Infant in pain
Pain management in babies | Pregnancy Birth and Baby
Pain management in babies | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Healthy babies will, at times, experience pain during events that are a normal part of growth and development, including teething pain, blood tests and vaccinations. A baby may also experience pain due to illness or injury. Just like adults, each baby’s reaction to pain is different, but unlike adults, babies can’t tell you how they are feeling, so they rely on you to recognise their pain and help them through it.
How do I know if my baby is in pain?
It can be difficult to know if a baby is in pain since they can’t directly communicate how they are feeling, but there are signs that can help you recognise when they are in pain. For example, if a baby is in pain:
- they may cry or whimper, and be unable to settle
- they may be tense, with clenched fists, and may keep their arms and legs close to their chest
- they may be fidgety, agitated or have an unclear wake/sleep schedule
- they may be pale, flushed or sweaty
- they may shut their eyes tightly, furrowing their eyebrows, or have larger than normal pupils
As a parent, you know your child best — if you notice your baby sounds, looks or behaves in an unusual way, and you are worried they may be in pain, seek medical advice. A doctor or baby health clinic can check for other signs that your baby might be unwell, such as an unusual heart rate or blood pressure.
Common pain
In the first year of life, your baby will undergo several procedures. These cause minor pain and distress, but they are very important since they help keep your baby well.
In the first 3 days of your newborn’s life, a small amount of blood will be taken from their heel. This newborn screening test (or 'heel prick test') is done to check for rare but serious conditions. You will also be offered a number of vaccinations, which help prevent some serious contagious diseases.
This newborn screening test (or 'heel prick test') is done to check for rare but serious conditions. You will also be offered a number of vaccinations, which help prevent some serious contagious diseases.
If your baby is born premature, or with a medical problem, they may also require blood tests, feeding tubes, IV lines or surgery to help them perform all the tasks our bodies do naturally. While these procedures may cause your child some pain in the short term, the aim is to ensure their long-term health and wellbeing.
How can I help my baby in pain?
You are one of the greatest sources of comfort to your baby, and your very presence may have a calming effect.
Some established pain-reducing techniques include:
- letting your baby hold your finger
- talking or singing to your baby
- swaddling your baby in the fetal position
- breastfeeding
- nappy changing
- offering them a dummy
- tactile soothing (stroking the head and back softly)
- 'kangaroo care' (skin-to-skin contact between parent and child, both covered by a blanket)
- holding your baby with both hands (to provide a feeling of security)
- taking your baby to a dark, quiet space
If your newborn undergoes a painful procedure, their doctor or nurse may suggest you breastfeed or hold your baby skin to skin if possible, or give them sugar (sucrose) solution. These techniques are proven to have a calming and pain-relieving effect on infants.
These techniques are proven to have a calming and pain-relieving effect on infants.
Video provided by Sharing Knowledge About Immunisation.
When can I give pain medicine?
You can give your child medicines such as paracetamol and ibuprofen for short-term relief of fever-like symptoms. While they won’t make the cause of the pain go away, they will make your baby feel and sleep better.
- Paracetamol may be taken from 1 month of age, every 4 to 6 hours in the correct dosage (based on age and weight), but no more than 4 times in 24 hours.
- Ibuprofen may be taken from 3 months of age, every 6 to 8 hours in the correct dosage (based on age and weight), but no more than 3 times in 24 hours. If your child has a bleeding disorder, do not give them ibuprofen.

- Never give your newborn aspirin, unless specifically instructed by your doctor.
Where to get help
If your newborn has been taking paracetamol or ibuprofen for 48 hours but is still unwell, seek medical advice.
Ask your pharmacist if you are unsure of the correct dose of medicine for your baby.
If you have given your child too much ibuprofen or paracetamol, call the Poisons Information Centre (13 11 26) immediately or take them to your nearest hospital emergency department.
Sources:
Raising Children Network (Immunisation in childhood), The Royal Children's Hospital Melbourne (Pain relief for children - paracetamol and ibuprofen), Royal Children’s Hospital (Neonatal Pain Assessment), International Association for the Study of Pain (Pain management in children), Better Health Channel (Pain management (acute) - children), SA Health (Too small too soon), Frontiers in Psychology (Pain, Parental Involvement, and Oxytocin in the Neonatal Intensive Care Unit), Royal Children’s Hospital (Sucrose (oral) for procedural pain management in infants)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Related pages
- Helping kids with medical procedures
- Breastfeeding your baby
- Immunisation and vaccinations for your child
- What is kangaroo care?
Need more information?
Children's medicines and medications | Raising Children Network
When kids are sick, you want to help them feel better. But it can be hard to know whether children’s medicine and medications will help. Our guide explains.
Read more on raisingchildren.net.au website
Helping kids with medical procedures
You play an important role in your child's medical procedure, by explaining why the procedure is needed, distracting them during it and talking them through the recovery.
Read more on Pregnancy, Birth & Baby website
Pain management (acute) - children - Better Health Channel
If you think your child is in pain, always see your doctor for diagnosis and treatment.
Read more on Better Health Channel website
ANZCA | Pain relief and having a baby
Labour is among the most painful human experiences.
