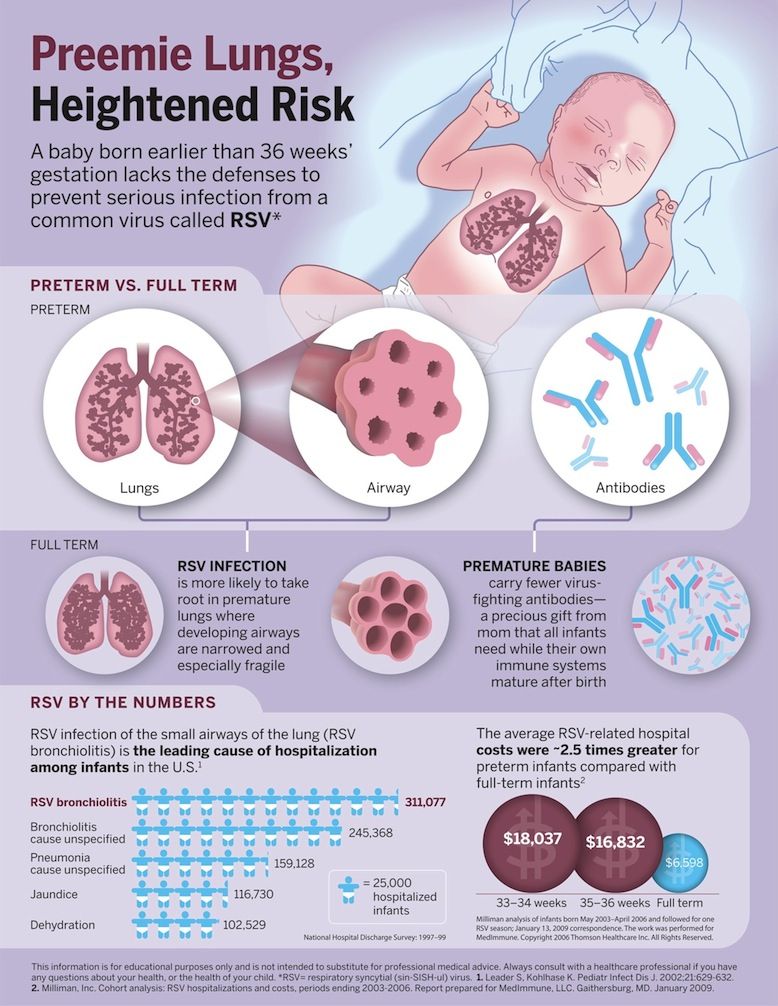
Jaundice in premature baby
Infant jaundice - Symptoms and causes
Overview
Infant jaundice is yellow discoloration of a newborn baby's skin and eyes. Infant jaundice occurs because the baby's blood contains an excess of bilirubin (bil-ih-ROO-bin), a yellow pigment of red blood cells.
Infant jaundice is a common condition, particularly in babies born before 38 weeks' gestation (preterm babies) and some breast-fed babies. Infant jaundice usually occurs because a baby's liver isn't mature enough to get rid of bilirubin in the bloodstream. In some babies, an underlying disease may cause infant jaundice.
Most infants born between 35 weeks' gestation and full term need no treatment for jaundice. Rarely, an unusually high blood level of bilirubin can place a newborn at risk of brain damage, particularly in the presence of certain risk factors for severe jaundice.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Yellowing of the skin and the whites of the eyes — the main sign of infant jaundice — usually appears between the second and fourth day after birth.
To check for infant jaundice, press gently on your baby's forehead or nose. If the skin looks yellow where you pressed, it's likely your baby has mild jaundice. If your baby doesn't have jaundice, the skin color should simply look slightly lighter than its normal color for a moment.
Examine your baby in good lighting conditions, preferably in natural daylight.
When to see a doctor
Most hospitals have a policy of examining babies for jaundice before discharge. The American Academy of Pediatrics recommends that newborns be examined for jaundice during routine medical checks and at least every eight to 12 hours while in the hospital.
Your baby should be examined for jaundice between the third and seventh day after birth, when bilirubin levels usually peak. If your baby is discharged earlier than 72 hours after birth, make a follow-up appointment to look for jaundice within two days of discharge.
