How to relieve pelvic pressure during pregnancy
What’s Causing It and How You Can Treat It
Message from our CEO Leighton McDonald
March 29, 2022
To Our Clients, Families and Caregivers,
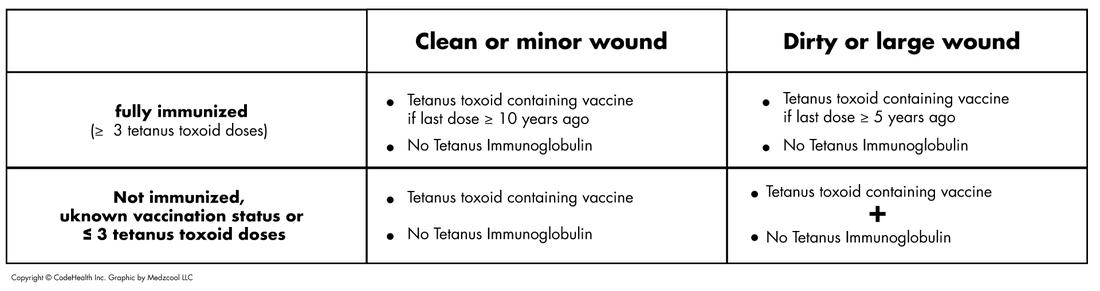
It has been a long two years while we have all worked so hard together to manage the impact of COVID-19 in our own lives and in our communities. Throughout this time, CTG has been committed to continuing to safely deliver high quality care. I am happy to share that 99% of all CTG team members are fully vaccinated against COVID. A very small number of team members have been granted a vaccine exemption and these individuals test themselves for COVID on a regular basis.
As we enter this new phase of the COVID-19 pandemic in Canada, some public health requirements in public settings are changing. Changes such as no longer needing to provide proof of vaccination to dine in a restaurant or no longer being required to wear a mask when we go for groceries.
While these may be welcome changes in public settings, in home care we work in close proximity to people for periods of time and throughout the day we are often providing service to individuals who are vulnerable to becoming very sick due to a COVID-19 infection. As such, we must continue to work together to keep you, other clients and their families, and our CTG team members safe.
Our number one priority will always be the safety and well-being of our clients and CTG team members, every day and at every community, school, or clinic visit. CTG team members follow best practices in infection prevention and control, and we need you to be part of the safety team. Here’s what we can do together to keep everyone safe.
Before your visit
• A CTG team member will be asking you a series of screening questions the day before your visit and again at the time of your visit or appointment.
• It is critical that you answer all the questions honestly as it will help us keep everyone safe. Be assured that regardless of the screening results, you will receive the care you need but we may need to take additional precautions for your safety and the safety of others.
During your visit
• Your CTG health care provider will be wearing both a mask and a face shield or goggles. This is for both their protection and yours.
This is for both their protection and yours.
• You are asked to wear a mask when the CTG provider is in your home; if you do not have a mask, one will be provided to you. All nursing and physiotherapy clients will be provided a new mask when they arrive at a CTG clinic.
• Younger clients are also asked to wear a mask when receiving services in home or at school.
• If caregivers must be present and close by during a visit, they will be asked to wear a mask or face covering.
• Individuals in the home will be asked to maintain a 2 metre (6 feet) physical distance from the CTG provider unless they are an essential part of the care.
• Now that winter is easing, when possible, kindly open doors and windows in your home to take advantage of natural ventilation when a CTG team member is in your home.
• CTG team members will clean their hands frequently for your safety and we ask you do the same.
CTG prides itself on being a Team Made for Caring and our team includes you. Together we can continue to ensure you safely receive the high-quality care you deserve, and our team members remain safe.
Together we can continue to ensure you safely receive the high-quality care you deserve, and our team members remain safe.
If you have any questions or would like more information, please feel free to reach out to us. You can also find current information at www.ontario.ca/coronavirus or www.novascotia.ca/coronavirus
Sincerely,
Leighton McDonald
President & Chief Executive Officer
Closing the Gap Healthcare
Vaginal pressure during pregnancy: Causes and relief
During pregnancy, many women feel pressure, or heaviness, around the vagina. This is normal and can happen in the first, second, or third trimester.
A pregnant woman’s uterus will expand from the size of an orange to the size of a watermelon or larger. Her body will not only need to provide space and nutrients for a new person to develop but will have to produce an entirely new organ in the form of a placenta.
With so many changes happening, it is not surprising that many women notice sudden and unusual shifts in how their bodies feel. Vaginal, pelvic, or lower abdomen pressure is common in all three trimesters of pregnancy.
Vaginal, pelvic, or lower abdomen pressure is common in all three trimesters of pregnancy.
Read on to learn about the causes and symptoms of vaginal pressure during each stage of pregnancy, as well as treatment options and possible complications.
Women will have different experiences of vaginal pressure during pregnancy.
Some may feel an intense pressure in the vagina, while others will have a dull ache throughout the pelvis, or feel like a weight is bearing down on their entire lower body.
Late in pregnancy, this pressure is often due to the baby’s weight pressing down on the pelvic floor, but many other factors can cause pelvic pressure during pregnancy.
Below, we discuss the different causes of vaginal pressure according to the trimester a woman is in:
First trimester
For most women, the first trimester is too early in pregnancy for weight gain to cause vaginal pressure.
