What does a baby rash look like
Baby Rashes: Types, Symptoms & More
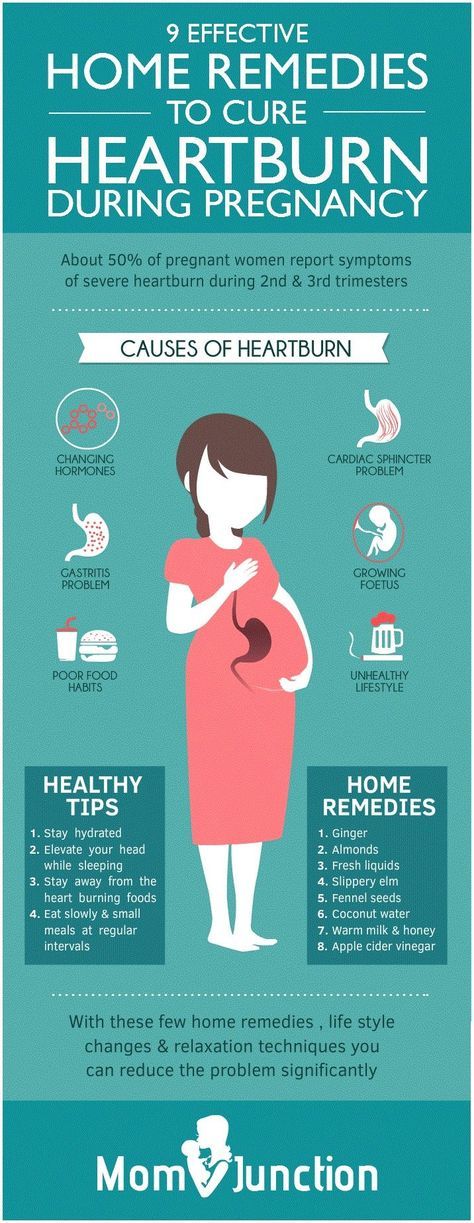
Baby’s have incredibly sensitive skin, which makes them more likely to develop rashes than adults and older kids. But with all the different types out there, it can be hard to identify what the baby rash is, what’s causing it and how to treat it. Plus, no parent wants to see their precious little one with a red or bumpy reaction on their soft skin. Many might wonder how rashes affect baby’s comfort level and whether they cause itchiness or pain. And how can parents tell if baby’s rash is a harmless diaper rash or something a little more serious?
Because there are so many types of baby rashes, it’s important to be aware of the symptoms to look out for and know when to call the pediatrician. To help you better identify a baby rash on the body, we’ve put together a handy guide on all things rashes. Keep reading to learn more about the common types of baby rash, tell-tale signs and symptoms and the best remedies to treat them.
In this article:
Baby rash causes
baby acne or baby rash?
Baby heat rash
Meningitis rash
Strep rash
Chicken pox
Baby drool rash
Baby eczema rash
Hives
Baby allergy rash
Baby fungal rash
Cradle cap
When to be concerned about baby rashes
Baby Rash Causes
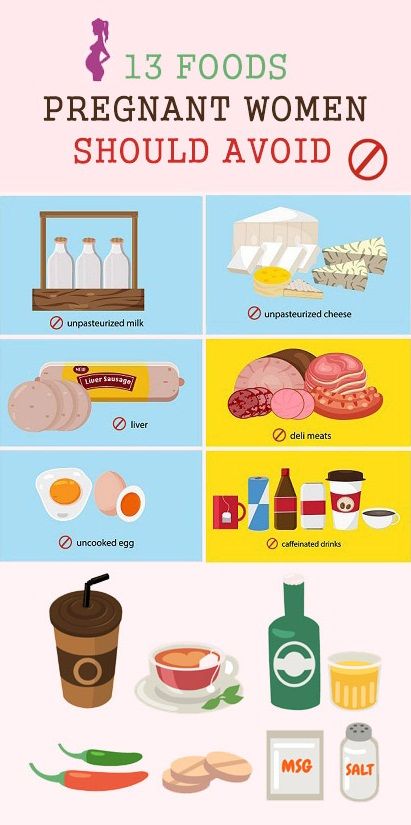
When it comes to baby rashes, there are many types and many culprits. Some common causes include:
-
Irritants. Common irritants that can bother baby’s sensitive skin are saliva and drool, poop, baby wipes, detergents, soaps, sunscreen and nickel.
-
Allergies. Allergic reactions can cause a baby rash to appear in a bunch of different forms. Rashes can be itchy, welt-like hives or dry, itchy patches. Eczema is the most common version of a baby rash caused by allergies.
-
Infections. Infections can lead to different types of baby rash, the most common of which are fungal rashes. Sometimes, however, a viral baby rash can develop. “These rashes occur when babies have specific viral illnesses and may be associated with fever or other symptoms,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. A viral baby rash can appear as small dots on the torso and sometimes arms and legs, and can last for several days to a week.
 It may spread for a few days and then begin to clear up.
It may spread for a few days and then begin to clear up.
“Baby’s skin barrier is especially fragile because it’s thinner, immature and the skin is still developing, so that makes it a lot more vulnerable to damage and dryness. It’s also more reactive, especially to things that could be irritants,” explains Lauren R. Crosby, MD, FAAP, a pediatrician at LaPeer Pediatrics in Beverly Hills, California. Baby’s skin is typically ultra-sensitive from birth until around age 2, although diaper rash can continue to rear its head past that age until kids are potty trained.
In our guide below, we outline the different ways baby rashes look and behave. Keep reading for the most common types of baby rash to keep an eye out for, plus how to prevent and treat them. From heat rashes to chicken pox, we help make sense of any bumps or blotches you may find on baby.
Baby Acne or Baby Rash?
Breakouts aren’t just for teenagers—it’s actually totally normal for babies to get acne. “Also known as neonatal acne, it’s a common rash in babies during the first month of life,” Bender says. “It’s thought that maternal hormones—those that pass from mother to baby in utero—may cause baby acne to flare.”
“Also known as neonatal acne, it’s a common rash in babies during the first month of life,” Bender says. “It’s thought that maternal hormones—those that pass from mother to baby in utero—may cause baby acne to flare.”
But how can you tell if it’s baby acne or a baby rash? Baby acne typically looks like a bunch of small, red bumps, as opposed to the lacy red of a baby rash.
