Itchy skin pregnancy 1st trimester
Itching and intrahepatic cholestasis of pregnancy
Itching is common in pregnancy. Usually it's thought to be caused by raised levels of certain chemicals in the blood, such as hormones.
Later, as your bump grows, the skin of your tummy (abdomen) is stretched and this may also feel itchy.
However, itching can be a symptom of a liver condition called intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC).
ICP needs medical attention. It affects 1 in 140 pregnant women in the UK.
Symptoms of ICP
The main symptom is itching, usually without a rash. For many women with ICP, the itching is often:
- more noticeable on the hands and feet, but can be all over the body
- worse at night
Other symptoms can include:
- dark urine
- pale poo
- yellowing of the skin and whites of the eyes (jaundice), but this is less common
Symptoms of ICP typically start from around 30 weeks of pregnancy, but it's possible to develop the condition as early as 8 weeks.
Non-urgent advice: Call your midwife or GP if you have itching that's:
- mild or distressing, possibly worse at night
- anywhere on your body, but may be worse on the palms of your hands and soles of your feet
Feeling itchy like this can be a sign of ICP and needs to be checked.
Mild itching
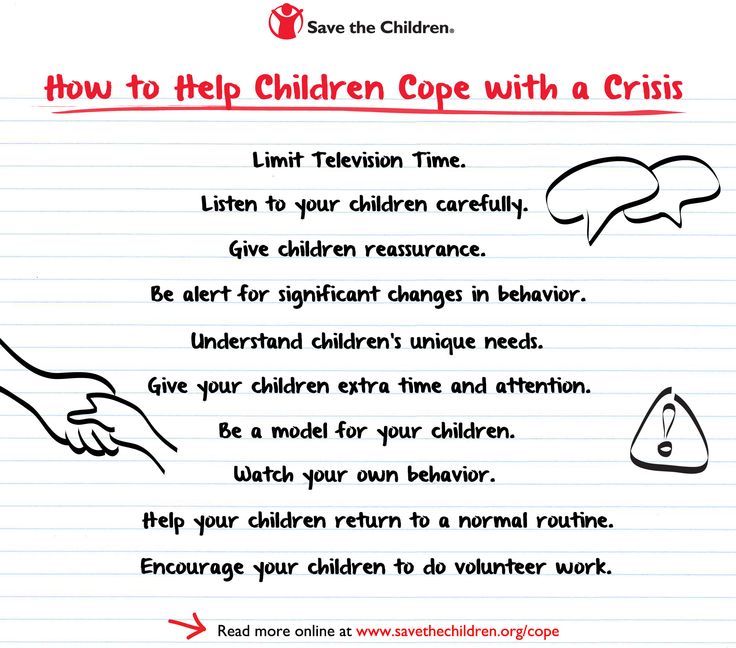
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation.
You may also want to avoid synthetic materials and opt for natural ones, such as cotton, instead. These are "breathable" and allow the air to circulate close to your skin.
You may find having a cool bath or applying lotion or moisturiser can help soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using unperfumed lotion or soap.
Mild itching is not usually harmful to you or your baby, but it can sometimes be a sign of a more serious condition, particularly if you notice it more in the evenings or at night.
Let your midwife or doctor know if you are experiencing itching so they can decide whether you need to have any further investigations.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a potentially serious liver disorder that can develop in pregnancy.
Normally, bile acids flow from your liver to your gut to help you digest food.
In ICP, the bile acids do not flow properly and build up in your body instead. There's no cure for ICP, but it should go once you've had your baby.
ICP seems to run in families, but it can happen even if there is no family history. It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
If you have had ICP in a previous pregnancy, you have a high chance of developing it again in another pregnancy.
Some studies have found that babies whose mothers have ICP have a higher chance of being born prematurely or stillborn.
Because of the link with stillbirth, you may be offered induction of labour. This could be any time from 35 weeks, depending on the level of bile acids in your blood.
If you have ICP, you will probably be advised to give birth in hospital under a consultant-led maternity team.
Diagnosis and treatment of ICPICP is diagnosed by excluding other causes of the itch. Your doctor will probably talk to you about your medical and family history and order a variety of blood tests.
These will include tests to check your liver function (LFT) and measure your bile acid levels (BA).
If you are diagnosed with ICP, you will have regular liver function tests so your doctor can monitor your condition.
There is no agreed guideline on how often these tests should happen, but the Royal College of Obstetricians & Gynaecologists (RCOG) and the British Liver Trust advise weekly tests.
ICP Support, the UK's largest research group investigating ICP, also recommends weekly bile acid measurements. These readings help doctors recommend when your baby should be born.
If your LFTs and bile acids are normal and you continue to have severe itching, the blood tests should be repeated every week or 2, to keep an eye on them.
