Feeling nauseous after eating pregnant
Nausea After Eating - Early Pregnancy
You’re pregnant. Congratulations!
However, nausea and other early pregnancy symptoms might start to put a dampener on your excitement in the first trimester.
Nausea after eating is a common complaint in early pregnancy.
Read on to find out what causes it and how to cope with this annoying pregnancy symptom.
Having nausea after eating in early pregnancy
During pregnancy, rising hormone levels cause changes to your digestive system and body. This means the food you eat spends longer in your small intestine.
This could contribute to nausea after eating food, in a number of ways:
- Increased estrogen levels. This can cause short-term nausea, bloating and vomiting, or a combination of all three.
- Increased human chorionic gonadotropin (hCG) levels. This hormone, which the body begins to produce the following conception, to maintain the uterine lining, is thought to cause morning sickness
- Increased progesterone levels.
This can cause the sphincters in the lower esophagus to relax, causing nausea and heartburn.
These hormones can be the indirect causes of any changes such as nausea after eating in early pregnancy. A lack of vitamin B6 in the diet is thought to be another possible cause.
How soon did you feel sick when pregnant?
Some women don’t experience any nausea when pregnant. Nausea after eating food most commonly begins around week 6 of pregnancy, when hormone levels really start to ramp up.
Other women, though can feel nausea as early as 4 weeks pregnant (which is only 2 weeks after conception).
Some women throw up frequently, some only have pregnancy nausea, and in others, nausea is only triggered by certain odors or foods. Everyone experiences pregnancy nausea differently and your overall health might play a part in this.
Whether nausea is triggered by eating one particular food, or you just feel nauseous all the time, a home pregnancy test can confirm whether you’re pregnant or something else is going on – such as the dreaded stomach flu.
What helps ease nausea after eating in pregnancy?
To help with nausea after eating you might like to try any or all of the following tips:
- Ginger root has been shown to ease nausea and settle the stomach. Drink it steeped in hot water or add it to your food and cooking. Ginger ale used to be suggested for nausea conditions but it’s been found to be less effective than ginger root
- Lemon is another natural remedy for nausea. A few slices in hot water can soothe your upset stomach, especially between meals
- Sniff peppermint oil to help reduce the feeling of nausea. It might be helpful to keep some oil next to your bed, so you can sniff before getting up in the morning, to avoid upsetting your stomach
- Take your prenatal vitamins when your stomach has settled and after some food if possible
- Drink plenty of fluid every day, get some fresh air, and rinse your mouth after eating food to help with that queasiness. This can improve your mood and your physical health as well
- You could also try chewing some gum.
 As strange as it sounds, chewing gum is a way to alleviate nausea for some women.
As strange as it sounds, chewing gum is a way to alleviate nausea for some women.
Anything that can help you feel better is worth a try.
Uncomfortably full after eating
As well as nausea after eating during the first trimester, it’s also really common to feel bloated and full.
This is due to progesterone, which relaxes the smooth muscle in your digestive system. This means food moves through the digestive tract much more slowly.
This slowing down of the digestive tract allows more time for all the nutrients in foods to be absorbed in the intestine and reach your growing baby.
However, this can also make you feel bloated and nauseous. All the food you eat will travel more slowly through your body; adding more or larger meals causes food buildup in your intestine.
As the baby gets bigger, your organs and digestive tract get squashed, causing discomfort due to indigestion and heartburn. If you choose to eat less food, it can lead to malnutrition, which will affect your health and potentially your baby’s health and development.
One tip is to eat small meals, more often. This may help with your appetite. A light meal can be beneficial for your digestive tract, preventing the food buildup in your intestine that causes bloating and nausea after eating.
Nausea after eating in early pregnancy – boy or girl?
Levels of the pregnancy hormone hCG, which triggers morning sickness, tend to be higher in mothers who are pregnant with female babies.
But a pregnant woman can certainly have nausea after eating, and even bad morning sickness, when she’s carrying a boy.
Some old wives’ tales suggest the foods that trigger nausea are a clue to whether you’re having a boy or a girl. But there’s little evidence to support this.
Please read this wonderful article on Boy or Girl – What Am I Having? 16 Old Wives Tales for more information.
What if nausea doesn’t stop in pregnancy?
A condition called hyperemesis gravidarum occurs in up to 2% of pregnancies.
It involves symptoms of severe and persistent vomiting and is a condition that compromises your health and that of your baby.
If you can’t keep foods or fluid down and have persistent nausea after eating, fatigue, and weight loss, these are signs you may have hyperemesis.
If you have any of these signs or symptoms, contact your health care provider or doctor for further advice. You might need hospitalization to treat dehydration.
Read When Is Morning Sickness Classed As Hyperemesis Gravidarum? for more information.
Is feeling nauseous after eating a sign of pregnancy?
Nausea after eating a meal is a common early sign of pregnancy. But nausea isn’t always the first (or only) symptom women experience in the first trimester.
