Infant rash cheeks
Rash on a baby's face: Pictures, causes, and treatments
In babies, most facial rashes are harmless and tend to clear up without treatment. Causes can include eczema, acne, and infection.
Sometimes, however, a rash on a baby’s face can indicate a more serious condition.
Being able to distinguish between different rashes can help a parent or caregiver know when to seek professional advice.
In this article, we describe common facial rashes in babies, treatments, and when to see a doctor.
Eczema refers to a group of conditions that cause the skin to become rough, irritated, itchy, and inflamed.
These conditions are common in young children, often appearing between the ages of 6 months and 5 years. Many children grow out of their eczema.
According to the National Eczema Association in the United States, if eczema develops within the first 6 months of life, it tends to appear on the cheeks, chin, forehead, or scalp. The rash will be dry, red, and itchy.
Between the ages of 6 and 12 months, eczema may develop in other parts of the body. The elbows and knees are particularly susceptible when babies start to crawl.
Treatment
Although the exact cause of eczema is unknown, experts believe that both genetic and environmental factors can play a role.
Certain environmental triggers may over-activate the immune system, causing inflammation and skin irritation.
When trying to establish the cause of a child’s eczema, it may help to keep a diary of symptoms and potential triggers. By avoiding these triggers, it may be possible to prevent flare-ups of symptoms.
Below are some common triggers of eczema in babies:
- heat and sweating
- dry skin
- irritants, such as soaps, washing detergents, and cigarette smoke
- allergens, such as dust mites, pollen, and pet dander
- certain fabrics, such as wool and nylon
Treatments for eczema include:
- over-the-counter (OTC) moisturizers
- prescription creams and ointments, such as steroid creams
- immunosuppressant drugs
- phototherapy
A doctor can consult with a pediatric dermatologist and recommend a course of treatment. They can also advise about triggers and how to avoid them.
They can also advise about triggers and how to avoid them.
Check that over-the-counter treatments are suitable for infants.
Seborrheic dermatitis causes a rash to develop on areas of skin that contain many oil-producing glands.
In babies, the rash mainly appears on the scalp, and people commonly refer to it as cradle cap. However, cradle cap can also affect the cheeks, particularly around the eyes and nose.
The rash may have the following characteristics:
- redness and inflammation
- an oily or greasy appearance
- white or yellow scaly or crusty patches
Treatment
Cradle cap is generally harmless and usually disappears between 6 and 12 months of age.
If the child is not experiencing any discomfort, treatment may not be necessary.
For mild symptoms, OTC medications, such as antifungal creams and medicated shampoos, may help to relieve discomfort and speed healing. However, talk to a doctor before using these products on an infant.
If the rash is scaly, applying mineral oil or petroleum jelly to the baby’s scalp 1 hour before using an anti-dandruff shampoo can help loosen and remove the scales.
For babies with more severe symptoms, a doctor may prescribe topical steroids to reduce inflammation.
Particularly severe cradle cap can increase the risk of infection. See a doctor immediately, if the baby’s skin:
- feels hot
- oozes fluid
- gives off an unpleasant odor
Around 40–50 percent of healthy newborns develop milia, which are tiny white or yellow bumps about 1–3 mm in size.
Milia result from blocked pores and typically develop on the face, often around the eye and nose. The bumps can appear in large numbers, and usually a roughly equal number form on each side of the face.
In babies, milia can also develop in the mouth. In this case, the medical name is Epstein pearls.
Treatment
Milia tends to clear up on their own within a few weeks, once the pores open up.
No treatment is usually necessary. Avoid using creams and ointments on the baby’s skin, as these can further clog the pores and lead to more milia.
Newborn, or neonatal, acne causes small, red pimples to develop, usually around 2–6 weeks of age. However, some babies are born with them.
The medical term for acne that develops between 6 weeks and 6 months of age infantile acne, and we discuss this below.
Neonatal acne affects around 20 percent of newborns, according to the American Academy of Dermatology.
The pimples tend to develop on the baby’s cheeks and nose, but breakouts can also appear on the:
- forehead
- chin
- scalp
- neck
- chest
- upper back
Treatment
Generally, newborn acne is not a cause for concern. It is unlikely to cause scarring and tends to clear up without treatment after a few weeks or months.
Parents and caregivers should:
- gently wash the baby’s skin with lukewarm water
- avoid scrubbing affected areas
- avoid oily or greasy skincare products
- seek advice from the child’s doctor before using acne medicines or cleansing products
Infantile acne develops in babies older than 6 weeks. It typically appears between 3 and 6 months of age.
