How to treat chest cold in child
Acute Bronchitis in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is acute bronchitis in children?
Bronchitis is an inflammation of the large breathing tubes (bronchi) in the lungs. The illness can be short-term (acute) or long-term (chronic). Acute bronchitis means that the symptoms often develop quickly and don’t last long. Most cases are mild.
What causes acute bronchitis in a child?
Acute bronchitis is most often caused by a viral infection. It may also be caused by bacteria or things such as dust, allergens, strong fumes, or tobacco smoke.
In children, the most common cause of acute bronchitis is a virus. The illness may develop after a cold or other viral infection in the nose, mouth, or throat (upper respiratory tract). Such illnesses can spread easily from direct contact with a person who is sick.
Which children are at risk for acute bronchitis?
Children who have a higher chance of developing acute bronchitis are those who have:
- Chronic sinusitis
- Allergies
- Asthma
- Enlarged tonsils and adenoids
- Exposure to secondhand smoke
What are the symptoms of acute bronchitis in a child?
These are the most common symptoms:
- Dry or mucus-filled cough
- Vomiting or gagging
- Runny nose, often before a cough starts
- Chest congestion or pain
- An overall body discomfort or not feeling well
- Chills
- Slight fever
- Back and muscle pain
- Wheezing
- Sore throat
These symptoms often last 7 to 14 days. But the cough may continue for 3 to 4 weeks. These symptoms may look like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
These symptoms may look like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
How is acute bronchitis diagnosed in a child?
Your child’s healthcare provider can often diagnose acute bronchitis with a health history and physical exam. In some cases, your child may need tests to rule out other health problems, such as pneumonia or asthma. These tests may include:
- Chest X-rays. This test makes images of internal tissues, bones, and organs.
- Pulse oximetry. An oximeter is a small device that measures the amount of oxygen in the blood. For this test, the healthcare provider puts a small sensor (like a clip) on your child's finger or toe. When the device is on, a small red light can be seen in the sensor. The sensor is painless and the red light does not get hot.
- Sputum and nasal discharge samples.
 These tests can find the germ causing an infection.
These tests can find the germ causing an infection.
How is acute bronchitis treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
In nearly all cases, antibiotics should not be used to treat acute bronchitis. That’s because most of the infections are caused by viruses. Even children who have been coughing for longer than 8 to 10 days often don't need antibiotics.
The goal of treatment is to help ease symptoms. Treatment may include:
- Plenty of rest
- Acetaminophen or ibuprofen for fever and mild pain
- Cough medicine for children over 4 years old
- More fluids
- Cool-mist humidifier in your child’s room
Talk with your child’s healthcare provider before giving over-the-counter cough and cold medicine to your child. The American Academy of Pediatrics does not recommend giving these medicines to children younger than 4 years old because they may cause harmful side effects. For children between ages 4 and 6, only use over-the-counter products when recommended by your child's healthcare provider. In most cases, also don’t give antihistamines. They can dry up the secretions. That can make the cough worse.
The American Academy of Pediatrics does not recommend giving these medicines to children younger than 4 years old because they may cause harmful side effects. For children between ages 4 and 6, only use over-the-counter products when recommended by your child's healthcare provider. In most cases, also don’t give antihistamines. They can dry up the secretions. That can make the cough worse.
Don’t give aspirin or medicine that contains aspirin to a child younger than age 19 unless directed by your child’s provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver.
.
What are possible complications of acute bronchitis in a child?
Most children who have acute bronchitis will get better without any problems. But the illness can lead to pneumonia.
How can I help prevent acute bronchitis in my child?
You can help prevent acute bronchitis by stopping the spread of viruses that may lead to it. Take these steps:
Take these steps:
- Teach your child to cover their nose and mouth when coughing or sneezing.
- Make sure your child washes his or her hands often.
- Check that your child is up-to-date on all vaccines, including the yearly flu shot.
When should I call my child’s healthcare provider?
Call your child’s healthcare provider right away if your child’s symptoms get worse, if new symptoms develop, or if he or she has:
- Trouble breathing
- A high fever
Key points about acute bronchitis in children
- Bronchitis is an inflammation of the large breathing tubes (bronchi) in the lungs. Acute bronchitis means that the symptoms often develop quickly and don’t last long.
