Mental health for pregnant women
Taking Care of Your Mental Health During Pregnancy (for Parents)
Pregnancy brings a mix of feelings, and not all of them are good. If you're feeling worried, you're not alone. Worry is common, especially during a woman's first pregnancy or an unplanned one. It can be even harder if you're dealing with depression or anxiety.
For your health and your baby's, take care of yourself as much as you can. Be sure to eat well, exercise, get enough sleep, and take your prenatal vitamins.
If you're feeling worried, sad, or nervous, talk to someone about it — and know when to reach out for help.
What Feelings Can Happen?
Mood swings are normal during pregnancy. But if you feel nervous or down all the time, it could be a sign of something deeper going on. Stress over being pregnant, changes in your body during the pregnancy, and everyday worries can take a toll.
Some pregnant women may have depression or anxiety:
- Depression is sadness or feeling down or irritable for weeks or months at a time.
Some women may have depression before getting pregnant. But it also can start during pregnancy for a number of reasons — for example, if a woman isn't happy about being pregnant or is dealing with a lot of stress at work or at home.
- Anxiety is a feeling of worry or fear over things that might happen. If you worry a lot anyway, many things can stress you out during pregnancy. You might worry that you won't be a good mother or that you can't afford to raise a baby.
Pregnant women may have other mental health issues, such as:
- bipolar disorder (episodes of low-energy depression and high-energy mania)
- post-traumatic stress disorder (PTSD)
- panic attacks (sudden, intense physical responses with a feeling of unexplained and paralyzing fear)
- obsessive-compulsive disorder (OCD)
- eating disorders (like bulimia or anorexia nervosa)
It's important to treat mental health concerns during pregnancy. Mothers who are depressed, anxious, or have another issue might not get the medical care they need. They might not take care of themselves, or they may use drugs and alcohol during the pregnancy. All of these things can harm a growing baby.
Mothers who are depressed, anxious, or have another issue might not get the medical care they need. They might not take care of themselves, or they may use drugs and alcohol during the pregnancy. All of these things can harm a growing baby.
If you have a mental health issue, talk with your doctor so you can get the help you need during and after your pregnancy.
How Can I Get Help?
If you feel anxious or depressed, talk to a doctor, counselor, or therapist, and get help right away. The sooner treatment starts, the sooner you'll feel better.
Also talk to a doctor about your overall health and any mental health issues you've had in the past. It's best for your doctor to know your full medical history, in case anything comes up during or after your pregnancy.
How Are Problems Treated?
Treatment for mental health problems may include:
- Prescription medicine. Always talk to a doctor before you start taking — or stop taking — any medicines during your pregnancy.
 If you take any kind of medicine for a mental health issue and are pregnant or planning to get pregnant, tell your doctor. Don't stop taking it unless your doctor tells you to. Some medicines may cause problems for a growing baby, but stopping your medicine may make things worse. Your doctor can make a treatment plan that is best for you and your baby.
If you take any kind of medicine for a mental health issue and are pregnant or planning to get pregnant, tell your doctor. Don't stop taking it unless your doctor tells you to. Some medicines may cause problems for a growing baby, but stopping your medicine may make things worse. Your doctor can make a treatment plan that is best for you and your baby. - Talk therapy. Talking one-on-one with a therapist can be a great way to manage stress, deal with depression, and ease anxiety during pregnancy. Finding a support group where you can share your concerns with other mothers who know what you're going through also can help. Talking with a social worker or counselor can help you deal with money issues, worries over raising a child, or other stresses in your life.
- Other approaches. Many women find comfort in activities like yoga, exercise, and meditation. If you're feeling stressed or overwhelmed, talking to a friend, family member, or faith leader can help you feel better.

Many moms feel anxious or depressed at some point in their pregnancy, and some may even need treatment for it. But a mental health problem doesn't have to be a problem for you or your baby. Get the help you need to feel better, and you'll be doing the best thing for you both.
Reviewed by: Mary L. Gavin, MD
Date reviewed: February 2017
Psychiatric Disorders During Pregnancy
Although pregnancy has typically been considered a time of emotional well-being, recent studies suggest that up to 20% of women suffer from mood or anxiety disorders during pregnancy. Particularly vulnerable are those women with histories of psychiatric illness who discontinue psychotropic medications during pregnancy. In a recent study which prospectively followed a group of women with histories of major depression across pregnancy, of the 82 women who maintained antidepressant treatment throughout pregnancy, 21 (26%) relapsed compared with 44 (68%) of the 65 women who discontinued medication. This study estimated that women who discontinued medication were 5 times as likely to relapse as compared to women who maintained treatment.
This study estimated that women who discontinued medication were 5 times as likely to relapse as compared to women who maintained treatment.
High rates of relapse have also been observed in women with bipolar disorder. One study indicated that during the course of pregnancy, 70.8% of the women experienced at least one mood episode. The risk of recurrence was significantly higher in women who discontinued treatment with mood stabilizers (85.5%) than those who maintained treatment (37.0%).
Although data accumulated over the last 30 years suggest that some medications may be used safely during pregnancy, knowledge regarding the risks of prenatal exposure to psychotropic medications is incomplete. Thus, it is relatively common for patients to discontinue or to avoid pharmacologic treatment during pregnancy.
The New U.S. FDA Pregnancy Labeling and Lactation Rule
In 1975, the U.S. Food and Drug Administration (FDA) provided guidelines to drug companies for labeling medications with regard to their safety during pregnancy. This system of classification used five risk categories (A, B, C, D and X) based on data derived from human and animal studies. While widely used to make decisions regarding the use of medications during pregnancy, many criticized this system of classification, indicating that this type of drug labeling was often not helpful and, even worse, may be misleading.
This system of classification used five risk categories (A, B, C, D and X) based on data derived from human and animal studies. While widely used to make decisions regarding the use of medications during pregnancy, many criticized this system of classification, indicating that this type of drug labeling was often not helpful and, even worse, may be misleading.
In an effort to improve the accuracy and usefulness of information regarding the safety of medications used during pregnancy and breastfeeding, the FDA proposed a newly designed system on June 30th 2015. The Pregnancy and Lactation Labeling Rule or PLLR will abolish the letter categories and instead will include more comprehensive information discussing the potential risks and benefits to the mother and the fetus, and how these risks may change during the course of pregnancy.
