How to relieve engorged breast when not breastfeeding
Breast Engorgement After Stopping Breast-Feeding Suddenly
Written by WebMD Editorial Contributors
In this Article
- What Is Engorgement?
- Breast Engorgement Symptoms
- Breast Engorgement Causes
- Breast Engorgement Treatment and Home Remedies
- Breast Engorgement Prevention
- If You’re Formula Feeding
What Is Engorgement?
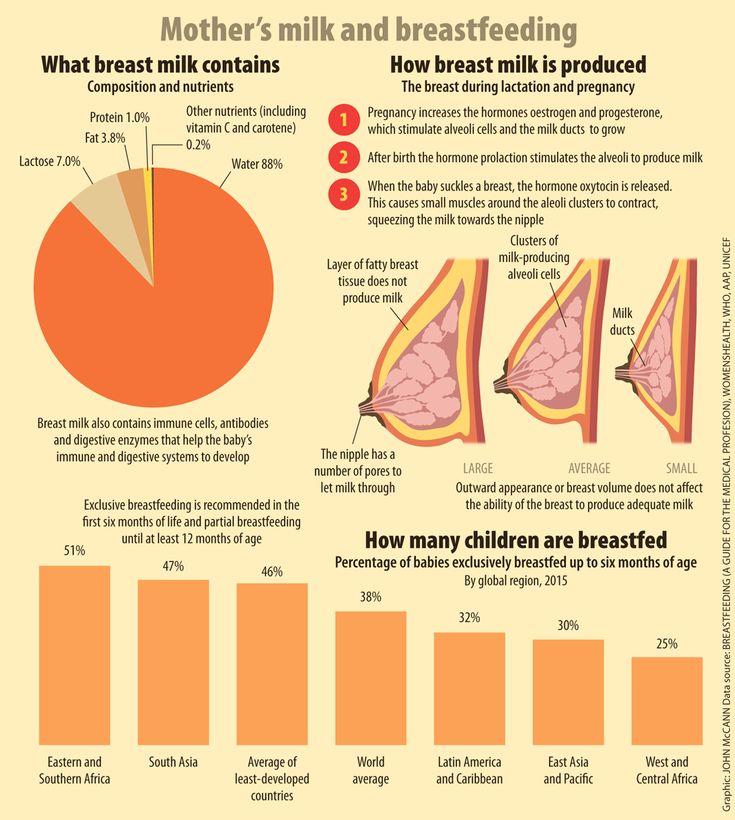
Breast engorgement means that your breasts are filled with too much milk. It can make them feel swollen, warm, and tender. It’s normal before you start breastfeeding and can mild or more intense.
After you deliver a baby, your body is still hard at work. Two of its new missions: helping you heal and getting food to your newborn.
In the hours and days following labor, circulation to your breasts increases. At first, they produce a thick, yellowish fluid called colostrum. It's full of protein and everything your baby needs to build a strong digestive system and stay healthy.
Three to 4 days after labor, your body makes milk all the time and stores it in your breast tissue. The first time your milk comes in, your breasts can become engorged, or filled with too much milk.