Some women feel bloated after eating food, and have feelings of fatigue, queasiness, and moodiness; others might just notice tenderness in their breasts.
Are You Getting BellyBelly’s Pregnancy Week By Week Emails?
We think they’re the best on the internet!
Click to get the FREE weekly updates our fans are RAVING about.
These are, of course, due to hormones. You might experience one, some, or even all of these when pregnant.
You’ll find information about other signs of pregnancy in Pregnancy Symptoms | 16 Signs Of Pregnancy.
Medication for nausea in pregnancy
When symptoms of nausea after eating persist, despite making changes to your diet or trying natural remedies, your doctor might recommend medication.
Here is a list of medications used to treat nausea and vomiting in pregnancy:
Pyridoxine
Pyridoxine (vitamin B6) is considered first-line therapy for nausea and can be taken in conjunction with other medications called antiemetics (anti-vomiting and nausea medications).
Doxylamine with pyridoxine
A sustained-release tablet, combining doxylamine (10 mg) and pyridoxine (10 mg) has been available for many years in Canada to treat nausea in pregnancy.
A similar product, Debendox, was voluntarily withdrawn in Australia in 1983, after claims it caused birth defects.
Subsequent research has shown that this assertion was unfounded. Even so, for 30 years Australian women have been denied this safe and effective treatment.
The two medicines can be purchased separately, over the counter, in Australia.
Metoclopramide
Metoclopramide is classified as a pregnancy category A medication and is the most commonly prescribed antiemetic in pregnancy.
This classification might appear reassuring, in terms of safety, but it doesn’t give any indication of the drug’s efficacy.
Many pregnant women report metoclopramide didn’t ease their nausea but didn’t make it worse.
OndansetronAlthough there is limited safety data for ondansetron in pregnancy, it’s often prescribed for women with hyperemesis gravidarum.
It’s not recommended as first-line therapy, especially in the first trimester of pregnancy.
Ondansetron commonly causes constipation and bloating, which might already be a problem in pregnancy. To reduce this side effect, it’s recommended to use laxatives and limit the use of ondansetron
To reduce this side effect, it’s recommended to use laxatives and limit the use of ondansetron
Mirtazapine
Mirtazapine is an antidepressant and an alternative when other antiemetics fail to treat hyperemesis. It should only be used under your doctor’s supervision.
Corticosteroids
Corticosteroid use should be limited to pregnant women with nausea and vomiting that are difficult to control.
Women should have a regular medical follow-up to ensure steroids aren’t taken for lengthy periods.
Corticosteroids are best avoided in the first 10 weeks of pregnancy due to a possible association with cleft lip and palate.
Other treatments
Acid reflux, heartburn, and bloating can all make nausea worse when you’re pregnant.
You can use calcium-based antacids safely. Other treatments include proton-pump inhibitors and h3 blockers, both of which reduce the amount of acid produced in the stomach.
Women who suffer from prolonged vomiting could be at risk of thiamine or vitamin B1 deficiency. Thiamine supplementation may be recommended by your care provider.
Thiamine supplementation may be recommended by your care provider.
Speak with your doctor or midwife for advice and information on what is right for you.
Alternative therapies for nausea in pregnancy
Alternative therapies are those that aren’t part of the standard medical treatments usually prescribed by medical doctors.
Some women turn to complementary therapies during pregnancy to help reduce symptoms such as nausea and bloating. These treatments usually include acupuncture or acupressure.
Acupuncture is an ancient therapy that involves inserting thin needles into certain points of the body to ease certain conditions and their symptoms. For nausea, treating acupuncture point PC6 on the inner forearm safely and effectively reduces nausea in pregnancy.
Always check your acupuncture therapist is qualified and experienced in the treatment of pregnant women.
Acupressure, or reflexology, works on the same principles to relieve symptoms, except instead of inserting needles, you apply pressure to points. You or your partner can do this at home.
You or your partner can do this at home.
Always check with your doctor before commencing any new therapies.
How long does morning sickness in pregnancy last?
Morning sickness typically starts about week 6 and finishes around the end of the first trimester, with a peak between weeks 8 and 10.
Although those weeks can seem brutally long, there is a strange comfort in knowing your hormones are doing their work and your baby is growing.
Unfortunately for some women, nausea, discomfort and even vomiting happen on and off throughout the entire pregnancy.
A queasy, crampy stomach is no fun at the best of times.
Some great remedies can be found in Morning Sickness – 10 Best Morning Sickness Remedies.
Why do smells cause nausea in pregnancy?
It’s a scientific fact that high levels of estrogen increase your sensitivity to smell.
When you’re pregnant, you produce much higher levels of estrogen. This sensitivity can affect your stomach, meaning every smell in the world is going to bother you for nine months.
Let’s face it! Some odors are worse than others, so avoid those that trigger your nausea during pregnancy.
Coping With Common Discomforts of Pregnancy
Pregnancy produces many physical changes. Aside from weight and body shape, other alterations in your body chemistry and function take place. The heart works harder, your temperature registers slightly higher, body secretions increase, joints and ligaments are more flexible and hormones are altered.