Instead, the hormone relaxin is often responsible. This hormone helps relax the muscles, making it easier for the baby to pass through the pelvic area during birth. However, relaxin levels are at their highest in early pregnancy. High levels of this hormone may help the fertilized egg to implant in the lining of the uterus.
However, relaxin levels are at their highest in early pregnancy. High levels of this hormone may help the fertilized egg to implant in the lining of the uterus.
For some women, relaxin can cause muscle pain or tension, including in or around the vagina.
According to studies in animal models, relaxin may also weaken the ligaments that support the pelvis. This can lead to a feeling of pressure, as though something is pushing down on the vagina.
Second and third trimesters
In the second and third trimesters, the combination of a weakening pelvic floor and increased weight putting pressure on the pelvis can cause vaginal pressure.
The pelvic floor resembles a sling made of muscle. It supports the organs of the pelvis, including the uterus, vagina, urethra, and bladder. Pregnancy can weaken the pelvic floor.
Women who have given birth previously may have damage to their pelvic floor, which could cause it to weaken further with a subsequent pregnancy.
The extra weight of pregnancy often becomes more noticeable in the second trimester. As pregnancy progresses, the uterus puts more and more pressure on the lower body.
As pregnancy progresses, the uterus puts more and more pressure on the lower body.
As the pelvic floor weakens, this pressure can cause a feeling of fullness in the vagina or generalized pain and pressure in the hips and pelvis.
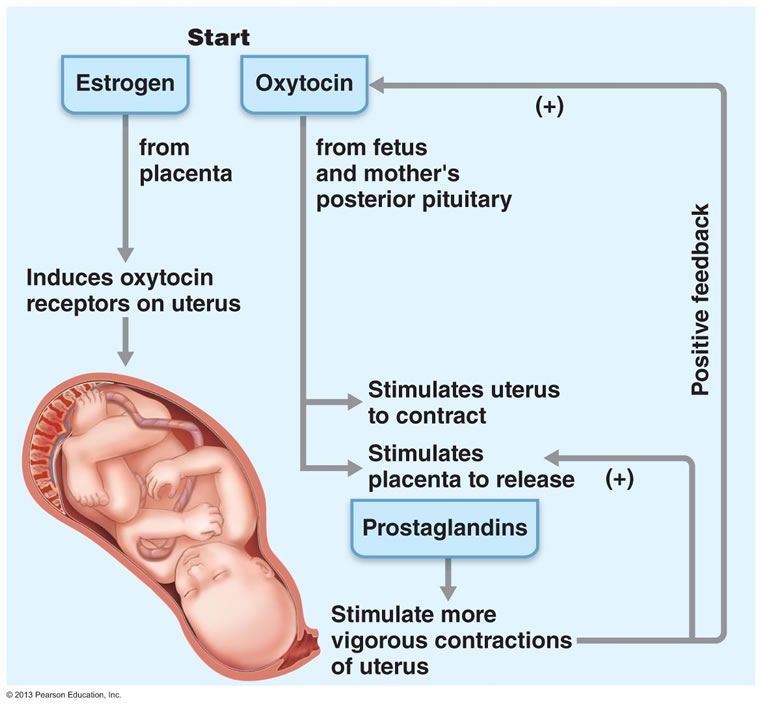
For some women in the later stages of pregnancy, a pressure in the pelvis may be an early sign of labor. If cramping in the stomach also occurs or they feel a sensation of something pressing down on the uterus, it could mean that they are about to give birth.
Common problems in all trimesters
Some factors can cause a feeling of vaginal or pelvic pressure in all stages of pregnancy. These include:
Constipation
Many women struggle with constipation throughout their pregnancy. Constipation can cause a feeling of fullness or pressure in the vagina, especially when the stool is hard or several days have passed since a bowel movement.
Drinking plenty of water and eating fruit and other high-fiber foods may help with constipation.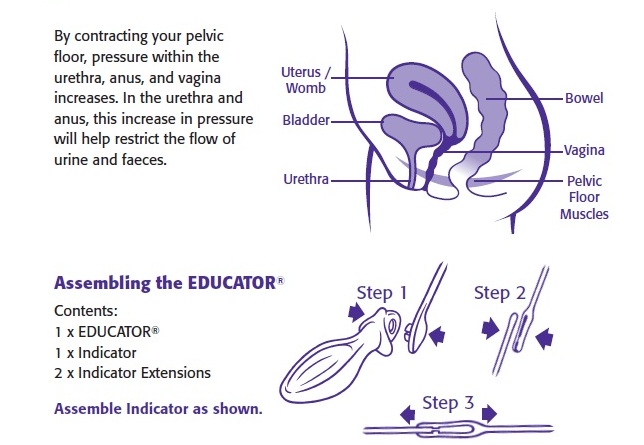
Bladder infections
For some women, pressure or pain can signify a bladder infection. Women are more likely to develop a bladder infection during pregnancy.
If the vaginal or pelvic pressure occurs alongside difficulty going to the bathroom, pain when urinating, or fever, it is essential to see a doctor.
Bladder infections are easy to treat, but, without treatment, they can worsen and increase the risk of health issues during pregnancy.
Pelvic organ prolapse (POP)
When vaginal pressure is intense, it could be a sign of POP. POP happens when organs in or near the pelvis move down, sometimes into the vagina or rectum.
POP is treatable but can cause incontinence, intense pain, and severe complications.
Women who suddenly feel intense pressure, have difficulty controlling their bowel or bladder, or notice that something seems to be pushing down into their vagina, should consult a doctor.