It typically appears between 3 and 6 months of age.
Infantile acne is less common than newborn acne. Symptoms can be more severe and may require treatment.
Before treating infantile acne, it is important to rule out other conditions, such as such as eczema and infections, which are more common in this age group.
Treatment
Infantile acne usually clears up within 6–12 months after it first appears.
After diagnosis, a dermatologist can advise about treating the acne and preventing scarring. If they suspect that the acne results from an underlying medical condition, they may consult a specialist.
A doctor can diagnose the cause of a rash.
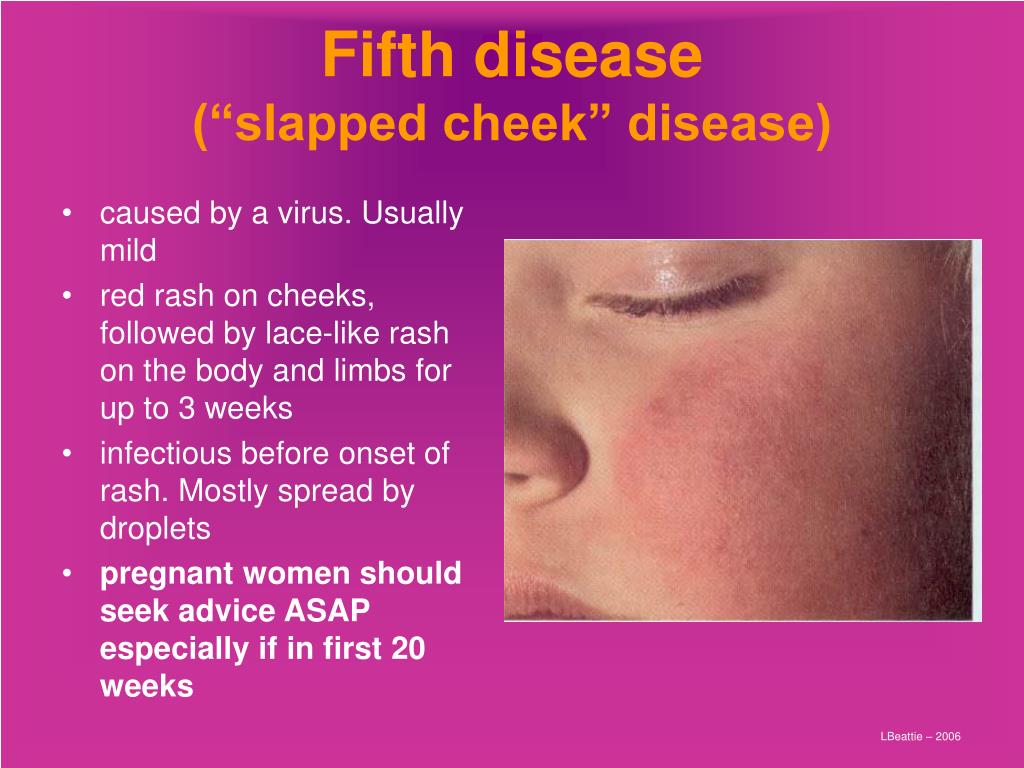
Slapped cheek syndrome is a viral infection. Anyone can get it, but it most commonly develops in school-aged children.
Other names for the syndrome include fifth disease and erythema infectiosum. It results from infection with the B19 parvovirus.
The defining characteristic is a bright red rash on one or both cheeks. The rash is not usually painful. It typically appears within 4–14 days of infection.
The rash is not usually painful. It typically appears within 4–14 days of infection.
The cheek rash often disappears in a few days, but another rash may develop on areas such as the chest, arms, and legs. This rash usually lasts for 7–10 days, but it may come and go.
The rash on the body is usually blotchy and light in color. It can be itchy, but it is not typically painful.
Slapped cheek syndrome can also cause the following symptoms:
- a fever of 38°C or higher
- a headache
- a runny nose
- a sore throat
Children can initially pass the infection to other children, but it usually stops being contagious once the rash appears.
Treatment
The symptoms of slapped cheek syndrome are usually mild, and the underlying infection typically clears up without treatment.
OTC medications, such as acetaminophen and ibuprofen, can help relieve any discomfort. However, speak to a doctor before giving these drugs to babies or young children.
Never give a child aspirin, as it may increase the risk of a serious condition called Reye’s syndrome.
