Preeclampsia in first trimester
Pre-eclampsia - Symptoms - NHS
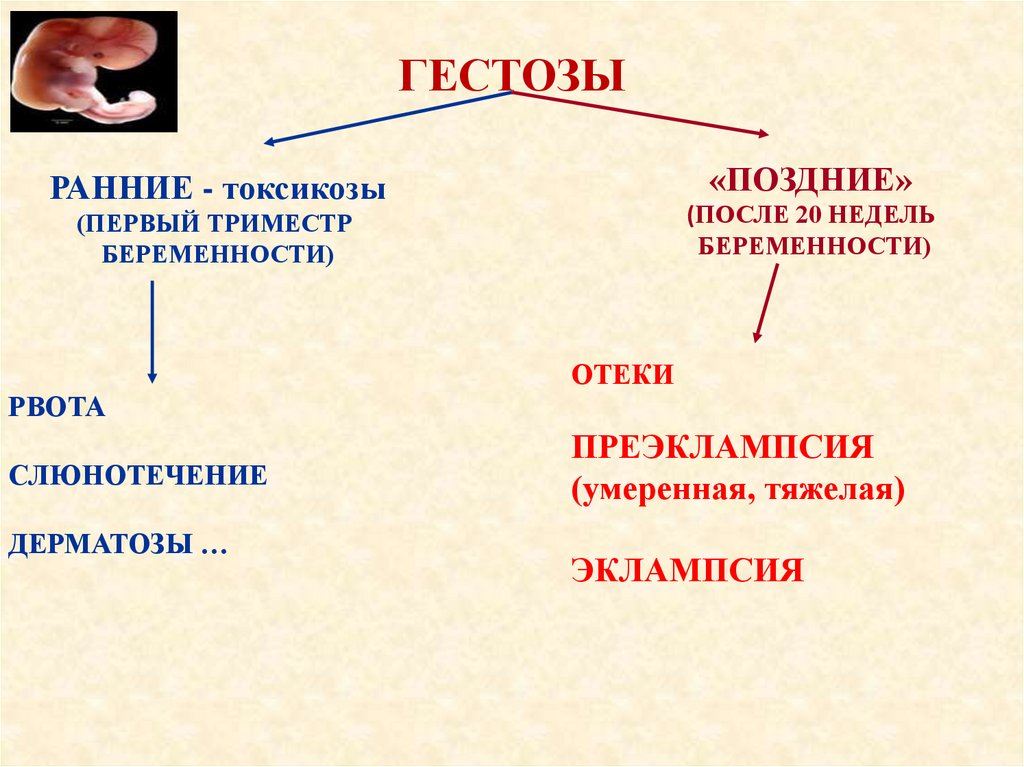
Pre-eclampsia rarely happens before the 20th week of pregnancy.
Although less common, the condition can also develop for the first time in the first 4 weeks after birth.
Most people only experience mild symptoms, but it's important to manage the condition in case severe symptoms or complications develop.
Generally, the earlier pre-eclampsia develops, the more severe the condition will be.
Early signs and symptoms
Initially, pre-eclampsia causes:
- high blood pressure (hypertension)
- protein in urine (proteinuria)
You probably won't notice any symptoms of either of these, but your GP or midwife should pick them up during your routine antenatal appointments.
High blood pressure alone doesn't suggest pre-eclampsia.
But if protein in the urine is found at the same time as high blood pressure, it's a good indicator of the condition.
Read more about diagnosing pre-eclampsia.
Further symptoms
As pre-eclampsia progresses, it may cause:
- severe headaches
- vision problems, such as blurring or seeing flashing lights
- pain just below the ribs
- vomiting
- sudden swelling of the feet, ankles, face and hands
If you notice any symptoms of pre-eclampsia, get medical advice immediately by calling your GP surgery or NHS 111.
Without immediate treatment, pre-eclampsia may lead to a number of serious complications, including:
- convulsions (eclampsia)
- HELLP syndrome (a combined liver and blood clotting disorder)
- stroke
But these complications are rare.
Read more about the complications of pre-eclampsia.
Signs in the unborn baby
The main sign of pre-eclampsia in the unborn baby is slow growth. This is caused by poor blood supply through the placenta to the baby.
The growing baby receives less oxygen and fewer nutrients than it should, which can affect development. This is called intra-uterine or foetal growth restriction.
