Different types of rashes on children
Skin rashes in children - Injuries & first aid
Childhood rashes are common and aren't usually a cause for concern. Most rashes are harmless and disappear without the need for treatment.
However, see your GP if your child has a rash and seems unwell, or if you're worried. They'll be able to investigate the cause and recommend any necessary treatment.
This page may give you a better idea about what could be causing the rash, but don't use this to self-diagnose your child's condition – always see a GP for a proper diagnosis.
The most common causes of rashes in children are:
- cellulitis
- chickenpox
- eczema
- erythema multiforme
- hand, foot and mouth disease
- impetigo
- keratosis pilaris ("chicken skin")
- measles
- molluscum contagiosum
- pityriasis rosea
- prickly heat
- psoriasis
- ringworm
- scabies
- scarlet fever
- slapped cheek syndrome
- urticaria (hives)
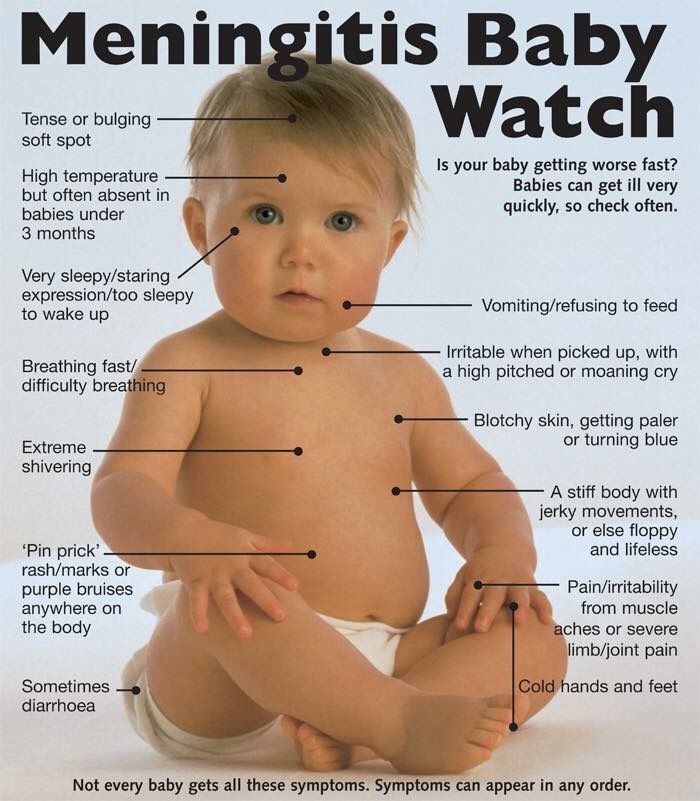
Although meningitis has become less common over recent years, it's important to be aware of the rash and the other signs and symptoms of meningitis.
Cellulitis
Cellulitis is an infection of the deeper layers of skin and underlying tissue. The affected area will be red, painful, swollen and hot. It often affects the legs, but can occur anywhere on the body. Your child will probably also have a fever.
See your GP immediately if an area of your child's skin suddenly turns red, hot and tender. If you can't see your GP on the same day, go to a walk-in centre or minor injuries unit.
Cellulitis can usually be diagnosed by assessing the symptoms and examining the skin. It usually responds well to treatment with antibiotics.
Chickenpox
Chickenpox is a viral illness that most children catch at some point. It most commonly affects children under 10 years of age.
A rash of itchy spots turns into fluid-filled blisters. They crust over to form scabs, which after a while drop off. Some children only have a few spots, whereas others have them over their entire body. The spots are most likely to appear on the face, ears and scalp, under the arms, on the chest and belly, and on the arms and legs.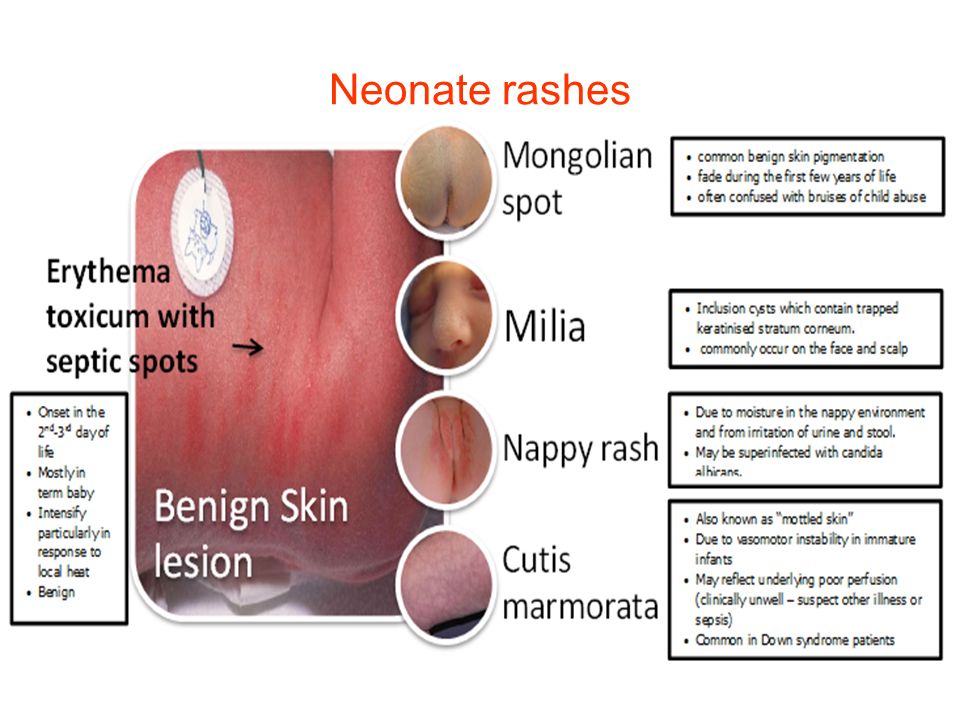
There's no specific treatment for chickenpox, but you can take steps to relieve the symptoms. For example, paracetamol can help relieve fever (don't give aspirin to children under 16), and calamine lotion and cooling gels can be used to ease itching.
Read more about treating chickenpox.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked. The most common type is atopic eczema, which mainly affects children but can continue into adulthood.
Atopic eczema commonly develops behind the knees or on the elbows, neck, eyes and ears. It isn't a serious condition, but if your child later becomes infected with the herpes simplex virus, it can cause the eczema to flare up into an outbreak of tiny blisters called eczema herpeticum, and will cause a fever.
About one in five children in the UK has eczema, and in eight out 10 cases it develops before the age of five, often before a child's first birthday.
