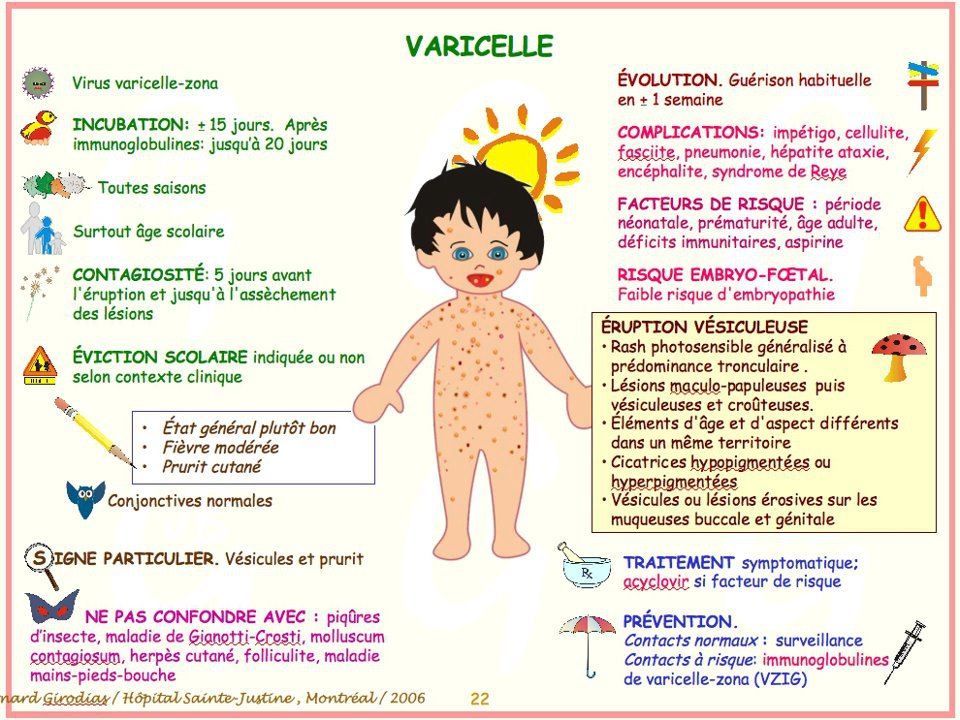
Anencephaly and spina bifida
Facts about Anencephaly | CDC
Anencephaly (pronounced an-en-sef-uh-lee) is a serious birth defect in which a baby is born without parts of the brain and skull.
Click here to view a larger image
What is anencephaly?
Anencephaly is a serious birth defect in which a baby is born without parts of the brain and skull. It is a type of neural tube defect (NTD). As the neural tube forms and closes, it helps form the baby’s brain and skull (upper part of the neural tube), spinal cord, and back bones (lower part of the neural tube).
Anencephaly happens if the upper part of the neural tube does not close all the way. This often results in a baby being born without the front part of the brain (forebrain) and the thinking and coordinating part of the brain (cerebrum). The remaining parts of the brain are often not covered by bone or skin.
How Many Babies are Born with Anencephaly?
Researchers estimate that about 1 in every 4,600 babies is born with anencephaly in the United States. 1
Causes and Prevention
The causes of anencephaly among most infants are unknown. Some babies have anencephaly because of a change in their genes or chromosomes. Anencephaly might also be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment or what the mother eats or drinks, or certain medicines she uses during pregnancy.