A weak cervix
Some women have a weak cervix, which is sometimes called cervical incompetence or cervical insufficiency.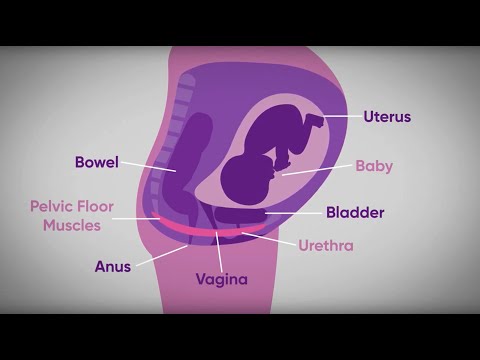
Some women with this condition may have a miscarriage or go into premature labor because the cervix is not strong enough to support the uterus. In most cases, a weak cervix is treatable with early intervention.
Women who feel unexplained vaginal pressure, especially early in pregnancy, could ask a doctor to check their cervix. A previous cervical procedure or injury, including those resulting from childbirth, may increase the risk of a weak cervix.
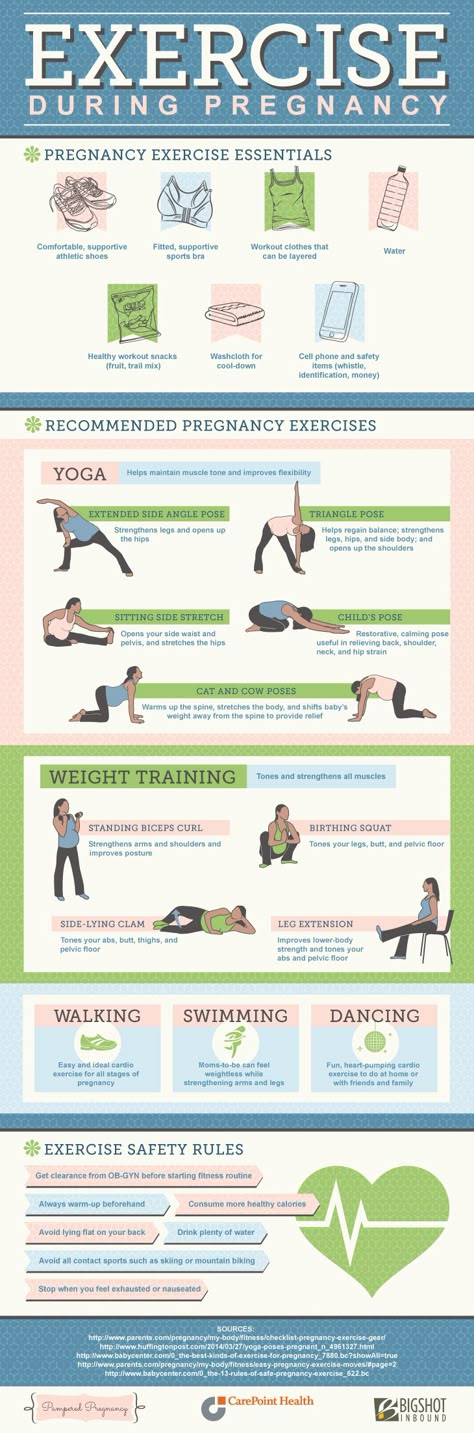
As vaginal pressure is often due to weak muscles and pressure on the pelvis, gentle stretches may help. Try stretching the back and hips to relieve pain and pressure.
A pregnancy yoga or gentle stretching class can help with finding comfortable and safe stretches.
Using a foam roller can help loosen tense muscles. If the pain is intense, applying a heating pad to the sore area may help. Keep the heat low, and remove the pad after a maximum of 10 minutes.
Other strategies may not offer immediate relief, but can reduce the risk of certain conditions that cause vaginal pressure.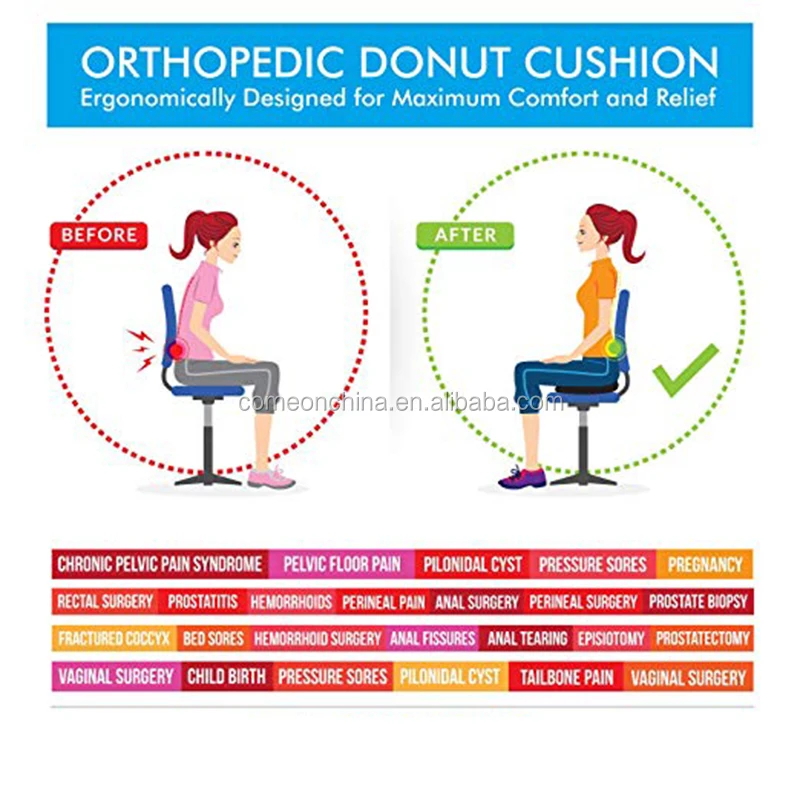 These strategies include:
These strategies include:
- Doing Kegel pelvic floor exercises. Tense the pelvic floor muscles as though trying to avoid urinating, hold for 10 seconds, then release. Repeat 10 times at least twice a day. This can also strengthen the muscles that the body uses to push out the baby.