Mood changes are common, resulting from a combination of hormonal changes and greater fatigue, as well as normal anxiety over body image, sexuality, finances, marriage roles and impending parenthood.
The following is a list of the most common discomforts of pregnancy and some guidelines for coping with them.
Nausea and Vomiting
- Eat small frequent meals. Going too long without eating during pregnancy can cause nausea or make it worse. If you experience continuous nausea, eat every one to two hours.

- Avoid greasy, high-fat foods. They are more difficult to digest.
- Consume dry starch foods, such as crackers, toast or cereal, in the morning before you get out of bed. Also, it helps if you stay in bed for 20 minutes or so after eating and get up slowly from the bed for a sudden change of position can aggravate nausea.
- Drinking carbonated beverages as well as peppermint, spearmint and chamomile teas may help.
- Eat plenty of carbohydrate-rich foods such as cereal, fruit, bread and rice. They are easy to digest and provide energy.
- Take prenatal vitamins only as directed. If they cause stomach upset, ask your practitioner if you can delay taking them for a few weeks.
- Some foods, such as milk or tea, that are soothing to one woman may be upsetting to another. However, most women find cold foods and beverages easier to tolerate than hot ones.
- Eat a high-protein snack before bed to stabilize blood sugar.
- Limit your consumption of coffee.
 It stimulates acid secretion, which can make the nausea worse.
It stimulates acid secretion, which can make the nausea worse. - Consume liquids separately from meals, waiting about 20 to 30 minutes.
- Wear sea sickness wrist bands. These can be found at most pharmacies.
- Increase the amount of fiber in your diet, eating foods high in fiber such as fruits, raw vegetables, whole grain products, nuts and dried fruits. Choose a breakfast cereal that has at least 5 grams of fiber per serving. These foods help soften the stool and promote natural bowel activity.
- Drink a lot of fluids.
- Exercise, even walking, will help relieve constipation.
- Eat prunes or figs, or drink prune juice. These fruits contain a natural laxative.
- Avoid laxatives. If the problem is not resolved with the above suggestions, let your health care practitioner know. Stool softeners that are safe during pregnancy can be prescribed.
- Iron supplements can aggravate constipation — the prescription for iron can be adjusted if it becomes a problem.
Continue reading
- To help avoid hemorrhoids, prevent constipation by maintaining a diet that is high in fluids and fiber.
- Witch hazel or Tucks pads can be applied to the hemorrhoid area to relieve symptoms.
- Avoid over-the-counter laxatives. If hard stools are aggravating hemorrhoids, stool softeners can be used, but first consult your practitioner for specific suggestions.
Fatigue
This is very common during the first trimester. Get as much sleep or rest as you can — even short naps will help. Your energy level will pick up after the first three months. However, fatigue and insomnia tend to recur in the last months of pregnancy. A warm bath, massage or hot drink before bed often helps you relax and get ready to sleep.
Breast Tenderness
Breast tenderness is most pronounced during the first three months. The breasts enlarge in size and can be quite tender. Wearing a good support bra may help you feel more comfortable.
Frequent Urination
Frequent urination is another pregnancy symptom that is most pronounced during the first trimester as well as the end of pregnancy. Do not restrict fluid intake in an effort to decrease the frequency of urination. As long as you do not experience burning or pain with urination, increased frequency is normal and will go away with time.
Leg Cramps
Cramps in your calf or thigh occur most frequently at night. One remedy may be to increase your intake of calcium. Ask your provider about a calcium supplement. While in bed, stretch with your heels pointed, not your toes. This will help relieve a cramp.
Heartburn
- Try eating smaller but more frequent meals.
- Avoid highly seasoned, rich and fatty foods.
- Do not lie down flat after eating. If you must lie down, elevate your head and shoulders with pillows.
- Carbonated beverages and milk often can help alleviate heartburn.
- Certain antacids are not recommended during pregnancy.
Check with your health care provider before using over-the-counter antacid preparations.
Backache
Lower back pain is common during pregnancy. It is caused by the shift in posture necessitated by carrying extra weight in front.
- Try not to stand in one position for too long.
- An exercise called the pelvic rock will help alleviate back pain and strengthen the lower back muscles that experience the most stress.
- Elevating the feet onto a stool while sitting will help.
Dizziness
Dizziness or lightheadedness can be caused by low blood sugar or a sudden change of position. To help avoid this feeling:
- Move slowly when getting up from a sitting or lying position.
- Eat well and frequently. Women who are prone to low blood sugar should carry snacks at all times. Juices and fruit are particularly good choices.
Swelling of the Hands and Feet
Slight swelling of the hands and feet are common in the later stages of pregnancy. Adequate fluid intake is always important. Improve the circulation in your legs and feet by elevating them as often as possible. Lie on a bed or floor and raise your legs up on the wall keeping your knees bent. If you are wearing elastic hose, drain your legs this way before putting them on.