- In children, the most common cause of acute bronchitis is a virus.
- A cough, fever, runny nose, and body aches are common symptoms.

- Treatment is aimed at easing symptoms. It may include plenty of rest and fluids. Medicines for fever or cough may also help.
- Antibiotics are not needed, unless the cause is a bacterial infection.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.

- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
How to treat a chest cold in children and adults
GEHA will perform system maintenance this Tuesday, November 1, from 9 p.m. - 11 p.m. Central time. Portions of this website might not be available during this time. We apologize for any inconvenience.
You are using a browser we no longer support. Current functionality may be reduced and some features may not work properly. For a more optimal geha.com experience, please click here for a list of supported browsers.
- View All
- Health and Wellness
- News
GEHA | December 14, 2021
Health and wellness Everyday health Well-being
Antibiotics are not an effective treatment option.
The common cold, or upper respiratory infection, is one of the leading reasons for physician visits. Generally caused by viruses, doctors treat the symptoms instead of prescribing antibiotics.
When a common cold settles in the chest and becomes a chest cold, it is known as acute bronchitis. “Acute” means sudden onset. If you recently had a cold that turned into a nagging cough, you might have acute bronchitis. Symptoms usually last less than three weeks.
Symptoms of acute bronchitis include:
- Coughing with or without mucus
- Soreness in the chest
- Feeling tired (fatigue)
- Mild headache
- Mild body aches
- Sore throat
- Temperature of 100.4 °F or higher
Acute bronchitis usually gets better on its own. Antibiotics are not effective in children or adults. When antibiotics aren’t needed, they won’t help you and their side effects could cause harm.
Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use these medicines as directed. Be careful about giving over-the-counter medicines to children. Not all of these medicines are recommended for children of certain ages.
Always use these medicines as directed. Be careful about giving over-the-counter medicines to children. Not all of these medicines are recommended for children of certain ages.
Here is some information about over-the-counter medicines and children:
- Pain relievers:
- Children younger than six months: only give acetaminophen
- Children six months or older: OK to give acetaminophen or ibuprofen
- Never give aspirin to children because it can cause Reye’s syndrome, a rare but serious illness that harms the liver and brain
- Cough and cold medicines:
- Children younger than four years old: do not use unless a doctor specifically tells you to because of the danger of serious and potentially life-threatening side effects
- Children four years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe for temporary symptom relief