Read about treating atopic eczema.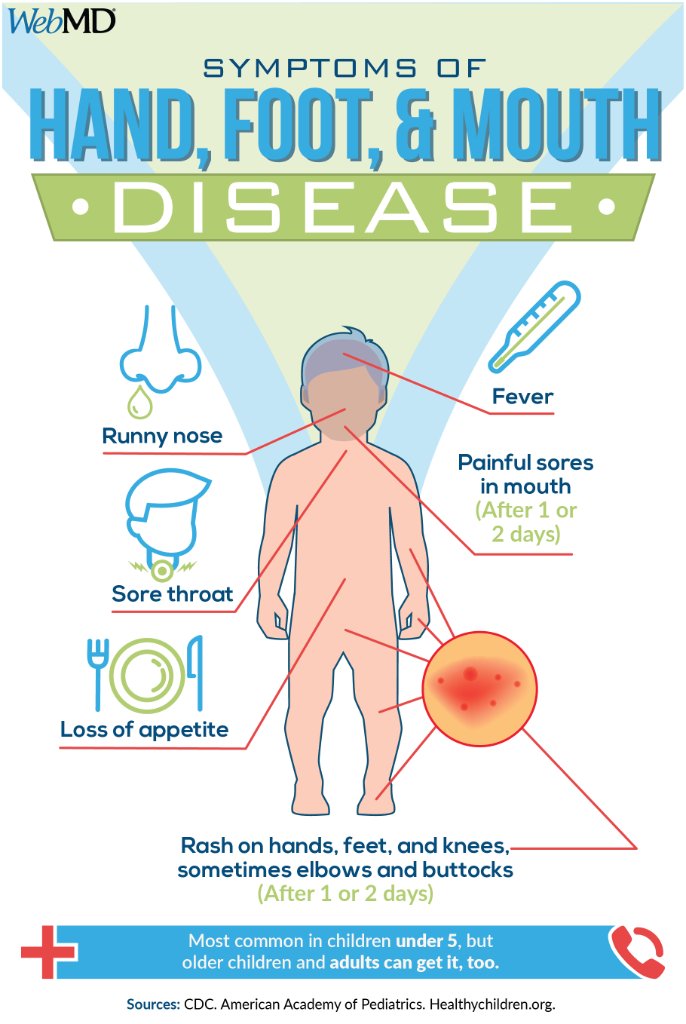
Erythema multiforme
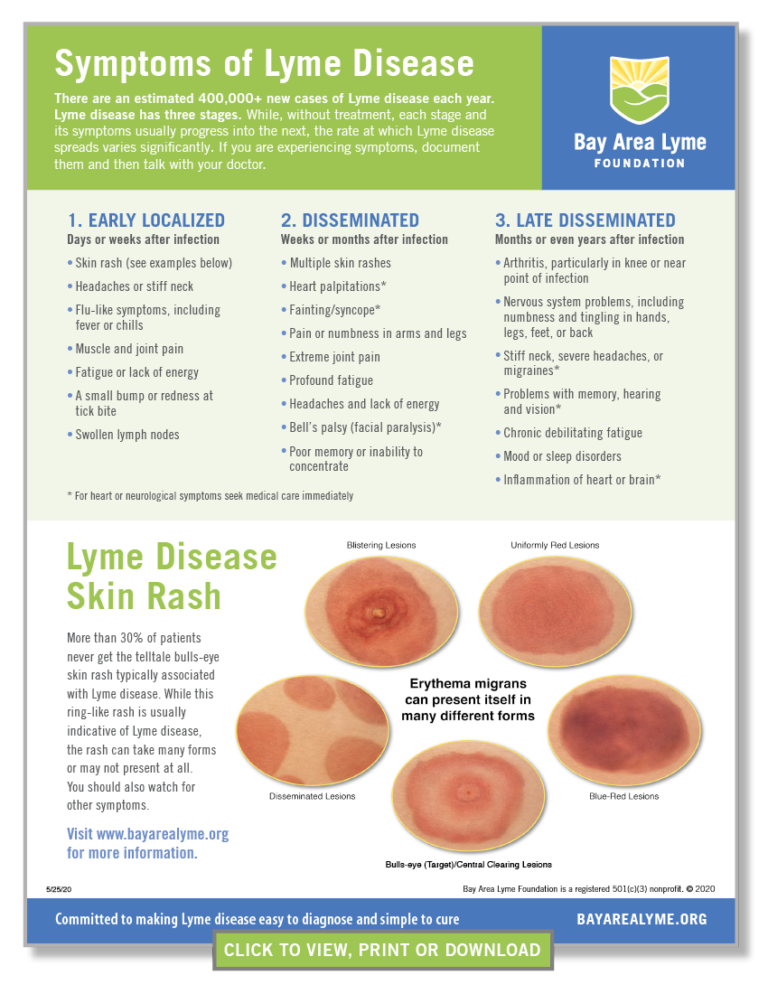
Erythema multiforme is a skin rash (usually mild) that's caused by an allergic reaction to the herpes simplex virus.
The spots look like targets, with a dark red centre and paler ring around the outside. The hands or feet tend to be affected first, followed by the limbs, upper body and face.
Your child will probably feel unwell and may have a fever, which you should be able to treat with over-the-counter medicine. It may take from two to six weeks before they feel better. See your GP if your child has a rash and seems unwell.
In rare cases, erythema multiforme can be triggered by a reaction to certain medications, such as an antibiotic or anticonvulsant. This more severe form is called Stevens-Johnson syndrome and it can be life-threatening.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, contagious infection that causes mouth ulcers and spots and blisters on the palms of the hands and soles of the feet.
It's most common in young children (particularly those under 10), but it can also affect older children and adults.
There's no cure for hand, foot and mouth disease and it's easily spread, so you should keep your child away from school or nursery until they're better. Your child's immune system will fight the virus and it should clear up after about seven to 10 days.
Make sure your child drinks plenty of fluid, and if eating and swallowing is uncomfortable, give them soft foods, such as mashed potatoes, yoghurt and soup.
Impetigo
Impetigo is a common and highly contagious skin infection that causes sores and blisters. It isn't usually serious and often improves within a week of treatment. There are two types of impetigo called non-bullous and bullous.
Non-bullous impetigo typically affects the skin around the nose and mouth, causing sores that quickly burst to leave a yellow-brown crust.
Bullous impetigo typically affects the trunk (the area of the body between the waist and neck), and causes fluid-filled blisters that burst after a few days to leave a yellow crust.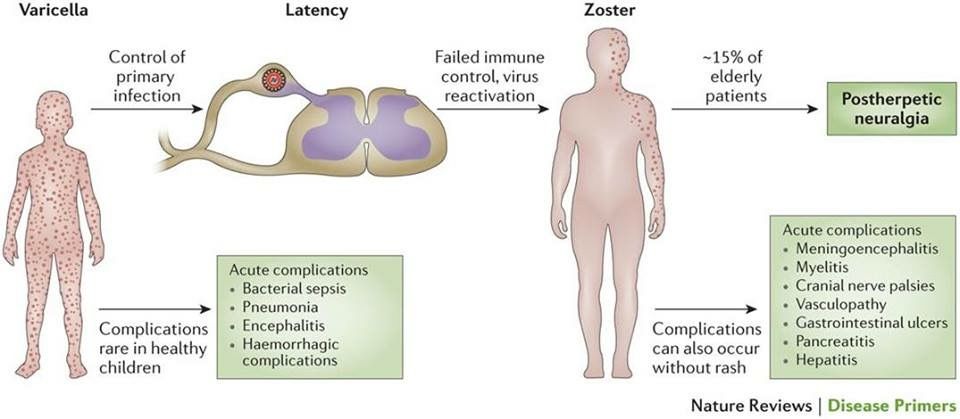
See your GP or pharmacist if you think your child has impetigo. Antibiotics, in the form of a cream or tablets, will be prescribed. This should reduce the length of the illness to around seven to 10 days.
Keratosis pilaris ("chicken skin")
Keratosis pilaris is a common and harmless skin condition. The skin on the back of the upper arms becomes rough and bumpy, as if covered in permanent goose pimples. Sometimes, the buttocks, thighs, forearms and upper back can also be affected.
Keratosis pilaris typically begins in childhood and gets worse during puberty. Some people find it improves after this and may even disappear in adulthood.