Adequate fluid intake is always important. Improve the circulation in your legs and feet by elevating them as often as possible. Lie on a bed or floor and raise your legs up on the wall keeping your knees bent. If you are wearing elastic hose, drain your legs this way before putting them on.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Recommended reading
Anemia and Pregnancy
During the last half of pregnancy, your body makes more red blood cells which can cause Anemia. Learn more about causes and prevention here.
Domestic Violence and Pregnancy
Domestic violence is the most common health problem among women during pregnancy. It greatly threatens both the mother's and baby's health. Learn more here.
Eating Right Before and During Pregnancy
It is important to get the nutrients you need both before getting pregnant and during your pregnancy. Find more nutrition information including macros here.
Find more nutrition information including macros here.
Exercise During Pregnancy
Most women can, and should, engage in moderate exercise during pregnancy. Exercise can help you stay in shape and prepare your body for labor and delivery
FAQ: Prenatal Tests
Commonly asked questions regarding Prenatal Tests including, types available, positive screenings, diagnostic testing, health insurance coverage, and more.
HIV and Pregnancy
If you are pregnant, we recommend you be tested for the human immunodeficiency virus (HIV) even if you do not think you are at risk. Learn more here.
Recognizing Premature Labor
Premature labor occurs between the 20th and 37th week of pregnancy, when uterine contractions cause the cervix to open earlier than normal. Learn more.
Sex During Pregnancy
The pregnancy may alter how a woman and her partner feel about making love, and differences in sexual need may arise. Learn more here.
Substance Use During Pregnancy
While pregnant, it is best to eat well, stay healthy and avoid ingesting anything that might be harmful to the mother's or baby's health. Learn more.
Learn more.
The Circumcision Decision
If you give birth to a boy, you will be asked if you'd like him circumcised. This is a matter to be considered carefully before the baby is born. Learn more.
Related clinics
Center for Minimally Invasive Gynecologic Surgery
1500 Owens St., Suite 380
San Francisco, CA 94158
(415) 885-7788
M-F, 8 a.m. - 5 p.m.
Obstetrics & Gynecology at Mount Zion
2356 Sutter St.
San Francisco, CA 94143
(415) 885-7788
M-F, 8 a.m. - 5 p.m.
Obstetrics, Gynecology & Perinatal Specialties at Mission Bay – Fourth Street
Ron Conway Family Gateway Medical Building
1825 Fourth St., Third Floor
San Francisco, CA 94158
(415) 885-7788
M-F, 8 a.m. - 5 p.m.
Great Expectations Pregnancy Classes
Get ready for the baby! Choose from a variety of classes that prepare moms and partners for pregnancy, birth, baby care, breastfeeding and parenting.
Patient Resource
Lactation Consultant Support
Get support for all your breastfeeding needs. Troubleshoot with a lactation consultant, find equipment and supplies, join a support group and more.
Patient Resource
Women's Health Resource Center
Access free health resources here, from classes and webinars to support groups and medical referrals, plus pregnancy, birth and breastfeeding services.
Why do you feel sick during pregnancy in the early stages, at what time can pregnancy be determined. What helps with nausea
Every second woman feels sick during pregnancy. An unpleasant symptom appears even before a woman finds out that she is in a position. We tell you why the malaise begins, how many months it lasts and how you can cope with unpleasant symptoms.
What is toxicosis?
Morning (and sometimes afternoon and evening) ailments, along with sore breasts and the absence of menstruation, are considered the main signs by which a woman understands that she is pregnant. But from what day of pregnancy does she start to feel sick? The period at which toxicosis begins varies.
But from what day of pregnancy does she start to feel sick? The period at which toxicosis begins varies.
Nearly a third of women experience nausea approximately 4 weeks after the end of their last period. In the remaining 70%, toxicosis occurs at week 8. At the same time, in addition to nausea, half of the women also experience vomiting. In the vast majority of pregnant women, all unpleasant symptoms disappear by the 14th week.
However, in the third trimester, nausea may return. Most often, nausea during pregnancy occurs after eating for a long time.
This is due to the fact that the growing uterus and the child in it begin to squeeze the stomach, which causes a feeling of overeating and nausea. But it also happens that this is a sign of preeclampsia, which must be treated.
Most often, morning sickness and vomiting occur. Unpleasant odors, being in a stuffy room, motion sickness in transport, as a reaction to a certain type of food, and other factors can also provoke an attack. However, discomfort can occur unexpectedly or in cases where everything was normal before.
However, discomfort can occur unexpectedly or in cases where everything was normal before.
Among the risk factors that lead to the development of toxicosis are migraines, overweight, endocrine disorders, bronchial asthma, depression, eating disorders, underweight, multiple pregnancy. However, these factors do not mean that a pregnant woman will definitely have toxicosis.
Nausea is not only an unpleasant symptom that overshadows the joy of future motherhood. It can lead to serious consequences. Among them are weight loss, insomnia, fluid and electrolyte imbalance, multiple organ failure, and spontaneous abortion.