Getting enough folic acid before and during early pregnancy can help prevent neural tube defects, such as anencephaly. If you are pregnant or could get pregnant, take 400 micrograms (mcg) of folic acid every day. If you have already had a pregnancy affected by an NTD, you can speak with your doctor about taking a higher dose of folic acid before pregnancy and during early pregnancy.
- Since the United States began fortifying grains with folic acid, there has been a 28% decline in pregnancies affected by neural tube defects (spina bifida and anencephaly).1
- In order to get the recommended 400 micrograms of folic acid every day, a woman of reproductive age can take a supplement containing folic acid or to eat foods fortified with folic acid, or both, depending on her dietary habits.
.jpg)
CDC is dedicated to better understanding the causes of birth defects. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011), to understand the causes of and risks for birth defects, including anencephaly.
If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Anencephaly can be diagnosed during pregnancy or after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (prenatal tests) to check for birth defects and other conditions. Anencephaly would result in an abnormal result on a blood or serum screening test or it might be seen during an ultrasound (which creates pictures of the body). For more information about screening and confirmatory tests during pregnancy, visit CDC’s birth defects diagnosis web page.
For more information about screening and confirmatory tests during pregnancy, visit CDC’s birth defects diagnosis web page.
After the Baby is Born
In some cases, anencephaly might not be diagnosed until after the baby is born. Anencephaly is immediately seen at birth.
