How to improve placental function
A Mother’s Magical Power: Growing a Healthy Placenta & Baby
November 22, 2021 November 22, 2021
Pam England
| “Nourishing the Life Within” Oil painting by Pam England copyright 2016 |
Alora called me for a consultation because she was concerned that, due to nausea in the first trimester, she had lost over 20 pounds. Her husband grew concerned because she was “eating like a bird,” nibbling on small amounts of food. When she asked her midwife for advice, she quickly offered blanket assurance that her “baby was fine, it is still small and doesn’t need much nutrition yet, and your blood work looks great!” Sadly, the midwife never asked Alora what she was eating, how much, and did not counsel on remedies to counter morning sickness. Blood work can rule out anemia but it can’t assess the growth and development of the placenta or fetus.
Routine prenatal care should include communication with a pregnant woman about her diet in each trimester, beginning in the first trimester “to prevent undesired birth outcomes and their immediate and long-term consequences on health and development. ”1
During our session I explained, “You’re not just growing a baby in there; you are also growing his or her placenta. Your baby and placenta are not desert air plants that can survive without soil or water for six to eight months! You have to feed your placenta in the first trimester and throughout pregnancy so that it can feed your baby. Has anyone told you about how your placenta grows and what foods it needs to be healthy?” She was eager to learn.
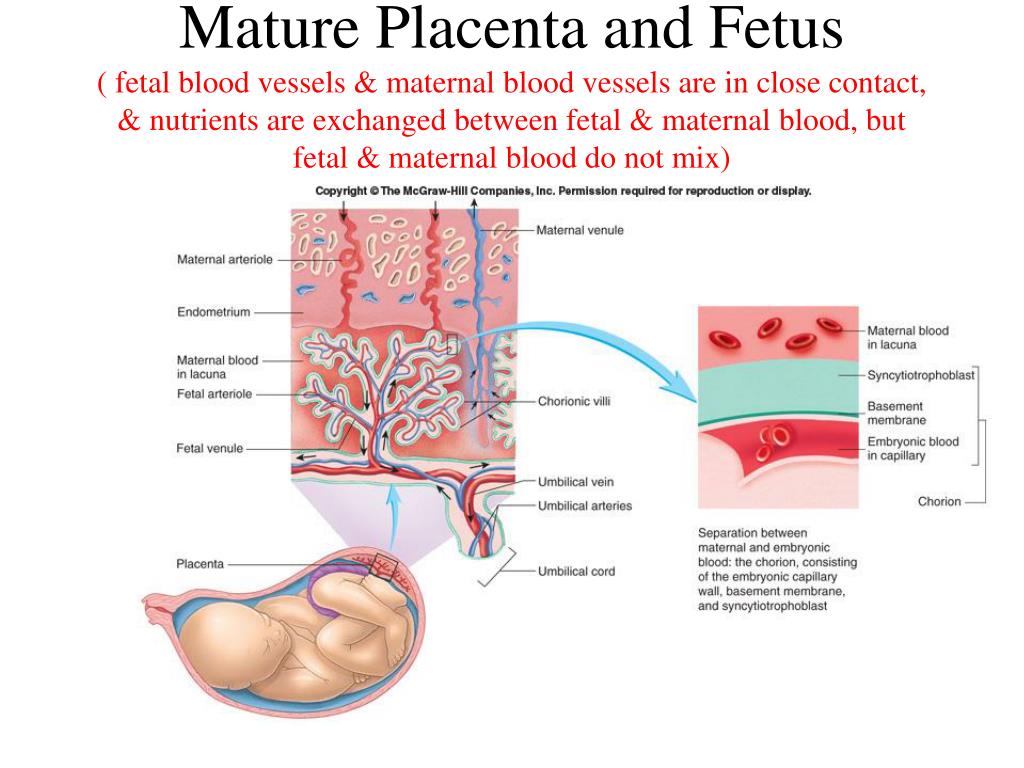
The placenta is an amazing organ. Its highly vascular network transfers oxygen and nutrients from mother to baby, and produces four hormones to sustain the pregnancy. It grows from the baby’s embryonic cells; some cultures refer to the placenta as “brother” or “sister” and after birth, treat it respectfully with rituals. By the end of the first trimester, the complex vascular structure of your baby’s placenta is formed, but it still continues to grow with your baby until about 34 weeks. When you eat well throughout pregnancy your placenta and baby thrive.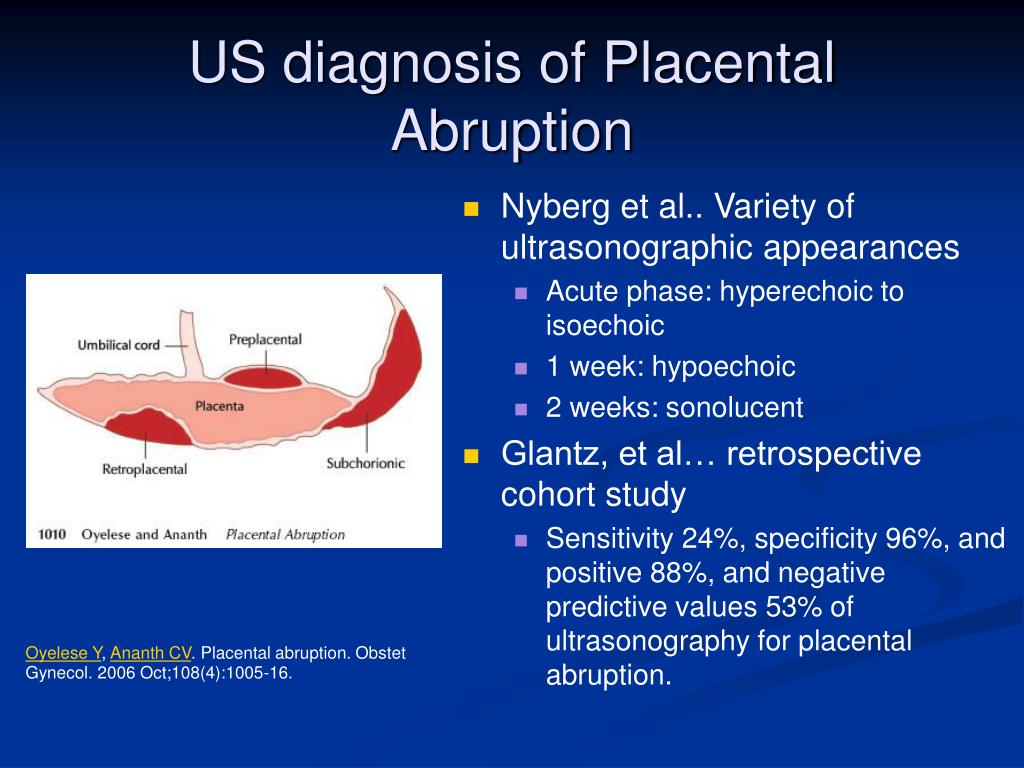 At birth, the placenta will weigh one to one-and-a-half pounds.
At birth, the placenta will weigh one to one-and-a-half pounds.
“The ability of the fetus to grow and thrive in utero depends on the placental function.”2
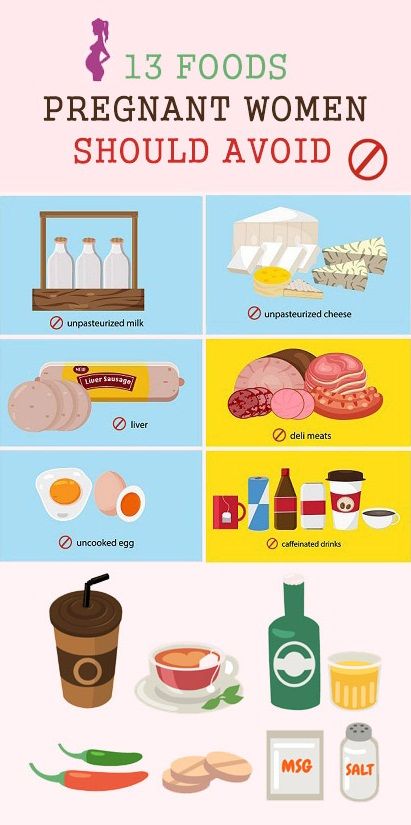
Multiple studies have shown that placental growth and weight are strictly dependent on maternal nutrition. A healthy size placenta has good blood flow and capacity to transfer sufficient oxygen and nutrients from mother to baby. The weight of a placenta directly correlates to maternal weight gain. When a mother loses weight or her weight gain is low in the first trimester, the placenta will be significantly smaller by 20 weeks’ gestation and have inadequate vascularity.3 When a placenta is malnourished and underdeveloped in the first half of pregnancy, the baby may be smaller for gestational age in the second half of pregnancy and when it is born.4 Other causes for placental insufficiency include smoking, drinking alcohol or taking recreational drugs including marijuana, immune disorders, and diabetes.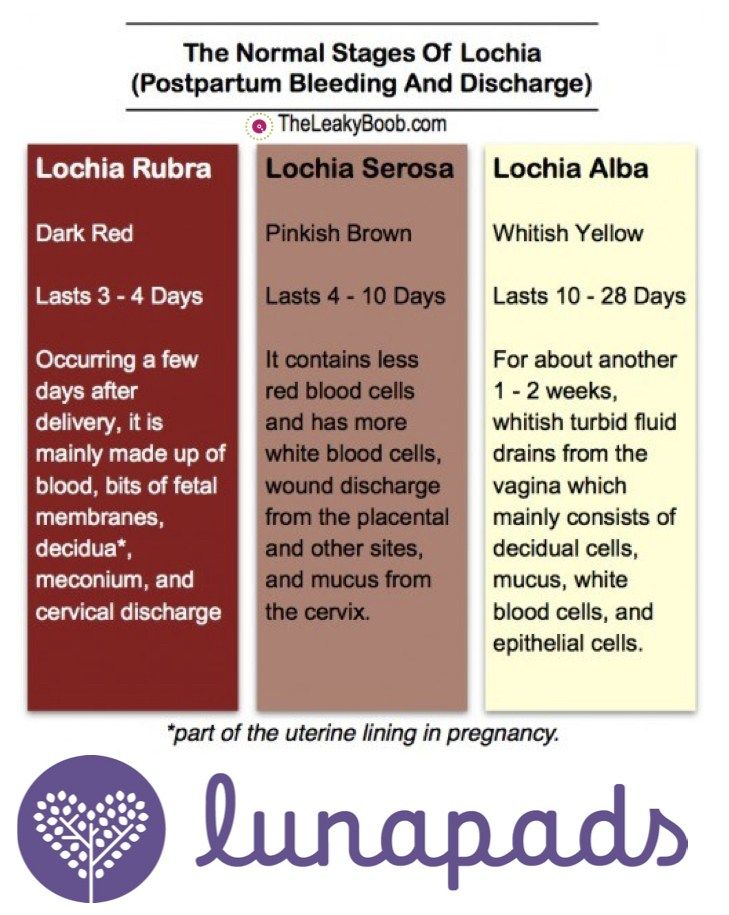 5
5
Placental insufficiency means the supply of oxygen and nutrients to the baby is compromised. Placental dysfunction is associated with placental abruption, preterm labor, intrauterine growth restriction, small for gestational age infants, and stillbirth, Placental insufficiency in labor manifests as fetal distress (decelerations in the baby’s heart rate) and may necessitate induction or cesarean surgery.6
“We studied 787 pregnant women and their newborns from a Spanish cohort study.