Here are some ways to feel better while recovering:
- Get plenty of rest
- Drink plenty of fluids
- Use a humidifier or cool mist vaporizer
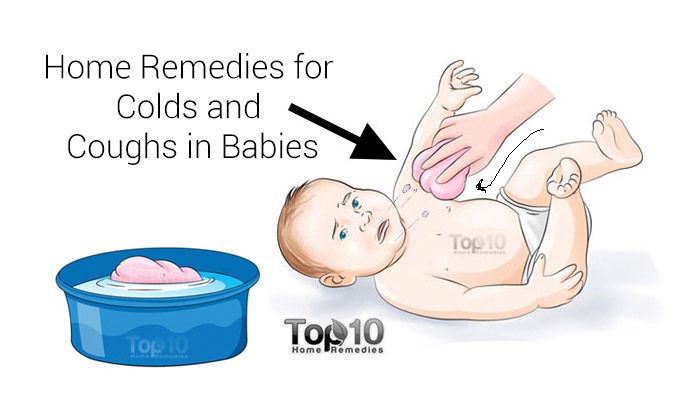
- Use saline nasal spray or drops to relieve a stuffy nose; for young children use a suction bulb to clear mucus
- Breathe in steam from a bowl of hot water or shower
- Suck on lozenges; do not give to children younger than four years old
- Use honey to relieve cough for adults and children at least one year of age or older
Sources:
“Chest Cold (Acute Bronchitis).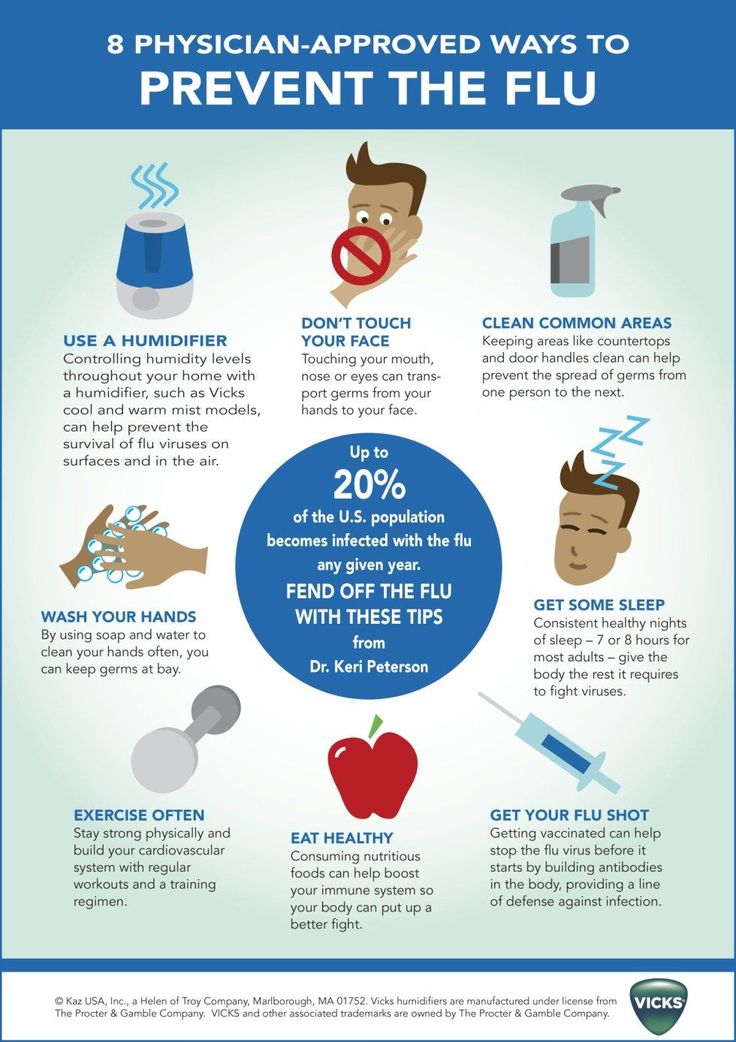 ” cdc.gov, Centers for Disease Control and Prevention, 1 July, 2021..
” cdc.gov, Centers for Disease Control and Prevention, 1 July, 2021..
“Bronchitis Diagnosis and Treatment: What to Know.” webmd.com / WebMD LLC, 7 December, 2020.
“Treatment of the Common Cold in Children and Adults.” aafp.org, Am Fam Physician, American Academy of Family Physicians, 15 July, 2012.
Proper treatment of the common cold in children
A common cold usually takes 7-10 days or more to develop, depending on the type of illness that provoked it. Serious illnesses, such as some types of acute respiratory viral infections (ARVI), as well as chronic rhinitis caused by specific infections (syphilis, tuberculosis, gonorrhea) are treated simultaneously with the underlying disease in specialized medical centers.
In this article we will talk about how to properly treat a simple infectious rhinitis in newborns, infants and older children. It is important that parents caring for sick children have some knowledge of how to properly care for a child with a cold and why this is important.
How to properly treat a runny nose in a child?
First aid
In all cases of a cold in a child, before starting any medical treatment (i.e. drug treatment), you should try to alleviate the child's condition with available means:
1. Raise the head of the bed on which the child is lying. To do this, a pillow can be placed under the shoulders of the child, so that the head and upper body of the child are located in relation to the body at an angle of 40–45? (make sure the child is comfortable in this position). This will make the phlegm that forms in your nose easier to pass and you may not need to use any medication.
2. If a newborn or infant has a very stuffy nose with phlegm, you can try to suck out the mucus from the nasal passages with a rubber bulb or a regular syringe. In general, sputum suction is used to help children who cannot blow their nose on their own. To suck out sputum, you can use a regular rubber bulb with a fairly thin tip or a regular syringe without a needle. The tip of a pear or syringe should be inserted into the nasal passage of a child with a runny nose carefully, so as not to injure the mucous membrane. Mucus is sucked out first from one, and then from the other nasal passage. This procedure can be repeated as often as needed.