- Remaining active during pregnancy. Even low-intensity exercises such as walking can help strengthen the muscles and promote good posture. This may relieve pain and pressure and keep the pelvic muscles strong.
- Drinking plenty of water. Stay hydrated, especially after exercising and in hot weather. This can help prevent constipation, which could otherwise lead to pressure.
Share on PinterestA doctor will prescribe treatment if an infection is causing the vaginal pressure.
In most cases, vaginal pressure is just an unpleasant pregnancy side effect resulting from weakened pelvic muscles and weight gain.
However, sometimes a more severe cause will need treating so that it does not harm the woman and baby. An untreated infection, for example, can spread throughout the body and put the baby in danger. It might even cause premature labor.
An untreated infection, for example, can spread throughout the body and put the baby in danger. It might even cause premature labor.
Very weak pelvic muscles can lead to POP. This painful condition can cause incontinence, pain during sex, and changes in the appearance of the genitals.
Some women experience muscle injuries during pregnancy or when giving birth. The hormone relaxin may increase the risk of muscle injuries. So it is important to remain physically active to keep the muscles strong. Always lift with the legs rather than the back, and see a doctor for unexplained muscle pain.
Any injury that a woman experiences during pregnancy can make childbirth more difficult. Pregnancy-related complications may also make the postpartum period more difficult, slowing recovery and potentially harming mental health.
Women should see their doctors or midwives routinely during pregnancy. It is vital to use these visits to discuss all symptoms, even if they seem minor.
Early in pregnancy, women may only see a doctor every few weeks. If they are experiencing intense pressure or pain or have other symptoms, such as fever, painful urination, bleeding, or a change in the baby’s movements, it is important that they seek medical care immediately.
If they are experiencing intense pressure or pain or have other symptoms, such as fever, painful urination, bleeding, or a change in the baby’s movements, it is important that they seek medical care immediately.
If it is after hours, they should go to the emergency room. Prompt treatment of pregnancy conditions can save both the woman and the baby.
Vaginal pressure during pregnancy is just one of the many symptoms women may experience while pregnant. It should not usually be cause for concern and can be a good sign that the body is releasing the right hormones, and the uterus is growing as expected.
A bit of caution in pregnancy can help to detect problems before they become emergencies. Never hesitate to see a doctor, even if the issue seems minor. It is unlikely that there is a severe problem, but reassurance can make pregnancy easier. If something is wrong, it is best to catch the issue as early on as possible.
Read the article in Spanish.
how to do it right, benefits, effectiveness, contraindications
The author of the technique to help strengthen the muscles of the pelvic floor is Arnold Kegel, a professor of gynecology and sexologist from the USA. Kegel exercises for women during pregnancy will help you learn how to control intimate muscles (useful during labor) and help reduce the risk of tears in the perineum. The muscles of the pelvic floor during pregnancy lose their elasticity due to the constant pressure on them from the enlarged uterus. Simple, but at the same time effective muscle training will help restore their elasticity and tone.
Kegel exercises for women during pregnancy will help you learn how to control intimate muscles (useful during labor) and help reduce the risk of tears in the perineum. The muscles of the pelvic floor during pregnancy lose their elasticity due to the constant pressure on them from the enlarged uterus. Simple, but at the same time effective muscle training will help restore their elasticity and tone.
The main thing is to correctly identify the right muscles and remember how to do the exercises. Finding muscles is not difficult - during the next visit to the toilet, you need to abruptly stop urination, and then alternately squeeze and relax the muscles found in this way several times, not including the muscles of the press, buttocks, legs in the process. If it works, you can start charging.
Benefits and harms of intimate gymnastics
Regularly performing each Kegel exercise for women before childbirth, you can get the following results in a month:
- flabby pelvic muscles become toned;
- general well-being improves;
- will manage to control the muscles during childbirth;
- reduces the level of pain during natural childbirth;
- reduces the risk of complications, ruptures.

The advantage of this workout is that you can do it anytime, anywhere - at home, at work or on public transport. Gymnastics does not require special training and has no age restrictions, but there are still some contraindications that those who are expecting a baby should be aware of. Below we will describe how to perform the Kegel exercise for pregnant women correctly so as not to harm yourself or your unborn baby.
Contraindications
Before a pregnant woman incorporates any additional physical activity into her daily routine, it is recommended to consult a gynecologist. The doctor will assess the condition of the mother and fetus and tell you if it is possible to train. There are restrictions under which Kegel gymnastics is completely excluded or adjusted according to the exercises so as not to harm yourself and the fetus, but to strengthen the muscles. Limitations are the threat of premature birth and miscarriage.
