Itching during early pregnancy
Itching and intrahepatic cholestasis of pregnancy
Itching is common in pregnancy. Usually it's thought to be caused by raised levels of certain chemicals in the blood, such as hormones.
Later, as your bump grows, the skin of your tummy (abdomen) is stretched and this may also feel itchy.
However, itching can be a symptom of a liver condition called intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC).
ICP needs medical attention. It affects around 1 in 140 pregnant women in the UK.
Symptoms of ICP
The main symptom is itching, usually without a rash. For many women with ICP, the itching is often:
- more noticeable on the hands and feet, but can be all over the body
- worse at night
Other symptoms can include:
- dark urine
- pale poo
- yellowing of the skin and whites of the eyes (jaundice), but this is less common
Symptoms of ICP typically start from around 28 weeks of pregnancy, but it's possible to develop the condition earlier.
Non-urgent advice: Call your midwife or GP if you have itching that's:
- mild or distressing, possibly worse at night
- anywhere on your body, but may be worse on the palms of your hands and soles of your feet
Feeling itchy like this can be a sign of ICP and needs to be checked.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation.
You may also want to avoid synthetic materials and opt for natural ones, such as cotton, instead. These are "breathable" and allow the air to circulate close to your skin.
You may find having a cool bath or applying lotion or moisturiser can help soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using unperfumed lotion or soap.
Mild itching is not usually harmful to you or your baby, but it can sometimes be a sign of a more serious condition, particularly if you notice it more in the evenings or at night.
Let your midwife or doctor know if you are experiencing itching so they can decide whether you need to have any further investigations.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a potentially serious liver disorder that can develop in pregnancy.
Normally, bile acids flow from your liver to your gut to help you digest food.
In ICP, the bile acids do not flow properly and build up in your body instead. There's no cure for ICP, but it should go once you've had your baby.
ICP seems to run in families, but it can happen even if there is no family history. It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
If you have had ICP in a previous pregnancy, you have a high chance of developing it again in another pregnancy.
Some studies have found that babies whose mothers have ICP have a higher chance of being born prematurely or stillborn.
Because of the link with stillbirth, you may be offered induction of labour. This could be any time from 35 weeks, depending on the level of bile acids in your blood.
If you have ICP, you will probably be advised to give birth in hospital under a consultant-led maternity team.
Diagnosis and treatment of ICPICP is diagnosed by excluding other causes of the itch. Your doctor will probably talk to you about your medical and family history and advise you to have some blood tests.
These will include tests to check your liver function (LFT) and measure your bile acid levels (BA).
If you are diagnosed with ICP, you will have regular liver blood tests (LFTs) and bile acid measurement tests so your doctor can monitor your condition.
Initially, you may be given these tests every week. You may then be given more, or less, frequent tests depending on the results and your symptoms.
Creams and medicines for ICPCreams, such as aqueous cream with menthol, are safe to use in pregnancy and can provide some relief from itching.
A medicine called ursodeoxycholic acid (UDCA) can be prescribed to try to relive itching. But recent evidence suggests it may not be effective in reducing bile acids and easing itching.
UDCA is considered safe to take in pregnancy, although it is prescribed on what is known as an "informed consent" basis as it has not been properly tested in pregnancy. It is usually only prescribed by a hospital doctor.
It is usually only prescribed by a hospital doctor.
A possible alternative, which can be helpful if itchiness is keeping you awake at night, is antihistamine medicine, such as chlorphenamine. Chlorphenamine tends to cause drowsiness so it can also help with sleep problems as well as itchiness. If you do feel drowsy do not drive or operate machinery.
You may also be offered a vitamin K supplement. This is because ICP can affect your absorption of vitamin K, which is important for healthy blood clotting.
Most experts on ICP only prescribe vitamin K if the mother-to-be reports pale poo, has a known blood clotting problem, or has very severe ICP from early in pregnancy.
If you are diagnosed with ICP, your midwife and doctor will discuss your health and your options with you.
Further information
There is information about obstetric cholestasis on the Royal College of Obstetricians & Gynaecologists (RCOG) website, including what it means for you and your baby, and the treatment that's available.
You can also get information about intrahepatic cholestasis of pregnancy (ICP) on the British Liver Trust website.
The charity ICP Support provides information about ICP. You can also watch a video about living with intrahepatic cholestasis of pregnancy (ICP) on the ICP support website featuring mums and clinical experts.