The following signs or symptoms may indicate severe jaundice or complications from excess bilirubin. Call your doctor if:
Call your doctor if:
- Your baby's skin becomes more yellow
- The skin on your baby's the abdomen, arms or legs looks yellow
- The whites of your baby's eyes look yellow
- Your baby seems listless or sick or is difficult to awaken
- Your baby isn't gaining weight or is feeding poorly
- Your baby makes high-pitched cries
- Your baby develops any other signs or symptoms that concern you
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.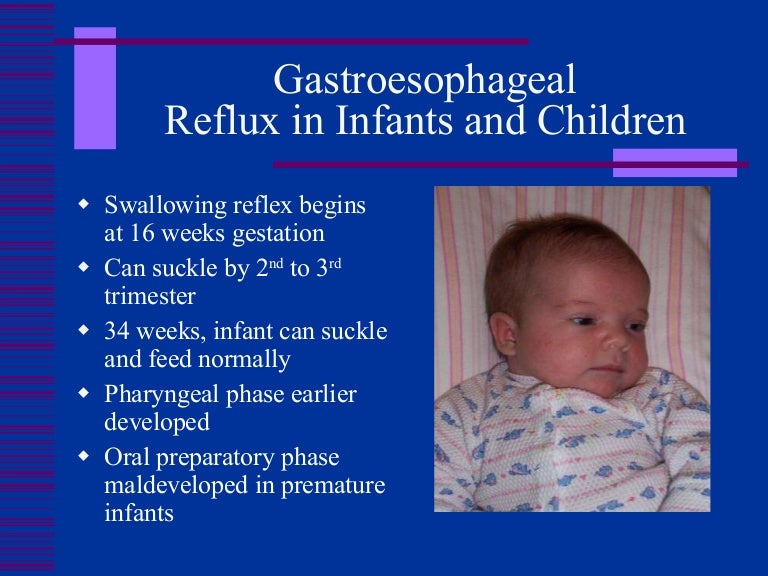 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Excess bilirubin (hyperbilirubinemia) is the main cause of jaundice. Bilirubin, which is responsible for the yellow color of jaundice, is a normal part of the pigment released from the breakdown of "used" red blood cells.
Newborns produce more bilirubin than adults do because of greater production and faster breakdown of red blood cells in the first few days of life. Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. A newborn's immature liver often can't remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life.
Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. A newborn's immature liver often can't remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life.
Other causes
An underlying disorder may cause infant jaundice. In these cases, jaundice often appears much earlier or much later than does the more common form of infant jaundice. Diseases or conditions that can cause jaundice include:
- Internal bleeding (hemorrhage)
- An infection in your baby's blood (sepsis)
- Other viral or bacterial infections
- An incompatibility between the mother's blood and the baby's blood
- A liver malfunction
- Biliary atresia, a condition in which the baby's bile ducts are blocked or scarred
- An enzyme deficiency
- An abnormality of your baby's red blood cells that causes them to break down rapidly
Risk factors
Major risk factors for jaundice, particularly severe jaundice that can cause complications, include:
- Premature birth.
 A baby born before 38 weeks of gestation may not be able to process bilirubin as quickly as full-term babies do. Premature babies also may feed less and have fewer bowel movements, resulting in less bilirubin eliminated through stool.
A baby born before 38 weeks of gestation may not be able to process bilirubin as quickly as full-term babies do. Premature babies also may feed less and have fewer bowel movements, resulting in less bilirubin eliminated through stool. - Significant bruising during birth. Newborns who become bruised during delivery gets bruises from the delivery may have higher levels of bilirubin from the breakdown of more red blood cells.
- Blood type. If the mother's blood type is different from her baby's, the baby may have received antibodies through the placenta that cause abnormally rapid breakdown of red blood cells.
- Breast-feeding. Breast-fed babies, particularly those who have difficulty nursing or getting enough nutrition from breast-feeding, are at higher risk of jaundice. Dehydration or a low caloric intake may contribute to the onset of jaundice. However, because of the benefits of breast-feeding, experts still recommend it.
 It's important to make sure your baby gets enough to eat and is adequately hydrated.
It's important to make sure your baby gets enough to eat and is adequately hydrated. - Race. Studies show that babies of East Asian ancestry have an increased risk of developing jaundice.
Complications
High levels of bilirubin that cause severe jaundice can result in serious complications if not treated.
Acute bilirubin encephalopathy
Bilirubin is toxic to cells of the brain. If a baby has severe jaundice, there's a risk of bilirubin passing into the brain, a condition called acute bilirubin encephalopathy. Prompt treatment may prevent significant lasting damage.