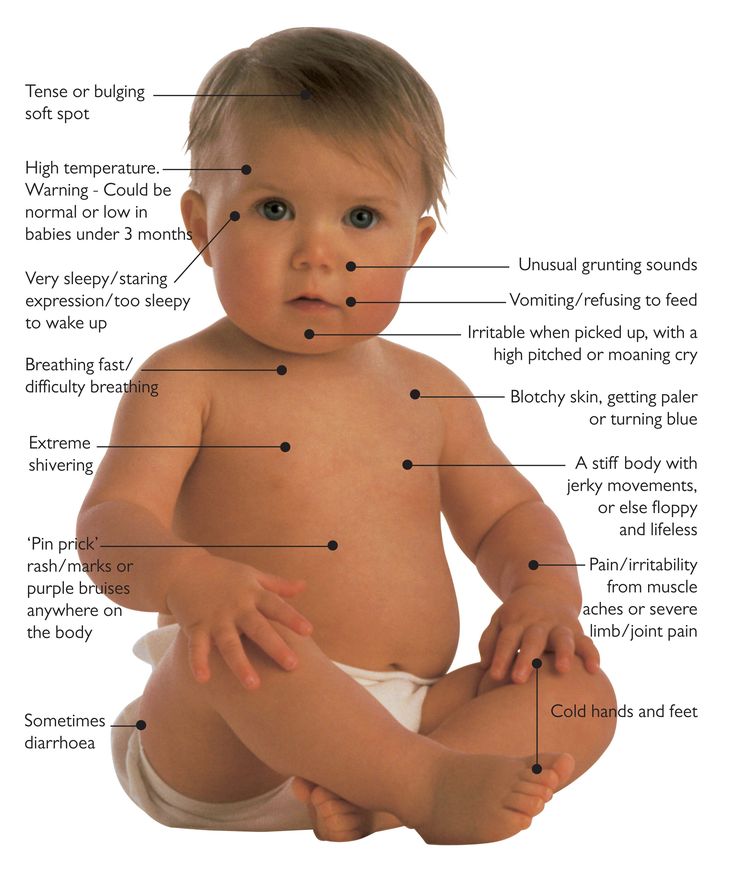
Breast Engorgement Symptoms
If your breasts are engorged, they may feel:
- Warm
- Heavy
- Tender and painful
- Swollen, which may extend to the armpit
- Hard
- Trouble for your baby to latch onto
You may also have lumps or flattened nipples.
- There’s a chance that engorgement could block milk ducts and lead to a breast infection if it’s severe.
Breast Engorgement Causes
Your breasts may naturally become engorged soon after you give birth as your milk comes in. It can also happen if you aren’t able to breastfeed or pump often enough.
Breastfeeding has many benefits for mother and baby alike. But it isn’t always easy. It may take your body a while to get used to it. And for some women, it might not work out.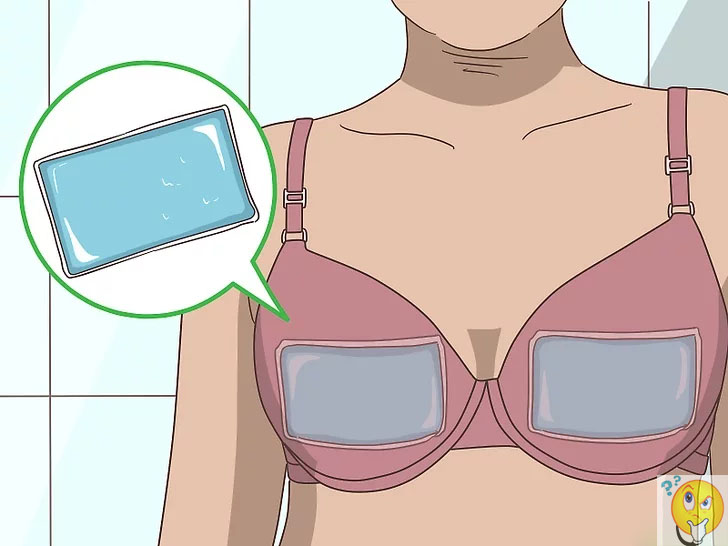 A lactation consultant or your doctor can help you get started.
A lactation consultant or your doctor can help you get started.
Breast Engorgement Treatment and Home Remedies
Engorgement can be painful and can cause trouble with your little one latching on. You may not want to breastfeed or pump. But that's the only way to make it go away.
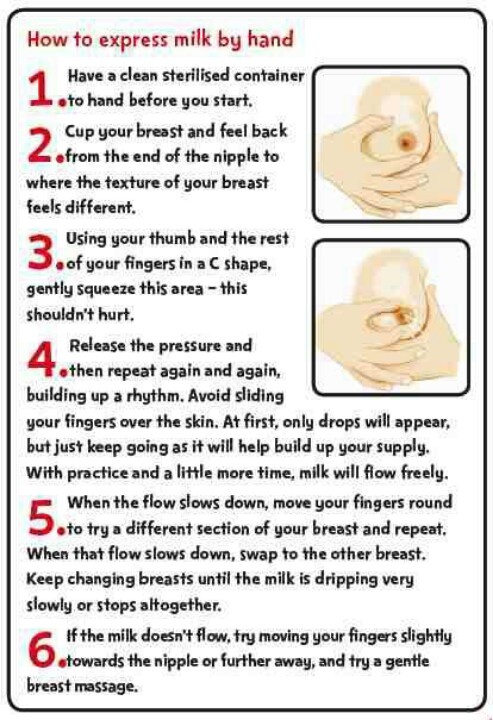
Sometimes engorgement can make your breasts feel hard to the touch. That's all the milk backed up in the breast tissue. If you're breastfeeding, this can make it tough for your baby to latch on or create a painful and improper latch. Pump or manually express milk first, then try again.
