In labor but not dilating
Why Is My Cervix Not Dilating? (In the First Stages of Labor)
Cervix dilation is one of the earliest signs that the birth of your baby is imminent. As you approach your due date, your doctor will check your weekly visits to see if you are dilated. Dilation begins once you have lost your mucus plug and cervical effacement has occurred. You may also experience a bloody show, a mix of blood and mucus when you lose your mucus plug.
There are three stages of labor: latent labor, active labor, and the delivery of the placenta, which is often glossed over when discussing labor.
As labor progresses, so will cervical dilation, from 1 cm, roughly the size of a blueberry, to 10 cm, the size of a bagel.
More: Labor Complications
Dilation During The 3 Stages of Labor:
- Latent Labor (the first stage of labor 1- 9 cm dilated)
- Active Labor (the second stage of labor 10 cm dilated)
- Placenta Delivery (the third stage of labor)
The first stage of labor could take several weeks, and you may stay dilated at only 1 or 2 centimeters for several ob-gyn visits in a row! When dilation fails to progress, women often wonder why is my cervix not dilating? Fortunately, there are many reasons why it may seem there is a failure to progress in labor. We will break down the various reasons for the cervix not dilating in the coming sections.
Failure to Progress in Labor
When labor fails to progress, it means your cervix is not dilating, and your baby is not descending. When this happens, your health care provider will likely assess what are known as the Three Ps.
- The Passenger (the size of the baby and his position in the uterus)
- The Powers (the efficiency of your contractions)
- The Passage (the size and shape of your pelvis)
In early labor, these three elements work together to progress towards the active phase of labor. If one of these elements is not aligned, the latent phase of labor may not progress as quickly or smoothly as mom and doctor would like.
More: Labor Complications
Cephalopelvic Disproportion (The Passenger)
Cephalopelvic Disproportion (CPD) occurs when the baby’s head is too large to fit through the women’s pelvis. The condition is considered rare and can only be fully diagnosed during labor, and 70% of pregnant women are able to deliver vaginally and without major complications.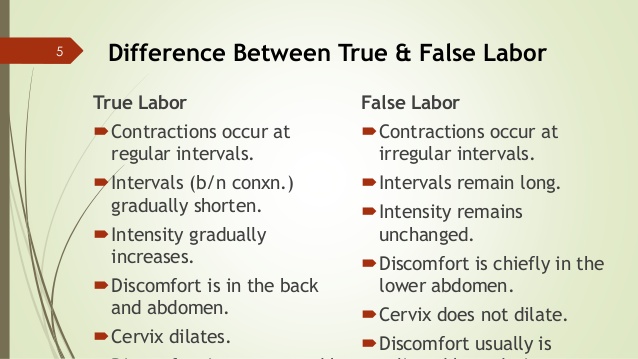
Sometimes Cephalopelvic Disproportion may be suspected before labor in late pregnancy if your doctor’s measurements indicate the baby will be large.
If CPD is suspected, but the baby's head has engaged, you can still attempt a vaginal birth. Your doctor and nurses will monitor the labor with a labor graph, and if there are signs that the baby is in distress, an emergency cesarean may be performed. Likewise, a planned cesarean may be offered if the head hasn't engaged toward the end of labor or your doctor suspects CPD may be a concern before labor.
Inefficient Contractions (The Power)
Another reason your labor may not be progressing could be because your cervix is dilating slowly or has stopped dilating. Once labor begins, regular contractions will occur every 2 to 3 minutes. Your doctor will also assess how strong the labor contractions are by palpating your abdomen: the firmer it feels during contractions, the more likely they are to be effective.
If your contractions become too intense, you can request an epidural to help with the pain. Keep in mind; however, it could be an hour or more after you request it before you are able to receive pain relief. Additionally, not all women and pregnancies can receive an epidural, so be sure to discuss the specifics with your doctor long before labor starts.
Keep in mind; however, it could be an hour or more after you request it before you are able to receive pain relief. Additionally, not all women and pregnancies can receive an epidural, so be sure to discuss the specifics with your doctor long before labor starts.
If you have begun having contractions but they are widely spaced, and their strength indicates they're unlikely to be effective, your doctor may use one or two techniques to speed up labor, known as augmenting labor.
First, they may artificially rupture the membranes if it hasn’t happened naturally. The rupturing of the membranes is also known as when your water breaks.
If this procedure fails to further dilation and the cervix opens only minimally. In that case, you may be given the drug oxytocin to increase the strength and frequency of contractions, also known as labor induction. It is more common for first-time moms to need an induction to produce uterine contractions than those who have experienced labor before.
Initially, a small dose is given and then increased over time until you're having three or four moderately strong contractions every 10 minutes. You’ll have continuous electronic fetal monitoring to ensure that the baby is not distressed by the sudden onset of stronger contractions if this is done.
If your labor is still not progressing several hours after the drugs have been started, then a cesarean may be recommended.
More: Cesarean Sections
Posterior Presentation (The Passage)
The best position for your baby in labor is an occiput-anterior position with the back of the head (occiput) facing your front. If the back of the head faces your back (occipito-posterior), this can make it hard for the baby to turn and move down the birth canal and can prolong labor. The doctor may suggest that you change positions to encourage the baby to turn. If the baby fails to rotate, forceps or vacuum may be needed to aid the delivery.
A gynecoid pelvis is a name given to a pelvis that has a circular shape. The generous proportions of this more typical "female-shaped" pelvis provide room for the head to pass through during birth.
The generous proportions of this more typical "female-shaped" pelvis provide room for the head to pass through during birth.
An android pelvis is a term used to describe a pelvis with a more triangular shape. This reduces the room available for the baby's head to pass through and is more likely to cause problems during vaginal delivery.
The good news is that the obstetrics community states that the shape and size of your pelvis have no bearing on fertility or your ability to become pregnant.