Companies will be required to remove the pregnancy letter categories from the labeling for all prescription drugs and will have to revise the labeling with updated information. Medications approved before June 30, 2001 are not covered by the PLLR.
Medications approved before June 30, 2001 are not covered by the PLLR.
Weighing the Risks
Women with histories of psychiatric illness frequently come in for consultations regarding the use of psychotropic medications during pregnancy. Not infrequently, women present with the first onset of psychiatric illness while pregnant. Many pregnancies are unplanned and may occur unexpectedly while women are receiving treatment with medications for psychiatric disorders. Many women may consider stopping medication abruptly after learning they are pregnant, but for many women this may carry substantial risks.
Decisions regarding the initiation or maintenance of treatment during pregnancy must reflect an understanding of the risks associated with fetal exposure to a particular medication but must also take into consideration the risks associated with untreated psychiatric illness in the mother. Psychiatric illness in the mother is not a benign event and may cause significant morbidity for both the mother and her child; thus, discontinuing or withholding medication during pregnancy is not always the safest option.
Depression and anxiety during pregnancy have been associated with a variety of adverse pregnancy outcomes. Women who suffer from psychiatric illness during pregnancy are less likely to receive adequate prenatal care and are more likely to use alcohol, tobacco, and other substances known to adversely affect pregnancy outcomes. Several studies have described low birth weight and fetal growth retardation in children born to depressed mothers. Preterm delivery is another potential pregnancy complication among women experiencing distress during pregnancy. Pregnancy complications related to maternal depression and anxiety in late pregnancy have also been described, including an increased risk for having pre-eclapsia, operative delivery, and infant admission to a special care nursery for a variety of conditions including respiratory distress, hypoglycemia, and prematurity. These data underscore the need to perform a thorough risk/benefit analysis of pregnant women with psychiatric illness, including evaluating the impact of untreated illness on the baby and the mother, as well as the risks of using medication during pregnancy.
What are the Risks of Medication Exposure?
All medications diffuse readily across the placenta, and no psychotropic drug has yet been approved by the Food and Drug Administration (FDA) for use during pregnancy. When prescribing medications during pregnancy, one must consider the following risks associated with prenatal exposure: risk of teratogenesis, risk of neonatal toxicity, and risk of long-term neurobehavioral sequelae.
Risk of Teratogenesis
The baseline incidence of major congenital malformations in newborns born in the United States is estimated to be between 2 and 4%. During the earliest stages of pregnancy, formation of major organ systems takes place and is complete within the first 12 weeks after conception. Therefore, discussion around risks of exposures during pregnancy may be broken down by the timing of exposure or trimester, with particular vigilance around first trimester exposures.
A teratogen is defined as an agent that interferes the in utero development process and produces some type of organ malformation or dysfunction. For each organ or organ system, there exists a critical period during which development takes place and is susceptible to the effects of a teratogen. For example, neural tube folding and closure, forming the brain and spinal cord, occur within the first four weeks of gestation. Most of the formation of the heart and great vessels takes place from four to nine weeks after conception, although the entire first trimester is often considered pertinent.
For each organ or organ system, there exists a critical period during which development takes place and is susceptible to the effects of a teratogen. For example, neural tube folding and closure, forming the brain and spinal cord, occur within the first four weeks of gestation. Most of the formation of the heart and great vessels takes place from four to nine weeks after conception, although the entire first trimester is often considered pertinent.
Risk of Neonatal Symptoms
Neonatal toxicity or perinatal syndromes (sometimes referred to as neonatal “withdrawal”) refer to a spectrum of physical and behavioral symptoms observed in the acute neonatal period that can be attributed to drug exposure at or near the time of delivery. Anecdotal reports that attribute these syndromes to drug exposure must be cautiously interpreted, and larger samples must be studied in order to establish a causal link between exposure to a particular medication and a perinatal syndrome.
Risk of Long-Term Effects
Although the data suggest that some medications may be used safely during pregnancy if clinically warranted, our knowledge regarding the long-term effects of prenatal exposure to psychotropic medications is incomplete. Because neuronal migration and differentiation occur throughout pregnancy and into the early years of life, the central nervous system (CNS) remains particularly vulnerable to toxic agents throughout pregnancy. While exposures to teratogens early in pregnancy may result in clear abnormalities, exposures that occur after neural tube closure (at 32 days of gestation) may produce more subtle changes in behavior and functioning.
Because neuronal migration and differentiation occur throughout pregnancy and into the early years of life, the central nervous system (CNS) remains particularly vulnerable to toxic agents throughout pregnancy. While exposures to teratogens early in pregnancy may result in clear abnormalities, exposures that occur after neural tube closure (at 32 days of gestation) may produce more subtle changes in behavior and functioning.
Behavioral teratogenesis refers to the potential of a psychotropic drug administered during pregnancy to have long-term neurobehavioral effects. For example, are children who have been exposed to an antidepressant in utero at risk for cognitive or behavioral problems at a later point during their development? To date, few studies have systematically investigated the impact of exposure to psychotropic medications in utero on development and behavior in humans.
Antidepressants and Pregnancy
Of all the antidepressants, fluoxetine (Prozac) is the best characterized antidepressant. Data collected from over 2500 cases indicate no increase in risk of major congenital malformation in fluoxetine-exposed infants. One prospective study of 531 infants with first trimester exposure to SSRIs (mostly citalopram, n=375) did not demonstrate an increased risk of organ malformation.
Data collected from over 2500 cases indicate no increase in risk of major congenital malformation in fluoxetine-exposed infants. One prospective study of 531 infants with first trimester exposure to SSRIs (mostly citalopram, n=375) did not demonstrate an increased risk of organ malformation.
Several meta-analyses combining studies with exposures to SSRIs do not demonstrate an increase in risk of congenital malformation in children exposed to these antidepressants, with the exception of paroxetine (Paxil). There has been particular controversy around paroxetine use in pregnancy, as past reports have suggested that first trimester exposure to paroxetine was associated with an increased risk of cardiac defects including atrial and ventricular septal defects. Other published studies have not demonstrated increased teratogenicity of paroxetine. Importantly, independently conducted meta-analyses of available data sets have consistently found a lack of association between paroxetine exposure and cardiovascular malformations. Even so, these findings prompted the FDA to change the category label of paroxetine from C to D.
Even so, these findings prompted the FDA to change the category label of paroxetine from C to D.