Signs of acute bilirubin encephalopathy in a baby with jaundice include:
- Listlessness
- Difficulty waking
- High-pitched crying
- Poor sucking or feeding
- Backward arching of the neck and body
- Fever
Kernicterus
Kernicterus is the syndrome that occurs if acute bilirubin encephalopathy causes permanent damage to the brain. Kernicterus may result in:
Kernicterus may result in:
- Involuntary and uncontrolled movements (athetoid cerebral palsy)
- Permanent upward gaze
- Hearing loss
- Improper development of tooth enamel
Prevention
The best preventive of infant jaundice is adequate feeding. Breast-fed infants should have eight to 12 feedings a day for the first several days of life. Formula-fed infants usually should have 1 to 2 ounces (about 30 to 60 milliliters) of formula every two to three hours for the first week.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Jaundice | Bliss
Find out more about how neonatal (newborn) jaundice can affect your baby, what signs to look out for, and how your baby might be looked after.
Jaundice (jawn-diss) is the name for yellowing of the skin and the whites of the eyes. It is very common for newborn babies to get jaundice. In most cases it is harmless and goes away without needing treatment by the time your baby is about two weeks old.
Sometimes jaundice can be serious and may be caused by a medical problem. Serious cases of newborn jaundice are more common in babies born premature. Because it can sometimes be serious, your midwife or baby’s doctor needs to know if they have jaundice. Your baby can then get any treatment they need quickly.
What causes jaundice?
The yellow colour is caused by a build-up of a substance called bilirubin (billy-roo-bin).
Bilirubin is a normal body chemical, which is produced when red blood cells are broken down and replaced by fresh cells. Bilirubin is then processed by the liver and leaves the body in urine (pee) and stools (poo).
Jaundice is common in newborn babies because the baby’s liver is not developed enough in the first few days to process all the bilirubin that is produced.vi Bilirubin then builds up in the blood, which causes jaundice.
Doctors call this ‘physiological jaundice’, which means it is not caused by a medical problem. This is the most common type of jaundice and starts at about two days after birth, but is usually gone by about two weeks.
This is the most common type of jaundice and starts at about two days after birth, but is usually gone by about two weeks.
Other types of jaundice
Other types of jaundice may be caused by serious medical problems. Jaundice that occurs within the first 24 hours of life, which doctors call ‘early jaundice’, could be caused by conditions such as:
- The mother and baby having different blood types (Rhesus disease)
- Severe infection (Sepsis).
There is also a type of jaundice which causes babies to be jaundiced for longer (after they are around two weeks old). This is called ‘prolonged jaundice’. It can also be referred to as ‘breastmilk jaundice’ because it is much more common in babies who are fed with their mother’s milk.
Doctors are not sure why this happens, but it does not harm the baby and will go away without treatment. This type of jaundice can sometimes carry on for up to 12 weeks, but this does not mean that feeding with breast milk should stop.
Prolonged jaundice is usually harmless, but may occasionally be caused by more serious medical problems. Babies with prolonged jaundice will usually have some extra blood tests to look for any medical problems. This is often at a clinic in the hospital or may be done at home by a community midwife in some areas.
In most cases, no medical condition is found and the jaundice gradually goes away without needing treatment, but occasionally important medical problems are picked up by these tests.
Which babies are most likely to get newborn jaundice?
Jaundice in newborn babies is very common, but in most cases is not severe enough to need treatment. There are some things which make a baby more likely to have jaundice that needs treating:
- Being born premature (less than 38 weeks) – the earlier a baby is born, the more likely they are to need treatment for jaundice.
- Having a low birth weight.
- Being male.
- Being from an Asian or black family.

- Getting jaundice in the first 24 hours after birth.
- Having a brother or sister who needed treatment for jaundice after birth.
- Being only fed with breastmilk.
Babies born prematurely are more likely to get jaundice. If they have jaundice, it is more likely to be severe and tends to last longer than in full term babies.
After your baby is born, they will be examined, both in hospital and at home. Every time your baby is examined, your care team will be checking for jaundice. You will be encouraged to check your baby too, especially after you take them home. If your baby has jaundice, their skin and the whites of their eyes will appear yellowish.
Signs of jaundice in babies with darker skin tones
It can be more difficult to tell if a baby has jaundice if they have darker skin, because the yellowing may be less obvious. Gently pressing on the tip of their nose or on their forehead can make it easier to see any yellowing.
The whites of the eyes should normally always be white, no matter how dark your baby’s skin. So checking your baby’s eyes is a good way to look for jaundice. It is best to check your baby in bright light, preferably daylight.
So checking your baby’s eyes is a good way to look for jaundice. It is best to check your baby in bright light, preferably daylight.
Tell your widwife, health visitor, or GP the same day if you think your baby has jaundice.
Jaundice on the neonatal unit
Jaundice is commonly seen on the neonatal unit, especially with preterm babies. Around 80% of preterm babies develop jaundice. The liver of a preterm baby is still developing, and is not yet able to process bilirubin as easily as term babies.
Preterm babies are also more sensitive to the potential complications of jaundice, so treatment often starts earlier than in babies born at full-term.