The tip of a pear or syringe should be inserted into the nasal passage of a child with a runny nose carefully, so as not to injure the mucous membrane. Mucus is sucked out first from one, and then from the other nasal passage. This procedure can be repeated as often as needed.
Do not let the sputum dry out!
The easiest way is to put a saline solution into a child's nose: In the case of a cold in newborns or infants, as well as a cold in older children, it is important not to allow mucus to dry in the nasal passages - this can completely upset nasal breathing.
In order to prevent mucus from drying up in the nasal passages, wetting the nasal passages with saline solution is recommended. To do this, you can use ordinary saline, or you can just use a solution of ordinary table salt in water.
Saline solution instilled 3-4 drops into each nostril. It is desirable that at this time the child lies with his head thrown back. The first entry of fluid into the nose can be very unpleasant, causing coughing, sneezing, or even the urge to vomit.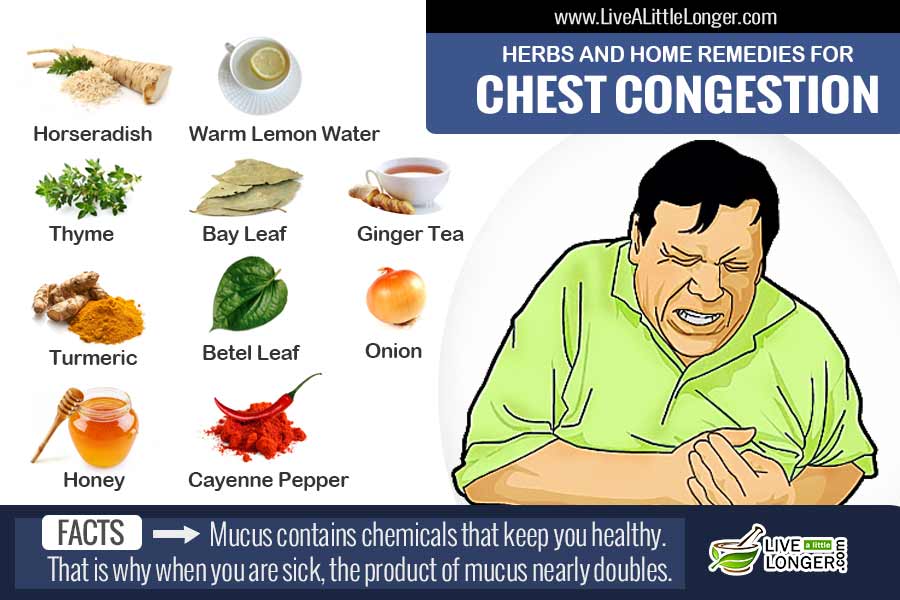 However, after several instillation procedures, such sensitivity of the nasal and pharyngeal mucosa disappears. The procedure can be repeated every 30-60 minutes. It is important to ensure that the mucus in the nose does not dry out. The saline solution helps thin the sputum and make it easier to excrete from the nose of a child with a runny nose.
However, after several instillation procedures, such sensitivity of the nasal and pharyngeal mucosa disappears. The procedure can be repeated every 30-60 minutes. It is important to ensure that the mucus in the nose does not dry out. The saline solution helps thin the sputum and make it easier to excrete from the nose of a child with a runny nose.
Instead of saline, some experts recommend using oily liquids, such as vitamin A or vitamin E oil, available from pharmacies. Such liquids not only prevent sputum from drying out, but also moisturize the nasal mucosa, relieve irritation, and have a regenerating effect.
Medications to relieve nasal breathing
In some sources, of course, you can read about the "danger" or "inappropriateness" of the use of decongestants (the so-called all types of drugs that, when instilled into the nose or when taken by mouth, facilitate nasal breathing) in treatment of acute rhinitis in newborns, infants and older children.