Three prospective and more than ten retrospective studies have examined the risk of organ malformation in over 400 cases of first trimester exposure to tricyclic antidepressants of TCAs. When evaluated on an individual basis and when pooled, these studies do not indicate a significant association between fetal exposure to TCAs and risk for any major congenital anomaly. Among the TCAs, desipramine and nortriptyline are often preferred since they are less anti-cholinergic and the least likely to exacerbate orthostatic hypotension that occurs during pregnancy.
Bupropion may be an option for women who have not responded to fluoxetine or a tricyclic antidepressant, as data thus far have not indicated an increased risk of malformations associated with bupropion use during pregnancy. The most recent information from the Bupropion Pregnancy Registry maintained by the manufacturer GlaxoSmithKline includes data from 517 pregnancies involving first trimester exposure to bupropion. In this sample, there were 20 infants with major malformations. This represents a 3.9% risk of congenital malformation that is consistent with what is observed in women with no known teratogen exposure. While this information regarding the overall risk of malformation is reassuring, earlier reports had revealed an unexpectedly high number of malformations of the heart and great vessels in bupropion-exposed infants. A retrospective cohort study including over 1200 infants exposed to bupropion during the first trimester did not reveal an increased risk of malformations in the bupropion-exposed group of infants nor did it demonstrate an increased risk for cardiovascular malformations.
In this sample, there were 20 infants with major malformations. This represents a 3.9% risk of congenital malformation that is consistent with what is observed in women with no known teratogen exposure. While this information regarding the overall risk of malformation is reassuring, earlier reports had revealed an unexpectedly high number of malformations of the heart and great vessels in bupropion-exposed infants. A retrospective cohort study including over 1200 infants exposed to bupropion during the first trimester did not reveal an increased risk of malformations in the bupropion-exposed group of infants nor did it demonstrate an increased risk for cardiovascular malformations.
Scant information is available regarding the reproductive safety of monoamine oxidase inhibitors (MAOIs), and these agents are generally not used in pregnancy as they may produce a hypertensive crisis when combined with tocolytic medications, such as terbutaline.
With regard to the newer antidepressants, prospective data on 150 women exposed to venlafaxine (Effexor) during the first trimester of pregnancy suggest no increase in risk of major malformation as compared to non-exposed controls. To date, the literature does not include prospective data on the use of duloxetine (Cymbalta).
To date, the literature does not include prospective data on the use of duloxetine (Cymbalta).
Another prospective study assessed outcomes in 147 women taking either nefazodone (n=89) or trazodone (n=58) during their first trimester of pregnancy and compared them to two control groups of women exposed to either non-teratogenic drugs (n = 147) or to other antidepressants (n=147). There were no significant differences among exposed and non-exposed groups with regard to rates of congenital malformations. In another report, there were no differences in malformation rates among women who took mirtazapine (Remeron) (n=104) during pregnancy as compared to women who took other antidepressants or controls exposed to known nonteratogens.
While these initial reports are reassuring, larger samples are required to establish the reproductive safety of these newer antidepressants. It is estimated that at least 500 to 600 exposures must be collected to demonstrate a two-fold increase in risk for a particular malformation over what is observed in the general population. In general, the SSRIs, specifically fluoxetine, citalopram, and sertraline, are the antidepressants most commonly used during pregnancy.
In general, the SSRIs, specifically fluoxetine, citalopram, and sertraline, are the antidepressants most commonly used during pregnancy.
Several recent studies have suggested that exposure to SSRIs near the time of delivery may be associated with poor perinatal outcomes. Attention has focused on a range of transient neonatal distress syndromes associated with exposure to (or withdrawal from) antidepressants in utero. These syndromes appear to affect about 25% of babies exposed to antidepressants late in pregnancy. The most commonly reported symptoms in the newborns include tremor, restlessness, increased muscle tone, and increased crying. Reassuringly, these syndromes appear to be relatively benign and short-lived, resolving within 1 to 4 days after birth without any specific medical intervention.
These studies deserve careful consideration, yet one of the major shortcomings is that most have failed to use raters blinded to the mother’s treatment status. The decision to admit a newborn to a special care nursery may represent a reasonable precaution for an infant exposed to medication in utero and may not be an indication of a serious problem. Another limitation is that few studies have attempted to assess maternal mood during pregnancy or at the time of delivery. There is ample evidence to suggest that depression or anxiety in the mother may contribute to poor neonatal outcomes, including premature delivery and low birth weight, and it is important to evaluate the contribution of maternal mood to neonatal outcomes.
The decision to admit a newborn to a special care nursery may represent a reasonable precaution for an infant exposed to medication in utero and may not be an indication of a serious problem. Another limitation is that few studies have attempted to assess maternal mood during pregnancy or at the time of delivery. There is ample evidence to suggest that depression or anxiety in the mother may contribute to poor neonatal outcomes, including premature delivery and low birth weight, and it is important to evaluate the contribution of maternal mood to neonatal outcomes.
Based on these findings, many women are advised to taper or discontinue treatment with SSRIs prior to delivery; however, this strategy has not been shown to change neonatal outcomes. Importantly, neonatal effects have been reported with both untreated mood and anxiety disorders, as well as with medication, and limited studies have adequately teased out these variables. One important consideration is that discontinuation of or reductions in the dosage of mediation in the latter part of pregnancy may increase the risk of postpartum depression, as the postpartum period is a time of increased vulnerability to psychiatric illness and depression or anxiety during pregnancy has been associated with postpartum depression.
Another concern has been that maternal SSRI use may be associated with a higher than expected number of cases of persistent pulmonary hypertension of the newborn (PPHN). In one report, the use of an SSRI antidepressant after the 20th week of gestation was significantly associated with a six-fold greater risk of PPHN. If we assume that these findings are correct, the risk is still relatively small; the authors estimate the risk of PPHN to be less than 1% in infants exposed to SSRIs in utero. Since the initial report on this topic, three studies have found no association between antidepressant use during pregnancy and PPHN, and one study showed a much lower risk than the 1% originally reported. These findings taken together bring into question whether there is an association at all and suggest that, if there is a risk, it is much lower than that reported in the original 2006 report.