Read more on ANZCA – Australian and New Zealand College of Anaesthetists website
Control of Pain in Children (Paediatric Pain Management) | HealthEngine Blog
Paediatric Pain Management: Paediatric Pain Management is the Control of Pain in Children. Pain can be associated with numerous paediatric diseases and conditions and the patient may require Paediatric Pain Management.
Read more on HealthEngine website
Making your child's test or procedure less stressful - InsideRadiology
InsideRadiology provides free and easily accessible, accurate, up to date and credible information about medical imaging tests and procedures.
Read more on InsideRadiology website
Opioid (pain reliever) infusion | Sydney Children's Hospitals Network
When children have strong pain due to surgery, injury or illness, they need constant pain relief
Read more on Sydney Children's Hospitals Network website
Medicines for your child
Here is some practical and reliable advice about giving your sick infant or child medicine, including what is the right dosage and possible side effects.
Read more on Pregnancy, Birth & Baby website
Community Child Health Program | WA Health
Community child health nurses support all families with young children. We provide a range of important free services to support families to raise happy, healthy children. We offer health and development assessments and screening, immunisation advice and support to families with young children.
Read more on WA Health website
Managing JIA — Arthritis Australia
Early diagnosis and active, long-term management provides the best chance for a positive outcome for your child
Read more on Arthritis Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pain in Infants (Babies)
Article Translations: (Spanish) (Hmong) (Somali)
Our commitment to pain management
We believe infants have a right to the best level of pain relief that can be safely provided. The Children’s Comfort Promise™ states we will do everything possible to prevent and treat pain, so we take a team approach to pain and anxiety management, using medicine and non-medicine therapies. Our goal is to have staff and families work together to assess pain promptly and treat it effectively.
Do infants have pain?
Even though infants are still developing and cannot tell us about their pain, they do feel pain, and their pain can be treated. The health care team will do all they can to relieve pain and make your baby comfortable.
Why do infants have pain?
Pain can have many causes, including:
- soreness after surgery caused by:
- the incision (an opening made in surgery)
- stretching or swelling of tissue or organs
- procedures such as starting an IV or drawing blood for a lab test
- nerves that sense tissue damage or swelling
- an achy feeling that can be caused by an infection
- sore muscles from being in bed for a long time
- discomfort from tubes
- skin abrasions or sores
How do we know an infant is in pain?
Infants cannot tell us about their pain in words, like older children, but they do give us clues by certain behaviors. We can measure pain by observing things like sleep, irritability, restlessness, appetite, movement, and vital signs (heart rate, breathing rate, blood pressure) to help decide if your baby is having pain.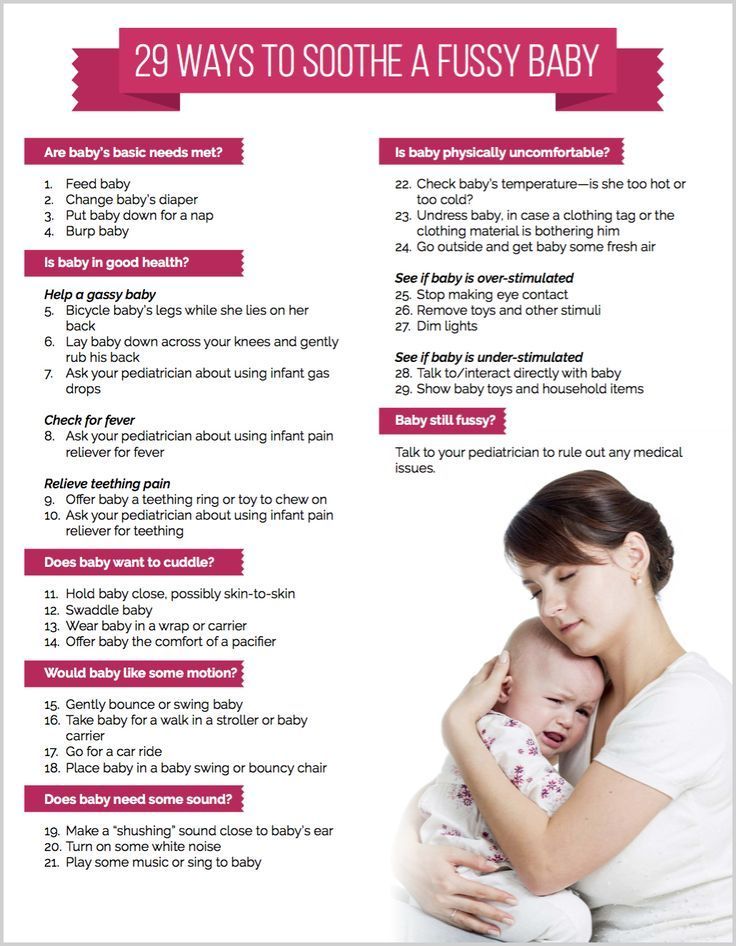
How do infants act when in pain?
Infants will act differently when they are in pain than when they are comfortable. Each infant will respond individually and may be inconsistent in how they react from time to time. Infants use a combination of behaviors to signal pain. These signs may occur when the infant is not in pain, but combinations are usually present in an infant with pain. Look for the clues listed below.
- Crying: Your baby may cry robustly. Crying is often increased in pitch and length of time. Babies who are very sick or premature and have less energy may be silent even though they are uncomfortable.