Clara L. Rodriguez-Bernal, et. al.7
The objective was to assess the effect of diet quality during the first trimester of pregnancy.
A positive association was observed between diet quality and newborn weight and length.
Conclusion:
A high-quality diet in the first trimester of pregnancy is associated with healthy birthweight and reducing fetal growth restriction.”
It’s never too late to start eating healthy in pregnancy. But, don’t wait until a preventable complication appears, such as the baby growing too slowly, to start eating well. Keep in mind that the placenta is mature at 34 weeks, and even if you begin eating better then, the placenta can’t recover from lost growth and development. Technology and birth attendants can measure the baby’s growth with ultrasound and monitor the heart rate; NICU can treat babies born early or small, but you have a magical power too! You can feed your baby right from the start.
But, don’t wait until a preventable complication appears, such as the baby growing too slowly, to start eating well. Keep in mind that the placenta is mature at 34 weeks, and even if you begin eating better then, the placenta can’t recover from lost growth and development. Technology and birth attendants can measure the baby’s growth with ultrasound and monitor the heart rate; NICU can treat babies born early or small, but you have a magical power too! You can feed your baby right from the start.
Five Foods to Grow a Happy Healthy Placenta in Your First Trimester
Your first task of motherhood is to eat healthy in pregnancy in the first trimester. You need to eat well, but you don’t need to eat the higher protein and calorie prenatal diet until 20 weeks. If you are busy working or going to school, include the following nutritious foods for breakfast and to bring along with you to eat during your busy day.
- Eggs
Placentas thrive on eggs! Eggs are a good source of high-quality protein—7 grams—and they contain all the amino acids, plus more than a dozen vitamins and minerals, including choline, which is good for your baby’s brain development.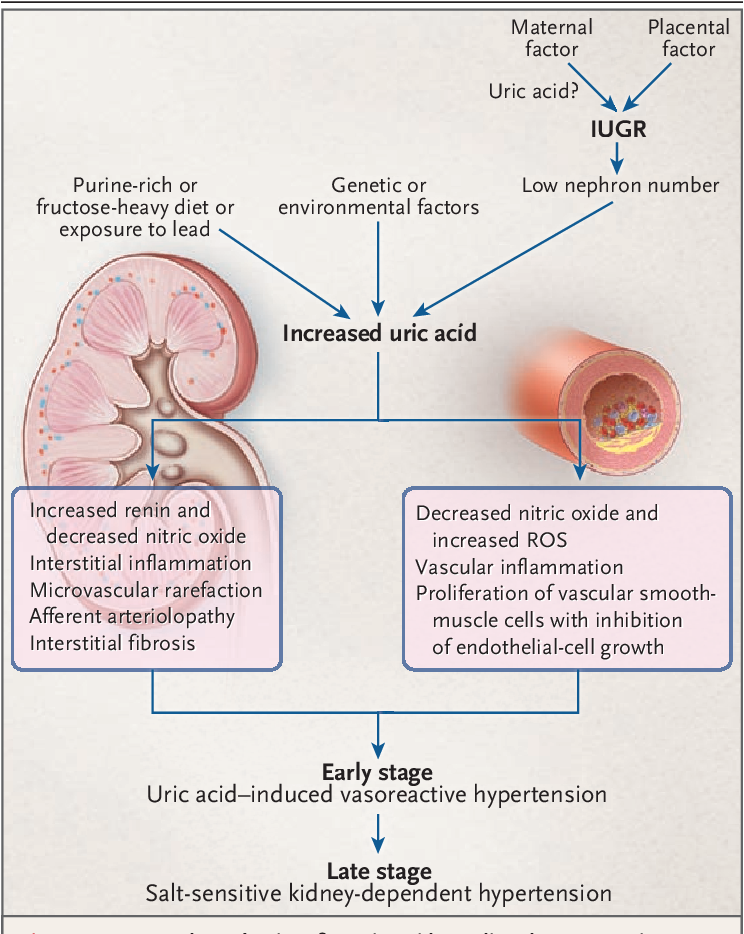 A good source of iron, too.
A good source of iron, too. - Sweet Potatoes for a Sweet Baby
Sweet potatoes, one of the best foods you can eat to build a healthy placenta, are loaded with fiber, potassium, iron, and vitamin A. The supply of vitamin A to the placenta is crucial for developing the baby’s eyes, bones, and skin. - Nuts
“Nuts nourish the placenta with healthy fats, protein, fiber, and magnesium. High levels of magnesium reduce the risk of premature labor and are crucial to the baby’s developing nervous system.” Nuts are a delicious snack for working or hiking moms. - Green vegetables
“The recommended intake of iron almost doubles during pregnancy. As such, iron-rich foods such as spinach, broccoli, and kale are crucial during pregnancy. Low iron levels could result in a deficiency and hinder the transfer of oxygen and nutrients to the placenta.” - Yogurt
Greek yogurt is a delicious, creamy superfood; it has more protein than regular yogurt.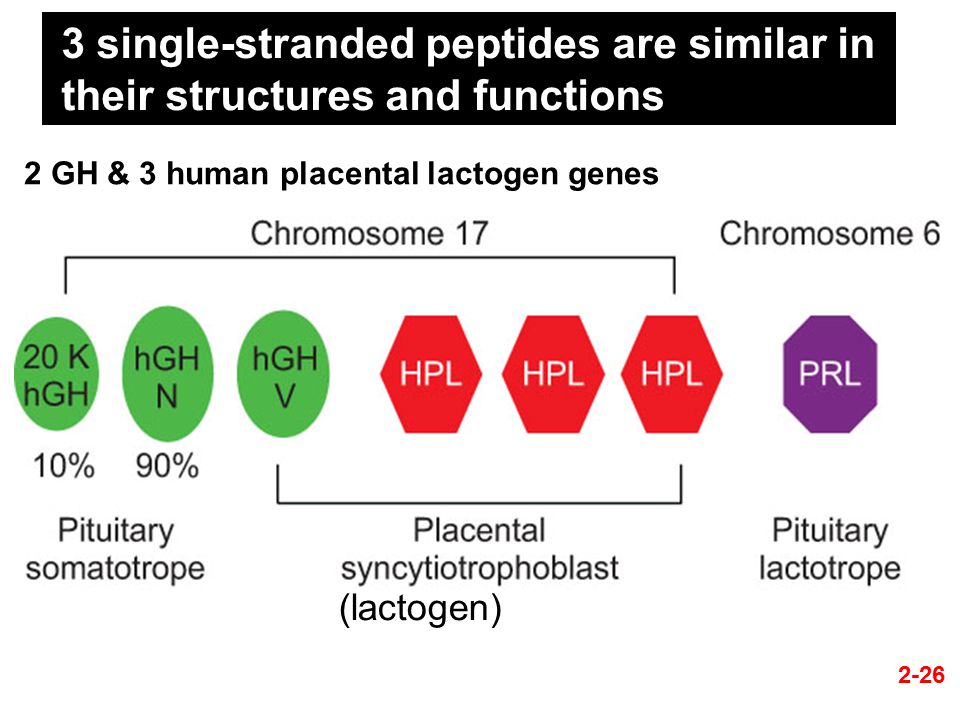 One-half cup of Greek yogurt has 12 grams of protein (double the amount in regular yogurt and equivalent to three ounces of red meat). It contains microbiota (bacteria), aids digestion, and supports gut health. It’ll strengthen your bones and your baby’s too. As a rich source of calcium and zinc, yogurt provides many benefits for a healthy placenta. In particular, Greek yogurt is a superfood to maintain a healthy placenta. Enjoy Greek yogurt for breakfast with fruit or cereal; add honey and nuts.
One-half cup of Greek yogurt has 12 grams of protein (double the amount in regular yogurt and equivalent to three ounces of red meat). It contains microbiota (bacteria), aids digestion, and supports gut health. It’ll strengthen your bones and your baby’s too. As a rich source of calcium and zinc, yogurt provides many benefits for a healthy placenta. In particular, Greek yogurt is a superfood to maintain a healthy placenta. Enjoy Greek yogurt for breakfast with fruit or cereal; add honey and nuts.
Eating well in first trimester matters.
Your baby’s birth weight and future well-being depends on placental size, rich vascularity and capacity to supply nutrients and oxygen to your baby.
it’s not complicated, it’s not a mystery; it’s common sense!
…and, it’s one way to change the Story you are bringing To birth.
Citations
- Clara L.
 Rodriguez-Bernal, et. al., (June 2010). Diet quality in early pregnancy and its effects on fetal growth outcomes: the Infancia y Medio Ambiente (Childhood and Environment) Mother and Child Cohort Study in Spain. American Journal of Nutrition, 19:6. https://academic.oup.com/ajcn/article/91/6/1659/4597271
Rodriguez-Bernal, et. al., (June 2010). Diet quality in early pregnancy and its effects on fetal growth outcomes: the Infancia y Medio Ambiente (Childhood and Environment) Mother and Child Cohort Study in Spain. American Journal of Nutrition, 19:6. https://academic.oup.com/ajcn/article/91/6/1659/4597271
2. Abubakar A Panti, et.al., The relationship between the weight of the placenta and birth weight of the neonate in a Nigerian Hospital. Nigeria Medical Journal. 2012 Apr-Jun; 53(2): 80–84. doi: 10.4103/0300-1652.103547
3. M. Thame, C. Osmond, F. Bennett, et al. (2004). Fetal growth is directly related to maternal anthropometry and placental volume. Eur J Clin Nutr 58,894–900. https://doi.org/10.1038/sj.ejcn.1601909 https://www.nature.com/articles/1601909
4. Janna L. Morrison and Timothy R Regnault (2016, June). Nutrition in Pregnancy: Optimising Maternal Diet and Fetal Adaptations to Altered Nutrient Supply. Nutrients. 8(6): 342. doi: 10.3390/nu8060342
8(6): 342. doi: 10.3390/nu8060342
5. R. Collin Carter, et.al., (2016). Alcohol, Methamphetamine, and Marijuana Exposure Have Distinct Effects on the Human Placenta. Wiley Online Library. https://doi.org/10.1111/acer.13022
6. Jaimie E. Wardinger and Shashikanth Ambati (2021). Placental Insufficiency. NCBI. https://www.ncbi.nlm.nih.gov/books/NBK563171/
7. Clara L. Rodriguez-Bernal, et. al.
8. Cells 4Life (Feb 4 2020). “What to Eat for a Healthy Placenta.”
https://cells4life.com/2020/02/what-to-eat-for-a-healthy-placenta/
5 Placenta Issues Every Woman Should Know
Problems with her placenta inspired physician Courtney Townsel to specialize in helping others understand the high risk pregnancy conditions that impact this vital organ.
For Courtney Townsel, M.D., M.Sc., working with patients experiencing high risk pregnancy conditions involving the placenta is a lived experience.