If your baby is growing more slowly than usual, this will normally be picked up during your antenatal appointments, when the midwife or doctor measures you.
Page last reviewed: 28 September 2021
Next review due: 28 September 2024
Preeclampsia - Symptoms and causes
Overview
Preeclampsia is a complication of pregnancy. With preeclampsia, you might have high blood pressure, high levels of protein in urine that indicate kidney damage (proteinuria), or other signs of organ damage. Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had previously been in the standard range.
Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had previously been in the standard range.
Left untreated, preeclampsia can lead to serious — even fatal — complications for both the mother and baby.
Early delivery of the baby is often recommended. The timing of delivery depends on how severe the preeclampsia is and how many weeks pregnant you are. Before delivery, preeclampsia treatment includes careful monitoring and medications to lower blood pressure and manage complications.
Preeclampsia may develop after delivery of a baby, a condition known as postpartum preeclampsia.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
Symptoms
The defining feature of preeclampsia is high blood pressure, proteinuria, or other signs of damage to the kidneys or other organs. You may have no noticeable symptoms. The first signs of preeclampsia are often detected during routine prenatal visits with a health care provider.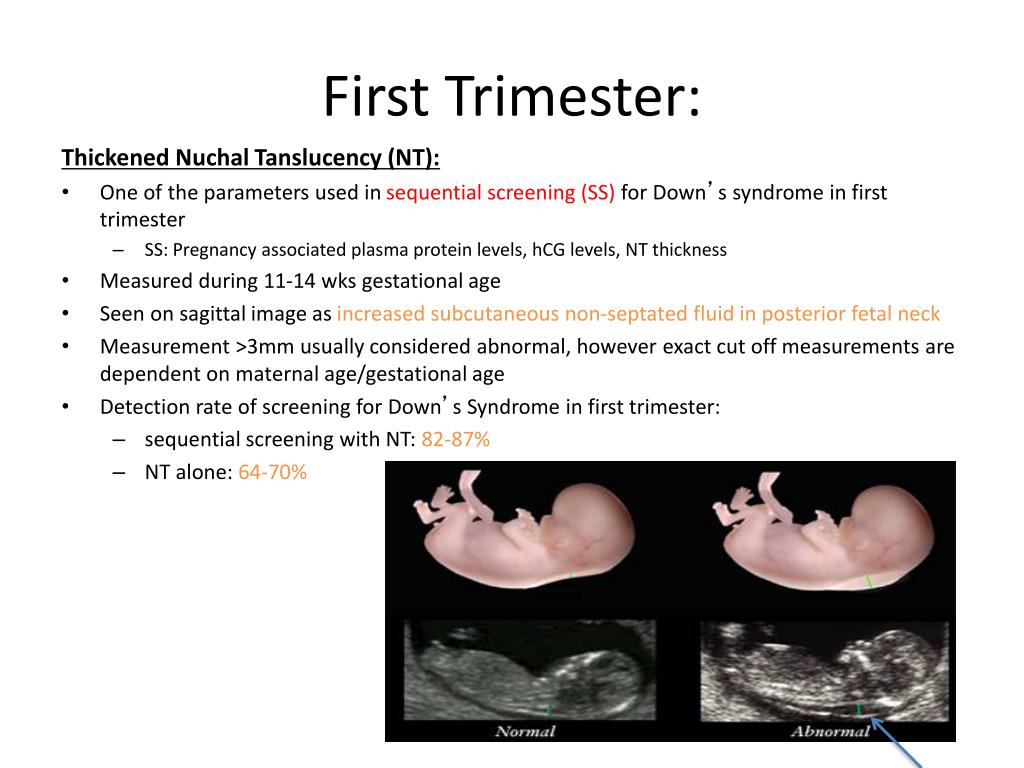
Along with high blood pressure, preeclampsia signs and symptoms may include:
- Excess protein in urine (proteinuria) or other signs of kidney problems
- Decreased levels of platelets in blood (thrombocytopenia)
- Increased liver enzymes that indicate liver problems
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
- Shortness of breath, caused by fluid in the lungs
- Pain in the upper belly, usually under the ribs on the right side
- Nausea or vomiting
Weight gain and swelling (edema) are typical during healthy pregnancies. However, sudden weight gain or a sudden appearance of edema — particularly in your face and hands — may be a sign of preeclampsia.