Creams and medicines for ICPCreams, such as aqueous cream with menthol, are safe to use in pregnancy and can provide some relief from itching.
There are some medicines, such as ursodeoxycholic acid (UDCA), that help reduce bile acids and ease itching.
UDCA is considered safe to take in pregnancy, although it is prescribed on what is known as an "informed consent" basis as it has not been properly tested in pregnancy.
You may also be offered a vitamin K supplement. This is because ICP can affect your absorption of vitamin K, which is important for healthy blood clotting.
Most experts on ICP only prescribe vitamin K if the mother-to-be reports pale stools, has a known blood clotting problem, or has very severe ICP from early in pregnancy.
If you are diagnosed with ICP, your midwife and doctor will discuss your health and your options with you.
Further information
The Royal College of Obstetricians & Gynaecologists (RCOG) has more information about obstetric cholestasis, including what it means for you and your baby, and the treatment that's available.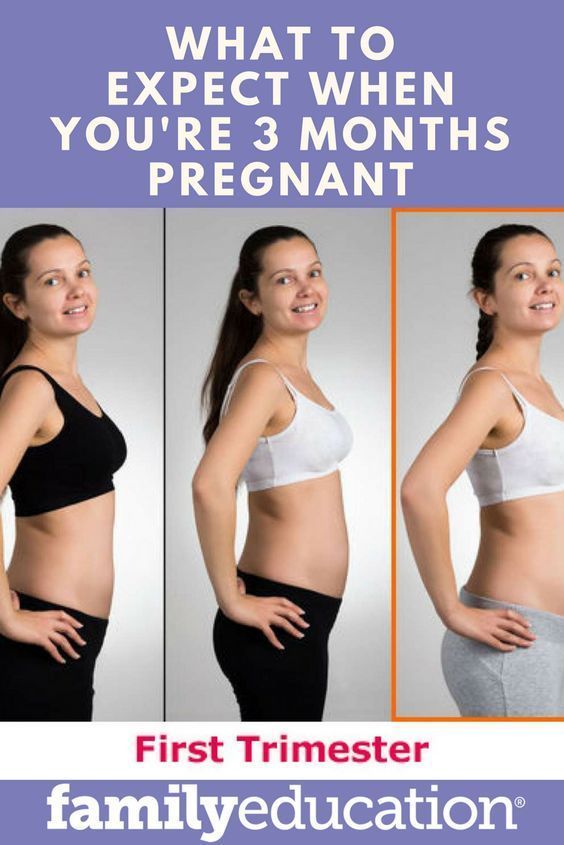 You can also get information about ICP from the British Liver Trust.
You can also get information about ICP from the British Liver Trust.
The charity ICP Support provides information about ICP. You can also watch their video about ICP featuring mums and clinical experts.
Community content from HealthUnlockedItching during pregnancy | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
Mild itching is common in pregnancy because of the increased blood supply to the skin. As your pregnancy progresses and as your baby grows, the skin of your abdomen is stretched and this may also feel itchy.
Mild itching is usually nothing to worry about, but if the itching becomes severe it can be a sign of a serious liver condition called obstetric cholestasis. This affects fewer than 1 in 100 pregnant women, but needs medical attention.
This affects fewer than 1 in 100 pregnant women, but needs medical attention.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation. You may also want to avoid synthetic materials and choose natural fabrics such as cotton that allow the air to circulate close to your skin. You may find that having a cool bath or applying lotion or moisturiser can help to soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using plain lotion or soap.
Serious itching: obstetric cholestasis
If you’re worried about your itching, or if you have severe itching, it’s important to see your midwife or doctor.
Obstetric cholestasis (OC), also called intrahepatic cholestasis of pregnancy, is a serious liver disorder that affects a small number of pregnant women, usually in the last 3 months of pregnancy.
Causes of obstetric cholestasis
The cause of OC is unclear, but it’s thought the rise of pregnancy hormones later in pregnancy may slow the normal flow of bile — the digestive fluid made in the liver that helps your digestive system break down fats. In OC, bile salts build up rather than leaving the liver, eventually entering the bloodstream, which can make you feel itchy.
In OC, bile salts build up rather than leaving the liver, eventually entering the bloodstream, which can make you feel itchy.
OC seems to run in families, although it can occur with no family history. It is also more common in women of Indian and Pakistani origin. If you have had OC in a previous pregnancy, you're more likely to develop it again in a subsequent pregnancy.
Babies of women with OC are more likely to be born prematurely or to be stillborn, or to have lung problems from breathing in meconium. Because of these complications, your doctor may consider inducing labour before you are due.
Symptoms of obstetric cholestasis
The classic symptom of OC is itching without rash, usually on the palms and soles of the feet, but it may be more widespread. The itching can be non-stop or unbearable, and worse at night.
Other symptoms include dark urine, jaundice (yellowing of the skin and whites of the eyes), and pale bowel movements (poo).