Townsel, an obstetric-gynecologist at Michigan Medicine, twice has been in her patients’ shoes.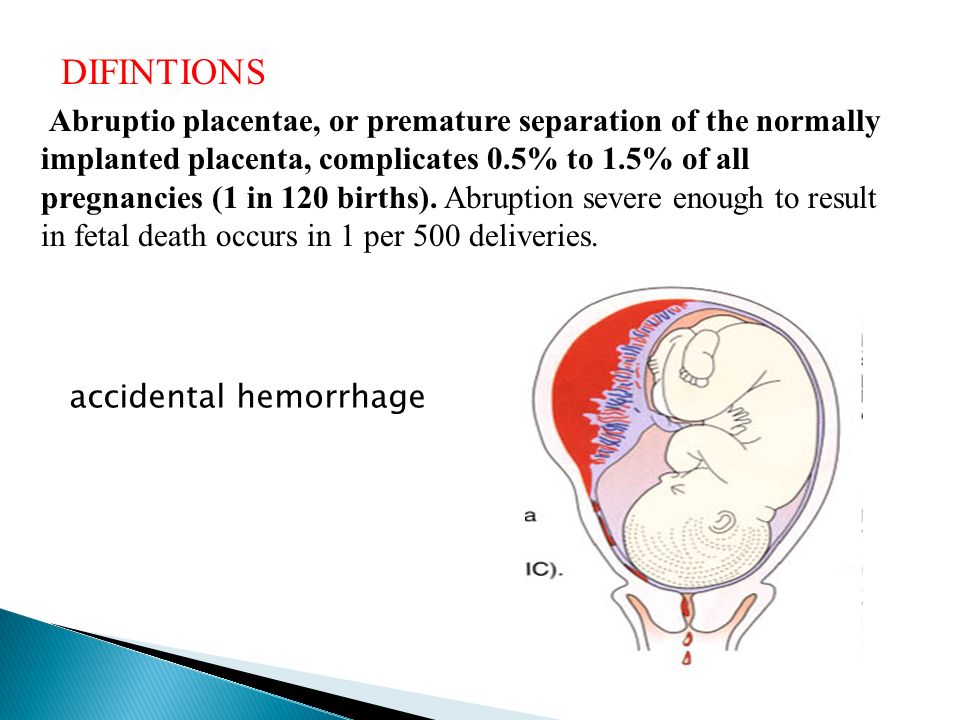 Both of her pregnancies involved two separate placental disorders.
Both of her pregnancies involved two separate placental disorders.
The placenta is a temporary organ that develops in the uterus during pregnancy. It provides the nutrients and oxygen to the baby for development and growth. Because a placenta is created with each pregnancy, it is possible for each pregnancy to have a different outcome.
Even as a trained OB-GYN in good health – she runs and plays basketball regularly – Townsel’s high risk pregnancies caught her off guard. Now she wants to share her knowledge. Here are five placental disorders she urges every woman to be aware of before pregnancy.
Placental InsufficiencyPlacental insufficiency is the diagnosis that catalyzed Townsel’s interest in researching high risk pregnancies. As a first year OB-GYN resident, she was hyper vigilant during her first pregnancy at age 27. Everything appeared to be progressing on schedule until, at 34 weeks, she noticed her baby wasn’t growing well and the fluid around her baby was low.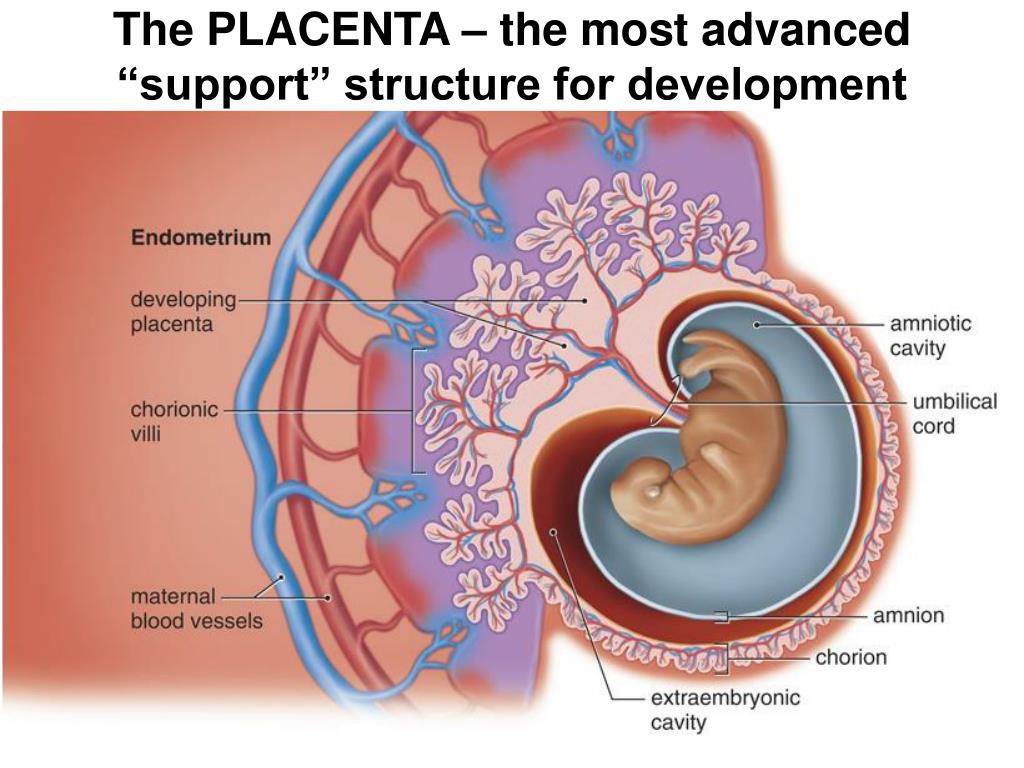 Some other moms-to-be may notice the baby isn’t moving often. In some cases, the only symptom is the death of the baby.
Some other moms-to-be may notice the baby isn’t moving often. In some cases, the only symptom is the death of the baby.
With this condition, the placenta can’t deliver enough oxygen and nutrients to the baby, which may lead to fetal growth restriction and possible issues with the baby’s development. The insufficiency occurs because the placenta doesn’t attach optimally to the uterus, which impedes the dilation of the arteries and restricts the flow of the important nutrients and oxygen.
To detect placental insufficiency, doctors may order:
-
An ultrasound to look at features of the placenta, calcium deposits or placental thickness, as well as the size of the fetus
-
A fetal nonstress test that monitors the baby’s heart rate and contractions
“The diagnosis surprised me,” Townsel says. “I had no prior medical conditions. The only thing that slightly increased my risk is I'm a Black woman.”
Other potential correlations include having diabetes, high blood pressure, anemia and blood clotting disorders or using blood thinners, drinking alcohol, taking drugs or smoking during pregnancy.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Moms with this condition require frequent visits to a high risk OB-GYN, as well as activity restrictions. Moms need to make sure all possible blood flow is going to the fetus, not to tired or fatigued muscles.
“I had a medical degree and I still wasn't fully aware of the risks that could happen, and that they could occur even if you're young and healthy,” says Townsel, who delivered a healthy son at 37 weeks.
PreeclampsiaPreeclampsia, a pregnancy complication that leads to high blood pressure and possible kidney damage, is another placental disorder that Townsel personally experienced.
Its symptoms include excess weight gain in a short period, swelling of the legs, hands and fingers and headaches. Detecting preeclampsia is one of the reasons doctors check blood pressure and measure protein in urine during prenatal care. It can be attributed to autoimmune disorders, genetic factors, diet and blood vessel-related issues. Ironically, preeclampsia also can cause placental insufficiency.
Ironically, preeclampsia also can cause placental insufficiency.
“Often a patient will start to show evidence of placental insufficiency. That can be an indicator of a future complication, such as developing a high blood pressure problem in pregnancy like preeclampsia, hypertension or diabetes,” Townsel says.
That was exactly how Townsel’s first pregnancy unfolded.
Her second pregnancy, however, was nearly picture perfect until after delivery. She was 32 and, because of her history, she was taking baby aspirin daily. Global studies have found that daily aspirin improves outcomes and reduces preeclampsia risks by 30%. It helps vessels better attach to the uterus and remain open during the pregnancy, studies indicate.
“My second pregnancy, I took aspirin, the baby grew well, and I went past my due date, but I still developed preeclampsia, but this time it was one week postpartum,” she says.
A week after delivery, she was still swollen, never really lost the fluids after giving birth, felt tired and was short of breath.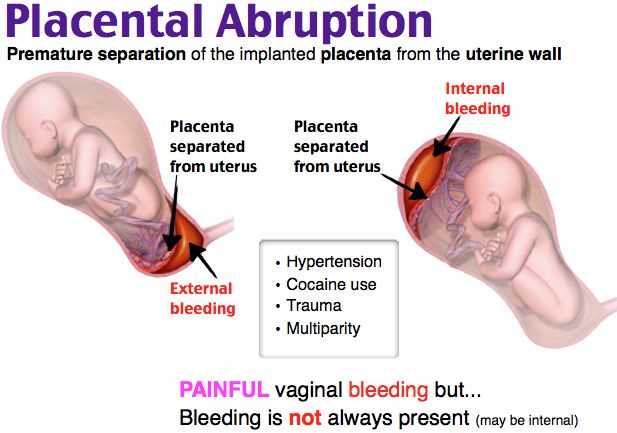 Her blood pressure was high. She ended up hospitalized for 72 hours to receive magnesium to prevent seizures.
Her blood pressure was high. She ended up hospitalized for 72 hours to receive magnesium to prevent seizures.
The experience made her a more in-tune physician.
“Whenever I start a woman on magnesium, I talk to her from a personal place about how it can make her feel and the concerns of having high blood pressure in pregnancy and how you get through it,” says Townsel.
Placenta PreviaPlacenta previa occurs when the placenta blocks or partially blocks the cervix, which is the opening to the uterus. This is an issue because a baby passes through the cervix and the birth canal during a vaginal delivery.
Symptoms for this condition include cramps and bleeding typically after 20 weeks. Treatment involves medication, pelvic rest, and activity restrictions, including sex. If the condition can’t resolve itself, which happens often, a delivery is typically by Cesarean section.
Researchers aren’t certain of the cause of placenta previa but it’s often related to women who have previously given birth, had scars on the uterus or are carrying multiple babies.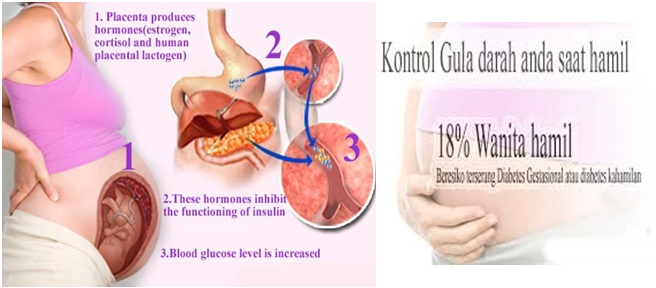 It’s found more often in non-white women, those over 35, and patients who smoke or use cocaine.
It’s found more often in non-white women, those over 35, and patients who smoke or use cocaine.
“While the risks of hemorrhaging and a preterm birth are higher, oftentimes, these pregnancies do just fine if the placenta previa is diagnosed,” Townsel says.
Placenta AbruptionA highly dangerous condition for both mom and baby, placenta abruption occurs when the placenta separates prematurely from the uterine wall. This may cut off the baby’s supply of oxygen and nutrients, restricting its growth, or prompt a premature or stillbirth delivery.
“This could also lead to heavy bleeding from mom and be life threatening for her, as well,” Townsel says. That may usher in transfusions, kidney failure, blood clotting issues or a hysterectomy.
Sometimes it occurs when the mom experiences trauma like a fall, a car accident, or a blow to the abdomen. A rapid loss of amniotic fluid, which cushions the baby in the uterus, could also be the cause.
