How do you perform cpr on a child
How to resuscitate a child
This page provides the full detailed cardiopulmonary resuscitation (CPR) sequence for infants (babies under 1 year old) and children.
It's highly recommended that every parent or carer goes on a first aid course, as it makes this process much easier to understand and remember.
If a baby or child is unresponsive and not breathing normally, call 999 and start CPR straight away.
When you call 999 for an ambulance, you should be given basic life-saving instructions over the phone, including advice about CPR.
Child and baby CPR steps
1. Ensure the area is safe
- Check for hazards, such as electrical equipment or traffic.
2. Check your child's responsiveness
- Gently stimulate your child and ask loudly: "Are you alright?"
3a.
- Leave them in the position they were found in (provided they're not in danger).
- Check their condition and get help if needed.
- Reassess the situation regularly.
3b. If your child does not respond
- Call for help.
- Carefully turn the child on their back.
If the child is under 1 year old:
- Ensure the head is in a neutral position, with the head and neck in line.
- At the same time, with your fingertips under the point of your child's chin, lift the chin. Do not push on the soft tissues under the chin as this may block the airway.
If the child is over 1 year old:
- Open your child's airway by tilting the head and lifting the chin.
- To do this, place your hand on their forehead and gently tilt their head back.
- At the same time, with your fingertips under the point of your child's chin, lift the chin. Do not push on the soft tissues under the chin as this may block the airway.
If you think there may have been an injury to the neck, tilt the head carefully, a small amount at a time, until the airway is open. Opening the airway takes priority over a possible neck injury.
4. Check their breathing
Keeping the airway open, look, listen and feel for normal breathing by putting your face close to your child's face and looking along their chest.
- Look for chest movements.
- Listen at the child's nose and mouth for breathing sounds.
- Feel for air movement on your cheek.
Look, listen and feel for no more than 10 seconds before deciding that they're not breathing. Gasping breaths should not be considered to be normal breathing.
Gasping breaths should not be considered to be normal breathing.
5a. If your child is breathing normally
- Turn them on their side.
- Check for continued breathing.
- Send or go for help – do not leave your child unless absolutely necessary.
5b. If your child is not breathing or is breathing infrequently and irregularly
- Carefully remove any obvious obstruction in the mouth.
- Give 5 initial rescue breaths (mouth-to-mouth resuscitation).
- While doing this, note any gag or cough response – this is a sign of life.
Rescue breaths for a baby under 1 year
- Ensure the head is in a neutral position and lift the chin.
- Take a breath, then cover your baby's mouth and nose with your mouth, making sure it's sealed.
 If you cannot cover both the mouth and nose at the same time, just seal either with your mouth. If you choose the nose, close the lips to stop air escaping.
If you cannot cover both the mouth and nose at the same time, just seal either with your mouth. If you choose the nose, close the lips to stop air escaping. - Blow a breath steadily into the baby's mouth and nose over 1 second. It should be sufficient to make the chest visibly rise.
- Keeping their head tilted and chin lifted, take your mouth away and watch for the chest to fall as air comes out.
- Take another breath and repeat this sequence 4 more times.
Rescue breaths for a child over 1 year
- Tilt the head and lift the chin.
- Close the soft part of their nose using the index finger and thumb of the hand that's on their forehead.
- Open their mouth a little, but keep the chin pointing upwards.
- Take a breath, then place your lips around their mouth, making sure it's sealed.

- Blow a breath steadily into their mouth over about 1 second, watching for the chest to rise.
- Keeping their head tilted and chin lifted, take your mouth away and watch for the chest to fall as air comes out.
- Take another breath and repeat this sequence 4 more times. Check that your child's chest rises and falls in the same way as if they were breathing normally.
5c. Obstructed airway
If you have difficulty achieving effective breathing in your child, the airway may be obstructed.
- Open the child's mouth and remove any visible obstruction. Do not poke your fingers or any object into the mouth.
- Ensure there's adequate head tilt and chin lift, but the neck is not overextended.
- Make up to 5 attempts to achieve effective breaths (enough to make the chest visibly rise).
 If this is still unsuccessful, move on to chest compressions combined with rescue breaths.
If this is still unsuccessful, move on to chest compressions combined with rescue breaths.
6. Assess the circulation (signs of life)
Look for signs of life. These include any movement, coughing, or normal breathing – not abnormal gasps or infrequent, irregular breaths.
Signs of life present
If there are definite signs of life:
- Continue rescue breathing until your child begins to breathe normally for themselves.
- Turn the child on their side into the recovery position and send for help.
- Continue to check for normal breathing and provide further rescue breaths if necessary.
No signs of life present
If there are no signs of life:
- Start chest compressions immediately.
- Combine chest compressions with rescue breaths, providing 2 breaths after every 30 compressions.