The itchiness usually goes away within a few days after giving birth.
Treatment of obstetric cholestasis
OC is diagnosed through taking a medical and family history, and blood tests that check your liver function (liver functions tests — LFTs). Once OC is diagnosed, you will have regular LFTs until your baby is born, so that your doctor can monitor your condition.
Creams, such as calamine lotion, are safe to use in pregnancy and can provide some relief from itching. Your doctor may prescribe a medication to reduce bile salts and ease itching.
OC can affect your absorption of vitamin K, which is important for healthy blood clotting so you may be offered a vitamin K supplement.
If you are diagnosed with OC, your midwife and doctor will discuss your health and your options with you.
Sources:
Mayo Clinic (Cholestasis of pregnancy), NSW Health (Having a baby), Royal Women’s Hospital (Common concerns in early pregnancy), SA Health Department (Clinical guideline obstetric cholestasis), Women's and Children's Health Network (Itching in pregnancy), King Edward Memorial Hospital (Cholestasis in pregnancy - clinical guidelines)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood.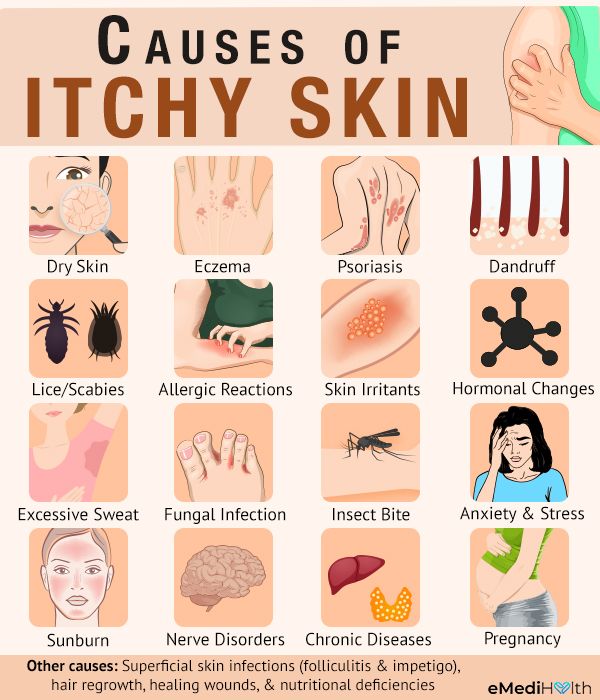 This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Why does the skin itch during pregnancy?
Itching during pregnancy is not very common. In most cases, the skin begins to itch unbearably (as with mosquito bites) in the late evening, which can provoke insomnia and negatively affect the mood of a woman as a whole. Itching usually does not affect the baby and goes away on its own after birth. However, it is recommended to consult with a gynecologist and dermatologist.
Pregnancy, a state of profound physiological and hormonal changes, is associated with a whole spectrum of changes in the skin and its appendages.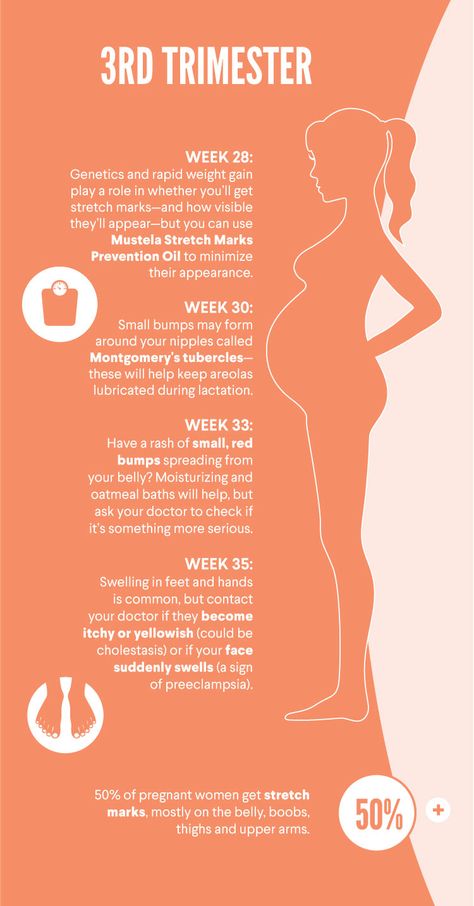 Over 90% of pregnant women experience one or more forms of skin changes. Up to 20% of women experience itching during pregnancy.
Over 90% of pregnant women experience one or more forms of skin changes. Up to 20% of women experience itching during pregnancy.
Specific dermatoses of pregnancy - skin lesions that occur during pregnancy and disappear after childbirth. Itching of pregnancy is a skin condition of pregnant women, manifested by itching and only secondary rashes in the form of excoriations with or without signs of cholestasis.