Treatments
There is no known cure or standard treatment for anencephaly. Almost all babies born with anencephaly will die shortly after birth.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
Neural Tube Defects | MedlinePlus
On this page
Basics
- Summary
- Start Here
- Diagnosis and Tests
- Prevention and Risk Factors
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- No links available
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
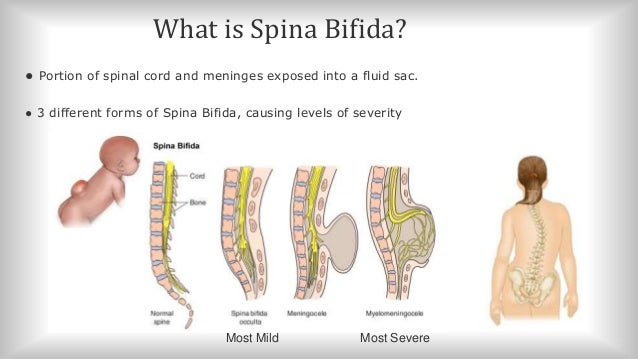
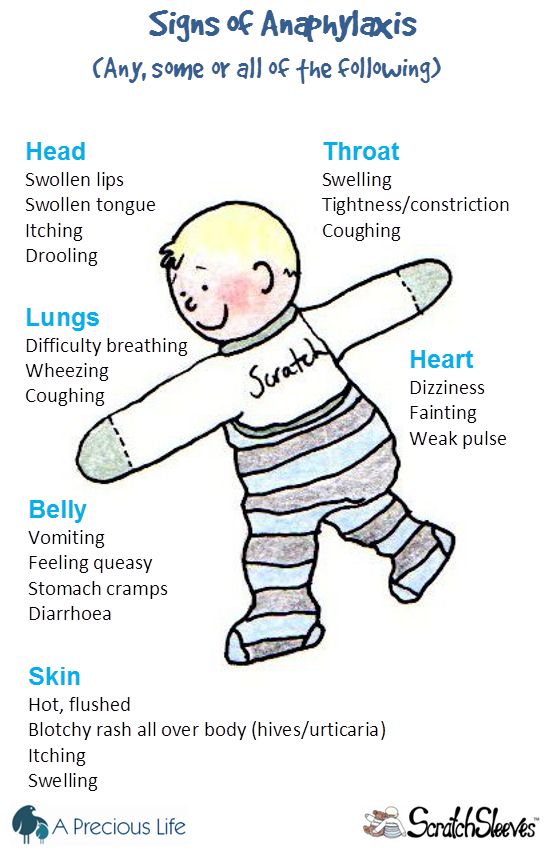
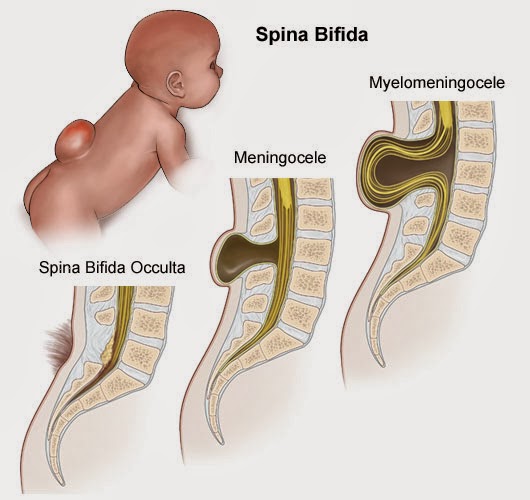
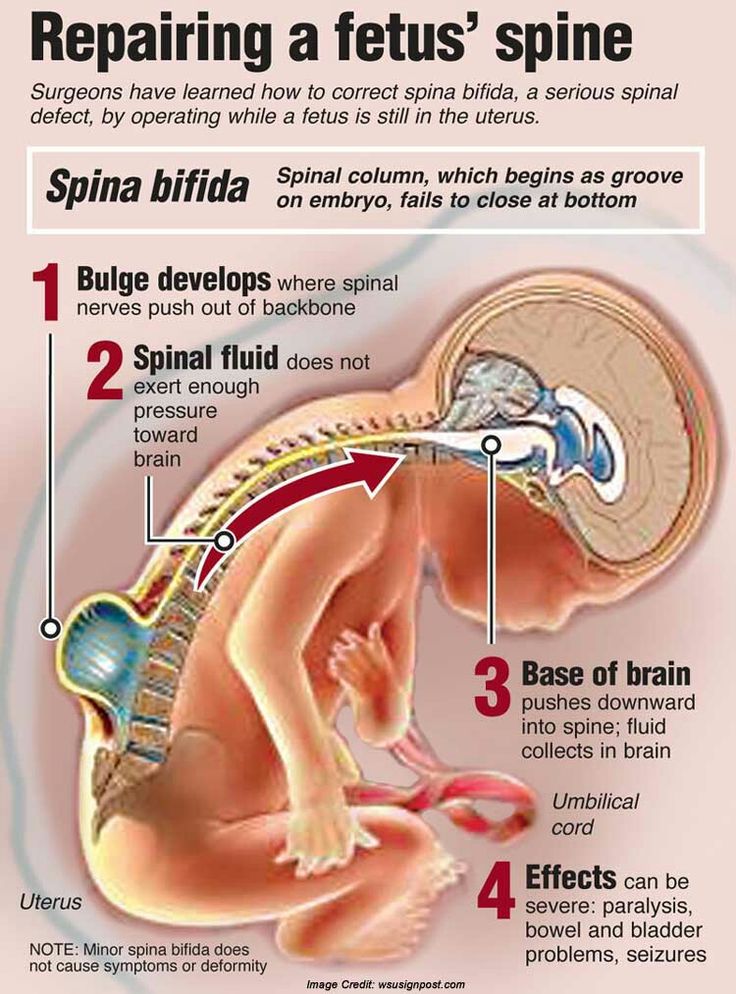
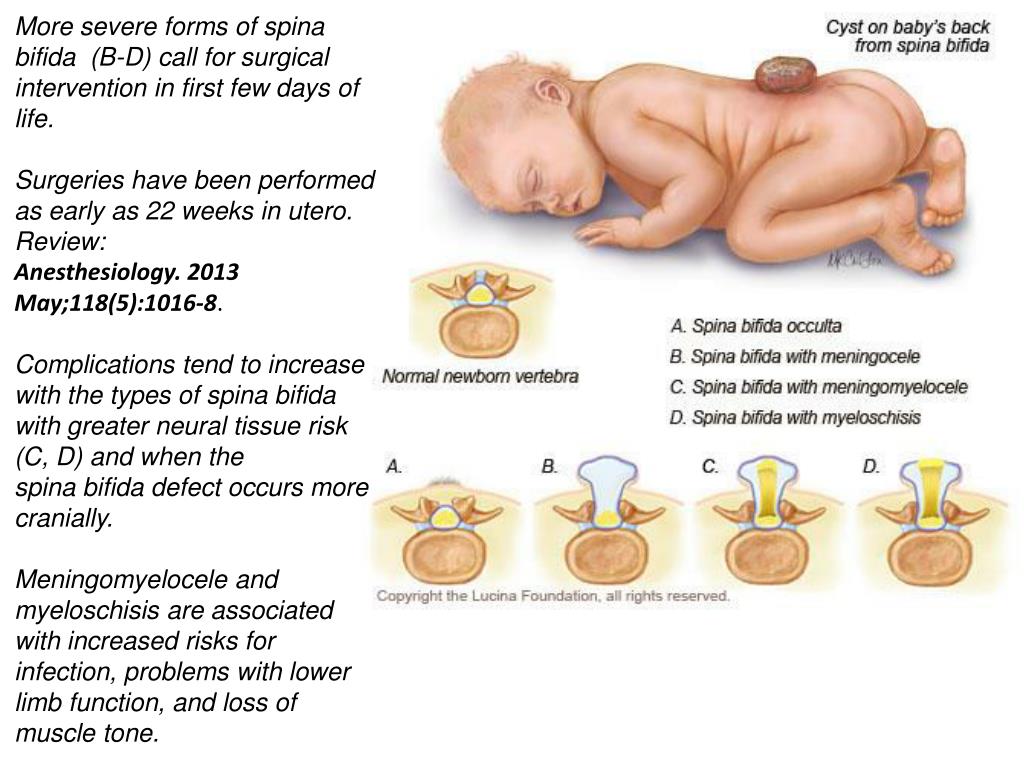
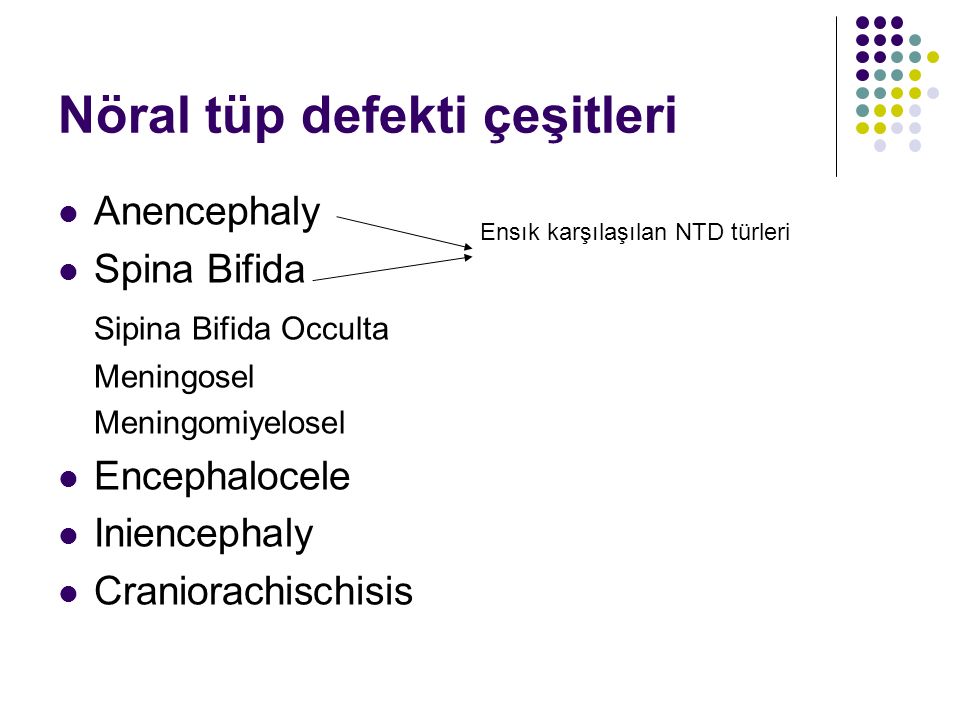
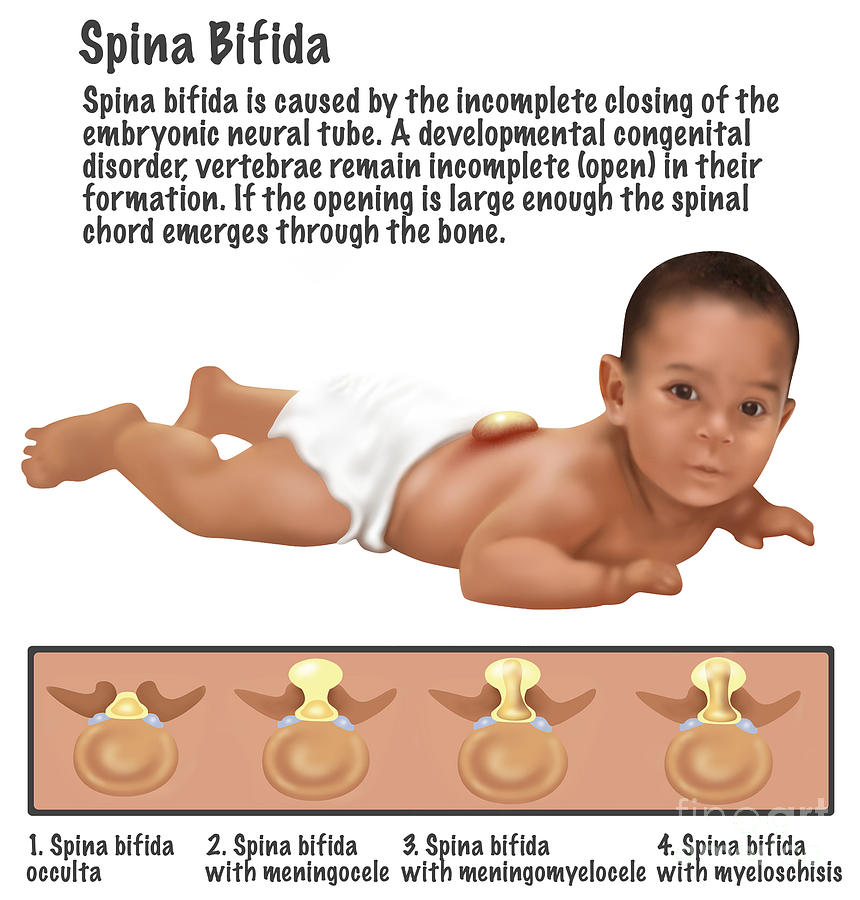
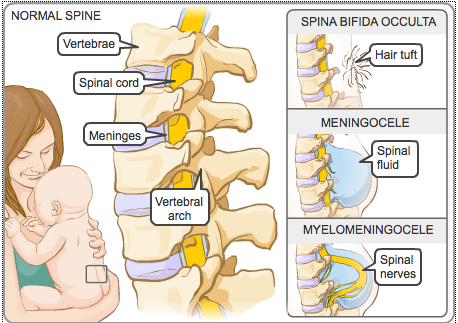
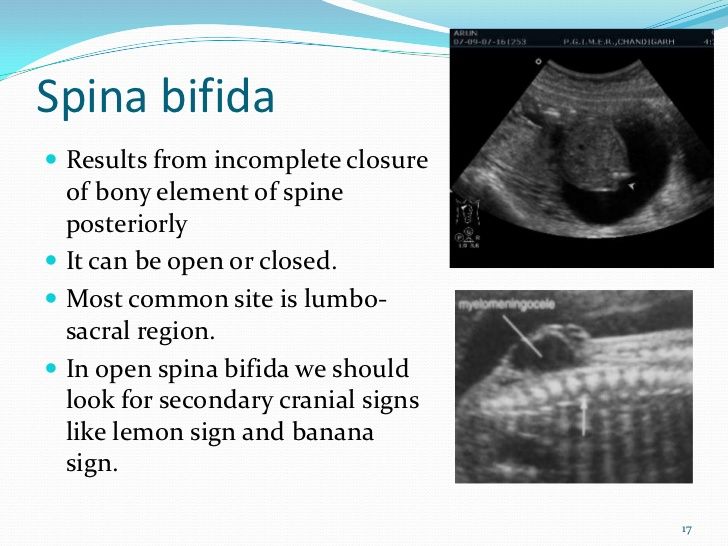
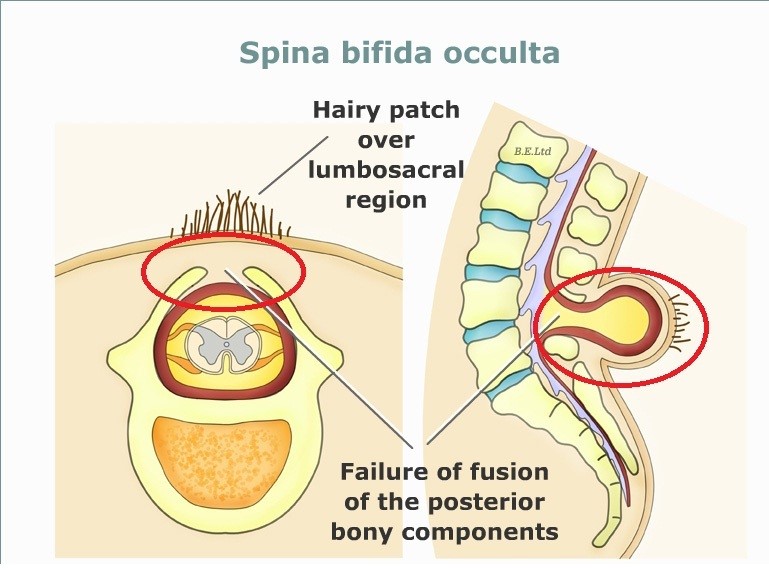
Neural tube defects are birth defects of the brain, spine, or spinal cord.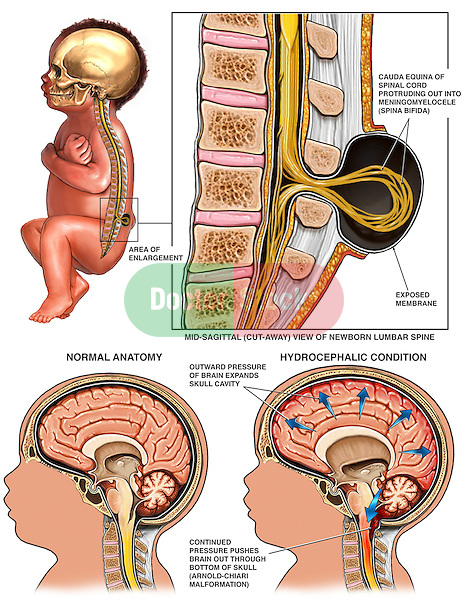 They happen in the first month of pregnancy, often before a woman even knows that she is pregnant. The two most common neural tube defects are spina bifida and anencephaly. In spina bifida, the fetal spinal column doesn't close completely. There is usually nerve damage that causes at least some paralysis of the legs. In anencephaly, most of the brain and skull do not develop. Babies with anencephaly are usually either stillborn or die shortly after birth. Another type of defect, Chiari malformation, causes the brain tissue to extend into the spinal canal.