You can also try to reduce the hardness in your breasts by massaging them, taking a warm shower, or applying a warm compress to your breasts before feeding. If that doesn't work, don't keep trying. The warmth may increase the swelling instead and prevent the milk from flowing.
Once you get some milk out, the engorgement should go away. Then your baby will be able to latch and transfer the rest of the milk, emptying the breast.
Once your body understands how much milk your baby needs and gets into a rhythm, engorgement shouldn't be an issue. If you still feel that tightness and pain, try these tips and talk to your doctor. If you have fever, discharge from the nipple, or body aches, you should also talk with your doctor. You could also check in with a lactation consultant.
You can also do these:
- Switch to a bra with more support.
- Take over-the-counter pain medication (consult with your baby's doctor beforehand).
- Try ice packs to reduce swelling.
- Try reverse pressure softening, where you gently press on the area around your nipple for about a minute to try to shift some of the engorged fluid away from that area.
Breast Engorgement Prevention
The key is to not let your breasts get overly full with milk.
Feed your baby whenever they are hungry. Breastfeed or pump often or as close to every 2-3 hours to set a routine. Pump if you skip a feeding, have given a bottle, or if your baby doesn't take enough milk or empty the breast enough.
It can help to use a warm compress or take a warm shower before you breastfeed or express your milk.
Make sure you stay hydrated and eat a healthy diet, too.
If You’re Formula Feeding
Your body takes its cues from you. If milk isn't leaving your body, it will stop making more. If your breasts are engorged when your milk comes in and you are planning to formula feed, wear a tighter sports bra and curb any kind of stimulation to the breast. After some days, the engorgement will steadily decline.
Breast Engorgement: Symptoms, Treatment, and More
Once your little one has arrived, you’ll notice a few changes in your body. Your bump will get smaller and your breasts will fill up with milk. Sometimes, your breasts can feel overly full, heavy, and tight, even to the extent they are uncomfortable or even painful shortly after giving birth when the milk starts to come in. Read on to learn all about what breast engorgement is, how to prevent this condition, and how to help relieve engorged breasts.
What Is Breast Engorgement?
If you’re making more milk than your baby needs, your breasts can become overfilled with milk, which is known as breast engorgement.
During pregnancy, your body starts producing colostrum, a thick and yellowish milk that’s full of antibodies and protein. This is the early milk that will nourish your newborn right after birth.
Approximately two to four days after you’ve given birth, you’ll experience a change in your hormones and your breasts will fill with the standard white breast milk.
When your hormones shift, the blood supply to your breasts increases and you make more milk; you’ll feel as if your breasts are fuller. A little fullness in the first few days is perfectly normal, but sometimes breast milk production can become excessive, leading to discomfort and possibly even causing pain in your engorged breasts.
If you notice your breasts are engorged, take steps to treat this as soon as possible, as engorgement could lead to blocked milk ducts or mastitis.
What Are the Symptoms of Breast Engorgement?
During milk production, it’s perfectly normal to have full breasts, but you may have breast engorgement if you notice your breasts feel:
very full
hard
tender
painful or achy.
How Can You Prevent Breast Engorgement?
Breast engorgement usually doesn’t occur if the breasts are emptied frequently, meaning you’re nursing approximately every two to three hours. And if you experience engorged breasts, this may go away once you and your baby settle into a regular nursing pattern.
If you’re breastfeeding your baby, then severe breast engorgement may go away within 36 hours.
In situations when you can’t breastfeed right away, you can help prevent breast engorgement by using warm compresses, by expressing your milk manually, or by using a breast pump. Emptying your breasts can help with the initial discomfort.
Emptying your breasts can help with the initial discomfort.
How Can You Relieve Engorged Breasts?