To date only two studies have systematically investigated the impact of exposure to antidepressants in utero on development and behavior in humans. The first of these studies followed a cohort of 135 children who had been exposed to either tricyclic antidepressants or fluoxetine (Prozac) during pregnancy (most commonly during the first trimester) and compared these subjects to a cohort of non-exposed controls. Results indicated no significant differences in IQ, temperament, behavior, reactivity, mood, distractibility, or activity level between exposed and non-exposed children followed up to 7 years of age. A more recent report from the same group that followed a cohort of children exposed to fluoxetine or tricyclic antidepressants for the entire duration of the pregnancy yielded similar results. The authors concluded that their findings support the hypothesis that fluoxetine and tricyclic antidepressants are not behavioral teratogens and do not have a significant effect on cognitive development, language or behavior.
The first of these studies followed a cohort of 135 children who had been exposed to either tricyclic antidepressants or fluoxetine (Prozac) during pregnancy (most commonly during the first trimester) and compared these subjects to a cohort of non-exposed controls. Results indicated no significant differences in IQ, temperament, behavior, reactivity, mood, distractibility, or activity level between exposed and non-exposed children followed up to 7 years of age. A more recent report from the same group that followed a cohort of children exposed to fluoxetine or tricyclic antidepressants for the entire duration of the pregnancy yielded similar results. The authors concluded that their findings support the hypothesis that fluoxetine and tricyclic antidepressants are not behavioral teratogens and do not have a significant effect on cognitive development, language or behavior.
Mood Stabilizers
For women with bipolar disorder, maintenance treatment with a mood stabilizer during pregnancy can significantly reduce the risk of relapse. However, many of the medications commonly used to treat bipolar disorder carry some teratogenic risk when used during pregnancy.
However, many of the medications commonly used to treat bipolar disorder carry some teratogenic risk when used during pregnancy.
Concerns regarding fetal exposure to lithium, have typically been based on early reports of higher rates of cardiovascular malformations (e.g., Ebstein’s anomaly) following prenatal exposure to this drug. More recent data suggest the risk of cardiovascular malformations following first trimester exposure to lithium is smaller than previous assessments and is estimated to be between 1 in 2000 (0.05%) and 1 in 1000 (0.1%). Compared to lithium, prenatal exposure to some anticonvulsants is associated with a far greater risk for organ malformation. First trimester use of carbamazepine (Tegretol) has been associated with a 1% risk of neural tube defect. Of all of the medications used for psychiatric disorders, the one with the greatest potential of serious birth defects is valproate (valproic acid, Depakote). Factors which appear to increase the risk for teratogenesis include higher maternal serum anticonvulsant levels and exposure to more than one anticonvulsant. With a risk of neural tube defect ranging from 1 to 6%, this drug is often considered one of last resort in reproductive aged women, since the risk for teratogenicity is high in very early pregnancy, before many women realize they are pregnant.
With a risk of neural tube defect ranging from 1 to 6%, this drug is often considered one of last resort in reproductive aged women, since the risk for teratogenicity is high in very early pregnancy, before many women realize they are pregnant.
Prenatal exposure to valproic acid has also been associated with characteristic craniofacial abnormalities, cardiovascular malformation, limb defects and genital anomalies, as well as other central nervous system structural abnormalities. Also, valproate exposure during pregnancy has been associated with poorer neurocognitive development in children followed to three years of age. In the same study, lamotrigine use (discussed below) did not affect neurocognitive development.
While other anticonvulsants are being used more frequently in the treatment of bipolar disorder, there is limited information on the reproductive safety of these newer anticonvulsants, specifically gabapentin (Neurontin), oxcarbazepine (Trileptal), tigabine (Gabitril), levetiracetam (Keppra), zonisamide (Zonegran). One report has raised concerns regarding potential teratogenicity of topiramate (Topamax).
One report has raised concerns regarding potential teratogenicity of topiramate (Topamax).
However, there is a growing body of information the reproductive safety of lamotrigine (Lamictal), and this may be a useful alternative for some women. The International Lamotrigine Pregnancy Registry was created by GlaxoSmithKline (GSK) in 1992 to monitor pregnancies exposed to lamotrigine for the occurrence of major birth defects. Data from the Registry did not show an elevated risk of malformations associated with lamotrigine exposure.
Other data from the North-American Anti-Epileptic Drug Registry indicates the prevalence of major malformations in a total of 564 children exposed to lamotrigine monotherapy was 2.7%; however, five infants had oral clefts, indicating a prevalence rate of 8.9 per 1000 births. In a comparison group of 221,746 unexposed births, the prevalence rate for oral clefts was 0.37/1000, indicating a 24-fold increase in risk of oral cleft in infants exposed to lamotrigine. However, other registries have not demonstrated such a significant increase in risk for oral clefts. It is important to put this risk into perspective. If we assume that the findings from the North American registry are true, the absolute risk of having a child with cleft lip or palate is about 0.9%.
However, other registries have not demonstrated such a significant increase in risk for oral clefts. It is important to put this risk into perspective. If we assume that the findings from the North American registry are true, the absolute risk of having a child with cleft lip or palate is about 0.9%.
Atypical antipsychotic agents (discussed in greater detail below) are commonly used often to manage the acute symptoms of bipolar illness, as well as for maintenance treatment. While the data regarding the reproductive safety of these newer agents is limited, no studies thus far have indicated any teratogenic risk associated with this class of medications. For this reason, some women may choose to use an atypical antipsychotic agent during pregnancy (especially during the first trimester) in order to avoid using a known teratogen, such as lithium or valproic acid.
Anti-Anxiety Medications
The consequences of prenatal exposure to benzodiazepines have been debated for over twenty years. Three prospective studies support the absence of increased risk of organ malformation following first trimester exposure to benzodiazepines. More controversial has been the issue of whether first trimester exposure to benzodiazepines increases risk for specific malformations. Although initial reports suggested that there may be an increased risk of cleft lip and palate, more recent reports have shown no association between exposure to benzodiazepines and risk for cleft lip or palate. This risk– if it exists — is calculated to be 0.7%, approximately a ten-fold increase in risk for oral cleft over that observed in the general population. Nonetheless, the likelihood that a woman exposed to benzodiazepines during the first trimester will give birth to a child with this congenital anomaly, although significantly increased, remains less than 1%.