When to see a doctor
Make sure you attend your prenatal visits so that your health care provider can monitor your blood pressure. Contact your provider immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbances, severe belly pain, or severe shortness of breath.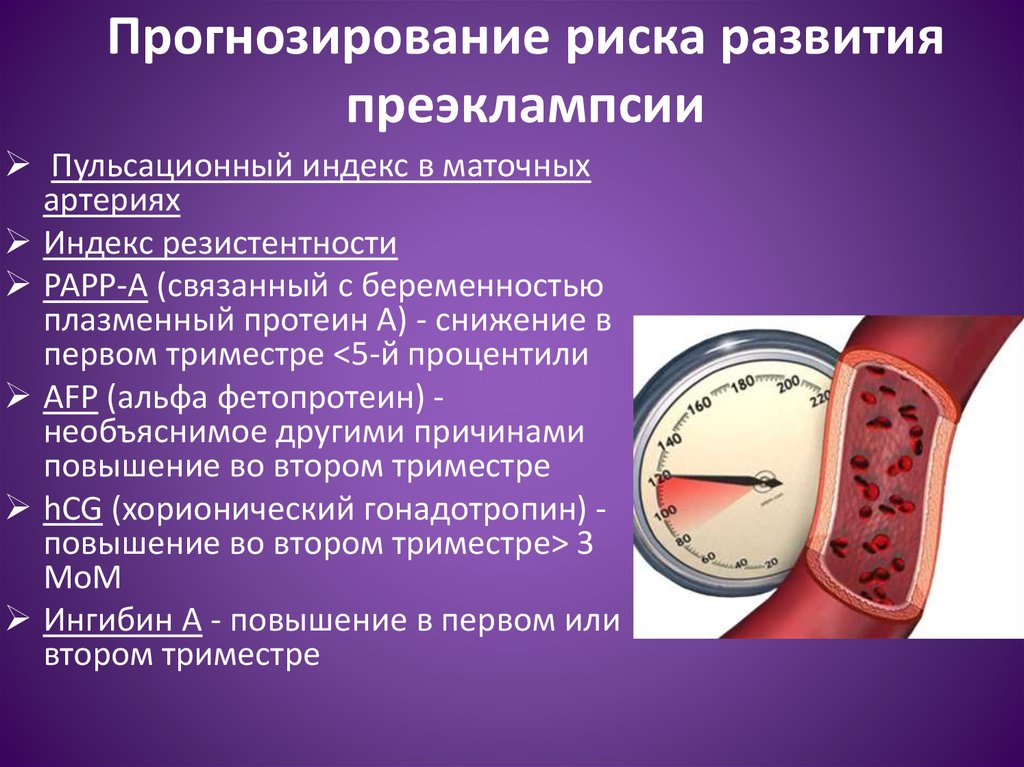
Because headaches, nausea, and aches and pains are common pregnancy complaints, it's difficult to know when new symptoms are simply part of being pregnant and when they may indicate a serious problem — especially if it's your first pregnancy. If you're concerned about your symptoms, contact your doctor.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of preeclampsia likely involves several factors. Experts believe it begins in the placenta — the organ that nourishes the fetus throughout pregnancy. Early in a pregnancy, new blood vessels develop and evolve to supply oxygen and nutrients to the placenta.
In women with preeclampsia, these blood vessels don't seem to develop or work properly. Problems with how well blood circulates in the placenta may lead to the irregular regulation of blood pressure in the mother.
Other high blood pressure disorders during pregnancy
Preeclampsia is one high blood pressure (hypertension) disorder that can occur during pregnancy. Other disorders can happen, too:
- Gestational hypertension is high blood pressure that begins after 20 weeks without problems in the kidneys or other organs.
 Some women with gestational hypertension may develop preeclampsia.
Some women with gestational hypertension may develop preeclampsia. - Chronic hypertension is high blood pressure that was present before pregnancy or that occurs before 20 weeks of pregnancy. High blood pressure that continues more than three months after a pregnancy also is called chronic hypertension.
- Chronic hypertension with superimposed preeclampsia occurs in women diagnosed with chronic high blood pressure before pregnancy, who then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.