Jaundice is also more common in babies who are born at full-term but unwell, for example with an infection, or who have other risk factors. Their care team will know what to look out for and will check your baby’s bilirubin level, but if you think your baby looks like they have jaundice, please mention this to them.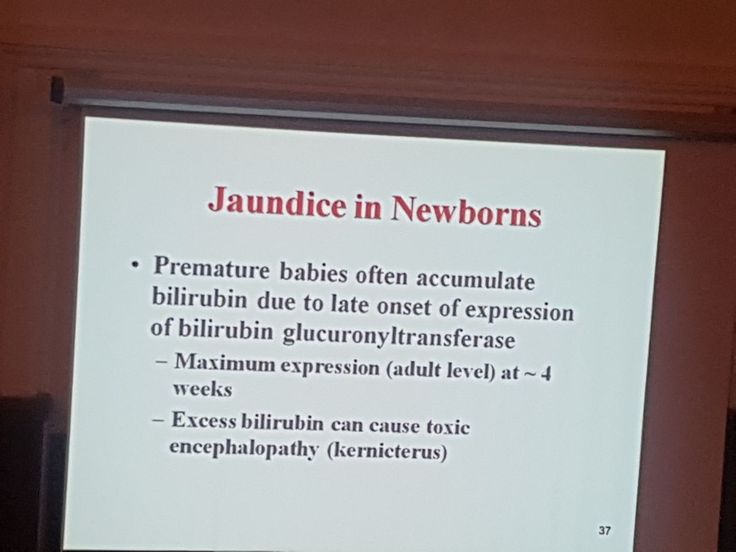
If you notice your baby has jaundice
If you think your baby may have jaundice, tell your midwife, health visitor or doctor straight away. Jaundice is not usually a serious problem, but it is best to get your baby checked.
If your baby’s jaundice does not go away (prolonged jaundice)
In full-term babies, jaundice usually goes away on its own by the time your baby is two weeks old, or three weeks if they were premature. If the jaundice does not go away, it might mean that there is an underlying medical problem.
If your baby has jaundice for more than two weeks, tell your midwife, health visitor or GP the same day. Prolonged jaundice is usually harmless, but it is important to have your baby checked in case they need treatment for a medical problem.
Pale stools (poo) and dark urine
A newborn baby’s stool should be yellowy orange and their urine should normally be colourless or yellow. If they are not, that can be a sign of a problem which needs to be investigated. If your baby has pale (cream or white coloured) stools then you should inform your Community Midwife, GP or Health Visitor immediately, and tests should be arranged that day.
If your baby has pale (cream or white coloured) stools then you should inform your Community Midwife, GP or Health Visitor immediately, and tests should be arranged that day.
Useful guide to baby stool colour.
When your baby needs immediate medical help
Get immediate medical help by contacting your GP or going to the hospital Accident and Emergency department if your baby:
- Has jaundice in the first 24 hours after they are born.
- Has jaundice and is unwell, becoming more drowsy or not feeding.
- Is becoming more and more yellow.
What tests might my baby have?
To accurately check whether your baby has jaundice, the level of bilirubin in their blood needs to be measured. Your midwife may be able to do this test at home, or you may need to take your baby to the hospital. If you are on a neonatal unit, doctors and nurses will check your baby’s bilirubin level regularly.
The two main ways to check your baby’s bilirubin level are:
- By using a small device called a bilirubinometer (billy-roo-bin-ometer), which shines a light onto your baby’s skin.

- With a blood test from a heel prick. This may be needed depending on the results of the bilirubinometer test and the age of your baby.
The results of the test are used to see whether your baby needs any treatment. The doctor may also recommend further tests to look for other causes of jaundice. If so, they will explain what these tests involve.
Most babies with newborn jaundice do not need treatment. If your baby does need treatment, this will usually be given in hospital, but sometimes it can be given at home. Some people believe that sunlight is a good treatment for newborn jaundice but this is not correct.