Community content from HealthUnlockedItching during pregnancy | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
Mild itching is common in pregnancy because of the increased blood supply to the skin. As your pregnancy progresses and as your baby grows, the skin of your abdomen is stretched and this may also feel itchy.
Mild itching is usually nothing to worry about, but if the itching becomes severe it can be a sign of a serious liver condition called obstetric cholestasis. This affects fewer than 1 in 100 pregnant women, but needs medical attention.
This affects fewer than 1 in 100 pregnant women, but needs medical attention.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation. You may also want to avoid synthetic materials and choose natural fabrics such as cotton that allow the air to circulate close to your skin. You may find that having a cool bath or applying lotion or moisturiser can help to soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using plain lotion or soap.
Serious itching: obstetric cholestasis
If you’re worried about your itching, or if you have severe itching, it’s important to see your midwife or doctor.
Obstetric cholestasis (OC), also called intrahepatic cholestasis of pregnancy, is a serious liver disorder that affects a small number of pregnant women, usually in the last 3 months of pregnancy.
Causes of obstetric cholestasis
The cause of OC is unclear, but it’s thought the rise of pregnancy hormones later in pregnancy may slow the normal flow of bile — the digestive fluid made in the liver that helps your digestive system break down fats. In OC, bile salts build up rather than leaving the liver, eventually entering the bloodstream, which can make you feel itchy.
In OC, bile salts build up rather than leaving the liver, eventually entering the bloodstream, which can make you feel itchy.
OC seems to run in families, although it can occur with no family history. It is also more common in women of Indian and Pakistani origin. If you have had OC in a previous pregnancy, you're more likely to develop it again in a subsequent pregnancy.
Babies of women with OC are more likely to be born prematurely or to be stillborn, or to have lung problems from breathing in meconium. Because of these complications, your doctor may consider inducing labour before you are due.
Symptoms of obstetric cholestasis
The classic symptom of OC is itching without rash, usually on the palms and soles of the feet, but it may be more widespread. The itching can be non-stop or unbearable, and worse at night.
Other symptoms include dark urine, jaundice (yellowing of the skin and whites of the eyes), and pale bowel movements (poo).
The itchiness usually goes away within a few days after giving birth.
Treatment of obstetric cholestasis
OC is diagnosed through taking a medical and family history, and blood tests that check your liver function (liver functions tests — LFTs). Once OC is diagnosed, you will have regular LFTs until your baby is born, so that your doctor can monitor your condition.
Creams, such as calamine lotion, are safe to use in pregnancy and can provide some relief from itching. Your doctor may prescribe a medication to reduce bile salts and ease itching.
OC can affect your absorption of vitamin K, which is important for healthy blood clotting so you may be offered a vitamin K supplement.
If you are diagnosed with OC, your midwife and doctor will discuss your health and your options with you.
Sources:
Mayo Clinic (Cholestasis of pregnancy), NSW Health (Having a baby), Royal Women’s Hospital (Common concerns in early pregnancy), SA Health Department (Clinical guideline obstetric cholestasis), Women's and Children's Health Network (Itching in pregnancy), King Edward Memorial Hospital (Cholestasis in pregnancy - clinical guidelines)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.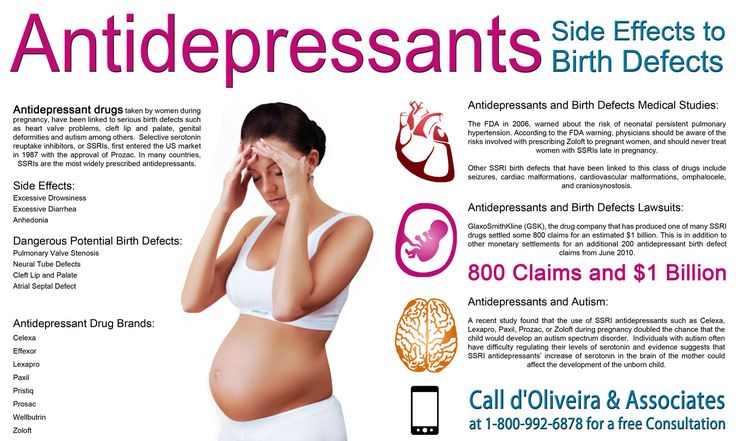
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Itching during pregnancy. What is Pregnancy Itching?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Itching during pregnancy is a pathological condition that is a symptom of various diseases that have arisen or worsened during gestation. It is manifested by a sensation of painful tickling irritation of the skin and mucous membranes, which causes a scratching reflex. There may be a rash, other skin symptoms, signs of damage to various organs and systems. It is diagnosed with the help of biochemical, immunological, hormonal, allergological, microbiological studies, PCR, RIF, ELISA, ultrasound. For pathogenetic and symptomatic treatment of itching, antihistamines, corticosteroids, emollients, and sedative herbal remedies are used.
ICD-10
L29.8 Pruritus other
- Causes
- Pathogenesis
- Symptoms of itching during pregnancy
- Complications
- Diagnostics
- Treatment of itching during pregnancy
- Prognosis and prevention
- Prices for treatment
General
According to observations of obstetricians-gynecologists, temporary or permanent itching sensations of varying intensity occur in more than half of pregnant women. 45-50% of patients complain of genital (intimate), 18-22% - skin, 8-10% - anal itching. In some women during pregnancy, the simultaneous appearance of different types of itching is noted. Usually, the disorder develops as a result of an exacerbation of pre-existing diseases. In some cases, the cause of diseases, the symptom of which is itching, is the changes that occur during pregnancy. The relevance of timely diagnosis of the pathology that caused itching of the skin or mucous membranes is due to the risk of developing serious obstetric complications in some pathologies.
45-50% of patients complain of genital (intimate), 18-22% - skin, 8-10% - anal itching. In some women during pregnancy, the simultaneous appearance of different types of itching is noted. Usually, the disorder develops as a result of an exacerbation of pre-existing diseases. In some cases, the cause of diseases, the symptom of which is itching, is the changes that occur during pregnancy. The relevance of timely diagnosis of the pathology that caused itching of the skin or mucous membranes is due to the risk of developing serious obstetric complications in some pathologies.
Itching during pregnancy
Causes
Specialists in the fields of obstetrics name many factors that can provoke the occurrence of itchy sensations in pregnant women. Itching can manifest diseases that have become aggravated or that have arisen in the gestational period, systemic responses of the body to the action of exogenous agents and endogenous metabolites. The most common causes of the disorder are:
The most common causes of the disorder are:
- Skin and fungal diseases. Itching is observed in atopic and contact dermatitis, dermatophytosis, chronic lichen simplex, psoriasis, seborrhea, eczema. Itchy sensations are characteristic of a parasitic skin lesion - head and pubic lice, scabies. In the cold season, itching accompanies the development of xerosis. In many patients, these disorders are detected even before pregnancy, although infection with skin parasites or the manifestation of pathology is possible during the gestation period.
- System processes. Itching is accompanied by endogenous intoxication with natural and pathological metabolites in some forms of oncopathology (Hodgkin's lymphoma, polycythemia vera), liver diseases with cholestasis (viral hepatitis, gallstone disease, hepatosis), endocrinopathies (diabetes mellitus, hyperthyroidism, hypothyroidism), iron deficiency anemia, terminal renal failure with glomerulonephritis, pyelonephritis, hydronephrosis, nephrolithiasis.
- Genital infections. Often they are manifested not by skin, but by intimate itching that occurs due to irritation with toxins, and pathological secretions (whites). The symptom is more pronounced with candidiasis, genital herpes, gardnerellosis, chlamydia, gonorrhea. Reduced immunity and hormonal changes characteristic of pregnancy often lead to the development of bacterial vaginosis, one of the signs of which is itching in the genital area.
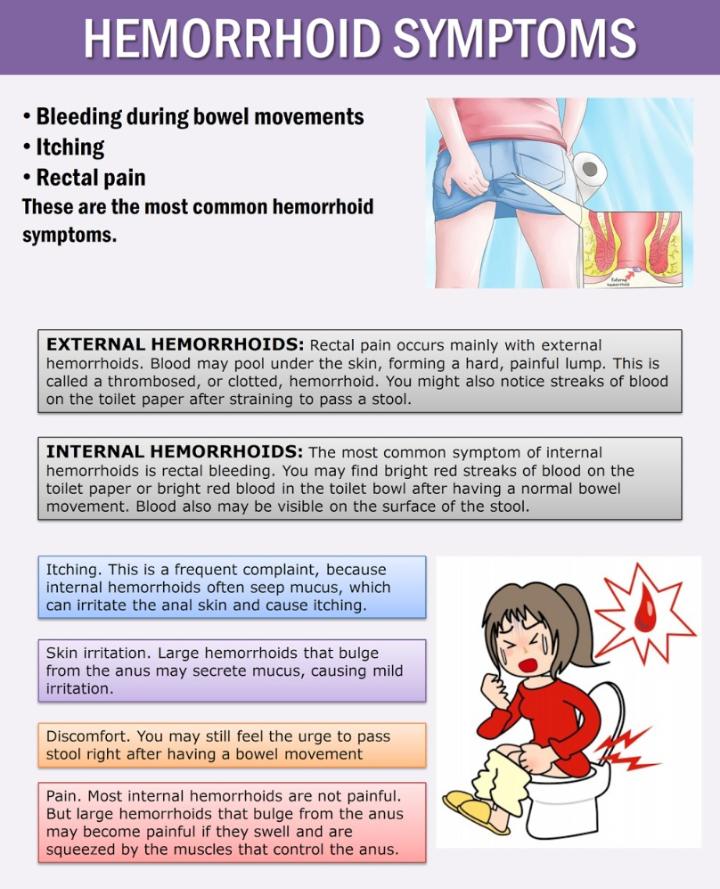
- Urological and proctological diseases. Itching in the perineum is caused not only by intense vaginal leucorrhea, but also by irritation with urine during frequent urination in pregnant women with urethritis, cystitis, pyelonephritis, pathological changes characteristic of hemorrhoids, anal fissures, local perianal dermatitis. One of the causes of anal itching is enterobiasis - helminthic invasion, in which part of the life cycle of the parasite is associated with skin lesions near the anus.
- Exogenous influences. The influence of a pathological agent can be external (through the skin and mucous membranes) and internal (after absorption in the gastrointestinal tract).
 In both cases, the development of an allergic or toxic systemic reaction with itching of varying intensity is possible. Provoking factors are most often drugs (aspirin, antibiotics, anesthetics), food, plant pollen, animal hair, dust, insect bites.
In both cases, the development of an allergic or toxic systemic reaction with itching of varying intensity is possible. Provoking factors are most often drugs (aspirin, antibiotics, anesthetics), food, plant pollen, animal hair, dust, insect bites. - Neurological and psychiatric disorders. Tingling, paresthesia, intermittent intense itching caused by changes in the peripheral nervous system may be early signs of multiple sclerosis, preceding the main neurological symptoms. Neurogenic itching can be a consequence of stress, a sign of postherpetic neuralgia, brain tumors. In rare cases, itching manifests itself as part of a tactile hallucinosis.
- Dermatoses of pregnancy. In 1.5-3.0% of patients, usually with a hereditary predisposition, physiological changes during pregnancy (skin stretching with damage to the connective tissue, hyperestrogenism, immune restructuring) provoke an allergic reaction or intrahepatic bile stasis. As a result, one of the specific gestational pruritic dermatoses develops - atopic dermatitis, pemphigoid, cholestasis of pregnancy.
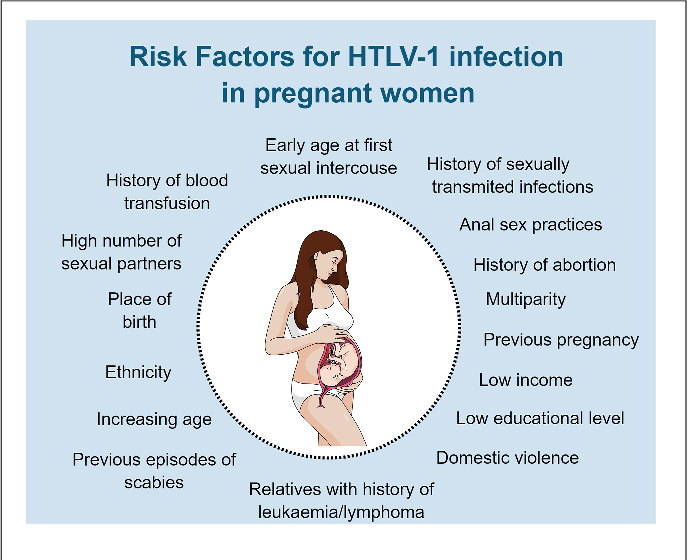
Probable prerequisites for more frequent occurrence of itching in various diseases in pregnant women are an increase in dryness of the skin as a result of the influence of progesterone, a physiological decrease in immunity aimed at maintaining gestation, stretching and rupture of the connective tissue fibers of the skin with the formation of autoantigens, and a violation of the natural microflora of the vagina. Pregnancy also serves as a trigger for the development of a number of diseases accompanied by itching - gestational diabetes, postpartum autoimmune thyroiditis, etc. Additional risk factors are obesity, wearing synthetic clothing and underwear, the use of scented pads and irritating alkaline products for skin and genital care, non-compliance with the rules personal hygiene, the use of spicy food with seasonings, spices.