If you’re not breastfeeding or expressing milk, then you may feel some discomfort from engorgement. But if the breasts are not stimulated to produce more milk, then the discomfort you feel from breast engorgement may go away gradually, usually within 7 to 10 days. You can try the following in the meantime to help with engorged breast pain relief even if you’re not breastfeeding:
Wear a well-fitting support bra or sports bra
Apply ice packs to your breasts to help reduce the swelling
Avoid expressing any milk if you don’t plan to continue nursing, as this will signal to your breasts to make more milk; you may want to discuss this with a lactation consultant or your healthcare provider
Take an over-the-counter pain medication, like ibuprofen, if you need it, but consult your healthcare provider if you’re unsure
You can try a popular home remedy—placing a refrigerated, clean cabbage leaf directly on the breast, so it's held in place by a bra.
 The coolness combined with the shape of the cabbage leaf, which fits the shape of breast, may help with the swelling, but this is a home remedy that may not work for all women.
The coolness combined with the shape of the cabbage leaf, which fits the shape of breast, may help with the swelling, but this is a home remedy that may not work for all women.
If you’re breastfeeding and still suffer from breast engorgement, in addition to some of the above tips, you may also want to try feeding your baby in more than one position.
The Bottom Line
Breast engorgement can be uncomfortable, but it’s not something to worry about. It can be easily treated either by feeding your baby regularly or with cool compresses until the swelling goes down.
However, sometimes a blocked milk duct or mastitis can feel like breast engorgement, so if you’re in doubt, consult your healthcare provider, especially if you notice any flu-like symptoms or your breasts are hot to the touch.
The good news is that the uncomfortable swelling most likely will go down, either with regular feedings or just with time. Soon your breasts will feel less heavy and achy, and you’ll have more energy to focus on your little one.
Soon your breasts will feel less heavy and achy, and you’ll have more energy to focus on your little one.
Breast engorgement symptoms and first aid
search support iconSearch Keywords
Home ›› How to relieve the unpleasant symptoms of breast engorgement
Home ›› How to relieve the unpleasant symptoms of breast engorgement
↑ 0 Top Let's look at all the important issues, including prevention, symptoms, and help with engorgement. Breast engorgement occurs for various reasons. The most common: - Skipping a feeding or pumping session. - Making more milk than the baby eats. - Insufficient outflow of milk (improper latching on to the breast by the baby). - Inflammation. Although engorgement and mastitis may appear similar, they are actually completely different conditions. How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement. 3. Make sure the baby is latching on correctly. To learn how to properly breastfeed a baby, a mother can seek advice from a breastfeeding specialist. Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples. 4. Wean the baby gradually. When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement. Philips Avent 2-in-1 thermal pads can both warm and cool your breasts to both stimulate and soothe your breasts after feeding.
One of the most common breastfeeding problems faced by mothers is breast engorgement. While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it.
What is breast engorgement?
Engorgement is an increase in the size of the mammary glands, in which the breast becomes painful and sensitive. This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth. In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs.
This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth. In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs.
How long does engorgement last?
All women are different, and, accordingly, the duration of this condition may vary. Some experience mild symptoms for only one day, while others may experience this condition for up to two weeks.

Breast engorgement symptoms
Breast engorgement symptoms vary, but the most common are:
Prevention of engorgement
There are several ways to prevent this condition.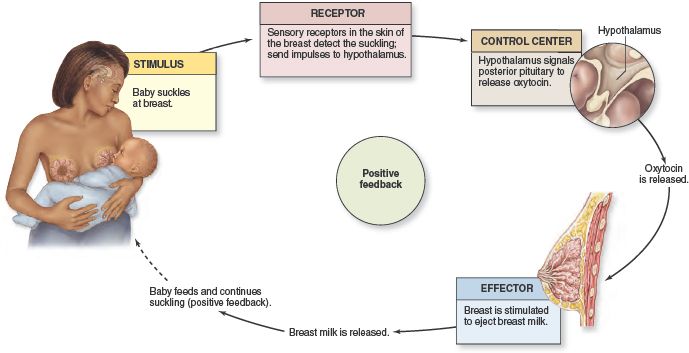 Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:
Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:
Electronic breast pump will help you to comfortably and efficiently express the right amount of milk between feedings, if necessary, or instead of feeding when the mother is away from the baby.
Helping with breast engorgement
Breastfeeding with engorgement is not only safe, but necessary to prevent symptoms from getting worse and provide relief. While the body is learning how to produce the right amount of milk, moms can use the Philips Avent bra pads to absorb excess milk and prevent stains on clothes all day long. Philips Avent
 Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result). Philips Avent
Multifunction thermal pads
SCF258/02
Overall rating / 5
- review review reviews Reviews
-
-{discount-value}
- Pictures It is important to achieve optimal outflow of milk during feedings. To stimulate the outflow of milk, during feeding, you can gently massage the breast.
- Express milk. There are situations when a nursing mother cannot be with the baby during feeding. It is important to empty your breasts by expressing milk to prevent engorgement and other problems.

- When feeding, change positions and alternate breasts. Changing your position while breastfeeding can be beneficial, as it improves the outflow of milk from different parts of the mammary glands. In addition, mothers can change their breasts during one feeding so that the baby can empty both of them.
Remember that minor pain and discomfort is completely natural during breastfeeding, but if these symptoms persist or worsen, the mother should consult a doctor.
Philips Avent Articles & Tips
Baby+ App
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Solving six first week breastfeeding problems
Having trouble breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Kathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home.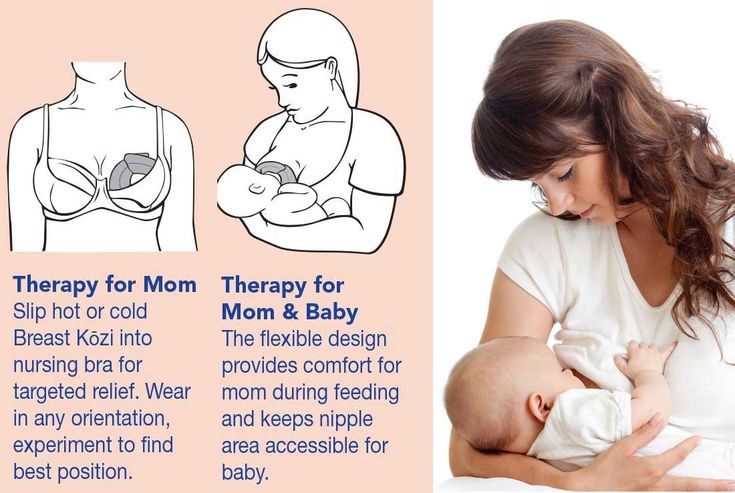 Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 young mothers surveyed, 92% had problems breastfeeding by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during breastfeeding is usually associated with sore or sore nipples, especially when milk comes in on the second to fourth day after delivery. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: for some mothers, the nipples crack, bleed or blister. This is, of course, very annoying.
Solutions 3
- Check for baby latch on.
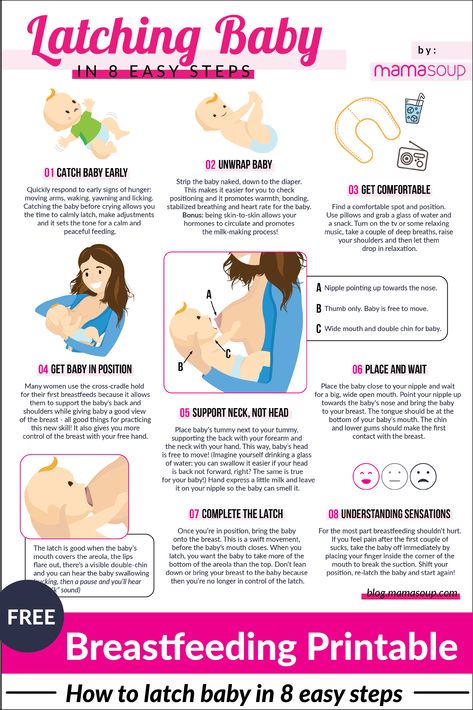
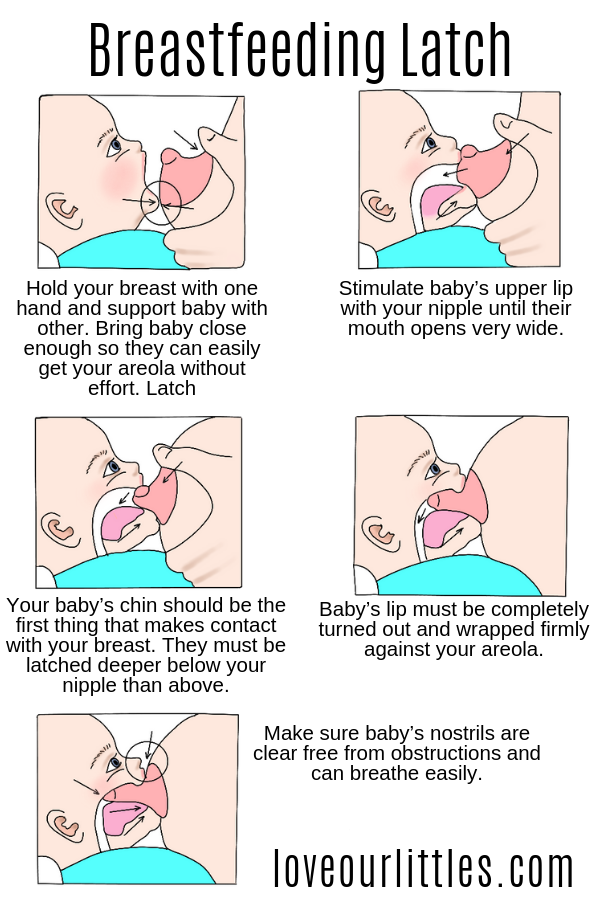
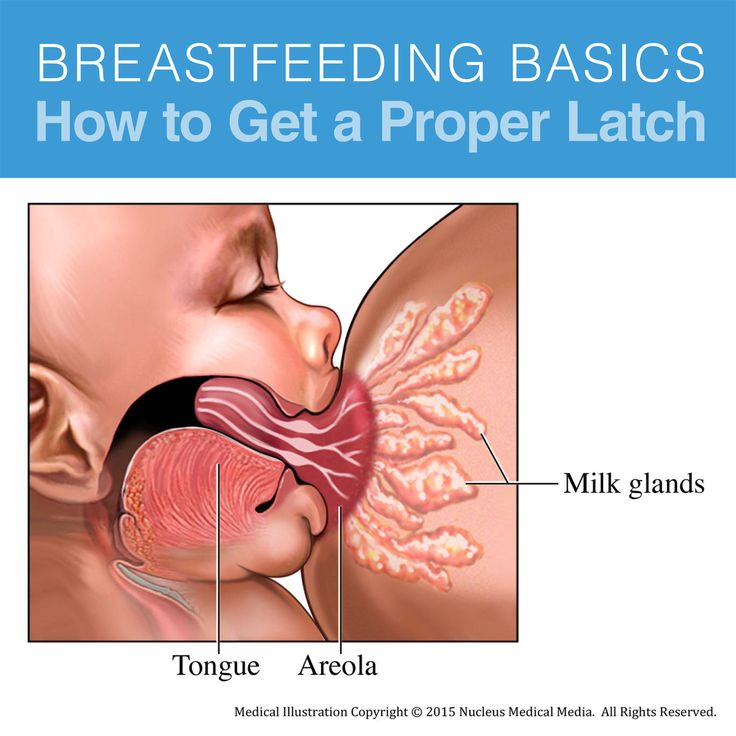
 An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue. - Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or pat dry with a clean, soft muslin or flannel cloth to prevent bacterial growth in humid environments.
 Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly. - Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not improve after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.

Problem #2. Baby doesn't latch on properly
Some newborns do not immediately latch on properly. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead.
 This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.

Problem #3. Not enough breast milk
You will not produce much breast milk at the very beginning, because the hormonal changes that trigger milk production are slow and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you are having problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night.
 Such frequent feeding helps to establish the production of breast milk.