The main treatment for newborn jaundice is called phototherapy. This is where your baby lies in an incubator with a blue light source above them. Some babies may be able to have phototherapy by lying on a special light-up blanket (called a ‘biliblanket’) instead. The blue light changes the bilirubin into a form that your baby’s body can more easily process.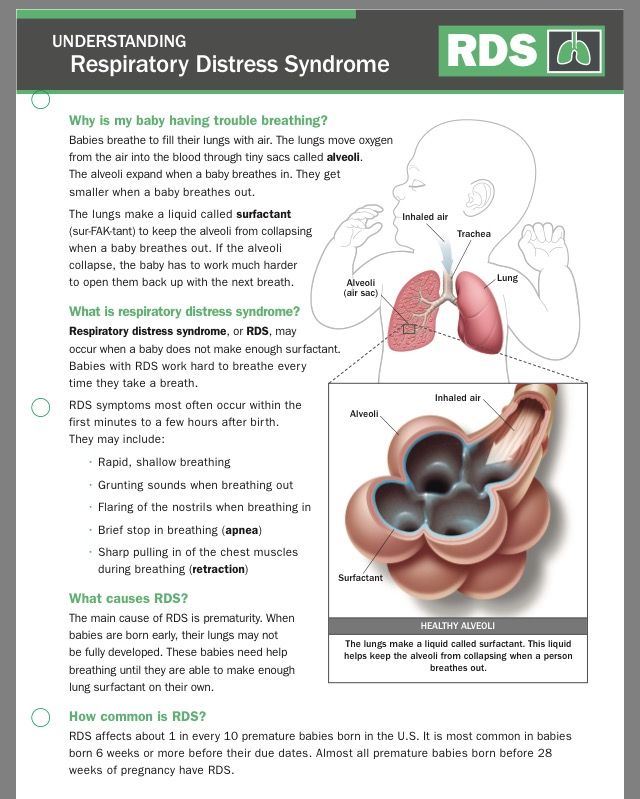
You will usually still be able to feed your baby, change their nappies, and give them a cuddle. Find guidance on how you can be more involved in your baby’s care on the unit.
Preterm babies may need multiple treatments over a number of days and sometimes weeks. The more preterm your baby is, the more likely it is they will need phototherapy. Once treatment has stopped, your baby's bilirubin level will be checked again as they may require more phototherapy.
Very occasionally, a baby with jaundice needs a treatment called exchange transfusion. This is where your baby’s blood is slowly replaced with blood from a blood donor, to remove the bilirubin. This treatment will happen in a neonatal unit and will only be done if your baby’s bilirubin level is very high, or if phototherapy has not worked.
Your baby may need other treatments if they have a medical condition causing their jaundice. You can ask your nurses or doctors to explain what these involve.
Are there any short-term or long-term effects from having newborn jaundice?
Most newborn babies who have jaundice are not ill, and the jaundice goes away on its own in a few weeks without causing any problems.
But high levels of bilirubin can be harmful. That is why some babies need treatment. Fortunately, treatment usually works well to bring down the high level of bilirubin before it causes harm.
In a small number of babies, levels of bilirubin go very high. This can affect the brain and cause a condition called kernicterus (ker-nic-ter-us). Babies with this condition will be very unwell and will need care in the neonatal intensive care unit (NICU). Signs of kernicterus include:
- Being overly sleepy
- Being irritable
- Being floppy, or stiff with an arched back
- Having pauses in breathing (apnoea)
- Having unusual movements (seizures)
Kernicterus can lead to long-term problems for babies. These include seizures (fits), learning difficulties, and hearing problems. If your baby has had kernicterus, they will have follow up appointments to check their development.
If jaundice is caused by a baby having a different blood type to their mother (Rhesus disease), this can also cause the baby to develop anaemia (ah-nee-mee-ya), which is when they have less healthy red blood cells.
Where can I get more help and support?
It is natural to feel worried if something seems wrong with your baby. Your midwife, health visitor, or your baby’s doctor will be able to talk to you about newborn jaundice. In most cases they will be able to reassure you that your baby’s jaundice will get better without causing problems.
If your baby needs treatment, you can talk to the nurses and doctors in the hospital. If you are unsure about any part of your baby’s diagnosis, treatment or care, just ask.
If you feel like you are struggling, we have lots of information and tips on how you can look after yourself and find support.
If your baby is found to have an underlying liver problem, you may find it helpful to visit the website of the Children’s Liver Disease Foundation. We also have some other links to charities and organisations who can provide support.
If you need someone to talk to, you can contact us on [email protected] or arrange a video call with one of our volunteers.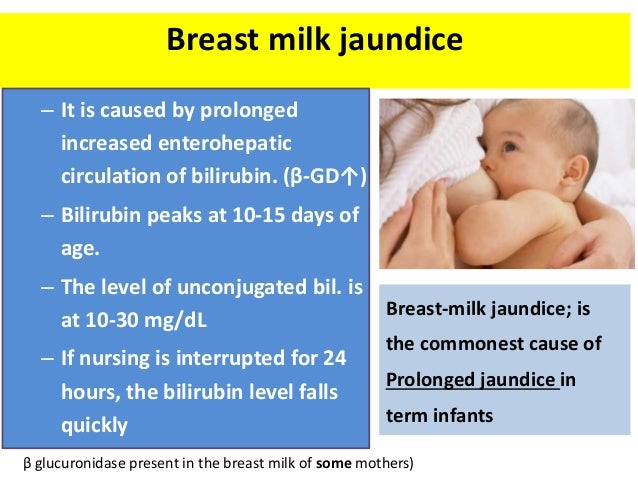
If you have any feedback about this page, please email: [email protected]
Related content
Neonatal jaundice | Ida-Tallinna Keskhaigla
The purpose of this information sheet is to provide parents with information about the causes of neonatal jaundice (jaundice of the newborn, hyperbilirubinemia) and related examinations, tests and treatment options.