Other factors that increase the risk are:
-
Hypertension or any high blood pressure-related conditions like preeclampsia
-
Smoking
-
Cocaine use
-
An infection in the uterus
-
Age, especially older than 40
It is not something you can prevent, Townsel says, but you can tamp down the risks by avoiding smoking and drug use.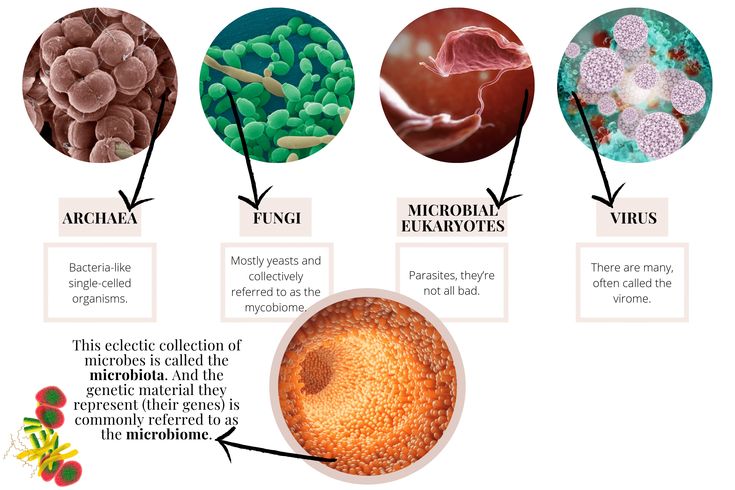 If any trauma to the abdomen occurs, seek a doctor immediately.
If any trauma to the abdomen occurs, seek a doctor immediately.
Sometimes the placenta attaches to the uterus too well. If it expands too far into the uterus, it’s called placenta accreta. It may even reach the bladder or wrap around the rectum.
Often this condition goes undetected until after childbirth when the placenta won’t detach from the uterine wall. Sometimes part or all of it hangs on. Removing it can lead to severe blood loss after a delivery. Occasionally, a doctor must perform a hysterectomy in such a case.
“Kim Kardashian reportedly had this issue (with her first pregnancy) where her placenta invaded into the uterus and could not be disconnected safely at the time of delivery,” Townsel says.
Another related condition is placenta increta, when the placenta invades the uterus’ muscles. Placenta percreta happens when the placenta grows through the uterine wall.
The cause is unknown, but risks are higher for those who have had prior surgery on the uterus (previous c-section or other uterine surgery), prior defects in the uterine muscle or in women older than 35.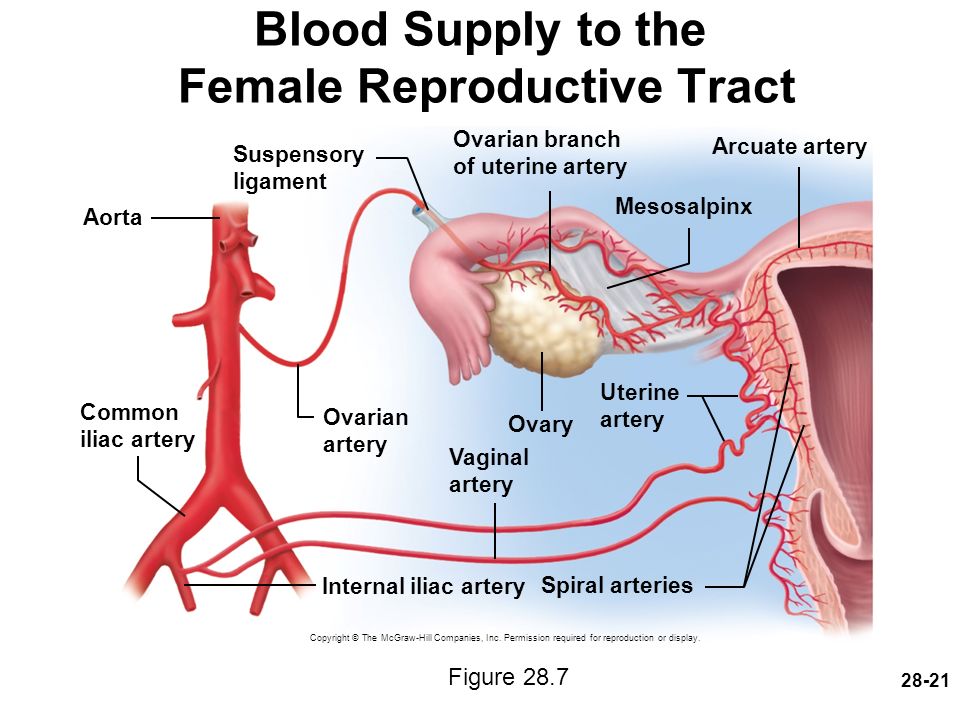 Sometimes it happens for no detectable reason.
Sometimes it happens for no detectable reason.
“Medical education, health literacy and advocacy for yourself and others is really important,” Townsel says. “Women just need to be aware that placental issues can happen. That’s how we improve outcomes.”
Placental insufficiency - what is it and how to treat it
- Types and causes of placental insufficiency
- Diagnosis of placental insufficiency
- Treatment of placental insufficiency
Most women know that the placenta connects mother and baby during pregnancy and provides nutrients and oxygen to the baby.
Are there situations when the placenta ceases to perform its function correctly and fully? Is it possible to somehow prevent this?
What is the function of the placenta
So, the placenta is an important organ that is formed only during pregnancy. The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg, starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.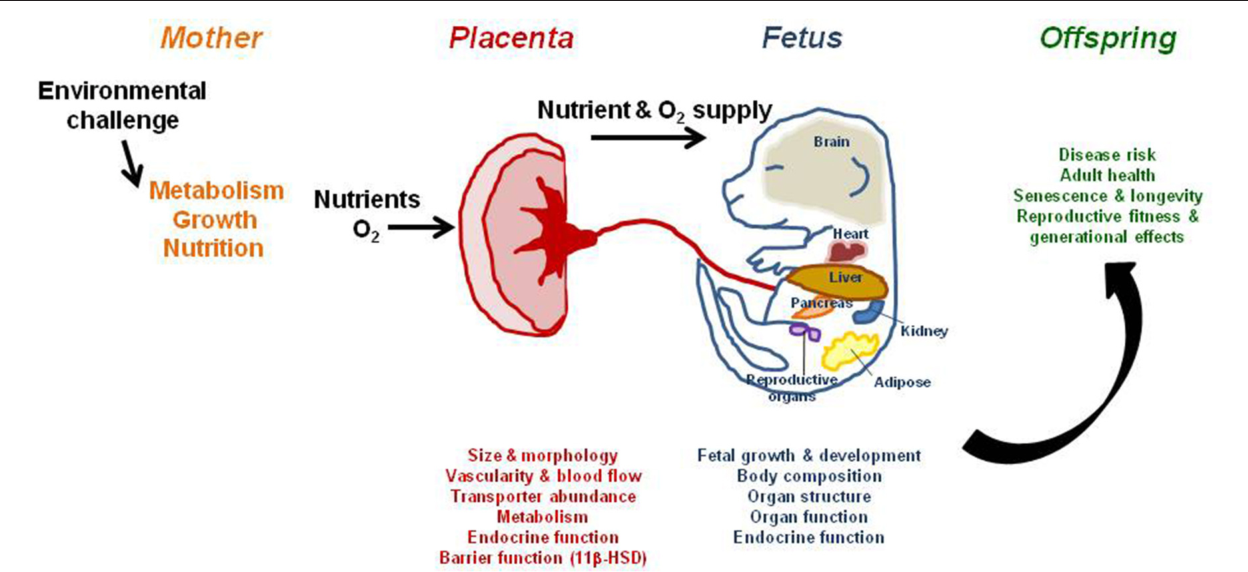
Inside the villi flows the blood of the baby, and outside they are bathed in the blood of the mother. Between the blood flow of mother and baby there is only one layer of cells, which plays the role of a barrier between the body of mother and child. Thanks to this membrane, the blood of the mother and fetus does not mix.
However, in recent years it has become known that fetal blood cells still penetrate the placental barrier into the mother's bloodstream, and thanks to this, it has become possible to conduct genetic analyzes and determine chromosomal abnormalities, Rh factor and fetal sex from the blood of a pregnant woman (non-invasive prenatal test) .
In the placenta, there is a constant exchange of substances between mother and child. Oxygen and nutrients are supplied from the mother's blood to the fetus, carbon dioxide and metabolic products from the fetus back to the mother, to be removed from the body.
The placental barrier performs an immunological function, as it allows some protective antibodies - blood cells that fight infectious agents, in addition, it is impervious to certain harmful substances, viruses and bacteria. Unfortunately, the placental barrier is easily overcome by drugs, alcohol, nicotine, components of many drugs and some viruses.
Unfortunately, the placental barrier is easily overcome by drugs, alcohol, nicotine, components of many drugs and some viruses.
An important function of the placenta is the production of hormones and biologically active substances. First of all, these are hormones that are important for successful pregnancy, for example, chorionic gonadotropin, placental lactogen, estrogens, etc.
Unfortunately, things don't always go well. Due to a variety of reasons, deviations in the development and functioning of the placenta may occur at different stages of pregnancy. These changes never go unnoticed for mom and baby, and often have dire consequences.
If the placenta ceases to perform its functions to the fullest, the so-called placental insufficiency develops. In fact, it consists in the deterioration of blood circulation in the mother-placenta-fetus system.
Types and causes of placental insufficiency
Doctors distinguish between acute and chronic placental insufficiency:
Acute placental insufficiency
This is a condition that requires urgent medical intervention.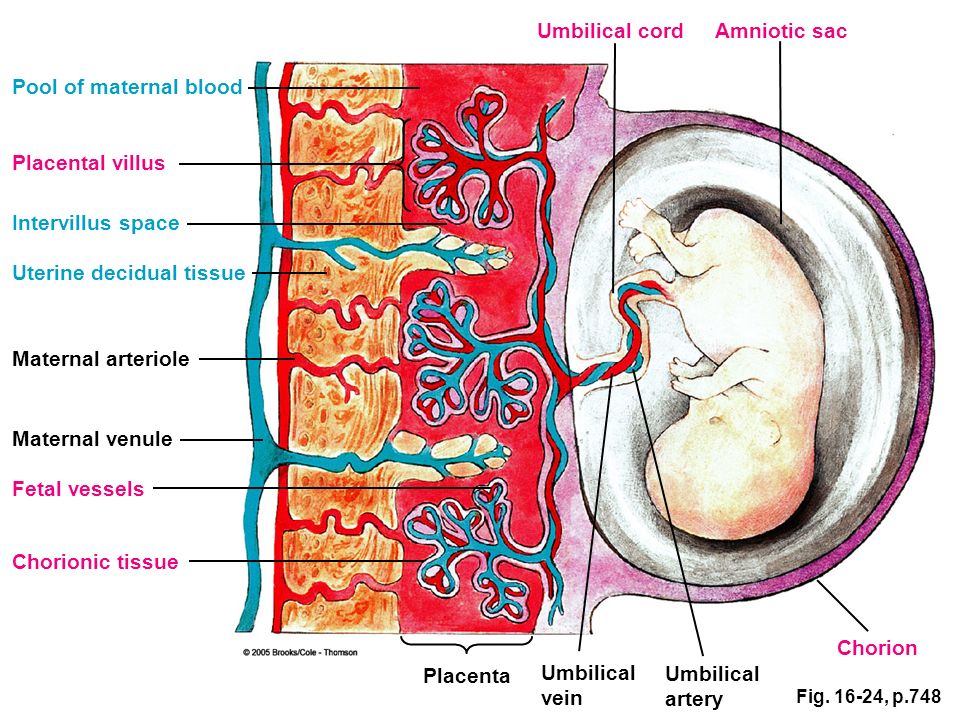 It is characterized by a rapid deterioration in placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or the death of certain areas of placental tissue, for example, during the formation of blood clots in the vessels. Abdominal trauma, antiphospholipid syndrome can serve as the cause of detachment.