There's no cure for keratosis pilaris, and it often gets better on its own without treatment. However, there are some measures you can take that may improve your child's rash, such as using non-soap cleansers rather than soap, and an emollient to moisturise their skin. Your GP or pharmacist will be able to recommend a suitable cream.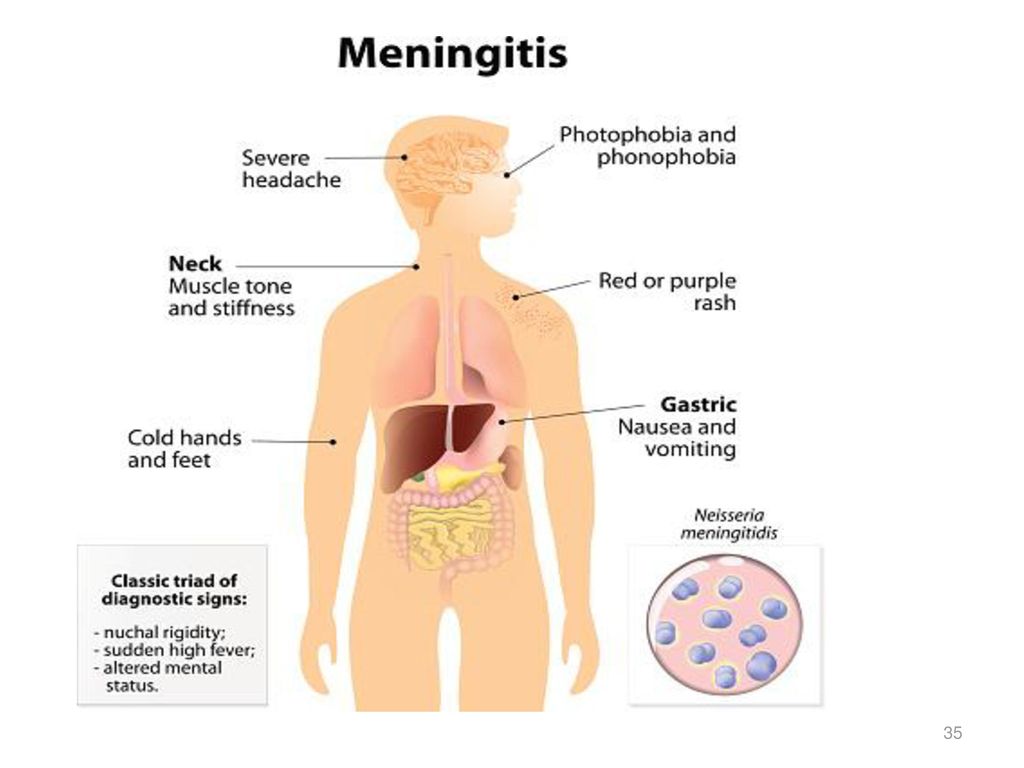
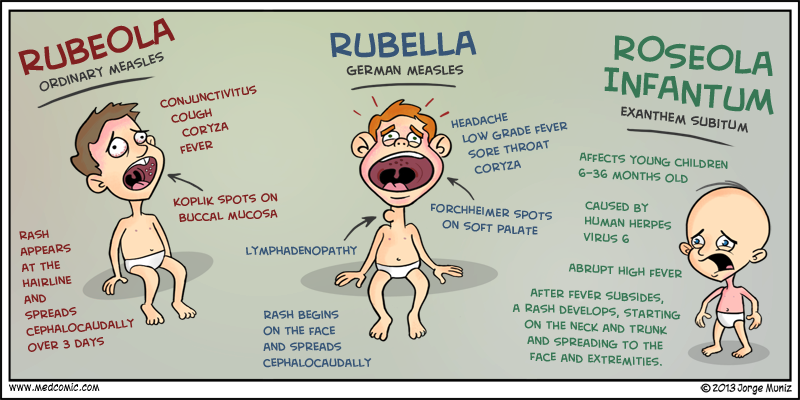
Measles
Measles is a highly infectious illness that most commonly affects young children. It's now rare in the UK because of the effectiveness of the measles, mumps and rubella (MMR) vaccine.
The measles rash is red-brown blotches. It usually starts on the head or upper neck and then spreads outwards to the rest of the body. Your child may also have a fever and cold-like symptoms.
Call your GP surgery immediately if you think your child has measles. It's best to phone before visiting because the surgery may need to make arrangements to reduce the risk of spreading the infection to others.
Measles usually passes in about seven to 10 days without causing further problems. Paracetamol or ibuprofen can be used to relieve fever, aches and pains (don't give aspirin to children under 16). Also, make sure your child drinks plenty of water to avoid dehydration.
Read more about treating measles.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that causes clusters of small, firm, raised spots to develop on the skin.
It commonly affects young children aged one to five years, who tend to catch it after close physical contact with another infected child.
The condition is usually painless, although some children may experience some itchiness. It usually goes away within 18 months without the need for treatment.
Molluscum contagiosum is highly infectious. However, most adults are resistant to the virus, which means they're unlikely to catch it if they come into contact with it.
Pityriasis rosea
Pityriasis rosea is a relatively common skin condition that causes a temporary rash of raised, red scaly patches to develop on the body. Most cases occur in older children and young adults (aged between 10 and 35).
The rash can be very itchy. In most cases, it clears up without treatment in 2 to 12 weeks, although in rare cases it can last up to five months.
Emollients, steroid creams and antihistamines can be used to help relieve the itchiness. The rash doesn't usually leave scars, although the skin can sometimes be discoloured afterwards.
Prickly heat (heat rash)
Prickly heat (heat rash), also known as miliaria, is an itchy rash of small, raised red spots that causes a stinging or prickly sensation on the skin.
It occurs when the sweat ducts in the outer layer of skin (epidermis) are obstructed. You can get a heat rash anywhere on your body, but the face, neck, back, chest or thighs are most often affected.
Infants can sometimes get a prickly heat rash if they sweat more than usual – for example, when it's hot and humid or if they're overdressed. It isn't a serious condition and rarely requires any specific treatment.
Psoriasis
Psoriasis is a long-lasting (chronic) skin condition that causes red, flaky, crusty patches of skin covered with silvery scales.
The severity of psoriasis varies greatly from person to person. For some people, it's just a minor irritation, but for others it can have a major impact on their quality of life.
There's no cure for psoriasis, but there are a number of treatments that can help improve the symptoms and appearance of skin patches.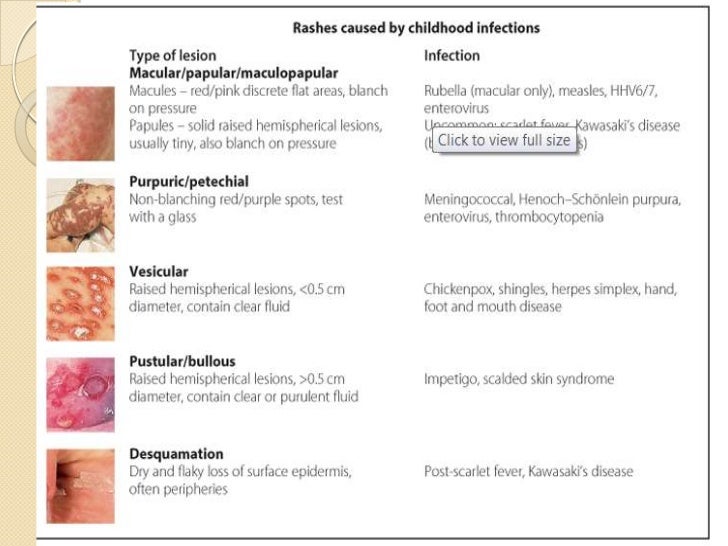 For example, topical corticosteroids are creams and ointments that can be applied to the skin.
For example, topical corticosteroids are creams and ointments that can be applied to the skin.
Ringworm
Ringworm is a highly infectious fungal skin infection that causes a ring-like red or silvery patch on the skin that can be scaly, inflamed or itchy.
Ringworm often affects the arms and legs, but it can appear almost anywhere on the body. Other similar fungal infections can affect the scalp, feet, groin and nails.
Ringworm can usually be easily treated with antifungal medicines, which are available from a pharmacy. Ringworm of the scalp can cause scaling and patches of hair loss. It's treated with antifungal tablets, often combined with antifungal shampoo.
Scabies
Scabies is a contagious skin condition that's intensely itchy. It's caused by tiny mites that burrow into the skin.
In children, scabies is usually spread through prolonged periods of skin-to-skin contact with an infected adult or child – for example, during play fighting or hugging.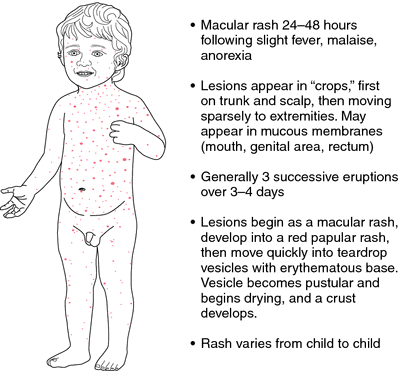
The mites like warm places, such as skin folds, between the fingers, under fingernails, or around the buttock creases. They leave small red blotches, which are often found on the palms of the hands or soles of the feet. In infants, blisters are commonly found on the soles of the feet.
See your GP if you think your child has scabies. It's not usually a serious condition, but it does need to be treated. Your GP will prescribe a lotion or cream. Read more about treating scabies.
Scarlet fever
Scarlet fever is a highly contagious bacterial infection that usually affects children between two and eight years of age. It causes a distinctive pink-red rash, which feels like sandpaper to touch and may be itchy.
It often starts with a sore throat, fever and headache, with the rash developing two to five days after infection. The rash usually occurs on the chest and stomach before spreading to other areas of the body, such as the ears and neck.