Visible yellow skin tone, or jaundice, is the most common sign of jaundice in the neonatal period (days 0-28). Physiological or natural jaundice May occur from age 24 hours to 14 days after birth .
Causes
Before birth, the fetus has more red blood cells (erythrocytes) than in later periods of life, and their (erythrocytes) life expectancy in the first days is somewhat shorter than usual. After the birth of a child, red blood cells begin to break down, and a bile pigment is formed in the blood - bilirubin . The liver of a newborn has to withstand a 2-3 times greater load than in the prenatal period in order to remove bilirubin from the body, which is released during the breakdown of red blood cells. The fact that some healthy newborns develop so-called physiological jaundice and others do not is mainly due to the different ability of their liver to remove bilirubin.
The liver of a newborn has to withstand a 2-3 times greater load than in the prenatal period in order to remove bilirubin from the body, which is released during the breakdown of red blood cells. The fact that some healthy newborns develop so-called physiological jaundice and others do not is mainly due to the different ability of their liver to remove bilirubin.
Sign of physiological jaundice - yellowing of the skin. The peak of jaundice is usually observed in children on the 3-6th day of life, in premature babies - on the 6-10th day of life. To prevent physiological jaundice, it is important that the newborn is adequately fed , preferably with breast milk, which speeds up the work of the intestines and thus accelerates the excretion of bilirubin from the body.
Non-physiological jaundice can be caused by preterm birth , excessive weight loss in newborns in the first days of life, inflammation (contributes to the destruction of red blood cells), hyperemia or polycythemia , as well as some rare diseases . If jaundice occurs during the first day of life, it may be due to Rh conflict (that is, Rh incompatibility) or a conflict in the AB0 blood type. Jaundice can also be caused by breast milk, this jaundice is called breast milk jaundice .
If jaundice occurs during the first day of life, it may be due to Rh conflict (that is, Rh incompatibility) or a conflict in the AB0 blood type. Jaundice can also be caused by breast milk, this jaundice is called breast milk jaundice .
Jaundice is not natural if it:
- occurs before the 24th hour of life;
- lasts more than 14 days in a newborn;
- lasts more than 21 days in a premature baby;
- flows in waves;
- observed dark urine and light feces.
Examinations
Photo 1. Percutaneous determination of bilirubin
A rapid skin test can be performed to detect jaundice early and when the above symptoms appear.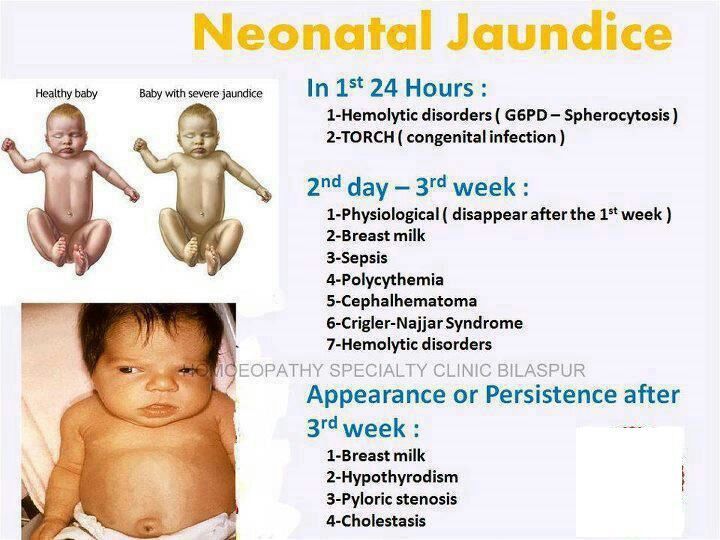 For this, an appropriate device is used, which measures the yellowness of the skin in the upper part of the child's ear. Measurement of yellowness of the skin is painless and fast for the child. If the results of measurements of bilirubin are in the range of 200-350 μmol / l, additional blood tests are carried out in the future. Measuring the level of bilirubin in the blood is important for assessing the condition of the child and making decisions about treatment.
