Clear chunky discharge
Clear Mucus Discharge | The Colors & Meanings of Vaginal Discharge
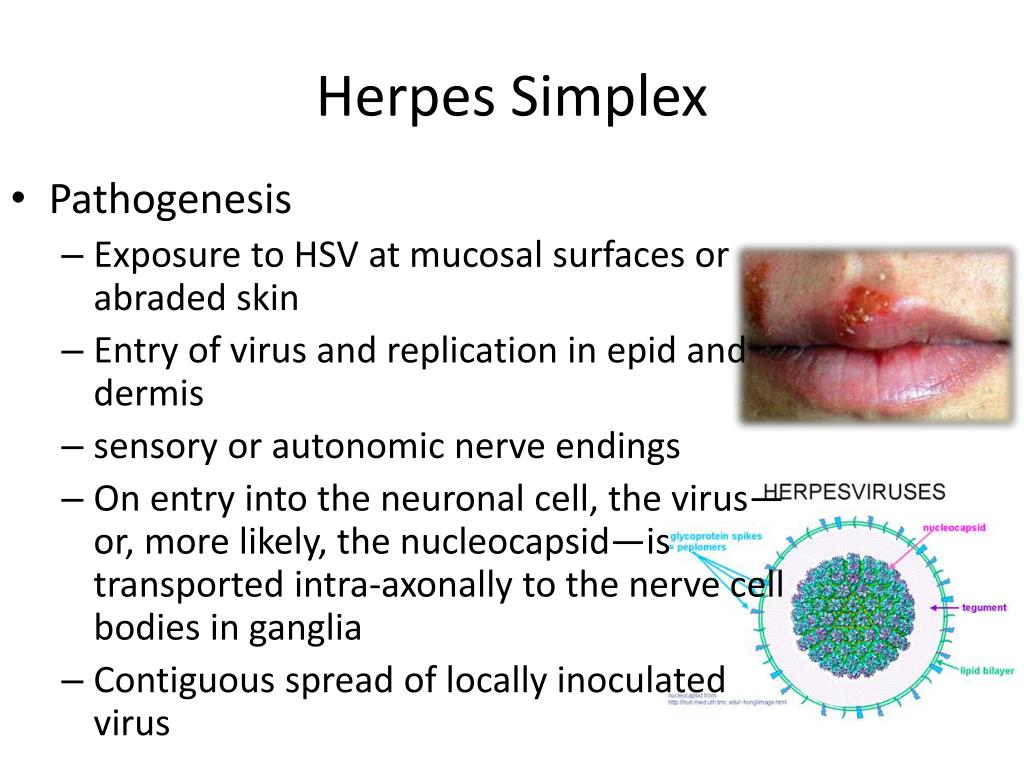
Yeast infection
A vaginal yeast infection, also called genital/vulvovaginal candidiasis, is actually caused by the fungus Candida albicans and is very common. The organism is a normal inhabitant of the mouth, gastrointestinal tract, and vagina.
Antibiotics can kill off the healthy bacteria in the vagina, allowing overgrowth of the fungus. Women who are pregnant, on the birth control pill, or diabetic are more prone to yeast infections, as are those who have weakened immune systems. It can also be transmitted through sex or through mouth-to-genital contact.
Symptoms include itching, burning, pain, and soreness inside the vagina and on the external tissues (the vulva,) and a thick, white vaginal discharge.
If not treated, the yeast infection can become "complicated," severe, and difficult to cure.
Most yeast infections are diagnosed simply through the patient's description of symptoms. Recurrent infections may be diagnosed through pelvic examination and vaginal swab.
Treatment often is just an over-the-counter cream, though oral anti-fungal medications are sometimes prescribed.
Vaginal trichomonas infection
Trichomonas vaginalis infection (or "Trichomoniasis" or "trich") is a common sexually transmitted disease caused by a parasite of the same name. It affects over 3 million people per year, but only about 30% have any symptoms.
You should go see your primary care doctor in the coming days. He or she may order a number of tests to identify if the bug is actually the cause of your symptoms. Treatment involves prescription metronidazole or tinidazole.
Symptoms of menopause
Menopause, or "change of life," refers to the time when a woman no longer has menstrual cycles and can no longer bear children.