Important! Be sure to tell the gynecologist in charge of the pregnancy if any meal causes vomiting, you have begun to lose weight significantly
Causes of toxicosis
Almost every woman is faced with the question of what causes nausea during pregnancy? Several factors play a role in the etiology of toxicosis. What exactly provokes its development in a particular woman is impossible. Among the main reasons are the following:
What exactly provokes its development in a particular woman is impossible. Among the main reasons are the following:
| Factors | Description |
| Genetic factors | If the mother had severe nausea, then the daughter may experience the same symptoms. |
| immune factors | With nausea and vomiting, the body reacts to antigens that arise in response to foreign genes of the fetus. |
| Toxic factors | There is a hypothesis according to which normal excretory processes are disrupted during pregnancy, which causes poisoning. |
| Nervous Factors | In women with identified vegetovascular dystrophy and somatotrophic disorders, nausea develops due to dysfunction of the nervous system. |
| Psychological factors | Identified depression, neurosis, increased anxiety, eating disorders and other disorders lead to gastrointestinal dysfunction. |
| Hormonal factors | A relationship has been found between the level of the hormone hCG and estradiol and the symptoms of toxicosis. It is also confirmed by the fact that the symptoms of toxicosis decrease along with a decrease in the level of these hormones. |
However, it is important to distinguish the symptoms of toxicosis from other diseases. Nausea and vomiting can also be a sign of other illnesses, such as kidney failure or peptic ulcers. Therefore, with severe toxicosis, it is imperative to undergo examinations to exclude other pathologies.
Usually, a general and biochemical blood test, a blood test for infections, ultrasound of the abdominal cavity and urinary system, as well as fibrogastroduodenoscopy and consultations with specialized specialists are prescribed. Treatment and examinations are carried out with care so that it does not harm the child.
Treatment and examinations are carried out with care so that it does not harm the child.
Be sure to consult a gastroenterologist, endocrinologist and nephrologist if the symptoms of toxicosis persist after the 14th week of pregnancy so that this does not pose a danger to the baby. Our doctors will answer all your questions by phone at any time of the day.
What to do in order not to feel sick
You can prevent the development of nausea and toxicosis even during preparation for it. It is necessary to undergo examinations and treat all pathologies found. Particular attention should be paid to diseases that are a risk factor in the development of discomfort.
Another important point is adjusting the diet. In general, it is recommended to give up fried, fatty and spicy foods, as well as start eating often and in small portions. Food should be at room temperature. In addition, it is recommended to drink more.
Plain water and tea can be replaced with mineral water and herbal infusions of mint, lemon balm, chamomile, cranberry and ginger. However, you should not get carried away with herbs, as they may have an impact on the course of pregnancy.
If these methods do not help, the gynecologist may recommend taking antiemetics, vitamin preparations, isotonic solutions, and sedatives. Consultation with a psychologist is also recommended to exclude psychogenic factors.
In severe cases and with signs of exhaustion, the pregnant woman is placed in a hospital where more intensive therapy is carried out. If the woman's condition does not improve, termination of the pregnancy may be recommended as a last resort.
If toxicosis does not cause trouble, it is not treated in any way. They only offer to slightly adjust the diet and try folk methods of dealing with toxicosis. These include a few sips of mineral water, saltine crackers, or a lemon wedge right after waking up.
Case study:
The patient went to the gynecologist with complaints of severe nausea, persistent vomiting and weight loss. The gynecologist did not write off everything for pregnancy and conducted a full examination. FGDS with a biopsy revealed the presence of Helicobacter pylori and signs of gastritis in a woman. After treatment of the underlying disease, the symptoms of toxicosis also decreased.
FAQ
At what time can pregnancy be determined?
+
A blood test for chorionic gonadotropin can show pregnancy as early as 6–8 days after conception. However, it is more reliable to carry it out 3-5 days after the delay or on the 12th day after conception.
How many days after conception does it start to vomit?
+
Nausea can develop from 4 to 7 weeks after the last menstruation, that is, even before the delay appears. Symptoms of toxicosis usually disappear by 12-14 weeks. Also, unpleasant symptoms may return in the third trimester.
Also, unpleasant symptoms may return in the third trimester.
What to do if the chest stops hurting during pregnancy?
+
If the chest stops hurting at any stage of pregnancy, this may indicate hormonal disorders in the expectant mother. It can lead to problems with gestation, so any changes in well-being must be reported to the gynecologist.
After how many weeks can you find out about pregnancy?
+
The first signs of pregnancy appear at least 4 weeks after the end of the last menstruation, even before the delay. They will fail in the form of nausea, mood changes, tearfulness. In addition, in the early stages of pregnancy, the breast hurts and enlarges.
How to distinguish toxicosis from ordinary nausea?
+
By external signs, it is almost impossible to distinguish them from each other. But there is a slight difference. Toxicosis usually manifests itself in the morning, and nausea - at any time of the day, including in the evening. If nausea is not complicated by vomiting, but does not go away within a few days, it is recommended to do a home pregnancy test or donate blood for hCG.