For this, an appropriate device is used, which measures the yellowness of the skin in the upper part of the child's ear. Measurement of yellowness of the skin is painless and fast for the child. If the results of measurements of bilirubin are in the range of 200-350 μmol / l, additional blood tests are carried out in the future. Measuring the level of bilirubin in the blood is important for assessing the condition of the child and making decisions about treatment.
Blood test determines the level of bilirubin and hemoglobin in the blood, which are the basis for choosing a treatment method. In addition, the blood group of both the mother and the child is determined, and the presence of antibodies in the child's blood is determined. If necessary, additional studies are carried out.
Treatment options
Photo 2 Intensive phototherapy with upper and lower lamps
The first and most effective method of treatment is phototherapy , or phototherapy. Under the influence of blue light, a form of bilirubin is formed in the skin, which is easily excreted through the intestines and kidneys and is not toxic. In phototherapy, various lamps are used (upper or lower light, optical fiber or the so-called cocoon lamp, etc.). Depending on the type of phototherapy lamp, masks or paper goggles are used to protect the child's eyes from the light. During phototherapy, the child is undressed, so he can only wear a diaper and glasses. You can wear socks on your feet and gloves on your hands. The effect of phototherapy is manifested through the skin. Phototherapy is carried out until the level of bilirubin in the blood remains constantly low.
Under the influence of blue light, a form of bilirubin is formed in the skin, which is easily excreted through the intestines and kidneys and is not toxic. In phototherapy, various lamps are used (upper or lower light, optical fiber or the so-called cocoon lamp, etc.). Depending on the type of phototherapy lamp, masks or paper goggles are used to protect the child's eyes from the light. During phototherapy, the child is undressed, so he can only wear a diaper and glasses. You can wear socks on your feet and gloves on your hands. The effect of phototherapy is manifested through the skin. Phototherapy is carried out until the level of bilirubin in the blood remains constantly low.
It is important to feed your baby during phototherapy. Breastfeeding eight to ten times a day is preferred. Care should be taken to ensure that the child actively eats, if necessary, wake the child, keep him awake during feeding; if necessary, give expressed milk at the end of a feed to stimulate urination and defecation.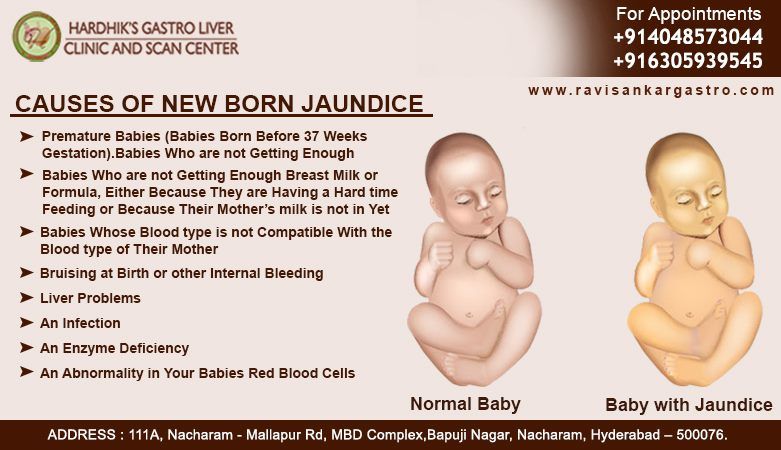 With timely treatment, jaundice usually resolves without problems.
With timely treatment, jaundice usually resolves without problems.
If the child's bilirubin level is very high or rises very quickly, phototherapy alone will not be enough. In this case, 9 is used for treatment.0005 exchange transfusion , which reduces both the amount of maternal antibodies and the amount of bilirubin in the baby's blood.
The prognosis of recovery depends on the level of bilirubin. Without treatment, the level of bilirubin rises above the acceptable level, and bilirubin begins to accumulate in the tissues. Bilirubin is toxic to the brain and can cause brain damage called kernicterus or bilirubin encephalopathy .
ITK1018
The information material was approved by the Health Care Quality Committee of East-Tallinn Central Hospital on 10.02.2021 (minutes no. 3-21).
Neonatal jaundice: to treat or not to treat
Jaundice in adults and older children is always associated with a dangerous disease. And indeed it is. And what is the reason for the appearance of jaundice in a newborn? We asked neonatologist Elena Zimina, head of the department of inpatient replacement technologies of the National Research Center for Children's Health of the Ministry of Health of Russia, about what this condition is, in what cases it can become dangerous for a newborn, and what parents should pay attention to.