Most rashes on babies’ faces are harmless. They usually clear up on their own.
However, a rash in this area can indicate an infection or an underlying health condition.
See a doctor if the rash is severe, or if the baby has:
- fluid-filled blisters
- a fever
- a loss of appetite
- red streaks extending from the rash
- tiny red or purple spots that do not fade when someone applies pressure
- swollen lymph nodes
- lethargy
- a cough
Facial rashes are common in babies and young children. The many possible causes include eczema, acne, and infection.
Most rashes clear up without treatment. However, see a doctor if a rash is severe or persistent, or if it accompanies other symptoms.
Read the article in Spanish.
Rash on a baby's face: Pictures, causes, and treatments
In babies, most facial rashes are harmless and tend to clear up without treatment. Causes can include eczema, acne, and infection.
Causes can include eczema, acne, and infection.
Sometimes, however, a rash on a baby’s face can indicate a more serious condition.
Being able to distinguish between different rashes can help a parent or caregiver know when to seek professional advice.
In this article, we describe common facial rashes in babies, treatments, and when to see a doctor.
Eczema refers to a group of conditions that cause the skin to become rough, irritated, itchy, and inflamed.
These conditions are common in young children, often appearing between the ages of 6 months and 5 years. Many children grow out of their eczema.
According to the National Eczema Association in the United States, if eczema develops within the first 6 months of life, it tends to appear on the cheeks, chin, forehead, or scalp. The rash will be dry, red, and itchy.
Between the ages of 6 and 12 months, eczema may develop in other parts of the body. The elbows and knees are particularly susceptible when babies start to crawl.
Treatment
Although the exact cause of eczema is unknown, experts believe that both genetic and environmental factors can play a role.
Certain environmental triggers may over-activate the immune system, causing inflammation and skin irritation.
When trying to establish the cause of a child’s eczema, it may help to keep a diary of symptoms and potential triggers. By avoiding these triggers, it may be possible to prevent flare-ups of symptoms.
Below are some common triggers of eczema in babies:
- heat and sweating
- dry skin
- irritants, such as soaps, washing detergents, and cigarette smoke
- allergens, such as dust mites, pollen, and pet dander
- certain fabrics, such as wool and nylon
Treatments for eczema include:
- over-the-counter (OTC) moisturizers
- prescription creams and ointments, such as steroid creams
- immunosuppressant drugs
- phototherapy
A doctor can consult with a pediatric dermatologist and recommend a course of treatment. They can also advise about triggers and how to avoid them.
They can also advise about triggers and how to avoid them.
Check that over-the-counter treatments are suitable for infants.
Seborrheic dermatitis causes a rash to develop on areas of skin that contain many oil-producing glands.
In babies, the rash mainly appears on the scalp, and people commonly refer to it as cradle cap. However, cradle cap can also affect the cheeks, particularly around the eyes and nose.
The rash may have the following characteristics:
- redness and inflammation
- an oily or greasy appearance
- white or yellow scaly or crusty patches
Treatment
Cradle cap is generally harmless and usually disappears between 6 and 12 months of age.
If the child is not experiencing any discomfort, treatment may not be necessary.
For mild symptoms, OTC medications, such as antifungal creams and medicated shampoos, may help to relieve discomfort and speed healing. However, talk to a doctor before using these products on an infant.
If the rash is scaly, applying mineral oil or petroleum jelly to the baby’s scalp 1 hour before using an anti-dandruff shampoo can help loosen and remove the scales.
For babies with more severe symptoms, a doctor may prescribe topical steroids to reduce inflammation.
Particularly severe cradle cap can increase the risk of infection. See a doctor immediately, if the baby’s skin:
- feels hot
- oozes fluid
- gives off an unpleasant odor
Around 40–50 percent of healthy newborns develop milia, which are tiny white or yellow bumps about 1–3 mm in size.
Milia result from blocked pores and typically develop on the face, often around the eye and nose. The bumps can appear in large numbers, and usually a roughly equal number form on each side of the face.
In babies, milia can also develop in the mouth. In this case, the medical name is Epstein pearls.
Treatment
Milia tends to clear up on their own within a few weeks, once the pores open up.
No treatment is usually necessary. Avoid using creams and ointments on the baby’s skin, as these can further clog the pores and lead to more milia.
Newborn, or neonatal, acne causes small, red pimples to develop, usually around 2–6 weeks of age. However, some babies are born with them.
The medical term for acne that develops between 6 weeks and 6 months of age infantile acne, and we discuss this below.