Scarlet fever usually clears up after about a week, but see your GP if you think your child may have it.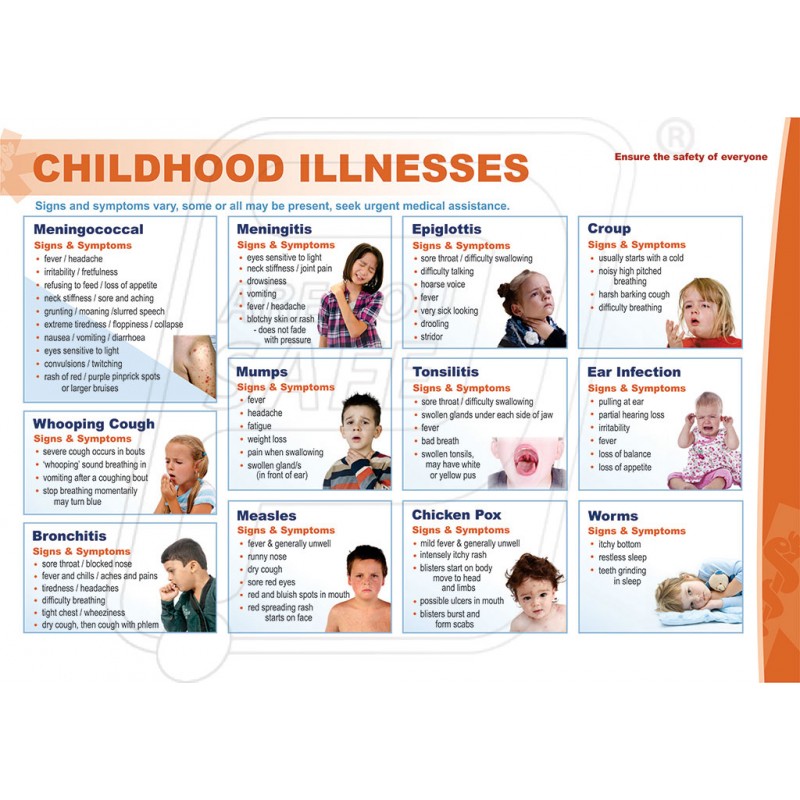 Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Slapped cheek syndrome
Slapped cheek syndrome – also known as fifth disease or parvovirus B19 – is a viral infection that's common in children aged six to 10.
It causes a distinctive bright red rash to develop on both cheeks. This can look alarming, but it usually clears up by itself in one to three weeks.
Unless your child is feeling unwell, they don't need to stay away from school. Once the rash appears, the infection is no longer contagious. However, it's a good idea to notify your child's school about the infection.
Urticaria (hives)
Urticaria – also known as hives, weals, welts or nettle rash – is a raised, itchy rash that can affect one part of the body or be spread across large areas. It's a common skin reaction that often affects children.
Urticaria occurs when a trigger causes high levels of histamine and other chemical messengers to be released in the skin.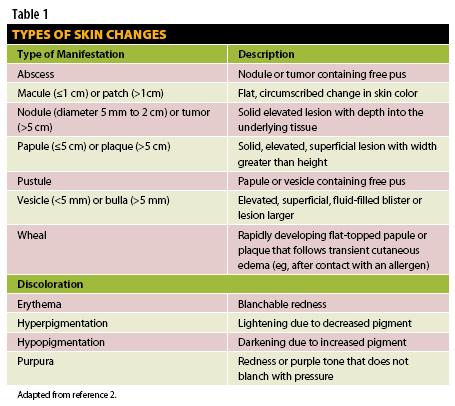 These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
There are many possible triggers of urticaria, including allergens, such as food or latex, irritants, such as nettles, medicines, and physical factors, such as heat or exercise. Sometimes, a cause can't be identified.
The rash is usually short-lived and mild, and can often be controlled with antihistamines.
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
Treating nappy rashIf your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.

- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.
- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.
Other rashes in the nappy areaIf the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
Skin rash in children: analyze the causes
Features of children's skin
The skin, like most other organs and systems, gradually develops until puberty. In a child, it is functionally and structurally more sensitive to external influences and allergic reactions. At the same time, the sweat and sebaceous glands do not yet work properly, which is associated with insufficient development of skin innervation.
At the same time, the skin from birth takes an active part in metabolism and respiration due to the many superficially located vessels. Because of this, skin diseases often greatly affect the general condition of the child.
Types of rash in children
Skin rash caused by a particular disease usually has its own characteristics. The most common types of rashes include:
- Papules.
 These are volumetric formations of a small size (up to 10 mm), which rise above the skin. The main color is red and pink. Occurs with lichen planus, roseola infantum, atopic dermatitis, etc.
These are volumetric formations of a small size (up to 10 mm), which rise above the skin. The main color is red and pink. Occurs with lichen planus, roseola infantum, atopic dermatitis, etc. - Vesicles. They are bubbles up to 5 mm in diameter, filled with a cloudy liquid. After opening, erosion is often left behind. May be a sign of chickenpox and other herpes infections.
- Petechiae. A purplish skin eruption that does not go away with pressure. Its elements do not exceed 3 mm in diameter, do not rise above the skin and are not felt to the touch. As a rule, they indicate meningococcal infection, vascular damage (vasculitis), platelet deficiency.
- Erosion. This is a skin defect that does not penetrate deeper than the epidermis. It has the appearance of a rounded, somewhat in-depth formation of red color with a weeping surface.
- Peel. A secondary element formed by the drying of secretions from vesicles, erosions, or blood. Solid, has a dark red, brown color.
- Macula or spot. This is an area of discoloration that is on the same level as adjacent areas of the skin. It can be both an independent element in rubella, measles, roseola, and a residual phenomenon after papules, vesicles or erosions.
- Wheals or urticaria. A rounded element of a rash of pale pink, red or purple-white color, the size of which varies from 1-2 mm to tens of centimeters. Leaves no secondary elements behind. Meet with allergic reactions, urticaria.
- Lichenification. These are areas of excessive thickening of the skin with increased skin pattern. Often a secondary element.
Diseases that cause skin rashes in children
Baby skin rashes can indicate various diseases, most often infections and allergic reactions.
Roseola infantum
Roseola infantum or sudden exanthema is a childhood infectious disease that occurs when infected with human herpesviruses type 6 or 7. Most often observed between the ages of 6 months and 2 years.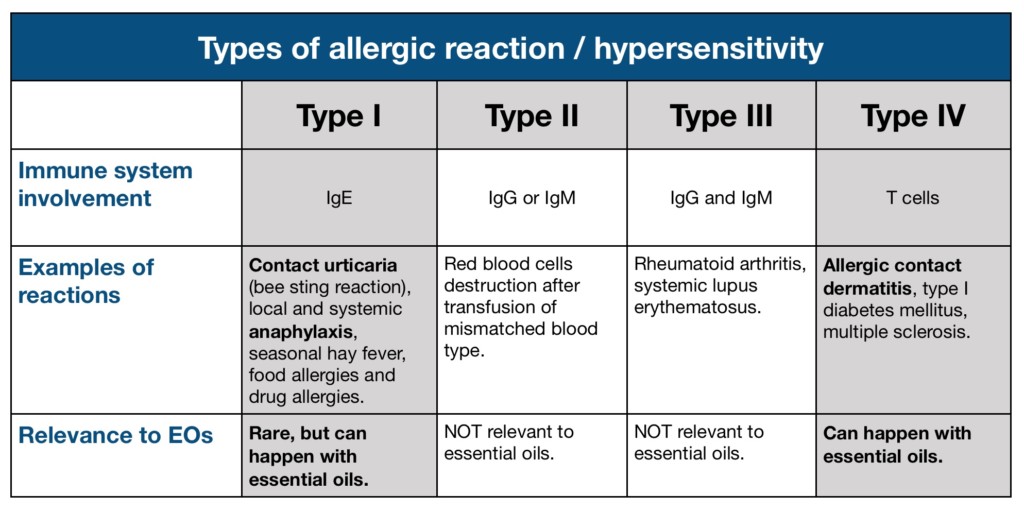
Sudden exanthema is accompanied by an increase in body temperature up to 39-40°C, which persists for 3-5 days, after which a bright red maculopapular rash appears on the child's skin. It occurs on the surface of the chest and abdomen, spreading throughout the body (Fig. 1). The elements of the rash, as a rule, are not felt by the fingers, but sometimes they can be raised. They disappear when the skin is stretched or when the glass of a glass is pressed on them.
In roseola infantum there may be white rings around some elements of the rash. Often the rash is limited only to the trunk and, not having time to reach the face and limbs, disappears. The rash does not cause discomfort or itching, but children usually become sharply capricious and "unbearable" during this time; the rash lasts from several hours to several days, and then disappears, leaving no pigmentation or peeling. An excerpt from the book by Sergei Butriy “Child health: a modern approach. how to learn to cope with illness and your own panic.