Image: iStock
Baby acne symptoms
- Pimples. Baby acne usually involves clusters of tiny red pimples and whiteheads.
- Irritated cheeks. Baby acne usually develops on the cheeks, but it can also appear on baby’s nose, forehead and sometimes behind the ears and on the scalp.
- Persistent symptoms. Baby acne can last up to three to four months.
Prevention and treatment
Usually, baby acne clears up on its own with gentle cleansing. Once in a while parents might need to see a dermatologist if it’s persisting beyond the normal three to four months, but that’s pretty rare.
Baby Heat Rash
Baby heat rash tends to happen when baby’s sweat glands become blocked and trap sweat under the skin, Crosby says. It’s usually seen in warm weather or when baby is overdressed. How do you know if the baby rash is caused by heat?
Image: Shutterstock
Heat rash symptoms
- Tiny red bumps. These typically appear on baby’s head, neck and shoulders, and sometimes on the chest.
- Itching. Sometimes heat rash can be itchy, so take note if baby is scratching at their irritated skin.
Prevention and treatment
To prevent baby heat rash, dress baby in lighter clothing to make sure they aren’t getting overheated or sweaty. In warm climates, it’s fine to let them sleep in just a onesie and diaper, and run a fan in the bedroom to keep the air cool and circulating. When baby heat rash does strike, “I recommend a daily bath with a non-fragrant sensitive skin cleanser to help clear out the sweat and keep the skin clear,” Crosby says. A baby rash from heat usually goes away on its own in three to four days, as long as baby isn’t overdressed and stays in a cool environment.
A baby rash from heat usually goes away on its own in three to four days, as long as baby isn’t overdressed and stays in a cool environment.
Baby Diaper Rash
It’s pretty self-explanatory where you can expect to see this baby rash. “Diaper rash can occur due to irritation from wet diapers and friction,” Bender says. Baby diaper rash is even more common in older babies who sleep through the night longer and may have wetter diapers in the morning.
Image: Shutterstock
Diaper rash symptoms
- Red patches. These typically appear on the rounded part of baby’s bottom.
- Puffy, warm skin. In some cases, baby’s skin may be slightly raised and feel warm to the touch.
Prevention and treatment
“Diaper rash can improve with frequent diaper changes and use of over-the-counter diaper paste containing zinc oxide, which helps in acting as a barrier to prevent friction and irritation in the diaper area,” Bender says. Ward off baby diaper rash by making sure the skin is completely dry before you put on a fresh diaper. In the past, baby powder was the go-to trick for absorbing moisture and protecting baby’s skin, but doctors no longer recommend using powder for diaper rash, since inhaled powder can irritate baby’s lungs.
Ward off baby diaper rash by making sure the skin is completely dry before you put on a fresh diaper. In the past, baby powder was the go-to trick for absorbing moisture and protecting baby’s skin, but doctors no longer recommend using powder for diaper rash, since inhaled powder can irritate baby’s lungs.
Sometimes a rash on baby’s butt can actually be a yeast rash caused by fungus that lives on our skin.
Image: iStock
Yeast rash symptoms
- Pink patches. These patches usually appear in baby’s skin folds, accompanied by small pink dots or pustules around the edge.
Prevention and treatment
To treat a baby yeast rash, apply a topical, over-the-counter antifungal cream a few times a day. Prevent yeast rash by keeping baby clean and dry.
Meningitis Rash
Meningitis is when the lining around the brain and spinal cord (the meninges) is inflamed, and “is a serious infection because it can be present in the blood and brain and cause organ damage, permanent brain damage or death,” Bender says.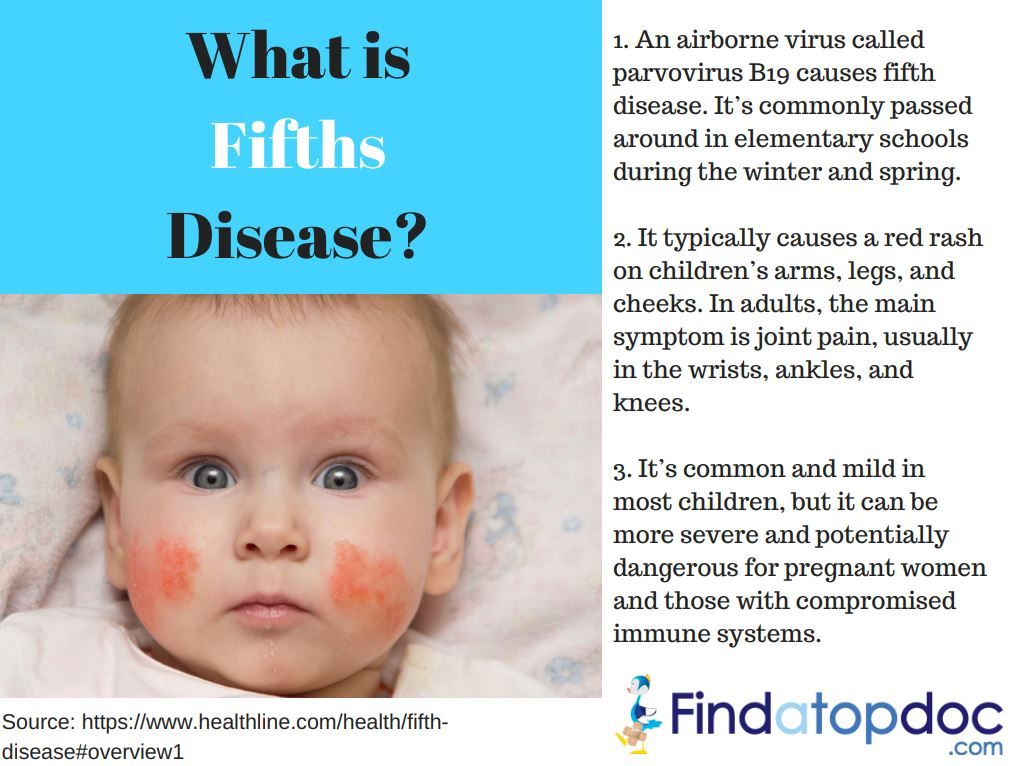
While the viral form of meningitis is serious, it’s almost never life-threatening, according to the Centers for Disease Control and Prevention (CDC). Bacterial meningitis, however, can be deadly and calls for immediate medical attention. There’s a vaccine for bacterial meningitis, but it typically isn’t given until later in childhood or before college. You can’t tell the difference between a baby rash caused by bacterial or viral meningitis, and in many cases a rash won’t appear at all.