It is a normal occurrence and usual happens between ages 45 to 55. Menopause can be artificially induced by surgical removal of both ovaries, and by chemotherapy and/or radiation therapy for cancer.
Symptoms usually begin many months before periods actually stop. There will be irregular periods, vaginal dryness, hot flashes, weight gain from slower metabolism, and dry skin.
If not treated, some symptoms may affect quality of life. Hot flashes and hormonal imbalances can disrupt sleep, sexual function, and emotional health.
At menopause, risks of heart disease, osteoporosis, and urinary incontinence increase. Because periods can become irregular while pregnancy is still possible, testing is advisable before any medical treatment is done.
Menopause is diagnosed when an entire year has gone by without the woman experiencing a menstrual period. Blood testing for hormone levels can confirm menopause.
Treatment can be done for any troublesome symptoms, including hormone replacement therapy to ease hot flashes.
Pelvic inflammatory disease
Pelvic inflammatory disease, or PID, is the general term for a bacterial infection of a woman's reproductive organs.
PID is most often a complication of a sexually transmitted disease (STD) such as gonorrhea or chlamydia. However, it is possible to get PID from other causes.
Any woman can be affected. It is most often found in sexually active women under age 25, especially those who have had PID before, have multiple partners, and/or douche frequently.
Symptoms include fever, lower abdominal pain, foul-smelling vaginal discharge, pain and/or bleeding during sex, and pain on urination.
Untreated PID can cause infertility due to damaged tissue in the reproductive tract, as well as chronic pelvic and abdominal pain. Unprotected sex partners will be infected as well.
Diagnosis is made through symptoms, pelvic examination, vaginal and cervical swabs, and urine tests.
Treatment is with a course of antibiotics. Be sure to finish all of the medication as directed, even when you begin feeling better.
To prevent PID, have all partners (male or female) tested for STDs and avoid unprotected sexual contact.
Rarity: Common
Top Symptoms: fever, abdominal pain or unusual vaginal discharge, vaginal discharge, nausea or vomiting, vaginal bleeding, pelvis pain
Symptoms that always occur with pelvic inflammatory disease:fever, abdominal pain or unusual vaginal discharge
Urgency: In-person visit
Ovulation pain (mittelschmerz) or midcycle spotting
Mittelschmerz is a German word that translates as "middle pain." It refers to the normal discomfort sometimes felt by women during ovulation, which is at the midpoint of the menstrual cycle.
Each month, one of the two ovaries forms a follicle that holds an egg cell. The pain occurs when the follicle ruptures and releases the egg.
This is a dull, cramping sensation that may begin suddenly in only one side of the lower abdomen. In a few cases, there may be vaginal spotting. Mittelschmerz occurs about 14 days before the start of the next menstrual period.
Actual Mittelschmerz is not associated with nausea, vomiting, fever, or severe pelvic pain. These symptoms should be evaluated by a medical provider since they can indicate a more serious condition.
Diagnosis is made through patient history.
Treatment requires only over-the-counter, nonsteroidal anti-inflammatory drugs to relieve the pain. An oral contraceptive will stop the symptoms, since it also stops ovulation.
Rarity: Common
Top Symptoms: abdominal pain (stomach ache), last period approximately 2 weeks ago, vaginal bleeding, bloody vaginal discharge, pelvis pain
Symptoms that always occur with ovulation pain (mittelschmerz) or midcycle spotting: last period approximately 2 weeks ago
Urgency: Self-treatment
Normal case of vaginal discharge
It is perfectly normal for every woman to have a clear or thin white vaginal discharge which is more or less constant.
The body protects the vaginal tissues by producing this light mucus from glands in the cervix and in the vaginal walls. This keeps the tissues lubricated so that they do not dry out and become irritated, and keeps the tissues slightly acidic because that helps to kill off any harmful germs.
The discharge is also a cleaning mechanism, clearing away any dead cells or bacteria as it moves out of the vagina. Douching is not necessary for normal discharge.
Vaginal discharge may change at different stages of life. During pregnancy, it becomes white and milky in appearance.
During and after menopause, the discharge lessens due to the drop in estrogen levels. If the dryness causes irritation or difficulty with sexual activity, a gynecologist can recommend an appropriate remedy.