We must give credit to our colleagues for noting that such drugs can indeed cause some complications and that, if used incorrectly, they can aggravate the child's condition. We note right away that the complications of the common cold do not arise because of the drugs themselves, but because of their illiterate use. It is absolutely unacceptable to treat children with decongestants intended for adults and give the child medicine when it pleases.
Below we will review some of the drugs recommended for the treatment of the common cold in children, but first we note that failure to treat modern decongestants can cause complications such as sinusitis. The fact is that all nasal sinuses (two maxillary, two frontal, ethmoid and sphenoid) open with small openings into the nasal cavity. Microbes are expelled from the sinuses through these openings. With a runny nose, children develop severe swelling of the nasal mucosa, which leads to complete closure of the holes that communicate the nasal cavity with the cavities of the paranasal sinuses. As a result, microbes accumulate in the sinuses, which eventually cause sinusitis - inflammation of the sinuses.
As a result, microbes accumulate in the sinuses, which eventually cause sinusitis - inflammation of the sinuses.
How do nasal breathing medicines work?
There are two large groups of drugs that facilitate nasal breathing: local (topical) and systemic decongestants. Both those and other types of cold medicine act in the same way: they constrict the vessels of the nasal mucosa. Due to the narrowing of the vessels, the swelling of the nasal mucosa decreases and nasal breathing is partially or completely restored. It also opens the communication channels between the nasal cavity and the paranasal sinuses, thereby reducing the risk of developing sinusitis.
What medicines are used to treat the common cold in children?
First, let's draw the attention of parents to the specifics of drug production: the same drug is produced by different companies under different names. However, on the packaging of the drug or in the instructions for its use, the active substance is always indicated, which is the same in all drugs of this type. Therefore, when buying a medicine, pay attention not to the commercial name, but to the name of the active substance that is part of the medicine, as well as to the concentration of the active substance in the preparation. Below we present several such examples.
Therefore, when buying a medicine, pay attention not to the commercial name, but to the name of the active substance that is part of the medicine, as well as to the concentration of the active substance in the preparation. Below we present several such examples.
|
A cold in a child: how to treat it correctly
Shcherbakova Alla Anatolievna
Pediatrician, Gastroenterologist
Clinic "Mother and Child" Savelovskaya
Many parents are ready for the fact that babies will pick up common, including seasonal infections, which is typical for childhood. Some parents study the methods of treating SARS and colds in advance, read about it from experienced mothers in blogs and diaries, consult with doctors they know, and watch medical programs. But even despite the fact that the child's body has a powerful immune system from birth, this protection is imperfect. Therefore, no matter how informed the mother is, when the child becomes ill, she has a lot of questions that require qualified answers.
What are acute respiratory infections and SARS
Most often, children experience acute respiratory diseases, abbreviated as acute respiratory infections or colds. This is especially evident when visiting children's groups, where they come into contact with other kids and actually exchange various pathogens. The mothers of "kindergarten" children are very familiar with the phrase: "We go for 2 days, then 2 weeks - on sick leave."