- Facial expression: Babies may have a furrowed or deeply wrinkled brow with eyes squeezed shut. Sometimes their chin quivers. Even babies on breathing machines may do this.
- Muscle tension: Babies will tense up their muscles, pulling the arms in and the legs up or sometimes stretching everything out (this is called flailing).
 They may also clench their fists or keep their body rigid. Babies who are very sick may lose muscle tension and become floppy.
They may also clench their fists or keep their body rigid. Babies who are very sick may lose muscle tension and become floppy. - Babies in pain are also often irritable, restless, may refuse to eat and might be unable to sleep.
- Movement will depend on your baby’s health status and energy level. Some babies will squirm and vigorously bend arms and legs. Babies that are frail may be very quiet and not move.
- Sleep/wake patterns: Babies in pain are often fussier and sleep less. Some babies may withdraw and seem to be asleep all the time.
What can parents do?
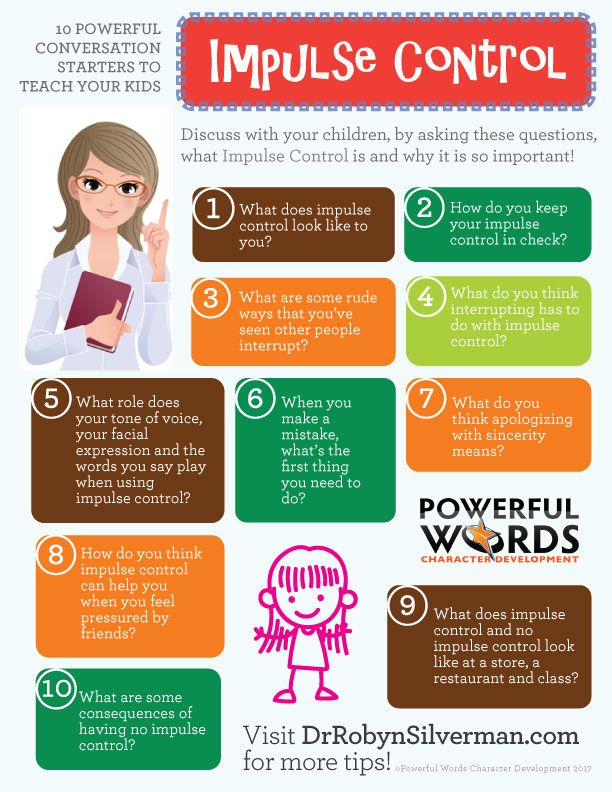
Parents have a very important role. Because you know your baby best, you can work closely with Children's staff (such as doctors, nurses, or child life specialists) to make decisions about managing pain. You are the best person to help your baby deal with new or difficult situations. To help your baby cope with pain, you can:
- Be present, or ask others who know your baby to visit.

- Tell the staff if you think the pain is not being controlled, or if your baby is ready to have pain medicine decreased because he or she is too sleepy or more active.
Use routine calming activities before and after a stressful event: gently patting or massaging your baby, holding, rocking, or talking in a soothing voice.
What can be done to reduce pain?
Non-medicine methods
Pain is both a physical and emotional state. Infants feel pain in their body, and they may also have thoughts and memories about pain. Because infants do not yet have language, it is hard for us to know exactly what they think of it. We will partner with you to try and reduce both the feelings and the worry about pain. Here are some things that can help reduce pain for your baby:
- Change the infant's environment. Less light, noise, and activity at the bedside will often help calm your baby.
- Sucking on a pacifier can help an infant cope with procedures and other painful events.

- Sugar water (24 % sucrose) is often used before, during, and after needle and other procedures to help with pain. (See the education sheet for Sucrose 24%)
- Distractions like using a soothing voice, music, stories, or songs can take an infant's attention away from the pain or the procedure.
- Holding your baby; rhythmic motion, rocking or other slow, steady movement can help.
- Positioning infants so that they are more contained and warmer can be very comforting.
- Doing Kangaroo Care or skin-to-skin contact can be very soothing and relieve pain.
- Rubbing or gentle massage helps relax the muscles and the nerves that send pain messages to the brain, so the brain does not sense as much pain.
We will help you to learn how to use any or all of these techniques with your baby. Please check with your child’s nurse or provider to learn more.
Medicines
There are many types of pain medicines we can use. Which type is best for your baby will depend on many things, including the type of pain, how long it will last, and the reason your child has pain. Some medicines are described below.
Some medicines are described below.
Numbing cream, such as 4% lidocaine, can be put on the skin to numb it before a needle procedure such as an IV start, lab draw, or injection. It has to be on for at least 30 minutes to work best and help reduce discomfort with needles. It is not usually used on babies less than 37 weeks of gestation. (See the education sheet, " Anesthetic (Numbing) cream.")
Non-steroidal anti-inflammatory drugs (NSAIDs) reduce pain and inflammation. They can be bought over the counter and help manage mild to moderate pain. To reduce stomachache, they should be taken with food or formula when possible. Ibuprofen (Pediaprofen®, Motrin®, Advil®, or another brand) is an example of an NSAID.
Acetaminophen (Tylenol® or another brand) is another over-the-counter medicine that helps treat mild to moderate pain. It has fewer side effects than NSAIDs but does not reduce inflammation.
Opioids are strong medicines used to treat moderate to severe pain, often used after surgery. They may be given by IV or taken by mouth. Opioids can have side effects of itching, nausea, and constipation. Infants will often become sleepy and their breathing can slow down. Sometimes NSAIDs or acetaminophen and opioids are used together. To prevent constipation, your baby may need more fluids than usual, or a stool softener.
They may be given by IV or taken by mouth. Opioids can have side effects of itching, nausea, and constipation. Infants will often become sleepy and their breathing can slow down. Sometimes NSAIDs or acetaminophen and opioids are used together. To prevent constipation, your baby may need more fluids than usual, or a stool softener.
After your baby goes home, follow your doctor' instructions about giving pain medicines. Give the medicine as soon as the pain starts. Severe pain is harder to take away. Be sure to give medicine at bedtime to help your baby sleep comfortably. Some medicines need to be given around the clock. Your doctor will tell you the schedule for this if it is needed.
Be sure to call the doctor if the medicine does not seem to help the pain, or if the pain becomes worse. If you call the doctor about pain you might be asked if your baby has a fever, how severe the pain is based on how your baby is acting, and what the wound or surgical site looks like (if there is one).
Questions?
This sheet is not specific to your child but provides general information. If you have any questions or concerns, please talk to the doctor or the staff working with your child. Your doctor or nurse can also access other pain experts in the hospital. Good pain management is a team effort.
Last Reviewed 6/2020
Back To Top
Recognizing and preventing pain in children
"Is my child restless, is he in pain?" Such questions are often asked to us by parents because the child is restless. How to find out what hurts the baby?
The World Health Organization definition of pain is: “Pain is what a person feels and describes in terms of time, place and intensity, frequency and type of pain. But what about children who have not yet learned to talk and cannot describe what hurts them? In their case, they may not receive suitable treatment because they cannot explain how they feel.
Sometimes even children who already speak well are very often embarrassed or afraid to tell what and where it hurts. The process of recognizing pain in each child is different, depending on age.
The process of recognizing pain in each child is different, depending on age.
Pain recognition in children who do not yet speak
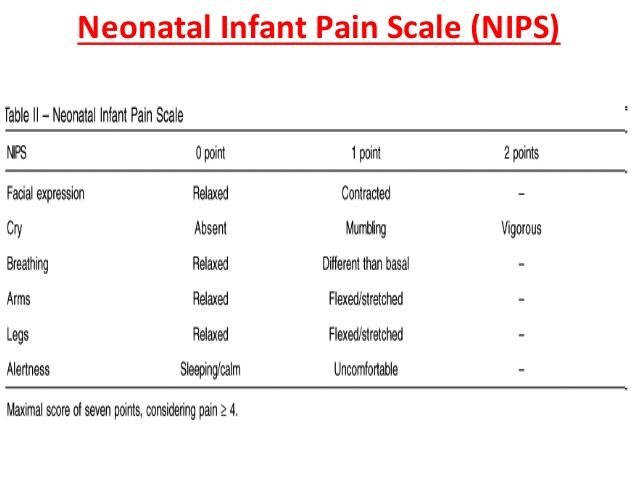
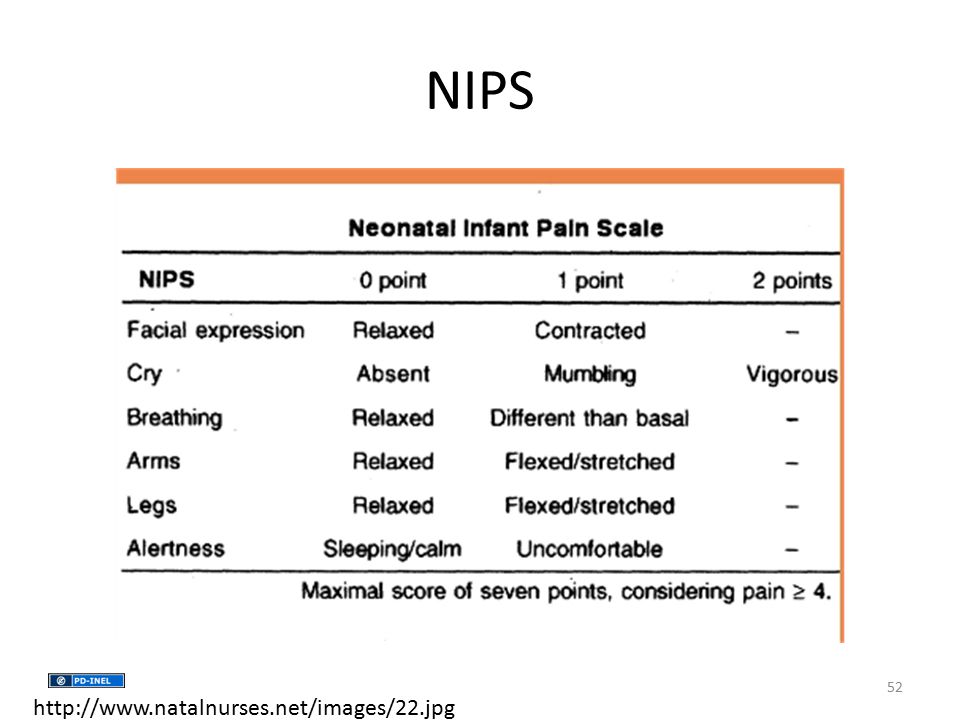
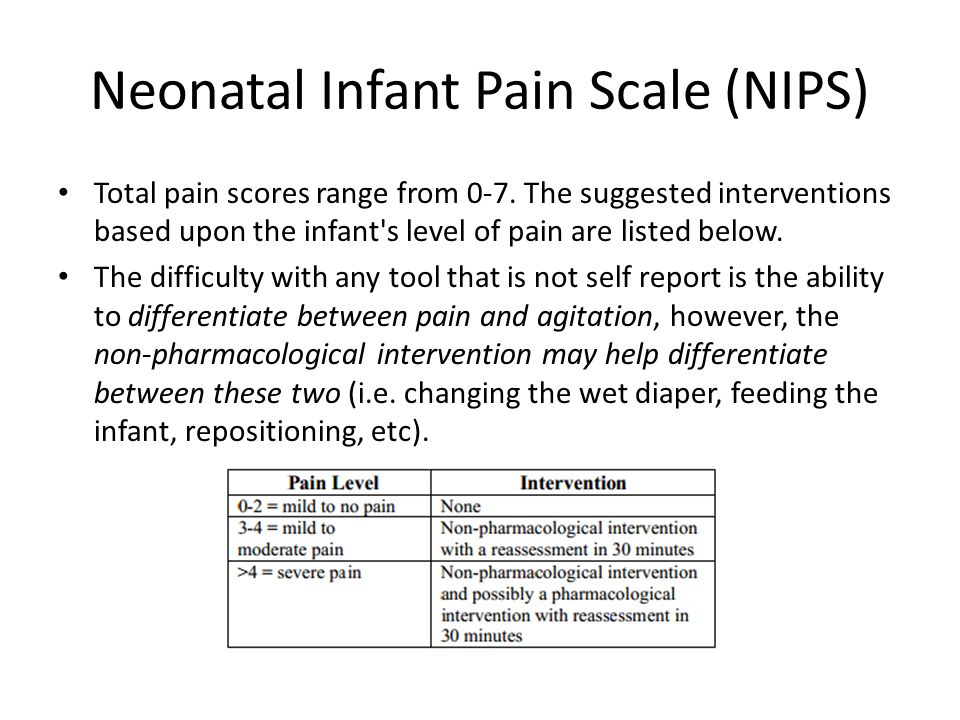
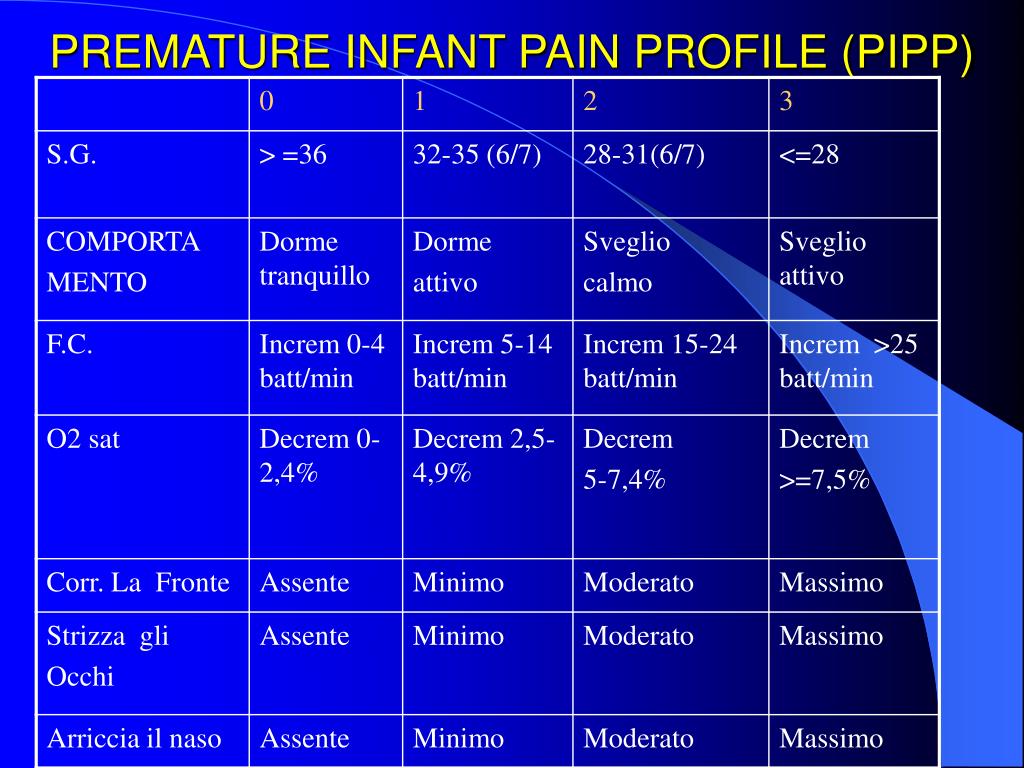
In children who do not yet speak, pain diagnosis is performed by an adult, depending on behavioral and physiological signs. In medical institutions, it is customary to measure pain in children using a special ruler, from a pain level of 0 (does not hurt at all) to 10 (unbearable pain).
Various ranges have been designed to suit different ages and development of the child. Some of them include behavioral and physiological traits and some of them are based only on behavior. However, it should be noted that most of the rulers designed to measure pain in children who do not yet speak were developed for research. Their application can be complex and time consuming.
Behavioral signs that are considered to understand the degree of pain - facial expression, tears, movements of the arms and legs and the ability to calm down. The more suffering is visible on the face of the child, the louder he cries, the more tense his limbs and it is impossible to calm him - so the degree of pain is higher.
The more suffering is visible on the face of the child, the louder he cries, the more tense his limbs and it is impossible to calm him - so the degree of pain is higher.
Common physiological signs - blood pressure, heartbeat (pulse), breathing - if there is a deviation from the norm, such as increased heart rate and rapid breathing - so the degree of "discomfort" is greater.
The doctor or nurse calculates the behavioral and physiological scores according to the chart or ruler while observing the child. The total score shows the child's level of discomfort.
FLACC range:
| Points | 0 | 1 | 2 |
| Person | without special changes in the expression or smiles at | Persons relatively irritated, looks without interest, is watched without interest, closed without interest, is closed without interest. expresses constant suffering, chin trembles, jaws clenched | |
| Legs | Leg tone normal or calm | Leg tones is increased, tense, unconventional | Twins or legs are composed of |
| Activity | Calm position, Lying, moves without difficulties | WITHING, WITHING . | Body position tense, arched or chills |
| Crying | Not crying | Complaints and sighs0003 | Constant crying, shouting, sobs, frequent complaints |
| ability to calm down | Calm, satisfied | Calm off or during communication, you can divert |
|
For example, a child with a calm expression, movable legs, sometimes crying, who is difficult to calm and hold in his arms, the degree of pain is 5 (out of 10). The scores confirm moderate discomfort, requiring diagnosis of the cause and finding an opportunity to alleviate the condition.
If the source of the pain is unknown, the child's behavior should continue to be monitored and examined. Since the behavioral and physiological signs do not specifically indicate pain, but may be associated with other problems such as hunger, a full diaper, noise, etc. , they appear as "general discomfort" and not necessarily pain. The source of discomfort should be clarified - whether it is pain or another factor.
, they appear as "general discomfort" and not necessarily pain. The source of discomfort should be clarified - whether it is pain or another factor.
How can you tell if a child is in pain or otherwise uncomfortable?
If the source of the pain is known, for example, if the child is injured or suffers from an illness accompanied by painful sensations, such as earaches, the discomfort is most likely associated with this.
If the child shows discomfort for no apparent reason, find out what the problem is - offer to drink, eat, change the diaper, check if the discomfort is related to uncomfortable clothing or a stuffy room. If, despite everything, the child is restless, pain is most likely the source of discomfort. Taking an over-the-counter pain medication as recommended by the doctor may help.
Identification of the degree of pain in children who can describe their problem, but do not yet know the numbers.
Roni, 5 years old, arrived at the emergency room after the car he was traveling in got into a road accident. He is scared and refuses to speak. Although he is a developed boy and can describe what hurts him, at this age children often refuse to cooperate in case of anxiety or fear and will not answer the question: “What hurts you? Where?"
He is scared and refuses to speak. Although he is a developed boy and can describe what hurts him, at this age children often refuse to cooperate in case of anxiety or fear and will not answer the question: “What hurts you? Where?"
Between the ages of 2.5 and 8 years (or until the age at which children understand the meaning of numbers and comparisons), children can report that something hurts them and show where it hurts (head, stomach, leg, etc.), but very often they find it difficult to answer the question about the degree of pain, what they feel and how pain affects their well-being.
It is recommended that you ask specific questions to help you gather the information you need. For example, to the question: “Can you draw?”, the child can answer in the negative and explain that his arm hurts.
Although it is not easy for children to describe the degree of pain, you can help them to do this with a ruler of facial expressions. Show the child this ruler:
Pointing your finger at each drawing, say:
- this facial expression - nothing hurts him
- and this hurts a little
- here there is pain that interferes
- here the pain is very strong
- and here there is pain that cannot be endured what he feels.
 Usually a child who is in pain will indicate the facial expression "great pain". Very often, children perceive this drawing as “I am sad”, and not as “I am in pain”, and therefore it is very important to ask these questions to the child in a relatively calm environment, and not after, for example, taking blood for analysis.
Usually a child who is in pain will indicate the facial expression "great pain". Very often, children perceive this drawing as “I am sad”, and not as “I am in pain”, and therefore it is very important to ask these questions to the child in a relatively calm environment, and not after, for example, taking blood for analysis. This ruler does not always help. Pain is an abstract concept and it is impossible to “show” it to a child, as they show it to an object or another person. Children perceive the meaning of pain according to what they have experienced. For example, if you ask a 4-year-old child who has not experienced serious pain to explain what pain is, the answer will usually be “When I hit my hand” - this is how he perceives pain. Most likely in this case the ruler will be useless.
Determination of the degree of pain in children who understand the numbers
Children and teenagers who understand numbers, as well as adults, can report their condition using a ruler from 0 (no pain at all) to 10 (unbearable pain).
 Presenting the ruler, they ask a question, pointing to it: 0 - does not hurt at all, the larger the number - the more painful sensations; for example, 5 is moderate pain, 9 is very severe pain, 10 is unbearable pain.
Presenting the ruler, they ask a question, pointing to it: 0 - does not hurt at all, the larger the number - the more painful sensations; for example, 5 is moderate pain, 9 is very severe pain, 10 is unbearable pain. According to the instructions of the Israeli Ministry of Health of 200, the degree of pain from 3 and above requires some kind of relationship - medicinal or otherwise.
A small child is in pain. What should I do?
During the first thousand days of life, a child needs special attention and care. A baby is born weighing 2.5-5 kg, without teeth and kneecaps, with soft bones and with a "fontanelle" in the skull. By the year, his weight increases by 2-3 times, the first teeth appear, the "font" overgrows, vision and hearing become almost like an adult, he begins to move independently, pronounce the first meaningful sounds and show emotions.
By the age of two, height doubles and is half of its "adult" height (for example, if at birth the height was 53 cm, at 2 years old - 90 cm, and at 25 years old it will be 180 cm).
 From two to three years old, the baby develops kneecaps, and he learns to run, milk teeth grow, and the intestines begin to digest solid food. Increased motor skills, reaction and learning.
From two to three years old, the baby develops kneecaps, and he learns to run, milk teeth grow, and the intestines begin to digest solid food. Increased motor skills, reaction and learning. Mothers know that diseases of the early period are different from diseases of adults, and even from diseases of older children. And many diseases do not need treatment at all - this is one of the manifestations of a growing organism.
Read more about infant diseases here:
A child under one year of age: what to fear and what not to pay attention toUntil a certain period, a small person cannot explain what and how it hurts, so mothers need to learn to determine it on their own or contact a pediatrician. At the first meeting of the "Healthy Journalist" club in 2018, organized by SANTO, pediatricians talked about what to pay attention to and how to cure simple childhood diseases. Neurologist, Director of the Department of Pediatrics Healthcity clinic (MBA) Konstantin Pushkarev and pediatrician, Doctor of Medical Sciences, Professor of the Department of KazNMU named after.
 SD Asfendiyarova Saule Sarsenbayeva shared their knowledge, experience and gave examples from their practice.
SD Asfendiyarova Saule Sarsenbayeva shared their knowledge, experience and gave examples from their practice.
Saule Sarsenbayeva and Konstantin Pushkarev
Why does the child have a fever?
Fever usually occurs in infectious diseases. The body fights pathogens, an antiviral substance, interferon, enters the bloodstream. In the blood, metabolism and bactericidal activity are enhanced in order to more effectively fight bacteria and viruses. Therefore, doctors do not recommend medication to lower the temperature on the first day or lower it if it is not too high. But a baby is not a smaller copy of an adult. Many processes are arranged differently, including heat transfer.
"Little children have problems with heat transfer - they quickly supercool and just as quickly overheat. If there are usually no issues with the cold - any mother first of all tries to warm her child, then in the second case a problem arises - we are used to wrapping children.
 But they cannot wrap up even in cold weather. Many inflammatory processes spread rapidly," said Saule Sarsenbayeva.
But they cannot wrap up even in cold weather. Many inflammatory processes spread rapidly," said Saule Sarsenbayeva. Babies have more pronounced symptoms of intoxication - at high temperatures they become lethargic, inactive, they feel nauseous. The loss of micro and macro elements, dehydration quickly sets in. If the temperature rises, parents need to water their babies more. On the other hand, babies have the advantage of recovering much faster than adults.
What to do if the baby has a fever?
- First, the temperature must be measured with a thermometer.
- If the temperature is not high (38 degrees for newborns and 39 degrees for children older than three months), nothing needs to be done. We must continue to observe, measuring the temperature every two hours, not forgetting to drink warm water.
- If the temperature is higher than 38-39 degrees or lasts for a long time, then you need to cool the child - first of all, undress and transfer to a ventilated room, closing the windows before that.

- You have cooled the child, but the temperature is not decreasing. Try to wipe the baby with a cotton swab moistened with ordinary boiled water or a weak vodka solution. The alcohol evaporates quickly, taking excess heat from the skin with it.
- If all of the above do not help, call your doctor. Most likely he will prescribe an antipyretic syrup. Be sure to specify the dose and frequency of administration and strictly adhere to the scheme. If after taking the drug the temperature immediately decreased, you still need to adhere to the appointment of a pediatrician.
Many parents are afraid of children's seizures and for good reason, because the brain remembers this reaction of the body to an increase in temperature. At the first manifestations of convulsions, immediately begin to bring down the temperature. Konstantin Pushkarev gives advice from American colleagues: at a high temperature, bathe the baby in a warm bath with a water temperature of 36.
 6 degrees. A few minutes is enough to return the baby to normal body temperature and avoid convulsions.
6 degrees. A few minutes is enough to return the baby to normal body temperature and avoid convulsions. Another point that parents should pay close attention to is how exactly a child has a fever at an elevated temperature. There are two types of fever - pink and white . With rose fever, the blood vessels dilate, the person is hot, everything is on fire. This is a good reaction to pathogens, which means that the body is actively getting rid of excess heat. First of all, physical methods of cooling help here, and often it does not come to antipyretic drugs. But white fever is characterized by fever and pale skin. Here, physical methods of lowering the temperature can do harm. A baby with such symptoms can only be helped by a pediatrician.