Three prospective studies support the absence of increased risk of organ malformation following first trimester exposure to benzodiazepines. More controversial has been the issue of whether first trimester exposure to benzodiazepines increases risk for specific malformations. Although initial reports suggested that there may be an increased risk of cleft lip and palate, more recent reports have shown no association between exposure to benzodiazepines and risk for cleft lip or palate. This risk– if it exists — is calculated to be 0.7%, approximately a ten-fold increase in risk for oral cleft over that observed in the general population. Nonetheless, the likelihood that a woman exposed to benzodiazepines during the first trimester will give birth to a child with this congenital anomaly, although significantly increased, remains less than 1%.
Currently, no systematic data are available on the reproductive safety of non-benzodiazepine anxiolytic agents such as buspirone and hypnotic agents zolpidem (Ambien) and zalepion (Sonata). Therefore, these medications are not recommended for use in pregnancy.
Therefore, these medications are not recommended for use in pregnancy.
Anti-Psychotic Medications
In addition to the atypical antipsychotic medications described above, recent studies have not demonstrated teratogenic risk associated with high-or medium-potency neuroleptic medications; however, a recent meta-analysis of the available studies noted a higher risk of congenital malformations after first trimester exposure to low-potency neuroleptic agents. In clinical practice, higher potency neuroleptic agents such as haloperidol (Haldol), perphenazine (Trilafon), and trifluoperazine (Stelazine) are recommended over the lower potency agents in managing pregnant women with psychiatric illness.
Atypical antipsychotic medications are increasingly being used to treat a spectrum of psychiatric disorders, including psychotic disorders and bipolar disorder, as well as treatment refractory depression and anxiety disorders. The first and largest published prospective study on the reproductive safety of the atypical agents provided reassuring data regarding the risk of malformations in the first trimester, although aripiprazole (Abilify) was not among the medications studied. Investigators prospectively followed a group of 151 women taking olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), or clozapine (Clozapine) and compared outcomes to controls without exposure to known teratogens. There were no differences between the groups in terms of risk for major malformations, or rates of obstetrical or neonatal complications.
Investigators prospectively followed a group of 151 women taking olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), or clozapine (Clozapine) and compared outcomes to controls without exposure to known teratogens. There were no differences between the groups in terms of risk for major malformations, or rates of obstetrical or neonatal complications.
While this information is reassuring, it is far from definitive, and larger studies are required to provide more information about the reproductive safety of these medications. To this end, the National Pregnancy Registry has been created to prospectively gather information regarding outcomes in infants exposed in utero to these newer atypical antipsychotic medications.
The U.S. Food and Drug Administration (FDA) recently updated labels for the entire class of antipsychotic drugs to include warnings regarding the use of antipsychotic drugs (both the typical and atypical agents) during pregnancy. The new drug labels now contain more details on the potential risk for abnormal muscle movements (extrapyramidal signs or EPS) and withdrawal symptoms in newborns exposed to these drugs during the third trimester of pregnancy. These recommendations were derived from adverse event reporting. While this may signal a potential problem associated with exposure to antipsychotic medications, it does not yield accurate information regarding the prevalence of an adverse event.
These recommendations were derived from adverse event reporting. While this may signal a potential problem associated with exposure to antipsychotic medications, it does not yield accurate information regarding the prevalence of an adverse event.
For the latest information on psychiatric disorders during pregnancy, please visit our blog.
How do I get an appointment?
Consultations regarding treatment options can be scheduled by calling our intake coordinator at 617-724-7792.
Pregnancy Research at the CWMH
Currently we are conducting several studies related to depression and pregnancy. To learn more about this study or to sign up for our research patient registry, please click here
Psycho-emotional state of women with spontaneous pregnancy and after the use of assisted reproductive technologies
HEALTH OF WOMAN. 2019.10(146): 10–15; doi 10.15574/HW.2019.146.10
Benyuk V. A., Vigovskaya L. N., Maidannik I. V., Oleshko V. F.
F.
National Medical University named after N.N. A.A. Bogomolets, Kyiv
The article highlights the relationship of psychological processes that accompany physiological changes in the body of a pregnant woman. After all, pregnancy is a state of functional tension of all systems and organs of a woman. Of course, increased stress is reflected in the psychological state of the pregnant woman.
From the point of view of psychology, during pregnancy, a woman undergoes certain successive psychological changes - making a decision to continue the pregnancy, the period of pregnancy before the fetal movement, the period after the onset of movement, the prenatal period and childbirth.
According to a literature review, each trimester of pregnancy has a certain psychological "portrait" of a pregnant woman. So, in the first trimester, many women are characterized by an increase in psychological passivity and the appearance of a sense of satisfaction and pleasure, other women note a feeling of depression and increased physical activity associated with the realization of the very fact of pregnancy.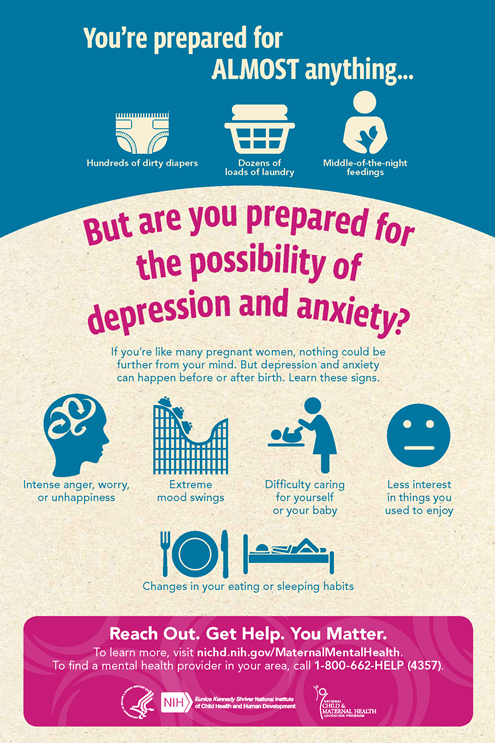
The second trimester of pregnancy is characterized by the normalization of the mental state and increased efficiency. However, it is precisely at this time that a restructuring takes place in the system of worldview and the formation of motherhood motivation, and the appearance of fetal movements allows concretizing the image of the child and provides a basis for interpreting his subjective state.
The third trimester of pregnancy is characterized by an increase in the level of anxiety and anxiety - fear of childbirth, regarding the health of the unborn child and an increase in the frequency of depressive disorders. Activity during this period is aimed at preparing for childbirth and the postpartum period, and activity not related to the birth of a child is reduced.