Normal vaginal discharge never causes itching or has a foul smell, and is never any color other than clear or white.
Rarity: Common
Top Symptoms: vaginal discharge, mild vaginal discharge, white/gray vaginal discharge, clear vaginal discharge, severe vaginal discharge
Symptoms that always occur with normal case of vaginal discharge: vaginal discharge
Symptoms that never occur with normal case of vaginal discharge:vaginal itch or burning, painful urination, severe vaginal discharge, vaginal pain, bleeding after sex, missed period, vulvovaginal odor
Urgency: Wait and watch
Bacterial vaginosis
Bacterial vaginosis is an inflammation of the vagina due to overgrowth of the bacteria which are normally present.
It is not considered an STD (sexually transmitted disease) but nearly all cases are found in women after unprotected sexual contact, especially with multiple partners.
Frequent douching is also a factor.
Male partners do not carry this condition, but it can spread between female partners.
Common symptoms include an itchy, foul-smelling discharge that may look grayish or greenish, as well as burning during urination. However, some women have no symptoms.
The greatest risks of bacterial vaginosis are secondary. The symptoms can be similar to actual STDs and so should not be ignored. This condition makes a woman more vulnerable to actual STDs, as well as to pelvic inflammatory disease and to infections following any gynecologic surgery.
Pregnant women with bacterial vaginosis are at risk for premature or low-birth-weight babies.
Diagnosis is made through symptoms, and/or pelvic exam and vaginal swab.
Treatment consists of oral medication, and sometimes a cream or gel that is inserted into the vagina.
Rarity: Uncommon
Top Symptoms: vaginal itch or burning, vulvovaginal odor, bloody vaginal discharge, white/gray vaginal discharge, thick vaginal discharge
Urgency: Primary care doctor
Atrophic vaginitis
Atrophic vaginitis is a condition causing dryness of the vagina. It is caused by a drop in estrogen levels, which happens due to menopause, stress, medication side effects, and childbirth. Other symptoms include painful sex and vaginal soreness.
You should consider visiting a medical professional to discuss your symptoms. Atrophic vaginitis is evaluated with a review of your symptoms and a pelvic exam. Once diagnosed, it can be treated with estrogen replacement, moisturizers, and lubricants. Avoiding douching and perfumes may help dryness from worsening.
Symptoms of menopause
Menopause is the name for the natural process by which the menstrual cycle (period) stops happening in a woman. Usually, the process is gradual (takes months or years) and occurs from the age of 45 to 55 years. Menopause is officially diagnosed once a woman stops having a period for 12 months continuously. A woman with menopause will notice a decrease in the number and regularity of her periods until they completely stop. In addition, she may notice a number of symptoms that occur as a result of decreased estrogen levels, such as hot flashes, changes in mood, sleep problems, vaginal dryness, changes in libido, and changes in sexual function. Certain medications exist that can decrease these symptoms.
Rarity: Common
Top Symptoms: fatigue, delay in or irregular periods, vaginal discharge, anxiety, trouble sleeping
Symptoms that always occur with symptoms of menopause: delay in or irregular periods
Urgency: Self-treatment
- Are you sexually active?
- Do you feel pain when you urinate?
- When was your last menstrual period?
- Do you use birth control beside condoms?
Self-diagnose with our free Buoy Assistant if you answer yes on any of these questions.
Pregnancy, Ovulation, and Other Causes
Vaginal discharge is fluid that’s naturally released by cells in your vagina and cervix. It serves as one of your body’s defenses by moving dead skin cells and bacteria out of the vagina while also maintaining a healthy pH balance.
Changes in the consistency and color of your discharge can sometimes offer clues about your body’s processes. Read on for more info on what clear, stretchy discharge could mean for your body.
Ovulation refers to the point in the middle of your cycle when your body releases an egg for potential fertilization. As you approach this point in your cycle, cervical mucus production increases. This results in more abundant discharge that’s clear and stretchy.
This increased discharge helps to usher sperm up your cervix so they can fertilize the released egg.
Some people check for signs of clear, stretchy discharge to figure out when they’re ovulating and are most fertile.
To use discharge to track your ovulation, you’ll need to check your cervical mucus on a daily basis:
- Sit on a toilet seat and use clean hands to wipe your vaginal opening with toilet paper.