They happen in the first month of pregnancy, often before a woman even knows that she is pregnant. The two most common neural tube defects are spina bifida and anencephaly. In spina bifida, the fetal spinal column doesn't close completely. There is usually nerve damage that causes at least some paralysis of the legs. In anencephaly, most of the brain and skull do not develop. Babies with anencephaly are usually either stillborn or die shortly after birth. Another type of defect, Chiari malformation, causes the brain tissue to extend into the spinal canal.
The exact causes of neural tube defects aren't known. You're at greater risk of having an infant with a neural tube defect if you:
- Have obesity
- Have poorly controlled diabetes
- Take certain antiseizure medicines
Getting enough folic acid, a type of B vitamin, before and during pregnancy prevents most neural tube defects.
Neural tube defects are usually diagnosed before the infant is born, through lab or imaging tests. There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
NIH: National Institute of Child Health and Human Development
- About Neural Tube Defects (NTDs) (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Neural Tube Defects (March of Dimes Birth Defects Foundation)
- Alpha-fetoprotein (AFP) Test (National Library of Medicine) Also in Spanish
- How Do Health Care Providers Diagnose Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Treatments for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Are There Disorders or Conditions Associated with Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Anencephaly (National Institute of Neurological Disorders and Stroke)
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) Also in Spanish
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) - Short Summary
- Encephaloceles (National Institute of Neurological Disorders and Stroke)
- Facts about Anencephaly (Centers for Disease Control and Prevention) Also in Spanish
- Facts about Encephalocele (Centers for Disease Control and Prevention) Also in Spanish
- Hydranencephaly (National Institute of Neurological Disorders and Stroke)
- Iniencephaly (National Institute of Neurological Disorders and Stroke)
- Tethered Spinal Cord Syndrome (National Institute of Neurological Disorders and Stroke)
- How Many People Are at Risk for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Anencephaly (National Institutes of Health)
gov: Anencephaly (National Institutes of Health) - ClinicalTrials.gov: Arnold-Chiari Malformation (National Institutes of Health)
- ClinicalTrials.
 gov: Neural Tube Defects (National Institutes of Health)
gov: Neural Tube Defects (National Institutes of Health)
- Article: Aetiology and diagnostics of paediatric hydrocephalus across Africa: a systematic review.
 ..
.. - Article: Analysis of DNMT1 gene variants in progression of neural tube defects-an...
- Article: Global prevalence of congenital anencephaly: a comprehensive systematic review and meta-analysis.

- Neural Tube Defects -- see more articles
- Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish
- Find a Genetic Counselor (National Society of Genetic Counselors)
- Find a Pediatrician or Pediatric Specialist (American Academy of Pediatrics) Also in Spanish
- March of Dimes Birth Defects Foundation Also in Spanish
- National Institute of Neurological Disorders and Stroke Also in Spanish
D.
 Nemescu • Three-dimensional ultrasound in the diagnosis of iniencephaly
Nemescu • Three-dimensional ultrasound in the diagnosis of iniencephaly Ultrasound machine HS40
Top seller in the high class. High definition 21.5" monitor, advanced cardio package (Strain+, Stress Echo), OB/GYN 3D expert capabilities (STIC, Crystal Vue, 5D Follicle), high density transducers.
Introduction
Iniencephaly is a rare neural tube pathology characterized by a triad: occipital bone defect, congenital spina bifida in the cervicothoracic region, and severe retroflexion of the head [1]. The name of this defect comes from the fusion of two roots - inion (external occipital protuberance) and encephalosis (enkephalos, brain). This phenomenon was first described by J. Saint-Hilaire [2]. H.Lewis identified two main groups: gap iniencephaly, with the formation of cerebral herniation, and closed iniencephaly, in which there is damage to the spine in the absence of cerebral herniation. The frequency of pathology varies: 0. 1-10:10,000 [3] and higher, depending on the possibilities of diagnosing the syndrome. Iniencephaly is more common among female fetuses - M:W=1:10 4 .
1-10:10,000 [3] and higher, depending on the possibilities of diagnosing the syndrome. Iniencephaly is more common among female fetuses - M:W=1:10 4 .
The etiology of the disease is unknown. There is seasonality and age fluctuations in the frequency of detection of the syndrome. The association of iniencephaly with the intake of substances such as sleeping pills, vinblastine, estreptonigrin, triparanol and with diseases such as syphilis (in the mother) and in the case of closely related relationships in parents has been described [5-7]. Other risk factors are low fertility and low socioeconomic status [8]. For example, the prevalence of this pathology in Northern China is 25 times higher than in the United States.