It is characterized by a rapid deterioration in placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or the death of certain areas of placental tissue, for example, during the formation of blood clots in the vessels. Abdominal trauma, antiphospholipid syndrome can serve as the cause of detachment.
Phospholipids are complex fats that are part of the membranes of all body cells. In some cases, the body's immune system produces a large number of antibodies to some of its own phospholipids and proteins that bind these lipids. They are called antiphospholipid antibodies and, when interacting with the cells of the body, cause cell damage and activation of the blood coagulation system, which leads to thrombosis.
Antiphospholipid syndrome is the most common cause of thrombotic complications in pregnancy, including placental abruption and acute placental insufficiency.
A severe course of gestosis, a formidable complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine, can also cause placental abruption.
Acute placental insufficiency develops when more than 2/3 of the placental surface is detached.
In case of acute placental insufficiency, it is necessary to perform a caesarean section as soon as possible to save the life of the baby and mother.
Chronic placental insufficiency
Chronic placental insufficiency is much more common in pregnant women. In this case, there is a violation of the formation and maturation of the placenta, the uteroplacental and fetal-placental blood flow decreases, gas exchange and metabolism in the placenta are limited, and the synthesis of placental hormones decreases. All these changes determine the insufficient supply of oxygen and nutrients to the baby, cause a delay in the growth and development of the fetus.
The most common causes of placental insufficiency are previous abortions, especially surgical abortion during the first pregnancy, smoking, while the number and strength of cigarettes smoked do not matter, since tobacco smoke, not nicotine, has a negative effect on the formation of defective placental vessels.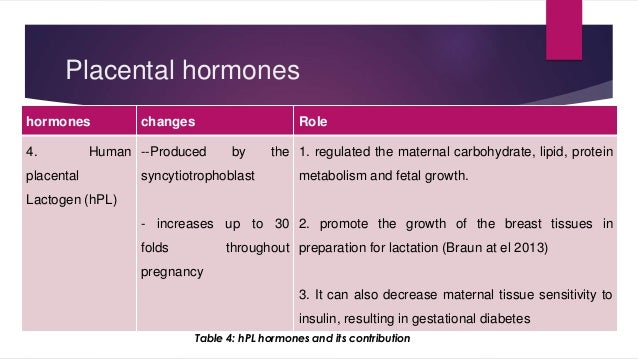
The risk group for the development of placental insufficiency also includes women with chronic diseases such as arterial hypertension, iron deficiency anemia, pyelonephritis, diabetes, thyroid disease.
In recent years, there has been a significant increase in placental insufficiency caused by bacteria, viruses, fungi. The reason for this can be both an acute infection suffered by the expectant mother during pregnancy, and the activation of a chronic infectious process in the body of a pregnant woman.
Of no small importance in the formation of chronic placental insufficiency is the pathology of the uterus: endometriosis, malformations of the uterus (saddle-shaped, bicornuate). Doctors also consider uterine fibroids to be a risk factor. Of course, a number of drugs have an adverse effect on the formation of the placenta and the development of the fetus. Currently, a list of drugs that are not approved for use during pregnancy has been defined.
Also of great importance in the development of placental insufficiency is thrombophilia - an increased tendency of the body to form blood clots - blood clots in the vessels.
In some cases, placental insufficiency may be due to the presence of chromosomal abnormalities in the fetus, in particular in Down syndrome (the presence of an additional chromosome 21 in the fetus) or Edwards syndrome (an additional chromosome 18 in the fetus), placental dysfunction is diagnosed already in the early stages of pregnancy.
It should be noted that among the complications of pregnancy, most often leading to the development of chronic placental insufficiency, a significant factor is preeclampsia (or late preeclampsia) - a complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine.
Regardless of the factors contributing to the development of placental insufficiency, it is based on circulatory disorders in the uterine-placental complex, leading to disruption of all functions of the placenta. Consequently, the symptoms of chronic placental insufficiency will be due to a lack of oxygen and nutrients to the fetus.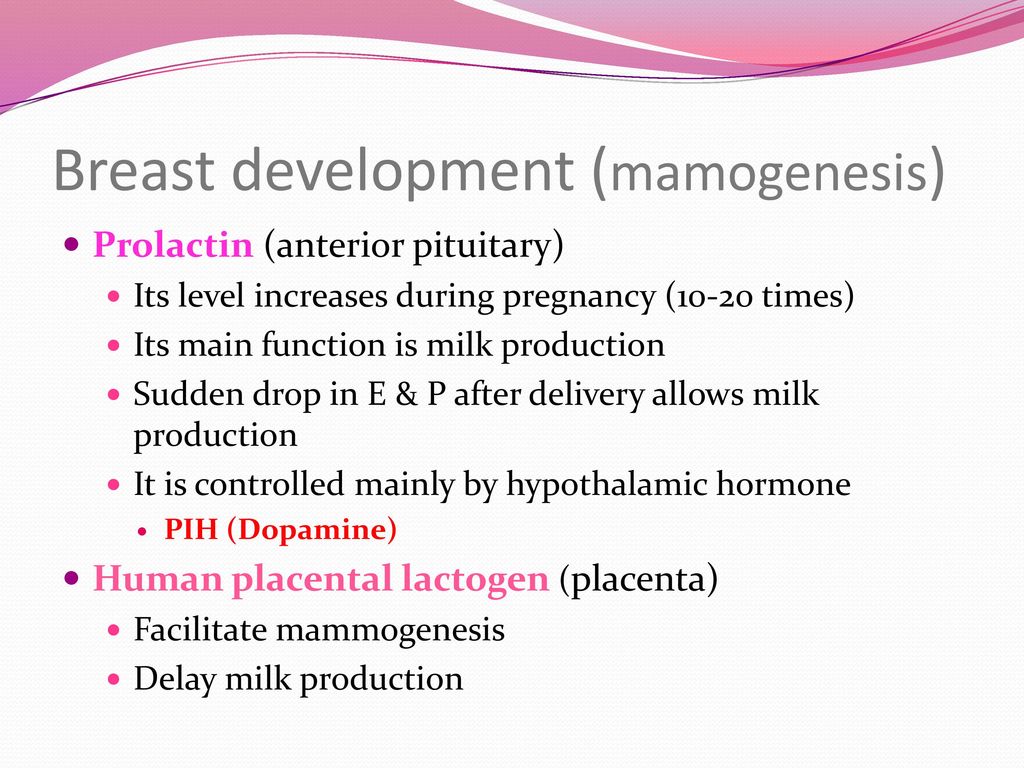
This is, first of all, intrauterine fetal growth retardation - a lag in the size of the fetus and a slowdown in its growth. Often there is a change in the motor activity of the fetus. At first there may be some increase in movements, and then a decrease. Violation of the protective function of the placenta leads to intrauterine infection of the fetus under the action of pathogenic (pathogenic) microorganisms penetrating the placenta. The fetus, the development of which occurs in conditions of placental insufficiency, is much more at risk of trauma during childbirth, they have a violation of adaptation to extrauterine life, increased morbidity in the first year of life.
According to the time of occurrence, doctors divide placental insufficiency into early and late.
Early (or primary) placental insufficiency
Develops before 16 weeks of gestation. It occurs already at the stage of placenta formation and is associated with diseases of a pregnant woman that are present before pregnancy, for example, with uterine pathology, chronic arterial hypertension, and endocrinological diseases.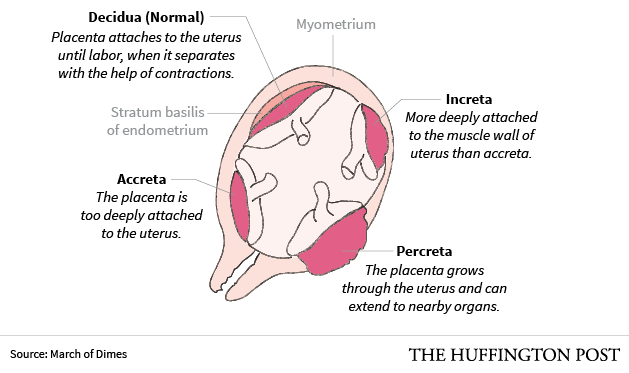 In this case, the formation of defective vessels in the placenta occurs.
In this case, the formation of defective vessels in the placenta occurs.
Late (or secondary) placental insufficiency
Occurs after 16 weeks of pregnancy and is most often associated with diseases that have already occurred during pregnancy. Most often, these are iron deficiency anemia (that is, a decrease in the concentration of hemoglobin and iron in the blood), gestational diabetes mellitus (that is, a violation of the absorption of glucose by the body that occurred during pregnancy), past viral and bacterial infections.
It is important to subdivide placental insufficiency into compensated and decompensated forms.
Compensated placental insufficiency
It develops, for example, with the threat of abortion and mild forms of late preeclampsia, if these complications are successfully amenable to medical correction.
Decompensated placental insufficiency
Causes the development of fetal growth retardation, chronic intrauterine hypoxia, up to fetal death.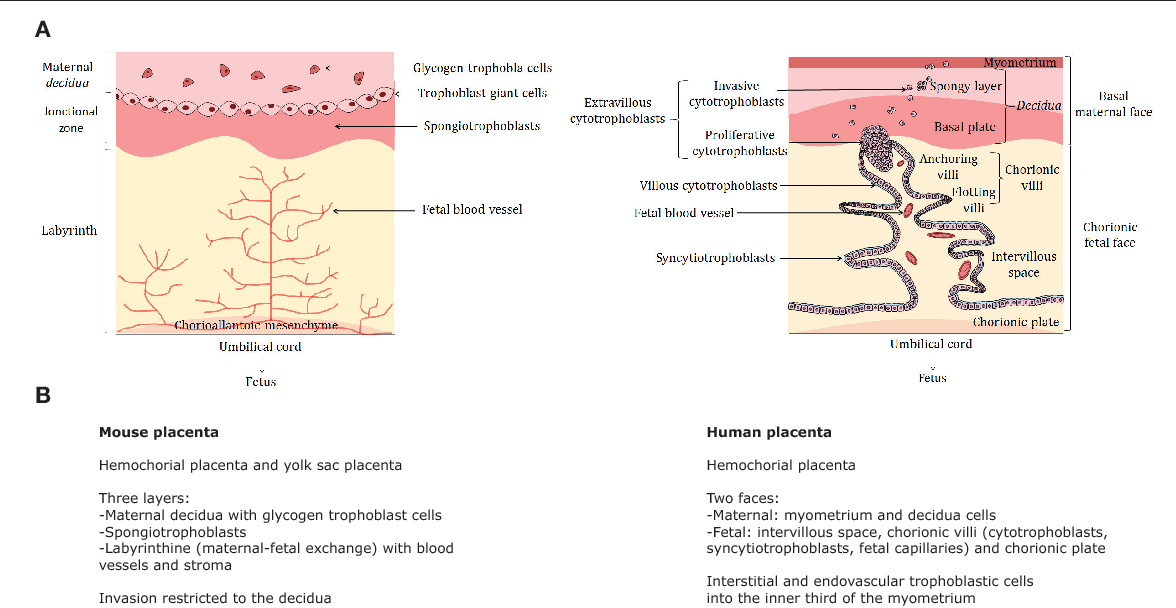
Diagnosis of placental insufficiency
It is almost impossible to treat an already developed placental insufficiency, so doctors actively seek to identify pregnant women at risk of developing placental dysfunction. If placental insufficiency is detected in the 3rd trimester of pregnancy, there is no effective treatment, unfortunately. Therefore, all methods of identifying in the early stages of pregnancy those women whose formation of the placenta has been disturbed are being very actively used.