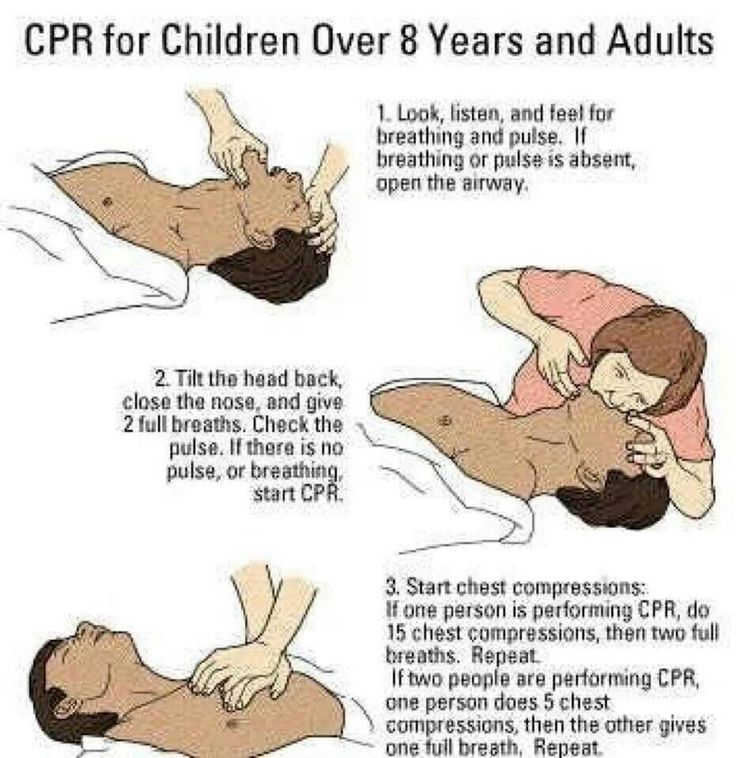
7. Chest compressions: general guidance
- To avoid compressing the stomach, find the point where the lowest ribs join in the middle, and then 1 finger's width above that. Compress the breastbone.
- Push down 4cm (for a baby or infant) or 5cm (a child), which is approximately one-third of the chest diameter.
- Release the pressure, then rapidly repeat at a rate of about 100-120 compressions a minute.
- After 30 compressions, tilt the head, lift the chin, and give 2 effective breaths.
- Continue compressions and breaths in a ratio of 2 breaths for every 30 compressions.
Although the rate of compressions will be 100-120 a minute, the actual number delivered will be fewer because of the pauses to give breaths.
The best method for compression varies slightly between infants and children.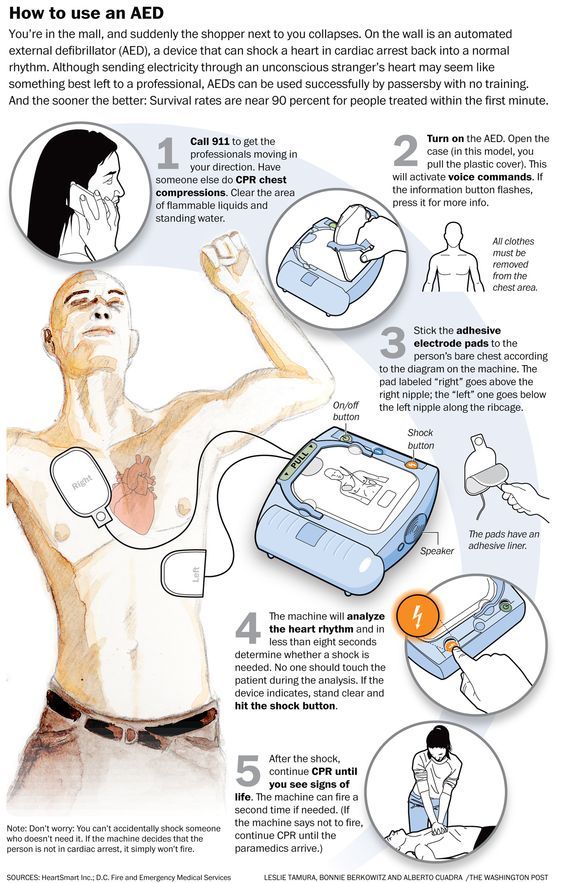
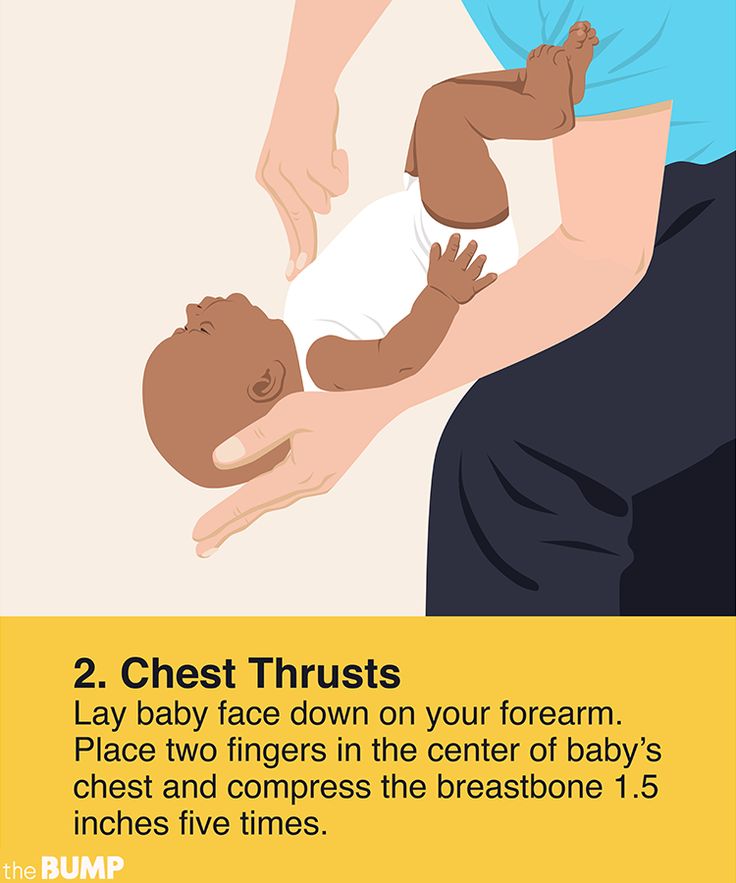
Chest compression in babies less than 1 year
- Do the compressions on the breastbone with the tips of 2 fingers, not the whole hand or with both hands.