Toxicosis usually manifests itself in the morning, and nausea - at any time of the day, including in the evening. If nausea is not complicated by vomiting, but does not go away within a few days, it is recommended to do a home pregnancy test or donate blood for hCG.
Expert opinion
Nausea in the later stages may indicate the development of preeclampsia. This complication affects all organs and leads to the development of severe multiple organ failure. In addition to nausea and vomiting, a pregnant woman is worried about swelling, severe headaches, rapid weight gain, high blood pressure and visual impairment.
Preeclampsia has the most serious consequences for both the mother and the unborn baby. Therefore, if late toxicosis is suspected, a woman is placed under the constant supervision of a doctor in the department of pregnancy pathology.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience. He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
- 1982 - 1986 NPO MONIIAG - obstetrician-gynecologist
- 1987 - 1989 VNITs OZMIR - obstetrician-gynecologist
- 1989 - 1992 departmental polyclinic st. Moscow - Kurskaya - obstetrician-gynecologist
- 1992 - 2001 NPO MONIIAG - obstetrician-gynecologist
- 2007 - 2008 NP KMIKM - doctor administrator
- 2009 - 2013 Pereslavl Central District Hospital, women's consultation - obstetrician-gynecologist
- 2020 to present Teledoctor24 LLC - doctor - consultant (gynecologist)
Early toxicosis of pregnant women - causes and treatment
- When early morning sickness starts during pregnancy
- Manifestation of early toxicosis
- Causes of toxicosis in the early stages
- Severity of toxicosis during pregnancy
- How to manage morning sickness and relieve symptoms
- Principles of treatment of early toxicosis
Most women, having barely learned about the onset of pregnancy, are waiting for poor health, nausea and even vomiting. Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms?
Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms?
Toxicosis (and doctors call this condition preeclampsia) is a syndrome that is defined as a violation of a woman's adaptation to pregnancy. According to the time of occurrence, early preeclampsia is distinguished, which will be discussed in this article, and late preeclampsia, which appears in the last 2-3 months of pregnancy and is manifested by edema, increased blood pressure and the appearance of protein in the urine.
When early morning sickness begins in pregnancy
Early morning sickness usually occurs in the first half of pregnancy. As a rule, after the end of the formation of the placenta, that is, at 12-13 weeks of pregnancy, the phenomena of toxicosis stop. During a normal pregnancy, adaptive changes in the function of almost all organs and systems occur in a woman's body, which are regulated by the nervous system with the participation of endocrine glands. Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus.
Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus.
Manifestation of early toxicosis
The most common manifestation of toxicosis is vomiting. Other forms of early toxicosis are very rare:
- pregnancy dermatosis is a group of skin diseases that occur during pregnancy and disappear after it. When it occurs in early pregnancy, dermatosis is caused by immune disorders in the body of a pregnant woman, and is also most often found in patients with diseases of the digestive and endocrine systems. The most common form of dermatoses of pregnancy is pruritus gravidarum, which can be on a small area of the skin or spread throughout the body, including the feet and palms.
- tetany (chorea) of pregnant women. This condition occurs when the function of the parathyroid glands decreases, as a result of which calcium metabolism in the body is disturbed.
 Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face.
Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face. - salivation - increased secretion of saliva, in connection with which there is a large loss of fluid (up to 1 liter per day). Salivation can be an independent manifestation of toxicosis or accompany vomiting of pregnant women. In the development of salivation, not only changes in the central nervous system are important, but also local disturbances in the salivary glands and their ducts under the influence of hormonal changes.
- bronchial asthma of pregnant women is an extremely rare form of preeclampsia.
- pregnancy osteomalacia - softening of the bones due to a violation of calcium and phosphorus metabolism, while the bones of the pelvis and spine are more often affected
- neuropathy and psychopathy of pregnancy.
Causes of toxicosis in the early stages
There are many theories trying to explain the causes and mechanisms of early toxicosis: the most recognized are the so-called neuro-reflex and immunological.
According to the neuro-reflex concept , vomiting occurs as a result of a violation of the relationship between the cerebral cortex and subcortical structures. During pregnancy, the subcortical centers of the brain begin to work more intensively than usual, which are responsible for most protective reflexes, including breathing and cardiac activity. In the same areas of the subcortical structures are the vomiting and salivary centers, the nuclei of the olfactory system of the brain. Excitation processes also capture them. Therefore, nausea and vomiting may be preceded by such phenomena as deepening of breathing, increased heart rate, an increase in the amount of saliva, pallor due to vasospasm, and a change in smell.
Immunological disorders play a certain role in the development of preeclampsia . The timing of the onset of vomiting usually coincides with the formation of blood circulation in the placenta, increased reproduction of white blood cells - lymphocytes, which are involved in immune reactions. The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
Human chorionic gonadotropin (hCG) plays a certain role in the development of vomiting in pregnant women. This hormone is produced by the placenta during pregnancy. Its high concentration can provoke vomiting.