And indeed it is. And what is the reason for the appearance of jaundice in a newborn? We asked neonatologist Elena Zimina, head of the department of inpatient replacement technologies of the National Research Center for Children's Health of the Ministry of Health of Russia, about what this condition is, in what cases it can become dangerous for a newborn, and what parents should pay attention to.
What is neonatal jaundice (NY) and why does it occur?
It is characterized by yellowness of the skin and sclera due to excessive accumulation of bilirubin in the body. In children under the age of 1 month, the digestive system improves. Specific processes take place in the bone marrow and hematopoietic system: fetal hemoglobin is destroyed and the so-called adult hemoglobin is formed. One of the breakdown products is the bile product bilirubin. It accumulates in the blood and turns the skin yellow. In most cases, HF proceeds physiologically and occurs due to the immaturity of the enzymatic systems of the newborn.
What are the types of VA
Physiological jaundice occurs in most babies and appears after 36 hours of life. This condition is not a disease and passes with time. It decreases by day 14 in a full-term newborn and by day 21 in a premature baby.
Jaundice that appears within the first 24 hours after birth is always a sign of pathology.
Pathological Jaundice is usually a sign of some other disease. It requires treatment prescribed by a doctor. With a very strong increase in the level of bilirubin, it penetrates into the nervous system. This can have a toxic effect, primarily on the vital nerve centers, the brain.
This condition is called "nuclear jaundice" or "bilirubin encephalopathy". A high level of bilirubin can cause damage to the central nervous system (CNS): lethargy, drowsiness, lethargy, inhibition of the sucking reflex - at an early stage. In the intermediate stage - an increase in muscle tone, increased irritability, often an increase in body temperature. In the advanced stage - CNS damage: convulsions, respiratory failure, coma. Nuclear jaundice irreversibly affects the central nervous system, hearing loss, gaze paralysis, mental retardation, cerebral palsy occur.
In the advanced stage - CNS damage: convulsions, respiratory failure, coma. Nuclear jaundice irreversibly affects the central nervous system, hearing loss, gaze paralysis, mental retardation, cerebral palsy occur.
Experts note:
- early jaundice - manifests itself in the first 36 hours of life;
- prolonged jaundice - persists for more than 14 days in full-term newborns and more than 21 days in premature newborns;
- late jaundice - appears after 7 days of life.
What factors assess the severity of jaundice
When examining a newborn, doctors evaluate: the color of the skin, sclera, mucous membranes, the stages of manifestation of icteric staining (according to the Cramer scale), the time of manifestation of jaundice, the general condition of the newborn (degree of activity, severity of reflexes, urination frequency and nature of urine, liver and spleen sizes, breastfeeding adequacy, laboratory parameters).
Newborn risk factors
1. Newborn born before 38 weeks of gestation.
Newborn born before 38 weeks of gestation.
2. The presence of hyperbilirubinemia in the previous child in the family.
3. Manifestation of jaundice in the first 24 hours of life.
How does the Rh factor affect the appearance and manifestations of WN
Incompatibility of the Rh factor of the mother and the unborn baby can provoke an Rh conflict, which after birth manifests itself as hemolytic disease of the newborn.
Rh-negative female organism detects the Rh-positive protein of the young organism as foreign. In this case, immune cells are secreted - antibodies.
Antibodies destroy the infant's red blood cells, releasing high levels of bilirubin, which severely affects the central nervous system of the young organism. Jaundice associated with Rhesus conflict in the blood type of mother and child is usually determined in the first days of a child's life.
Prevention
In order for the baby to grow strong and healthy, the expectant mother needs to maintain a healthy lifestyle during pregnancy. If a woman has a negative Rh factor, she needs to inform the doctor as fully as possible about possible previous pregnancies, abortions, blood transfusions and operations. In addition, it is important to determine the level of Rh antibodies in a pregnant woman and conduct an immunological examination of the future father. After the birth of a child, it is imperative to maintain adequate natural feeding.
If a woman has a negative Rh factor, she needs to inform the doctor as fully as possible about possible previous pregnancies, abortions, blood transfusions and operations. In addition, it is important to determine the level of Rh antibodies in a pregnant woman and conduct an immunological examination of the future father. After the birth of a child, it is imperative to maintain adequate natural feeding.
Treatment
A doctor can determine whether or not jaundice is dangerous for a baby by looking at the level of bilirubin in the baby's blood. This will allow you to develop a treatment strategy and understand whether the child needs specialist help or just wait.
One of the treatments for jaundice in newborns is phototherapy. These are blue lamps with a certain type of wave that are not dangerous for a child. They help bilirubin break down and leave the body faster.
Bilirubin leaves the body with stool. When the process of defecation in a child takes place regularly and in sufficient volume, then the level of bilirubin drops quite quickly.