Pruritus pruritus and intrahepatic cholestasis of pregnancy are terms used interchangeably in the medical literature, where the term pruritus gravidarum describes patients with pruritus in the absence of primary skin changes.
To reiterate, there is no specific rash associated with pruritus pruritus, but many patients will have signs of scratching to try and alleviate the symptoms of pruritus. Itching can vary from mild to severe and most commonly affects the palms and soles. Symptoms may get worse at night. It is important for clinicians to recognize pruritus gravidarum because these patients should be evaluated for intrahepatic cholestasis of pregnancy.
Most obstetricians will experience intrahepatic cholestasis of pregnancy during their career, as it is the most common liver disease associated with pregnancy. If patients are diagnosed with intrahepatic cholestasis of pregnancy, this information may change the treatment plan, timing of delivery, antenatal fetal assessment, and management of future pregnancies.
What causes itching?
No definitive explanation for pruritus in pregnancy has yet been found. It is believed that hormonal and genetic factors have a significant influence on its development.
However, itching during pregnancy is most often caused by impaired liver function: the production and secretion of bile, a general increase in the level of bilirubin in the blood. This happens as a result of a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to the pressure of the fetus on the bile ducts.
A large amount of fatty acids formed with the blood flow enters the woman's skin and irritates the nerve endings, causing unbearable itching. Similar conditions associated with stagnation of bile in the body can occur in the third trimester of pregnancy. Itching can also sometimes be accompanied by dangerous diseases such as diabetes.
Similar conditions associated with stagnation of bile in the body can occur in the third trimester of pregnancy. Itching can also sometimes be accompanied by dangerous diseases such as diabetes.
The condition usually begins in the third trimester, when hormone levels are highest, and ends in childbirth. It may also return with successive pregnancies, indicating that the condition is caused by a hormonal imbalance.
Pregnancy itch is a condition that affects people differently depending on their ethnicity and location. This ethnic and geographic grouping of cases suggests that the disease has a hereditary basis.
Heterozygous mutations in the MDR3 gene, also known as ABCB4, are associated with the etiology of the disease. The canalicular transport protein of phosphatidylcholine translocase is encoded by the MDR3 gene.
A personal or family history of intrahepatic cholestasis during a previous pregnancy, multiple pregnancies, chronic hepatitis C, and advanced maternal age are all risk factors for intrahepatic cholestasis during pregnancy. In pregnancy pruritus, skin biopsy findings are often nonspecific; epidermal ulceration is found as a result of excoriations.
In pregnancy pruritus, skin biopsy findings are often nonspecific; epidermal ulceration is found as a result of excoriations.
Who is affected?
Pregnancy pruritus is commonly seen in women with chronic biliary tract disease and elevated blood cholesterol levels. These future mothers should regularly (at least once a month) undergo a biochemical blood test to exclude toxic effects on liver cells.
How can you control this?
A pregnant woman should talk to her gynecologist about discomfort associated with itching. In some cases, itching can be a sign of the onset of a serious illness, such as hepatitis. The doctor will conduct the necessary tests.
If the physical examination shows that itching is not a problem, the discomfort can often be relieved by eating a cholesterol-lowering diet and limiting fatty, spicy, and salty foods that impair liver function. secretion of bile, as well as drinking plenty of water - this is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic (cholagogue) drugs suitable for pregnant women.
If the diet does not help, the doctor may prescribe choleretic (cholagogue) drugs suitable for pregnant women.
It is important to find the cause of the irritating itching by excluding a whole group of skin diseases that can occur during pregnancy.
Itching on the abdomen and chest
This type of itching should be considered separately. The skin on the abdomen or chest itches in the second and third trimesters due to stretching, as these parts of the body increase in size during pregnancy. In this case, it is very important not to scratch the skin.
This will cause stretch marks, which, unlike itching, will not disappear after childbirth. You should regularly use moisturizing creams and special formulas against stretch marks, light massage of the chest and abdomen with circular movements of the fingers, do not take hot showers.
Epidemiology
The prevalence of pruritus during pregnancy varies worldwide. Incidence rates of 1% to 27. 6% have been reported. In Chilean women of Araucanian Indian origin, the incidence rate was 22.1 percent, with prevalence increasing in direct proportion to the degree of "ethnic purity". In European countries, the incidence rate ranges from 0.5 to 1.5 percent, with the highest rates being seen in Scandinavian women.
6% have been reported. In Chilean women of Araucanian Indian origin, the incidence rate was 22.1 percent, with prevalence increasing in direct proportion to the degree of "ethnic purity". In European countries, the incidence rate ranges from 0.5 to 1.5 percent, with the highest rates being seen in Scandinavian women.