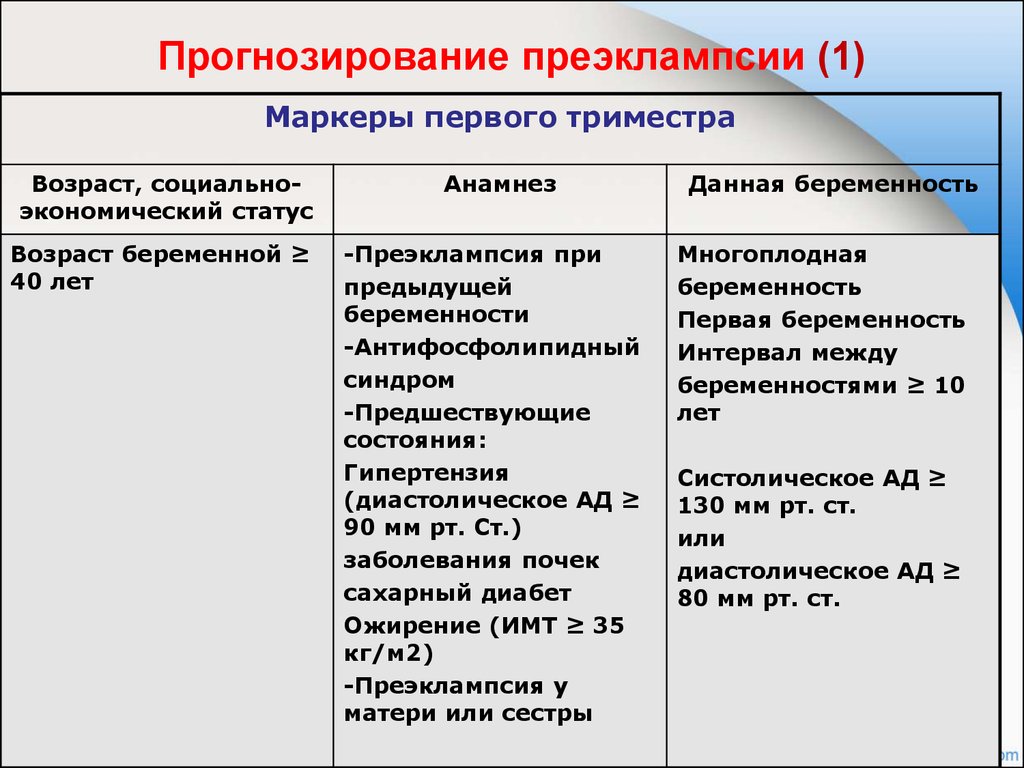
Risk factors
Conditions that are linked to a higher risk of preeclampsia include:
- Preeclampsia in a previous pregnancy
- Being pregnant with more than one baby
- Chronic high blood pressure (hypertension)
- Type 1 or type 2 diabetes before pregnancy
- Kidney disease
- Autoimmune disorders
- Use of in vitro fertilization
Conditions that are associated with a moderate risk of developing preeclampsia include:
- First pregnancy with current partner
- Obesity
- Family history of preeclampsia
- Maternal age of 35 or older
- Complications in a previous pregnancy
- More than 10 years since previous pregnancy
Other risk factors
Several studies have shown a greater risk of preeclampsia among Black women compared with other women. There's also some evidence of an increased risk among indigenous women in North America.
There's also some evidence of an increased risk among indigenous women in North America.
A growing body of evidence suggests that these differences in risk may not necessarily be based on biology. A greater risk may be related to inequities in access to prenatal care and health care in general, as well as social inequities and chronic stressors that affect health and well-being.
Lower income also is associated with a greater risk of preeclampsia likely because of access to health care and social factors affecting health.
For the purposes of making decisions about prevention strategies, a Black woman or a woman with a low income has a moderately increased risk of developing preeclampsia.
Complications
Complications of preeclampsia may include:
- Fetal growth restriction. Preeclampsia affects the arteries carrying blood to the placenta. If the placenta doesn't get enough blood, the baby may receive inadequate blood and oxygen and fewer nutrients.
 This can lead to slow growth known as fetal growth restriction.
This can lead to slow growth known as fetal growth restriction. - Preterm birth. Preeclampsia may lead to an unplanned preterm birth — delivery before 37 weeks. Also, planned preterm birth is a primary treatment for preeclampsia. A baby born prematurely has increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatments before preterm delivery may decrease some risks.