Roseola infantum should be treated symptomatically, preferably with antipyretics and plenty of fluids. In immunodeficiency states (HIV infection, congenital disorders of the immune system), antiherpetic drugs are additionally prescribed.
Figure 1. Rash in roseola infantum. Source: WikipediaNo matter how hard baby roseola flows, it is perfectly safe. Complications are extremely rare and are usually limited to febrile convulsions. An excerpt from the book by Sergei Butriy “Child health: a modern approach. how to learn to cope with illness and your own panic.
Enteroviral exanthems: chicken pox and enteroviral pharyngitis
The viral pemphigus, also known as turkish varicella, is caused by enterovirus 71 (EV-71). Enteroviral pharyngitis is caused by Coxsackie A16, B2, B5 viruses. They occur mainly among children under the age of 10 years, infection often occurs during holidays in southern countries.
The primary signs of pathologies are pain in the mouth and throat, because of which the child refuses to eat and does not even swallow saliva, but spits it out. Then the body temperature rises to 39°C. The fever persists for about 4 days and is accompanied by nausea and vomiting, loss of appetite and excessive irritability. With enteroviral pharyngitis, small white sores usually occur only on the palatine arches (Fig. 2), but Turkish chickenpox is a rash throughout the mouth, including the tongue, around the mouth, on the palms and feet. The rash on the skin may resemble chickenpox - red spots or blisters.
Figure 2. Rashes in the mouth with herpangina (enteroviral pharyngitis). Source: James Heilman, MD/Wikipedia
Symptomatic treatment:
- Oral hygiene and rinsing with antiseptic solutions.
- Non-steroidal anti-inflammatory drugs (NSAIDs) that help control pain while lowering body temperature.
- Plentiful warm fluids to prevent dehydration, cold drinks and ice cream may be given (these are more easily tolerated by sick children).
- Diet with the exception of mechanically hard, sour and salty foods.
- Enteroviral exanthems are self-limiting, the disease usually recedes after 3-7 days. However, the condition of the child during the illness must be monitored in order to consult a doctor in time in case of complications. The most common are dehydration and secondary bacterial infections. In the latter case, abscesses, yellow crusts appear on the skin, the skin swells. Rarely enterovirus infection leads to serous meningitis.
Chickenpox
Chickenpox or chickenpox is an infectious disease caused by the human herpesvirus type 3 (Varicella Zoster). People of any age get sick with it, but mostly it is children 5-9years.
The main symptom is skin rashes that have a certain sequence of development. Small pink spots appear first, quickly transforming into papules, and then into vesicles (Fig. 3) with reddening around. After a couple of days, they open or dry out, forming crusts of dark red, brown color on their surface.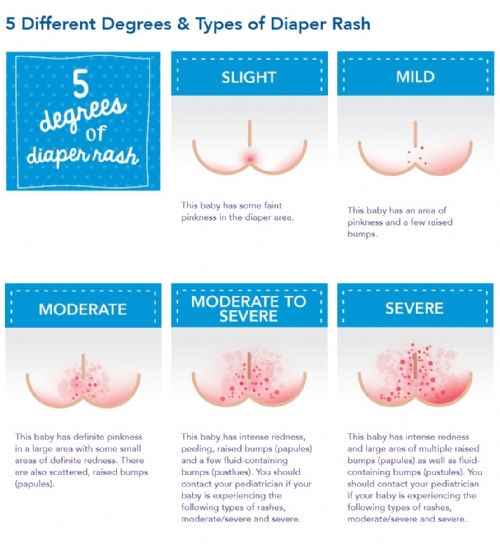 A characteristic feature is severe itching.
A characteristic feature is severe itching.
The total period of rashes lasts from 2 to 9days. At the same time, the general condition practically does not suffer, but fever may occur.
There are no drugs that can completely eliminate the virus, so the treatment tactics are aimed at eliminating the symptoms and normalizing the child's condition:
- Bed rest in the presence of fever.
- Treatment of elements of the rash with a solution of manganese, methylene blue or brilliant green (brilliant green).
- Antihistamines for itching.
- Antipyretics.
- Taking regular warm showers without using a washcloth or brush.
Complications of chickenpox occur against the background of suppression of the body's immune system. These include: inflammation of the lungs (pneumonia), lesions of the nervous system (neuralgia, meningitis, encephalitis, damage to the facial nerve), eyes (keratitis, conjunctivitis, uveitis), etc.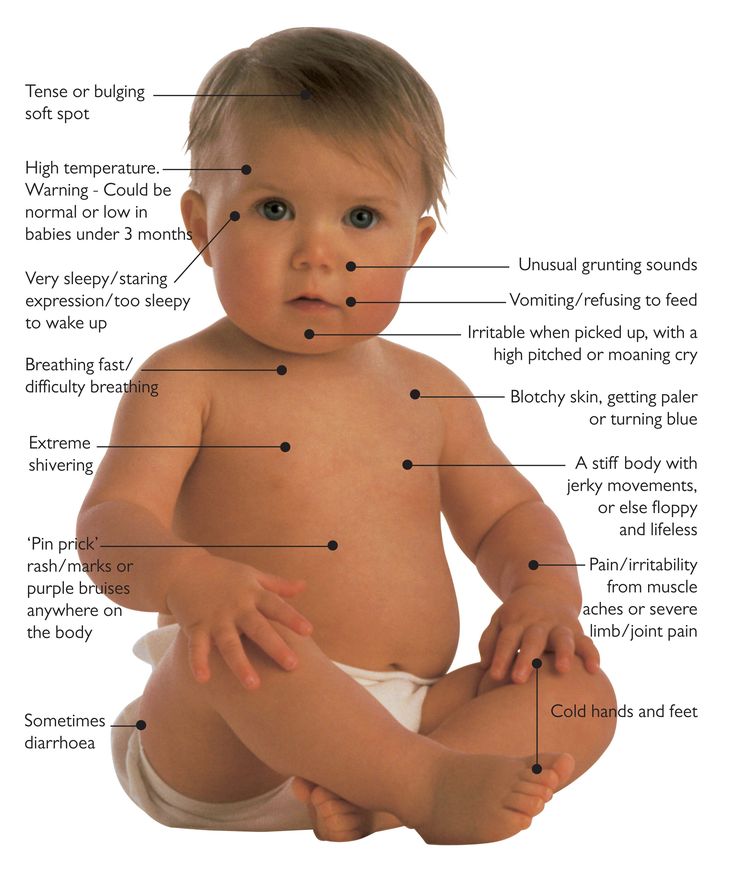
Important ! For the prevention of chickenpox, especially for adults, against the background of a weakened immune system and a high risk of complications, vaccination is recommended. It can also be carried out as an emergency prophylaxis up to 2 days from the moment of contact with a sick person.
Measles
Measles is a viral infectious disease. Often it occurs in unvaccinated children from 2 to 5 years and older.