First of all, when registering for pregnancy, the most significant risk factors are identified - smoking, abortions, aggravated heredity (low birth weight, tendency to thrombosis), the presence of chronic diseases of the heart, blood vessels, diabetes mellitus.
Preventive measures against the development of placental insufficiency are especially relevant and necessary until 16-17 weeks of pregnancy, when the formation of placental structures occurs.
Significant assistance in assessing the risk of developing placental insufficiency is provided by prenatal screening, which is carried out at 11-14 weeks of pregnancy.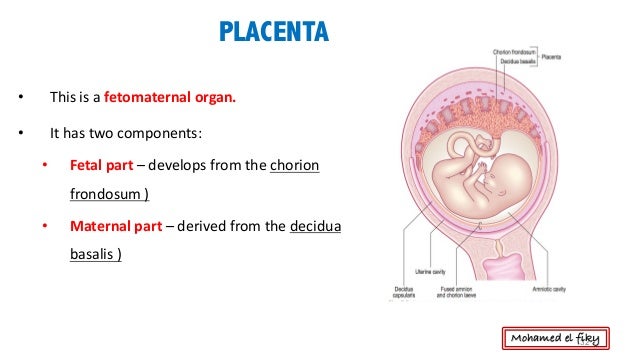 It is carried out to detect Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most relevant is to conduct a comprehensive early screening of a pregnant woman to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation. Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic within the framework of compulsory medical insurance, but is available to everyone in prenatal diagnostic centers.
It is carried out to detect Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most relevant is to conduct a comprehensive early screening of a pregnant woman to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation. Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic within the framework of compulsory medical insurance, but is available to everyone in prenatal diagnostic centers.
Determination of proteins produced by the placenta
First of all, the PAPP-A protein is determined, it is also a marker of chromosomal abnormalities of the fetus. A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of gestation occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
The second placental hormone that helps in assessing the risk of placental insufficiency is PIGF (placental growth factor).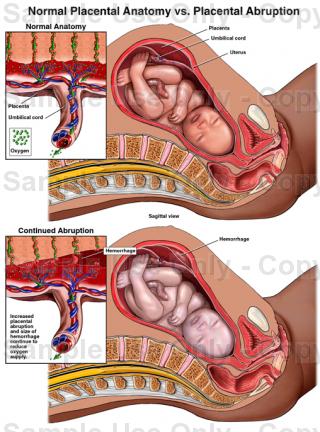 Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not as widely used as PAPP-A, but many laboratories have already included this protein in 1st trimester prenatal screening. It is extremely important when screening the 1st trimester to measure blood flow in the vessels of the uterus. It has been unambiguously proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and lead to a decrease in the nutrition of the baby and the supply of oxygen, that is, to the development of placental insufficiency and fetal growth retardation. With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not as widely used as PAPP-A, but many laboratories have already included this protein in 1st trimester prenatal screening. It is extremely important when screening the 1st trimester to measure blood flow in the vessels of the uterus. It has been unambiguously proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and lead to a decrease in the nutrition of the baby and the supply of oxygen, that is, to the development of placental insufficiency and fetal growth retardation. With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
The next mandatory screening ultrasound is at 20-21 weeks of gestation. In this case, measurements of the fetus must be carried out in order to assess whether there is a lag in growth.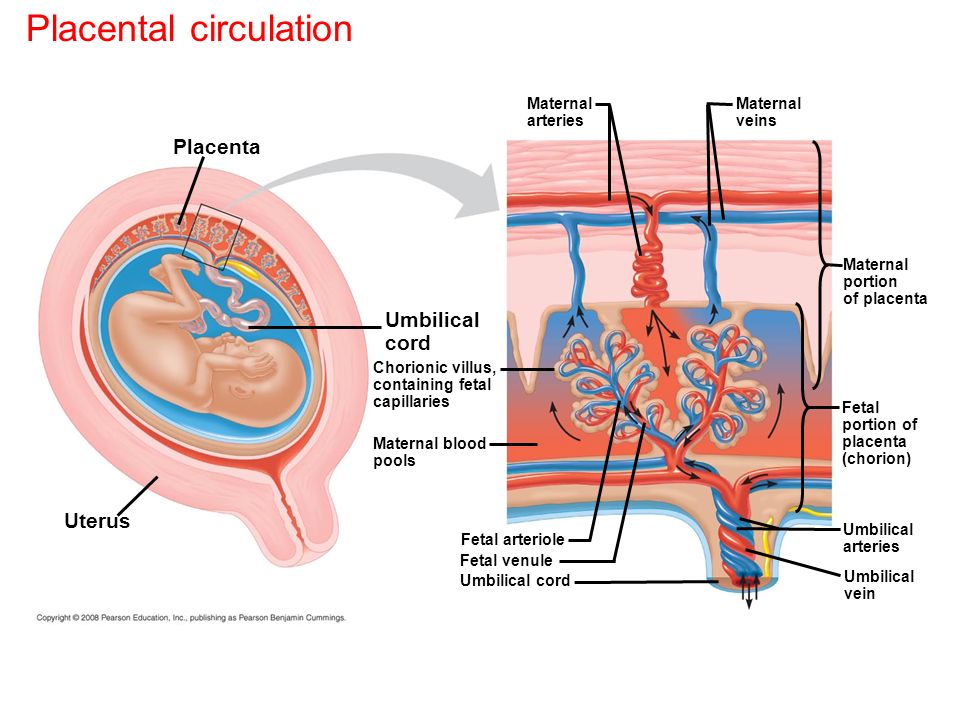 After all, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each period of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta. During ultrasound, dopplerometry of the uterine vessels is also performed to detect early changes that precede the clinical manifestations of placental insufficiency.
After all, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each period of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta. During ultrasound, dopplerometry of the uterine vessels is also performed to detect early changes that precede the clinical manifestations of placental insufficiency.
In patients belonging to the high-risk group, in addition to ultrasound and dopplerometry, daily monitoring of blood pressure fluctuations is also carried out, the amount of protein in the urine sample collected per day is determined, and the indicators of the blood coagulation system are evaluated.
The third ultrasound is performed for all expectant mothers at 30-34 weeks of pregnancy. The doctor measures the circumference of the head and abdomen of the crumbs, the length of the bones of his arms and legs, and calculates the estimated weight of the fetus. These measurements allow the doctor to make sure that the baby is developing normally.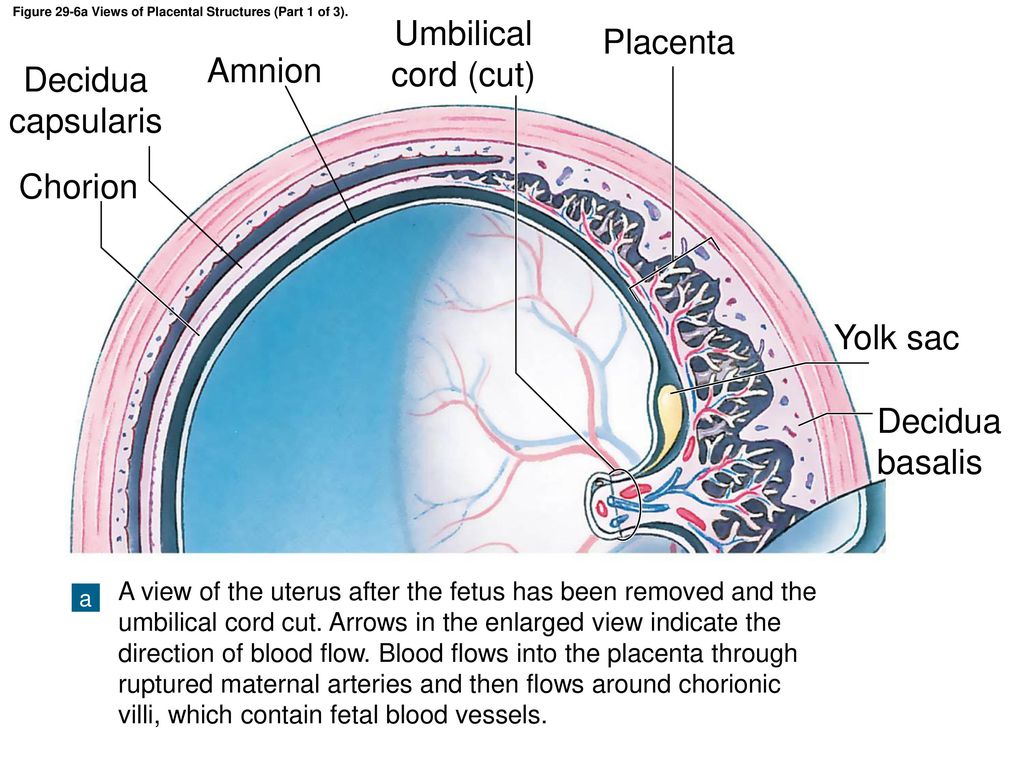 The structure of the placenta is also important, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that it ceases to have enough oxygen and nutrients and the development of the child is disturbed. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
The structure of the placenta is also important, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that it ceases to have enough oxygen and nutrients and the development of the child is disturbed. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
Doppler
Doppler of the placental and umbilical cord vessels (method of studying blood flow velocities in these vessels) also allows you to assess the well-being of the baby. The doctor examines the blood flow in the arteries of the uterus, umbilical cord, heart and brain of the child. This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of preeclampsia in the mother. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.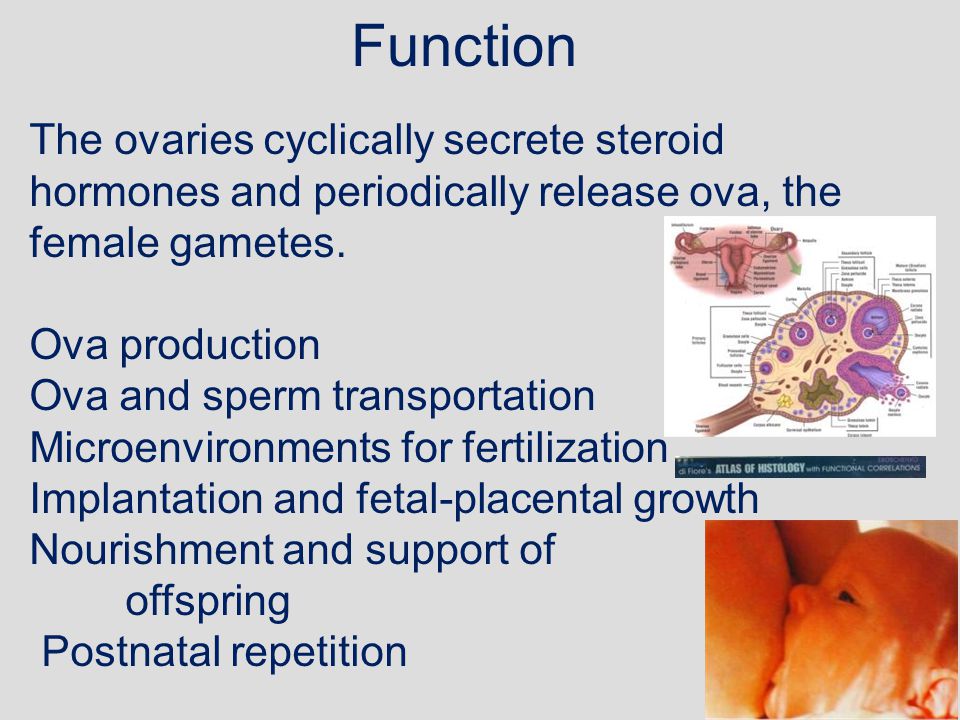
A well-timed examination makes it possible to identify the initial stages of blood supply deficiency. In such cases, treatment can prevent formidable complications, such as hypoxia and intrauterine growth retardation of the baby. Dopperometry is carried out at 20-21 weeks and at 30-32 weeks of pregnancy, if there are changes, control is carried out at least every two weeks.
