neutralize the foreign substance, and the immune system becomes resistant to the allergen.
The treatment of lactose intolerance is aimed at combating the enzyme deficiency. The patient is recommended a diet based on a restriction in the diet of dairy products. A complete rejection of milk is not welcome, as it contains the nutrients the body needs. As an alternative, soy milk is also allowed. To normalize the intestinal microflora, the patient is prescribed enzyme preparations and multivitamin complexes.
reaction to milk may go away, but sensitivity to peanuts will remain forever
- Main
- All about allergies
- Allergy in children
- Baby allergy: reaction to milk may go away, but sensitivity to peanuts remains forever
Contents
Allergies in children
The most common allergy in children is food. It is diagnosed in approximately 1-1.5% of newborns. At the same time, if the baby is on artificial or mixed feeding, the risk of developing a reaction to food is higher.
And by the age of two, the percentage of children with food allergies, according to the American Academy of Allergy, Asthma and Immunology, is about 6%.
Among infants who are formula fed, the percentage of food allergies at this age is even higher - about 7%. In addition, there is evidence that approximately 2-8% of children in the first year of life show symptoms of an allergy to cow's milk proteins. And while milk allergy usually subsides by the age of three, in some cases it can persist until the age of seven or eight.
What's more, children with milk allergies are more likely to develop other allergies in the future, such as seasonal allergic rhinitis, allergies to other foods, or even asthma.
For this reason, pediatricians recommend for the first six months of a baby's life, if possible, to exclusively breastfeed the baby, and then gradually add a variety of complementary foods to the food, gradually increasing the number of new products. Such early prevention of food allergies has become recommended by doctors only recently. However, it doesn't always work either.
Causes of allergies in a child
Causes of allergic manifestations
If one of the parents has a food allergy, the risk of the same sensitivity in a child doubles. If both parents have food allergies, the risk is even greater. The seasonal allergic rhinitis and asthma mentioned above are also among the ailments that contribute to the development of sensitivity in a child to certain foods.
If both parents have food allergies, the risk is even greater. The seasonal allergic rhinitis and asthma mentioned above are also among the ailments that contribute to the development of sensitivity in a child to certain foods.
What foods can a baby be allergic to?
Although there are over 160 foods that can trigger allergies, 90% of all food reactions are caused by just eight of them. These include:
- Cow's milk
- Eggs
- Peanuts
- Tree nuts (e.g. walnuts, hazelnuts or almonds)
- Fish
- Shellfish
- Soya
- Wheat
At the same time, often up to 85% of all reactions are caused by just one allergen - cow's milk proteins. Next come eggs, peanuts and nuts.
Pediatricians have previously advised against introducing potential allergens into the baby's diet until the age of two or three. Today, the American Academy of Pediatrics believes that there is no evidence that such waiting prevents food allergies. Moreover, there is a hypothesis that early exposure to allergens (not earlier than 6-7 months of age) may contribute to the development of tolerance to them. Therefore, the child is advised to introduce the same peanuts (in the form of a paste) up to 12 months, with an egg - about 7-8 months, but the introduction of whole milk is best done after 12 months, not only because of its allergenic potential, but also its severity digestion. You also need to do with honey, which can be the causative agent of infant botulism. It is better to refrain from him until 1-2 years.
Moreover, there is a hypothesis that early exposure to allergens (not earlier than 6-7 months of age) may contribute to the development of tolerance to them. Therefore, the child is advised to introduce the same peanuts (in the form of a paste) up to 12 months, with an egg - about 7-8 months, but the introduction of whole milk is best done after 12 months, not only because of its allergenic potential, but also its severity digestion. You also need to do with honey, which can be the causative agent of infant botulism. It is better to refrain from him until 1-2 years.
In addition, when introducing a new product to a child, one should strictly adhere to certain rules, and not give several types of food unfamiliar to the baby at the same time. Each new ingredient is introduced no more than with a 3-5 day interval, and the introduction of products with a high level of allergic risk is better to "stretch" for a week. Such a scheme, in the event of a reaction, will help answer the frequent question of young parents: "How to understand what a child is allergic to?"
After all, observing the following recommendations, with changes in the behavior of the baby, the parents will have one specific "suspect". It is he who should be temporarily excluded from the menu in the event of a child's reaction. If the reaction occurs again - with the repeated introduction of food - the child should be shown to the doctor.
It is he who should be temporarily excluded from the menu in the event of a child's reaction. If the reaction occurs again - with the repeated introduction of food - the child should be shown to the doctor.
However, if it is too early for a formula-fed infant to introduce complementary foods with other foods and the infant still has a food reaction, or if the reaction persists despite avoiding various foods, the cause of the allergy may be "baby milk" .
Baby allergy symptoms
How do you know if a baby is allergic to formula and not, for example, digestive problems or contact dermatitis due to detergents? There is no single answer. After all, the symptoms in some babies can develop immediately, while others may take hours, or even days. But the following symptoms will help you understand what an allergy looks like in young children.
First, your baby may have gas. Due to the swollen and tense tummy, the child may often raise his legs up. If the baby cries at the same time, this may indicate colic.
If the baby cries at the same time, this may indicate colic.
Secondly, the child may openly show negativity towards feeding: have difficulty swallowing due to reflux (backward reflux of food from the stomach into the esophagus), vomit or spit food. By
in addition, diarrhea may occur. Watery stools with blisters and foul odors are a common sign of formula allergy, which can lead to severe dehydration, so check with your pediatrician right away. However, sometimes instead of diarrhea in children, on the contrary, constipation is observed, which can also indicate an allergy.
Persistent runny nose, shortness of breath, active breathing, phlegm in the throat and chronic cough may also be due to an allergy to infant formula.
And finally, the most direct clue that a child has an allergy is a rash. The rashes may be itchy, ooze fluid, or look like crusts.
Milk protein allergy can be diagnosed using multicomponent molecular allergy tests. With a mixture whose ingredients are not always exactly known, it can be more difficult. However, your doctor may suggest certain tests after you inform him of your symptoms. These include allergy skin tests, blood tests, and stool tests. However, even positive results of such tests are not always evidence of a real allergy. Therefore, the doctor may recommend other methods, such as an elimination diet (diet for elimination).
However, your doctor may suggest certain tests after you inform him of your symptoms. These include allergy skin tests, blood tests, and stool tests. However, even positive results of such tests are not always evidence of a real allergy. Therefore, the doctor may recommend other methods, such as an elimination diet (diet for elimination).
As the baby matures, some allergy symptoms may disappear. For example, in most children, “colic” disappears after reaching six months. If you introduce a new food to your child, watch for one or more of the following symptoms:
- urticaria
- blush skin, rash
- swelling of the face, tongue or lips
- vomiting and/or diarrhea
- cough or wheezing
- shortness of breath
- loss of consciousness
If you see mild symptoms such as hives or a rash, see your pediatrician for a follow-up evaluation.
Types of allergic rashes in children
Common types of allergic rashes in children include:
Eczema is one of the most common skin conditions in newborns. There are different types of eczema, but atopic eczema is one of the most common in infants and young children. An eczema rash may consist of tiny red bumps or may look like scaly, dry skin. Babies under 6 months of age are more likely to develop eczema-like rashes on the scalp, face, and forehead, according to the National Eczema Association. In children aged 6 months to 1 year, the rash often appears on the knees and elbows.
There are different types of eczema, but atopic eczema is one of the most common in infants and young children. An eczema rash may consist of tiny red bumps or may look like scaly, dry skin. Babies under 6 months of age are more likely to develop eczema-like rashes on the scalp, face, and forehead, according to the National Eczema Association. In children aged 6 months to 1 year, the rash often appears on the knees and elbows.
Papular urticaria is a localized allergic reaction to a bug bite. Bites from various insects, including mosquitoes, ticks, and bed bugs, can cause a reaction that produces small clusters of red bumps. Although the disease usually affects children aged 2-6 years, papular urticaria can also occur in newborns.
Urticaria. Skin lesions may itch and vary in shape. But, as a rule, they are pink or red with a thin red border. Urticaria can develop anywhere on the body.