Clinical observation
A 35-year-old woman with her 8th pregnancy at 13.5 weeks (Fig. 1) was referred for examination to assess fetal pathology (Fig. 2). Ultrasound scanning revealed pathology of the fetal shape in the form of a lack of a clear separation between the head and body with the face turned upwards, excessive lordosis in the cervical and thoracic spine, significant shortening of the spine, and complete underdevelopment of the anterior cerebral bladder (Fig.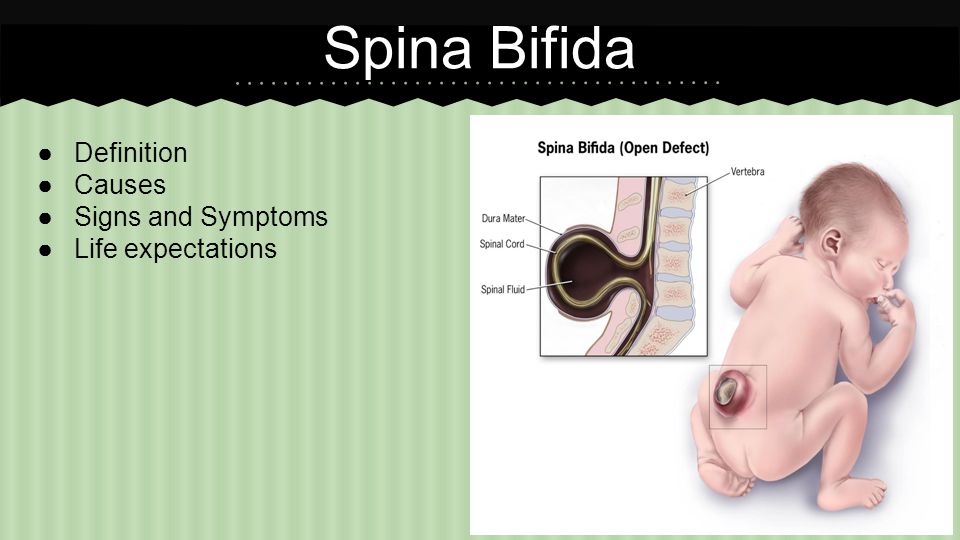 2, 3).
2, 3).
Fig. 1. Fetal thigh of normal length for a given gestational age.
Fig. 2. Pathology of the shape of the fetus in the form of a lack of a clear separation between the head and body. Excessive lordosis in the cervicothoracic spine. An abnormal position of the face in relation to the body is noted. 3D reconstruction of the posterior surface of the head (lower right) shows a defect - the absence of the occiput.
Fig. 3. Pathology of the cervical spine, absence of the neck and complete underdevelopment of the anterior cerebral bladder. Longitudinal scan.
Primary superficial 3D reconstruction showed the absence (defect) of the occiput, especially in the high threshold mode (Fig. 4). At the same time, the longitudinal sections (Fig. 2, 3) showed the continuity of the contour of the posterior surface of the head. When using the maximum mode, the 3D volumetric reconstruction in longitudinal section also shows retroflexion with lordosis of the cervical spine, but with a clearly identifiable undeveloped vertebra (Fig.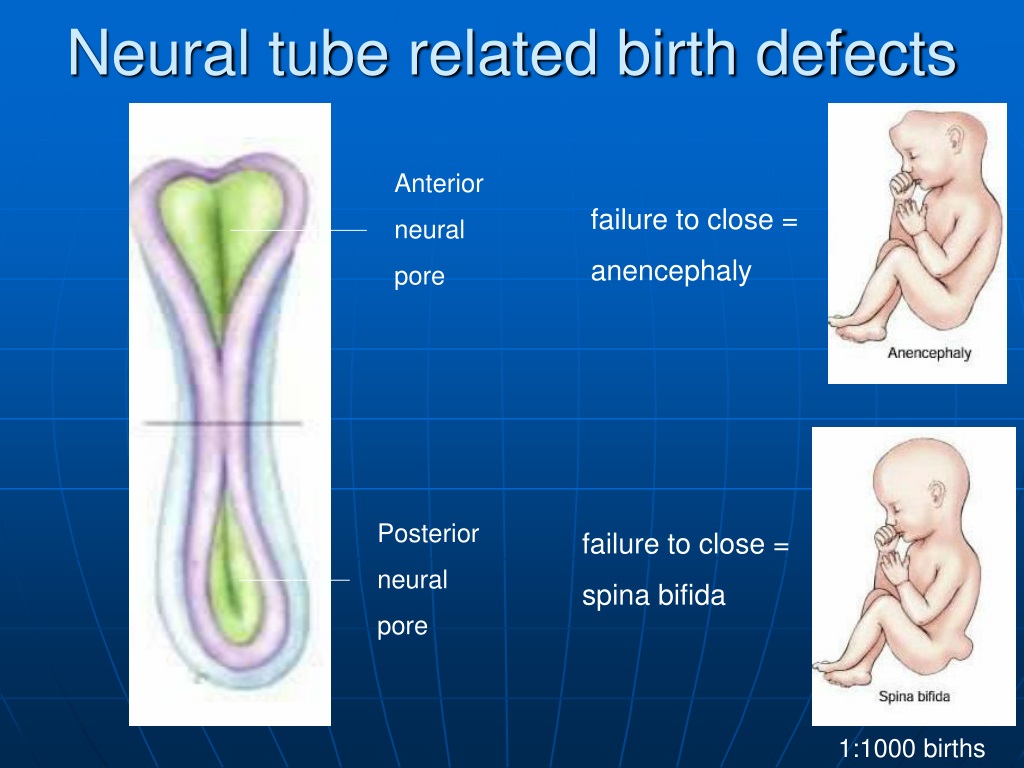 5).
5).
Fig. 4. Dorsal view of the fetus showing the absence of the occiput. 3D reconstruction, surface mode.
Fig. 5. Pathology of the spine - undeveloped cervical vertebra (arrow). 3D reconstruction, maximum mode.
A high axial scan at the level of the lateral ventricles did not reveal a bilateral prominent intrahemispheric echogenic choroid plexus that normally almost completely fills the lumens of the lateral ventricles at this gestational age. Instead, a wide single ventricle filled with fluid was observed, in which there was no median echo, which displaced the cerebral cortex laterally (Fig. 2). When examining the face from the front, hypotelorism was noted (Fig. 6).
Fig. 6. Hypothelorism, fetal face when viewed from the left and front.
a) B-mode.
b) 3D surface reconstruction.
The above signs characterize the complete underdevelopment of the anterior cerebral bladder and correspond to the diagnosis of iniencephaly.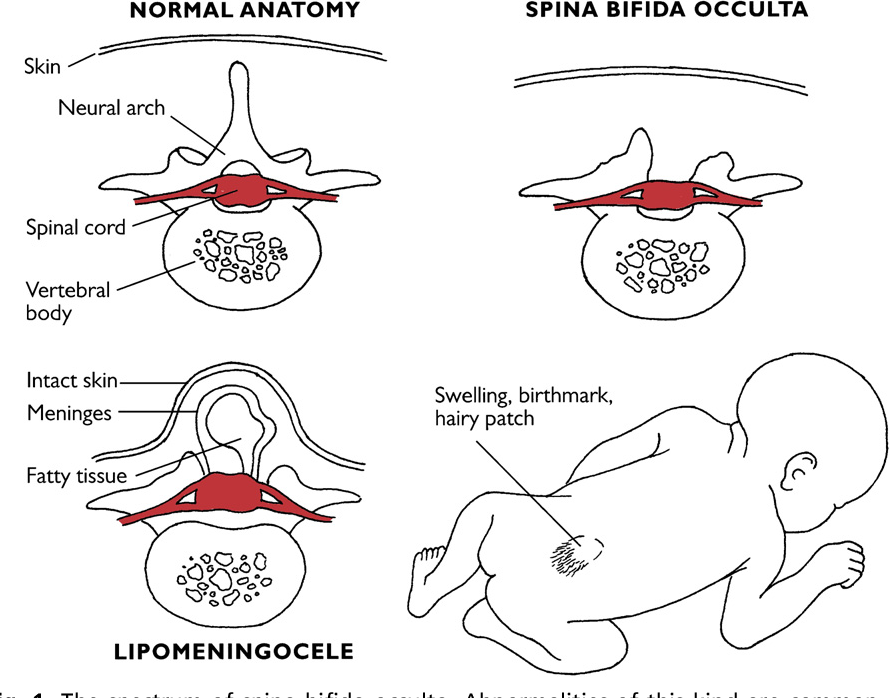
The pregnancy was terminated, and the results of the post-mortem examination fully coincided with the ultrasound findings (Fig. 7). A leading lesion of the spine was noted, which is very characteristic of iniencephaly.