- The quality (depth) of chest compressions is very important. If the depth of 4cm cannot be achieved with the tips of 2 fingers, use the heel of 1 hand.
Chest compression in children over 1 year
- Place the heel of 1 hand over the lower third of the breastbone.
- Lift the fingers to ensure pressure is not applied over the ribs.
- Position yourself vertically above the chest and, with your arm straight, compress the breastbone so you push it down 5cm, which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important.
- In larger children or if you're small, this may be done more easily by using both hands with the fingers interlocked, avoiding pressure on the ribs.

If you had no response to your call for help and you're alone, continue resuscitation for about 1 minute before trying to get help – for example, by calling 999.
8. Continue resuscitation until
- Your child shows signs of life – normal breathing, coughing, movement of arms or legs.
- Qualified help arrives.
Further information on first aid
- St John Ambulance: How to do baby CPR
- St John Ambulance: How to do CPR on a child
- British Red Cross: First aid training courses
Page last reviewed: 28 September 2022
Next review due: 28 September 2025
How to Perform Child and Baby CPR
Your browser's Javascript functionality is turned off.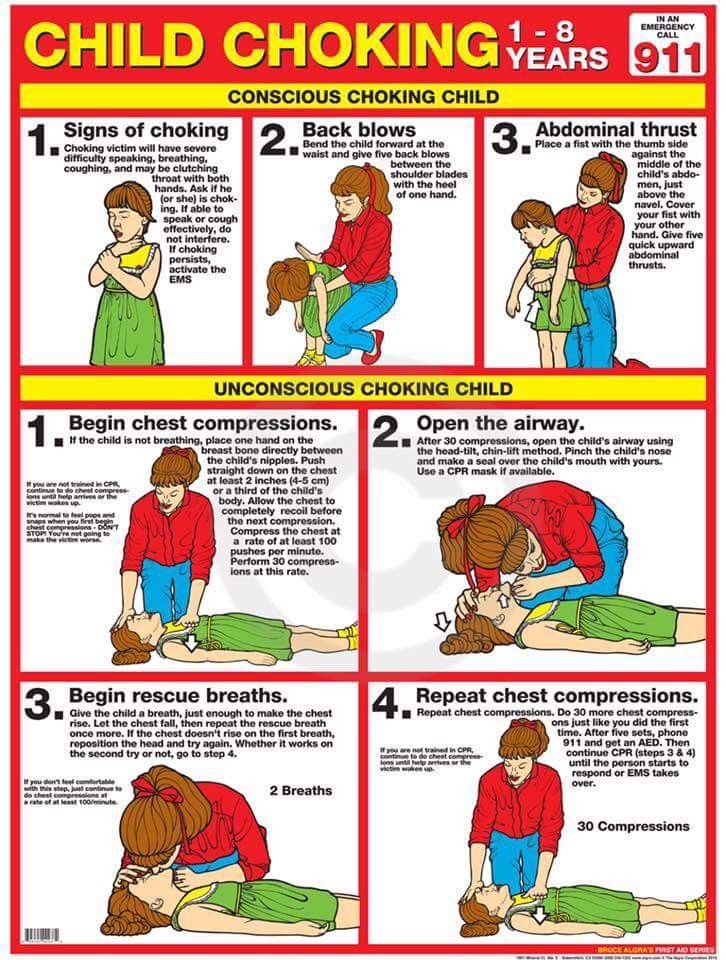 Please turn it on so that you can experience the full capabilities of this site.
Please turn it on so that you can experience the full capabilities of this site.
-
Although you hope you'll never use cardiopulmonary resuscitation (CPR) for a child or infant, it's important to know the steps so that you can help in the event of a cardiac or breathing emergency. And although you may have taken a class in child CPR, it's a good idea to keep the steps handy so that the information stays fresh in your memory. With our printable step-by-step guide, you can access the child and baby CPR steps anytime, anywhere. Simply print them up and place them in your car, your desk, your kitchen or with your other first aid supplies, then read over them from time to time to help maintain your skills.
Find a Class
Before Giving Child or Baby CPR
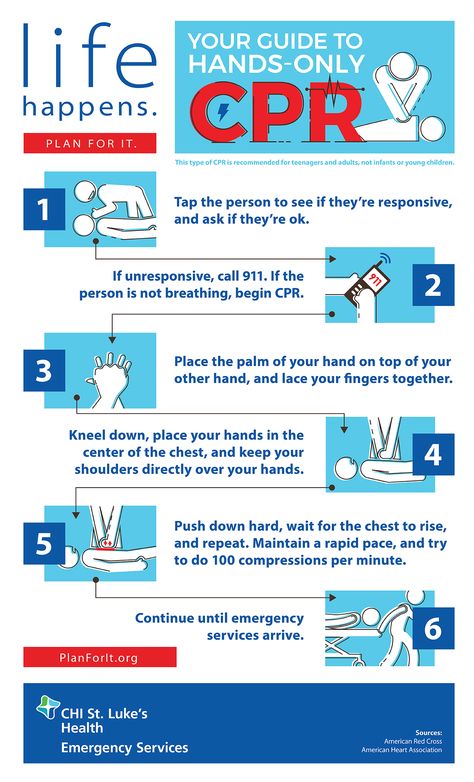
1
Check the scene for safety, form an initial impression, obtain consent from the parent or guardian, and use personal protective equipment (PPE)
2
If the child or baby appears unresponsive, check the child or baby for responsiveness (shout-tap-shout)
- For a child, shout to get the child’s attention, using the child’s name if you know it.