- Placental abruption. Preeclampsia increases your risk of placental abruption. With this condition, the placenta separates from the inner wall of the uterus before delivery. Severe abruption can cause heavy bleeding, which can be life-threatening for both the mother and baby.
-
HELLP syndrome. HELLP stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count.
 This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.
This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.Signs and symptoms include nausea and vomiting, headache, upper right belly pain, and a general feeling of illness or being unwell. Sometimes, it develops suddenly, even before high blood pressure is detected. It also may develop without any symptoms.
-
Eclampsia. Eclampsia is the onset of seizures or coma with signs or symptoms of preeclampsia. It is very difficult to predict whether a patient with preeclampsia will develop eclampsia. Eclampsia can happen without any previously observed signs or symptoms of preeclampsia.
Signs and symptoms that may appear before seizures include severe headaches, vision problems, mental confusion or altered behaviors.
 But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery.
But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery. - Other organ damage. Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on how severe the preeclampsia is.
- Cardiovascular disease. Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you've had preeclampsia more than once or you've had a preterm delivery.
Prevention
Medication
The best clinical evidence for prevention of preeclampsia is the use of low-dose aspirin. Your primary care provider may recommend taking an 81-milligram aspirin tablet daily after 12 weeks of pregnancy if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
It's important that you talk with your provider before taking any medications, vitamins or supplements to make sure it's safe for you.
Lifestyle and healthy choices
Before you become pregnant, especially if you've had preeclampsia before, it's a good idea to be as healthy as you can be. Talk to your provider about managing any conditions that increase the risk of preeclampsia.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Pre-eclampsia screening at 11-14 weeks of gestation
The first trimester OSCAR detection of women at risk for early preeclampsia is important because early treatment with small doses of aspirin can promote placental blood vessel growth, thus improving attachment to the placenta and reducing possibility of early preeclampsia.
In the first trimester, the OSCAR test can identify with 76.7% accuracy women at risk of developing early preeclampsia before the 37th week of pregnancy, and with an accuracy of 43.1% - those with who will develop preeclampsia after 37 weeks.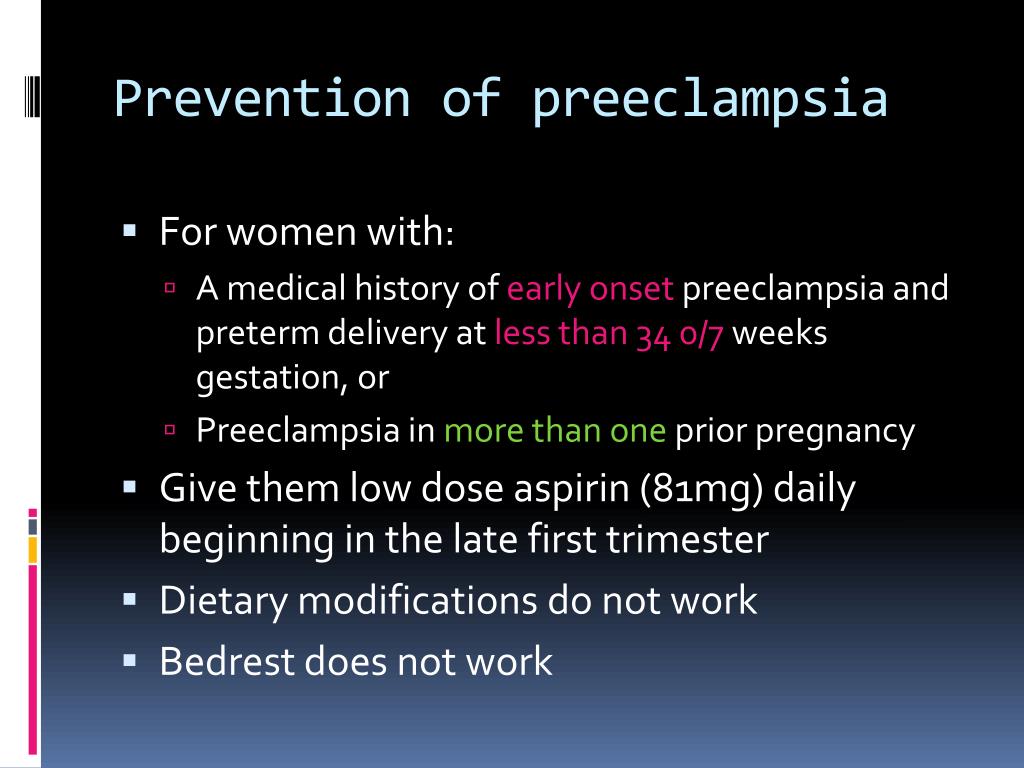 Among pregnant twins, all women who can develop early preeclampsia can be identified before the 37th week of pregnancy. In the case of twins, the disadvantage of the test is that it produces 75% false positives.