The severity of toxicosis during pregnancy
The main symptom of early toxicosis of pregnant women is vomiting. Depending on the frequency of its occurrence, as well as the degree of metabolic disorders in the body of the expectant mother, doctors distinguish three degrees of severity of vomiting during pregnancy.
Managing and Relieving Symptoms of Toxicosis
Mild toxemia is usually treated at home. But, nevertheless, a pregnant woman should be under the supervision of doctors, take all the tests recommended by the doctor, and follow the appointments. This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown.
This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown.
Proper nutrition
You need to eat in small portions, fractionally, every 2-3 hours. Food should be easily digestible, high-calorie and fortified whenever possible. In connection with a decrease in appetite, they recommend varied and pleasant food for the expectant mother, that is, products are selected taking into account the desires of the pregnant woman, with the exception of spicy dishes and smoked meats. It is important to remember that very hot or very cold food often induces vomiting, so the dishes should be warm. Reception of alkaline mineral waters in small volumes 5-6 times a day is shown.
If nausea and vomiting occur in the morning, immediately after waking up, it is recommended to have breakfast while lying in bed without getting up. For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
Every woman chooses for herself a remedy that helps to fight nausea. Someone helps a slice of orange, lemon or apple, some expectant mothers carry crackers or mint sweets with them to alleviate the symptoms of toxicosis. Pumpkin juice has a good antiemetic effect. Many pregnant women benefit from ginger tea. It is prepared very simply:
ginger root finely chopped or grated on a coarse grater is poured with boiling water and infused for 15-20 minutes. Tea can be drunk warm or chilled, adding lemon, mint or honey to it.
Fats and proteins of animal origin are recommended to be consumed in the morning, when pancreatic enzymes are more active. Dairy products are best eaten after dinner or before bed.
Do not use food with preservatives, broiler meat, fast food, fast food.
To maintain metabolic processes in the body, it is advisable to drink 2-2.5 liters of fluid per day. With increased vomiting, it is not recommended to consume solid and liquid food at the same time. Liquids should not be drunk 30 minutes before and within 1.5 hours after eating, as this provokes vomiting by stretching the walls of the stomach and affecting the receptors.
Decoctions and infusions
Oat broth
As an enveloping agent, that is, a substance that forms a mucous film and prevents irritation of receptors on the walls of the stomach and intestines, oat broth is recommended. It is prepared as follows: 2-3 tbsp. spoons of oat grains are washed, pour 500-700 ml of water, boil over low heat under a lid for 30 minutes. The broth is drained, the grains are crushed and poured with new water and boiled until fully cooked. The resulting mass is crushed with a blender. You need to use the decoction on an empty stomach and in the evening before going to bed, but not earlier than 2 hours after dinner, and also throughout the day in small portions.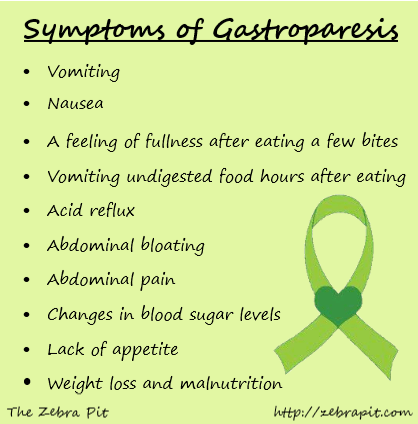
It has a particularly good effect in combination with rosehip infusion.
Rosehip tincture
This tincture is a good source of vitamins and microelements – it contains vitamins C, K, P and PP, potassium, manganese, iron, it contributes to the normalization of the gallbladder function. To prepare it, you need 1 tbsp. pour a spoonful of crushed rose hips with 250 ml of boiling water and insist in a thermos for about 2 hours.
The following infusions and decoctions contribute to reducing nausea and improving the condition of the expectant mother.
Herbal infusion
Take equally: valerian root, common anise fruits, fireweed leaves, linden flowers, marigold flowers, common blueberry shoots, blood red hawthorn fruits. 1 st. Pour 500 ml of boiling water over a spoonful of the mixture ground in a coffee grinder and insist in a thermos for 2 hours, then strain. Take the infusion as needed, up to 6 times a day in a heated form, 1/3 cup.
Benediktov's collection
To prepare this collection you will need: common yarrow (10 g), peppermint herb (20 g), shepherd's purse herb (20 g), valerian officinalis rhizomes (10 g), calendula officinalis inflorescences (20 g) and inflorescences of chamomile officinalis (20 g). Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks.
Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks.
Viburnum with honey
Grind 2 tbsp. tablespoons of fresh viburnum berries, pour 250 ml of boiling water over them, heat for 10 minutes in a water bath, strain, add a little honey. Take 1/3 cup of warm infusion before meals 3-4 times a day.
