Leg aches at night during pregnancy
Aching, Painful, Or Heavy Legs During Pregnancy
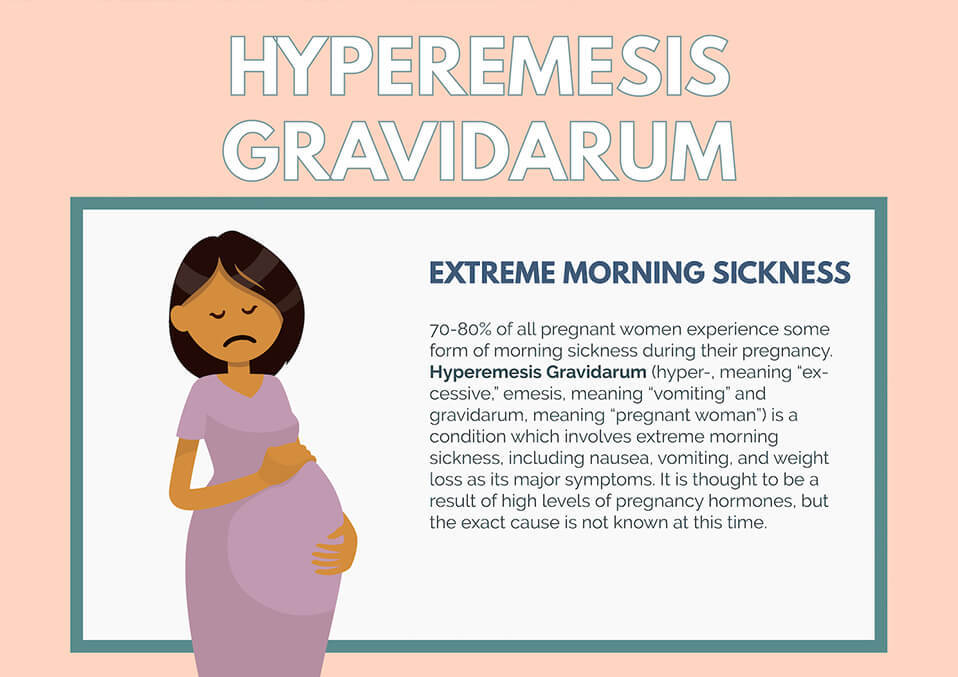
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels.
Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.
- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen. Veins, on the other hand, return blood to the heart.
Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
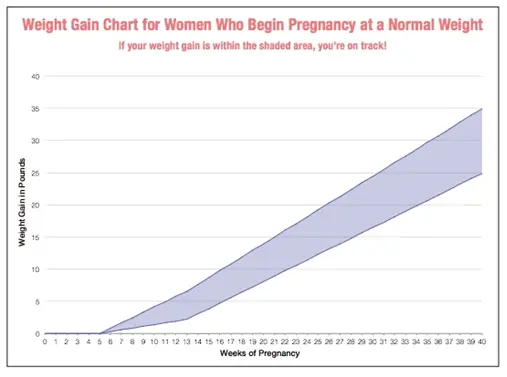
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.

- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.

A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
Leg aches and pains during pregnancy
If your legs feel like lead while you’re pregnant, you’re not alone; over half of us suffer with aching and tired legs in pregnancy.
“The aches happen due to increased blood volume and because your legs have to support a whole lot more of you than usual,” explains Boots UK Pharmacist, Angela Chalmers.
“You’re also adjusting to ferrying around a body that's carrying more of its weight out front.”
Charming. Oh well, suppose it's just another lovely pregnancy niggle to look forward to...
Well, sorry to be the bearer of more bad news, but the aches and pains can actually start fairly early on in pregnancy as the body is flooded with oestrogen and progesterone.
And as we get heavier and larger, they really go into over-drive.
"I had achy legs with all 3 of my boys. Drove me mad by the end of my pregnancies and dh with me moaning about them lol," mumof3blues on our forum tells us.
Angela Chalmers explains: “Your growing uterus is also putting pressure on the veins whose job it is to carry blood back from your lower body – this partially blocks the blood flow, keeping fluid in your legs and feet and making them feel swollen and tired. ”
”
And it's often worse at night, when we’re horizontal-ish in bed, desperately trying to get some shut eye. Typical...
As forum mum cookieandcream says: "I've started getting really achy and crampy legs when i'm in bed."
It’s all about the circulation
Leg aches are all to do with circulation, so be on the look out for other such glamorous side effects as varicose veins.
Another of our forum-posters, supersquish, explains it like this: "Sounds like your growing belly putting pressure on you nerves and vessels! I used to get restless legs with my first with is similar, was very annoying! Sounds normal."
You should also be aware that the dull ache of leg pains is not the same as the sharper, more acute pain of leg cramps in pregnancy.
So what can I do to relieve the ache?
Anything that improves your circulation should have the knock on effect of alleviating leg ache.
Here are our 6 top tips:
- Elevate your legs – Raising your legs above your heart will help improve circulation.
 Simply put a couple of cushions under your ankles when sitting or lying down at night.