 If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition - For a baby, shout to get the baby’s attention, using the baby’s name if you know it. If the baby does not respond, tap the bottom of the baby’s foot and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
- Check for no more than 10 seconds
3
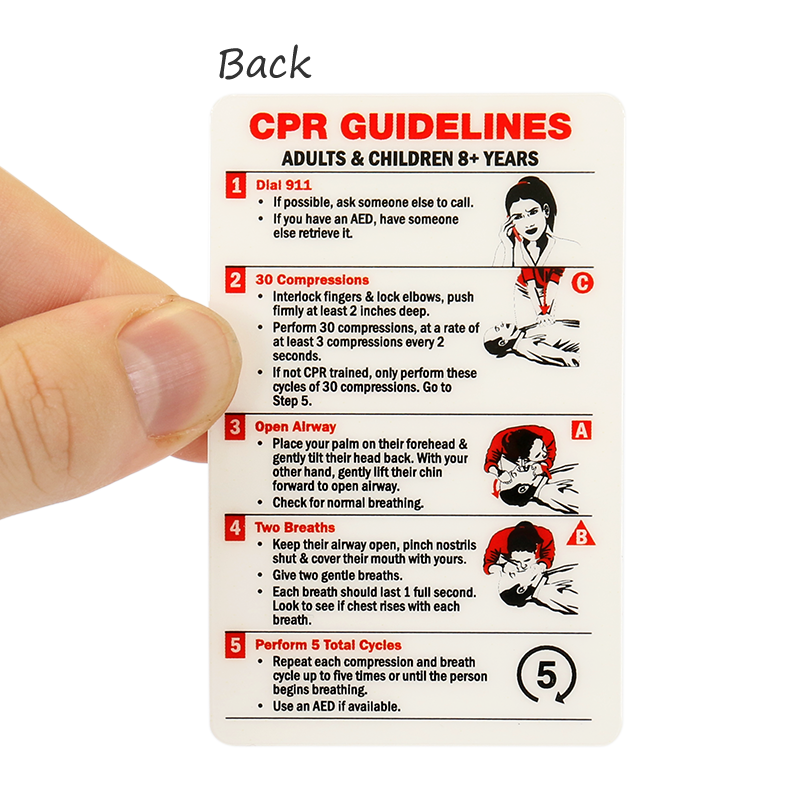
If the child or baby does not respond and is not breathing or only gasping, CALL 9-1-1 and get equipment, or tell someone to do so
Performing Child & Baby CPR
1
Place the child or baby on their back on a firm, flat surface
- For a child, kneel beside the child
- For a baby, stand or kneel to the side of the baby, with your hips at a slight angle
2
Give 30 compressions
- For a child, place the heel of one hand in the center of the child’s chest, with your other hand on top and your fingers interlaced and off the child’s chest
- Position your shoulders directly over your hands and lock your elbows
- Keep your arms straight
- Push down hard and fast about 2 inches at a rate of 100 to 120 per minute
- Allow the chest to return to normal position after each compression
- For a small child, use a one-handed CPR technique
- Place the heel of one hand in the center of the child’s chest
- Push down hard and fast about 2 inches at a rate of 100 to 120 per minute
- For a baby, place both thumbs (side-by-side) on the center of the baby’s chest, just below the nipple line
- Use the other fingers to encircle the baby’s chest toward the back, providing support
- Using both thumbs at the same time, push hard down and fast about 1 ½ inches at a rate of 100 to 120 per minute
- Allow the chest to return to its normal position after each compression
- Alternatively, for a baby, use the two-finger technique
- Use two fingers placed parallel to the chest in the center of the chest
- For a baby, if you can’t reach the depth of 1 ½ inches, consider using the one-hand technique
3
Give 2 breaths
- For a child, open the airway to a slightly past-neutral position using the head-tilt/chin-lift technique
- For a baby, open the airway to a neutral position using the head-tilt/chin-lift technique
- Blow into the child or baby’s mouth for about 1 second
- Ensure each breath makes the chest rise
- Allow the air to exit before giving the next breath
- If the first breath does not cause the chest to rise, retilt the head and ensure a proper seal before giving the second breath.
 If the second breath does not make the chest rise, an object may be blocking the airway
If the second breath does not make the chest rise, an object may be blocking the airway
4
Continue giving sets of 30 chest compressions and 2 breaths until:
- You notice an obvious sign of life
- An AED is ready to use
- Another trained responder is available to take over compressions
- EMS personnel arrive and begin their care
- You are alone and too tired to continue
- The scene becomes unsafe
- You have performed approximately 2 minutes of CPR (5 sets of 30:2), you are alone and caring for baby, and you need to call 9-1-1
Be prepared for moments that matter by taking a CPR class and you could help save a life.
Find a Class
- For a child, shout to get the child’s attention, using the child’s name if you know it.
How to resuscitate a child: chest compressions and artificial respiration
The first minutes after an injury are the most important. If you immediately provide competent first aid, then the victim is more likely to live and live without consequences.
 But how can you help your child? How to resuscitate a child, how to perform artificial respiration and chest compressions? In relation to babies, there are some critical features, especially for children under 1 year old.
But how can you help your child? How to resuscitate a child, how to perform artificial respiration and chest compressions? In relation to babies, there are some critical features, especially for children under 1 year old. Updated:
We remind you that apteka24.ua has a mobile application: 12,000 drugs with detailed instructions and, of course, delivery throughout Ukraine. Look for us on the App Store and Google Play.
P.S. UAH 100 discount on the first order from UAH 1000 with the promo code APP100
- What you need to know about resuscitation of a child?