Cranberries with mint, honey and lemon
Squeeze the juice from 250 g of cranberries, cool it, boil the pulp in 1 liter of water, add 1 tbsp. a spoonful of mint leaves and leave for 15 minutes under the lid. Strain, dissolve in a hot broth 2-3 tbsp. tablespoons of honey, let cool to room temperature, add chilled cranberry juice and a slice of lemon. Drink 0.5 cup after meals or when nausea occurs.
Rose hips with apples
Crushed rose hips (about 1 tbsp) pour 250 ml of boiling water, add 0.5 tbsp. tablespoons of dried apples, heat in a water bath for 15-20 minutes. This drink can be consumed throughout the day instead of tea.
This drink can be consumed throughout the day instead of tea.
Rosehip with garden berries
To make a drink you will need: 1 tbsp. a spoonful of rose hips, 1 tbsp. spoon of raspberries, 1 tbsp. spoon of blackcurrant leaves, 1 tbsp. a spoonful of lingonberry leaves. 2 tbsp. spoons of the mixture pour 500 ml of boiling water, boil for 5 minutes, leave for 1 hour, strain. Take 100 ml of decoction 3 times a day.
Therapeutic exercise
Among non-drug remedies, exercise therapy has a good effect. The complex of exercises includes walking, deep breathing with stretching of the muscles of the trunk and limbs. It is necessary to exclude inclinations, they can increase nausea. The complex includes dynamic exercises for training the muscles of the arms, legs, relaxation exercises. Remedial gymnastics also includes training in breathing techniques. As a result, the body is saturated with oxygen, the excitability of the vomiting center decreases - toxicosis is relieved.
Physiotherapeutic procedures
Physiotherapeutic procedures for the treatment of early toxicosis include electrosleep, acupuncture, laser therapy . Electrosleep is a method that uses low frequency currents to induce sleep. The duration of the procedure is from 60 to 90 minutes, the course of treatment is 6-8 sessions.
Laser therapy
In the complex therapy of early toxicosis, blood is irradiated with a helium-neon laser through a light guide passed through a needle placed in the cubital vein. The procedure lasts 15-20 minutes. The therapeutic effect is achieved due to the influence of the laser on blood cells, changes in its properties, accumulation of biologically active substances in the blood. As a result, the metabolism in cells changes, the resistance of tissues and the body to adverse conditions increases, and the vitality increases.
Acupuncture, acupuncture
These are methods of treatment based on irritation of biologically active points and zones on the body and face. With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
With morning sickness and vomiting of pregnant women, the method of acupressure is effective. To do this, you need to press your finger on a point that is located on the inside of the wrist, in the middle, 3 transverse fingers above the palm.
Aromatherapy
The use of plant aromas has a positive effect on the expectant mother and baby. By inhaling pleasant aromas, you can achieve a good psychological effect, create a good mood, and reduce the effects of toxicosis. During pregnancy, aroma lamps, aroma medallions, pads - sachets are mainly used. To relieve nausea and vomiting, oils of noble laurel, lemon, lavender, cardamom present, dill, lemon balm, peppermint, anise, eucalyptus, ginger are suitable. To flavor the air, you can use the following mixture 0 3 drops of lavender oil, 1 drop of peppermint oil, 1 drop of eucalyptus oil.
Principles of treatment of early toxicosis
Even with a mild course of early toxicosis of pregnant women, the attending physician will definitely prescribe a number of tests - a general blood test, a general urinalysis, a biochemical blood test, a hemostasiogram. This is necessary to control the condition of a pregnant woman and to timely prescribe medications to correct the changes that occur in the body.
If non-drug remedies are ineffective, the doctor prescribes medications that help fight toxicosis. First of all, these are herbal sedatives, homeopathic medicines for nausea, vitamin B6 preparations, antiemetics.
If, despite all therapy, vomiting increases, the doctor detects changes in blood and urine tests, and body weight continues to progressively decrease, hospitalization is indicated.
The hospital provides intravenous infusion of medicines that restore fluid, trace elements and proteins lost by the body. A pregnant woman receives at least 2-2. 5 liters of fluid intravenously per day.
5 liters of fluid intravenously per day.
To improve blood flow through the placenta and improve oxygen supply to the fetus, oxygen therapy can be prescribed - inhalation of an oxygen-air mixture for 20-30 minutes twice a day.
Most often, the effects of toxicosis gradually decrease by 12-13 weeks of pregnancy.
Mild
Mild vomiting on an empty stomach or after meals occurs 3 to 5 times a day. Despite vomiting, part of the food is still retained and significant weight loss is not observed in such pregnant women. The general condition does not suffer significantly, there are no changes in blood and urine tests. Such vomiting is easily treatable with various non-drug means, and often resolves on its own after the normalization of the diet and rest.
Moderate vomiting
Moderate vomiting (or moderate vomiting) is expressed in the increase in vomiting up to 10 times a day, regardless of food intake. Characterized by persistent nausea. There comes dehydration of the body, a decrease in body weight by 3-5 kg (6% of the initial weight).