After the 16th week of pregnancy, gymnastics should not be performed in the supine position in order to eliminate pressure on the inferior vena cava.
In addition to the threat of premature birth and miscarriage, Kegel exercises for women during pregnancy are prohibited with severe toxicosis, uterine bleeding, and diseases accompanied by a feverish state. It is advisable to discuss all innovations in the daily routine and diet in advance with your doctor. He is responsible for the condition of the mother and child, has sufficient experience and knowledge to make informed decisions.
The doctor will determine which Kegel exercises are acceptable and which ones should be avoided. Even in the case of a calm pregnancy without any pathologies, you should not practice in a lying position, only sitting or standing.
Powerful 4-piece set
It is convenient to study yoga classes from a video, but this will not work with Kegel gymnastics - you will have to carefully read the description of the exercise and perform it as accurately as possible. In addition to the starting position of standing and sitting, pelvic exercises during pregnancy can be performed on all fours. You need to start with 3-5 repetitions, eventually bringing the number of repetitions of each element to 20-30.
You need to start with 3-5 repetitions, eventually bringing the number of repetitions of each element to 20-30.
Among the large number of exercise options for pregnant women, 4 main elements are suitable:
- Sit comfortably. Bend your legs and slightly spread apart. Tighten the muscles of the perineum for 5-10 seconds, relax. Repeat 3-5 times.
- Imagine the vagina as an elevator shaft, where the entrance is the lower floor, the cervix is the upper one. The task is to smoothly contract the muscles from the bottom up, lingering for 2-3 seconds on each imaginary floor. “Having risen to the last floor”, you gradually need to “go down”, relaxing the muscles in turn on each “floor”. At first, performing such a pelvic floor exercise for pregnant women will seem difficult, but with each workout it will become easier.
- In addition to the vaginal muscles, the muscles of the anus are involved. The exercise is performed at a fast pace. Squeeze the vagina, then the anus, then relax the muscles in reverse order.

- Attention! Before performing the Kegel exercise for pregnant women, you need to empty your bladder and intestines. Take a comfortable posture. Hold your breath, gently and smoothly push, as during a bowel movement, but not with the anus, but with the vagina. To assess the correctness of the exercise, put your hand on the perineum. If you feel the pressure of the muscles of the vagina, then everything is correct. After relaxing, repeat the task. The exercise will teach you to control the muscles that are needed for effective attempts during labor.
The right approach: what are the nuances to consider
If you are going to perform Kegel exercises during the 1st, 2nd and 3rd trimesters, you must adhere to the following recommendations:
- take a comfortable position, so that nothing presses or causes pain;
- breathe calmly and measuredly;
- strain only the necessary muscles so as not to harm the child and yourself;
- do not be zealous, unnecessary fatigue is useless;
- practice daily;
- If you experience discomfort, stop exercising and consult a doctor.
It is advisable to start gymnastics early, performing 20-30 contractions every day. The goal of training is to feel and control the work of the muscles. It may be difficult at first, but over time, the muscles will be easy to control. The load should be increased gradually.
Kegel exercises are useful not only for strengthening the muscles of the vagina, they help control the anal muscles, tone the muscles of the small pelvis. The main condition for success is to regularly perform the training complex, and then the result from daily exercises will be felt after a couple of weeks.
Kegel exercises, like other exercises, help strengthen muscles. The muscles that are strengthened with Kegel exercises are located in the lower part of the pelvic region and are responsible for the correct positioning of the pelvic organs and also regulate urination. And this is very important for pregnant women. Due to the increase in the size of the uterus and the weight of the growing baby, this area of the body is under a lot of pressure, which can sometimes lead to urinary incontinence and other problems.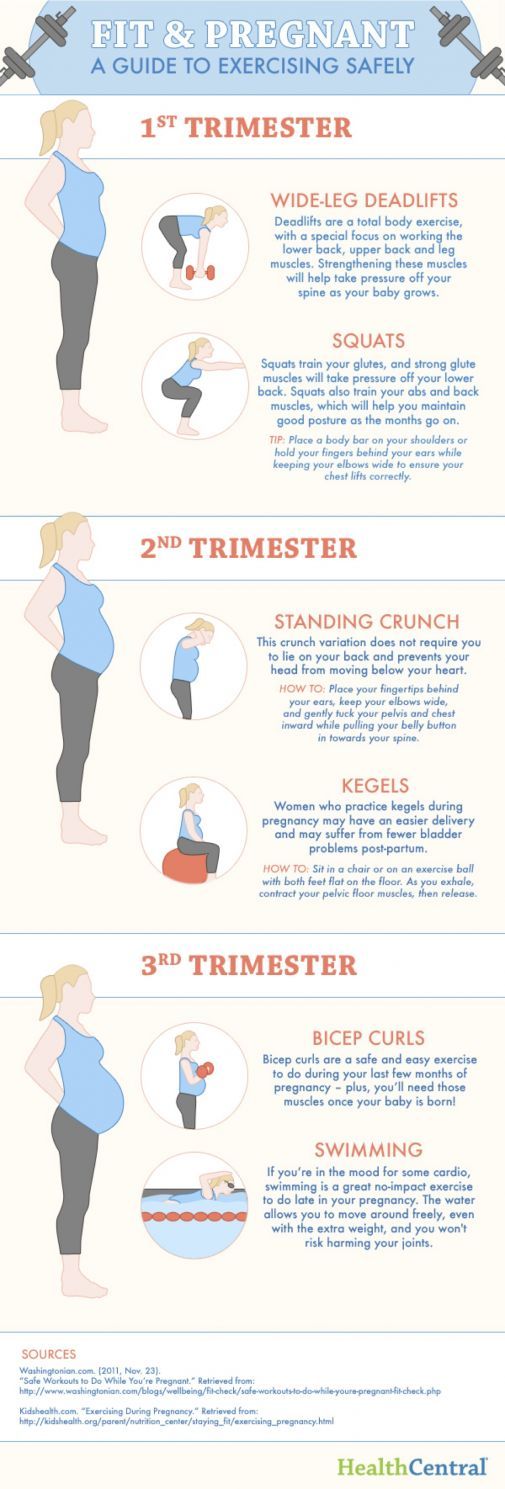 To do Kegel exercises, you need to find the right muscles, and then train them.