Simply put a couple of cushions under your ankles when sitting or lying down at night. - Sleep on the left side - as well as improving blood flow to your baby, it relieves pressure on the vena cava, the largest vein leading to the heart
- Uncross your legs – it might feel comfy but sitting cross legged is a big no-no if you want to improve blood flow.
- Get moving – Ironically, taking your bump for a walk might stop your legs aching. Just half an hour should get the circulation going and relieve the pain.
- Wear loose clothing – Back away from the skinny jeans (or buy stretchy maternity ones!) Anything too tight around your body will hinder circulation.
- Massage – if all else fails get someone to give your legs and ankles a good going over, or better still get your other half to do it.
What can I do to stop it happening in the first place?
Sadly, aching legs are just part and parcel of life with a baby on board, but prolific sufferers like mrs_platt2b do have some personal avoidance techniques.
"I have a few tips for you all tho that i have required over the year:
1. Keep your legs elevated as much as poss, ideally above your heart to allow for better circulation.
2. When your legs are achy i have found walking along a really cold surface or however you can keep them cold (my mum also swears by this who has suffered with restless legs since being pregnant with me
3. Bananna's are very good apparently, also cutting out as much caffeine as much a poss, i dnt have any caffeeine at all now and have found it really helps
4. Magnesium or iron deficiency has been known to be a cause of achy, bad circulated, visit a health food shop and speak to them about vitamins."
And what if it's something more serious?
It’s natural to worry that aching legs may be a sign of something more serious: “I was just worried in case it was a sign of DVT or something,” says forum user HappyArchie. “I suppose being pregnant, we all worry constantly about our changing bodies. ”
”
Thankfully, aching legs by themselves are not generally a cause for concern. But if it develops into a constant muscle pain and is accompanied by swelling, you should consult a doctor to rule out a blood clot.
Likewise, if your legs are swollen and your face is also swollen and puffy and you have headaches, see your GP or midwife asap. These could be signs of pre-eclampsia.
Some women suffer from restless legs syndrome during pregnancy - think jittery, can't-stop-moving limbs - and this typically happens at night. Again, like aching legs, it's not serious but it can be very annoying.
So, in a nutshell, try not to worry - all these aches and pains, annoyances, niggles and downright complaints are merely small stones on the road to becoming a mother.
And if you need somewhere to offload and have a good old moan, check out our forums where a problem shared is always a problem solved. Or at least acknowledged by like-minded souls!
Read more
- Farting and burping in pregnancy
- Mood swings in pregnancy
- Swelling in pregnancy
Reduces legs during pregnancy: what to do?
Pregnancy is a time of waiting and doubts. Probably, women never have so many questions. Why does it bring her legs together so often? What to do if you wake up with cramps at night? How to deal with this scourge and avoid bouts of pain in the legs? We are looking for answers to these and other questions.
Probably, women never have so many questions. Why does it bring her legs together so often? What to do if you wake up with cramps at night? How to deal with this scourge and avoid bouts of pain in the legs? We are looking for answers to these and other questions.
What are seizures?
Legs cramps not only during pregnancy, from time to time every person faces unpleasant painful cramps. A cramp is a sudden, uncontrollable muscle contraction that a person cannot relax. This condition can be caused by neurological disorders (for example, seizures are characteristic of epilepsy), a number of diseases (such as diabetes mellitus, osteochondrosis, and others), and can also be associated with physiological conditions. After all, convulsions occur, for example, after a strong overload, dehydration, hypothermia, etc. Sometimes cramps cause severe sharp pain. Sometimes it seems that the legs are pulling. During pregnancy, this condition, unfortunately, is noted quite regularly.
Why do pregnant women cramp their legs?
The mechanism of muscle contraction is quite complex, it involves different ions (charged particles): potassium, calcium, sodium and magnesium. If we are talking about a cramp, that is, a condition when we cannot relax a muscle, then magnesium ions play a leading role here. It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
The lack of minerals in the body of the expectant mother is simply explained: such consequences are the restructuring of metabolism and functioning in the "double load" mode. In particular, the expectant mother needs one and a half times more magnesium than usual.
In addition to helping muscles relax, magnesium is also involved in a number of important physiological processes. In particular, magnesium is needed to regulate the processes of formation and expenditure of energy, it is involved in several hundred enzymatic reactions, and if there is little magnesium, then disturbances can occur in the work of almost any body system. Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored.
Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored.
Why do pregnant women cramp their legs at night?
The answer to this question is very simple. The fact is that during the day the body of the expectant mother bears an increased load. And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
What should I do if my legs cramp during pregnancy?
To begin with, tell the doctor you are seeing about this. The magnesium preparations already mentioned, which he most likely recommends to you, can help solve the problem.
However, the reason that the expectant mother cramps her legs during pregnancy may be not only a metabolic disorder. Often muscle spasms begin as a result of varicose veins - the "faithful" companion of pregnancy. The veins of a woman carrying a baby are subject to increased stress. In addition, hormonal changes in the body seriously affect the state of blood vessels. All this contributes to the development of varicose veins. And a violation of the blood supply to the muscles of the legs, in turn, leads to convulsions.