A cold can be both viral and bacterial, even fungal and of a different nature, in 70-80% of cases it is of a viral nature. It is impossible to establish the origin of a cold with accuracy on a pediatric examination, as well as "by eye" to distinguish one infection from another. However, there are certain signs that indicate the action of viruses, harmful bacteria and other pathogens. For example, mucous nasal discharge testifies in favor of an acute respiratory viral infection, which usually begins with a slight malaise, loss of appetite, capriciousness, sleep disturbance in a child.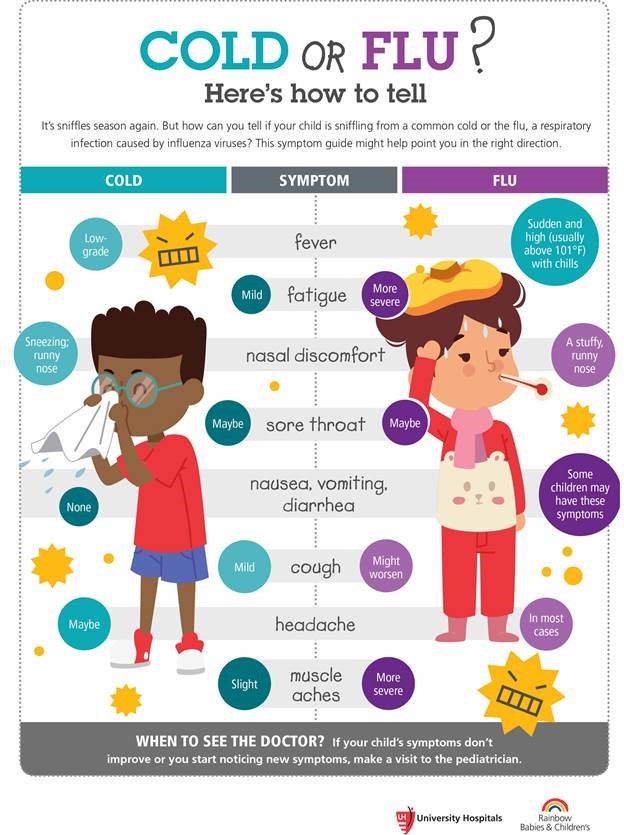 This is a prodromal period, it lasts from several hours to 1-2 days. And such a viral infection as the flu begins acutely, immediately with a very high temperature, intoxication, there is almost no prodromal period, dry cough appears in the late stages of the disease. Often ARVI goes away with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, cough, sore throat and swallowing.
This is a prodromal period, it lasts from several hours to 1-2 days. And such a viral infection as the flu begins acutely, immediately with a very high temperature, intoxication, there is almost no prodromal period, dry cough appears in the late stages of the disease. Often ARVI goes away with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, cough, sore throat and swallowing.
What to do?
First of all, you need to remember that parents should not panic if the child has a fever and other unpleasant symptoms of a cold. Any mood of the mother is transmitted to the baby. A cold with a competent approach is simply MUST go away in 5-7 days without complications. And it is important to know that the treatment of a cold is complex, which includes the main drugs - antiviral, antibacterial, etc., as well as symptomatic therapy. You should not rely on just one kind of medicine as a panacea, a magic pill from an advertisement or the advice of a pharmacy worker.
How to treat?
- Antivirals. Now there is a lot of false information regarding antiviral drugs. They are credited with mythical side effects and actions. If this comes from a doctor, then he must provide data confirming his point of view in official sources, which are state medical institutions, major scientific journals.
- Antibiotics. As for antibiotics, their use is currently limited by very clear indications, contraindications, age of the patient, etc. In addition, antibiotics, especially with uncontrolled, frequent use, contribute to the formation of new strains of harmful bacteria that are difficult to treat. Usually, against the background of antibiotic treatment, it is customary to prescribe biological products - live microbes that make up the human intestinal microflora. But there is an opinion that the antibiotic has a detrimental effect on these bacteria, and such therapy does not bring the desired result.
- Auxiliaries.
 In the treatment of colds of any origin, symptomatic therapy is used, the action of which is directed against the symptoms of the disease. They are called auxiliary, as they help to alleviate the course of a cold. They do not get rid of the cause of SARS, but the child's own antibodies work against viruses.
In the treatment of colds of any origin, symptomatic therapy is used, the action of which is directed against the symptoms of the disease. They are called auxiliary, as they help to alleviate the course of a cold. They do not get rid of the cause of SARS, but the child's own antibodies work against viruses. - How to treat a runny nose? In case of a runny nose, a nasal toilet with saline solutions is performed. The procedure is simple, but requires certain skills and caution. To do this, you should seat the child with his back to him, first clean his nose. For babies, this can be done with cotton buds (for children under six months old, only with ordinary cotton turundas), and at an older age, children can already blow their nose. After that, you need to raise your chin, holding the child’s face with your palm in a raised state. Using a pipette, drip a saline solution into both nasal passages, lower the child's head forward. Part of the medicine may spill out of the nose, but the result of such a procedure will still be achieved.
 If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But it is preferable with a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the underlying airways, the development of complications such as inflammation of the trachea, bronchi, and lungs.
If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But it is preferable with a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the underlying airways, the development of complications such as inflammation of the trachea, bronchi, and lungs.