- Cardiopulmonary resuscitation of a child: what should be done?
Unfortunately, today little Ukrainians become victims of military battles taking place on the territory of Ukraine. And in these realities, we, adults, should know how to help a child in an emergency before the ambulance arrives, because it is the first minutes after the injury that are decisive - if you provide the right help, the child will be able to continue to lead a normal life after recovery.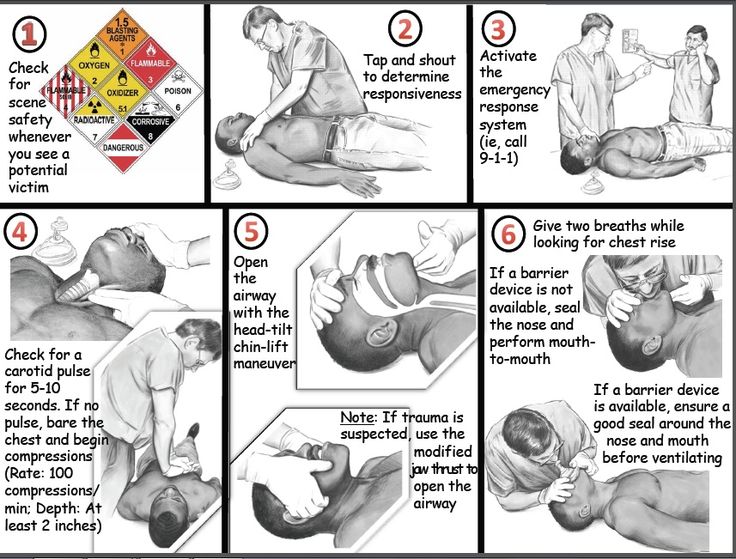
In this article, our medical experts tell you how to resuscitate a child, give artificial respiration and chest compressions before the arrival of an ambulance, because little patients have their own peculiarities.
What do you need to know about resuscitation of a child?
Emergency cardiopulmonary resuscitation is needed in various sudden situations, in particular in accidents.
Circulatory arrest leads to disruption of oxygen supply to all organ systems. The brain is most sensitive to hypoxia (lack of oxygen), in its tissues, first of all, when blood circulation stops, irreversible changes occur. This period can last 3-6 minutes maximum. For this reason, assistance must be provided in a timely, correct and fast manner.
Assessing the child's condition, first of all, it is necessary to check such parameters as:
- consciousness;
- breath;
- blood circulation.
Check the signs of consciousness in the child: does he answer the question addressed to him, does he react to touch? See if the child has any injuries or bleeding. If the child does not react, it is necessary to determine whether the child is breathing. Bring your ear to your child's mouth and nose. Is there breath on your cheek? Is the baby's chest moving?
If the child is unconscious but breathing, place the child in a stable lateral position to maintain a clear airway.
Position the child's arm on your side at a right angle to their body. Place the far hand of the child with the back of your hand on his opposite cheek, holding it with your hand. After that, bend the farthest leg of the child at the knee, place it resting on the foot, push the knee of this leg towards you and turn the child. After turning the child on its side, slightly tilt the head to open the airway and pull the leg lying on top closer to the stomach.
Cardiopulmonary resuscitation of a child: what should be done?
If the child is not responding and not breathing, urgently call an ambulance and perform cardiopulmonary resuscitation.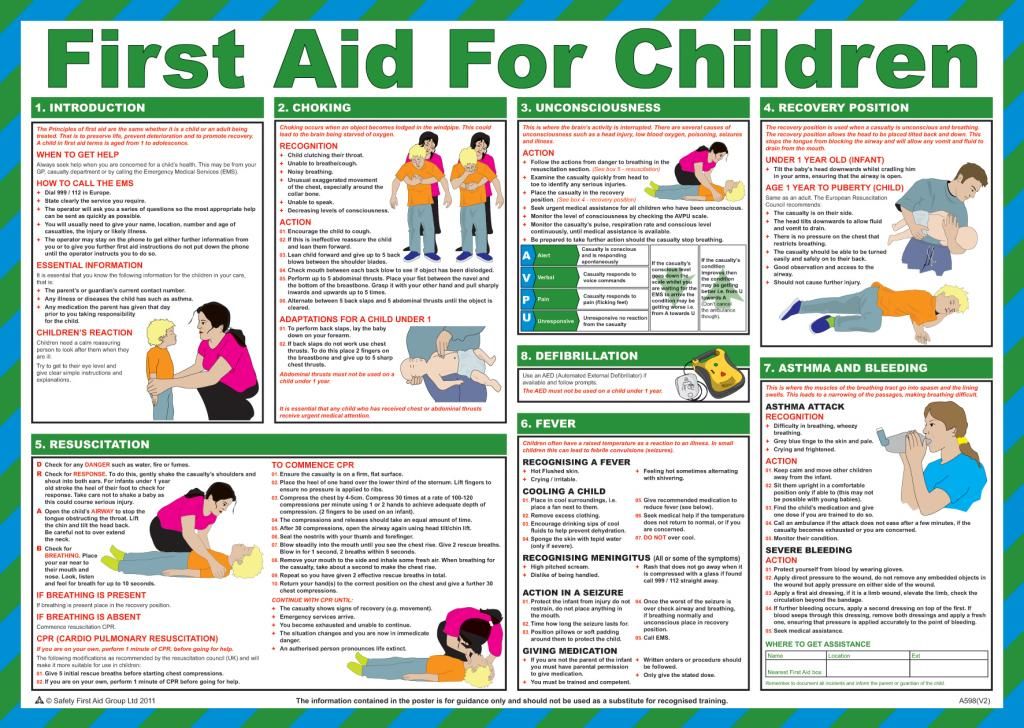 Required:
Required:
- ensure airway patency;
- determine the pulse on the carotid artery;
- if the pulse is not detected - urgently perform chest compressions.