In the United States, the Hispanic population in Los Angeles had the highest incidence rate at 5.6 percent and Connecticut at 0.32 percent. The frequency ranged from 1.2 to 1.5 percent in Indian-Asian and Pakistani-Asian women. There were more cases of itching in winter than in warm weather.
Although dry skin is the most common cause, it can also indicate an underlying problem with pregnancy. dermatoses of pregnancy include pruritic urticarial papules and plaques of pregnancy (PUPPP), intrahepatic cholestasis of pregnancy (ICP), pemphigoid of pregnancy (PH), and atopic rash of pregnancy.
Pathophysiology
Itching develops as a result of an increase in the level of bile acids in the skin and blood serum. The exact process by which bile acids cause itching is not known. Solubilization of lipid cell membranes with bile salts can lead to the release of histamine and proteolytic enzymes due to their detergent properties. Itching can be caused by the release of histamine and other enzymes that activate free nerve endings.
The exact process by which bile acids cause itching is not known. Solubilization of lipid cell membranes with bile salts can lead to the release of histamine and proteolytic enzymes due to their detergent properties. Itching can be caused by the release of histamine and other enzymes that activate free nerve endings.
Bile acid levels rise as a result of hormonal and hereditary causes. Hormones such as estrogen and progesterone, which increase during pregnancy, have a cholestatic effect and reduce the excretory function of the liver. Mutations in the MDR3 gene can potentially lead to cholestasis.
Signs and symptoms
The most common symptom of itching during pregnancy is itching, an unpleasant sensation that makes you want to scratch. Itching usually begins in the late second to early third trimester, but itching has been reported as early as the eighth week of pregnancy. In at least half of the women, the onset of symptoms coincided with the onset of a urinary tract infection, according to the study.
Itching is more often episodic at first, then becomes continuous. Itching begins on the abdomen and then spreads to the whole trunk, palms and soles. Itching can range from mild to severe, and people experience the most discomfort at night.
In only about 20% of cases, jaundice appears after itching has been present for at least four weeks. Patients with jaundice may develop steatorrhea, leading to malabsorption of fats. Symptoms persist throughout pregnancy, disappear after childbirth, and reappear in subsequent pregnancies.
In case of itching of pregnant women, the examination does not reveal primary lesions. In fact, if any primary lesions are present, the diagnosis of pruritus gravidarum is ruled out. The most common findings on examination are irritation and scratches caused by itching.
Diagnosis
Because pruritus without primary skin lesions is a key feature of pruritus in pregnancy, a comprehensive history and physical examination are essential.
An increase in the concentration of bile acids in the blood serum is an important laboratory sign of itching in pregnancy. This is usually the initial and only erroneous test result. Itching causes an increase in the level of bile acids in the blood serum. The choline/chenodeoxycholic ratio is skewed because cholic acid levels rise faster than chenodeoxycholic acid levels. In women with pruritus of pregnancy, the choline/chenodeoxycholine ratio was 3.4 compared to 1.1 in pregnant women without the disease.
This disease differs from viral hepatitis by an increase in serum aminotransferases not exceeding 1000 IU/l. Due to placental isoenzyme synthesis, alkaline phosphate levels, although high, are not specific to pruritus pruritus. The presence of hyperbilirubinemia suggests the presence of intrahepatic cholestasis associated with pregnancy.
There is no pathology on ultrasound of the liver. Cholestasis without inflammation may be detected histologically, but a liver biopsy is not required to make the diagnosis.
Management of pruritus
The aim of therapy should be to relieve symptoms as well as to prevent adverse effects on the fetus. Calming, antipruritic agents such as calamine lotion, soothing oatmeal baths, menthol in water cream, and mild steroid ointments may be used to treat cases with mild symptoms. Patients should be reassured and asked to stay away from stressful situations and uncomfortable clothing. Rest and a low-fat diet should be encouraged.
Patients should also be informed about the transient nature of the disease and the rapid remission of their symptoms after delivery. First generation antihistamines such as diphenhydramine, chlorpheniramine, pheniramine, or tripelennamine are safe to use during pregnancy and can be taken as a supplement.
Ursodeoxycholic acid may be used to treat severe or unresponsive pruritus associated with biochemical disorders (UDCA). By replacing other hydrophobic ions in the enterohepatic circulation, UDCA, a hydrophilic bile acid, eliminates them. At a dosage of 15mg/kg/day, UDCA helps reduce itching and also corrects metabolic imbalances.
At a dosage of 15mg/kg/day, UDCA helps reduce itching and also corrects metabolic imbalances.
UDCA is non-teratogenic and more effective than other modern drugs. It is very important to remember that although UDCA preparations may help the mother's symptoms, they do not reduce the risk to the fetus.
Colestyramine, S-adenosyl-D-methionine, oral corticosteroids, nonerythemogenic UV radiation, and phenobarbital are some of the other drugs that may be used. Although these drugs are more commonly used to treat intrahepatic cholestasis of pregnancy, they are worth mentioning here because pruritus gravidarum and intrahepatic cholestasis of pregnancy have much in common.