Do this before you urinate.
- If you don’t see any discharge on the toilet paper, insert your fingers into your vagina and remove them, checking the mucus for color and consistency.
- Examine the discharge’s color and texture.
- Wash your hands and record your findings.
Learn more about tracking your cervical mucus and what to look for at different stages of you menstrual cycle.
Many people report experiencing changes in cervical mucus early in their pregnancy.
Usually, your discharge becomes drier and thinner after ovulation, when estrogen decreases. But if sperm successfully fertilize an egg, you might notice that your discharge remains thick, clear, and stretchy. It might also take on a whitish color.
This happens because hormones, including estrogen and progesterone, continue to rise after ovulation if an egg’s been fertilized. This thicker discharge can last for up to about eight weeks. At that point, the mucus starts to form a mucus plug, which protects the embryo and cervix.
Keep in mind that cervical mucus changes aren’t a very reliable way to tell if you’re pregnant, but they can be a useful indicator of when you might want to take a pregnancy test.
Many things besides ovulation and pregnancy can cause changes in your vaginal discharge. This is why you shouldn’t rely solely on tracking your cervical mucus to determine fertility.
Other things that can cause clear, stretchy discharge include:
- exercising
- sexual arousal
- sexual activity
- dietary changes
- stress
- recent surgery involving your cervix or nearby organs
- starting a new medication, especially hormonal birth control
These are expected changes and aren’t usually cause for concern.
Clear, stretchy vaginal discharge usually isn’t anything to worry about, but there are a few exceptions.
For example, vaginitis, a bacterial infection of the vagina, can cause changes in pH that cause the cervix to produce extra mucus. Sometimes, the mucus remains clear. In other cases, it might turn yellow, gray, or green.
Yeast infections and sexually transmitted infections, including gonorrhea, chlamydia, or trichomoniasis, can all cause changes in cervical discharge.
Make an appointment with your healthcare provider if you have unusual clear, stretchy discharge that’s accompanied by:
- burning sensation in your vagina
- fever
- vaginal itching
- painful intercourse
- redness around your vulva
- soreness around your vulva or vagina
Vaginal discharge - causes, examination and treatment | Symptoms
Foreign object (often toilet paper, forgotten tampon) in the vagina
Signs: The discharge is usually foul-smelling, often containing a small amount of blood. Often redness in the genital area and pain during urination, and sometimes pain during intercourse.
Infections (yeast, pinworm, streptococcus, staphylococcus)
Signs: Itching, redness and swelling in the genital area. Often pain during urination. With pinworms - itching, which increases at night. With streptococcal and staphylococcal infections - redness and swelling in the genital area.
Personal hygiene
Signs: Itching, redness and unpleasant odor from the genital area. Sometimes pain during urination.
Sexual abuse
Signs: Soreness in the genital area. Sometimes discharge that smells bad or contains blood. Often vague symptoms (fatigue or abdominal pain) or behavioral changes (tantrums or withdrawal).
Bacterial vaginosis
Signs: Liquid, white or gray cloudy discharge with a fishy smell. Itching and irritation.
Yeast infections
Signs: Irritation, itching, redness and swelling in the genital area. Thick, white, lumpy cheesy discharge. Sometimes worsening of symptoms after intercourse and before menstruation. Sometimes taking antibiotics in the recent past or having a history of diabetes.
Trichomoniasis (protozoal infection)
Signs: Usually copious yellow-green frothy discharge with a fishy odor. Itching, redness, swelling and soreness in the genital area. Sometimes pain during intercourse and urination.
Pelvic inflammatory disease
Signs: Aching growing pain in the pelvic area, which can be felt on one or both sides. A discharge that is sometimes foul-smelling and may become pus-like and yellow-green in color as the infection progresses. Abnormal vaginal bleeding. Sometimes pain during intercourse and urination, fever or chills, nausea or vomiting.
Thinning of the vaginal mucosa (atrophic vaginitis)
Signs: Scanty discharge. Pain during intercourse.
R irritation (urine-induced)
Signs: General redness in the genital area and anus. Conditions that increase the risk of this type of irritation (urinary incontinence or when women are bedridden with illness).