Measles debuts with a sharp rise in temperature to 39-40°C, dry cough, runny nose, headache, hoarseness. Characteristic features are swelling and redness of the eyelids, pharynx and red spots in the sky. On the 2-3rd day of development, a symptom specific to measles occurs - Filatov-Belsky-Koplik spots. These are white spots with a red border, observed on the inner surface of the cheeks near the molars. On the 4-5th day from the appearance of the first signs of the disease, these spots disappear, and they are replaced by a skin rash.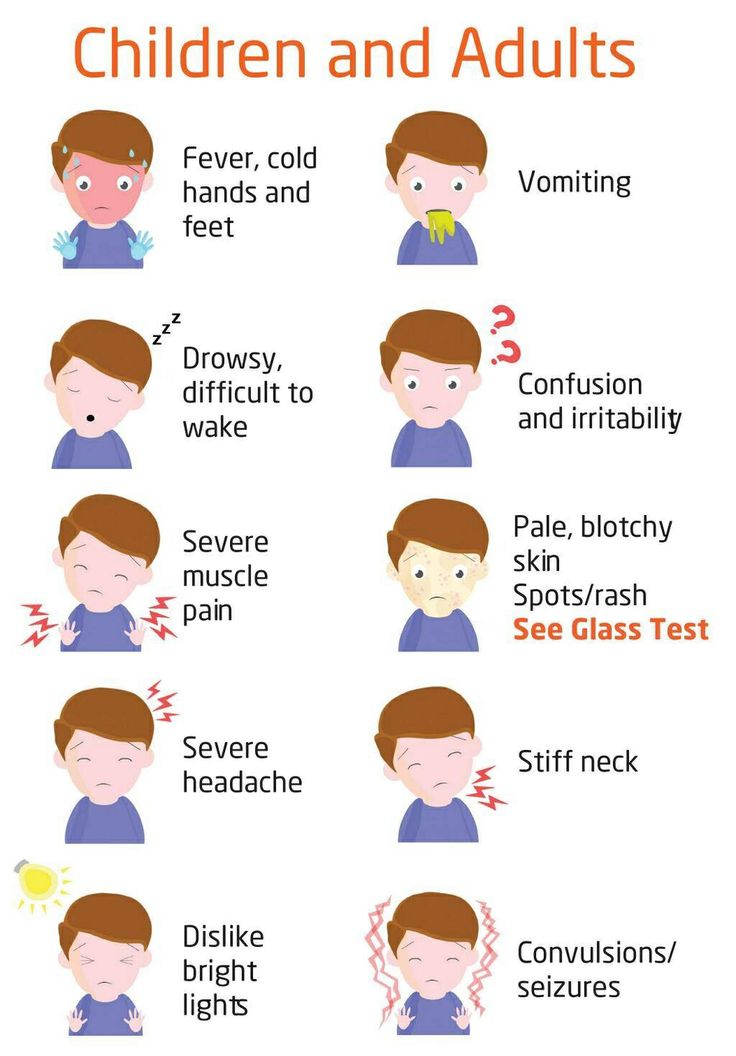
The primary localization of measles papular rash is the outer surface of the elbow, knees, fingers. Further, it spreads throughout the body (Fig. 4). The elements of the rash are surrounded by red spots and tend to merge with each other. After 4 days from the moment they appear, the child's condition returns to normal, and the elements of the rash become darker and peel off. Residual effects and pigmentation disappear after 7-10 days.
Figure 4. Skin rash in measles. Source: CDC
There is no specific treatment for measles; helping a child involves managing individual symptoms:
- NSAIDs to reduce body temperature.
- Expectorants for relief of coughs.
- Antiseptic mouth rinses.
- Topical treatment of rash elements with astringents or tea to relieve itching and soreness.
Measles is very dangerous. Possible complications of measles:
- Stenosis of the larynx - croup.
- Primary measles or secondary bacterial pneumonia.
- Inflammation of the respiratory tract - bronchitis, tracheitis, laryngitis, pharyngitis.
- Otitis media.
- Hepatitis.
- Encephalitis and subacute sclerosing panencephalitis.
Scarlet fever
Scarlet fever is a bacterial infection caused by group A beta-hemolytic streptococcus. Most cases occur in children between 3 and 7 years of age.
The first manifestation of scarlet fever is an intoxication syndrome - an increase in body temperature up to 38-39°C, headache, general weakness and loss of appetite. On the 2-4th day from the moment the first signs of the disease appear, one of the characteristic symptoms appears - "crimson tongue" (Fig. 5). It is manifested by pronounced graininess and bright red color of the surface. Angina also occurs - inflammation of the palatine tonsils.
Figure 5. Crimson tongue in scarlet fever. Source: ResearchGate
From the first days of scarlet fever, a characteristic red punctate rash appears, which does not disappear when pressed with glass, but becomes yellowish with effort.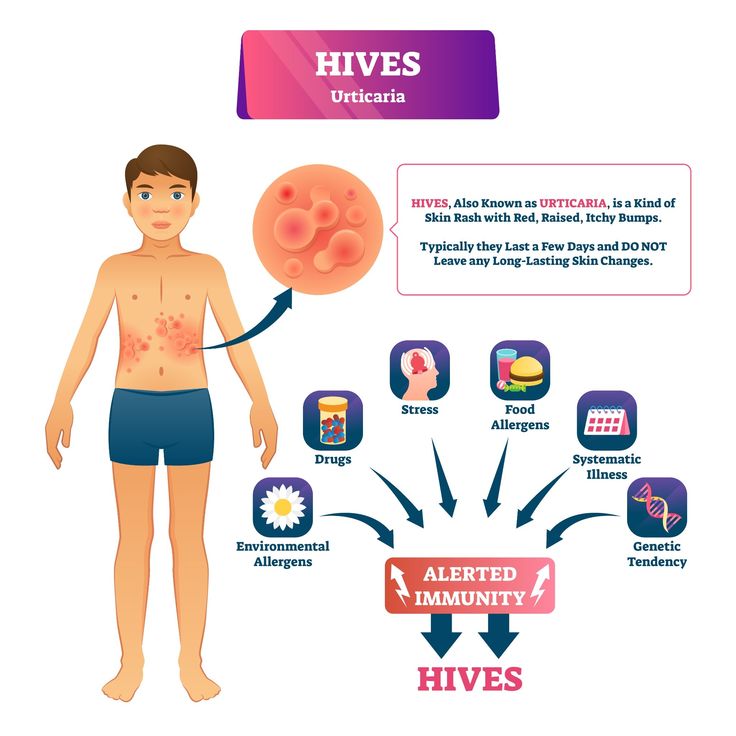 It is located on the flexion surfaces: the inner parts of the elbows, under the knees, in the inguinal pits, on the cheeks and sides of the body. It lasts up to 1 week, after which it disappears, leaving no pigmentation behind. A specific sign is the pallor of the nasolabial triangle.
It is located on the flexion surfaces: the inner parts of the elbows, under the knees, in the inguinal pits, on the cheeks and sides of the body. It lasts up to 1 week, after which it disappears, leaving no pigmentation behind. A specific sign is the pallor of the nasolabial triangle.
Another characteristic feature of scarlet fever is the peeling of the skin that occurs after the rash has disappeared. At the same time, the skin "moves away" in whole layers in the area of the palms and feet, while in other areas - in small fragments.
Treatment is based on antibiotics from the penicillin group. Vitamin C and B vitamins, symptomatic preparations are used as adjuvants. Plentiful warm drink and bed rest are recommended. In severe cases, glucocorticosteroids and intravenous drip of glucose solutions and plasma substitutes are used.
The most common complications of scarlet fever: otitis media, sinusitis and frontal sinusitis (inflammation of the maxillary and frontal paranasal sinuses, respectively), cervical lymphadenitis (inflammation of the lymph nodes of the cervical region).
Rubella
Rubella is caused by Rubella virus. The majority of patients are children aged 3 to 9 years.
Rubella begins with an intoxication syndrome of moderate severity: fever up to 38-38.5°C, headache and increased fatigue, signs of pharyngitis and conjunctivitis, pronounced enlargement of the lymph nodes of the cervical and occipital region.
After 1.5-2 days from the onset of the disease, a skin rash appears in the form of spots, which spreads downward over several hours - appearing on the face, gradually moving to the trunk and limbs. Outwardly, the rash initially resembles measles, then scarlet fever. Itching and peeling are absent, and the spots, unlike measles, do not merge with each other. The bulk of the spots are located on the buttocks and lower back, the outer surface of the elbows and knees. After 3-5 days, the rash disappears without a trace.
There is no specific treatment for rubella, and the main actions are aimed at eliminating individual symptoms of the disease.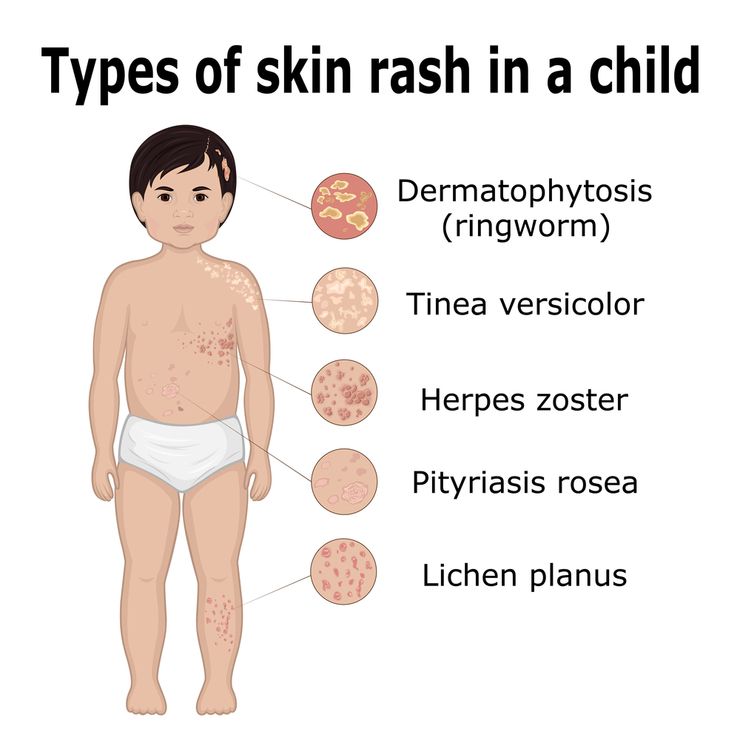 Complications are very rare, as a rule - against the background of disorders of the immune system. In such cases, the development of pneumonia, arthritis, otitis media is possible.