Neonatal acne affects around 20 percent of newborns, according to the American Academy of Dermatology.
The pimples tend to develop on the baby’s cheeks and nose, but breakouts can also appear on the:
- forehead
- chin
- scalp
- neck
- chest
- upper back
Treatment
Generally, newborn acne is not a cause for concern. It is unlikely to cause scarring and tends to clear up without treatment after a few weeks or months.
Parents and caregivers should:
- gently wash the baby’s skin with lukewarm water
- avoid scrubbing affected areas
- avoid oily or greasy skincare products
- seek advice from the child’s doctor before using acne medicines or cleansing products
Infantile acne develops in babies older than 6 weeks. It typically appears between 3 and 6 months of age.
Infantile acne is less common than newborn acne. Symptoms can be more severe and may require treatment.
Before treating infantile acne, it is important to rule out other conditions, such as such as eczema and infections, which are more common in this age group.
Treatment
Infantile acne usually clears up within 6–12 months after it first appears.
After diagnosis, a dermatologist can advise about treating the acne and preventing scarring. If they suspect that the acne results from an underlying medical condition, they may consult a specialist.
A doctor can diagnose the cause of a rash.
Slapped cheek syndrome is a viral infection. Anyone can get it, but it most commonly develops in school-aged children.
Other names for the syndrome include fifth disease and erythema infectiosum. It results from infection with the B19 parvovirus.
The defining characteristic is a bright red rash on one or both cheeks. The rash is not usually painful. It typically appears within 4–14 days of infection.
The rash is not usually painful. It typically appears within 4–14 days of infection.
The cheek rash often disappears in a few days, but another rash may develop on areas such as the chest, arms, and legs. This rash usually lasts for 7–10 days, but it may come and go.
The rash on the body is usually blotchy and light in color. It can be itchy, but it is not typically painful.
Slapped cheek syndrome can also cause the following symptoms:
- a fever of 38°C or higher
- a headache
- a runny nose
- a sore throat
Children can initially pass the infection to other children, but it usually stops being contagious once the rash appears.
Treatment
The symptoms of slapped cheek syndrome are usually mild, and the underlying infection typically clears up without treatment.
OTC medications, such as acetaminophen and ibuprofen, can help relieve any discomfort. However, speak to a doctor before giving these drugs to babies or young children.
Never give a child aspirin, as it may increase the risk of a serious condition called Reye’s syndrome.
Most rashes on babies’ faces are harmless. They usually clear up on their own.
However, a rash in this area can indicate an infection or an underlying health condition.
See a doctor if the rash is severe, or if the baby has:
- fluid-filled blisters
- a fever
- a loss of appetite
- red streaks extending from the rash
- tiny red or purple spots that do not fade when someone applies pressure
- swollen lymph nodes
- lethargy
- a cough
Facial rashes are common in babies and young children. The many possible causes include eczema, acne, and infection.
Most rashes clear up without treatment. However, see a doctor if a rash is severe or persistent, or if it accompanies other symptoms.
Read the article in Spanish.
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
Usually, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.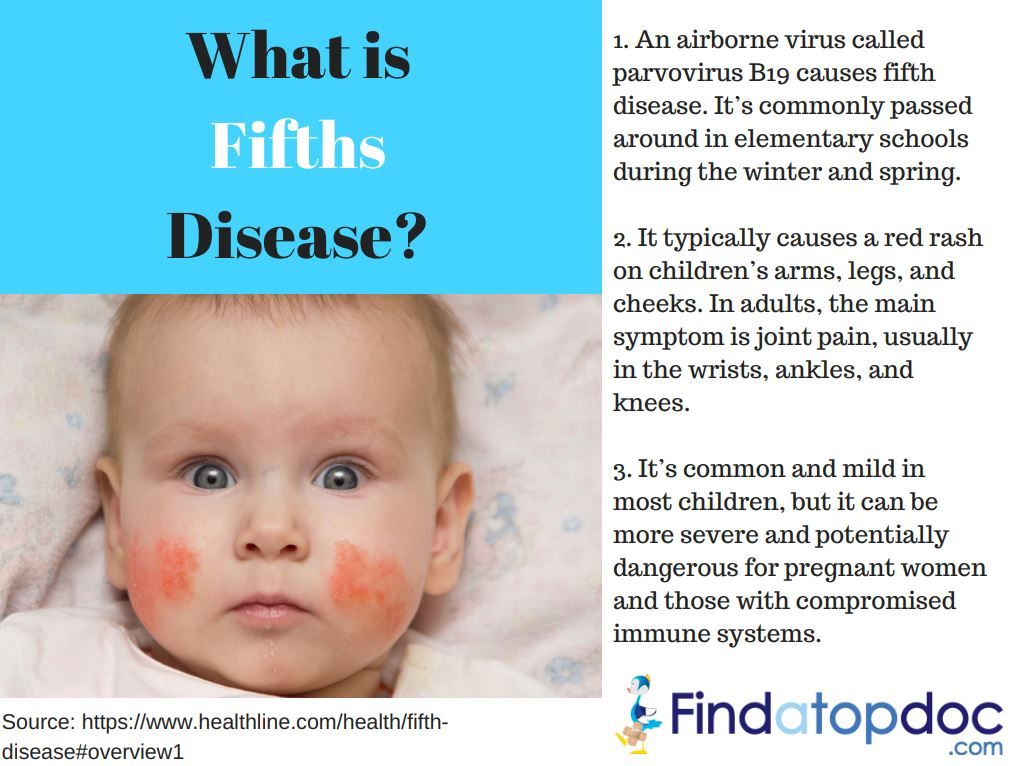
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc. ). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.