To do Kegel exercises, you need to find the right muscles, and then train them.
Method 1 of 3: Identifying the “right” muscles
1. Try to contract your pelvic floor muscles while urinating. If you squeeze the right muscles, it will stop urination. If you succeeded, you have identified the muscles that need to be activated by doing Kegel exercises.
2. Try to hold back gases. The muscles that are used to expel gas are the muscles you are trying to identify. If you can tense these muscles to keep from gassing, you've found the right muscles.
3. Try to find these muscles with your fingers. If you're not sure you're squeezing the right muscles, try finding them with your fingers. For this:
Wash your hands and put your finger in your vagina. If you feel pressure around him as you try to squeeze your pelvic muscles, you are squeezing the right muscles.
4. Identify these muscles while making love. Try to tighten these muscles when you have sex with your partner. Ask him if he felt pressure around his penis when you tightened the muscles.
Identify these muscles while making love. Try to tighten these muscles when you have sex with your partner. Ask him if he felt pressure around his penis when you tightened the muscles.
If he feels it, you are squeezing the right muscles.
5. Check with your doctor. If you're not sure which muscles you should be training, don't hesitate to contact your doctor to see if you're doing everything right.
Your doctor may also give you some advice regarding these exercises.
Method 2 of 3: Kegel Exercises
1. Empty your bladder before you start exercising. While you may have identified your pelvic floor muscles while urinating, it's not a good idea to practice Kegel exercises while urinating. This is because holding on to urine can lead to unnecessary infections. To avoid infections, always empty your bladder before exercising.
2. Take a comfortable position.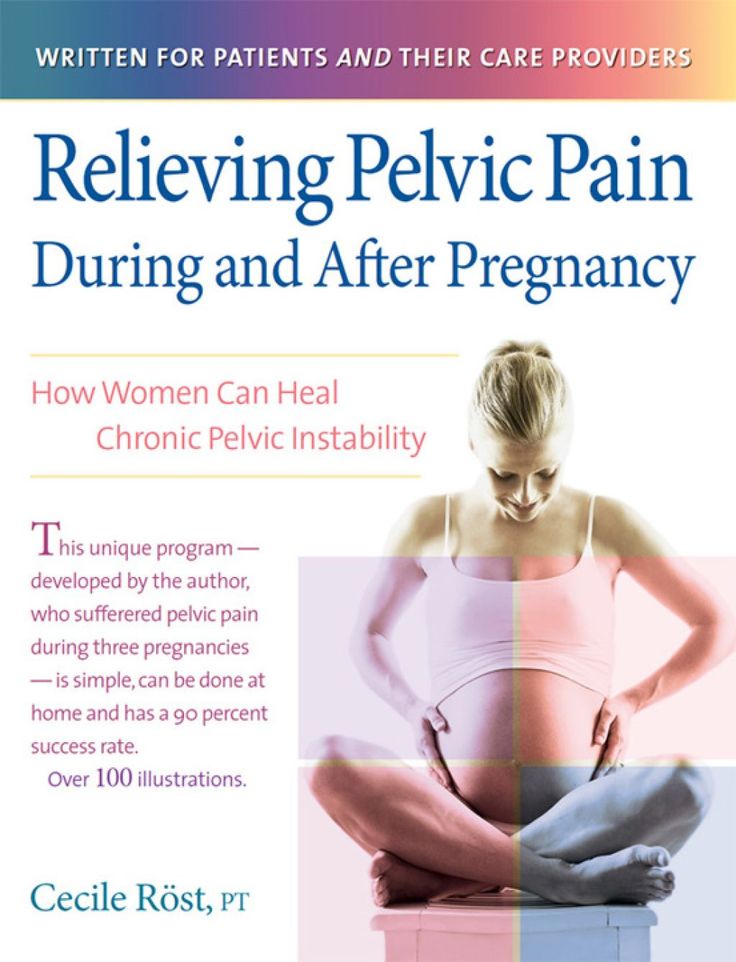 Kegel exercises are so easy that you can do them in any position and even during pregnancy. In addition, no one will know that you are doing the exercises. Find the position that suits you best.
Kegel exercises are so easy that you can do them in any position and even during pregnancy. In addition, no one will know that you are doing the exercises. Find the position that suits you best.
Lie down, sit down or stand up. The only thing you should keep in mind is that you should not put pressure on your stomach while doing these exercises.
3. Contract your pelvic floor muscles and hold for three to four seconds. Then relax your muscles. Let them rest for a few seconds, then squeeze them again. It's a good idea to start with three or four seconds.