In the setting of intrahepatic cholestasis during pregnancy, there is an increased risk of preterm birth, meconium staining of amniotic fluid, neonatal depression, respiratory distress syndrome, and stillbirth, among others.
The American College of Obstetricians and Gynecologists (ACOG) recommends prenatal surveillance with non-stress testing of the fetus after determining fetal viability, beginning at diagnosis of cholestasis and continuing once or twice a week until birth to reduce the risk of adverse outcomes.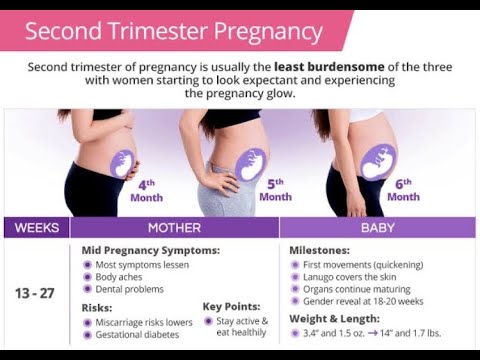
According to ACOG, total serum bile acids affect the optimal timing of labor. If the total bile acid level is less than 100 µmol/L, delivery should take place between 36 and 39 weeks of gestation. Delivery at 36 0/7 is indicated for total bile acids of 100 µmol/l or greater. If a patient is diagnosed with cholestasis after the optimal gestational age for delivery, delivery is recommended at the time of diagnosis.
Differential
Because pruritus is such a common symptom of pregnancy, it is important to rule out other possible causes:
- Specific dermatoses of pregnancy
- Atopic dermatitis
- Pregnancy pemphigoid
- Erythema multiforme
- Polymorphic eruptions during pregnancy
- Atopic rash during pregnancy
- Pustular psoriasis of pregnancy
- Scabies
- Pediculosis
- Neurodermatitis
- Contact dermatitis
- Drug eruptions.
Other causes of liver dysfunction should be ruled out if the patient has concomitant liver dysfunction: viral hepatitis, acute fatty liver of pregnancy, HELLP syndrome (hemolysis, elevated liver enzymes and low platelets), and drug-induced liver injury.
Intrahepatic cholestasis of pregnancy
Although ICP is a pruritic disease of pregnancy that mainly involves secondary skin changes, it is classified as dermatosis of pregnancy because early detection is critical to reduce the risk of adverse fetal outcomes.
Idiopathic jaundice of pregnancy, obstetric cholestasis, and pruritus gravidarum are all terms for intrahepatic cholestasis of pregnancy. The outflow of hepatic bile is disturbed during pregnancy, which causes it. ICP is common in North America, affecting 0.5 to 1% of the population, but is more common in Scandinavia and South America, with the highest incidence in Chile (15 to 28%). It tends to be inherited and recur in subsequent pregnancies.
Clinical picture
Pregnancy-related intrahepatic cholestasis presents in the second or third trimester with a rapid onset of severe itching that begins on the palms and soles and soon spreads throughout the body. Itching continues throughout pregnancy and is most pronounced at night.
Scratches cause secondary lesions that include linear excoriations and excoriated papules. Associated extrahepatic cholestasis causes jaundice in about 10% of patients, which is usually accompanied by dark urine and clayey stools. When malabsorption of fat-soluble vitamins, especially vitamin K, these individuals are at increased risk of developing steatorrhea, which can lead to bleeding problems and gallstones.
Pathophysiology
Intrahepatic cholestasis associated with pregnancy is hormonally induced cholestasis. It manifests itself in genetically predisposed women in late pregnancy who have a deficiency in bile acid excretion, which leads to an increase in the level of bile acids in the blood.
This causes severe itching in the mother, and since toxic bile acids can enter the fetal circulation, the fetus may suffer as a result of severe placental anoxia and cardiac depression. In half of the cases, the disease has a family history, cases with a family component are more severe.
Diagnosis
The typical symptom of itching of the palms and soles, not accompanied by a rash, is usually used to make the diagnosis. To confirm the diagnosis, an increase in the total level of bile acids in the blood serum can be used. Levels of total bile acids in the blood up to 11.0 mol/l in the third trimester are considered normal in a healthy pregnancy.
Blood levels of total bile acids greater than 40.0 mol/l in women with ICP are associated with a higher risk of adverse fetal outcome. There may also be a slight increase in the activity of hepatic transaminases, such as aspartate aminotransferase and alanine aminotransferase; this increase may appear several weeks after the onset of itching.
Steatorrhea may also occur in vitamin K deficiency. Close monitoring of prothrombin time may be required. Liver ultrasound and serology may be needed to rule out other conditions, such as gallstones and viral hepatitis.