The prenatal period is characterized by a decrease in the activity of the pregnant woman, general relaxation and emotional "exhaustion", which protects the mother and child from unnecessary stress and worries. In a pregnant woman, the fear of childbirth decreases and the ability to concentrate on only one dominant essence increases, which will be extremely necessary during childbirth and postpartum interaction with the child.
In a pregnant woman, the fear of childbirth decreases and the ability to concentrate on only one dominant essence increases, which will be extremely necessary during childbirth and postpartum interaction with the child.
The postpartum period is characterized by an adjustment to feelings of emptiness and a sense of inner emptiness.
The psychological state is of leading importance in carrying a pregnancy. Some researchers point out that it is impossible to explain preterm birth only in terms of physiological and chemical changes during pregnancy.
Taking into account a number of physiological changes in the psychological sphere of women with spontaneous pregnancy, an analysis was made of the psychological state of 249 pregnant women after the use of assisted reproductive technologies and 50 pregnant women with spontaneous pregnancy.
A study of the psycho-emotional state of pregnant women after the use of assisted reproductive technologies revealed deviations in the level of personal and reactive anxiety that are inherent in women after the use of assisted reproductive technologies. With this in mind, we consider it appropriate to involve a psychologist in work with pregnant women after the use of assisted reproductive technologies in order to correct the identified deviations.
With this in mind, we consider it appropriate to involve a psychologist in work with pregnant women after the use of assisted reproductive technologies in order to correct the identified deviations.
Key words: pregnancy, assisted reproductive technologies, psychological state, personal anxiety, reactive anxiety.
BIBLIOGRAPHY
1. Ayvazyan E.B. The development of a woman's bodily and emotional experience during pregnancy: Diss. … cand. psychol. Sciences. - M., 2005. - 319 p.
2. Bodyazhina V.I., Semenchenko I.B. (2005). Obstetrics [proc. allowance for medical students. colleges] / Ed. 4th. - Rostov-on-Don: Phoenix. - 477 p.
3. Broipgigam W., Christian I., Rad M. (1999). Psychosomatic medicine / Per. With him. – M.: Geotar medicine. – S. 295–310.
4. Brutman V.I., Varga A.Ya., Rodionova M.S. (1998). The study of the states of consciousness at various stages of the reproductive period of women. Social and mental health of the child and family: protection, assistance, return to life. - M. - S. 142-143.
Social and mental health of the child and family: protection, assistance, return to life. - M. - S. 142-143.
5. Brutman V.I., Varga A.Ya., Khamitova I.Yu. (2000). Influence of family factors on the formation of deviant behavior of the mother // Psychological journal. 2:48–57.
6. Brutman V.I., Pankratova M.G., Enikolonov S.N. (1995). Unwanted pregnancy of victims of sexual violence (psychological and psychiatric aspects) // Questions of psychology. 1:33–39.
7. Brutman V.I., Filippova G.G., Khamitova I.Yu. (2002). Dynamics of the psychological state of women during pregnancy and after childbirth // Questions of psychology. 6:49–57.
8. Volodin N.N. (2009). Perinatal psychology and psychiatry. - M.: Publishing Center "Academy". – 364 p.
9. Gusev A.N., Izmailov C.A., Mikhalevskaya M.B. (1997). Measurement in psychology: general psychological practice. - M.: "Meaning", 1997. - 280 p.
10. Grigorieva E.S. (2011). The role of a woman's personality traits in the occurrence of pregnancy pathology (a review of modern research). Psychology of corporeality: Theoretical and practical research. 4:177-185.
11. Dermanova I.B. (2002). Anxiety research (C.D. Spielberger, adaptation by Yu.L. Khanin). Diagnostics of emotional and moral development. - St. Petersburg. - S. 124-126.
12. Dobryakov I.V., Prokhorov V.N., Prokhorova O.V. (2016). Psychological diagnostics in perinatal psychology. Diagnostics in medical (clinical) psychology: current state and prospects / Collective monograph. - S. 118-132.
13. Dobryakov I.V. (2011). Perinatal psychology. - "Peter", 1st edition. - 272 p.
14. Eltsova-Strelkova V.I. (1987). Obstetrics (textbook) / Ed. E.V. Mareev. – M.: Ed. UDN. – 301 s.
15. Zalevsky G.V., Mamysheva N.L., Shelekhov I.L. (2005). Individual psychological characteristics of pregnant women in the prediction of the formation of deviant forms of maternal behavior. Siberian Journal of Psychology. 22:7–12.
Siberian Journal of Psychology. 22:7–12.
16. Karaseva A.E., Kiselev V.D., Fadeeva N.I. (2001). Psychological features of women with a diagnosis of weakness of the birth forces // Obstetrics and Gynecology. 1:44-45.
17. Kopyl O.A., Baz L.L., Bazhenova O.V. (1994). Readiness for motherhood: identification of factors and conditions of psychological risk for the future development of the child // Zhurn. Synapse. 5:27–38.
18. Kochneva M.A. (1992). Features and role of mental reactions of pregnant women in the development of complicated pregnancy and childbirth: Dis. … cand. honey. Sciences. - M. - 191 p.
19. Krechetov A.B., Abramchenko V.V. (1968). On some neuropsychic reactions in pregnant women and women in childbirth // Journal of Neurology and Psychiatry named after Korsakov. 7:7-18.
20. Leskov G.A., Piskunova T.V., Zhabina T.P. (1992). Assessment of the level of neuroticism and psychopathization in women in the department of pathology of the reproductive function of women. - S-P. – S. 104–06.
- S-P. – S. 104–06.
21. Misyuk M.N., Kovalenko E.S. (2008). Anxiety and fears as a manifestation of the emotional sphere of pregnant women. Management in social and economic systems: materials of the XVII International Scientific and Practical Conference (June 2–6, 2008, Minsk) // Minsk Int. management; redol. - Minsk. - S. 413-414.
22. Noskova O.V. (2008). Features of the anxiety state of women during pregnancy and its psychocorrection // Medical psychology. 3:52-56.
23. Pines D. Unconscious use of her body by a woman. - S-P.: Ed. East European Institute of Psychoanalysis, 1997. - 196 p.
24. Plotnikov V.V., Mironova T.A., Kazarenko L.L. (1996). Psychophysiological factors in miscarriage. History of Saburova dacha: Advances in psychiatry, neurology, neurosurgery and narcology / Collection of scientific works of the Ukrainian Research Institute of Clinical and Experimental Neurology and Psychiatry and Kharkiv City Clinical Psychiatric Hospital No. 15 (Saburova dacha). Under total ed. I.I. Kutko and P.T. Petryuk. - Kharkiv. 3:307 - 309.