Among pregnant twins, all women who can develop early preeclampsia can be identified before the 37th week of pregnancy. In the case of twins, the disadvantage of the test is that it produces 75% false positives.
Studies have shown that aspirin taken in small doses before the 16th week of pregnancy improves the blood supply to the developing placenta and in 62% of cases reduces the risk of early preeclampsia, which can lead to preterm birth before the 37th week of pregnancy and in 30% placental abruption. Therefore, women with an increased risk of preeclampsia are advised to take 150 milligrams of aspirin once a day, in the evenings, until the 36th week of pregnancy.
Aspirin only works when taken regularly. If a woman at high risk of preeclampsia regularly takes 150 mg of aspirin every evening, then in 74% of cases it is possible to prevent early preeclampsia that develops before the 37th week of pregnancy.
Aspirin prophylaxis will not prevent preeclampsia in women with chronic hypertension. If a woman at risk who does not suffer from chronic hypertension regularly takes 150 mg of aspirin every evening, then at 9In 5% of cases, it is possible to prevent early preeclampsia that develops before the 37th week of pregnancy.
If a woman at risk who does not suffer from chronic hypertension regularly takes 150 mg of aspirin every evening, then at 9In 5% of cases, it is possible to prevent early preeclampsia that develops before the 37th week of pregnancy.
- High risk group. This group includes women for whom the risk of early, before the 34th week, pre-eclampsia was higher than 1:200 according to the results of screening. The group includes 10% of the study participants, of which 75% develop preeclampsia before the 37th week of pregnancy. These women are advised to start aspirin prophylaxis (150 mg in the evening) before 36 weeks of gestation and reassess the risk of preeclampsia at 20 weeks of gestation.
- Low risk group. This group includes women for whom the risk of early, before the 34th week of pregnancy, pre-eclampsia was less than 1:200 according to the results of screening. The group includes 90% of screening participants who receive a feeling of confidence that before the 37th week of pregnancy they are very unlikely to develop preeclampsia.
 They are advised to reassess their risk at 20 weeks of gestation, as early detection of preeclampsia is then more accurate. What is preeclampsia?
They are advised to reassess their risk at 20 weeks of gestation, as early detection of preeclampsia is then more accurate. What is preeclampsia? - Pre-eclampsia screening at 19-22 weeks of gestation
- Pre-eclampsia screening at 35-37 weeks of gestation
- Preeclampsia Screening Information Sheet
- Preeclampsia Risk Calculator
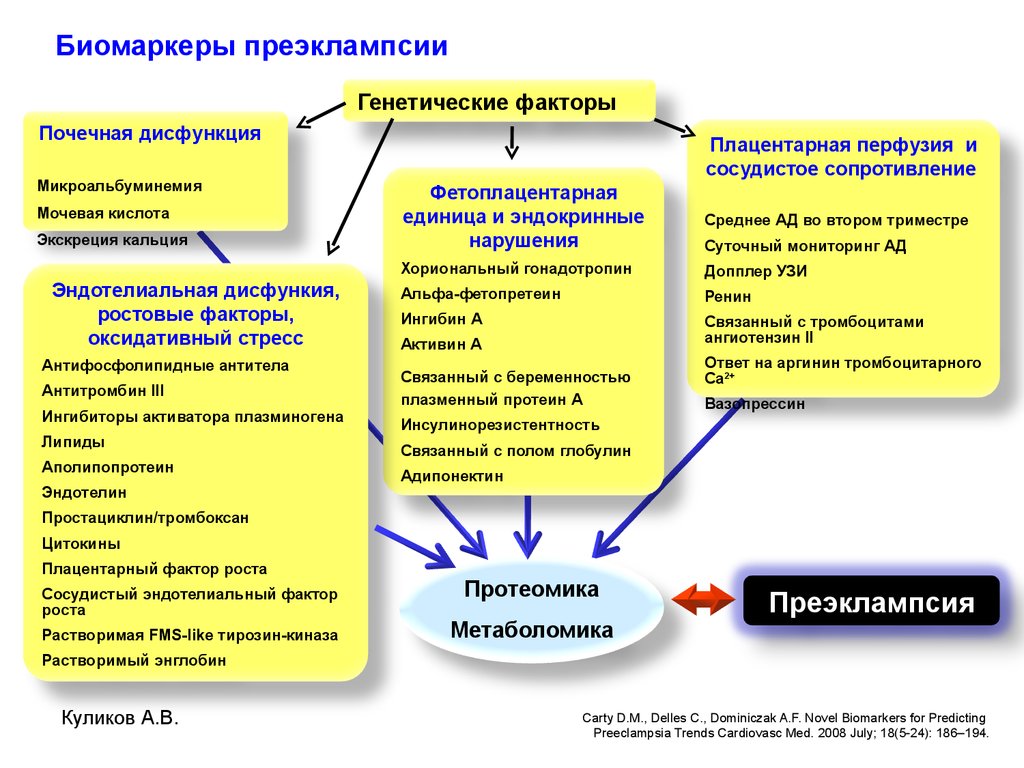
1st trimester prenatal screening with preeclampsia risk calculation
Investigated biomaterial: Venous blood (serum)
Research method: The study is carried out by the method of fluorescent immunoassay with subsequent automated evaluation of the results in the program for calculating the degree of risk. Calculation of the risks of chromosomal pathology is carried out using the DELFIA LifeCycle program (PerkinElmer, Inc. USA.). The calculation of the risk of preterm birth and preeclampsia is carried out using the DELFIA Predictor program (PerkinElmer, Inc. USA.).