Sources
- Cervix Dilation Chart: Stages of Labor (healthline.com)
- The 5 P’s of Normal Labour and Birth - Kiwi Families
- Cephalopelvic Disproportion: Signs, Causes, and Potential Risks (flo.health)
- Epidural Pros and Cons: Should I Get One During Labor? (healthline.com)
- Premature rupture of membranes: MedlinePlus Medical Encyclopedia
- Do you know what your pelvis type is? (modernfertility.com)
A gynecoid pelvis is the name given to a pelvis that has a circular shape. The generous proportions of this more typical "female-shaped" pelvis provides room for the head to pass through during the birth.
The generous proportions of this more typical "female-shaped" pelvis provides room for the head to pass through during the birth.
Android pelvis
An android pelvis is the term used to describe a pelvis that has a more triangular shape. This reduces the room available for the baby's head to pass through and is more likely to cause problems during vaginal delivery.
Slow progress in labour – signs and management
beginning of content8-minute read
Listen
What is slow progress in labour?
Slow progress in labour is when any of the stages of your labour take longer than expected. It may also be called failure to progress or prolonged labour.
Slow progress in labour can be difficult to define. This is due to variations in labour for different people and the evidence available to support this.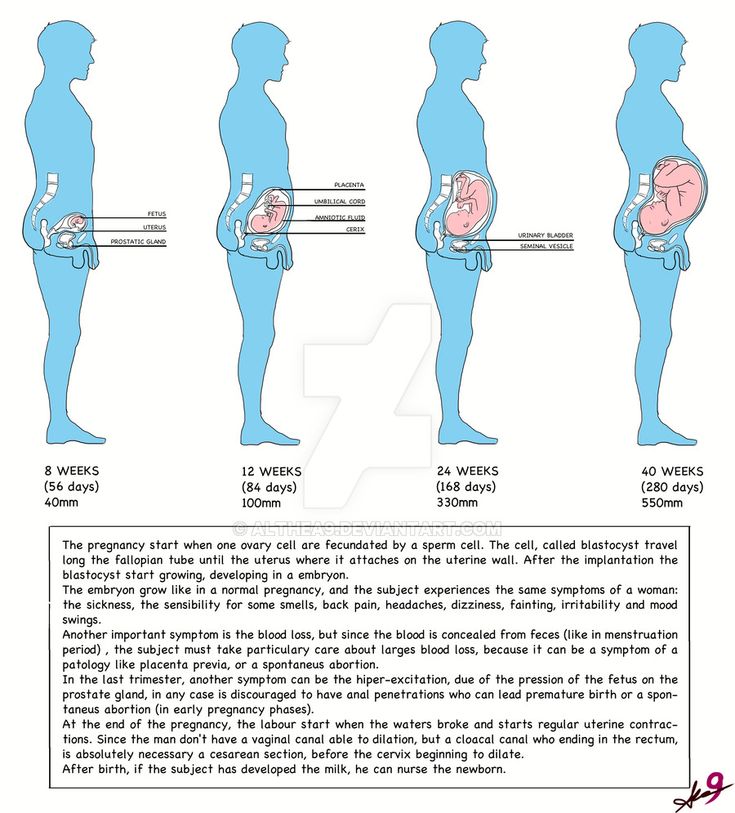 It’s important to note that when labour progress is checked, many factors are taken into consideration. This includes the wellbeing of both you and your baby. Your birthing preferences are also important.
It’s important to note that when labour progress is checked, many factors are taken into consideration. This includes the wellbeing of both you and your baby. Your birthing preferences are also important.
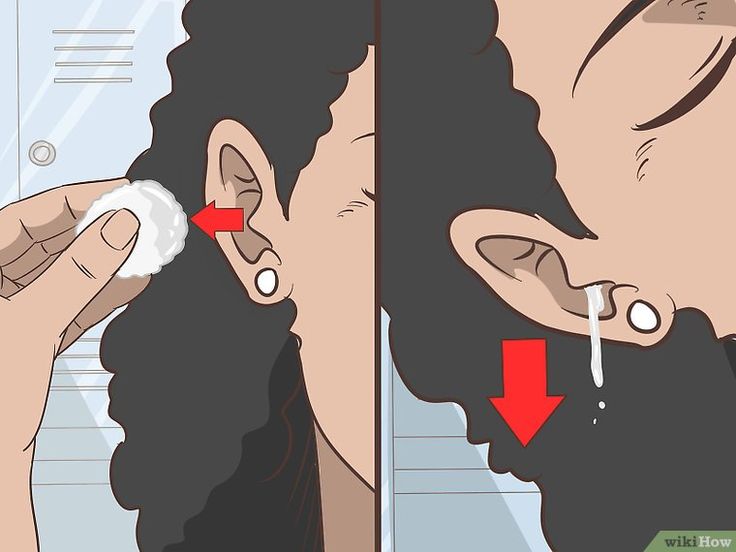
Your healthcare team will assess labour progress through observations and physical examinations, including:
- cervical dilatation (opening of the cervix)
- cervical effacement (thinning out of the cervix)
- lowering of your baby’s head in your pelvis
- increasing strength and duration of your contractions
Slow progress in labour can be risky to both you and your baby.
What are the causes of slow progress in labour?
Slow progress in labour may be more likely if your:
- the baby is large
- the baby has a large head
- the baby is in a difficult position
- contractions aren’t strong enough and your cervix doesn’t open (dilate)
- pelvis is too small to fit your baby through
You may also have a greater chance of slow progress in labour if:
- you are overweight
- you have gained a lot of weight during your pregnancy
- this is your first baby
When does slow progress in labour happen?