15 (Saburova dacha). Under total ed. I.I. Kutko and P.T. Petryuk. - Kharkiv. 3:307 - 309.
25. Rymashevsky N.V. Kovalenko V.M., Volkov A.E., Trufonova O.K. (1990). Personality characteristics of pregnant women in normal and pathological conditions // Journal of Nervous Pathology and Psychiatry. Korsakov. 5.97-101.
26. Filippova G.G. (1995). The image of the world and the motivational foundations of motherhood. Problems of studying and developing the personality of a preschooler. - Perm. – P. 31–36.
27. Filippova G.G. (1992). Psychology of motherhood and early ontogenesis. - M. "Life and Thought". - 192 p.
28. Horney K. (1997). Collected works in 3 volumes. - M .: "Meaning". - T. 1. - 496 p.
29. Bems B. (1988). The Different Faces of Motherhood. Eds., F. Hay. N. J., L. 292.
30. Dufoyer L.P. (1982). La naissance et le development de la personnality dans la premiere annee de la vie. 429.
429.
31. Louis G., Margolis E. The motherhood report: how women feel about being mothers. N. J. 1987. 482.
Psycho-emotional disorders during pregnancy. The need for their correction | Tyutyunnik V.L., Mikhailova O.I., Chukhareva N.A.
Currently, more and more attention is paid to the influence of a woman's psycho-emotional state on reproductive function, pregnancy and perinatal outcomes [2,4,14]. In recent years, in developed countries, there has been an increase in the frequency of various mental disorders in women of reproductive age, the proportion of patients taking psychotropic drugs has increased, including among women who are planning a pregnancy and pregnant women [3,6,9].
Almost all pregnant women are subject to sharp emotional swings, since the expectation of a child is associated with changes - both physical and emotional. Hormonal changes during pregnancy lead to the fact that the mood of a pregnant woman changes dramatically almost every hour.
A future mother can get rid of such emotional swings and feel calm during pregnancy by observing the rules of emotional health. Emotional balance and physical fitness are equally important for a pregnant woman, they equally help her prepare for motherhood. Due to the lack of maternal experience, a pregnant woman may experience sudden emotional outbursts. The first pregnancy is a new experience that is quite difficult to comprehend. Ignoring the fact that the emotions of a woman who is expecting a child is much more complex and sharper than usual, can lead to a number of problems, including in relations with her spouse. Acceptance of this fact is the basis of emotional health during pregnancy [1,5,11].
Also, if a woman is pregnant for the first time, she experiences many fears, which include fear of childbirth and untimely termination of pregnancy, concern about the health of the unborn child and her own health, fear of labor pains and inevitable pain, fear of partner / spouse disappointment due to changes occurring with body. Modern women have to worry about careers, financial problems, and many additional costs associated with the appearance and upbringing of a new family member.
Modern women have to worry about careers, financial problems, and many additional costs associated with the appearance and upbringing of a new family member.
All these fears can lead to many negative emotions, such as anxiety, depression, irritation, anxiety, stress, anger, feelings of loneliness, confusion. Most often, changes in the psycho-emotional background during pregnancy lead to the development of depressive and anxiety disorders. Until the end, the pathogenesis of these changes is unclear, several theories are discussed, it is believed that changes in the hormonal background during pregnancy, including a significant increase in estrogens, and especially progesterone, in the blood serum can exacerbate existing emotional disorders [5,7,15]. As a rule, minor manifestations in the form of irritability, tearfulness, resentment accompany manifestations of early toxicosis in the first trimester of pregnancy - nausea, vomiting, etc. [6,10]. After the disappearance of these symptoms, the neuropsychic state of pregnant women usually improves. At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
The state of psycho-emotional stress with the presence of anxiety of various levels is observed in 40% of women with a normal pregnancy [2,7,11]. Borderline neuropsychiatric disorders can be presented in the form of hypochondriacal and hysterical syndromes. However, there are other forms of gestational borderline neuropsychiatric disorders, their features are the invariable inclusion in the clinical picture of certain psychopathological phenomena directly related to pregnancy: various fears for the successful course of pregnancy, obsessive fears for the fate of the fetus, expectation of childbirth, conditioned reflex fears associated with unfavorable past pregnancies and childbirth [5,6,8]. A study of pregnant women who do not have signs of borderline neuropsychiatric disorders showed that character accentuation was established only in a quarter of women. The first trimester of pregnancy is usually characterized to some extent by the sharpening of existing character traits. Soft, vulnerable, insecure women become even more impressionable, sometimes excessively tearful, and anxious (those women who have had miscarriages in the past or this pregnancy are not going well, in this case, the fear of another abortion can become simply obsessive) ).
Borderline neuropsychiatric disorders can be presented in the form of hypochondriacal and hysterical syndromes. However, there are other forms of gestational borderline neuropsychiatric disorders, their features are the invariable inclusion in the clinical picture of certain psychopathological phenomena directly related to pregnancy: various fears for the successful course of pregnancy, obsessive fears for the fate of the fetus, expectation of childbirth, conditioned reflex fears associated with unfavorable past pregnancies and childbirth [5,6,8]. A study of pregnant women who do not have signs of borderline neuropsychiatric disorders showed that character accentuation was established only in a quarter of women. The first trimester of pregnancy is usually characterized to some extent by the sharpening of existing character traits. Soft, vulnerable, insecure women become even more impressionable, sometimes excessively tearful, and anxious (those women who have had miscarriages in the past or this pregnancy are not going well, in this case, the fear of another abortion can become simply obsessive) ). Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
Anxiety disorders may first appear during pregnancy, there may be a change in the course of already existing disorders. In one retrospective study in women with panic attacks, 20% of cases showed a decrease in symptoms during pregnancy, 54% remained unchanged, and 26% worsened the course of the disease [12]. The detection of depression in pregnant women is difficult. Many symptoms, such as emotional lability, increased fatigue, changes in appetite and cognitive decline, are often found in physiologically normal pregnancy. Under stress, the mother's adrenal hormones release catecholamines (stress hormones) into the blood, and during the experience of positive emotions (joy, calm, etc. ), the hypothalamic structures produce endorphins, which, penetrating the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
), the hypothalamic structures produce endorphins, which, penetrating the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
According to the literature [2,5,11,15], a significant effect of anxiety disorders on the course of pregnancy and perinatal outcomes has been noted: the frequency of placental insufficiency, fetal growth retardation, premature birth, the birth of children with low body weight, which subsequently affects negatively on long-term forecast for them.