Fig. 7. Iniencephaly. Pathological study. Different types (a-c).
Discussion
Iniencephaly is a pathology of the neural tube. Probably, during embryogenesis, it manifests itself several days later than anencephaly. Pathological development of the coracoid segment of the brain tube and impaired segmentation of the cervical-occipital region cause incomplete development of the base of the skull, excessive stretching of the head and shortening of the spine with its congenital splitting.
This pathology differs from anencephaly in that the anterior part of the brain tube is closed in iniencephaly. Microscopic examination of the brain reveals a number of anomalies, "including microencephaly, polymicrogyria, heterotopic glial tissue in the meninges, atresia of the ventricular system, marked disorganization of the brainstem and spinal cord tissue, and large cerebellar cysts" [9].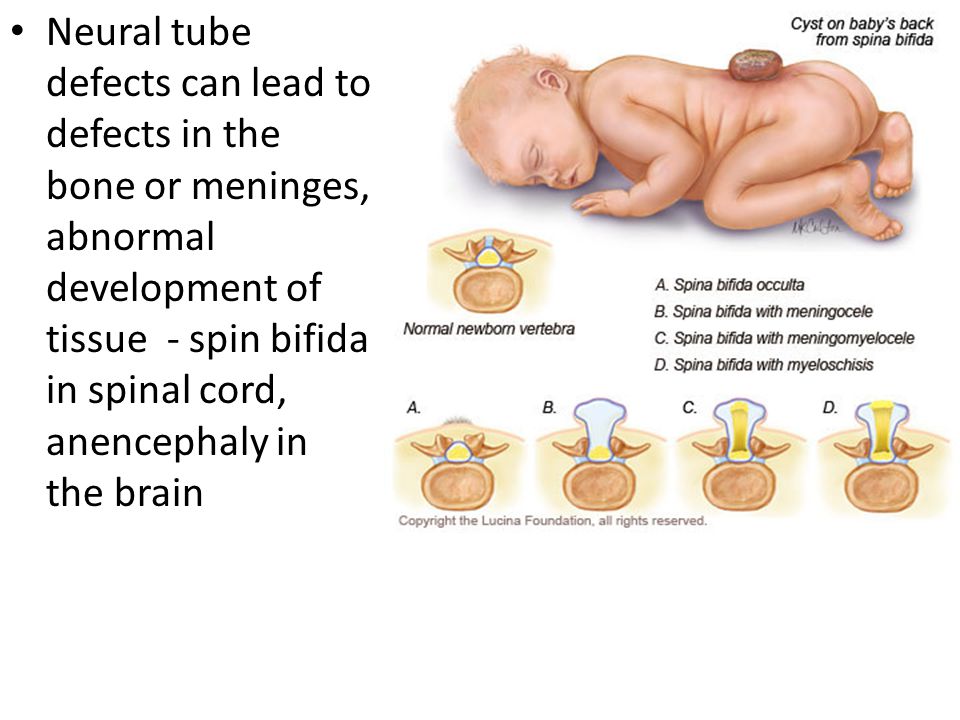
There are a number of hypotheses trying to explain the appearance of iniencephaly. The latter was associated with dilatation and rupture of the neural tube [10], non-closure of the neural tube during embryogenesis [11], early vascular disorders [12] with a restructuring of the normal angiogenesis of the vessels responsible for perfusion in the neural tube, followed by their malformation. M.Jones et al. obtained clinical evidence supporting the hypothesis that axial dysraphic disorders may be the result of primary rearrangement of the embryonic mesoderm. This may explain the presence of mesodermal lesions observed in iniencephaly [13].
This anomaly is inherited in isolated cases. I. Kjaer et al. argue that iniencephaly may be the result of "gene changes in the embryonic period that disrupt the dorsoventral orientation of the body axis, anatomically manifested by the incorrect position of the notochord" [14].
Diagnostic criteria for iniencephaly [15,16] - deficiency of the occipital bones of varying severity, manifested in an enlarged foramen magnum; partial or complete absence of the cervical and thoracic vertebrae, accompanied by incomplete closure of the vertebral arches and (or) bodies; a significant shortening of the spinal column due to pronounced lordosis with overstretching of the malformed spinal cord in the cervicothoracic region, which is determined by medial-sagittal scanning [17]; excessive dorsal flexion of the head, upward turning of the face, and a direct transition of the mandibular skin to the thorax due to the absence of a neck.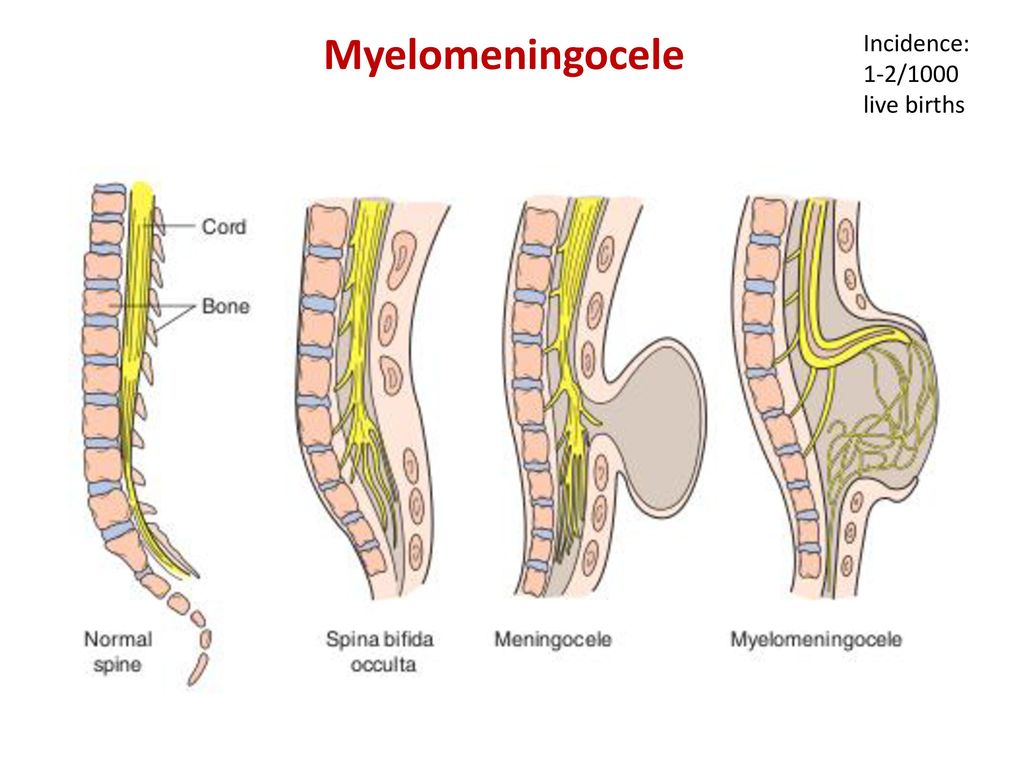
Other ultrasound findings include: open cervical spine with meningocele, often anencephaly, lumbosacral myelomeningocele, or caudal regression.
Diagnosis is based on excessive dorsal head flexion, very short and deformed cervical and thoracic spine, and general shortening of the fetus. Many cases diagnosed prenatally had high AFP levels and/or polyhydramnios. There is evidence that the earliest diagnosis was made at 13 weeks [18].
Iniencephaly is manifested by various anomalies: it is a defect of the occiput, prolapse of the brain through the enlarged occipital foramen, sharp lordosis in the cervical spine, microencephaly, polymicrogyria, ectopic glial tissue in the meninges, atresia of the ventricular system of the brain, cerebellar cysts, disorganization of the brainstem brain, circulatory disorders in the vessels of the neck and spine, common carotid trunk.
Iniencephaly may be accompanied by a number of other anomalies: anencephaly, cerebral herniation, complete underdevelopment of the anterior cerebral bladder, congenital absence of the jaw, microstomia, synmyelia, hydrocephalus, spina bifida.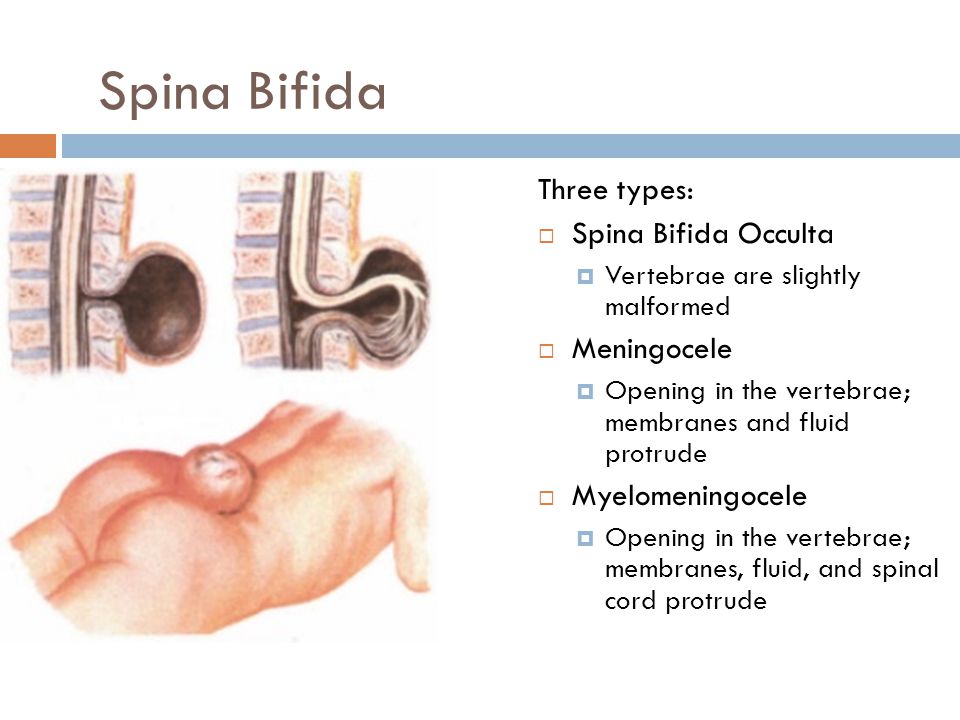 May present with cleft palate, cardiac malformations (right-sided heart, common carotid artery, transposition of large arteries), hiatal hernia or diaphragmatic agenesis, pulmonary hypoplasia or hyperplasia, umbilical artery agenesis, umbilical hernia, polycystic kidney disease, horseshoe kidney, overgrowth arms comparable to legs, backward bending of the knees, arthrogryposis, clubfoot and polyhydramnios [1,15,16,19,twenty].
May present with cleft palate, cardiac malformations (right-sided heart, common carotid artery, transposition of large arteries), hiatal hernia or diaphragmatic agenesis, pulmonary hypoplasia or hyperplasia, umbilical artery agenesis, umbilical hernia, polycystic kidney disease, horseshoe kidney, overgrowth arms comparable to legs, backward bending of the knees, arthrogryposis, clubfoot and polyhydramnios [1,15,16,19,twenty].
The differential diagnosis is made with Klippel-Feil syndrome (shortening of the neck with fusion of the cervical vertebrae), anencephaly with cervical retroversion, cervical spinal hernia and cervical teratoma [3]. The differential diagnosis between iniencephaly and Klippel-Feil syndrome is difficult and controversial. Some authors believe that Klippel-Feil syndrome may be a mild form of iniencephaly [21]. The distinction between slit iniencephaly and anencephaly with dorsal retroflexion appears from the outset [19]. Anencephaly appears before the closure of the neural folds on the 24th day of pregnancy [22]. On the other hand, iniencephaly develops after the brain tube has closed [19].
On the other hand, iniencephaly develops after the brain tube has closed [19].
Neonatal iniencephaly is always fatal. Four cases of long-term survival have been described for very mild slit iniencephaly [23], but in these cases the deformity was minimal and could probably be regarded as Klippel-Feil syndrome. In all cases of detection of this anomaly, termination of pregnancy is recommended. In subsequent pregnancies, some experts prescribe folic acid.
Iniencephaly was previously regarded as a rare pathology of the neural tube. Nowadays, due to the improved diagnosis of iniencephaly by ultrasound criteria using 3D ultrasonography, an increasing number of cases are detected prenatally.
Literature
- Lewis HL. Iniencephalus. Am J Obstet Gynecol 1897; 35:11-53
- SaintxHilaire IG. Iniencephalus. In Histoire des Anomalies de l'Organisation. Paris: J.B. Baillier. 1986: Vol.2:308-10
- Romero R, Pilu G, Jeanty P, et al.