Why is the child in pain and what to do about it?There is an "onion" theory that originated in the pre-war years, but finally formed in 2014, which says that all pain consists of the same components:
- Nociception - mechanical, thermal, chemical stimuli or genetic predisposition to pain.

- Pain is the interaction of the nociceptive system with the antinociceptive system and their influence on each other.
- Experience is an affective component in which the limbic system plays a role, which determines human behavior. Several factors play a role. For example, genetics, gender, age and scope of work.
- Pain behavior that depends on the patient's age, activity and past knowledge of this type of pain.
- Relationships with others. It has been proven that trusting relationships with other people, colleagues, relatives or medical personnel reduce sensitivity to pain.
"All people, big and small, are afraid of pain," said Konstantin Pushkarev. "Pain is a four-component process. It is simultaneously social, physical, mental and psychological."
What kind of pain is there?
Nociceptive is caused by tissue damage. Neuropathic appears when the nervous system is damaged.
 The third type has no name, but this pain occurs due to neurological dysfunction. All three types of pain are experienced differently by people. The pain is sharp, throbbing, burning, shooting, aching, but in any case, it brings a person only suffering, and in some cases brings death closer. According to Konstantin Pushkarev, even very young children can experience phantom pain. For example, if a child experienced discomfort during fetal development, these sensations may be repeated. The problem with childhood pain is that babies almost up to a year old cannot show where it hurts, and up to two years old they cannot explain exactly how it hurts.
The third type has no name, but this pain occurs due to neurological dysfunction. All three types of pain are experienced differently by people. The pain is sharp, throbbing, burning, shooting, aching, but in any case, it brings a person only suffering, and in some cases brings death closer. According to Konstantin Pushkarev, even very young children can experience phantom pain. For example, if a child experienced discomfort during fetal development, these sensations may be repeated. The problem with childhood pain is that babies almost up to a year old cannot show where it hurts, and up to two years old they cannot explain exactly how it hurts.
"If a very small child is crying, it is possible that something hurts him. The first actions of the mother: take him in her arms, shake him, stroke him, feed him and talk to him in an affectionate, calm voice. Mother's native smell, soothing voice, gentle hugs - all this calms the baby. Breast milk contains painkillers. We must remember that the emotional state of the mother is immediately transmitted to the child.
 If the mother is angry and worried, the child will also cry. But then dad will come, take him in his arms, stroke, kiss and will give him calming testosterone. Thus, the pain and anxiety associated with them will gradually pass, "said Konstantin Pushkarev.
If the mother is angry and worried, the child will also cry. But then dad will come, take him in his arms, stroke, kiss and will give him calming testosterone. Thus, the pain and anxiety associated with them will gradually pass, "said Konstantin Pushkarev. It is not always possible to calm the pain with parental love, and then painkillers are used. Analgesics for children are divided into several categories, and paracetamol and Ibufen ® are considered the safest and most effective, which also lower the temperature. Each of these drugs has its own contraindications and advantages - for example, paracetamol has not yet been proven safe for long-term use, and Ibufen ® should not be given to children under three months old. But doctors emphasize that any antipyretic and analgesic syrup should be given to the child not out of necessity, but according to the scheme described in the instructions for the drug, or on the recommendation of a doctor. At the same time, babies should easily swallow the medicine, so it should not be in solid form.
 The ideal form is syrup. Ibufen ® (ibuprofen) is prescribed for children with colds, childhood infections accompanied by fever, influenza, pharyngitis, pain syndrome: toothache / teething, headache, ear pain and even post-vaccination reactions. It is important to remember about the dosage, which is easy to follow with a dosing syringe, and not to exceed the recommended rate for children of different ages.
The ideal form is syrup. Ibufen ® (ibuprofen) is prescribed for children with colds, childhood infections accompanied by fever, influenza, pharyngitis, pain syndrome: toothache / teething, headache, ear pain and even post-vaccination reactions. It is important to remember about the dosage, which is easy to follow with a dosing syringe, and not to exceed the recommended rate for children of different ages. The main thing to remember is that a child under 15 should never be given aspirin. Saule Sarsenbayeva gave an example from her practice: parents wanted to quickly put their 8-year-old daughter on her feet with a cold and stuffed her with everything they found in the first-aid kit. As a result, the baby was brought to the intensive care unit with bleeding from literally all organs: in addition to internal bleeding, blood oozed from the eyes, nose, and urethra. Aspirin is a very effective medicine for colds, but deadly for children, including those who have not yet been born.

How to communicate with a child who is in pain?According to statistics, 70% of those with ARVI in Kazakhstan are under 14 years old. This means that children are the main recipients of doctors and pharmacies. And therefore, further information applies to everyone who is in one way or another in contact with sick children - parents, pharmacy staff, doctors and nurses.
But the problem is that even doctors were not taught to treat a sick child properly before. The main thing was to help, this is the necessary good, and in what form it is caused, it was not important. But, for example, in the United States, doctors have long understood that a friendly conversation with a patient not only calms him down before unpleasant treatment procedures, but also has a high therapeutic effect.
Kazakh doctors are gradually mastering communication skills, this discipline has already begun to be taught in medical universities. Often in small towns and rural clinics, doctors do not consider it necessary to pay attention to a small patient.