Image: iStock
Meningitis symptoms
- High fever. Take baby’s temperature, since a high fever is a classic sign of meningitis.
- Lethargy. If baby is less active than usual, it could be another signal of meningitis.
- Vomiting. This symptom is more common in infants, along with a loss of appetite and irritability.
- Rashes. Meningitis rashes can vary in appearance, but the most common ones include pink or red dots all over, purple rashes that can look like tiny bruises or broken capillaries in the skin, and an itchy, red rash.
Prevention and treatment
Viral meningitis usually clears up on its own in seven to 10 days, but bacterial meningitis requires immediate medical attention so antibiotics can be given as soon as possible. Serious cases may call for hospitalization. If you think baby might have meningitis, call your doctor right away—they can determine if baby has the disease and the type of meningitis.
Strep rash
A strep rash on baby is another type of viral baby rash. Your child is more prone to strep rash if other family members have been exposed to strep throat.
Image: iStock
Strep rash symptoms
- Bright red skin. Strep rash on baby can be bright red and beefy-looking with wet, oozing patches in neck folds, or as a bright red circle patch in the area around baby’s anus, Bender says.
- Blisters and scabbing. Spotting scabs and blisters on baby’s skin is another common sign of strep.
Prevention and treatment
Since strep can spread from person to person through close contact, keep baby away from infected people. Unlike your run-of-the-mill neck rash, which can be treated with over-the-counter antifungal creams, strep requires a visit to the doctor. Once the diagnosis of strep rash is confirmed—typically with a skin swab test—your pediatrician may prescribe an oral antibiotic as treatment.
Chicken Pox
Chicken pox appears as a baby rash on the body. Before the chicken pox—or varicella—vaccine became available in 1995, practically every child came down with chicken pox before age 9, according to the American Academy of Pediatrics (AAP). Nowadays, it’s pretty rare for babies to get chicken pox, thanks to the vaccine. It’s a super-contagious viral infection caused by the varicella zoster virus, so avoid contact with infected people to keep baby safe.
Image: Shutterstock
Chicken pox symptoms
- Red bumps and blisters. Chicken pox causes a blister-like baby rash on the skin, starting on the back, tummy or face and spreading all over baby’s body.
 The blisters are often in different stages of healing, so some may look like pink bumps, some look like scabbed bumps and others may look like blisters.
The blisters are often in different stages of healing, so some may look like pink bumps, some look like scabbed bumps and others may look like blisters. - Itchiness. Chicken pox rashes are renowned for their intense itchiness.
- Fever. A temperature of 101 to 102 degrees Fahrenheit is common with chicken pox.
Prevention and treatment
Doctors recommend daily baths and keeping baby’s nails short so they can’t scratch and dig into their skin, which could cause a secondary infection. Typically, the course of treatment for chicken pox is to wait it out—it can last five to seven days—but in severe cases (which aren’t common), an antiviral medication may be prescribed. To prevent chicken pox, the APP recommends that healthy babies get the first dose of the vaccine between 12 and 15 months old, followed by a second dose at age 4 to 6.
Baby Drool Rash
Noticing a baby rash on your little one’s face? When babies’ saliva glands turn on, usually around 3 or 4 months of age, they start to drool. A lot. “If you think about it, saliva is part of your digestive tract,” Crosby says. “It’s not just water, so it’s irritating.”
A lot. “If you think about it, saliva is part of your digestive tract,” Crosby says. “It’s not just water, so it’s irritating.”
Image: Courtesy of Wissabo/Instagram
Baby drool rash symptoms
- A red, irritated baby rash on the face. Because the skin around baby’s mouth, chin and neck is constantly wet, these areas are especially prone to drool rash.
- Flaking skin. Baby rash from drool can also appear slightly flaky and dry-looking.
Prevention and treatment
One way to prevent and heal a baby rash caused by drool? Have a soft bib handy to keep the skin on baby’s face and chest dry. Apply a gentle over-the-counter ointment before and after meals as a barrier to prevent saliva from touching the skin, so baby’s drool rash can heal underneath it.
Baby Eczema Rash
Eczema, often-chronic red, dry patches of skin, is one of the most common skin disorders in babies—in fact, 60 percent of infants get eczema in the first year of life.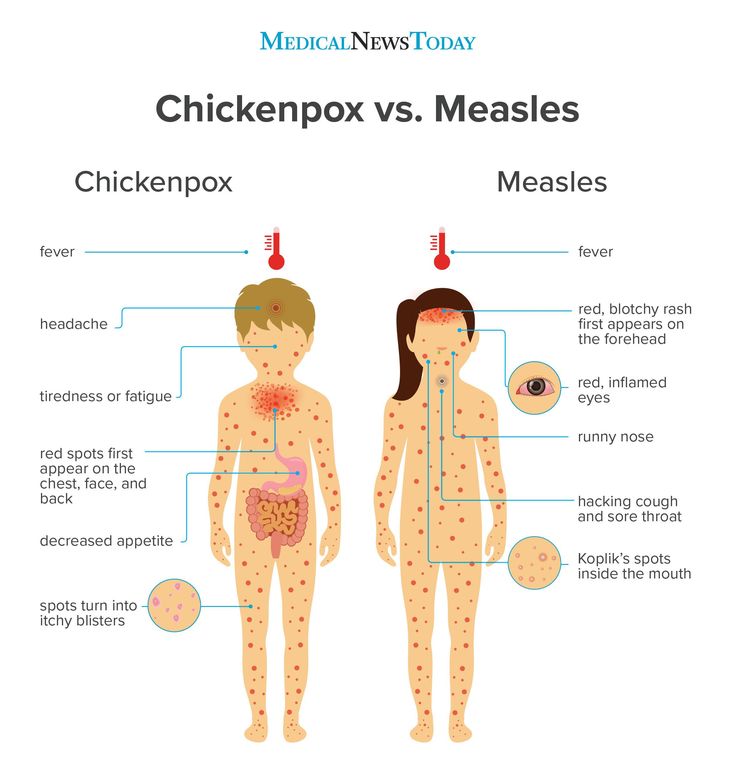 “Sometimes babies scratch so much, it can lead to bleeding and can interfere with sleep,” Bender says. “Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
“Sometimes babies scratch so much, it can lead to bleeding and can interfere with sleep,” Bender says. “Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
Image: iStock
Baby eczema symptoms
- Itchiness. The more severe baby’s eczema is, the more itchy the rash.
- Dry skin patches. This is a common sign of mild eczema.
- Pinker patches of dry, flaky skin. This signifies a moderate case of eczema.
- Red, flaky patches of skin. If baby’s skin is a darker red, it signifies severe eczema, which usually comes with worsened symptoms and intense itchiness across more of the body.
Prevention and treatment
Keeping baby’s skin well moisturized with a daily application of a thick cream can prevent the onset of eczema in infants who are at higher risk for the condition—aka those who have a strong family history of eczema or eczema-related diseases. A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
“Hives can occur soon after baby eats something they’re allergic to or if baby is fighting a virus, in which case the hives may last for several days off and on,” Bender says. They can appear anywhere on the body, even if caused by food. If the baby rash is sparked by something your child touched, it usually appears on the part of baby’s body that came in contact with the allergen. If hives are accompanied by wheezing or if baby’s mouth or tongue starts to swell, see a doctor immediately.
Image: Shutterstock
Hive symptoms
- Pink, blotchy welts. These welts can come and go on baby’s skin.
- Itching. Hive welts are often very itchy.
Prevention and treatment
An oral antihistamine, such as Benadryl, can help treat hives. For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
Baby Allergy Rash
As you expose baby to new products, foods and materials, there’s always a small chance they could be allergic to a certain ingredient or chemical. These rashes can be caused by food or medication that baby’s allergic to, or when baby’s skin comes into contact with an irritant, Crosby says.
So what does an allergy rash look like on a baby? A baby allergy rash can manifest in different ways, but the two most common signs are hives and eczema. As mentioned above, hives usually show up as pink blotchy welts, while eczema appears as red, dry, flaky patches. Both rashes are itchy.
Image: Shutterstock
Allergy symptoms
If you notice the following symptoms, take baby to the ER:
- Swelling of the lips or face. If baby’s lips or face become swollen, it’s a sign of a severe allergic reaction and should be treated by a doctor immediately.

- Wheezing. Any sign of difficulty breathing is a red flag.
Prevention and treatment
“Treatment depends on the age of the child and what is triggering it,” Crosby says. “You want to remove the allergen or trigger if you can, and use a topical or oral allergy medicine.” Sometimes a blood or skin test might be needed to figure out what baby is having an allergic reaction to, and then a baby rash treatment can be prescribed.
Baby Fungal Rash
A fungal baby rash is often caused by chronically wet or irritated skin. A yeast infection is the most common type of fungal rash. It can also appear in babies if another family member or family pet has ringworm.
Image: iStock
Fungal rash symptoms
- Pink, ring-like flaking patches of skin. These flaky patches can pop up anywhere on the skin, including the scalp and diaper area.
Prevention and treatment
“A fungal rash needs a special antifungal cream, or if it’s on the scalp and hair, it may need an oral antifungal medication,” Bender says. To prevent fungal baby rash, keep the skin clean and dry.
To prevent fungal baby rash, keep the skin clean and dry.
Cradle Cap
Essentially dandruff for babies, cradle cap is relatively common and typically caused by yeast. This type of baby rash usually shows up in the first month of life but can occur any time, Crosby says.
Image: iStock
Cradle cap symptoms
- Flaky skin. Rough, yellowish or pink crustry or oily scaly patches on the scalp are a classic sign of this type of baby rash.
- A slight oily scent. This results from the buildup of oil on baby’s scalp in moderate to severe cases.
Prevention and treatment
Most cases of cradle cap can be treated with regular shampooing and a soft scalp brush to loosen the flakes. If that doesn’t cut it, your pediatrician may recommend a medicated shampoo.
In general, the trick to preventing baby rash is keeping your child’s skin healthy. It’s best to keep baths to 10 minutes or less and use lukewarm water, since “during a bath, skin can really lose moisture, and babies are much more prone to getting dry skin,” Crosby says. Hydrating baby’s skin regularly is crucial. The best time to apply lotion? The first five minutes after a bath, to lock in moisture. “The skin is the largest organ in the body and it’s there to protect us from the elements and infections,” Crosby says. “The importance of really caring for it from infancy through adulthood can’t be stressed enough.”
Do baby’s lumps or bumps not line up with any of those listed in this guide? Baby can also develop a rash as a result of bug bites, sunburns, poison ivy and even dry skin. If you’re still not sure about baby’s rash, don’t hesitate to give your pediatrician a call or schedule an appointment.
When to Be Concerned About Baby Rashes
Now that you are familiar with some of the most common kinds of baby rashes, you’re probably wondering, “when should I be concerned about my baby’s rash?”
The truth is, many baby rashes are harmless, and some will come and go on their own without any medical treatment. The other good news is that there are vaccinations to prevent many serious rashes from developing in the first place.
With that said, there are some signs you should keep an eye out for when you notice a baby rash on the body. Some baby rashes can indicate a potentially grave condition, particularly if the rash is persistent or if baby is experiencing swelling or wheezing.
Contact a doctor if baby experiences any of the following:
- If there is pain at the site of the rash
- If baby runs a fever
- If the rash develops bruise-like lesions
- If the rash oozes, bleeds or blisters
- If the rash continues to spread across baby’s body
- If baby develops any cold symptoms (coughing, wheezing, etc.)
- If baby has swollen neck glands or swollen lips
- If the baby rash doesn’t go away after two days
It’s true babies tend to get rashes left and right, but that doesn’t mean you should shrug them off as nothing. Whenever you notice a baby rash on their face or body, keep a watchful eye on it and look out for other symptoms. When it comes to baby’s health, it’s always best to be precautious and proactive.
About the experts:
Anna Bender, MD, is a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. She earned her medical degree from Columbia University College of Physicians and Surgeons in 2007. After completing her residency training in dermatology at New York Presbyterian Hospital - Weill Cornell Medical Center, Bender completed an additional year of specialized fellowship training in pediatric dermatology at the Johns Hopkins University School of Medicine.
Lauren R. Crosby, MD, FAAP, is a parenting expert and pediatrician at LaPeer Pediatrics in Beverly Hills, California. She earned her medical degree at UCLA School of Medicine and afterwards trained at Cedars-Sinai Medical Center, during which time she served as chief resident. She is a member and official spokesperson of the American Academy of Pediatrics.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Baby Skin Care 101
13 Diaper Rash Creams That Work Wonders
The Best Baby Eczema Creams, Shampoos and Washes
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
Treating nappy rashIf your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.

- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.
- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.
Other rashes in the nappy areaIf the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
Childish rash on the body of a child
What is strawberry tongue and slapped cheek syndrome? Why is measles called the first disease and scarlet fever the second? Why does the banal roseola scare parents so much? In honor of Children's Day, we are talking about childhood infections.
Any medical student knows about the six primary exanthems. These are infectious diseases with similar manifestations: they always begin with a fever and are accompanied by skin rashes, which are otherwise called exanthems. Mostly children get sick of them - usually easily, but some infections from this list can be dangerous, while others, although harmless, often make parents nervous. Here is the famous classic six.
First: measles
Measles, which practicing pediatricians have not encountered for a long time, is now on everyone's lips - the outbreak of the first disease has spread to a dozen European countries, and the incidence is growing in Russia.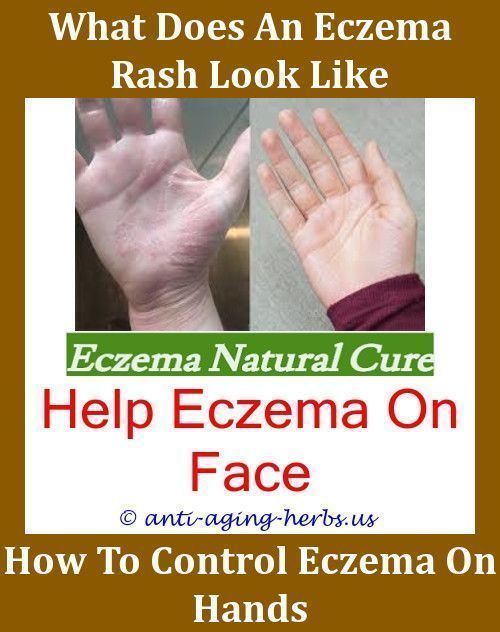 Measles is not as mild a disease as is commonly believed. It is unpleasant to get sick with it even in childhood, and adults, due to the peculiarities of the immune system, endure it hard. In addition, it is dangerous with complications that can develop in anyone: measles pneumonia, purulent otitis media, laryngeal stenosis, bronchitis, kidney, liver and brain damage. The consequence of measles can be deafness or blindness, people still die from it.
Measles is not as mild a disease as is commonly believed. It is unpleasant to get sick with it even in childhood, and adults, due to the peculiarities of the immune system, endure it hard. In addition, it is dangerous with complications that can develop in anyone: measles pneumonia, purulent otitis media, laryngeal stenosis, bronchitis, kidney, liver and brain damage. The consequence of measles can be deafness or blindness, people still die from it.
A typical symptom: spots of Belsky - Filatov - Koplik - a white rash similar to semolina, surrounded by a red border. They appear on the mucous membrane of the cheeks about a day before the measles rash.
Prevention and treatment : there is no cure for measles, the most reliable prevention of infection is a double vaccination.
Second: scarlet fever
All Soviet schoolchildren knew about the existence of this disease - from the gloomy poem "Death of a Pioneer" by Eduard Bagritsky, the heroine of which was dying in the hospital. In the 30s of the last century, when this work was written, scarlet fever was one of the most severe childhood infections. In our time, it is incomparably easier - experts attribute this to both improving the quality of life of children and the availability of antibiotics.
In the 30s of the last century, when this work was written, scarlet fever was one of the most severe childhood infections. In our time, it is incomparably easier - experts attribute this to both improving the quality of life of children and the availability of antibiotics.
Scarlet fever is caused by group A hemolytic streptococcus. It is similar to a sore throat, but is manifested not only by high fever, general malaise and sore throat, but also by a small rash, which usually appears on the cheeks, on the folds of the arms and legs, under the armpits a day after the onset of the disease , on the sides of the body. Scarlet fever is a very contagious disease, according to sanitary standards it is subject to control: having made such a diagnosis, the doctor must inform the epidemic surveillance authority. After recovery, quarantine is established for up to 12 days.
Typical symptom: strawberry tongue - the surface of the tongue is scarlet, dotted with white dots.
Prevention and treatment : hemolytic streptococcus is transmitted by airborne droplets, the risk of infection is reduced by personal hygiene - hand washing, wet cleaning, etc. Scarlet fever is treated with antibiotics.
Scarlet fever is treated with antibiotics.
Third: rubella
Given the high contagiousness of rubella and the fact that the patient begins to isolate the virus long before the onset of the first symptoms, it is easy to get sick with it if there is no vaccination. Often rubella is very mild, sometimes only with a rash, or even asymptomatic. Sometimes, when there are no rashes, it is mistaken for a mild SARS. However, the patient is still contagious.
The main danger of rubella is for pregnant women: infection during pregnancy can lead to interruption or severe pathologies in the fetus. The risk is higher the shorter the gestational age, which is why a blood test for antibodies to rubella and, if it is negative, a subsequent vaccination, are included in the preparation plan for conception. Children are vaccinated against rubella at the same time as measles - at 12 months and 6 years.
A typical symptom: an increase in the cervical lymph nodes before the appearance of a rash, red dots in the sky - the so-called Forksheimer's spots. The rash itself is smooth to the touch, similar to drops of paint. She acts first on the face and behind the ears, then on the rest of the skin.
The rash itself is smooth to the touch, similar to drops of paint. She acts first on the face and behind the ears, then on the rest of the skin.
Prevention and treatment : there is a vaccine for rubella, but no specific treatment.
Fourth: mononucleosis
Previously, the fourth was Filatov-Dukes disease - scarlatinal rubella. It was described as a mild form of scarlet fever, with a low fever, swollen lymph nodes, and a similar rash that went away on its own without complications. Subsequently, it ceased to be considered an independent disease.
Now the fourth disease is called infectious mononucleosis, although it is not always accompanied by a rash. The symptoms of this disease caused by the Epstein-Barr virus are very diverse - it usually manifests itself with fever, sore throat, liver enlargement, general malaise, but joint pain, headaches, herpes on the skin, etc. can also occur. The rash with mononucleosis is similar to red spots are irregular in shape and occur in about 25 percent of cases. There is another type of rash characteristic of this disease: in the event that the patient takes antibiotics prescribed by mistake or "just in case", the so-called ampicillin rash may develop. She, unlike the usual, not associated with antibiotics, can itch - including at night, causing severe discomfort.
There is another type of rash characteristic of this disease: in the event that the patient takes antibiotics prescribed by mistake or "just in case", the so-called ampicillin rash may develop. She, unlike the usual, not associated with antibiotics, can itch - including at night, causing severe discomfort.
Typical symptoms: prolonged fever, inflammation of the tonsils, significant enlargement of the lymph nodes, ampicillin rash.
Prevention and treatment : personal hygiene - Epstein-Barr virus is very common and easily transmitted by airborne droplets and through household contact (mononucleosis is also called the kissing disease). The disease is treated with antiviral and symptomatic drugs.
Fifth: erythema infectiosum
The fifth disease, parvovirus infection, slap disease, is all erythema infectiosum, very common among children. It begins with fever, headache and runny nose, but differs from acute respiratory infections in rashes on the cheeks, and then on the body. The rash slowly passes, sometimes itches, becomes brighter, for example, in the heat. The fifth disease, caused by parvovirus B19, is mild and without consequences. However, there are two categories of people for whom this infection can be dangerous - pregnant women, especially in the early stages, and patients with anemia, in particular sickle cell. If they become infected with parvovirus, they need to see a doctor.
The rash slowly passes, sometimes itches, becomes brighter, for example, in the heat. The fifth disease, caused by parvovirus B19, is mild and without consequences. However, there are two categories of people for whom this infection can be dangerous - pregnant women, especially in the early stages, and patients with anemia, in particular sickle cell. If they become infected with parvovirus, they need to see a doctor.
A typical symptom: in children - slapped cheek syndrome (bright red skin on the cheeks), in adults - joint pain. The rash on the body looks like lace.
Prevention and treatment : personal hygiene, no treatment usually required.
Sixth: roseola
This disease is very frightening for parents, and doctors do not always recognize it, which leads to unnecessary prescription of antibiotics. The child suddenly develops a high temperature, which is difficult to reduce with the help of antipyretics. There are no other symptoms - no cough, no runny nose, no pain of any kind.
In fact, there is nothing dangerous in roseola. It develops when a child becomes infected with the herpes simplex virus type 6. This happens so often that almost all children have time to get sick with roseola before the age of 5. You can only transfer it once in your life.
A typical symptom: exactly after 3 days the temperature returns to normal sharply (hence another name for roseola - children's three-day fever) and a rash appears in another day.
Prevention and treatment : not required - roseola is not dangerous and goes away on its own.
How to recognize scarlet fever and why "stars" on the skin are alarming
Of course, the list of infections that may be accompanied by rashes is not limited to these six diseases. It is quite large - this is chickenpox, and enterovirus infection, and yersiniosis, and shingles, and many others. Unfortunately, among such infections there are also very dangerous ones, in which delay can lead to serious consequences and death of a person. How not to miss such situations, what to pay special attention to when a rash is an alarming symptom, in which cases laboratory tests are needed, says pediatrician Elena Nikiforova, medical expert at the laboratory of personalized medicine LabQuest.
How not to miss such situations, what to pay special attention to when a rash is an alarming symptom, in which cases laboratory tests are needed, says pediatrician Elena Nikiforova, medical expert at the laboratory of personalized medicine LabQuest.
In what cases is it necessary to take tests?
– As a rule, these diseases are diagnosed clinically, because there is a typical picture of the disease. This applies to measles, rubella, roseola, infectious erythema, in which the rash appears at a certain point and in stages. With measles, the diagnosis is further confirmed in the infectious diseases department - this disease is not treated at home. With rubella, the doctor may order general blood and urine tests if there is a suspicion that a bacterial infection has joined.
With scarlet fever, the diagnosis is a test for group A streptococcus. There are home tests that help to differentiate the pathogen on the spot, a throat swab is taken in the laboratory. You need to take the test promptly, at the first symptoms, before starting treatment and even using symptomatic remedies - a throat spray, lozenges, etc. If the result is positive, and the child has a fever, red throat, raids on the tonsils, an antibiotic is prescribed.
You need to take the test promptly, at the first symptoms, before starting treatment and even using symptomatic remedies - a throat spray, lozenges, etc. If the result is positive, and the child has a fever, red throat, raids on the tonsils, an antibiotic is prescribed.
Now, a blood test for antibodies to the Epstein-Barr virus, which causes mononucleosis, is being massively prescribed. And often, treatment is prescribed even if IgG antibodies are detected, which indicate a previous infection and developed immunity. Mononucleosis is treated only in the acute period - this can be determined using a blood test for type M antibodies (IgM).
When is a fever and rash a reason to call an ambulance?
- There is a principle that doctors adhere to and that parents should take note of: any fever and rash is a reason to immediately call an ambulance. First of all, it is necessary to diagnose meningococcemia. Meningococcal infection affects the lining of the brain.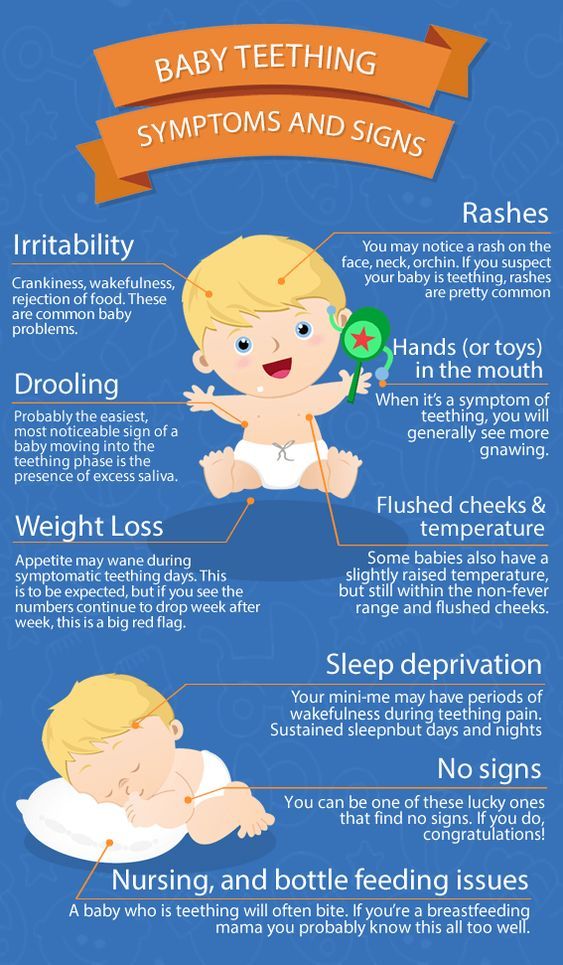 Very rarely, this happens at lightning speed, with meningitis there is at least a day to diagnose this disease and begin to treat it. Meningococcemia develops when the infection begins to affect the walls of blood vessels, it actively multiplies, a toxin is released into the blood, and sepsis develops. This is a lightning-fast disease in which a child can die in just a matter of hours. The rash in this case is specific - it resembles hemorrhagic "asterisks". If a child has a fever, and there are at least one or two such elements on the skin, this is a reason to immediately call an ambulance or take him to the infectious diseases department of the nearest hospital on his own.
Very rarely, this happens at lightning speed, with meningitis there is at least a day to diagnose this disease and begin to treat it. Meningococcemia develops when the infection begins to affect the walls of blood vessels, it actively multiplies, a toxin is released into the blood, and sepsis develops. This is a lightning-fast disease in which a child can die in just a matter of hours. The rash in this case is specific - it resembles hemorrhagic "asterisks". If a child has a fever, and there are at least one or two such elements on the skin, this is a reason to immediately call an ambulance or take him to the infectious diseases department of the nearest hospital on his own.
A hemorrhagic rash can also appear with a disease such as idiopathic thrombocytopenia. This is an autoimmune disease that can develop against the background of any infectious process. The patient's platelet count drops in the blood and a characteristic rash may appear - usually on the legs, on the stomach. Idiopathic thrombocytopenia can be life-threatening, therefore, if a purple rash, spots, small bruises are found on the skin, you should consult a doctor.
Idiopathic thrombocytopenia can be life-threatening, therefore, if a purple rash, spots, small bruises are found on the skin, you should consult a doctor.
266866 views
Author-physician: Savchenko Svetlana Petrovna
Expert in the field of laboratory diagnostics, healthcare organization, diagnostics and treatment of therapeutic diseases.
Article publication date: 06/21/2019
Updated: 08/19/2022
Types of baby rash: instructions for parents
Anna Devyatukhina
Journalist, author Daily Baby
#skin rashes #health #children #rash
The appearance of rashes in a child is often not perceived by parents as a serious reason to see a doctor. Often, mothers and fathers attribute the rash to an allergy, but there are more than a hundred reasons for its occurrence - alas, not all of them are harmless. The author of The Daily Baby prepared instructions for parents: how to determine what kind of rash attacked the child, how dangerous it is and when to run to the doctor.
The author of The Daily Baby prepared instructions for parents: how to determine what kind of rash attacked the child, how dangerous it is and when to run to the doctor.
From prickly heat to severe infection
Children's skin is incredibly delicate, so redness and rashes often appear on it. External changes in the skin, of course, signal some kind of malfunction in the body.
- There are dozens of various types of skin rashes. Among them, there are dangerous ones that require an emergency visit to a pediatrician, and there are those that can be observed at home, without a doctor.
The most important thing is to learn how to identify a hemorrhagic rash. This type always requires a doctor's consultation on the same day. Especially if the child has a temperature.
Hemorrhagic rash - one that will not disappear if you press on it with a glass. This rash looks like this: like a hemorrhage into the skin. It can be very small, the size of a dot, or it can cover the skin with large spots. Regardless of the size, we need a doctor and urgently,” says Anna Ganina, mother of three children, pediatrician at the Family Doctor clinic, Kemerovo.
Regardless of the size, we need a doctor and urgently,” says Anna Ganina, mother of three children, pediatrician at the Family Doctor clinic, Kemerovo.
Pediatrician of the mobile clinic DOC+ Natalia Makarova notes: the rash itself is not a disease, it is a symptom of some disease or a reaction to an external stimulus.
- A rash is a pathological change on the skin and mucous membranes. It can be divided into two main groups: infectious and non-infectious. Non-infectious include allergic reactions, insect bites, prickly heat. Infectious rashes appear with various infections, most often viral.
On examination, the doctor pays attention to the location, area of the rash, the nature of the rash, concomitant symptoms, and the patient's complaints. As a rule, if the rash is accompanied by severe intoxication - an increase in body temperature, weakness, refusal to eat and drink - the doctor decides on hospitalization.
Doctor of the highest category, candidate of medical sciences, allergist-immunologist Galina Chernyshova recommends that in any case, if a rash appears, contact a specialist in a timely manner, who will find out its cause and tell you what to do next.
- The cause of rashes on the body of a child can be either a banal food allergy or a severe infectious disease. The rash is never a separate disease or cause of the disease. The most common causes of its occurrence in children are allergic reactions, insect bites, infections, clotting disorders, mechanical damage to the skin and allergies to the sun.
Manifestations are very variable, from red or almost any shade of pale pink to bright brown speck, vesicle, bump to hemorrhage or even bruising.
Pediatrician Anna Ganina advises, first of all, to find out why a rash appeared on the child's body.
- Many rashes in children do not require self-treatment. We are waiting for it to pass by itself, and at the same time we are looking for the cause - a viral, bacterial infection, a blood clotting disorder.
It is often difficult to deal with a rash on your own: there are a lot of their types. Parents should immediately show the child to the doctor if it is hemorrhagic.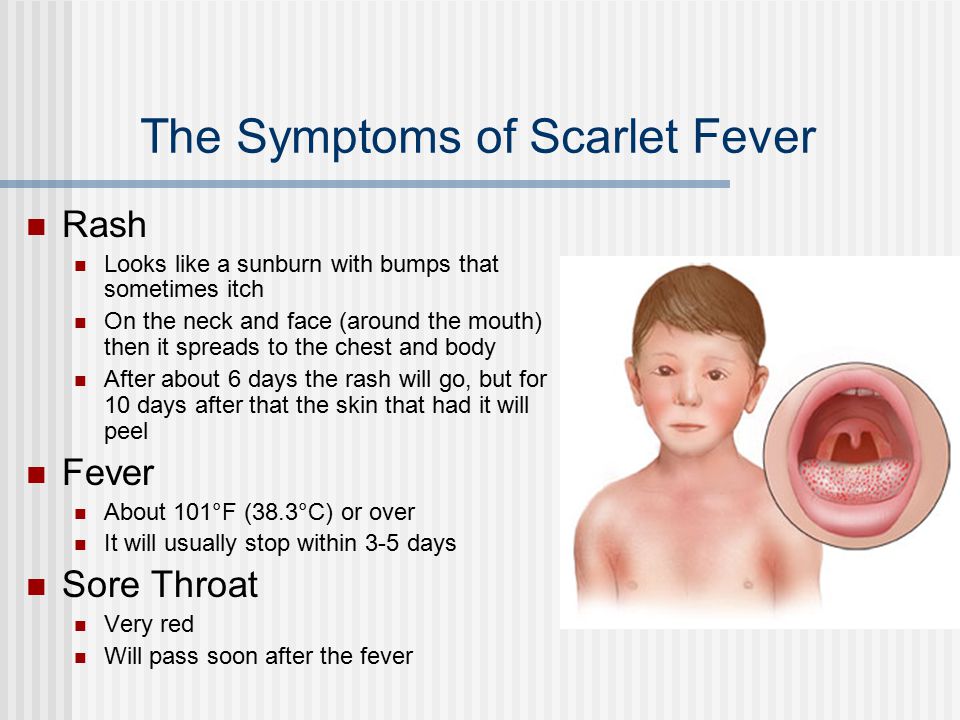 If the rash is not hemorrhagic, but with a temperature, it is also advisable to show the doctor in the next day or two.
If the rash is not hemorrhagic, but with a temperature, it is also advisable to show the doctor in the next day or two.
And if it appeared against the background of full health and it does not particularly disturb the child, the skin does not suffer - show the pediatrician in a calm planned manner.
Types of rashes and their degree of danger
There are a lot of types of children's rashes, they differ visually and are caused by different reasons. Consider some types of rashes - from the rare and most dangerous to the most common.
Meningococcal infection
© medmoon.ru
What it looks like: purple or red star-shaped spots located on the buttocks, thighs, legs, less often on the arms, trunk, face. The temperature rises strongly, vomiting appears, impaired consciousness.
Hazard: high.
What to do: urgently call an ambulance and hospitalize the child.
Measles
What it looks like: Measles presents with cough, runny nose, conjunctivitis, sore throat, fever, and a red patchy rash on the skin that appears as bright pink patches that may coalesce.
Hazard: high.
What to do: Seek immediate medical attention, do not self-medicate.
Coxsackie
What it looks like: reddish itchy blisters that appear all over the body and even on the child's mucous membranes. The temperature rises, appetite disappears, nausea, vomiting, dehydration are possible.
Hazard: high.
What to do: contact a doctor immediately.
Chicken pox
What it looks like: first small bubbles appear with clear contents, then it becomes cloudy, the blisters break out and a crust forms. Eruptions occur all over the body and cause itching. Other symptoms: fever, usually up to 4 days, abdominal pain, itching, headache, malaise, lack of appetite, cough and runny nose, sore throat.
Hazard: moderate.
What to do: be sure to contact a doctor who will diagnose and prescribe treatment.
rubella
It is poured all over the body, the temperature rises, the state of health worsens.
Hazard: medium.
What to do: see a doctor.
Allergy
What it looks like: the rash is usually red or pink in color, unevenly distributed over the skin, similar to small pimples. May cause itching.
Hazard: medium.
What to do: avoid contact with the allergen, if you guess what could have provoked the rash, give the child an antihistamine and consult a doctor.
Atopic dermatitis or diathesis
Appearance: the skin turns red and begins to peel off, sometimes weeping crusts are observed.
Hazard: medium.
What to do: avoid contact with the allergen, improve hygiene, give the child an antihistamine. If necessary, contact a doctor.
Roseola
What it looks like: Most common in children under 2 years of age. A rubella-like rash appears after 2-5 days of fever, while the child has almost no other symptoms (cough, runny nose). Roseola is usually not complicated by anything, and a rash means that the child is on the mend.
A rubella-like rash appears after 2-5 days of fever, while the child has almost no other symptoms (cough, runny nose). Roseola is usually not complicated by anything, and a rash means that the child is on the mend.
Hazard: medium/low.
What to do: The main thing is to exclude the presence of more serious diseases in the child. Treatment for roseola in children includes bed rest, drinking plenty of fluids, and medications to reduce fever.
Insect bites
What it looks like: pink or red swelling with a bite mark in the center.
Hazard: low.
What to do: If you are sure that the child was bitten by a mosquito or midge, just spread the bite with a special ointment or cream. If you suspect a bite from another insect, you should go to the hospital.
Newborn acne
Hazard: low.
What to do: go to the hospital to determine the cause of the rash.
Diaper dermatitis
What it looks like: slight reddening of the skin, usually occurs in the delicate intimate parts of the baby. Blisters and redness of the skin may appear.
Hazard: low.
What to do: regularly wash your baby, change diapers in a timely manner and arrange air baths for the baby's skin. You don’t have to go to the doctor, the main thing is to improve hygiene, and the rash will pass.
Milia
What it looks like: appears on the skin as whiteheads.
Hazard: low.
What to do: milia do not have a negative effect on the child's body and after a while, most likely, they will disappear on their own. If the appearance of whiteheads is accompanied by poor health of the child, fever and itching, you should consult a doctor.
— share with your friends!
Experts: Anna Ganina Natalia Makarova Galina Chernyshova
Read more
- 4 times more people got measles this year than last year
- "There are no hypoallergenic animals.