Management of patients with intrahepatic cholestasis
The goal of therapy is to reduce the level of bile acids in the blood.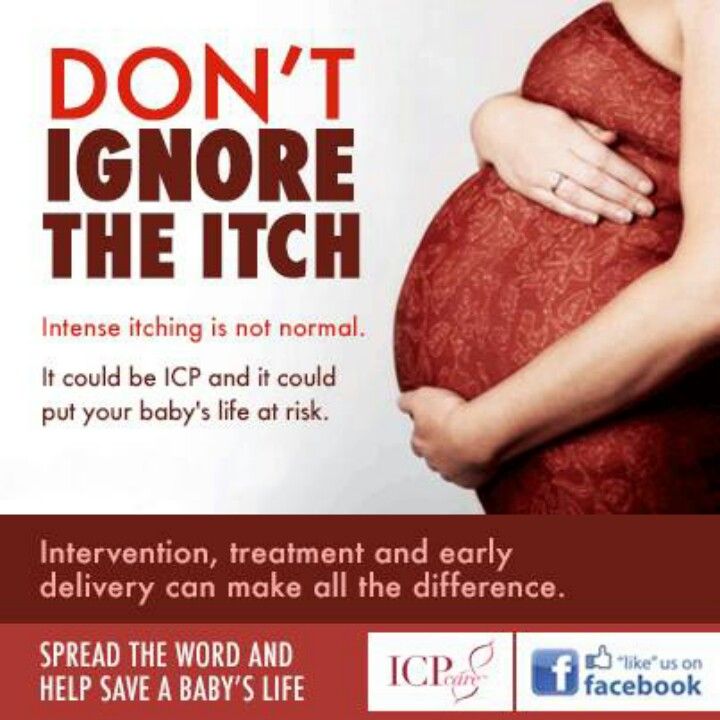 Ursodeoxycholic acid is the preferred therapy because it reduces maternal pruritus, lowers hepatic transaminases and bile acids, and may reduce the risk of adverse fetal outcomes, however the latter benefit is controversial. Until the birth of the child, the daily dose is 15 mg/kg or 1 g.
Ursodeoxycholic acid is the preferred therapy because it reduces maternal pruritus, lowers hepatic transaminases and bile acids, and may reduce the risk of adverse fetal outcomes, however the latter benefit is controversial. Until the birth of the child, the daily dose is 15 mg/kg or 1 g.
Before treatment with ursodeoxycholic acid, cholestyramine was used to treat ICP. This medicine, on the other hand, can cause vitamin K deficiency, which may already be present in this condition. Antihistamines may also help the mother's symptoms.
Stillbirths are more common between 37 and 39 weeks, so planned delivery between 36 and 38 weeks is recommended. According to some publications, induction of labor at 37 weeks is recommended only in situations of severe ICP (defined as total serum bile acids above 40 mol/L).
Prognosis
The prognosis for the mother is usually good. Itching usually goes away on its own within a few days or weeks after delivery, but may reappear with subsequent pregnancies or when taking hormonal contraception. There is a higher risk of intrapartum and postpartum hemorrhage if you have jaundice and vitamin K deficiency.
There is a higher risk of intrapartum and postpartum hemorrhage if you have jaundice and vitamin K deficiency.
This syndrome has been associated with fetal complications such as preterm birth, meconium in the amniotic fluid, fetal discomfort, and fetal death. It is important to note that some have documented that fetal death in ICP occurs as a result of rapid onset, even if the fetal heart rate was previously normal.
Indeed, there is little evidence that intensive prenatal monitoring can prevent fetal death in ICP situations. As a result, it is proposed to induce labor between 36 and 38 weeks. The need for early diagnosis, accurate treatment, and careful obstetric follow-up cannot be overstated. In ambiguous or severe situations, a gastroenterologist should be consulted.
Pregnancy pemphigoid
Pregnancy pemphigoid is a self-limiting autoimmune bullous disease that appears after the 20th week of pregnancy and may occur only after childbirth.
Herpes gestationis is the name given to PG in the past due to the characteristic development of "creeping" blisters. Milton coined the phrase in 1872. This phrase, however, can be misleading because the disease has nothing to do with the herpes virus and is now known as pregnancy pemphigoid. This is a fairly rare disease that affects about 1 in 10,000 pregnant women.
Milton coined the phrase in 1872. This phrase, however, can be misleading because the disease has nothing to do with the herpes virus and is now known as pregnancy pemphigoid. This is a fairly rare disease that affects about 1 in 10,000 pregnant women.
Clinical presentation
Skin lesions in pregnancy pemphigoid may be preceded by acute itching. Itchy, urticarial, erythematous papules and plaques around the umbilicus and extremities are the first signs of a rash. Ulcers become firm blisters as the disease progresses.
Mucosal involvement occurs in about 20% of cases, while the face, palms and soles remain unaffected. PH often worsens during childbirth, but then goes away on its own.
Diagnosis
Diagnosis requires skin biopsy. In the diagnosis of PH, direct immunofluorescence of the skin around lesions is the gold standard. It shows linear deposition of complement C3 along the dermoepidermal junction. The results of a biopsy in other dermatoses of pregnant women do not give such results.
PUPPP is the most common differential diagnosis, especially early in the condition, before hard blisters appear. In cases of suspected PUPPP with unusual and severe manifestations that do not respond to standard therapy, a skin biopsy is recommended.
Prognosis
Exacerbations and remissions define the normal course of the disease throughout pregnancy, with frequent recovery in late pregnancy, followed by an exacerbation at birth. Lesions usually disappear within a few weeks or months. It tends to recur at an earlier gestational age and with increasing severity in successive pregnancies. It can also happen during menstruation or when using hormonal contraception. Other autoimmune conditions, including Graves' disease, are at higher risk.
Pregnancy with BE is considered high risk because there is an association between this condition and a higher chance of adverse fetal outcomes such as preterm birth and low birth weight. About 10% of newborns may suffer from small skin lesions that spontaneously heal within days or weeks due to passive transfer of maternal autoantibodies to the fetus.
Management of pemphigoid patients
The goal of treatment is to reduce itching and prevent blistering. Topical corticosteroids in combination with oral antihistamines may be adequate in cases of mild pre-blistering. Systemic steroids, such as prednisone at a dose of 20 to 60 mg per day, are required in all other cases. To avoid exacerbation during childbirth, the dose of prednisolone should be increased gradually.
Pregnancy pruritus prognosis
Pregnancy pruritus has a favorable prognosis, symptoms quickly disappear after childbirth. Itching and jaundice usually resolve within 24 to 48 hours after birth, but may last up to four weeks. Bile acid levels return to normal after 4-6 weeks. In 40-70% of women, itching of pregnancy may recur in subsequent pregnancies. In some cases, estrogen-containing drugs can cause relapses.
Complications of pruritus in pregnancy
Complications of mother and fetus differ. The mother may experience malabsorption or postpartum hemorrhage as a result of low vitamin K levels caused by liver problems. According to the study, gallbladder diseases, including gallstones, are more common in these patients.
According to the study, gallbladder diseases, including gallstones, are more common in these patients.
Prematurity, intrauterine asphyxia, meconium staining of amniotic fluid, and low birth weight are all risks to the fetus. Bile acid levels of 40 µmol/L or higher have been shown to be statistically significant in increasing adverse fetal outcomes in the study. It is believed that placental anoxia causes problems with the fetus.
Home remedies for itching
- Olive oil
Any type of rash can cause significant damage to the skin. Olive oil is a great choice for both healing and renewing skin after a rash. Irritant dermatitis, diaper rash, and allergic contact dermatitis benefit from the anti-inflammatory and antibacterial properties of olive oil.
You can use olive oil to massage the rash with honey or by itself. You can also add a pinch of turmeric powder. It is a powerful antibacterial and anti-inflammatory agent. Mix it with olive oil and apply it on the rash several times a day.
Mix it with olive oil and apply it on the rash several times a day.
- Coconut oil
Coconut oil is a fantastic replacement for olive oil for moisturizing and soothing rashes. Coconut oil also protects the skin. Coconut oil, unlike olive oil, has a thick viscosity similar to that of most diaper rash creams. Virgin coconut oil is recommended because it retains the antibacterial and anti-inflammatory properties of raw coconut oil.
- Cold compress
A simple but effective remedy for a rash is a cold compress. This helps relieve the annoying symptoms of the rash as well as reduce its intensity. Heat rashes respond best to cold compresses, which minimize swelling and irritation.
- Oatmeal bath
Oatmeal bath has even been certified by the US Food and Drug Administration as a skin protectant. Oatmeal has anti-inflammatory properties as well as soothing properties.
Conclusions
When itching occurs during pregnancy, a detailed history and physical examination is required. Laboratory tests, such as liver transaminase levels, serum bile acid levels, and, in certain situations, skin biopsy may be required to determine the most likely diagnosis. Dermatoses of pregnancy should be included in the differential diagnosis of pruritus and treated accordingly.
Since some of these disorders are associated with an increased risk of adverse fetal outcome, a correct diagnosis is required. Therapy for the disorders listed above is considered safe during pregnancy.
Patients should be instructed to minimize scratching to avoid subsequent lesions and hyperpigmentation. When patients' symptoms become unmanageable and cause concern, they should be asked to see a doctor. Patients should be comforted by their prognosis and the danger to the fetus. These people should also be advised to avoid or take estrogen-containing oral contraceptives at the lowest possible doses.