If the runny nose is profuse, watery, painful, accompanied by nasal congestion, vasoconstrictor drugs (based on oxymetazoline, xylometazoline) are used in the form of drops at bedtime, before walking with a child. This helps the baby to have a good rest in a dream without waking up, and on a walk it is normal to breathe through the nose without taking cold air into the mouth. It should not be instilled into the nose of a child in a supine state, since there is a high probability of a change in pressure during such manipulation and there is a risk of otitis media. All instillations must be done while sitting. The use of special preparations in the form of soft (spray with limited jet pressure) should be carried out with great care, since there is also a risk of promoting the spread of infection under pressure.
All instillations must be done while sitting. The use of special preparations in the form of soft (spray with limited jet pressure) should be carried out with great care, since there is also a risk of promoting the spread of infection under pressure. - Antipyretics. Often there are questions about the use of antipyretics, for children - these are drugs based on paracetamol or ibuprofen, for babies - in syrup, suppositories. It should be noted that if there are no special recommendations in this regard, it is necessary to reduce the temperature above 38.3-38.5°C. If the child feels well, plays, has an appetite, and, in general, tolerates temperature well, antipyretic drugs can not be used. If parents see that the child's condition is bad, he refuses to eat and drink, becomes lethargic, vomiting occurs, headache, the temperature rises further, you can start giving antipyretics even at a low temperature.
- How to treat a cough? Questions about cough are the most frequent and sometimes the most difficult at a pediatric appointment for SARS.
 It is best if the doctor dynamically observes the coughing child. In this case, the specialist can distinguish changes in the tone of the voice, a barking component, a dry or wet cough, wheezing, localization of wheezing. If the pediatrician recommends taking an x-ray, you should not refuse such an examination, this will help to make the correct diagnosis and prescribe adequate treatment. Currently, in the treatment of cough, inhalation drugs are widely used - through a special device - an inhaler. This tactic reduces the systemic effect of the drug on the child's body, where the drug reaches the point of its application - large and medium bronchi, and even alveoli. Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and frequency of use.
It is best if the doctor dynamically observes the coughing child. In this case, the specialist can distinguish changes in the tone of the voice, a barking component, a dry or wet cough, wheezing, localization of wheezing. If the pediatrician recommends taking an x-ray, you should not refuse such an examination, this will help to make the correct diagnosis and prescribe adequate treatment. Currently, in the treatment of cough, inhalation drugs are widely used - through a special device - an inhaler. This tactic reduces the systemic effect of the drug on the child's body, where the drug reaches the point of its application - large and medium bronchi, and even alveoli. Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and frequency of use.
Activities before the doctor arrives
Sometimes, especially during the season of high incidence of influenza and colds, there are difficulties with a doctor's visit, you have to wait for an appointment, the doctor does not have time to come as quickly as parents would like. There are measures that can be taken before the arrival of a specialist. It is necessary to measure the temperature of the child and write down the data on the thermometry carried out in a diary, which is then shown to the doctor. If the temperature is high, do not wrap or even dress the child warmly. At home, you can generally strip to your underwear. Disposable diapers are also recommended to be removed from infants. Do not forget about physical methods of cooling - you can wipe it with cool water, you can put a cloth moistened with water on your head, stomach, places of the main vessels. A sick child should be given plenty of fractional water, even if he refuses to drink, it is necessary to constantly offer from a teaspoon, moisten his lips.
There are measures that can be taken before the arrival of a specialist. It is necessary to measure the temperature of the child and write down the data on the thermometry carried out in a diary, which is then shown to the doctor. If the temperature is high, do not wrap or even dress the child warmly. At home, you can generally strip to your underwear. Disposable diapers are also recommended to be removed from infants. Do not forget about physical methods of cooling - you can wipe it with cool water, you can put a cloth moistened with water on your head, stomach, places of the main vessels. A sick child should be given plenty of fractional water, even if he refuses to drink, it is necessary to constantly offer from a teaspoon, moisten his lips.
There are no children who do not get sick. Everyone gets sick, only some often, and others not so much. The main thing to remember is that any medicines should be prescribed by a doctor at a full-time appointment, after an examination.

 025%
025%  1%
1%  05%
05%