USA.).
Deadline from the receipt of the biomaterial to the laboratory: 6 c.d.
Description
This research program makes it possible to calculate the risk of developing preeclampsia and the presence of chromosomal pathologies. Screening data, ultrasound and blood pressure measurements are used for the calculation.
Preeclampsia is a pathological condition that can appear after the 20th week of pregnancy. The disease is manifested by proteinuria and high blood pressure. Perhaps the development of insufficiency of internal organs, the appearance of edema. Pre-eclampsia is divided into early and late (before the 34th week and after). The early one is much more difficult than the later one.
Pre-eclampsia risk factors:
- multiple pregnancy;
- over 35 years of age;
- first pregnancy;
- hereditary predisposition;
- overweight;
- repeated births after a break of more than 10 years;
- proteinuria;
- history of preeclampsia;
- the presence of chronic diseases.
Research Program
PAPP-A. This is a protein that pregnant women produce in large quantities. It ensures the normal growth of the placenta and its development. In the presence of various pathologies of the fetus, the level of PAPP-A is significantly reduced. Also, a decrease in the production of this protein may indicate a high risk of developing pregnancy complications.
Free beta-hCG is a subunit of human chorionic gonadotropin molecules. It is formed in the shell of the embryo and is a marker of pregnancy. This hormone is necessary for the normal course of pregnancy. According to the results of the analysis, it is possible to judge the anomalies in the development of the fetus.
placental growth factor. A low concentration of this protein indicates an increased risk of preeclampsia. Also, according to the results of this analysis, it is possible to suspect or exclude Down syndrome, metabolic syndrome, preeclampsia in the fetus.
Indications for the study: pregnant women for a period of 11-14 weeks.
Preparation:
Blood sampling is carried out no earlier than 3 hours after the last meal, the use of non-carbonated water is allowed.
Prenatal screening of the first trimester of pregnancy is carried out at 11 weeks -13 weeks 6 days. It is necessary to have with you the ultrasound data performed during this period; it is permissible to have a difference between the ultrasound data and blood donation: no more than 1 day. Risk calculation is possible only with a KTP indicator (Coccyx-parietal size) from 45 mm to 80 mm.
Result format and unit of measurement: a conclusion is issued based on the results of the study
Result interpretation:
The results of laboratory tests are not the only criterion taken into account by the attending physician when making a diagnosis and prescribing appropriate treatment, and should be considered in conjunction with anamnesis data and the results of other possible examinations, including instrumental diagnostic methods.