How to give artificial respiration to a child?
Lay the child on a hard surface on their back to ensure a good airway, then examine the airway. The oral cavity is freed from blood, vomit with a finger with a gauze swab, napkin or handkerchief.
The next step is to ensure the patency of the larynx. Place one hand on your forehead, tilt your head back and lift your chin. Remove your hand from your forehead and pinch the soft part of your nose. Before starting an indirect heart massage, five breaths (breaths) must be taken. These are short breaths and should not be longer than 1 second each.
Tilt your head, inhale and grasp the child's mouth.
Blow slowly and evenly into his mouth for one second until his chest rises.
The main criterion for the effectiveness and control of mechanical ventilation is chest excursion, the anterior wall of which should rise during inspiration and fall during expiration.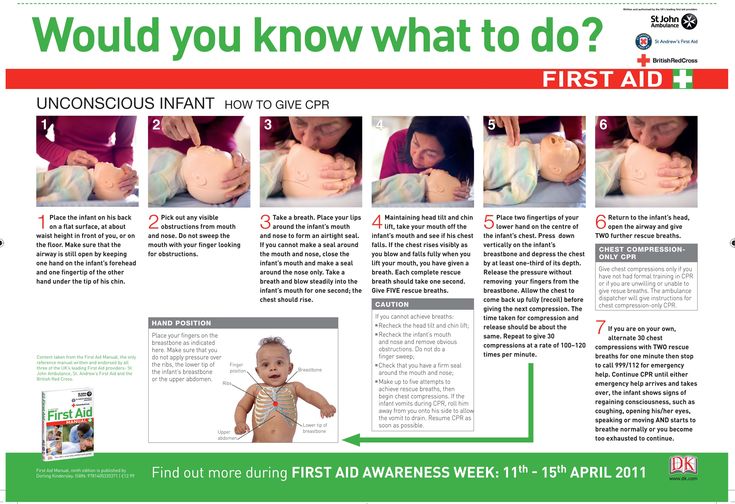 Make sure that the chest rises. Watch your chest sink as the air comes out.
Make sure that the chest rises. Watch your chest sink as the air comes out.
How to give chest compressions to a child?
In addition to ensuring an adequate supply of oxygen to the alveoli, cardiopulmonary bypass must be provided. For this purpose, indirect heart massage is used.
It is necessary to stand on the side of the child, the base of one palm is placed in the middle of the sternum, the second on top along the sternum. Then, with straight arms, without bending them at the elbow joint, it is necessary to press the chest to a depth of 4 cm or ⅓ of the sternum with a frequency of 100-120 per minute.
To prevent fracture of the ribs, the force must be concentrated only on the base of the palm, fingers should not press on the ribs. Hand pressure on the sternum is performed by the weight of the torso of the first aid participant.
Next, do 30 chest compressions, then 2 breaths. Continue compressions and breaths at a ratio of 2 breaths for every 30 compressions.
In children under 1 year of age the procedure is different, it consists in pressing one or more index fingers on the sternum with a frequency of more than 100 beats per minute. If there are two rescuers, it is necessary to clasp the lower part of the sternum with the hands and compress with the tips of 2 thumbs.
The criteria for the effectiveness of chest compressions are:
the appearance of a pulse in the central peripheral arteries;
constriction of the pupils with the appearance of a reaction to light.
It should be remembered that long (more than 5-10 seconds) pauses should not be made during chest compressions.
If spontaneous breathing occurs before the arrival of medical personnel, place the child in a stable side position, control his breathing.
Also find out what should be in a first aid kit: a list of medicines and medical supplies for emergencies.
It is also important to know what to do before the ambulance arrives: how to provide first aid for burns, injuries, concussions and loss of consciousness.
Learn more about health at apteka24.ua.
Sources
How to give CPR (mouth to mouth) to a baby or child / HSE
How to resuscitate a child / NHS
CPR for Children / WebMD
Child & Baby CPR / Red cross
Disclaimer
apteka24.ua provides comprehensive and reliable information on issues of medicine, health and well-being, however, the diagnosis and choice of treatment methods can only be made by your doctor! Self-medication may not be safe for your health. apteka24.ua is not responsible for possible negative consequences resulting from the use of information posted on the site by users of apteka24.ua.
parental access to the child in intensive care – Pro Palliative
Contents
Before visiting the intensive care unit, a certificate of the absence of diseases is required. It is legal?
Are there any restrictions in the new requirements?
The doctor claims that only the child's mother can enter the intensive care unit. What to do?
What to do?
Can a grandparent visit a child in a hospital?
The doctor claims that the hospital is under quarantine and internal regulations prohibit parents from coming. What to do?
The doctor is not against parents in intensive care, but he allows them to come in strictly allotted hours. What to do?
Medical staff demand money for access to the child in intensive care. It is legal?
Can a doctor forbid visiting a child because the conditions are not created in the hospital?
What to do if the doctors still do not let the child into the intensive care unit?
Since January 1, 2012, the Federal Law “On the Fundamentals of Protecting the Health of Citizens in the Russian Federation” guaranteed parents, legal representatives or other family members the right to stay together with the child in a hospital. Nevertheless, the issue of access to intensive care is very acute: doctors refer to infections brought by parents from the external environment, to quarantine and the lack of conditions for visitors. Legal adviser of the Vera Foundation Anna Povalikhina told what actions will help parents gain access to intensive care.