Slow progress in labour can happen at any stage of your labour.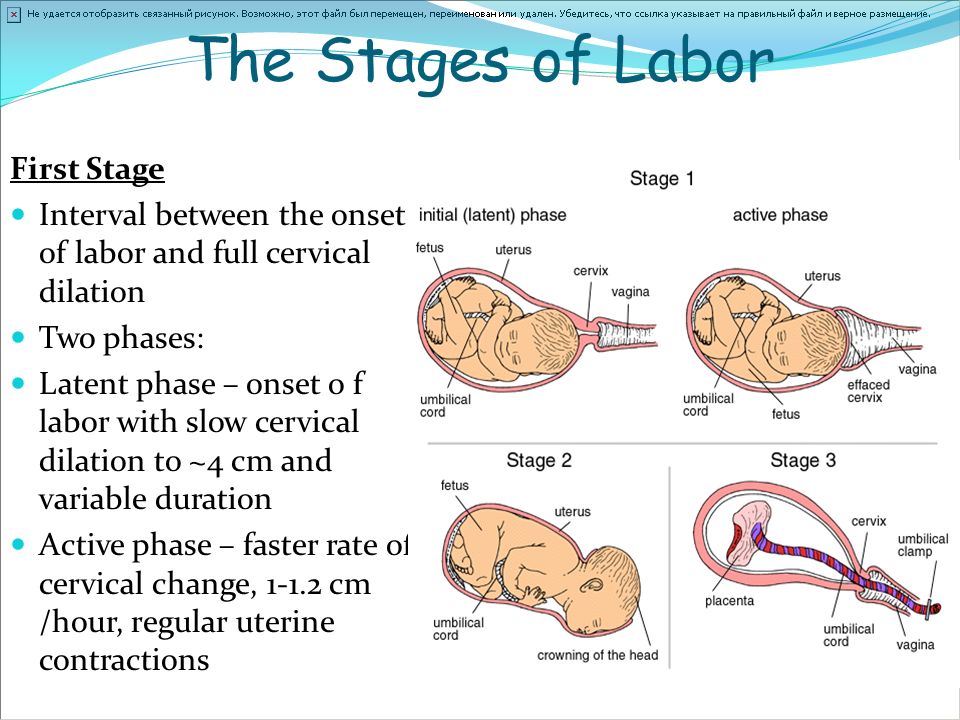
First stage of labour
The first stage of labour happens in 3 phases:
- the latent phase
- the active phase
- the transition phase
This stage of labour often stops and starts. It may take up to:
- 12 hours if it’s your first baby
- 10 hours if you’ve had a baby before
Sometimes your contractions won’t be strong enough to dilate your cervix fully. This happens when:
- your cervix doesn’t dilate by about 1cm every hour
- your labour stops altogether
If this happens, your doctor might talk with you about options to intervene and get your labour moving. You have the right to make your own choices about the interventions you want.
Second stage of labour
The second stage of labour is the time between full cervical dilatation (10cm) and the birth of your baby.
This stage could last:
- up to 3 hours if it’s your first child
- up to 2 hours if you’ve had a baby before
If the second stage of labour is taking longer than expected, your doctor will talk with you about your options.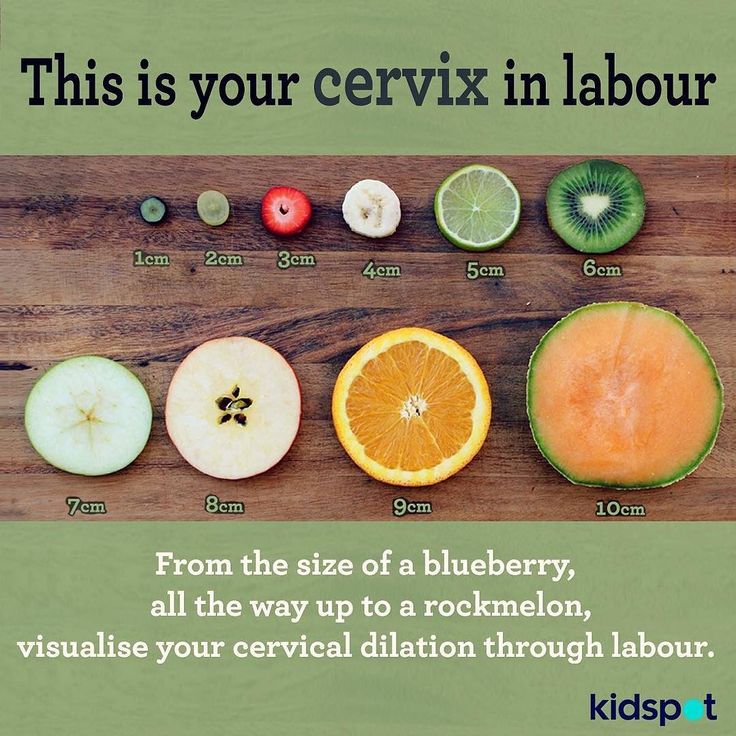 They may recommend intervening. It is your choice to have any interventions to help speed up the delivery of your baby.
They may recommend intervening. It is your choice to have any interventions to help speed up the delivery of your baby.
Third stage of labour
The third stage of labour is the time between the birth of your baby and the delivery of the placenta. This usually lasts about 30-60 minutes depending on how this stage is managed (active or physiological). This stage of labour is carefully supervised.
Active management of labour is recommended to reduce the risk of postpartum haemorrhage (bleeding after the birth). Your midwife or doctor will give you an injection of a medicine called oxytocin after your baby is born. They will clamp and cut the umbilical cord and apply gentle traction to the cord to deliver the placenta.
This is optional and some people choose to deliver the placenta naturally without intervention. This is called physiological management.
How is slow progress in labour managed?