And when a child develops a rash after touching something, it is called allergic contact dermatitis . Its presence is evidenced by redness and itching, spots on the skin, etc. Nickel, metal in fasteners and buttons, poison ivy or hogweed, cosmetics, chemical dyes, skin medications such as the antibiotic neomycin, antihistamines, and pain relievers can provoke such reactions.
Its presence is evidenced by redness and itching, spots on the skin, etc. Nickel, metal in fasteners and buttons, poison ivy or hogweed, cosmetics, chemical dyes, skin medications such as the antibiotic neomycin, antihistamines, and pain relievers can provoke such reactions.
The child may also develop angioedema . It occurs in the deeper layers of the skin along with hives or separately from it. Swelling can happen anywhere, but is most common around the eyes and mouth, and on the arms and legs.
What should I do if my newborn has an allergy?
If your child has difficulty breathing/wheezing, swelling of the face/lips, or severe vomiting or diarrhea after eating, call 911 immediately as the child may go into anaphylactic shock. If in this case adrenaline is not administered on time, the consequences can be even fatal.
And if a child develops a mild allergic reaction, this is no reason not to seek medical help. True, in this case a visit to the family doctor or pediatrician will be enough. The danger is that allergy symptoms may increase and worsen after further exposure to the allergen.
The danger is that allergy symptoms may increase and worsen after further exposure to the allergen.
Your pediatrician can refer you to an allergist who will ask more questions, do a physical exam, and give you a better diagnosis.
If your doctor detects a food allergy to a particular food, the best strategy is to avoid that allergen.
You will have to read food labels carefully and avoid them unless you are sure of their ingredients.
Some allergies go away with time, such as allergies to eggs and milk. But allergies to peanuts, tree nuts, and shellfish most often persist for life.
Baby Allergy Diet
Although formula-fed babies are at greater risk of developing allergies, sometimes even a baby who has never eaten anything other than breast milk can have a reaction. Then the cause should be sought in the diet of the mother. Allergenic proteins from foods are stored in milk for 3-6 hours after consumption.
If a child develops a food allergy, the mother's main task will be to determine what exactly is causing the reaction.
 Since allergy testing in young children is often not reliable, one way to determine which foods are a problem for your child is to keep a food diary.
Since allergy testing in young children is often not reliable, one way to determine which foods are a problem for your child is to keep a food diary. Most babies react to the same eight major allergens found in breast milk, most commonly cow's milk. If the reason is indeed in milk, the nursing mother will have to temporarily abandon products based on it. In this case, you will have to look for an alternative to protein among fish, beef, chicken, eggs, nuts and beans. You can also consume soy milk fortified with calcium or calcium supplements.
If it is a matter of another product, you will have to look for a replacement for its nutritional properties according to the same principle.
However, you need to understand that allergens can remain in breast milk for a long time, disappearing completely only after 1-2 weeks.
The child's symptoms may start to improve at this time, or it may take a month or more. But if the child does not show signs of improvement, or symptoms worsen after a month of dieting, you may need to eliminate other foods, but before doing so, be sure to consult a doctor.
Sometimes babies are allergic to more than one food. You don't have to give up breastfeeding. After all, breast milk provides protection against infections, reduces the risk of obesity and diabetes. In addition, breastfed babies are believed to have higher IQs.
Information sources:
- https://www.parents.com/baby/health/allergy/all-about-baby-allergies/
- https://doc.ua/bolezn/allergiya/allergiya-u-grudnogo-rebenka-i-detej
- https://www.momjunction.com/articles/common-baby-skin-allergies-and-its-causes_0083576/? amp=1
- http://www.healthofchildren.com/EF/Food-Allergies-and-Sensitivities.html
- https://www.medicalnewstoday.com/articles/322484
- https://www.webmd.com/parenting/baby/introducing-new-foods
- https://www.nhs.uk/conditions/pregnancy-and-baby/ food-allergies-in-babies-and-young-children /
- http://www.healthofchildren.com/EF/Food-Allergies-and-Sensitivities.html
- https://www.parents.