Legal adviser of the Vera Foundation Anna Povalikhina told what actions will help parents gain access to intensive care.
On August 19, 2020, the Ministry of Health of Russia by order No. 869n approved general requirements for organizing visits to the patient by relatives and other family members or legal representatives of the patient in a medical organization, including in its structural divisions intended for intensive care and resuscitation .
The order came into force on September 21, 2020.
Important
Please note that the new requirements refer specifically to visits to patients, and not to joint permanent residence with a child.
Before visiting the intensive care unit, they ask me for a certificate of the absence of diseases. It is legal?
No. The new requirements, as well as the 2016 methodological letter of the Ministry of Health “On the rules for visiting patients in the intensive care unit by relatives”, lists all the conditions under which relatives are allowed to visit children in intensive care.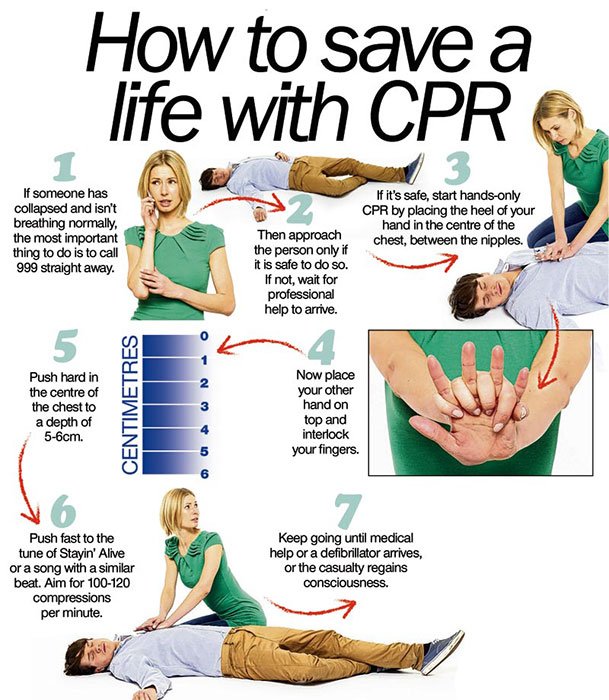 Among them, there is no requirement to provide doctors with certificates of the absence of diseases or test results.
Among them, there is no requirement to provide doctors with certificates of the absence of diseases or test results.
Are there any restrictions in the new requirements?
Visitors are not allowed to use mobile phones and other electronic devices.
The rule that no more than two visitors can be in the room at the same time is still preserved.
But the restrictions on the appearance of visitors have been removed. Now, before entering the department, you do not need to wear shoe covers, a gown, a mask, a cap. At least there are no such requirements in the document.
Before visiting the intensive care unit, read the Rules, or rather, print them out so that in case of disagreement you can show them to medical workers.
The doctor says that only the child's mother can enter the intensive care unit. What to do?
When it comes to visiting a child in intensive care, there are no obstacles for either mom or dad.
If we are talking about living together, then by law only one parent can be with a child. However, parents have equal rights and bear equal responsibilities towards their children, and hence equal responsibility for their health. This is stated in articles 61 and 64 of the Family Code of the Russian Federation. This means that they have the right to decide for themselves which of them will be with the child permanently.
However, parents have equal rights and bear equal responsibilities towards their children, and hence equal responsibility for their health. This is stated in articles 61 and 64 of the Family Code of the Russian Federation. This means that they have the right to decide for themselves which of them will be with the child permanently.
Can a grandparent visit a child in a hospital?
Can. According to the accepted requirements, the patient can be visited not only by relatives and family members, but also by other persons, for example, friends, but only with the consent of the patient.
Now the patient in the hospital, even in the ICU, can be visited by children without age restrictions.
The doctor claims that the hospital is under quarantine and internal regulations prohibit parents from coming. What to do?
It is forbidden to visit patients who are in infectious disease wards and infectious disease wards, as well as during the introduction of restrictive measures (quarantine) in a medical organization (its structural subdivision).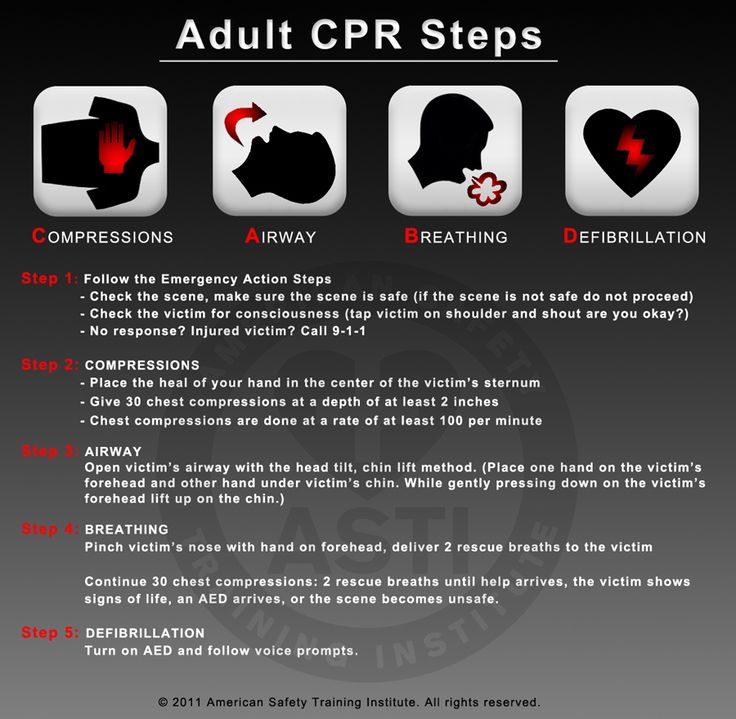
Internal regulations are no reason to refuse you. Such restrictions are not provided for either by law or by the Visiting Rules. Any medical instruction, directive, or document of any kind that does not authorize a visit to a relative violates federal law and may not be enforced.
However, the new rules contain a clause that the visit to the patient is carried out taking into account the patient's condition, compliance with the anti-epidemic regime and the interests of other persons working and (or) located in the medical organization. Unfortunately, nowhere is it indicated what requirements for compliance with the anti-epidemic regime can become a reason to ban a visit, what interests and what persons will be the grounds for refusal.
The doctor is not against the parents in the intensive care unit, but allows them to come in strictly allotted hours. What to do?
Parents and other legal representatives of a child under 18 have the right to decide for themselves whether to stay with the child in the hospital permanently or choose a visiting regime.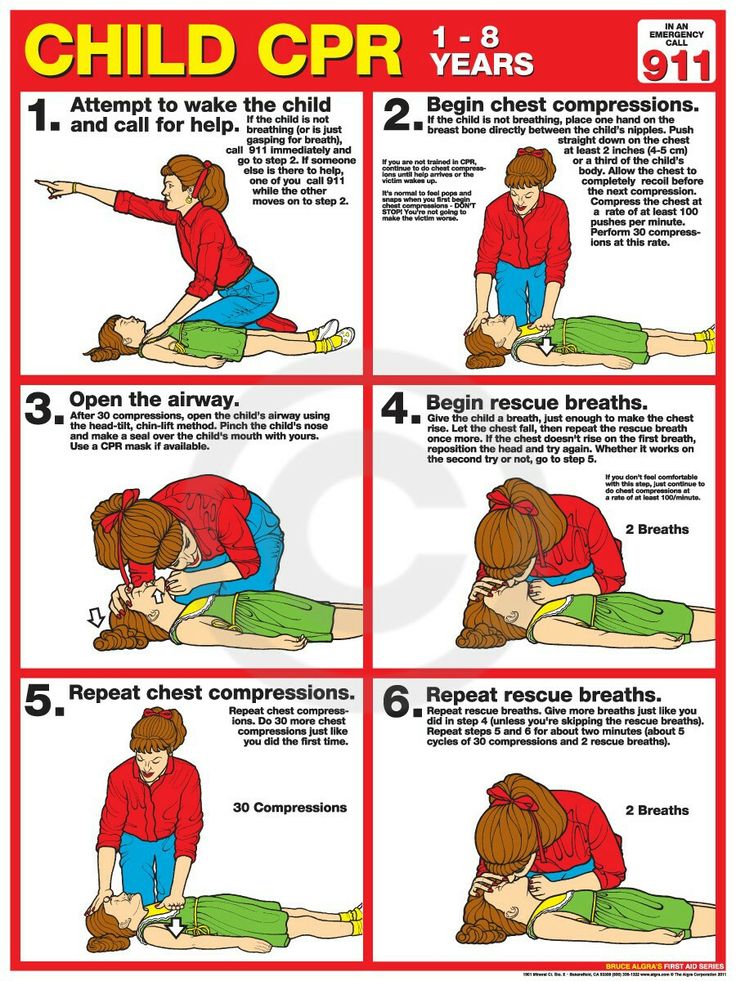
However, the time of visits really needs to be agreed with the head of the department. If the parent wants to stay with the child all the time, the requirement
to come at certain hours is illegal and contradicts paragraph 3 of Article 51 No. treatment.
Medical staff demand money for access to the child in intensive care. It is legal?
No. You may only be charged for bed and board if your child is over 4 years old. And only if the doctor decides that there are no medical indications for the joint stay of the parent with the child.
On January 13, 2022, the Ministry of Health of the Russian Federation sent an information letter to the regional ministries of health about the joint stay of a parent with a disabled child over 4 years old in a hospital. The letter lists the conditions of the child, in which medical institutions must provide parents with the conditions to be with the child around the clock.
Bed and meals must be provided to the parent free of charge.
Download information letter of the Ministry of Health of the Russian Federation dated 01/13/2022 No. 15-3 / I / 2-223
Can a doctor forbid visiting a child because conditions are not created for this in the hospital?
No. The doctor does not have the right to refuse to jointly stay with the child in the hospital, regardless of his age, due to the fact that there are no appropriate conditions.
According to the territorial programs of state guarantees of free provision of medical care to citizens of any constituent entity of the Russian Federation, the conditions for providing medical care must include the provision of a bed and meals when one of the parents, another family member or other legal representative is in a medical organization in a hospital with a child until he reaches the age of 4 years, and with a child older than the specified age - if there are medical indications. Now these indications are listed in the information letter of the Ministry of Health of the Russian Federation, the link to which we gave above.
The territorial program of state guarantees of free medical care for citizens of the constituent entity of the Russian Federation where you live can be found on the website of the department/ministry of health in your region.
What to do if the doctors still do not let the child into the intensive care unit?
If the attending physician refuses access to the intensive care unit, go to the head of the department, and if he refuses, to the head physician. Before the meeting, print or hand-write two copies of the application for admission to the child (see application form). If the doctor is not available, please contact his secretary with a request to accept the application and register it officially. Give one copy to the secretary, on your copy you must put the incoming number, the date of acceptance of the application and the signature of the person who received it.
If you are denied again, file a complaint with the name of the chief physician (see the complaint form) with mandatory registration with the secretary (see instructions for sending complaints), and fulfill this promise after the conversation.