 Prenatal Diagnosis of Congenital Anomalies. Norwalk, CT: Appleton and Lange, 1988:64-7
Prenatal Diagnosis of Congenital Anomalies. Norwalk, CT: Appleton and Lange, 1988:64-7 - Morocz I, Szeifert T, Molnar P, et al. Prenatal diagnosis and pathoanatomy of iniencephaly. Clin Genet 1986:30:81-6
- Garofalo R, Simosa V, Morean F. Defectos del cierre del tubo neural. Arch Venez Pueric Pediat 1990;53:85-9.
- Sosa Olavarria A. Ultrasonografia y Clinica Embriofetal. Valencia, Venezuela: Editorial Tatum, 1994
- Bermudez A, Sosa Olavaria A, Rivas M, Mira M. Iniencefalia: serie de seis casos. Rev Obstet Ginecol Venez. 1995:55:161-5
- Nyberg DA, Mahomy BS, Pretorius DH: Diagnostic Ultrasound of FetalAnomalies - Text and atlas. Littleton, MA: Year Book Medical Publishers, 1990:146.
- Morocz I, Molnar P, Toth Z, et al. Diagnostic criteria of iniencephaly based on the authors own cases and the review of the literature.
 Morphol Igazsagugyi Orv Sz 1985; 25:58-65.
Morphol Igazsagugyi Orv Sz 1985; 25:58-65. - Gardner WJ. Klippel Feil syndrome, iniencephalus, anencephalus, hindbrain, hernia and mirror movement. Overdistention of the neural tube. Child's Brain 1990;5:361-79.
- Scherrer C, Hammer F, Schmzel A, Briner J. Brain stem cervical cord dysrraphic lesion in iniencephaly. Pediafr Pathol 1992;12:469-76
- Stevenson RE, Kely JC, et al. Vascular basis for neural tube defects: a hypothesis. Pediatrics 1987;80:102-6
- Jones MC, Jones KL, Chernoff GF. Possible mesodermal origin for axial dysraphic disorders. J Pediatr 1982; 101:845-9
- Kjaer I, Mygind H, Fischer Hansen B. Notochordal remnants in human iniencephaly suggest disturbed dorsoventral axis signaling. Am J Med Genet 1999;84:425-32
- Cimmino CV, Painter JW. Iniencephaly. Radiology 1962;84:425-32
- Bose S, Makhani JS, Thacker SV.
 Iniencephaly. Ind J Med Sci 1964;18:590-4
Iniencephaly. Ind J Med Sci 1964;18:590-4 - Morocz I, Szeifert T, Molnar P, et al. Prenatal diagnosis and pathoanatomy of iniencephaly. Clin Genet 1986;30:81-6
- Sherer DM. Endovaginal sonographic diagnosis of iniencephaly apertus and craniorachischisis at 13 weeks, menstrual age. J Clin Ultrasound 1993;2:127
- Lemire, RJ, Beckwith, B, Shepard TH. Iniencephaly and anencephaly with spinal retroflexion, a comparative study of eight human specimens. Teratology 1972;6:27-36
- Schram JHN, Krenning RA, Olthof R, et al. A case of iniencephaly. Ned Tijdschr Geneeskd 1980; 124:1108-11
- Gilmour JR. The essential identity of Klippel-Feil syndrome and iniencephaly. J Pathol 1941 ;53:117-31
- Streeter GL. developmental horizons in human embryos. Age groups XI to XXIII. Embryology reprint Vol. II, Carnegie Inst. Wash.
 , Washington DC, 1951
, Washington DC, 1951 - Katz VL, Aylsworth AS, Albright SG. Iniencephaly is not uniformly fatal. Prenat Diagn 1989;9:595-9
Ultrasound machine HS40
Top seller in the high class. High definition 21.5" monitor, advanced cardio package (Strain+, Stress Echo), OB/GYN 3D expert capabilities (STIC, Crystal Vue, 5D Follicle), high density transducers.
Anencephaly - intrauterine fetal malformation
09/10/2021
This is one of the malformations of the central nervous system collectively referred to as neural tube defects.
The disease is easily manifested at birth due to the absence of the skull and scalp and the effect on the brain . The condition is also called
acrania (absence of the skull) and acephaly (absence of the head). In the most severe form, the entire skull and scalp are missing.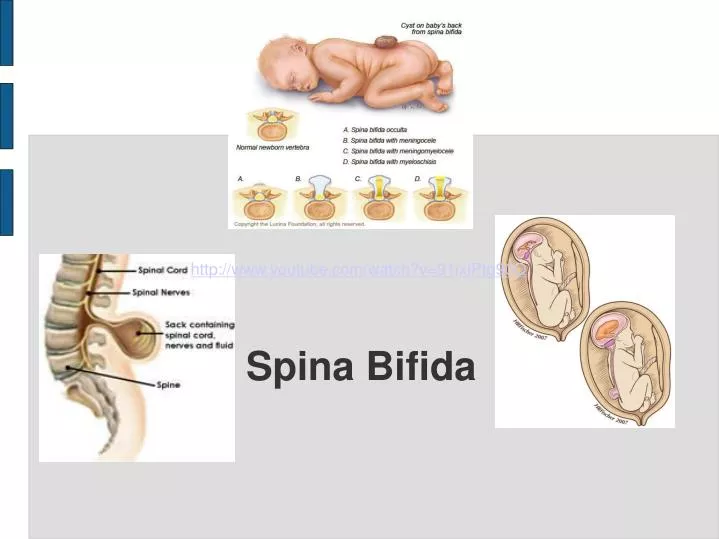
In some cases, called meroacrania or merodisease, part of the skull may be present. In most cases
the disease occurs as an isolated congenital defect with other organs and tissues of the body forming correctly.
In about 10% of cases, other malformations coexist with anencephaly.
Demographics
The disease occurs in all races and ethnic groups. Prevalence rates range from less than one per 10,000 births
(European countries) to over 10 per 10,000 births (Mexico, China).
Causes and symptoms.
As an isolated defect, the disease appears to be caused by a combination of genetic and environmental factors that predispose
to the malformation of the nervous system . The specific genes and environmental factors that contribute to this multifactorial
causality are not fully understood. It is known that nutritional deficiency, especially folic acid deficiency,
is one of the predisposing environmental factors, and that mutations in the genes involved in the metabolism of such a necessary for
development of folic acid are genetic risk factors. The risk of recurrence after the birth of a child with anencephaly is 3-5%.
The risk of recurrence after the birth of a child with anencephaly is 3-5%.
May be disease or other neural tube defect such as spina bifida . The disease is easily manifested at birth due to
effects on parts of the brain . Not only is 's brain distorted, but it is also damaged due to the absence of an overlying protective sheath.
Diagnosis
The disease is diagnosed by observation. Prenatal diagnosis can be performed by ultrasound after
12-14 weeks of pregnancy . Prenatal diagnosis of the disease can also be carried out by screening for alpha-fetoproteins in the mother's blood serum
. The level of alpha-fetoprotein in maternal blood is elevated due to leakage of this fetal protein into the amniotic fluid.
No treatment. A pregnant woman or couple expecting a child with anencephaly needs supportive care and,
perhaps some additional psychological support as they face the inevitable death of their infant, usually before or
shortly after birth.