Cardiotocography
This is an important method for assessing the condition of the fetus. CTG is performed at a gestational age of 33 weeks or more, since only at this stage of the intrauterine development of the baby is a complete regulation of the activity of the cardiovascular system of the fetus established by the centers of the spinal cord and brain. Recording of fetal heartbeats is carried out for 20-40 minutes, and if necessary, the study can be extended up to 1.5 hours.
The device registers and records the baby's heart rate. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach.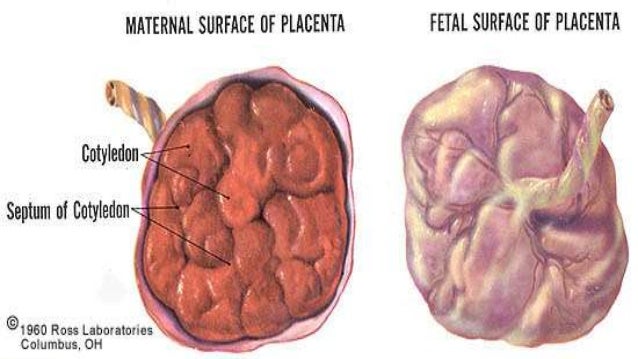 For example, with a decrease in the concentration of oxygen in the blood of the fetus, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks 1 time in 10-14 days, sometimes more often. Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant in the presence of signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby's heart activity and these data are transmitted via the Internet to the attending physician.
For example, with a decrease in the concentration of oxygen in the blood of the fetus, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks 1 time in 10-14 days, sometimes more often. Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant in the presence of signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby's heart activity and these data are transmitted via the Internet to the attending physician.
Treatment of placental insufficiency
There are currently no specific treatments for placental insufficiency because there are no drugs that selectively improve uteroplacental blood flow. That is why all measures to combat placental insufficiency are aimed at prevention. If the patient is at high risk for the development of placental insufficiency, from early pregnancy she is prescribed drugs whose effectiveness is well proven and which prevent the early development of severe placental dysfunction.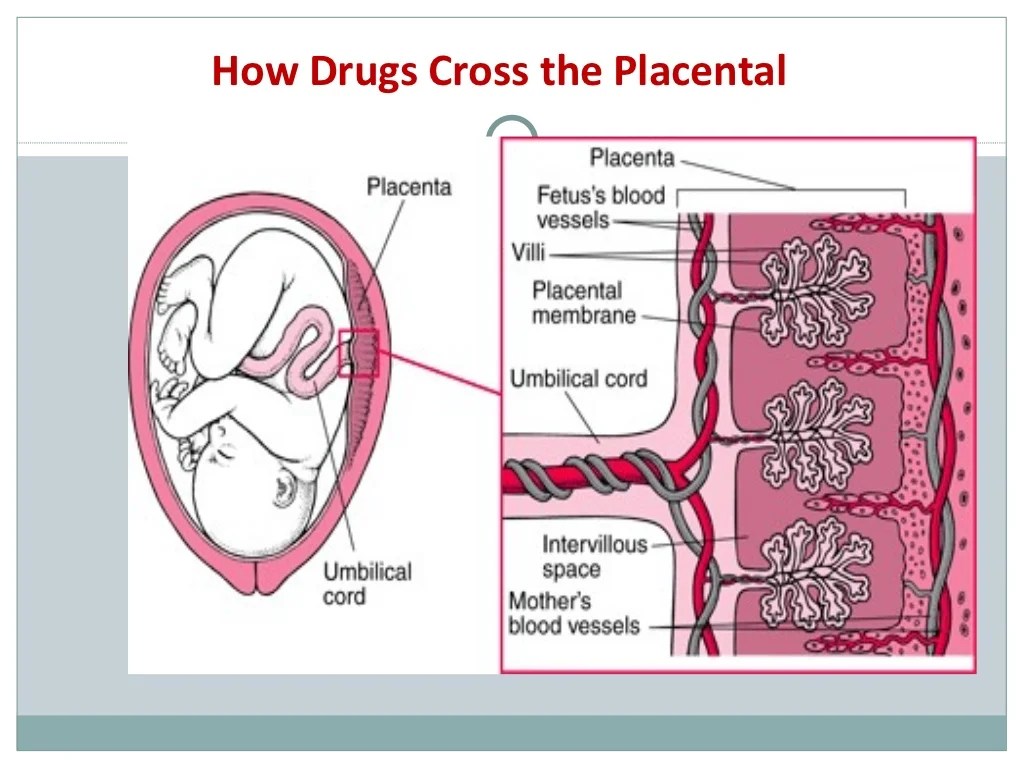
If during the additional methods of assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the flow of blood and oxygen through the placenta and mandatory control examinations against the background of ongoing therapy. If the changes are serious and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, then in such cases an emergency delivery is performed.
Complex therapy of pregnant women with metabolic syndrome and placental insufficiency
One of the main indications for the use of hyperbaric oxygen therapy (HBO) in obstetrics is placental insufficiency (PN). This is a complex dysfunctional state of the placenta, which occurs as a result of a violation of trophoblast invasion, leading to metabolic disorders in the fetus, a decrease in its compensatory-adaptive reactions [7]. The widespread use in obstetric practice of ultrasound diagnostics with Doppler ultrasound has made it possible to diagnose and treat this pathology at an earlier stage of pregnancy [4, 8]. The effectiveness and safety of the HBOT method gave grounds for its widespread use in the complex therapy of PN [3].
The effectiveness and safety of the HBOT method gave grounds for its widespread use in the complex therapy of PN [3].
Violation of blood circulation in the placenta is accompanied by changes in metabolism, which contributes to the development of enzymatic and hormonal insufficiency of the placenta [12].
The placenta plays a significant role in the regulation of lipid peroxidation (LPO) in the fetus [1, 6]. With PN, the content of total lipids, free cholesterol, and triglycerides in the placenta is significantly reduced. At the same time, lipid peroxidation was increased against the background of a decrease in the activity of the antioxidant system. The accumulation of toxic lipid peroxidation products in cells leads to disruption of the structure and permeability of biological membranes. Increased lipid peroxidation and changes in the activity of the antioxidant system play a role in the pathogenesis of preeclampsia, PI, and intrauterine growth retardation.
Pregnant women with metabolic syndrome represent a special group.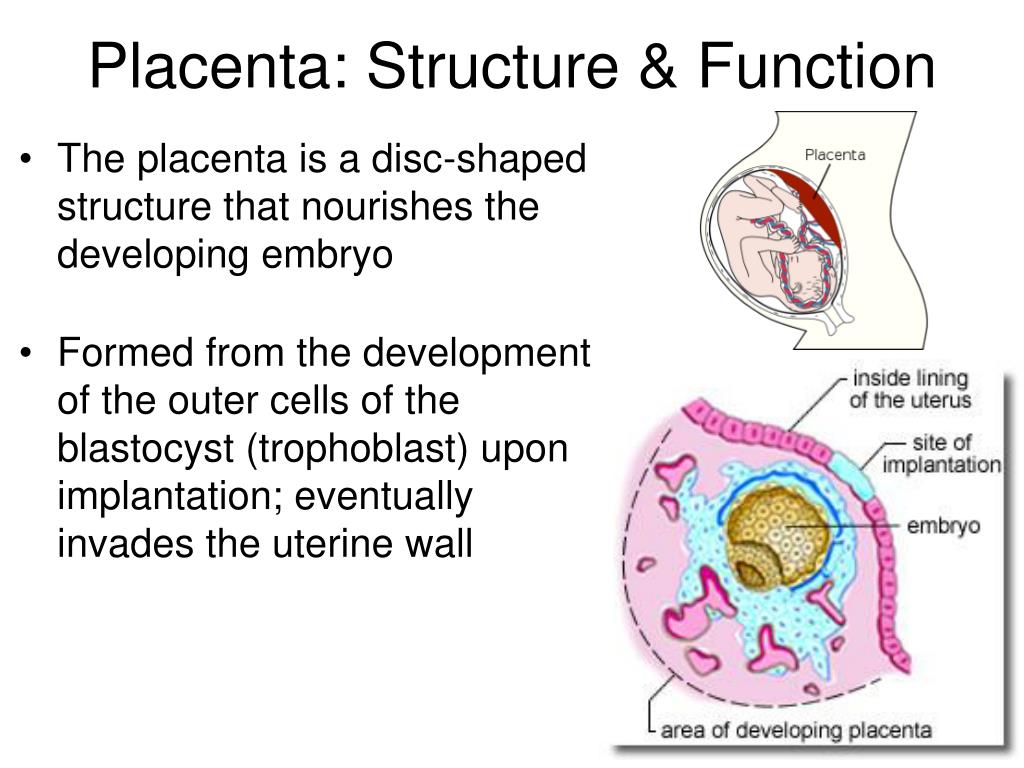 Along with various complications of pregnancy (preeclampsia, gestational diabetes mellitus, etc.) [14], this group of patients has PI, manifested by pronounced changes in the uteroplacental, fetal-placental blood flow. In this regard, the study of methods for correcting this pathology is an important problem in obstetric practice [10, 11].
Along with various complications of pregnancy (preeclampsia, gestational diabetes mellitus, etc.) [14], this group of patients has PI, manifested by pronounced changes in the uteroplacental, fetal-placental blood flow. In this regard, the study of methods for correcting this pathology is an important problem in obstetric practice [10, 11].
The purpose of this study is to evaluate the effectiveness of complex treatment of PI in pregnant women with metabolic syndrome using HBO.