When it is not so difficult for you to do this exercise, you can increase the time to five seconds.
Repeat this procedure 10 times.
4. Do Kegel exercises three times a day. As mentioned earlier, you can do them anytime, like when you're watching your favorite TV show or standing in line at the grocery store.
Doing these exercises 50 times a day is usually enough to strengthen your pelvic floor muscles.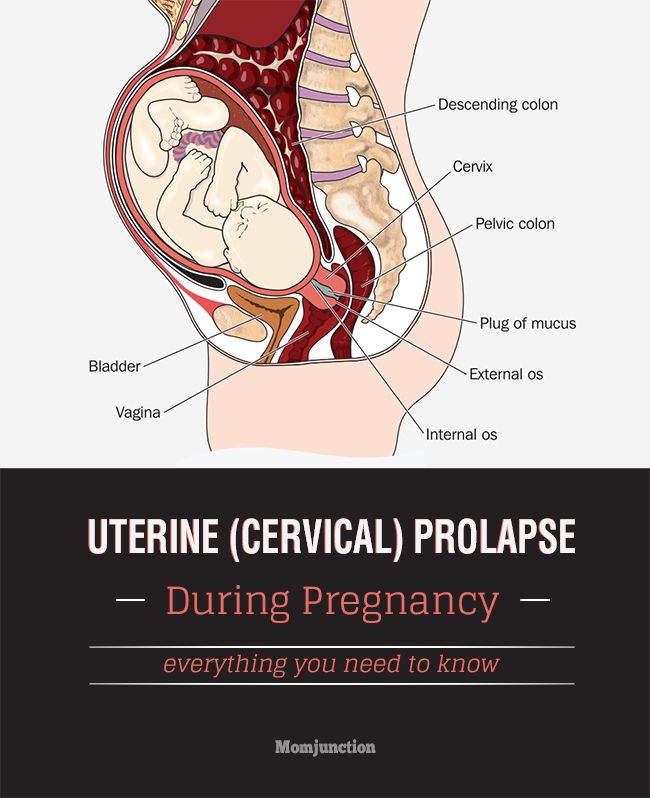 [1]
[1]
5. Try not to pull in your stomach. If you pull in your abdominal muscles while doing Kegel exercises, you won't get the same results when you just squeeze your pelvic floor muscles. To make sure you don't pull in your abdominal muscles:
Place your hand on your stomach and tighten your pelvic floor muscles. If your stomach is shrinking, you need to pay more attention to holding it when you do these exercises.
6. Don't move your feet. Kegel exercises do not require you to move and tense your leg muscles. If you are doing this, you are not doing the exercise correctly and you should consult someone, such as a doctor, who can help you identify the muscles that are involved in Kegel exercises.
7. Try not to hold your breath. Kegel exercises are not meant to be strenuous and you should not hold your breath during the exercises. If you have trouble breathing when you do these exercises, or if you can't help but hold your breath, talk to your doctor to help you do the exercises correctly.
8. Do these exercises throughout your pregnancy. This will help you hold on to urine even if your child is pressing on the bladder. In addition to this, strong pelvic floor muscles will help you during childbirth. They can help:
- Push during childbirth.
- Avoid tissue rupture during childbirth.
Method 3 of 3: Understanding Kegel Exercises
1. Learn about the benefits of Kegel exercises. As your baby begins to grow in your uterus, your enlarged uterus may press on your bladder, making it difficult for you to control your urination. Kegel exercises can help you control your urination. They can also help:
Prevent fecal incontinence.
Make you stronger in childbirth.
Increase blood circulation, which can help prevent hemorrhoids, which happen quite often during pregnancy.
Accelerate the recovery process after pregnancy.
2. Find out when is the best time to start doing these exercises. It is generally recommended that women start doing Kegel exercises in the first trimester of pregnancy. This gives a woman more time to strengthen her pelvic floor muscles before they are put under pressure by the baby's weight and other factors that come along at the end of pregnancy. Starting to train your muscles early gives you enough time to perfect your exercises to the point where they become natural, something you don't even have to think about when you're under the emotional and physical stress of late pregnancy.
Find out when is the best time to start doing these exercises. It is generally recommended that women start doing Kegel exercises in the first trimester of pregnancy. This gives a woman more time to strengthen her pelvic floor muscles before they are put under pressure by the baby's weight and other factors that come along at the end of pregnancy. Starting to train your muscles early gives you enough time to perfect your exercises to the point where they become natural, something you don't even have to think about when you're under the emotional and physical stress of late pregnancy.
3. Do not stop exercising after pregnancy and childbirth. As soon as you recover from childbirth, you can start doing the exercises again. Keep doing them all your life if you want. If you do these exercises, they will help prevent uncontrolled urination due to sneezing, coughing, laughing, as well as fecal incontinence and hemorrhoids.
TIP
Kegel exercises can significantly improve the quality of sex and prevent organ prolapse through the vaginal canal, which occurs in older women.
The source of information
Pelvic floor exercises - second youth
In various women's magazines, a lot of attention is paid to diets, hair condition, face and body skin care, body shaping problems, invasive and minimally invasive plastic surgery techniques to change the shape of the ears, eyes, mammary glands, lifting and the right lifestyle. And at the same time, there are very few publications on the problem of pelvic floor muscle failure, vaginal wall prolapse, genital prolapse and urinary incontinence during exercise.
And this problem is global, because at least 40% of all women suffer from this disease.