Such frequent feeding helps to establish the production of breast milk. - Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem number 5. Leaking milk
Leaking milk from the breast is very common in the early days of breastfeeding when milk production begins.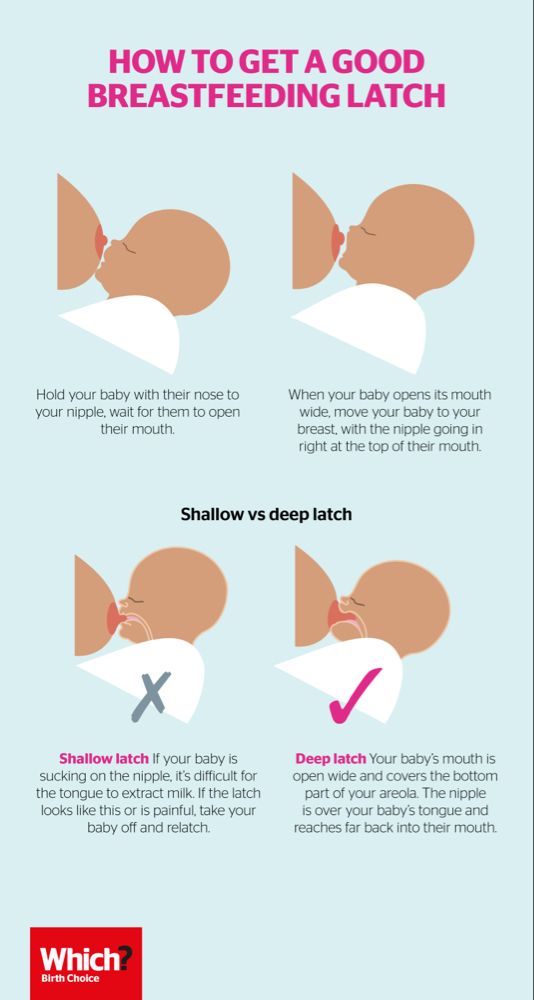 Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads, which should be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control milk flow. The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm.
 The torso of the baby will be located diagonally on you.
The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." F Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642.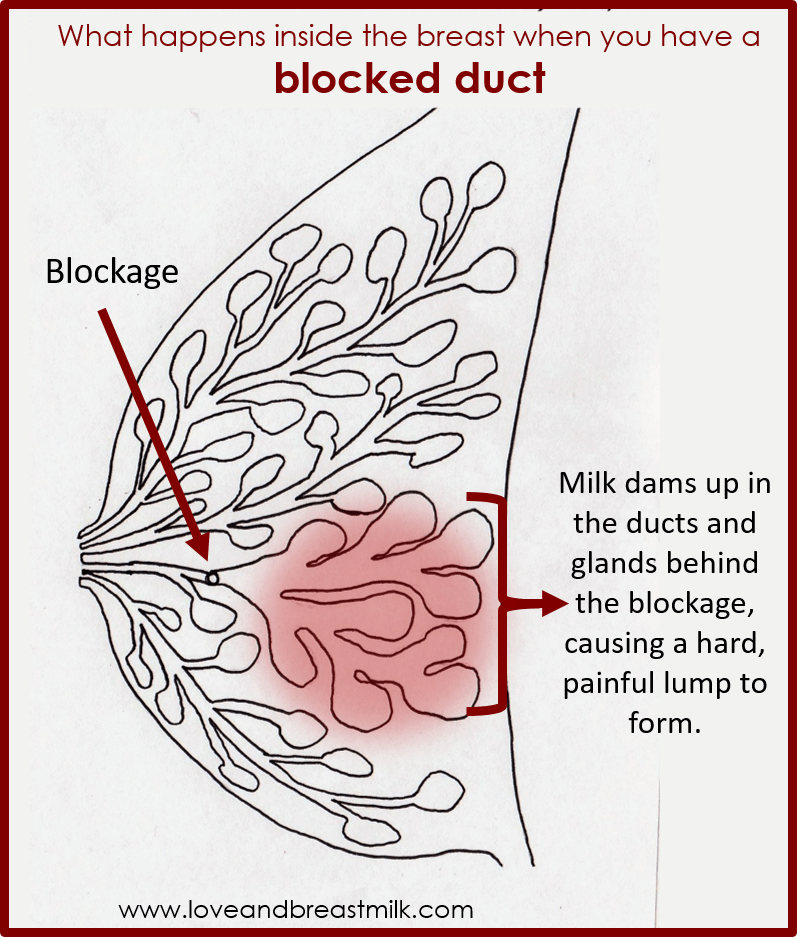 — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014.