Cancer of the vagina, cervix, body of the uterus
Signs: Watery or bloody discharge. Pathological vaginal bleeding. Often there are no other symptoms until the cancer has spread. Pain that develops gradually and sometimes becomes chronic. Sometimes weight loss.
Irritation due to use of chemicals (due to use of soaps, bubble baths, hygiene sprays or vaginal creams and ointments)
Signs: Redness, itching, swelling and soreness in the genital area.
Fistula (abnormal canal) between intestines and genital tract
Signs: Causes of formation: trauma during childbirth, surgery, inflammatory bowel disease. cancer of the digestive tract or genital organs. Discharge with an unpleasant odor. Presence of stool in the vagina or in vaginal discharge.
Inflammation (after radiotherapy, pelvic surgery, chemotherapy drugs)
Signs: Recently treated for disorders of the pelvic organs. Discharges containing pus. Pain during urination and intercourse. Sometimes irritation, itching, redness, burning pain and minor bleeding.
Skin diseases (psoriasis, lichen sclerosus and ringworm)
Signs: Rash, itching, or other symptoms, depending on the disorder.
Stretching discharge - norm or pathology
Medical expert - Lysenko Oksana Borisovna.
Editor and medical expert - Harutyunyan Mariam Harutyunovna.
Number of views: 850 299
Date last updated: 03/25/2022
Average time to read: 4 minutes
What discharge in women are considered the norm
Why are the stretching discharge
Signs of pathology
The importance of observing high -quality intimate hygiene with stretching excretions of 9000 9000
9000 9000 7 inflammatory processes. In fact, viscous mucus from the genital tract does not always indicate any pathological conditions, if there are no additional complaints. Sticky discharge from the vagina performs a protective function and cleanses the genital tract. Mucus secretion maintains an optimal level of hydration, as well as comfort during intimate intercourse 1 . Depending on the phase of the menstrual cycle and the hormonal background of a woman, vaginal discharge may have a different volume and consistency 2,3,15 .
What discharges are considered normal in women
Normal discharges have the following signs and characteristics:
- no unpleasant odor, slight sour smell is allowed 4.5 ;
- At the beginning of the cycle, there is a sticky vaginal discharge that becomes stretchy closer to the day of ovulation, profuse and more liquid 3-4 days before the period 3 ;
- secretion insignificant in volume 6 .
Why do stretching discharges appear
Stretching discharges of increased viscosity appear as a result of changes in the body associated with preparation for conception. An increase in the amount of cervical mucus allows sperm to reach the egg faster and complete fertilization. The nature of the discharge from the vagina is affected by the amount of estrogen and progesterone - female sex hormones. Immediately after menstruation, the discharge is slight, sticky. Shortly before ovulation, the mucus liquefies, becomes viscous and elastic 3 . Similar discharge also appears within 1–2 days after unprotected intercourse 7 . This is also considered the norm 3 . If a woman is very worried about viscous vaginal discharge, it is better to consult a gynecologist and undergo an examination. Some diseases, especially those of an inflammatory nature, can lead to increased secretion of vaginal secretions, but other health complaints are usually present.
Most often, the nature of vaginal discharge changes with urogenital infections. They can appear not only due to unprotected intimate contacts, but also as a result of changes in the vaginal microflora under the influence of adverse external and internal factors. Contribute to a change in the microbial balance of hormonal disorders, prolonged use of antibiotics and a general weakening of the immune system 9 .
Signs of pathology
When vaginal discharge is associated with gynecological diseases, additional pathological signs appear:
- pain in the lower abdomen and lower back 8 ;
- copious yellow-green discharge with an unpleasant odor or curdled consistency 10.11 ;
- discomfort during urination and intercourse 12 ;
- redness of the vulva, swelling of the external genitalia 12 ;
- menstrual irregularities, etc. 13
If the above signs are present, a woman should be alert. It is recommended to make an appointment with a gynecologist, tell the specialist about your problems and undergo a comprehensive examination. Based on the results of the examination and tests, the doctor can make a diagnosis and, if necessary, select the appropriate treatment.
The importance of maintaining good intimate hygiene with lingering discharge
A lingering vaginal discharge should not cause significant discomfort. But mucus often stains laundry. In addition, sticky vaginal discharge is a breeding ground for many bacteria and fungi. In order to prevent the development of infectious and inflammatory diseases, it is necessary to monitor the quality of personal hygiene 14 , wash regularly and use special protective equipment. This will allow you to maintain maximum comfort in the intimate area throughout the day. When choosing personal care products, give preference to products with a natural and safe composition that does not irritate the skin 16 and supports a healthy vaginal flora.