Causes and symptoms of pathology
The very first symptoms of the disease are the gaping of the genital slit when the hips are bred at rest or when straining (straining). With the continued progression of the process, there is a slow (over several years) descent of the walls of the vagina and cervix into the formed perineal defect (i. e. through the gaping vagina). In this case, there may be a sensation of some kind of foreign body in the perineum, pulling pains in the lower abdomen and in the lower back.
e. through the gaping vagina). In this case, there may be a sensation of some kind of foreign body in the perineum, pulling pains in the lower abdomen and in the lower back.
In addition, sexual discomfort arises, that is, a woman and a man stop feeling each other the way they did during their youth. This can lead to a feeling of sexual dissatisfaction that loving spouses hide from each other. The consequences of latent dissatisfaction during sexual intercourse can be infidelity of spouses and even divorces, for which, of course, other reasons are put forward.
With further progression of genital prolapse (as scientists call this disease), first a partial, and then a complete prolapse of the uterus and vaginal walls outside the genital slit occurs. In this case, sexual life becomes completely impossible, there are violations of the functions of adjacent pelvic organs - the bladder and rectum, manifested in difficulty urinating or urinary incontinence, impaired defecation, intestinal gas incontinence.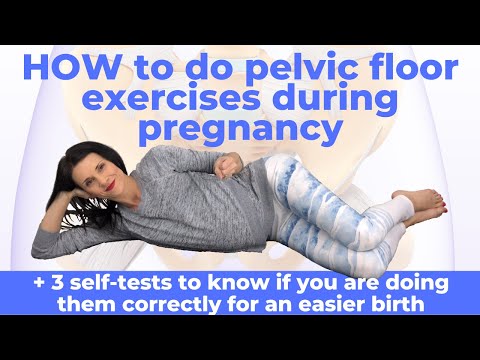
The most common cause of genital prolapse is childbirth. It can be one birth, but rapid, it can be a birth with a large fetus, repeated births, or births in which there were ruptures or a perineal dissection was performed with its subsequent restoration (i.e., suturing). Even when the doctor tells you that there were no ruptures in childbirth, or they were minimal and it was necessary to put 1, 2 sutures on the vaginal mucosa, there may be internal ruptures of the muscles and fascia of the pelvic floor, which subsequently lead to prolapse and prolapse of the genital organs .
What else does the gaping of the genital slit lead to, except for the prolapse of the genital organs, sexual problems and dysfunctions of adjacent organs? Many authors have proven that this pathology often causes inflammatory diseases of the vagina (colpitis, vaginitis), diseases of the cervix (cervicitis, ectopia), which are difficult to treat, due to a violation of the normal biocenosis of the vagina.
Why does the pathology progress before menopause?
With similar problems, women mostly of perimenopausal age turn to doctors. Why is this happening? We have already said that prolapse progresses slowly over 10-15 years. In the initial stages, its development is restrained by estrogenic effects on the muscles and mucous membranes of the pelvic floor. Women at a young age are sexually active, go in for sports, fitness, and this, to a certain extent, is a prevention of the progression of the disease.
In perimenopausal and postmenopausal age, the overall tone of all muscles decreases, including the muscles of the perineum, the stimulating effect of estrogens ceases, and this quickly leads to the progression of the disease. It is at this time that many women notice urine leakage when coughing, laughing, or exercising. Bladder dysfunction often accompanies prolapse and prolapse of the genital organs. What to do in such a situation? How to protect yourself from this disease? Don't give birth? Of course, it is possible and necessary to give birth, but it is necessary to know about the possible consequences of childbirth through the birth canal, how to prevent gaps in childbirth, how to strengthen and train the muscles of the perineum.
Kegel exercises
As a result of training the muscles of the perineum, the blood supply and tone of the muscular-ligamentous apparatus improves. Pelvic floor muscle training in the postpartum period is effective in reducing the risk of early genital prolapse and stress urinary incontinence. The mistake of most women is that they primarily seek to restore the figure in the postpartum period - "remove" the stomach, loading the abdominal muscles. At the same time, they forget or do not know that strengthening the press should be preceded by exercises that strengthen the muscles of the perineum. An increase in intra-abdominal pressure with a decrease in the tone of the pelvic floor muscles ultimately exacerbates the failure of the perineal muscles.
Exercises that strengthen the muscles of the pelvic floor were first published by Kegel back in 1948. The essence of the exercises is that in a certain rhythm it is necessary to contract the muscles of the perineum, while simultaneously drawing in the anal sphincter and straining the buttocks.
Exercises must be performed in an anti-orthostatic position on the back, in the knee-elbow, stop-hand, stop-elbow position. Muscle contraction should occur on inhalation, and relaxation on exhalation. The duration of muscle tension is from 2 to 7 seconds, the number of repetitions is from 3 to 8. Harmful can be considered in the postpartum period - jumping, running, jerking movements, straining.
Effective for strengthening the muscles of the pelvis are vaginal simulators. They come in different forms (balls, olives), which are inserted into the vagina and the muscles of the perineum are held in it in a standing position with legs apart from 5 seconds to 1-2 minutes, the weight of the simulators gradually increases.
However, if prolapse nevertheless develops, which must be considered as a hernia of the pelvic floor, it is necessary to contact a gynecologist to perform a corrective operation. Even if it was the first birth, and repeated ones are planned in 4-7 years, you should not walk with perineal insufficiency, experience sexual discomfort and constantly be treated for inflammatory diseases.