Material and methods
For the study, 148 pregnant women with metabolic syndrome were selected whose pregnancy was complicated by PI. The age of the surveyed ranged from 21 to 32 years (mean age 26±1.8 years), the average body mass index (BMI) was 27±1.1 kg/m 2 . The control group included 50 healthy pregnant women with normal body weight, mean BMI 21±1.6 kg/m 2 . All patients underwent a general clinical examination (anamnesis, assessment of anthropometric parameters), instrumental (Doppler study of blood flow in the uterine and spiral arteries, in the umbilical artery and its terminal branches, aorta and middle cerebral artery of the fetus) and laboratory examination (determination of the content of placental lactogen - PL, products of free radical oxidation of lipids: diene conjugates - DC; malondialdehyde - MDA).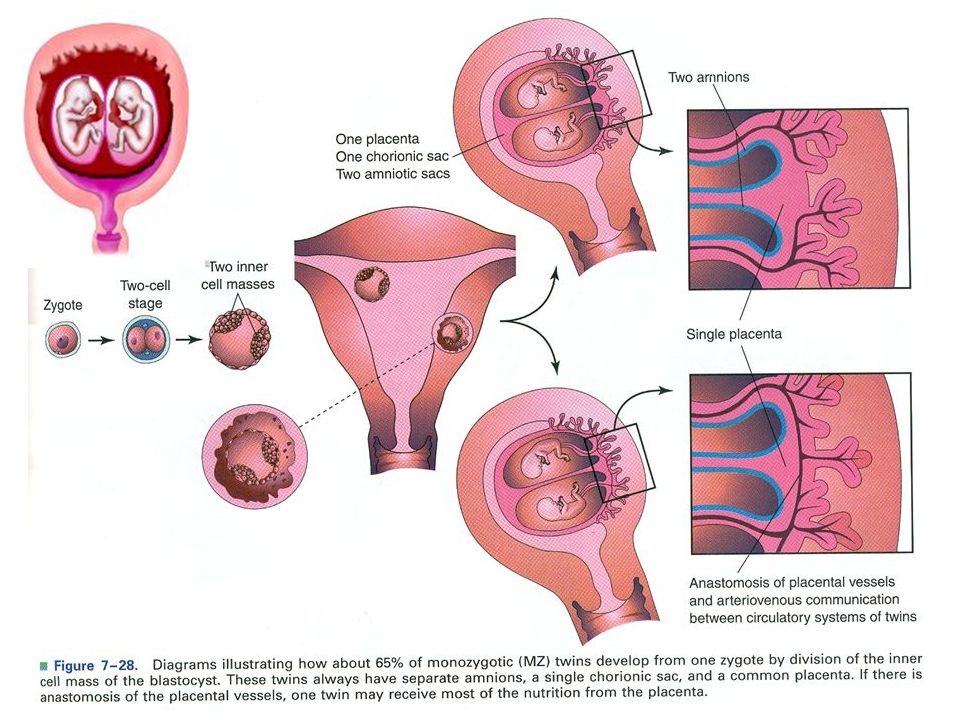
Statistical data processing was performed using the Statistica 5.0 program, the significance of the obtained differences was assessed by the nonparametric Wilcoxon and Mann–Whitney tests. Differences were considered significant at p<0.05.
Treatment of PN was carried out in accordance with the recommendations of G.M. Savelyeva (2008). As a traditional therapy, all patients were prescribed standard schemes of β-agonists (ginipral), vasoactive drugs (trental), antihypoxants (actovegin), hepatoprotectors (Essentiale forte) and vitamin therapy. In terms of pregnancy more than 38 weeks, preparation for childbirth was carried out, which included the introduction of antispasmodics and prostaglandins.
Treatment of preeclampsia was carried out by complex infusion therapy, including magnesium, as well as antihypertensive and sedative therapy. In case of ineffectiveness of the treatment of preeclampsia, early delivery was performed. If concomitant somatic pathology was detected, it was corrected.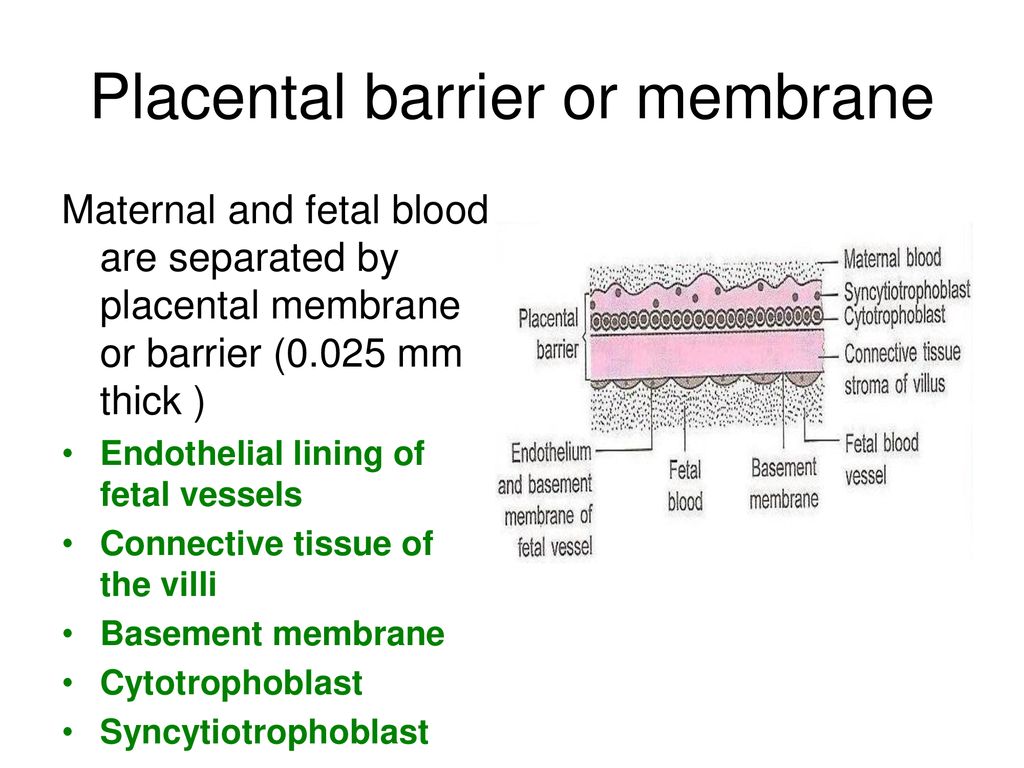
In addition to therapy, a course of HBO was prescribed. Oxygen therapy was carried out in the pressure chamber OKA-NT and BL-301 in the mode of 1.3 ata per isopressure for 40 minutes at an oxygen circulation rate of 40 l/min. The total duration of the session, taking into account compression and decompression, is 60 minutes. The course consisted of 8-10 sessions, 1 time per day.
Before and after the HBOT session, it was obligatory to measure the frequency of respiration, pulse, arterial pressure and heart rate of the fetus.
To evaluate the effectiveness of this therapy, the patients were divided into two groups: group 1 — 78 patients who received in combination with the main HBO therapy; group 2 (comparisons) — 70 patients who did not receive HBO.
Results and discussion
Obtained data (Table 1) showed that the content of PL in the blood serum of pregnant women suffering from metabolic syndrome with PI is reduced by 26% compared with the control group.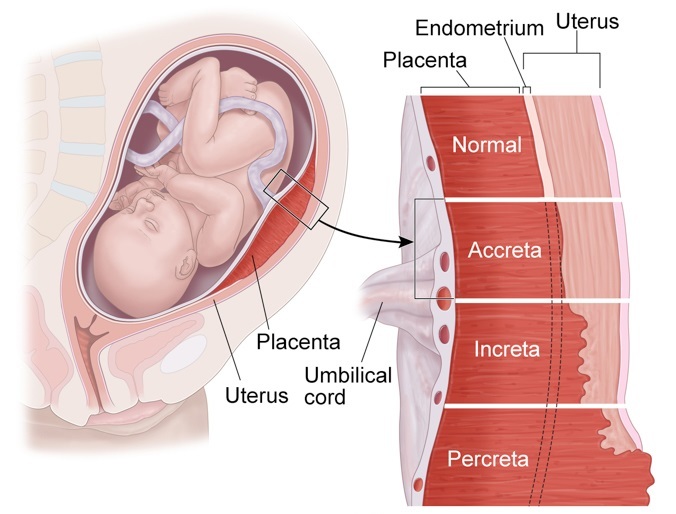 After treatment, the concentration of PL increased, and in the group of pregnant women who received HBO in the complex therapy, to a greater extent than in the group without HBO.
After treatment, the concentration of PL increased, and in the group of pregnant women who received HBO in the complex therapy, to a greater extent than in the group without HBO.
One of the main manifestations of PI is a violation of the hormonal function of the placenta, which is 2–3 weeks ahead of clinical manifestations [5, 15].
Thus, the appointment of HBO in the complex treatment of PI leads to an improvement in the indicators of the hormone-synthesizing function of the placenta.
Based on the results obtained, it can be concluded that it is possible to use the dynamic determination of the hormone to assess the condition of the fetus, the effectiveness of the treatment and decide on the tactics of pregnancy and delivery, which is consistent with the data of domestic studies [9].
In the study by V.N. Serov [12] revealed a significant pattern of changes in the level of PL in the blood of pregnant women with late toxicosis, depending on its severity.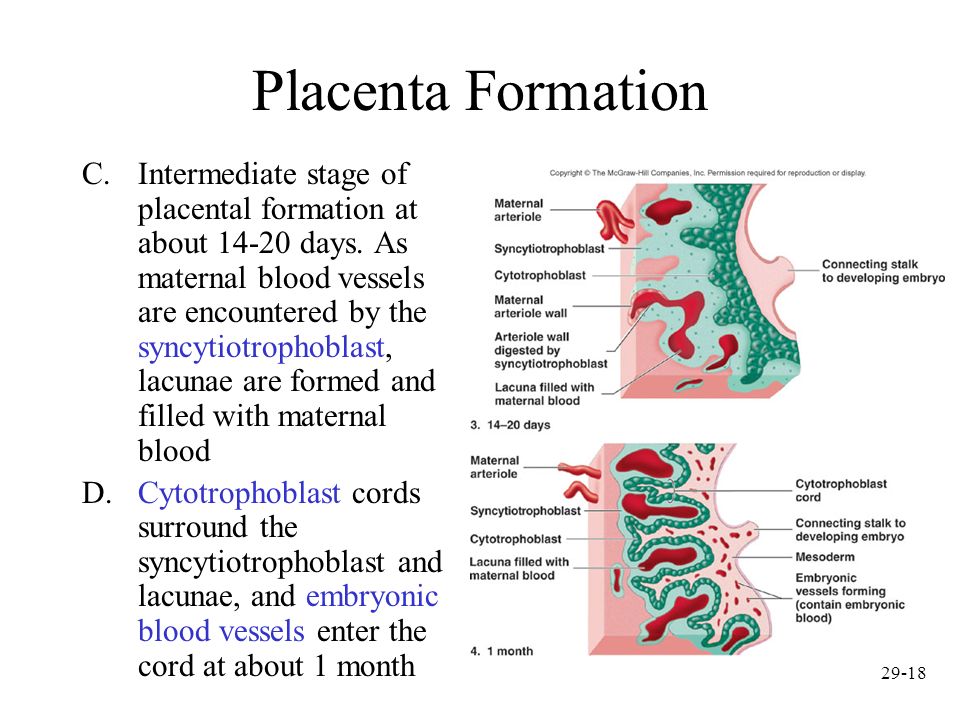
I.S. Sidorova et al. [13] also showed that chronic PI is accompanied by a decrease in the concentration of PL in proportion to the degree of fetal growth retardation syndrome.
In the present study, it was found that in the metabolic syndrome there is an increase in the processes of free radical oxidation of lipids and HBO directly affects this process (Table 2).
The concentration of MDA and DC before treatment in pregnant women with metabolic syndrome was significantly increased compared with the control group of patients. After treatment, the concentration of lipid peroxidation products significantly decreased compared to the values before treatment, and in the 1st group of patients to a greater extent than in the comparison group.
The results obtained are consistent with the study by G.Ts. Aroyan [2], who showed that in the syndrome of fetal growth retardation, there is a pronounced increase in the level of MDA, a change in the concentration of free fatty acids, and a decrease in the activity of growth hormone.