Pathogenesis
The mechanism of itching during pregnancy depends on the causes that caused it, however, the key link in the pathogenesis in all cases is the irritation of certain sections of the afferent pathways that transmit nerve impulses. Most often, itching occurs due to stimulation of peripheral nocireceptors. The receptor apparatus is usually affected by mediators formed during a local inflammatory, allergic, autoimmune reaction, microbial toxins, metabolites (bile acids, nitrogenous compounds, high concentrations of glucose), drugs.
Most often, itching occurs due to stimulation of peripheral nocireceptors. The receptor apparatus is usually affected by mediators formed during a local inflammatory, allergic, autoimmune reaction, microbial toxins, metabolites (bile acids, nitrogenous compounds, high concentrations of glucose), drugs.
Perhaps the development of itchy sensations due to damage, in which the inflammatory reaction is secondary, constant local influences (insect bites, movement of helminths, irritation with urine, leucorrhoea). Sometimes pathological afferentation, characteristic of itching, is noted against the background of microcirculatory disorders (for example, in diabetes mellitus), damage to sensory nerve fibers (with multiple sclerosis). With volume neoplasms of the brain, strokes, neurotic and mental disorders, the focus of pathological impulses, subjectively perceived as itching, is localized in the central parts of the nervous system.
Symptoms of itching during pregnancy
The main symptom of the disorder is local or generalized itching sensations of varying intensity, from slight tingling and burning to an unbearable desire to scratch or rub the skin, mucous membranes. Depending on the causes of itching, it can be constant or periodic, serve as the only sign of the disease or be accompanied by other skin manifestations - redness, scratching, macular, papular, vesicular, pustular rash, peeling. In general, the clinical picture is characterized by significant polymorphism, determined by the leading pathology, the symptom of which was skin or intimate itching.
Depending on the causes of itching, it can be constant or periodic, serve as the only sign of the disease or be accompanied by other skin manifestations - redness, scratching, macular, papular, vesicular, pustular rash, peeling. In general, the clinical picture is characterized by significant polymorphism, determined by the leading pathology, the symptom of which was skin or intimate itching.
Complications
Diseases with intense itching can be complicated by secondary infection of excoriated sites. The likelihood of developing obstetric complications depends on the influence of the underlying disease on pregnancy. Most skin diseases, transient allergic reactions, dermatosis of pregnant women cause discomfort and worsen the quality of life, but do not pose a serious threat to the woman and the fetus. In severe cholestasis of pregnant women, many systemic processes, the likelihood of gestosis, spontaneous miscarriage, premature birth, fetoplacental insufficiency, fetal growth retardation, anomalies in labor, coagulopathic bleeding, DIC increases. Possible complications of infectious diseases that occur with itching are chorioamnionitis, intrauterine infection of the fetus, postpartum endometritis, obstetric peritonitis.
Possible complications of infectious diseases that occur with itching are chorioamnionitis, intrauterine infection of the fetus, postpartum endometritis, obstetric peritonitis.
Diagnostics
The main task of a diagnostic search for complaints of a patient about itching of the skin, genitals, and perianal area is to identify the cause that caused the disorder. To make a diagnosis, a wide range of laboratory and instrumental diagnostic methods are used to determine the state of various organs and systems, to detect biochemical markers of the disease. In addition to a gynecological examination, general blood and urine tests during pregnancy, the following are recommended:
- Biochemical blood test. Indicative for some diseases are data on the level of glucose, bile acids, total bilirubin, cholesterol, triglycerides, serum iron, urea, uric acid, creatinine, enzymes (AlT, AST, alkaline phosphatase), the composition of blood protein fractions.
- Hormonal studies.
 To exclude endocrinopathies, manifested by itching of the skin, mucous membranes, an insulin resistance index, an assessment of the blood levels of insulin, TSH, thyroxine, triiodothyronine, and thyroxin-binding globulin are used. In some cases, determine the level of sex hormones.
To exclude endocrinopathies, manifested by itching of the skin, mucous membranes, an insulin resistance index, an assessment of the blood levels of insulin, TSH, thyroxine, triiodothyronine, and thyroxin-binding globulin are used. In some cases, determine the level of sex hormones. - Study of immune and allergic status. Confirmation of the atopic nature of the disease is an increased concentration in the blood of IgE, histamine. In some disorders, specific markers of autoimmune processes (antibodies to collagen, AT-TPO, AT rTTG) are detected.
- Diagnosis of infections. Highly sensitive methods for detecting infectious diseases are polymerase chain reaction, RIF, ELISA. With their help, you can detect signs of genital herpes, candidiasis, chlamydia, mycoplasmosis, ureaplasmosis, and other urogynecological diseases.
- Culture of the discharged urogenital tract. Microbiological examination allows not only to determine the causative agent of an infectious disease, but also to assess its sensitivity to antibacterial drugs.
 The method is especially indicated for patients with itching of the vulva, vagina, urethra.
The method is especially indicated for patients with itching of the vulva, vagina, urethra.
In the presence of elements of the rash, a scraping or separated skin is analyzed. To assess the morphological state of various organs, ultrasound diagnostics that is safe for the fetus is used - ultrasound of the kidneys, liver, gallbladder, small pelvis. As additional methods, chemical and toxicological analyzes, histological examination of biopsy specimens, scraping for enterobiasis, and fecal analysis for helminth eggs can be recommended. Differential diagnosis is usually carried out between diseases in which itching occurs during pregnancy. In addition to an obstetrician-gynecologist and a dermatologist, according to indications, the patient is consulted by a venereologist, an infectious disease specialist, an endocrinologist, a gastroenterologist, a hepatologist and a urologist.
Treatment of itching during pregnancy
When developing tactics for managing a patient with complaints of itchy sensations, the influence of the underlying disease on gestation is taken into account. In most cases, it is possible to prolong pregnancy until the term of physiological birth. The treatment regimen is determined by the protocol for the relevant disorder, may include antibiotics, hormones, antifungal, hormonal, anticonvulsant drugs, drugs from other pharmacotherapeutic groups, taking into account their possible impact on fetal development. To reduce or eliminate itching, nonspecific pathogenetic and symptomatic therapy is effective:
In most cases, it is possible to prolong pregnancy until the term of physiological birth. The treatment regimen is determined by the protocol for the relevant disorder, may include antibiotics, hormones, antifungal, hormonal, anticonvulsant drugs, drugs from other pharmacotherapeutic groups, taking into account their possible impact on fetal development. To reduce or eliminate itching, nonspecific pathogenetic and symptomatic therapy is effective:
- Antihistamines. Due to the blockade of histamine receptors, the transmission of excitation along sensitive C-fibers decreases, the release of mediators by mast cells decreases. Suppression of an allergic reaction can significantly reduce the intensity of itching or completely stop it.
- Glucocorticoids. Local application of corticosteroid ointments, creams, emulsions has a pronounced antipruritic effect. Local treatment is more effective with limited dermatitis and dermatosis. Given the possible effects on the fetus, systemic corticosteroids during gestation are used to a limited extent.

- Emollients. Since the skin becomes drier during pregnancy, which increases itching, its moisturizing and softening have a positive therapeutic effect. Means of this group also allow you to accelerate the restoration of damaged epidermis and lipid intercellular structures of the skin.
- Herbal sedatives. Due to the mutual influence of itching and emotional disorders (bad mood, irritability), the appointment of sedative preparations makes it possible to reduce the intensity of perception of uncomfortable sensations at the level of the central nervous system. Sedative therapy also contributes to the normalization of disturbed sleep.
The patient is advised to exclude from the diet foods that increase irritation or can cause allergies, normalize the drinking regimen, get enough rest, and avoid stress. Usually, natural delivery is recommended for pregnant women with itching. Caesarean section is performed only if there are obstetric indications.
Prognosis and prevention
In the absence of systemic disease, pregnancy outcomes in women with pruritus are usually favorable. The prognosis worsens when serious somatic diseases, endocrinopathies are detected. As a preventive measure, for patients suffering from skin and other pathologies, when planning pregnancy, it is necessary to take into account the recommendations of a dermatologist and specialized specialists. Pregnant women without concomitant pathology are advised to carefully observe the rules of personal hygiene, refuse synthetic underwear, moisturize the skin with natural means, avoid situations in which sweating increases sharply - staying in stuffy rooms, overheating in the sun. For washing linen and clothes, it is better to use phosphate-free neutral washing powders.
You can share your medical history, what helped you with the treatment of itching during pregnancy.
Sources
- Dermatoses in pregnant women: Abstract of the dissertation / Alenkina A.