In addition, hormonal changes in the body seriously affect the state of blood vessels. All this contributes to the development of varicose veins. And a violation of the blood supply to the muscles of the legs, in turn, leads to convulsions.
If the expectant mother is faced with varicose veins, then the best prevention of its progression is to wear compression stockings selected by the doctor in accordance with the gestational age. You also need to give birth in stockings, so that during a particularly intense load on the veins to avoid worsening their condition.
It is important to remember that any discomfort in the well-being of a pregnant woman must be discussed with the doctor who is seeing the expectant mother. Even if the legs cramp infrequently, what to do during pregnancy should be determined by a specialist. This is the only way to avoid serious problems and ensure the health and comfort of both mother and child.
Restless legs syndrome
- Main
- Restless legs syndrome
Restless legs syndrome (RLS) is a neurological disease manifested by paresthesias of sleep in the lower extremities and their excessive motor activity during rest or during sleep.
Restless legs syndrome was first described by Thomas Willis in 1672: “In some people, when they are going to sleep and lie down in bed, immediately after this there is a movement of the tendons, arms and legs, accompanied by colic and such restlessness that the patient cannot sleep like he's under torture." The modern definition of this syndrome was proposed by the Swedish scientist K. Ekbom in 1945:
Restless legs syndrome can be primary (idiopathic) and secondary.
One of the most likely causes of the development of primary restless legs syndrome is considered to be the insufficiency of dopaminergic systems in the subcortical structures of the brain involved in inhibitory processes.
Secondary restless legs syndrome can develop during pregnancy and various pathological conditions.
The main causes of secondary restless leg syndrome are:
- Iron deficiency. Iron deficiency disrupts the production of dopamine in the brain, which in turn provokes the development of secondary RLS.
 A patient's iron stores may be depleted even without clinically significant anemia. Studies have shown that a decrease in iron stores, defined as a decrease in ferritin levels below 50 µg/L, can cause or exacerbate the symptoms of RLS.
A patient's iron stores may be depleted even without clinically significant anemia. Studies have shown that a decrease in iron stores, defined as a decrease in ferritin levels below 50 µg/L, can cause or exacerbate the symptoms of RLS. - Neurological disorders. Secondary RLS is often observed in injuries of the spinal cord and peripheral nervous system, as well as peripheral neuropathies of various origins (diabetic, alcoholic, toxic).
- Pregnancy. RLS occurs in 15-20% of women during pregnancy. Symptoms can be quite severe, but usually disappear completely within a few weeks after delivery. Iron deficiency anemia, folic acid deficiency, hormonal changes, and venous congestion in the lower extremities are thought to be the causes of RLS during pregnancy.
- Uremia. Up to 50% of patients with ESRD have RLS. The frequency of RLS was shown to correlate with blood urea levels, anemia, peripheral neuropathy, and a decrease in parathyroid hormone levels in this category of patients.
 Especially severe symptoms are noted directly during dialysis, when the patient is forced to lie motionless for several hours. Reduction or disappearance of RLS symptoms has been shown after kidney transplantation.
Especially severe symptoms are noted directly during dialysis, when the patient is forced to lie motionless for several hours. Reduction or disappearance of RLS symptoms has been shown after kidney transplantation. - The use of medicines. Symptoms of RLS may develop or worsen with the use of various medications, such as tricyclic antidepressants (amitriptyline, azafen, etc.), selective serotonin reuptake inhibitors (trazodone, Prozac), lithium preparations, metoclopramide (raglan), calcium channel blockers (corinfar, finoptin). Caffeine also worsens the symptoms of RLS.
Clinical manifestations of RLS can be grouped into several main symptom complexes:
Discomfort in the legs. They are usually described as crawling, trembling, tingling, burning, twitching, electric shock, wiggling under the skin, etc. About 30% of patients characterize these sensations as pain. Sometimes patients cannot accurately describe the nature of the sensations, but they are always extremely unpleasant. These sensations are localized in the thighs, shins, feet and undulate every 5-30 seconds. There are significant fluctuations in the severity of these symptoms. In some patients, symptoms may occur only at the beginning of the night, in others - continuously disturb throughout the day.
These sensations are localized in the thighs, shins, feet and undulate every 5-30 seconds. There are significant fluctuations in the severity of these symptoms. In some patients, symptoms may occur only at the beginning of the night, in others - continuously disturb throughout the day.
Symptoms worse at rest. The most characteristic and unusual manifestation of RLS is an increase in sensory or motor symptoms at rest. Patients usually report worsening while sitting or lying down and especially when falling asleep. Usually, before the onset of symptoms, it takes from several minutes to an hour when you are in a calm state.
Symptoms are relieved by movement. Symptoms are greatly relieved or disappear on movement. The best effect most often has a simple walk. In some cases, sipping, bending over, exercising on a stationary bike, or just standing up helps.
Symptoms are circadian. Symptoms are significantly worse in the evening and in the first half of the night (between 6 pm and 4 am).