Author:
Eroshkina Maria Sergeevna
pediatrician
How to care for the skin of a newborn.
After discharge from the hospital, mother and baby gradually get used to the daily routine. The child should eat well and be warm - this is the first on the list. No less important is the care of the skin of the baby, which is very delicate and sensitive to external stimuli. To adapt to the new environment, the baby needs time and care of parents. Chemicals, fragrances, dyes in clothes, and detergents cause redness, diaper rash, or a rash. How to properly care for the skin of a newborn to protect the child from contact dermatitis, allergies, and other rashes?
Bathing
The baby is born with a protective coating. During this period, there is no need to bathe the baby or use baby lotions and creams.
A full bath is normal from the first days of a baby's life, the main thing is to follow the rules:
- bathe your baby in a warm room.
- water should be at body temperature: 36-37 degrees to the touch.
- make sure that the necessary items for the procedure are within reach. - remove jewelry that can scratch the child.
- hold the newborn firmly by lifting his head above the water.
- do not use cotton swabs to clean the nose and ears.
- to wash the baby's face, use water without soap.
- never leave a child unattended while bathing, even for a moment.
- For the first 2-3 months after birth, give up shampoo and soap, which can cause an allergic reaction in the baby.
- if you do use baby bath products, make sure they are soft, suitable for babies and odorless.
- then carefully wrap the baby in a cotton towel or a special corner robe for newborns.
- the room in which the baby will be after the bath should be warm, and air conditioners and fans should be turned off to prevent colds.
Umbilical Cord Care
By the time of discharge from the hospital, this organ, which connected mother and baby during all 9 months of pregnancy, will begin to dry out. Gradually, the umbilical cord atrophies and falls off within 1-2 weeks. Until then, the place of its attachment to the belly of the newborn must be kept clean and dry. All you need is plain water. You can not pull the keratinized part, even if it begins to fall off. The process will end by itself. To protect your baby's delicate skin, buy diapers for newborns that have a notch in the waistband for the unhealed navel. If you are using regular diapers, fold the edge so that the fabric does not rub against the tummy. In some cases, the child may need a doctor. Contact your pediatrician if your child has a fever of 38°C or more along with changes in the navel: the area is red and swollen; oozing yellow pus; there is an unpleasant smell. Many mothers are worried about the appearance of small specks of blood on the baby's undershirt or diaper, the child's bed. A little bleeding is normal.
A little bleeding is normal.
Diapers and diapers
Change diapers more often as soon as you notice that they are wet or dirty. If left for too long, it can cause infections. For newborn hygiene, thoroughly clean the genital area after every diaper change. Wash your baby under warm, running water to prevent irritation. Allow a few minutes for the skin to air dry, or gently pat dry with a soft towel. Use baby wipes less often to care for your newborn's skin. Perfume and alcohol in them can cause irritation, cause a rash. Make sure you buy diapers in a size that fits your baby. If the baby's skin in the diaper area is irritated, choose a different brand or stop using them for a while. . Wash reusable diapers and diapers with a mild, unscented detergent or clean, hot water. Most diaper rashes on a newborn's skin are not dangerous, but some can be a sign of an infection and need to be looked after. If the baby's skin is very reddened, itchy, or causes pain, contact your pediatrician immediately.