If you have slow progress during labour, your midwife and doctor will monitor you closely.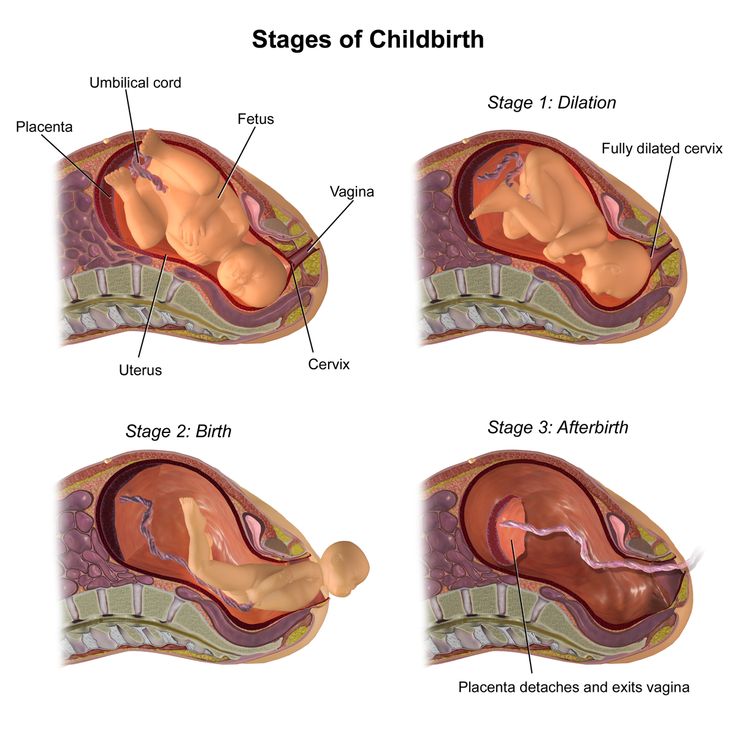
They will measure:
- how much your cervix is dilating
- how long your contractions last
- how often you are having contractions
They will continuously check the health of both you and your baby. If there are any concerns these will be discussed with you.
If you are in the first stage of labour, your midwife and doctor may recommend:
- breaking your waters
- giving you a medicine called oxytocin
This will speed up your contractions and make them stronger.
Other things you can try to help your labour progress include:
- changing position
- moving around and staying active
- relaxation techniques
- pain medicine
If your baby has already entered your birth canal, your doctor may suggest delivering your baby using: forceps or ventouse (vacuum cup).
In some cases, an emergency caesarean may be recommended if there is concern that you or your baby are unwell.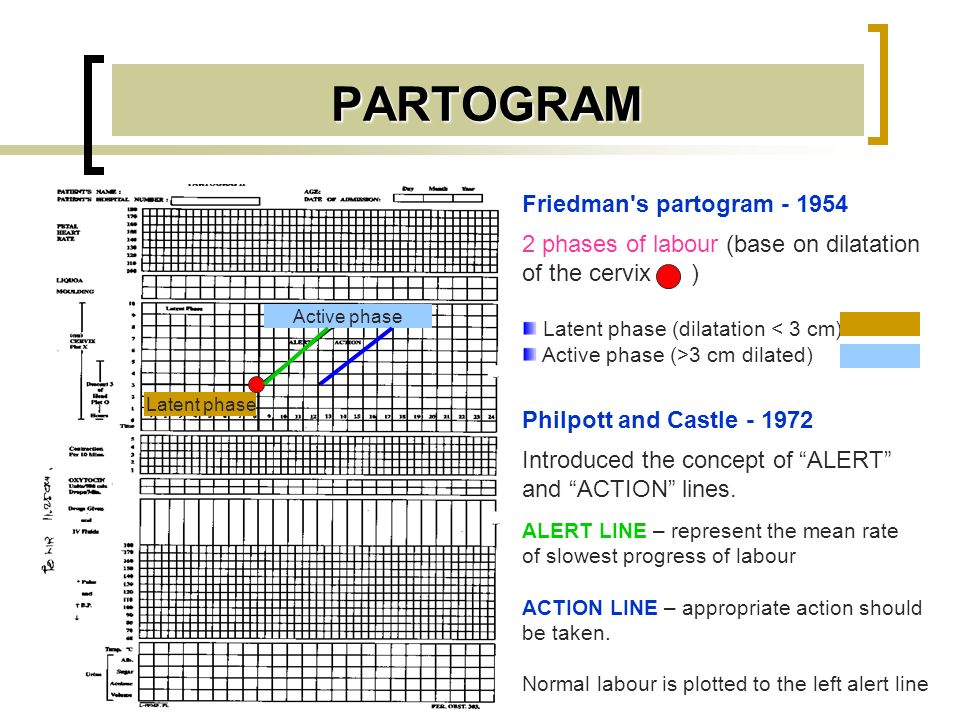
What are the risks of slow progress in labour?
Sometimes, slow progress in labour can result in health issues for you and your baby.
What are the risks to my baby?
The risk of slow progress in labour to your baby depends on many factors. Your healthcare team will explain any concerns they may have about your baby’s health.
They may have an increased risk of:
- low oxygen levels
- abnormal heart rhythm
- meconium (poo) in the amniotic fluid
- infection (when germs get in their body)
If meconium (poo) is in the amniotic fluid, this can be a sign that your baby is distressed. Meconium is your baby’s first poo and is very sticky and tar-like. Babies usually have their first poo after they are born. But some babies who are stressed during labour may pass meconium when they are still in the womb. If this happens your baby might breathe in amniotic fluid containing meconium. This can make it difficult for them to breathe after birth.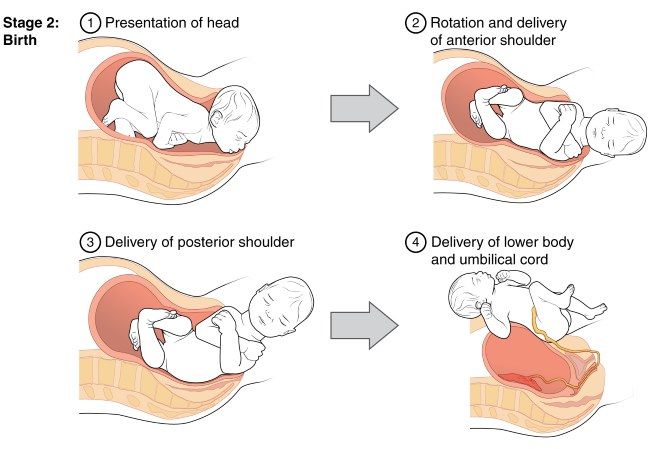 When they are born they may require special care.
When they are born they may require special care.
If either forceps or ventouse are used to help you have your baby, there is a risk your baby may have some swelling or marks on their head. These usually fade quite quickly.
What are the risks to me?
Slow labour can increase the risks of post-partum haemorrhage and uterine infection. Assisted delivery can injure the mother, but most injuries will be temporary and will heal over time. Sometimes the injury can be more long lasting and may need further treatment.
Your medical team may suggest an emergency caesarean if other interventions don’t work. As with any type of surgery, there are some risks. At this point a caesarean is usually the safest option for both you and your baby.
What happens after my baby’s birth?
If your labour didn’t go to plan, you might feel different emotions about your birth. You may feel stressed and experience anxiety about motherhood.
If you feel sad, disappointed or distressed by what happened, it’s important to talk to someone. You might want to consider contacting:
You might want to consider contacting:
- Your doctor
- Perinatal Anxiety & Depression Australia (PANDA) on 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blue on 1300 22 4636
Will I have slow progress in future births
Every pregnancy and birth are different. You won’t necessarily have slow progress in your next labour.
If you’re worried about any future pregnancies, you should talk to your doctor or midwife. They can explain what happened and discuss any further pregnancy risks.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Safe Care Victoria (Care during labour and birth), Queensland Government (Stages of labour), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) (Provision of routine intrapartum care in the absence of pregnancy complications), Queensland government (Guideline: Normal Birth)Learn more here about the development and quality assurance of healthdirect content.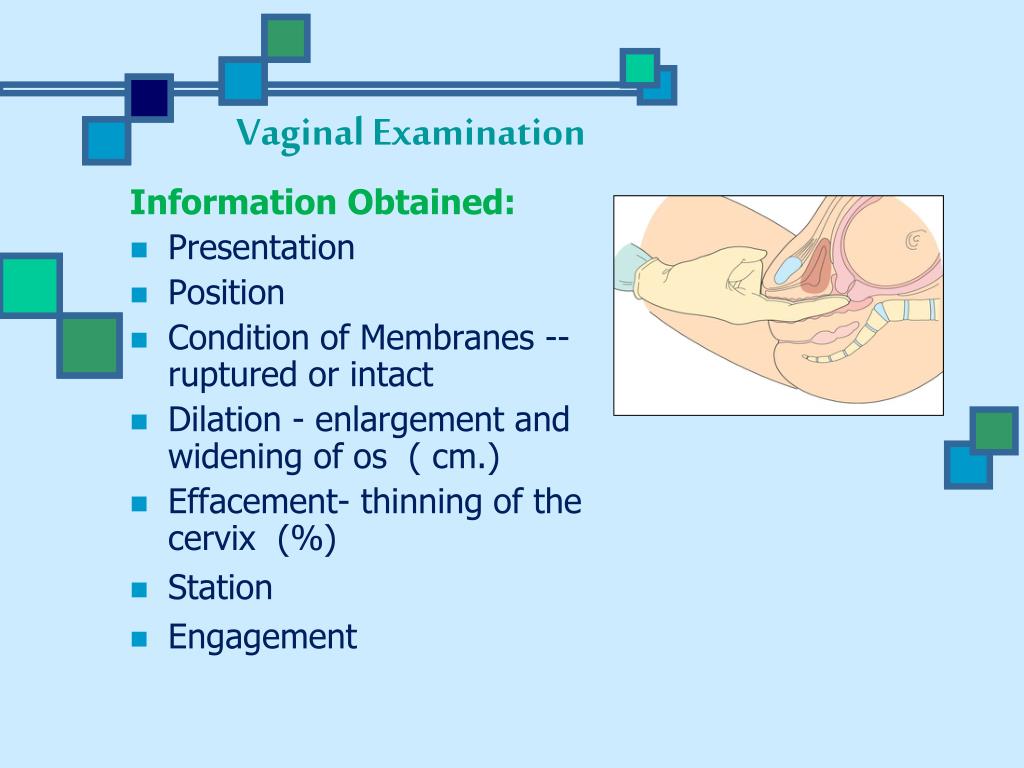
Last reviewed: July 2022
Back To Top
Related pages
- Labour complications
- Interventions during labour
- Induced labour
- Giving birth - stages of labour
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Interventions during labour
An ‘intervention’ is an action taken by a midwife or doctor that literally intervenes in the birthing process. Read about the different types of intervention.
Read more on Pregnancy, Birth & Baby website
Assisted delivery (forceps or ventouse)
An assisted delivery, sometimes called an 'instrumental delivery', is when your doctor will help in the birthing process.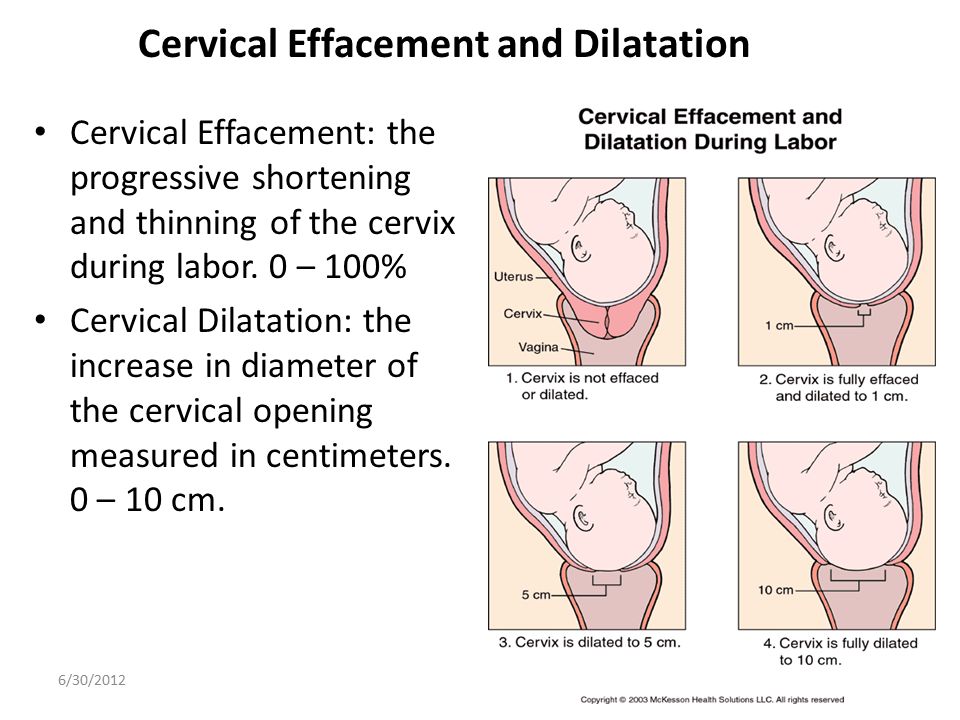
Read more on Pregnancy, Birth & Baby website
Shoulder dystocia
Shoulder dystocia happens when a baby's shoulder gets stuck behind the mother’s pubic bone during birth. It is a medical emergency that requires immediate intervention. Find out why here.
Read more on Pregnancy, Birth & Baby website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after the baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Complicated births | PANDA
Giving birth can lead to a range of complex feelings, especially when the experience is a difficult or traumatic one.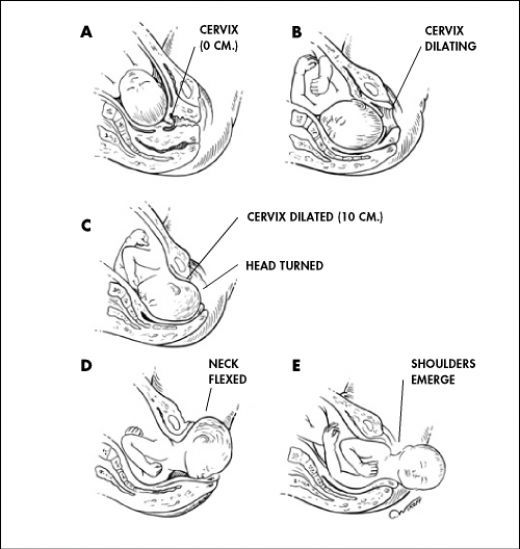
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Placenta accreta
Placenta accreta is a serious but rare pregnancy complication that causes heavy bleeding. If you have it, you will need special care at the birth.
Read more on Pregnancy, Birth & Baby website
Childbirth trauma and recovery | PANDA
While many pregnant women and their partners know birthing their baby will be hard work, very few expect labour and childbirth could be complicated.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Pregnant with twins? About twin pregnancy | Raising Children Network
Pregnant with twins? Twin pregnancy can have more complications, so you’ll need more check-ups.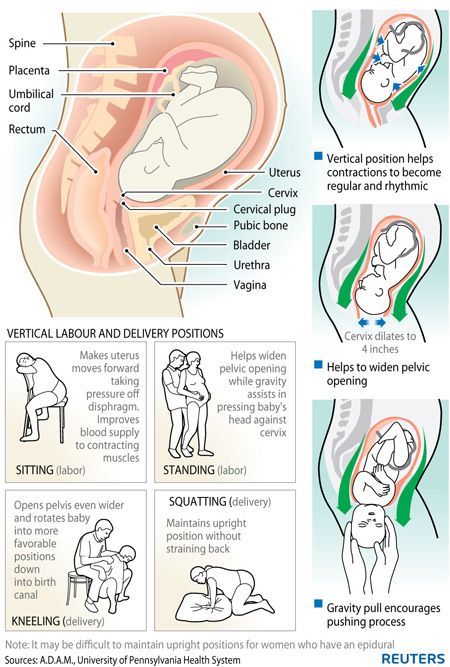 Here’s what to expect in your pregnancy and antenatal care.
Here’s what to expect in your pregnancy and antenatal care.
Read more on raisingchildren.net.au website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKThis information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.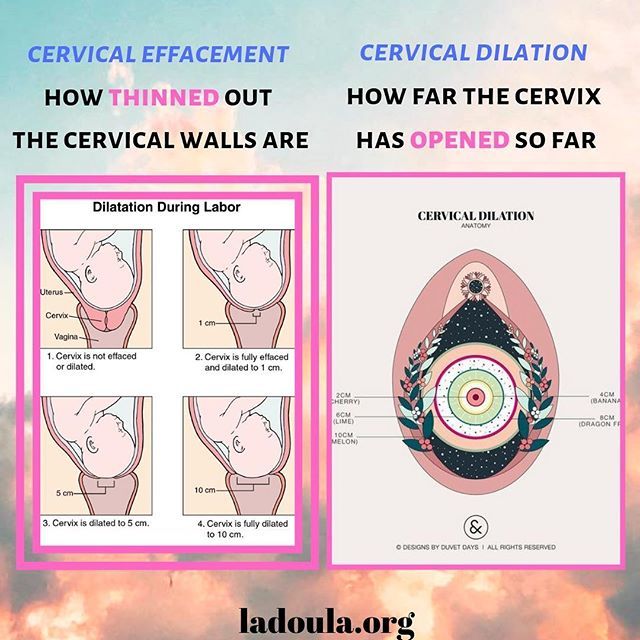
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Some features, tools or interaction may not work correctly.
What will help in childbirth - articles from the specialists of the clinic "Mother and Child"
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now, on the contrary, obstetricians recommend that the expectant mother move . For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how.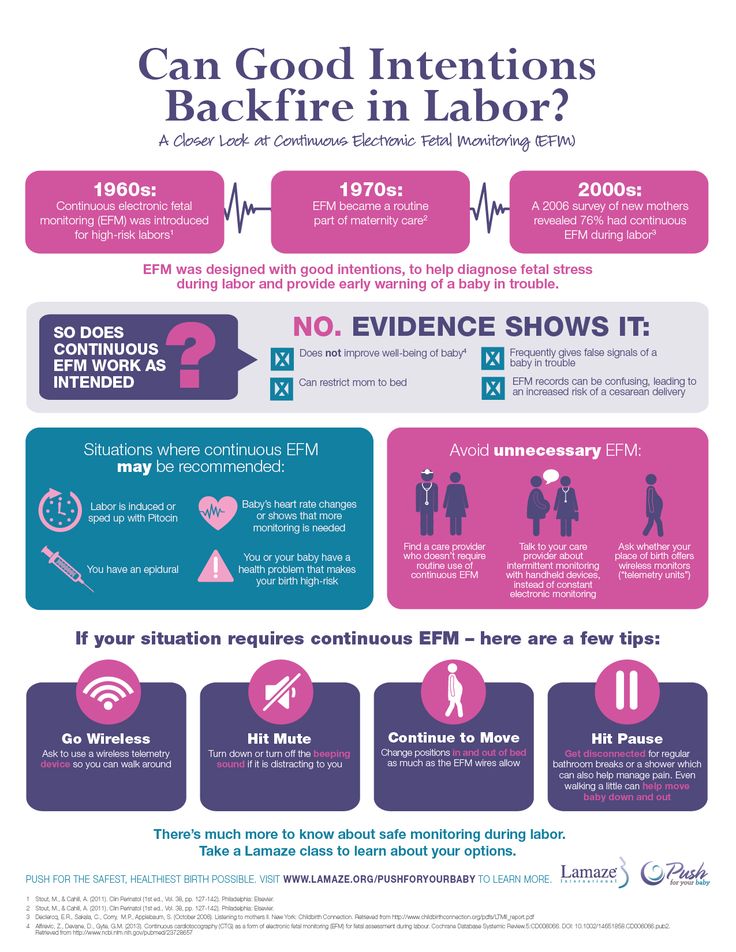 For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements.
For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements.
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease. Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions.
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals.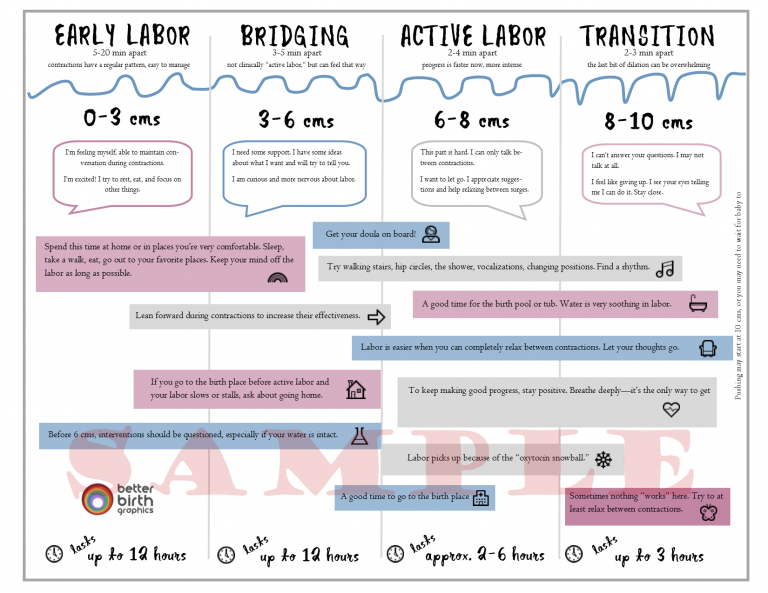 And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
We hang on a rope or wall bars
When the contractions become very strong and painful, you can take poses in which the stomach is, as it were, in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow.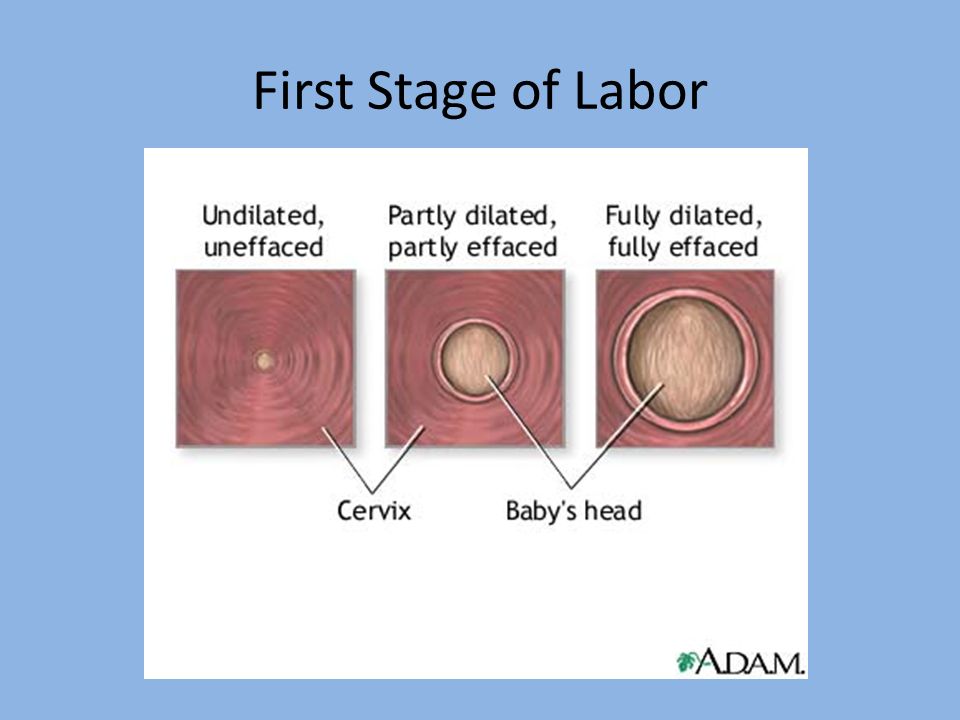 In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain.
In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain.
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If during childbirth a woman wants not to move, but, on the contrary, to lie down, then, of course, she can lie down. In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control.
We use everything we have
In any road block, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
And don't be afraid to look stupid during childbirth. No one in the delivery room cares about how you move or lie down as long as it helps you get through your contractions, so calmly find your comfortable position.
Giving birth in an uncomfortable position is both difficult and inefficient.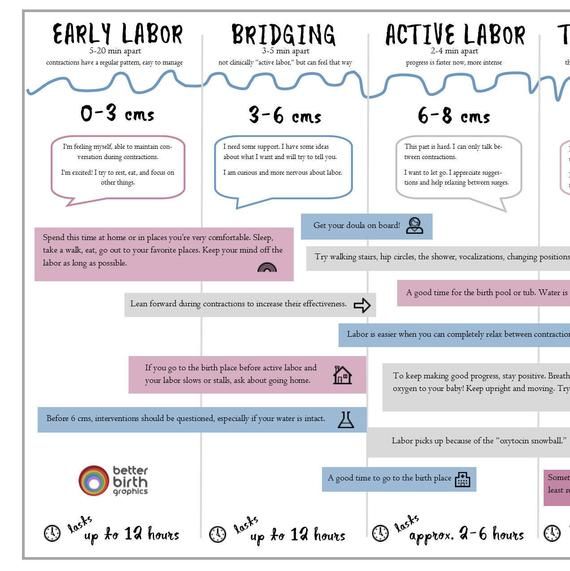 So memorize and rehearse some poses beforehand, and if there are any fixtures in the rodblock, try using them. Something of this will definitely help you to comfortably and easily survive childbirth.
So memorize and rehearse some poses beforehand, and if there are any fixtures in the rodblock, try using them. Something of this will definitely help you to comfortably and easily survive childbirth.
When we move, take various postures, the blood supply to the uterus improves, as a result, it contracts better, and the cervix opens faster. In addition, uteroplacental blood flow improves, and therefore the baby does not suffer from hypoxia
strength to push
By clicking on the send button, I consent to the processing of personal data
Important to know - St. Petersburg citizen's health
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions to the full dilation of the cervix. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is completely flattened and opens about 4 cm.
Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is completely flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm.
3. Transitional (transient) phase, or deceleration phase (lasts from 40 minutes to 2 hours, may be absent in multiparas). This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of expulsion is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because in a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of the amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing.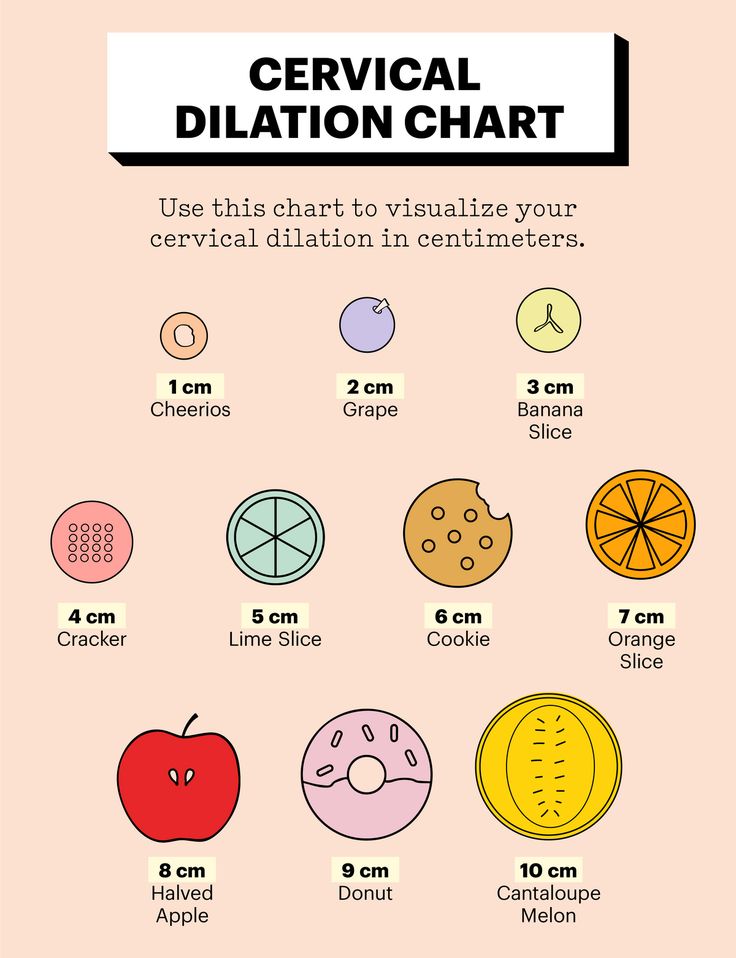 The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
During one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).