Thus, emotional swings are dangerous not only for the woman herself, but also for her unborn child. When a pregnant woman experiences stress, her body produces more of the hormone cortisol, the main “stress hormone”. Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Stress during pregnancy is dangerous for a variety of reasons. Chronic stress experienced for several weeks can slow down the development of the cells of the body of the embryo, the growth of the fetus. This increases the risk of miscarriage or spontaneous abortion or premature birth. Elevated levels of stress hormones can damage the brain of an unborn baby and lead to parenting problems later on.
Psychological stress in the perinatal period brings with it a whole range of problems that require serious attention to the psychological sphere of a pregnant woman in order to avoid obstetric and other complications. However, diagnostic criteria for the transition of the stress syndrome from the link of adaptation to the link of pathogenesis of various diseases have not yet been found [2,4,15].
Emotional control is necessary to maintain normal emotional balance during pregnancy. A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
There are several basic rules that will help to cope with emotional imbalance:
• You must come to terms with the fact that physical and emotional changes are an inevitable part of the pregnancy period. You need to understand that this is a temporary stage that will last only a few months and end a maximum of 1-2 months after the birth of the child.
• Each trimester of pregnancy brings new changes, both in the body and in the emotional state. The main source of information about pregnancy is special literature and the experience of women who have recently given birth, who can share their feelings and experiences.
• A pregnant woman is responsible for the emergence of a new life. Taking care of yourself means taking care of your child. Proper nutrition, rest and self-indulgence are essential.
• A pregnant woman should be open to dialogue and not be afraid to discuss her problems with a gynecologist, partner or friends - anyone who can provide emotional support. You should not keep fears and worries in yourself - this will only aggravate internal tension.
You should not keep fears and worries in yourself - this will only aggravate internal tension.
• Changes associated with pregnancy can lead to low energy and, as a result, rapid fatigue. You need to slow down, re-prioritize your work, and give yourself a break.
• Emotional tension and negative emotions can be overcome by being distracted by pleasant activities or hobbies. When emotions overwhelm you, try to analyze what is bothering you, and then find an adequate solution.
• Engaging in certain physical activities designed specifically for expectant mothers will help improve both physical and emotional health.
• The main components of emotional health during pregnancy are rest and comfort.
However, unfortunately, during pregnancy, a woman cannot always cope with nervous tension, irritability, anxiety, excitement and other symptoms of stress on her own. Therefore, in some situations, she needs medical help.
The relative risk of using drugs during pregnancy makes it difficult to choose therapy, therefore, for the correction of psycho-emotional disorders that occur during pregnancy, herbal drugs that have practically no side effects can be considered as highly safe therapy.
The basis of anti-anxiety complex herbal remedies is valerian. It has been used in traditional medicine for many years for its hypnotic and sedative effects and remains a highly sought after remedy to this day. The mild hypnotic effect of valerian makes it possible to use it for the relief of shallow insomnia caused by anxiety. In addition, the vegetotropic effect of valerian is well known, its ability to have a uniform effect on both mental and somatic (vegetative) symptoms of anxiety. Valerian preparations also have anxiolytic and neuroprotective effects. The spectrum of side effects of valerian is very narrow and practically limited only to allergic reactions. Although valerian extract is metabolized by the cytochrome P450 system, it has virtually no effect on the metabolism of other drugs, and thus unwanted drug interactions are excluded.
Among the phytopreparations used by clinicians for the treatment of psycho-emotional disorders, Persen, a modern combined sedative preparation of plant origin, is widely used to relieve stress symptoms (anxiety, irritability and emotional stress) without causing drowsiness. Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
The advantages of Persen over other sedatives are:
• the preparation contains only natural ingredients;
• the effectiveness and safety of herbal ingredients Persena are well studied;
• does not contain alcohol and bromine;
• can be combined with any psychotropic drugs, including antidepressants;
• effective as a fast-acting symptomatic remedy when it is necessary to stop the symptoms of anxiety, agitation, and during a course of treatment for stress conditions, anxiety and phobic disorders.
Due to the natural components of plant origin that are part of Persen, this drug can be used during pregnancy. In each case, the doctor must evaluate the benefits and risks of taking Persen and other drugs, depending on the severity of the symptoms of the disease.
Thus, to prevent possible development, as well as to treat psycho-emotional disorders in pregnant women, it is advisable to use sedatives, the effect of which softens the damaging effects of psychogenic factors.
Literature
1. Abramchenko V.V., Kovalenko N.P. Perinatal psychology: Theory, methodology, experience. Petrozavodsk, 2004. 350s.
2. Avedisova A.S. Anxiety disorders // Alexandrovsky Yu.A. "Mental disorders in general medical practice and their treatment". M: GEOTAR-MED. 2004, pp. 66–73.
3. Voznesenskaya T.G., Fedotova A.V., Fokina N.M. Persen-forte in the treatment of anxiety disorders in patients with psychovegetative syndrome // Treatment of nervous diseases. 2002. No. 3 (8). pp. 38–41.
No. 3 (8). pp. 38–41.
4. Vorobieva O.V. Psychovegetative syndrome associated with anxiety (issues of diagnosis and therapy) // Russian Medical Journal. 2006. V.14. No. 23. S. 1696–1699.
5. Grandilevskaya I.V. Psychological features of women's response to the identified pathology of pregnancy: Abstract of the thesis. dis. ... cand. psychol. Sciences. SPb., 2004.
6. Kasyanova O.A. Socio-psychological factors in preparing women for pregnancy, childbirth and motherhood: Abstract of the thesis. dis. ... cand. psychol. Sciences. Yaroslavl, 2005.
7. Kovalenko N.P. Psychoprophylaxis and psychocorrection of women during pregnancy and childbirth: Abstract of the thesis. dis. … doc. psychol. Sciences. SPb., 2001.
8. Filippova G.G. Psychological readiness for motherhood // Reader on perinatal psychology: Psychology of pregnancy, childbirth and the postpartum period. M., Izd-vo URAO, 2005. 328 p.
9 Davidson J.R.T. Pharmacotherapy of generalized anxiety // J.