Complications are very rare, as a rule - against the background of disorders of the immune system. In such cases, the development of pneumonia, arthritis, otitis media is possible.
Important ! Rubella is especially dangerous for pregnant women, as it causes problems in the fetus, so when planning a pregnancy, all unvaccinated people should be vaccinated against this infection.
Urticaria
Urticaria or urticaria is a type of dermatitis caused by allergies. The disease is very common among both children and adults. In total, about 20% of the adult population and 2-7% of children suffer from it.
Medications (most often antibiotics), various foods, vaccines and physical influences: cold, sunlight, mechanical pressure can provoke the development of urticaria.
The leading symptom of the pathology is a skin rash in the form of dense red or pink vesicles or nodules 2-10 mm in diameter with clear edges, which become pale when pressed (Fig. 6). A characteristic feature is the sudden appearance and equally rapid disappearance of the elements of the rash without a trace, as well as severe itching.
6). A characteristic feature is the sudden appearance and equally rapid disappearance of the elements of the rash without a trace, as well as severe itching.
Treatment, depending on the form of the disease, is represented by antihistamines, histamine receptor blockers or glucocorticosteroids.
Complications occur in the absence of treatment and include angioedema, anaphylactic shock, heart and kidney damage in the form of myocarditis or glomerulonephritis, respectively.
Lichen planus
Lichen planus is a chronic dermatitis of unknown origin. Most of the patients are people aged 30 to 60 years. However, about 5% of the total number of patients are children.
A typical form of the disease is accompanied by the appearance of gray-white papules up to 2 mm in diameter on the oral mucosa, namely: the inner surface of the cheeks behind the molars, on the lateral parts of the tongue and on the palate.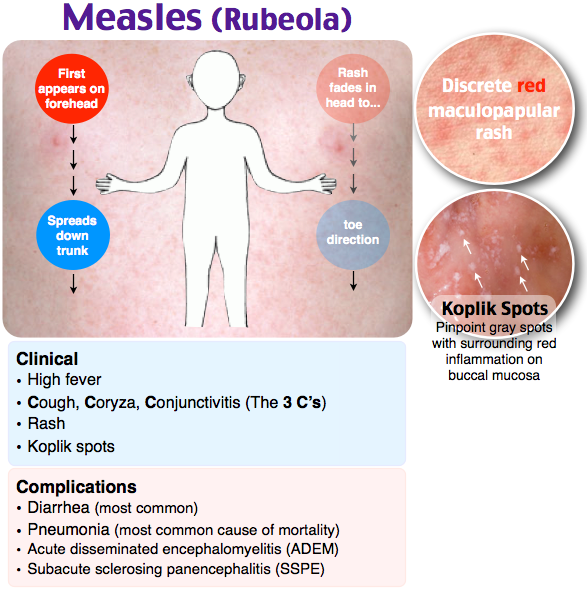 Sometimes the rashes can merge, forming patterns.
Sometimes the rashes can merge, forming patterns.
In some patients, a rash also appears on the skin of the flexor surfaces of the limbs of the arms and legs, the inner thighs. It has the appearance of small papules of various shapes and pinkish-purple color with a shiny surface and a depression in the center.
Treatment includes a diet with restriction of salt, smoked and fried foods, rough, irritating mucous membranes food. Glucocorticosteroids are prescribed as medical support.
Pityriasis rosea
Pityriasis rosea, or Gibert's versicolor, is a variant of a skin lesion with no known cause. Exacerbations occur against the background of immune suppression - colds, hypothermia, chronic stress, etc. Most cases of this pathology are observed in people aged 20 to 40 years, as well as in adolescents.
The disease begins with the formation of a primary scaly focus of pinkish or yellowish color from 1 to 10 cm in diameter with a clear rim. After 1-2 weeks, secondary plaques and smaller papules appear on the body and limbs - up to 2 cm (Fig.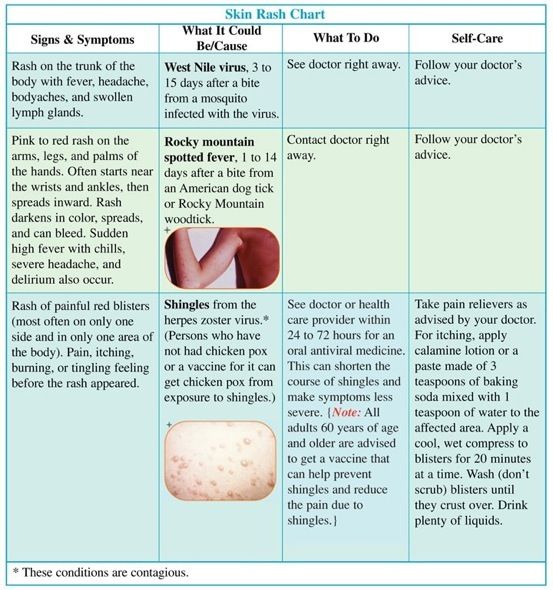 7). Gradually, the elements of the rash turn pale, and the outer edge becomes rougher. The rash may be accompanied by itching, fever and other manifestations of the intoxication syndrome.
7). Gradually, the elements of the rash turn pale, and the outer edge becomes rougher. The rash may be accompanied by itching, fever and other manifestations of the intoxication syndrome.
The disease tends to self-heal within 4-5 weeks. Treatment is mainly local in the form of ointments based on glucocorticosteroids, and antihistamines and NSAIDs are prescribed to combat itching and fever.
Figure 7. Skin rash with rosacea. Source: James Heilman, MD/Wikipedia
Atopic dermatitis
Atopic dermatitis or eczema is a genetically determined inflammatory skin lesion of an autoimmune nature. Most often, children under 14 years of age living in large, industrial cities get sick.
Atopic dermatitis develops with a probability of 80% if both parents have a history of this pathology, and with a 50% probability if only one of them.
The first symptoms occur before the age of 2 years due to exposure to allergens, which can be food, plant pollen, dust and mold, cosmetics.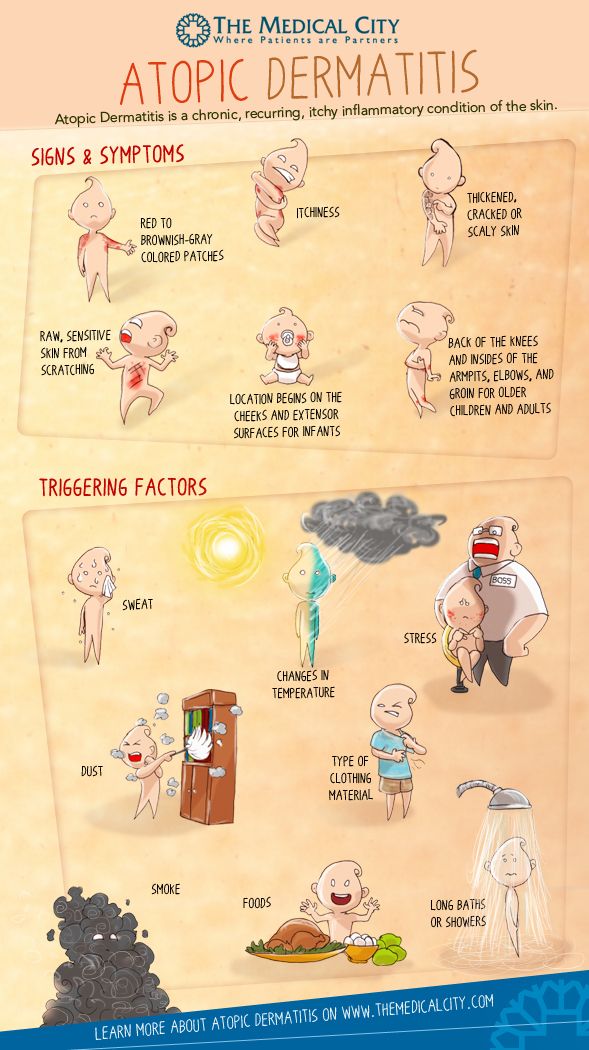
Typical symptoms are skin rashes, which vary depending on the stage of the disease. When exacerbated, red spots, papules and small vesicles appear, accompanied by severe itching. In infants, the typical site is the face, scalp, and neck. At an older age, the flexion surfaces of the limbs and the neck are affected. In the remission stage, they are replaced by foci of increased dryness of the skin, peeling and lichenification. During the year, on average, there are 2-4 exacerbations.