What to do in case of skin problems
In the first months after birth, the baby may develop a rash, irritation, diaper rash, which seem unusual to parents.
Most of the newborn skin problems do not need treatment:
- baby pimples - a small red rash on the face. As a rule, it disappears over time without intervention.
- milia are tiny whiteheads on a child's face.
- erythema is a common patchy rash that can affect newborns. Some appear as yellow or white bumps surrounded by a red halo. The rash tends to migrate to different parts of the body. It is most common on the second day of life, but may appear at birth or within the first two weeks. There is no cure - erythema gradually disappears on its own.
Eczema
This rash appears as red bumps that may fester. It usually appears on the forehead, cheeks, or scalp, and sometimes spreads to other parts of the body. The risk group includes infants who suffer from allergies from birth or have a genetic predisposition to the disease. In case of pathology, it is recommended to use special moisturizers: ointments, creams, oils. Do not bathe the baby for a long time with this disease. When an allergic rash appears, a consultation with a pediatrician is required.
The risk group includes infants who suffer from allergies from birth or have a genetic predisposition to the disease. In case of pathology, it is recommended to use special moisturizers: ointments, creams, oils. Do not bathe the baby for a long time with this disease. When an allergic rash appears, a consultation with a pediatrician is required.
Diaper rash
Causes:
- late diaper change. Urine or stool in a diaper irritates a newborn's skin, causing red weeping spots.
- bacterial or yeast infection. Taking antibiotics can cause the growth of fungi of the genus Candida. It usually appears around the genitals and buttocks of an infant. It looks like red spots with a whitish coating.
How to properly care for your skin to prevent diaper rash:
- do not use reusable diapers frequently.
- give up talcum powder: it dries the skin of a newborn very much.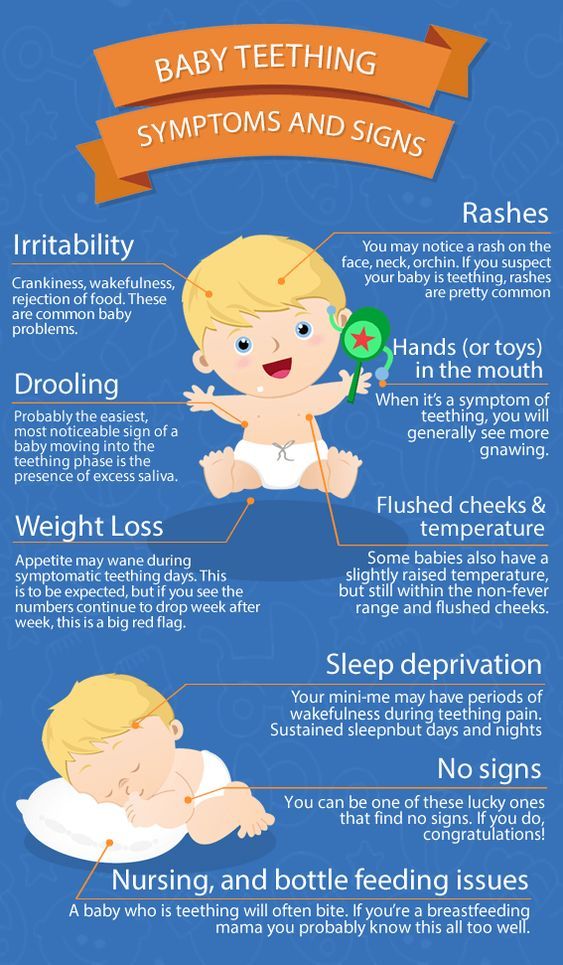
- air baths for half an hour.
Prickly heat
Heat rash is caused by overheating of the body. It is usually visible in the folds of the baby's skin. Hot, humid weather is a favorable time for prickly heat. To avoid rashes, keep your newborn cool by dressing him in loose cotton clothing.
Contact dermatitis
This disease develops when an infant's skin comes into contact with an irritant. The rash appears at the points of contact with the allergen: metal latches on T-shirts; dyes in clothes; washing powder; inappropriate soap, shampoo; allergic to the oil used. Parents need to trace, after which rashes appear, and eliminate the irritant. To bathe the baby, you need to use shampoo and soap that do not cause allergies in the newborn; iron baby clothes before putting them on. For washing, special powders or gels are used that do not contain fragrances and dyes, the child's clothes, bed linen and blankets are washed separately from the family's wardrobe items.