Carefree® panty liners help with non-menstrual bleeding, which can be quite heavy, especially in the middle of a woman's cycle. The delicate surface immediately absorbs mucus, allowing you to feel comfortable.
References
- Donnikov A.E. Bacterial vaginosis and vaginitis. A new look at an old problem // Farmateka. 2016 - No. 12
- Dobrokhotova Yu. E., Zatikyan N.
G. Hormonal status and microbiocenosis of the vagina // Obstetrics, gynecology and reproduction. 2008. No. 3. URL: https : //cyberleninka . ru/article/n/gormonalnyy-status-i-mikrobiotsenoz-vlagalischa (Date of access: 12/06/2021).
- Murakov S.V., Obraztsov I.G., Budaev A.I., Veredchenko A.V., Pustovalov D.A., Kuznetsov R.E., Popkov S.A. Comparative evaluation of the fertile properties of cervical mucus and features of the ultrastructure of the epithelium of the endocervix against the background of urogenital infections. Vestnik RUDN University. Series: Medicine. 2014. №3. URL: https : //cyberleninka . ru/article/n/sravnitelnaya-otsenka-fertilnyh-svoystv-tservikalnoy-slizi-i-osobennostey-ultrastruktury-epiteliya-endotserviksa-na-fone (date of access: 12/06/2021).
- Pestrikova T.Yu., Pikhovskaya V.G., Pivkina O.A. Modern view on the therapy of bacterial vaginosis // Gynecology. 2014. No. 1. URL: https : //cyberleninka .
ru/article/n/sovremennyy-vzglyad-na-terapiyu-bakterialnogo-vaginoza (date of access: 12/06/2021).
- Medzhidova MK, Zaidieva ZS, Veresova AA Vaginal microbiocenosis and factors influencing its condition // MS. 2013. No. 3-2. URL: https : //cyberleninka . ru/article/n/mikrobiotsenoz-vlagalischa-i-faktory-vliyayuschie-na-ego-sostoyanie (Date of access: 12/06/2021).
- Dobrokhotova Yu. E., Zatikyan NG Microecology and protective mechanisms of the vagina // Obstetrics, gynecology and reproduction. 2007. No. 2. URL: https : //cyberleninka . ru/article/n/mikroekologiya-i-zaschitnye-mehanizmy-vlagalischa (date of access: 12/06/2021).
- Kocharyan GS The phenomenon of female ejaculation // Men's health. - 2012. - No. 4 (43). – P. 79–87.
- Shurshalina A.V. Inflammatory diseases of the pelvic organs: modern tactics of therapy // Gynecology. - 2011. - No. 5. - C. 23-26.
- Mozheiko L.F., Novikova E.V. Modern principles of therapy for vulvovaginal candidiasis // Medical News.
2012. №2. URL: https : //cyberleninka . ru/article/n/sovremennye-printsipy-terapii-kandidoznogo-vulvovaginita (date of access: 12/06/2021).
- Tkachenko L.V., Uglova N.D., Sviridova N.I., Skladanovskaya T.V. Modern approach to the treatment of vulvovaginal infections // Obstetrics and Gynecology: News. Opinions. Learning. 2018. No. 4 (22). URL: https : //cyberleninka . ru/article/n/sovremennyy-podhod-k-lecheniyu-vulvovaginalnyh-infektsiy (date of access: 12/06/2021).
- Efimov B.A. , Tyutyunnik V.L. , Mejidova M.K. , Basic principles of treatment of vulvovaginal candidiasis - breast cancer. Mother and child No. 20 dated 20.09.2011
- Malova I.O., Afanasyeva I.G., Gusevskaya K.A. Acute vaginitis of mixed etiology: a modern approach to treatment // Obstetrics and Gynecology: News. Opinions. Learning. 2019. No. 4 (26). URL: https : //cyberleninka . ru/article/n/ostrye-vaginity-smeshannoi-etiologii-sovremennyi-podhod-k-lecheniyu (date of access: 12/06/2021).