Ointments and creams based on glucocorticosteroids, calcineurin inhibitors, and zinc are used in the treatment. In severe cases, hormonal drugs are used in the form of tablets or intravenous injections. Antihistamines are also used to combat itching.
Infectious mononucleosis
Infectious mononucleosis is the result of infection with human herpesvirus type 4 (Epstein-Barr virus). It is believed that already before the age of 5, about 50% of children become infected with this virus, and its prevalence among adults reaches 95% of the population.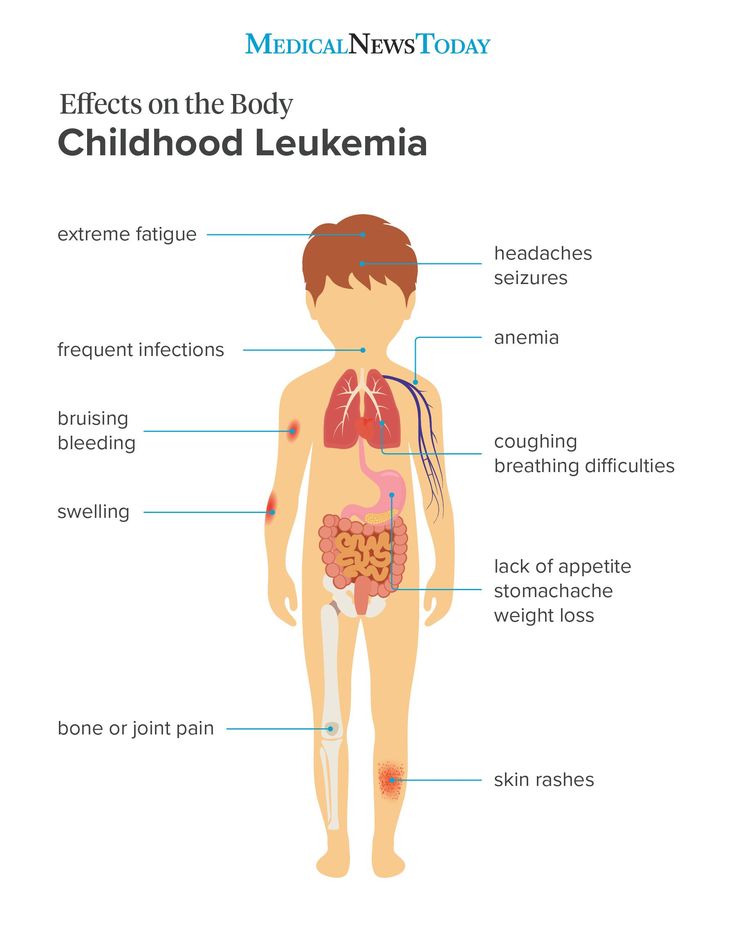 Most often, clinical signs of pathology occur at the age of 14-18 years.
Most often, clinical signs of pathology occur at the age of 14-18 years.
Typical symptoms of infectious mononucleosis include:
- General weakness and malaise.
- Sore throat and pain when swallowing
- Headache.
- Slight increase in body temperature.
- Sensation of aching in muscles and joints.
- Enlargement and soreness of the lymph nodes in the region of the lower jaw and neck.
Skin rash occurs in less than ¼ of patients. Most often, they occur on the 5th-10th day of the course of the disease against the background of the erroneously prescribed antibiotics ampicillin or amoxicillin. The rash is represented by spots and papules and is located in the face, trunk, thighs and shoulders. It is accompanied by swelling of the skin and itching, sometimes peeling. The rash disappears within 5-7 days.
Since mononucleosis is of viral origin, antibiotic therapy is not used against it. Treatment of the disease involves the elimination of individual symptoms.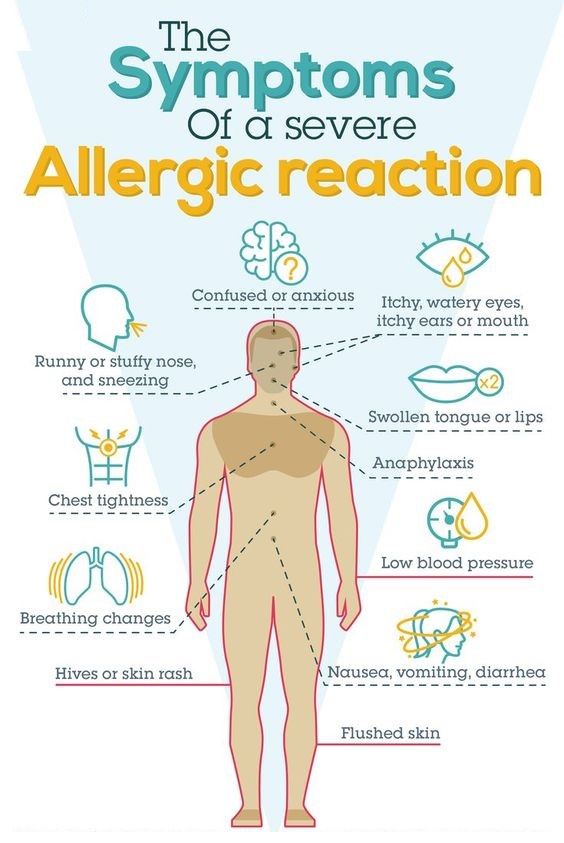 In severe cases and with concomitant immunodeficiency, antiherpetic drugs are prescribed: ganciclovir, valaciclovir.
In severe cases and with concomitant immunodeficiency, antiherpetic drugs are prescribed: ganciclovir, valaciclovir.
Prevention of rashes
In cases of infectious diseases, the only way to avoid rashes is to prevent infection, namely by limiting contact with sick people and practicing basic personal hygiene.
In case of allergic pathologies, it is important to exclude contact with triggers, and if this is not possible, take antihistamines or corticosteroids previously agreed with the attending physician in advance.
A series of recommendations to help avoid skin rashes of other origin for people with sensitive skin:
- Avoid direct skin contact with aggressive, irritating substances such as household chemicals.
- Limit skin exposure to sunlight, cold.
- Give preference to clothing and underwear made from natural fabrics.
- Avoid tight, uncomfortable clothing and mechanically rough objects such as washcloths.
- Use ointments or other skin care products recommended by a dermatologist or esthetician.
Conclusion
Skin rash is an important symptom of many diseases. She can tell you exactly what kind of disease you have to deal with. This, in turn, makes it possible to provide the right assistance before going to the doctor, avoiding mistakes or even coping with the problem on your own.
References
- Federal Clinical Guidelines. Dermatovenereology 2015. Skin diseases. Sexually transmitted infections. - 5th ed. revised and additional - M: Business Express, 2016. - 768 p.
- V.M. Kozin, Yu.V. Kozina, N.N. Yankovskaya "Dermatological diseases and sexually transmitted infections: Educational and methodological manual" - Vitebsk: VSMU, 2016. - 409 p.
- P.D. Walk. "Skin and venereal diseases: Textbook" - Grodno: Grodno State Medical University, 2003. - 182 p.
- Yu.V. Odinets, M.K. Biryukova “Atopic dermatitis, allergic rhinitis, urticaria in children: method.
 decree. for stud. and interns" - Kharkiv: KhNMU, 2015. - 52 p.
decree. for stud. and interns" - Kharkiv: KhNMU, 2015. - 52 p. - S. A. Butriy “Child health: a modern approach. How to learn to cope with diseases and your own panic ”-“ Eksmo ”, 2018.
Rash in a child on body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies.