Pregnancy psychosis treatment
Psychiatric Disorders During Pregnancy
Although pregnancy has typically been considered a time of emotional well-being, recent studies suggest that up to 20% of women suffer from mood or anxiety disorders during pregnancy. Particularly vulnerable are those women with histories of psychiatric illness who discontinue psychotropic medications during pregnancy. In a recent study which prospectively followed a group of women with histories of major depression across pregnancy, of the 82 women who maintained antidepressant treatment throughout pregnancy, 21 (26%) relapsed compared with 44 (68%) of the 65 women who discontinued medication. This study estimated that women who discontinued medication were 5 times as likely to relapse as compared to women who maintained treatment.
High rates of relapse have also been observed in women with bipolar disorder. One study indicated that during the course of pregnancy, 70.8% of the women experienced at least one mood episode. The risk of recurrence was significantly higher in women who discontinued treatment with mood stabilizers (85. 5%) than those who maintained treatment (37.0%).
Although data accumulated over the last 30 years suggest that some medications may be used safely during pregnancy, knowledge regarding the risks of prenatal exposure to psychotropic medications is incomplete. Thus, it is relatively common for patients to discontinue or to avoid pharmacologic treatment during pregnancy.
The New U.S. FDA Pregnancy Labeling and Lactation Rule
In 1975, the U.S. Food and Drug Administration (FDA) provided guidelines to drug companies for labeling medications with regard to their safety during pregnancy. This system of classification used five risk categories (A, B, C, D and X) based on data derived from human and animal studies. While widely used to make decisions regarding the use of medications during pregnancy, many criticized this system of classification, indicating that this type of drug labeling was often not helpful and, even worse, may be misleading.
In an effort to improve the accuracy and usefulness of information regarding the safety of medications used during pregnancy and breastfeeding, the FDA proposed a newly designed system on June 30th 2015.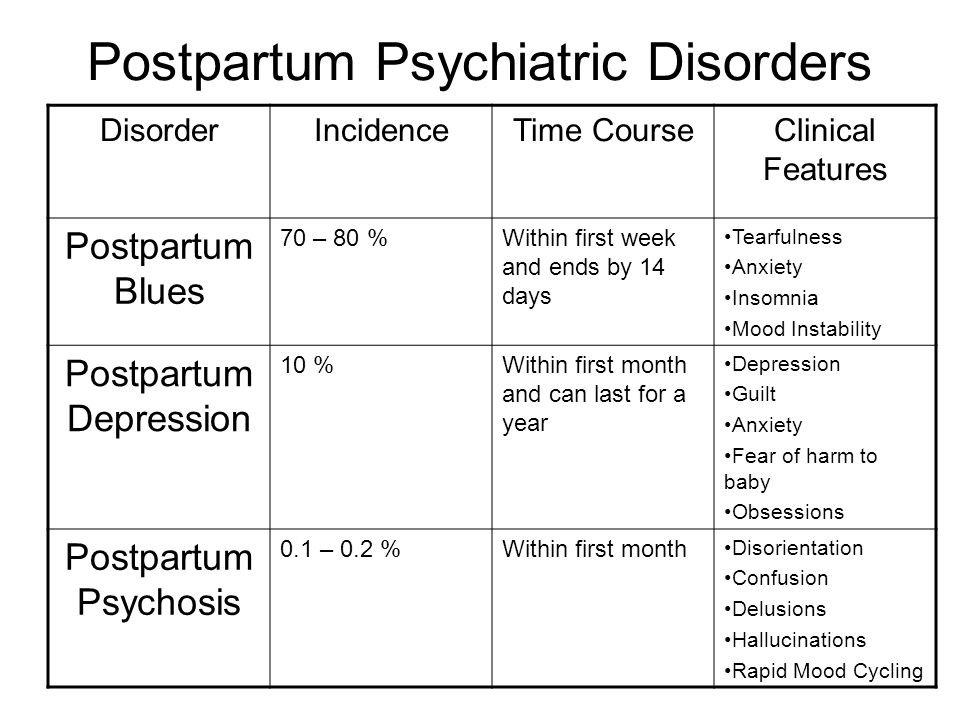 The Pregnancy and Lactation Labeling Rule or PLLR will abolish the letter categories and instead will include more comprehensive information discussing the potential risks and benefits to the mother and the fetus, and how these risks may change during the course of pregnancy.
The Pregnancy and Lactation Labeling Rule or PLLR will abolish the letter categories and instead will include more comprehensive information discussing the potential risks and benefits to the mother and the fetus, and how these risks may change during the course of pregnancy.
Companies will be required to remove the pregnancy letter categories from the labeling for all prescription drugs and will have to revise the labeling with updated information. Medications approved before June 30, 2001 are not covered by the PLLR.
Weighing the Risks
Women with histories of psychiatric illness frequently come in for consultations regarding the use of psychotropic medications during pregnancy. Not infrequently, women present with the first onset of psychiatric illness while pregnant. Many pregnancies are unplanned and may occur unexpectedly while women are receiving treatment with medications for psychiatric disorders. Many women may consider stopping medication abruptly after learning they are pregnant, but for many women this may carry substantial risks.
Decisions regarding the initiation or maintenance of treatment during pregnancy must reflect an understanding of the risks associated with fetal exposure to a particular medication but must also take into consideration the risks associated with untreated psychiatric illness in the mother. Psychiatric illness in the mother is not a benign event and may cause significant morbidity for both the mother and her child; thus, discontinuing or withholding medication during pregnancy is not always the safest option.
Depression and anxiety during pregnancy have been associated with a variety of adverse pregnancy outcomes. Women who suffer from psychiatric illness during pregnancy are less likely to receive adequate prenatal care and are more likely to use alcohol, tobacco, and other substances known to adversely affect pregnancy outcomes. Several studies have described low birth weight and fetal growth retardation in children born to depressed mothers. Preterm delivery is another potential pregnancy complication among women experiencing distress during pregnancy. Pregnancy complications related to maternal depression and anxiety in late pregnancy have also been described, including an increased risk for having pre-eclapsia, operative delivery, and infant admission to a special care nursery for a variety of conditions including respiratory distress, hypoglycemia, and prematurity. These data underscore the need to perform a thorough risk/benefit analysis of pregnant women with psychiatric illness, including evaluating the impact of untreated illness on the baby and the mother, as well as the risks of using medication during pregnancy.
Pregnancy complications related to maternal depression and anxiety in late pregnancy have also been described, including an increased risk for having pre-eclapsia, operative delivery, and infant admission to a special care nursery for a variety of conditions including respiratory distress, hypoglycemia, and prematurity. These data underscore the need to perform a thorough risk/benefit analysis of pregnant women with psychiatric illness, including evaluating the impact of untreated illness on the baby and the mother, as well as the risks of using medication during pregnancy.
What are the Risks of Medication Exposure?
All medications diffuse readily across the placenta, and no psychotropic drug has yet been approved by the Food and Drug Administration (FDA) for use during pregnancy. When prescribing medications during pregnancy, one must consider the following risks associated with prenatal exposure: risk of teratogenesis, risk of neonatal toxicity, and risk of long-term neurobehavioral sequelae.
Risk of Teratogenesis
The baseline incidence of major congenital malformations in newborns born in the United States is estimated to be between 2 and 4%. During the earliest stages of pregnancy, formation of major organ systems takes place and is complete within the first 12 weeks after conception. Therefore, discussion around risks of exposures during pregnancy may be broken down by the timing of exposure or trimester, with particular vigilance around first trimester exposures.
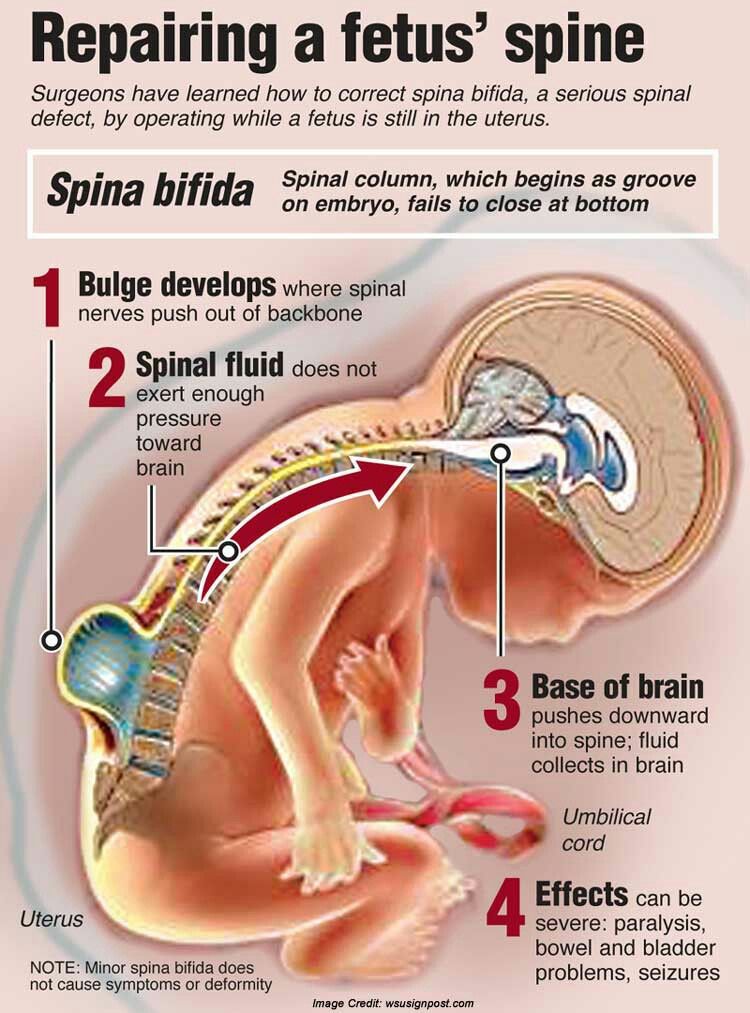
A teratogen is defined as an agent that interferes the in utero development process and produces some type of organ malformation or dysfunction. For each organ or organ system, there exists a critical period during which development takes place and is susceptible to the effects of a teratogen. For example, neural tube folding and closure, forming the brain and spinal cord, occur within the first four weeks of gestation. Most of the formation of the heart and great vessels takes place from four to nine weeks after conception, although the entire first trimester is often considered pertinent.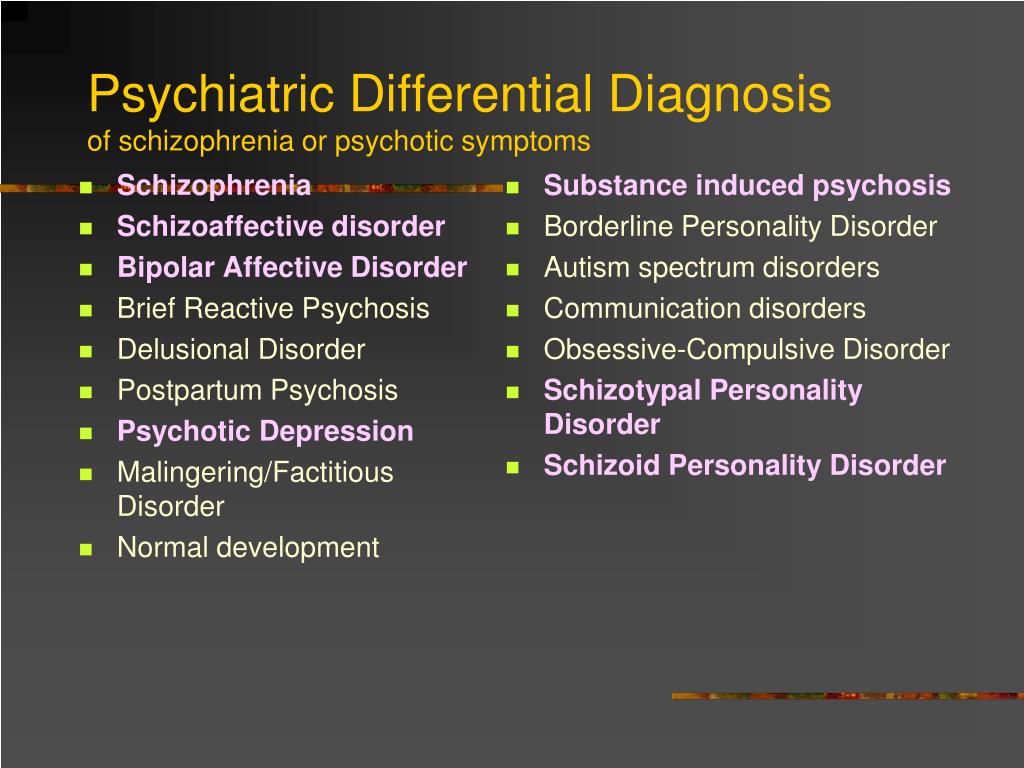
Risk of Neonatal Symptoms
Neonatal toxicity or perinatal syndromes (sometimes referred to as neonatal “withdrawal”) refer to a spectrum of physical and behavioral symptoms observed in the acute neonatal period that can be attributed to drug exposure at or near the time of delivery. Anecdotal reports that attribute these syndromes to drug exposure must be cautiously interpreted, and larger samples must be studied in order to establish a causal link between exposure to a particular medication and a perinatal syndrome.
Risk of Long-Term Effects
Although the data suggest that some medications may be used safely during pregnancy if clinically warranted, our knowledge regarding the long-term effects of prenatal exposure to psychotropic medications is incomplete. Because neuronal migration and differentiation occur throughout pregnancy and into the early years of life, the central nervous system (CNS) remains particularly vulnerable to toxic agents throughout pregnancy.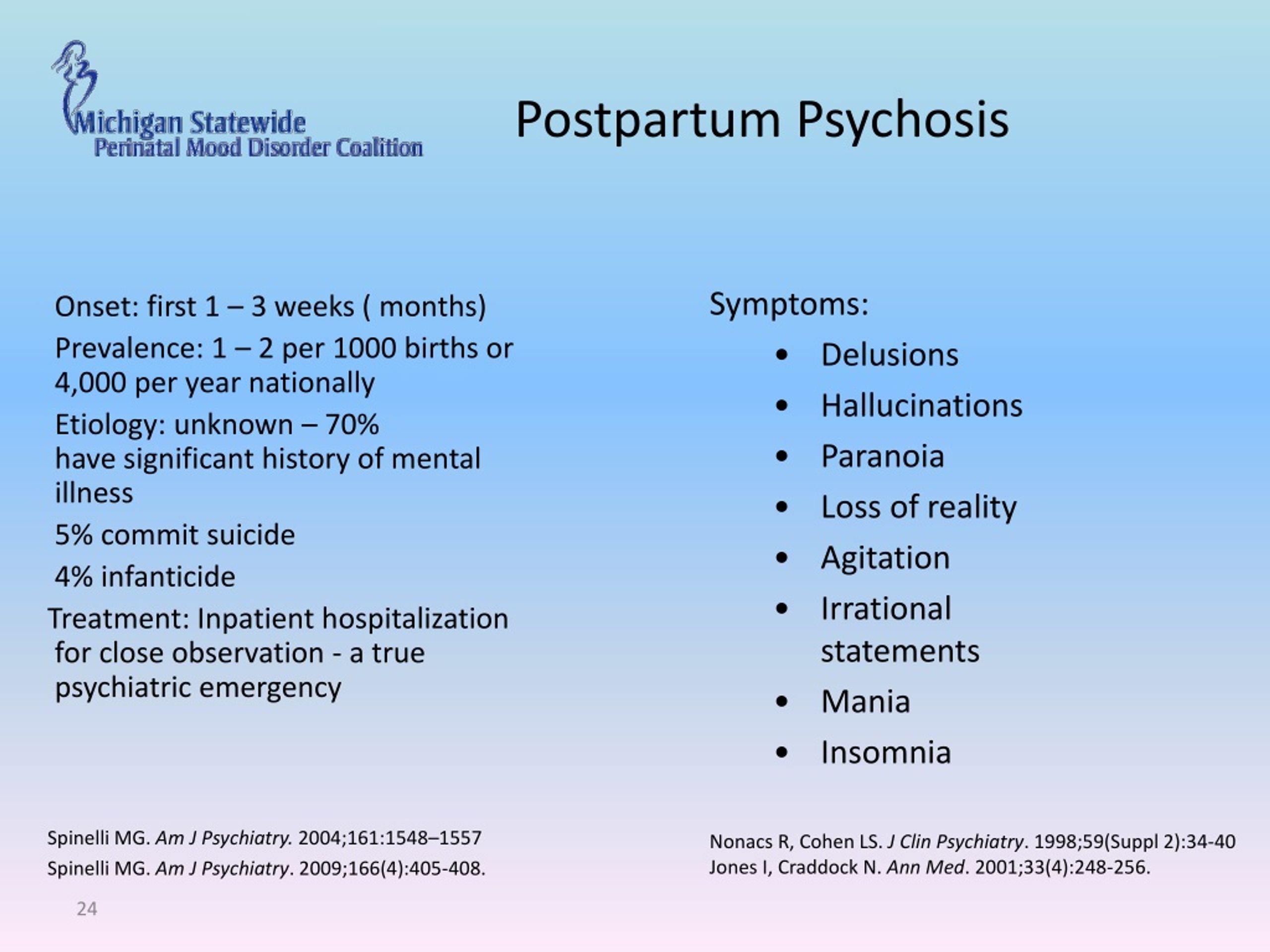 While exposures to teratogens early in pregnancy may result in clear abnormalities, exposures that occur after neural tube closure (at 32 days of gestation) may produce more subtle changes in behavior and functioning.
While exposures to teratogens early in pregnancy may result in clear abnormalities, exposures that occur after neural tube closure (at 32 days of gestation) may produce more subtle changes in behavior and functioning.
Behavioral teratogenesis refers to the potential of a psychotropic drug administered during pregnancy to have long-term neurobehavioral effects. For example, are children who have been exposed to an antidepressant in utero at risk for cognitive or behavioral problems at a later point during their development? To date, few studies have systematically investigated the impact of exposure to psychotropic medications in utero on development and behavior in humans.
Antidepressants and Pregnancy
Of all the antidepressants, fluoxetine (Prozac) is the best characterized antidepressant. Data collected from over 2500 cases indicate no increase in risk of major congenital malformation in fluoxetine-exposed infants. One prospective study of 531 infants with first trimester exposure to SSRIs (mostly citalopram, n=375) did not demonstrate an increased risk of organ malformation.
One prospective study of 531 infants with first trimester exposure to SSRIs (mostly citalopram, n=375) did not demonstrate an increased risk of organ malformation.
Several meta-analyses combining studies with exposures to SSRIs do not demonstrate an increase in risk of congenital malformation in children exposed to these antidepressants, with the exception of paroxetine (Paxil). There has been particular controversy around paroxetine use in pregnancy, as past reports have suggested that first trimester exposure to paroxetine was associated with an increased risk of cardiac defects including atrial and ventricular septal defects. Other published studies have not demonstrated increased teratogenicity of paroxetine. Importantly, independently conducted meta-analyses of available data sets have consistently found a lack of association between paroxetine exposure and cardiovascular malformations. Even so, these findings prompted the FDA to change the category label of paroxetine from C to D.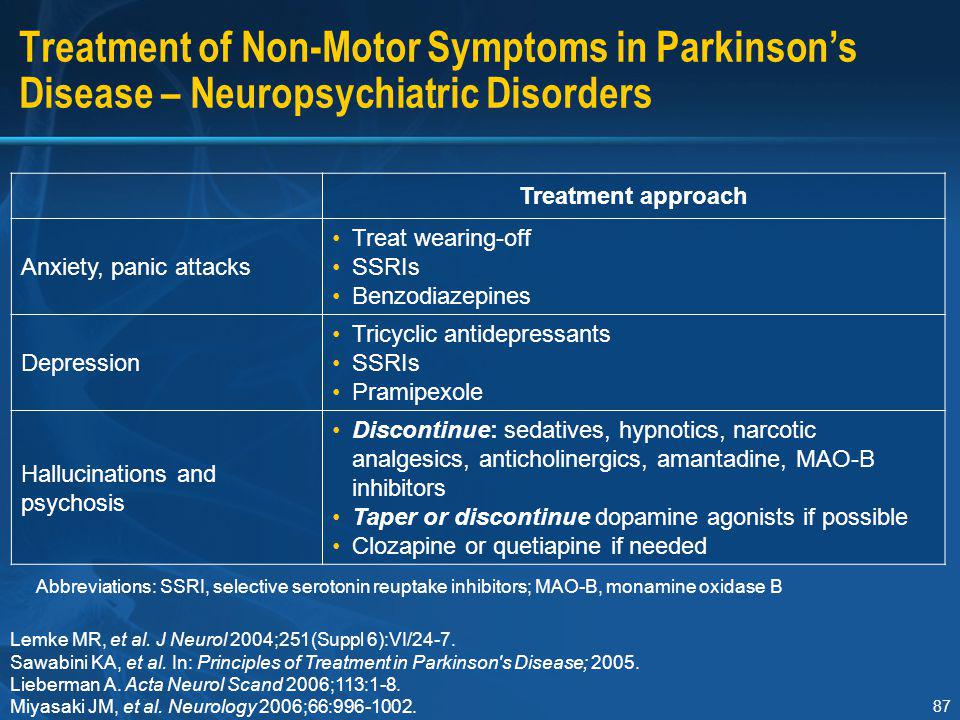
Three prospective and more than ten retrospective studies have examined the risk of organ malformation in over 400 cases of first trimester exposure to tricyclic antidepressants of TCAs. When evaluated on an individual basis and when pooled, these studies do not indicate a significant association between fetal exposure to TCAs and risk for any major congenital anomaly. Among the TCAs, desipramine and nortriptyline are often preferred since they are less anti-cholinergic and the least likely to exacerbate orthostatic hypotension that occurs during pregnancy.
Bupropion may be an option for women who have not responded to fluoxetine or a tricyclic antidepressant, as data thus far have not indicated an increased risk of malformations associated with bupropion use during pregnancy. The most recent information from the Bupropion Pregnancy Registry maintained by the manufacturer GlaxoSmithKline includes data from 517 pregnancies involving first trimester exposure to bupropion. In this sample, there were 20 infants with major malformations. This represents a 3.9% risk of congenital malformation that is consistent with what is observed in women with no known teratogen exposure. While this information regarding the overall risk of malformation is reassuring, earlier reports had revealed an unexpectedly high number of malformations of the heart and great vessels in bupropion-exposed infants. A retrospective cohort study including over 1200 infants exposed to bupropion during the first trimester did not reveal an increased risk of malformations in the bupropion-exposed group of infants nor did it demonstrate an increased risk for cardiovascular malformations.
This represents a 3.9% risk of congenital malformation that is consistent with what is observed in women with no known teratogen exposure. While this information regarding the overall risk of malformation is reassuring, earlier reports had revealed an unexpectedly high number of malformations of the heart and great vessels in bupropion-exposed infants. A retrospective cohort study including over 1200 infants exposed to bupropion during the first trimester did not reveal an increased risk of malformations in the bupropion-exposed group of infants nor did it demonstrate an increased risk for cardiovascular malformations.
Scant information is available regarding the reproductive safety of monoamine oxidase inhibitors (MAOIs), and these agents are generally not used in pregnancy as they may produce a hypertensive crisis when combined with tocolytic medications, such as terbutaline.
With regard to the newer antidepressants, prospective data on 150 women exposed to venlafaxine (Effexor) during the first trimester of pregnancy suggest no increase in risk of major malformation as compared to non-exposed controls.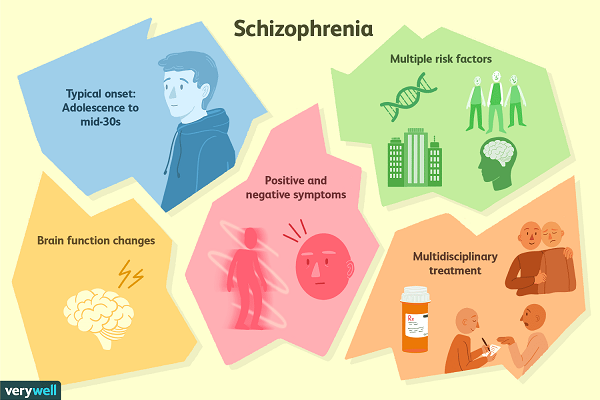 To date, the literature does not include prospective data on the use of duloxetine (Cymbalta).
To date, the literature does not include prospective data on the use of duloxetine (Cymbalta).
Another prospective study assessed outcomes in 147 women taking either nefazodone (n=89) or trazodone (n=58) during their first trimester of pregnancy and compared them to two control groups of women exposed to either non-teratogenic drugs (n = 147) or to other antidepressants (n=147). There were no significant differences among exposed and non-exposed groups with regard to rates of congenital malformations. In another report, there were no differences in malformation rates among women who took mirtazapine (Remeron) (n=104) during pregnancy as compared to women who took other antidepressants or controls exposed to known nonteratogens.
While these initial reports are reassuring, larger samples are required to establish the reproductive safety of these newer antidepressants. It is estimated that at least 500 to 600 exposures must be collected to demonstrate a two-fold increase in risk for a particular malformation over what is observed in the general population.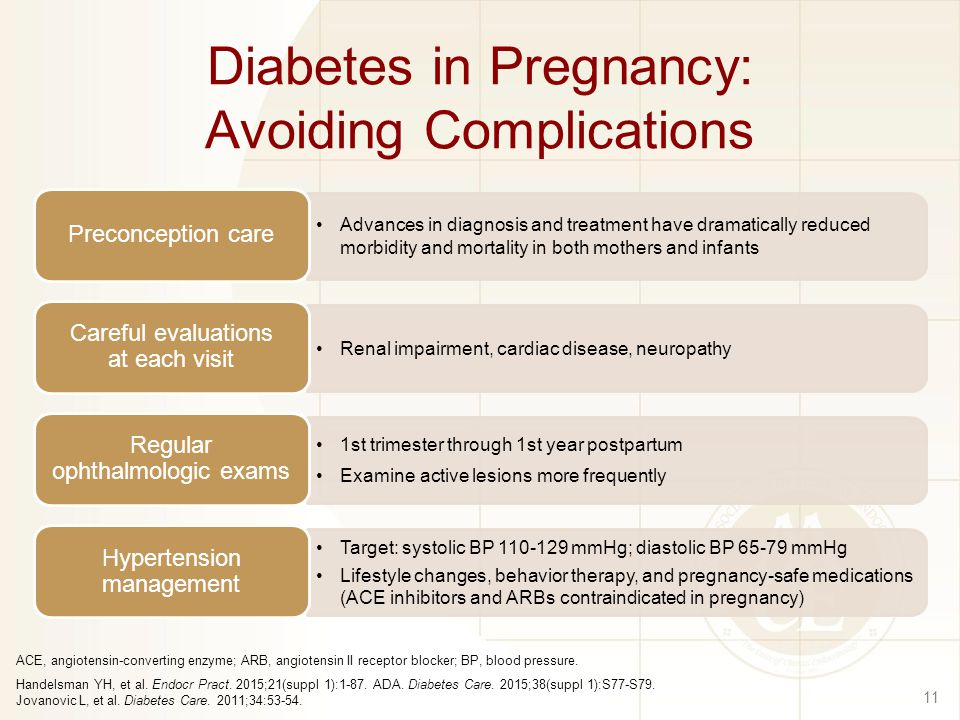 In general, the SSRIs, specifically fluoxetine, citalopram, and sertraline, are the antidepressants most commonly used during pregnancy.
In general, the SSRIs, specifically fluoxetine, citalopram, and sertraline, are the antidepressants most commonly used during pregnancy.
Several recent studies have suggested that exposure to SSRIs near the time of delivery may be associated with poor perinatal outcomes. Attention has focused on a range of transient neonatal distress syndromes associated with exposure to (or withdrawal from) antidepressants in utero. These syndromes appear to affect about 25% of babies exposed to antidepressants late in pregnancy. The most commonly reported symptoms in the newborns include tremor, restlessness, increased muscle tone, and increased crying. Reassuringly, these syndromes appear to be relatively benign and short-lived, resolving within 1 to 4 days after birth without any specific medical intervention.
These studies deserve careful consideration, yet one of the major shortcomings is that most have failed to use raters blinded to the mother’s treatment status. The decision to admit a newborn to a special care nursery may represent a reasonable precaution for an infant exposed to medication in utero and may not be an indication of a serious problem. Another limitation is that few studies have attempted to assess maternal mood during pregnancy or at the time of delivery. There is ample evidence to suggest that depression or anxiety in the mother may contribute to poor neonatal outcomes, including premature delivery and low birth weight, and it is important to evaluate the contribution of maternal mood to neonatal outcomes.
The decision to admit a newborn to a special care nursery may represent a reasonable precaution for an infant exposed to medication in utero and may not be an indication of a serious problem. Another limitation is that few studies have attempted to assess maternal mood during pregnancy or at the time of delivery. There is ample evidence to suggest that depression or anxiety in the mother may contribute to poor neonatal outcomes, including premature delivery and low birth weight, and it is important to evaluate the contribution of maternal mood to neonatal outcomes.
Based on these findings, many women are advised to taper or discontinue treatment with SSRIs prior to delivery; however, this strategy has not been shown to change neonatal outcomes. Importantly, neonatal effects have been reported with both untreated mood and anxiety disorders, as well as with medication, and limited studies have adequately teased out these variables. One important consideration is that discontinuation of or reductions in the dosage of mediation in the latter part of pregnancy may increase the risk of postpartum depression, as the postpartum period is a time of increased vulnerability to psychiatric illness and depression or anxiety during pregnancy has been associated with postpartum depression.
Another concern has been that maternal SSRI use may be associated with a higher than expected number of cases of persistent pulmonary hypertension of the newborn (PPHN). In one report, the use of an SSRI antidepressant after the 20th week of gestation was significantly associated with a six-fold greater risk of PPHN. If we assume that these findings are correct, the risk is still relatively small; the authors estimate the risk of PPHN to be less than 1% in infants exposed to SSRIs in utero. Since the initial report on this topic, three studies have found no association between antidepressant use during pregnancy and PPHN, and one study showed a much lower risk than the 1% originally reported. These findings taken together bring into question whether there is an association at all and suggest that, if there is a risk, it is much lower than that reported in the original 2006 report.
To date only two studies have systematically investigated the impact of exposure to antidepressants in utero on development and behavior in humans.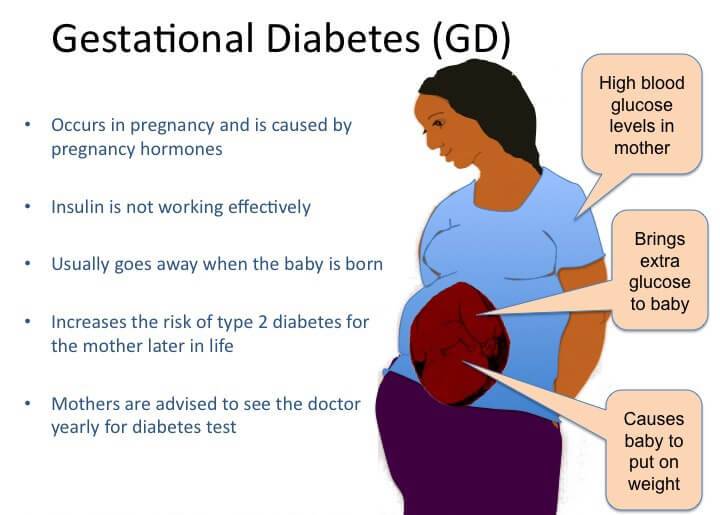 The first of these studies followed a cohort of 135 children who had been exposed to either tricyclic antidepressants or fluoxetine (Prozac) during pregnancy (most commonly during the first trimester) and compared these subjects to a cohort of non-exposed controls. Results indicated no significant differences in IQ, temperament, behavior, reactivity, mood, distractibility, or activity level between exposed and non-exposed children followed up to 7 years of age. A more recent report from the same group that followed a cohort of children exposed to fluoxetine or tricyclic antidepressants for the entire duration of the pregnancy yielded similar results. The authors concluded that their findings support the hypothesis that fluoxetine and tricyclic antidepressants are not behavioral teratogens and do not have a significant effect on cognitive development, language or behavior.
The first of these studies followed a cohort of 135 children who had been exposed to either tricyclic antidepressants or fluoxetine (Prozac) during pregnancy (most commonly during the first trimester) and compared these subjects to a cohort of non-exposed controls. Results indicated no significant differences in IQ, temperament, behavior, reactivity, mood, distractibility, or activity level between exposed and non-exposed children followed up to 7 years of age. A more recent report from the same group that followed a cohort of children exposed to fluoxetine or tricyclic antidepressants for the entire duration of the pregnancy yielded similar results. The authors concluded that their findings support the hypothesis that fluoxetine and tricyclic antidepressants are not behavioral teratogens and do not have a significant effect on cognitive development, language or behavior.
Mood Stabilizers
For women with bipolar disorder, maintenance treatment with a mood stabilizer during pregnancy can significantly reduce the risk of relapse. However, many of the medications commonly used to treat bipolar disorder carry some teratogenic risk when used during pregnancy.
However, many of the medications commonly used to treat bipolar disorder carry some teratogenic risk when used during pregnancy.
Concerns regarding fetal exposure to lithium, have typically been based on early reports of higher rates of cardiovascular malformations (e.g., Ebstein’s anomaly) following prenatal exposure to this drug. More recent data suggest the risk of cardiovascular malformations following first trimester exposure to lithium is smaller than previous assessments and is estimated to be between 1 in 2000 (0.05%) and 1 in 1000 (0.1%). Compared to lithium, prenatal exposure to some anticonvulsants is associated with a far greater risk for organ malformation. First trimester use of carbamazepine (Tegretol) has been associated with a 1% risk of neural tube defect. Of all of the medications used for psychiatric disorders, the one with the greatest potential of serious birth defects is valproate (valproic acid, Depakote). Factors which appear to increase the risk for teratogenesis include higher maternal serum anticonvulsant levels and exposure to more than one anticonvulsant.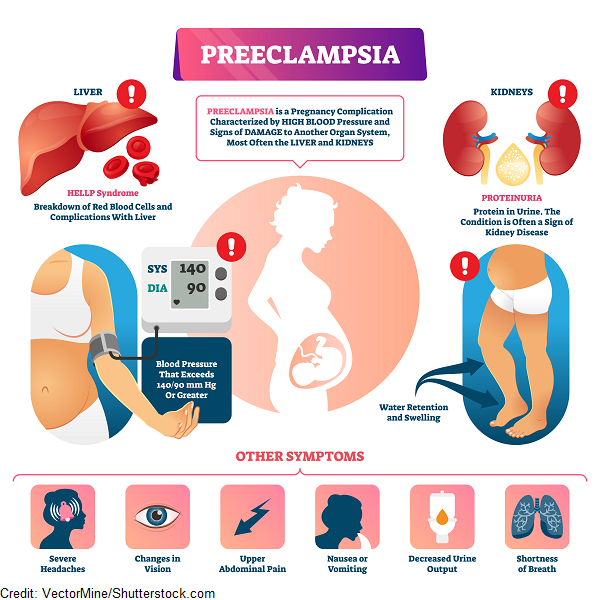 With a risk of neural tube defect ranging from 1 to 6%, this drug is often considered one of last resort in reproductive aged women, since the risk for teratogenicity is high in very early pregnancy, before many women realize they are pregnant.
With a risk of neural tube defect ranging from 1 to 6%, this drug is often considered one of last resort in reproductive aged women, since the risk for teratogenicity is high in very early pregnancy, before many women realize they are pregnant.
Prenatal exposure to valproic acid has also been associated with characteristic craniofacial abnormalities, cardiovascular malformation, limb defects and genital anomalies, as well as other central nervous system structural abnormalities. Also, valproate exposure during pregnancy has been associated with poorer neurocognitive development in children followed to three years of age. In the same study, lamotrigine use (discussed below) did not affect neurocognitive development.
While other anticonvulsants are being used more frequently in the treatment of bipolar disorder, there is limited information on the reproductive safety of these newer anticonvulsants, specifically gabapentin (Neurontin), oxcarbazepine (Trileptal), tigabine (Gabitril), levetiracetam (Keppra), zonisamide (Zonegran).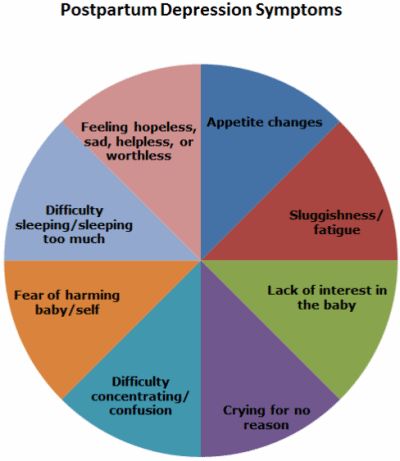 One report has raised concerns regarding potential teratogenicity of topiramate (Topamax).
One report has raised concerns regarding potential teratogenicity of topiramate (Topamax).
However, there is a growing body of information the reproductive safety of lamotrigine (Lamictal), and this may be a useful alternative for some women. The International Lamotrigine Pregnancy Registry was created by GlaxoSmithKline (GSK) in 1992 to monitor pregnancies exposed to lamotrigine for the occurrence of major birth defects. Data from the Registry did not show an elevated risk of malformations associated with lamotrigine exposure.
Other data from the North-American Anti-Epileptic Drug Registry indicates the prevalence of major malformations in a total of 564 children exposed to lamotrigine monotherapy was 2.7%; however, five infants had oral clefts, indicating a prevalence rate of 8.9 per 1000 births. In a comparison group of 221,746 unexposed births, the prevalence rate for oral clefts was 0.37/1000, indicating a 24-fold increase in risk of oral cleft in infants exposed to lamotrigine.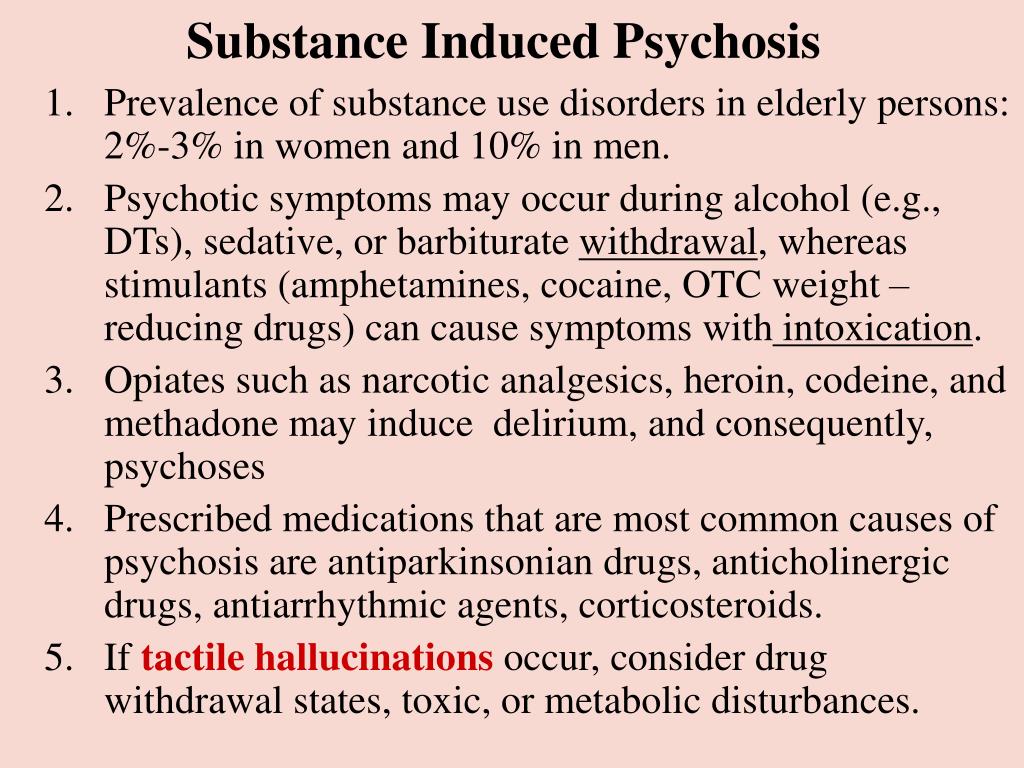 However, other registries have not demonstrated such a significant increase in risk for oral clefts. It is important to put this risk into perspective. If we assume that the findings from the North American registry are true, the absolute risk of having a child with cleft lip or palate is about 0.9%.
However, other registries have not demonstrated such a significant increase in risk for oral clefts. It is important to put this risk into perspective. If we assume that the findings from the North American registry are true, the absolute risk of having a child with cleft lip or palate is about 0.9%.
Atypical antipsychotic agents (discussed in greater detail below) are commonly used often to manage the acute symptoms of bipolar illness, as well as for maintenance treatment. While the data regarding the reproductive safety of these newer agents is limited, no studies thus far have indicated any teratogenic risk associated with this class of medications. For this reason, some women may choose to use an atypical antipsychotic agent during pregnancy (especially during the first trimester) in order to avoid using a known teratogen, such as lithium or valproic acid.
Anti-Anxiety Medications
The consequences of prenatal exposure to benzodiazepines have been debated for over twenty years.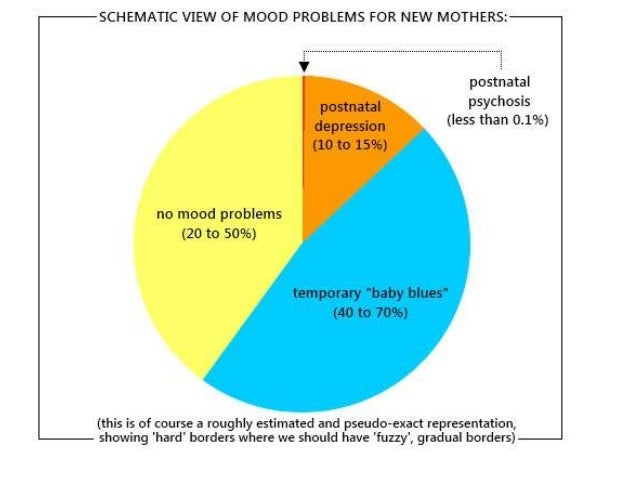 Three prospective studies support the absence of increased risk of organ malformation following first trimester exposure to benzodiazepines. More controversial has been the issue of whether first trimester exposure to benzodiazepines increases risk for specific malformations. Although initial reports suggested that there may be an increased risk of cleft lip and palate, more recent reports have shown no association between exposure to benzodiazepines and risk for cleft lip or palate. This risk– if it exists — is calculated to be 0.7%, approximately a ten-fold increase in risk for oral cleft over that observed in the general population. Nonetheless, the likelihood that a woman exposed to benzodiazepines during the first trimester will give birth to a child with this congenital anomaly, although significantly increased, remains less than 1%.
Three prospective studies support the absence of increased risk of organ malformation following first trimester exposure to benzodiazepines. More controversial has been the issue of whether first trimester exposure to benzodiazepines increases risk for specific malformations. Although initial reports suggested that there may be an increased risk of cleft lip and palate, more recent reports have shown no association between exposure to benzodiazepines and risk for cleft lip or palate. This risk– if it exists — is calculated to be 0.7%, approximately a ten-fold increase in risk for oral cleft over that observed in the general population. Nonetheless, the likelihood that a woman exposed to benzodiazepines during the first trimester will give birth to a child with this congenital anomaly, although significantly increased, remains less than 1%.
Currently, no systematic data are available on the reproductive safety of non-benzodiazepine anxiolytic agents such as buspirone and hypnotic agents zolpidem (Ambien) and zalepion (Sonata).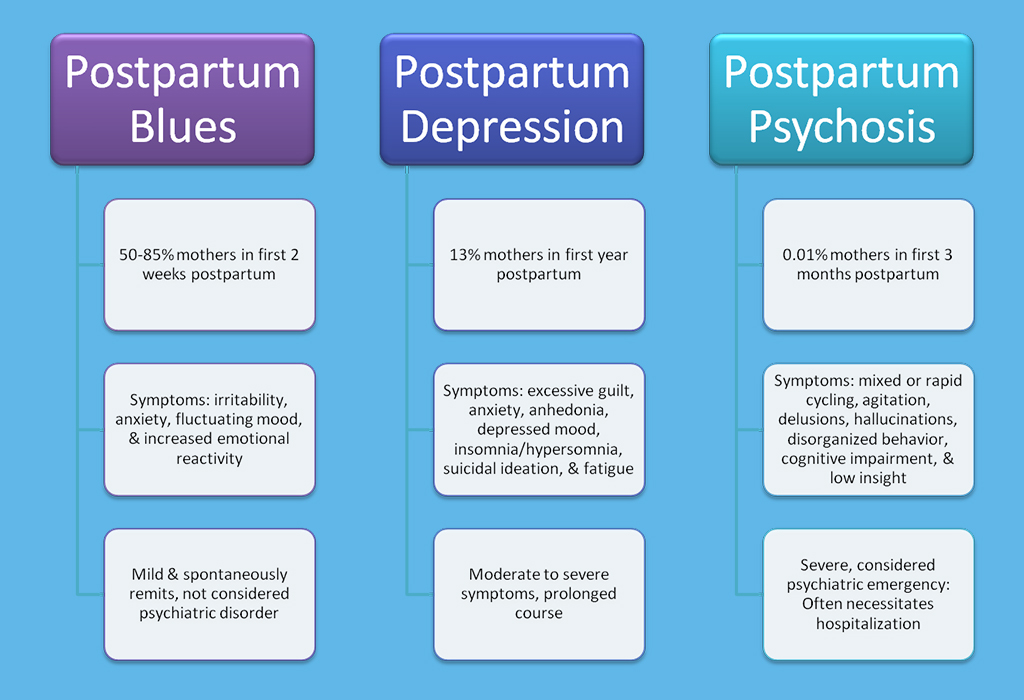 Therefore, these medications are not recommended for use in pregnancy.
Therefore, these medications are not recommended for use in pregnancy.
Anti-Psychotic Medications
In addition to the atypical antipsychotic medications described above, recent studies have not demonstrated teratogenic risk associated with high-or medium-potency neuroleptic medications; however, a recent meta-analysis of the available studies noted a higher risk of congenital malformations after first trimester exposure to low-potency neuroleptic agents. In clinical practice, higher potency neuroleptic agents such as haloperidol (Haldol), perphenazine (Trilafon), and trifluoperazine (Stelazine) are recommended over the lower potency agents in managing pregnant women with psychiatric illness.
Atypical antipsychotic medications are increasingly being used to treat a spectrum of psychiatric disorders, including psychotic disorders and bipolar disorder, as well as treatment refractory depression and anxiety disorders. The first and largest published prospective study on the reproductive safety of the atypical agents provided reassuring data regarding the risk of malformations in the first trimester, although aripiprazole (Abilify) was not among the medications studied.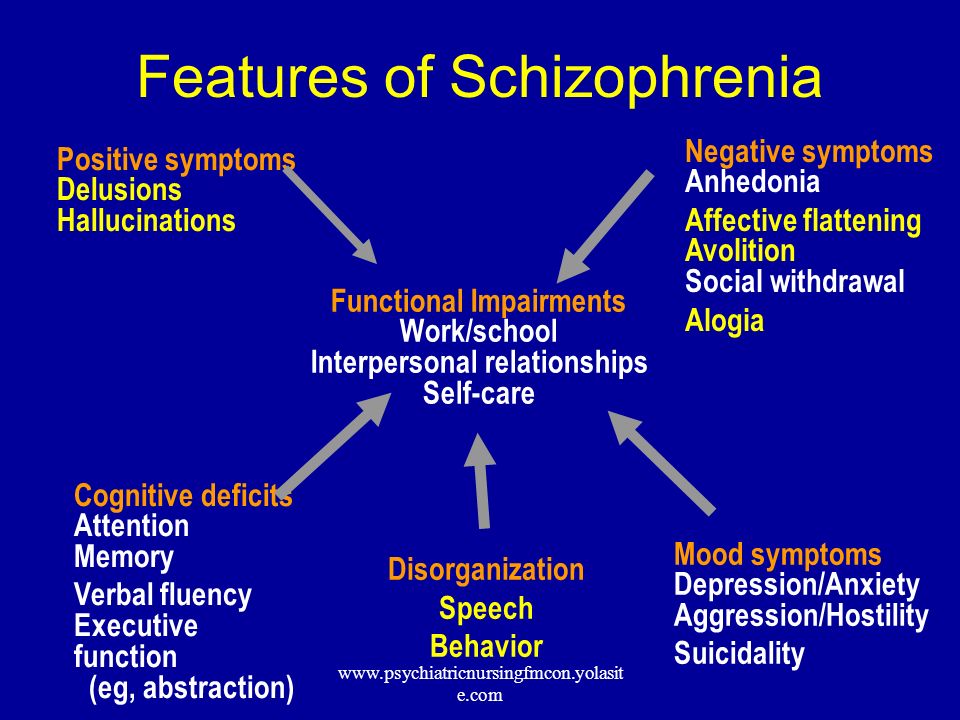 Investigators prospectively followed a group of 151 women taking olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), or clozapine (Clozapine) and compared outcomes to controls without exposure to known teratogens. There were no differences between the groups in terms of risk for major malformations, or rates of obstetrical or neonatal complications.
Investigators prospectively followed a group of 151 women taking olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), or clozapine (Clozapine) and compared outcomes to controls without exposure to known teratogens. There were no differences between the groups in terms of risk for major malformations, or rates of obstetrical or neonatal complications.
While this information is reassuring, it is far from definitive, and larger studies are required to provide more information about the reproductive safety of these medications. To this end, the National Pregnancy Registry has been created to prospectively gather information regarding outcomes in infants exposed in utero to these newer atypical antipsychotic medications.
The U.S. Food and Drug Administration (FDA) recently updated labels for the entire class of antipsychotic drugs to include warnings regarding the use of antipsychotic drugs (both the typical and atypical agents) during pregnancy. The new drug labels now contain more details on the potential risk for abnormal muscle movements (extrapyramidal signs or EPS) and withdrawal symptoms in newborns exposed to these drugs during the third trimester of pregnancy.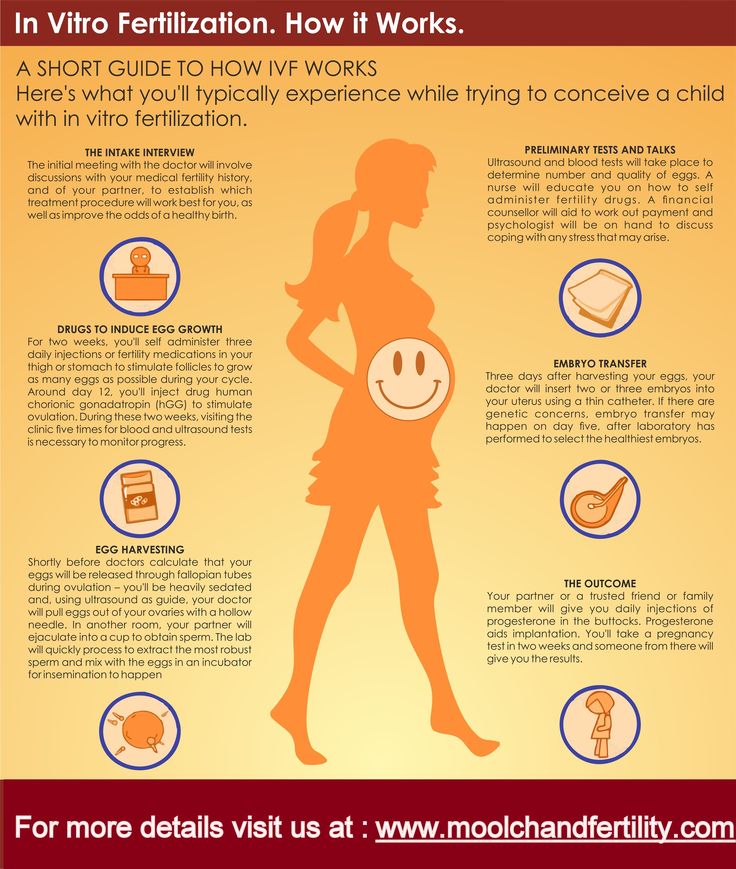 These recommendations were derived from adverse event reporting. While this may signal a potential problem associated with exposure to antipsychotic medications, it does not yield accurate information regarding the prevalence of an adverse event.
These recommendations were derived from adverse event reporting. While this may signal a potential problem associated with exposure to antipsychotic medications, it does not yield accurate information regarding the prevalence of an adverse event.
For the latest information on psychiatric disorders during pregnancy, please visit our blog.
How do I get an appointment?
Consultations regarding treatment options can be scheduled by calling our intake coordinator at 617-724-7792.
Pregnancy Research at the CWMH
Currently we are conducting several studies related to depression and pregnancy. To learn more about this study or to sign up for our research patient registry, please click here
Postpartum psychosis - NHS
Postpartum psychosis is a serious mental health illness that can affect someone soon after having a baby. It affects around 1 in 500 mothers after giving birth.
Many people who have given birth will experience mild mood changes after having a baby, known as the "baby blues".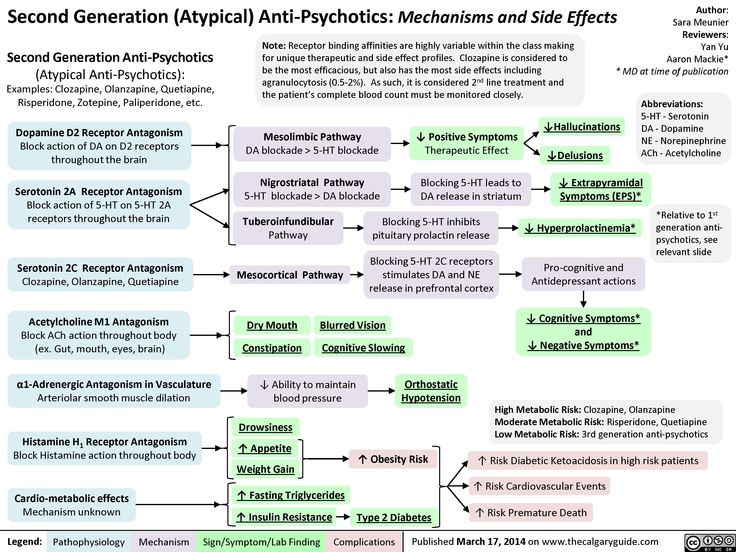 This is normal and usually only lasts for a few days.
This is normal and usually only lasts for a few days.
But postpartum psychosis is very different from the "baby blues". It's a serious mental illness and should be treated as a medical emergency.
It's sometimes called puerperal psychosis or postnatal psychosis.
Symptoms of postpartum psychosis
Symptoms usually start suddenly within the first 2 weeks after giving birth - often within hours or days of giving birth. More rarely, they can develop several weeks after the baby is born.
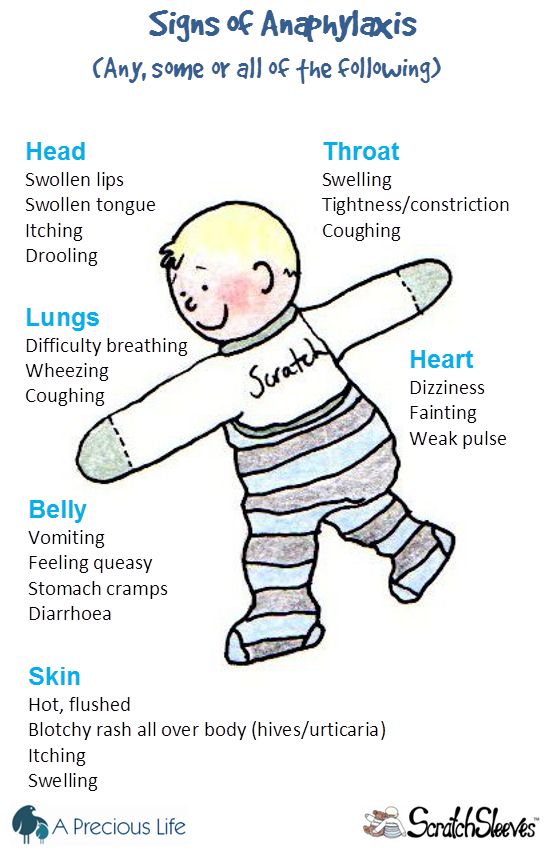
Symptoms can include:
- hallucinations - hearing, seeing, smelling or feeling things that are not there
- delusions – thoughts or beliefs that are unlikely to be true
- a manic mood – talking and thinking too much or too quickly, feeling "high" or "on top of the world"
- a low mood – showing signs of depression, being withdrawn or tearful, lacking energy, having a loss of appetite, anxiety, agitation or trouble sleeping
- sometimes a mixture of both a manic mood and a low mood - or rapidly changing moods
- loss of inhibitions
- feeling suspicious or fearful
- restlessness
- feeling very confused
- behaving in a way that's out of character
When to get medical help
Postpartum psychosis is a serious mental illness that should be treated as a medical emergency. It can get worse rapidly and the illness can risk the safety of the mother and baby.
It can get worse rapidly and the illness can risk the safety of the mother and baby.
See a GP immediately if you think you, or someone you know, may have developed symptoms of postpartum psychosis. You should request an urgent assessment on the same day.
You can call 111 if you cannot speak to a GP or do not know what to do next. Your midwife or health visitor may also be able to help you access care.
Call your crisis team if you already have a care plan because you've been assessed as being at high risk of developing postpartum psychosis.
Go to A&E or call 999 if you think you, or someone you know, may be in danger of imminent harm.
Be aware that if you have postpartum psychosis, you may not realise you're ill. Your partner, family or friends may spot the signs and have to take action.
Treating postpartum psychosis
Treatment usually happens in hospital. Ideally, this would be with your baby in a specialist psychiatric unit called a mother and baby unit (MBU). But you may be admitted to a general psychiatric ward until an MBU is available.
Ideally, this would be with your baby in a specialist psychiatric unit called a mother and baby unit (MBU). But you may be admitted to a general psychiatric ward until an MBU is available.
Medicine
You may be prescribed 1 or more of the following:
- antipsychotics – to help with manic and psychotic symptoms, such as delusions or hallucinations
- mood stabilisers (for example, lithium) – to stabilise your mood and prevent symptoms recurring
- antidepressants – to help ease symptoms if you have significant symptoms of depression and may be used alongside a mood stabiliser
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) is sometimes recommended if all other treatment options have failed, or when the situation is thought to be life threatening.
Most people with postpartum psychosis make a full recovery as long as they receive the right treatment.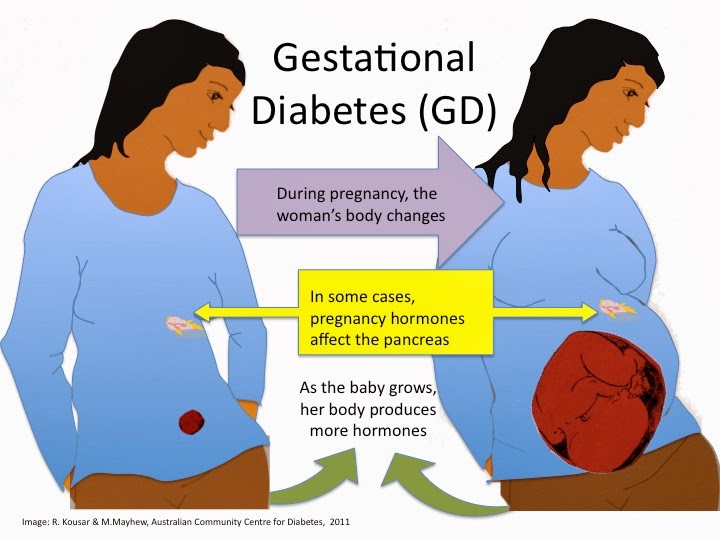
Psychological therapy
As you move forward with your recovery, you may benefit from seeing a therapist for cognitive behavioural therapy (CBT). CBT is a talking therapy that can help you manage your problems by changing the way you think and behave.
Other forms of support
It can be hard to come to terms with the experience of postpartum psychosis as you recover.
Talking to peers and others with lived experience of the illness may be helpful. Some inpatient units and communities have peer support workers who have experienced the illness, and you can also access support through charities.
Causes
We're not sure what causes postpartum psychosis, but you're more at risk if you:
- already have a diagnosis of bipolar disorder or schizophrenia
- have a family history of mental health illness, particularly postpartum psychosis (even if you have no history of mental illness)
- developed postpartum psychosis after a previous pregnancy
Reducing the risk of postpartum psychosis
If you're at high risk of developing postpartum psychosis, you should have specialist care during pregnancy and be seen by a perinatal psychiatrist.
You should have a pre-birth planning meeting at around 32 weeks of pregnancy with everyone involved in your care. This includes your partner, family or friends, mental health professionals, your midwife, obstetrician, health visitor and GP.
This is to make sure that everyone is aware of your risk of postpartum psychosis. You should all agree on a plan for your care during pregnancy and after you've given birth.
You'll get a written copy of your care plan explaining how you and your family can get help quickly if you become ill, as well as strategies you can use to reduce your risk of becoming ill.
In the first few weeks after your baby is born, you should have regular home visits from a midwife, health visitor and mental health nurse.
Recovering from postpartum psychosis
The most severe symptoms tend to last 2 to 12 weeks, and it can take 6 to 12 months or more to recover completely from the condition.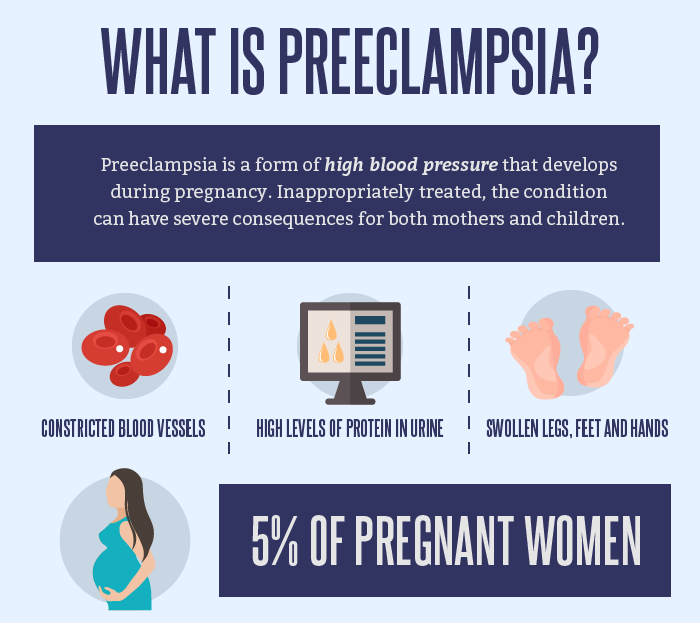 But with treatment and the right support, most people with postpartum psychosis do make a full recovery.
But with treatment and the right support, most people with postpartum psychosis do make a full recovery.
An episode of postpartum psychosis is sometimes followed by a period of depression, anxiety and low confidence. It might take a while for you to come to terms with what happened.
Some mothers have difficulty bonding with their baby after an episode of postpartum psychosis, or feel some sadness at missing out on time with their baby. With support from your partner, family, friends and your mental health team, or talking to others with lived experience, you can overcome these feelings.
Many people who've had postpartum psychosis go on to have more children. Although there is about a 1 in 2 chance you will have another episode after a future pregnancy, you should be able to get help quickly with the right care and the risks can be reduced with appropriate interventions.
Support for postpartum psychosis
Postpartum psychosis can have a big impact on your life, but support is available.
It might help to speak to others who've had the same condition, or connect with a charity.
You may find the following links useful:
Action on Postpartum Psychosis (APP)
Action on Postpartum Psychosis (APP) have produced a series of guides with the help of women who have experienced postpartum psychosis.
These guides cover topics such as:
- recovering from postpartum psychosis
- supporting partners
- planning pregnancy
- parenting after postpartum psychosis
- pregnancy for women with bipolar disorder
There is also an APP forum, where you can connect with others affected by postpartum psychosis.
Other useful links
- Mind: what is postpartum psychosis?
- Royal College of Psychiatrists: postpartum psychosis
Supporting people with their recovery
People with postpartum psychosis will need support to help them with their recovery.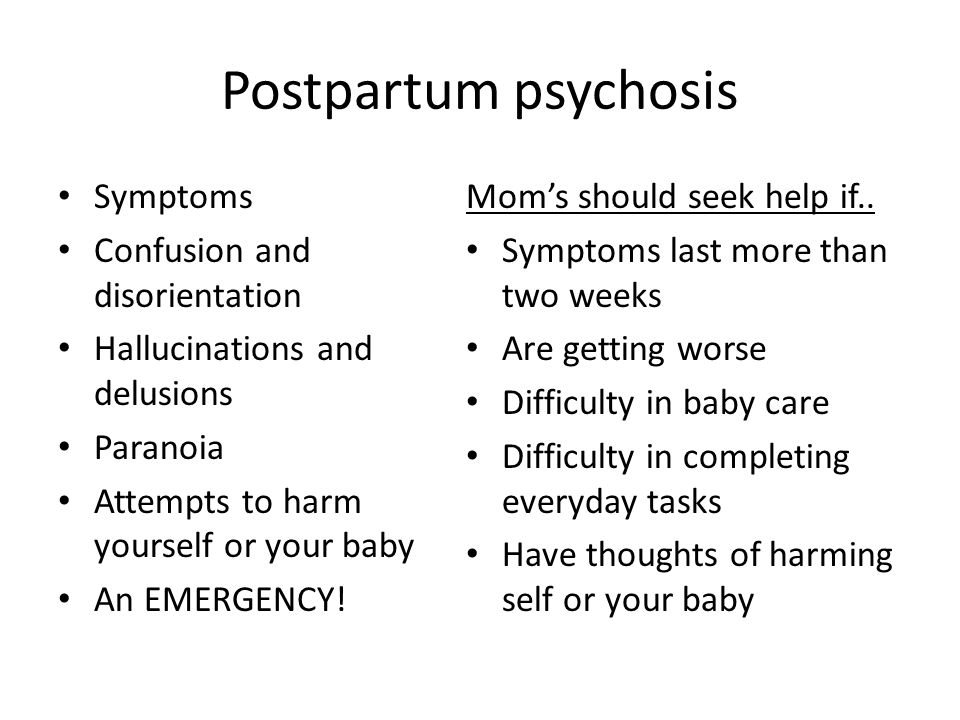
You can help your partner, relative or friend by:
- being calm and supportive
- taking time to listen
- helping with housework and cooking
- helping with childcare and night-time feeds
- letting them get as much sleep as possible
- helping with shopping and household chores
- keeping the home as calm and quiet as possible
- not having too many visitors
Support for partners, relatives and friends
Postpartum psychosis can be distressing for partners, relatives and friends, too.
If your partner, relative or friend is going through an episode of postpartum psychosis or recovering, do not be afraid to get help yourself.
Talk to a mental health professional or approach the charities listed.
Psychosis in women (postpartum, during pregnancy)
Contents↓[show]
Psychosis is an acute disorder of mental functions, in which sudden mood swings occur, inappropriate behavior is noted, in some cases delusional thoughts and hallucinations appear. Signs of psychosis in women appear most acutely and rapidly against the background of hormonal changes or any shocks. Psychosis during pregnancy or after the birth of a child cannot be treated at home without the help of a specialist.
Specialists of the Yusupov Hospital offer comfortable conditions, quality service and high-level medical care to patients. Psychiatrists carry out complex treatment of various types of neurosis in patients over the age of 18 years.
Pregnancy psychosis
Pregnancy psychosis is a common condition characterized by a distorted perception of reality, depression, tearfulness and mood swings. Psychosis is most common in late pregnancy and persists for a period of time after the baby is born.
Psychoses in pregnant women develop due to several reasons:
- hormonal changes;
- emotional instability and anxious expectations of future events;
- mental illness;
- hereditary predisposition to mental disorders;
- past infectious diseases and weakened immune system;
- intoxication of the body due to the use of alcohol or drugs;
- lack of vitamin B and other nutrients.
Severe stress during pregnancy is the greatest danger to the fetus. Psychosis, the symptoms and signs of which appear during pregnancy in women, can lead to low birth weight or premature birth. Women who, before pregnancy, noted the occurrence of stress in themselves under the influence of various stimuli, when planning a pregnancy, you should contact a psychiatrist to exclude psychosis when carrying a child.
Experienced psychiatrists at the Yusupov Hospital accompany patients with this problem throughout their pregnancy. Modern methods of correction allow you to effectively deal with the initial signs of emotional distress, anxiety and psychosis.
Modern methods of correction allow you to effectively deal with the initial signs of emotional distress, anxiety and psychosis.
Postpartum psychosis
Postpartum psychosis most often develops in women who give birth for the first time or in repeated births that are accompanied by complications. The period from 1 to 4 weeks after the birth of a child is the most dangerous for a woman, since against the background of hormonal changes, the likelihood of a mental disorder is high.
Depressive, asthenic condition, refusal to eat, depression and thoughts of suicide are serious reasons for seeking professional help at the Yusupov Hospital. Experts have found that women whose relatives have experienced postpartum psychosis are prone to this problem, so the likelihood of developing a mental disorder is 3%.
The Yusupov Hospital selects safe drugs and methods for the treatment of postpartum psychosis. Every day, experienced psychiatrists and psychologists interact with women, who consult patients after discharge. Postpartum psychosis in women is about 9% of the total number of cases of mental disorders in women.
Postpartum psychosis in women is about 9% of the total number of cases of mental disorders in women.
Signs of psychosis in women
Symptoms of psychosis in women are varied, so a psychiatrist can make a diagnosis after a comprehensive diagnosis. Psychosis in women during pregnancy or after childbirth may have the following manifestations:
- confusion and cognitive impairment;
- mood swings;
- not accepting one's own state;
- increased anxiety or extremely positive mood;
- auditory or visual hallucinations;
- delusional thoughts;
- discrepancy between judgments and reality;
- lethargy, maintaining one posture for a long time.
In a state of psychosis, the behavior, thinking and emotional manifestations of a woman change. These changes do not allow to realistically assess the events and realize what is happening, therefore, to solve the problem, a woman needs the help of loved ones. Postpartum psychosis affects women's consciousness, so patients may be hospitalized and treated, so in some cases, relatives turn to the Yusupov hospital for help.
Postpartum psychosis affects women's consciousness, so patients may be hospitalized and treated, so in some cases, relatives turn to the Yusupov hospital for help.
When referring to a psychiatrist at the Yusupov hospital with this problem, a diagnosis is made, during which an experienced specialist studies the manifestations and nature of the symptoms. Some signs of a mental disorder may appear before the onset of psychosis and are good reasons to seek expert advice. Women before the onset of psychosis note sleep disturbance, lack of appetite, increased anxiety and irritability.
The appearance of fear, depression, problems when communicating with others are the first signs of a developing mental disorder, at this stage, a thorough examination and treatment can prevent serious consequences. When assisting patients with psychosis, psychiatrists at the Yusupov Hospital delicately justify the need for therapy, talk about the main activities and their expected impact on the mental state.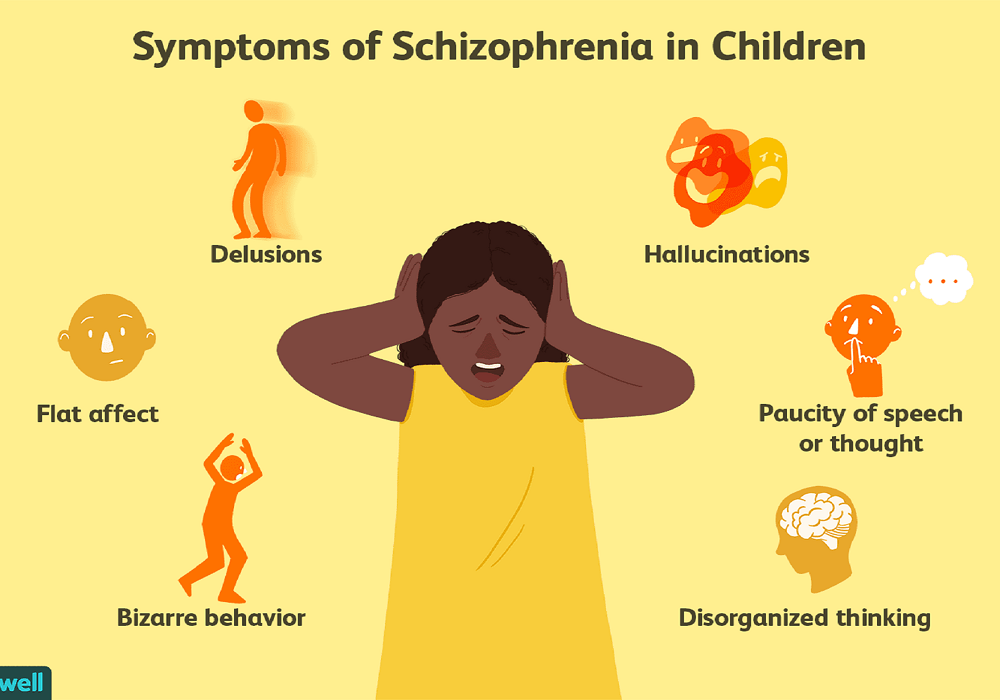
Treatment of psychosis in pregnancy
Postpartum psychosis in women whose symptoms require treatment at the initial stage of therapy is not a basis for registration. In addition, the treatment of this disorder in the Yusupov hospital is carried out anonymously. In most cases, a woman is not aware of the problem, so relatives turn to specialists for help.
Intense manifestations of psychosis during pregnancy or after childbirth may be hospitalized. Patients of the Yusupov hospital are accommodated in comfortable rooms and provided with the necessary hygiene products. Upon admission to the Yusupov hospital, a comprehensive diagnosis is carried out, during which physical problems can be identified, in this case, one of the areas of therapy is their elimination.
The treatment of psychosis in women is carried out in several stages. At the initial stage, the general practitioner, together with other specialists, takes measures to relieve symptoms. During this period, it is necessary to exclude breastfeeding, since the woman is shown taking drugs of various effects.
The next stage of treatment is psychotherapy. After stopping the manifestations of psychosis in women, there is an awareness of the problem, which can cause depression, feelings of guilt. To correct negative attitudes, the therapist uses modern techniques aimed at self-acceptance and stabilization of emotional manifestations. The support of loved ones is important in the treatment of psychosis in women, so relatives can visit the Yusupov hospital patient at any time.
For expert advice and GP visits, contact Yusupov Hospital staff and make an appointment by phone.
Psycho-emotional disorders during pregnancy. The need for their correction | Tyutyunnik V.L., Mikhailova O.I., Chukhareva N.A.
Currently, more and more attention is paid to the influence of a woman's psycho-emotional state on reproductive function, pregnancy and perinatal outcomes [2,4,14]. In recent years, in developed countries, there has been an increase in the frequency of various mental disorders in women of reproductive age, the proportion of patients taking psychotropic drugs has increased, including among women who are planning a pregnancy and pregnant women [3,6,9].
Almost all pregnant women are subject to sharp emotional swings, since the expectation of a child is associated with changes - both physical and emotional. Hormonal changes during pregnancy lead to the fact that the mood of a pregnant woman changes dramatically almost every hour.
A future mother can get rid of such emotional swings and feel calm during pregnancy by observing the rules of emotional health. Emotional balance and physical fitness are equally important for a pregnant woman, they equally help her prepare for motherhood. Due to the lack of maternal experience, a pregnant woman may experience sudden emotional outbursts. The first pregnancy is a new experience that is quite difficult to comprehend. Ignoring the fact that the emotions of a woman who is expecting a child is much more complex and sharper than usual, can lead to a number of problems, including in relations with her spouse. Acceptance of this fact is the basis of emotional health during pregnancy [1,5,11].
Also, if a woman is pregnant for the first time, she experiences many fears, which include fear of childbirth and untimely termination of pregnancy, concern about the health of the unborn child and her own health, fear of labor pains and inevitable pain, fear of partner / spouse disappointment due to changes occurring with body. Modern women have to worry about careers, financial problems, and many additional costs associated with the appearance and upbringing of a new family member.
All these fears can lead to many negative emotions, such as anxiety, depression, irritation, anxiety, stress, anger, feelings of loneliness, confusion. Most often, changes in the psycho-emotional background during pregnancy lead to the development of depressive and anxiety disorders. Until the end, the pathogenesis of these changes is unclear, several theories are discussed, it is believed that changes in the hormonal background during pregnancy, including a significant increase in estrogens, and especially progesterone, in the blood serum can exacerbate existing emotional disorders [5,7,15]. As a rule, minor manifestations in the form of irritability, tearfulness, resentment accompany manifestations of early toxicosis in the first trimester of pregnancy - nausea, vomiting, etc. [6,10]. After the disappearance of these symptoms, the neuropsychic state of pregnant women usually improves. At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
As a rule, minor manifestations in the form of irritability, tearfulness, resentment accompany manifestations of early toxicosis in the first trimester of pregnancy - nausea, vomiting, etc. [6,10]. After the disappearance of these symptoms, the neuropsychic state of pregnant women usually improves. At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
The state of psycho-emotional stress with the presence of anxiety of various levels is observed in 40% of women with a normal pregnancy [2,7,11]. Borderline neuropsychiatric disorders can be presented in the form of hypochondriacal and hysterical syndromes. However, there are other forms of gestational borderline neuropsychiatric disorders, their features are the invariable inclusion in the clinical picture of certain psychopathological phenomena directly related to pregnancy: various fears for the successful course of pregnancy, obsessive fears for the fate of the fetus, expectation of childbirth, conditioned reflex fears associated with unfavorable past pregnancies and childbirth [5,6,8]. A study of pregnant women who do not have signs of borderline neuropsychiatric disorders showed that character accentuation was established only in a quarter of women. The first trimester of pregnancy is usually characterized to some extent by the sharpening of existing character traits. Soft, vulnerable, insecure women become even more impressionable, sometimes excessively tearful, and anxious (those women who have had miscarriages in the past or this pregnancy are not going well, in this case, the fear of another abortion can become simply obsessive) ). Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
Anxiety disorders may first appear during pregnancy, there may be a change in the course of already existing disorders. In one retrospective study in women with panic attacks, 20% of cases showed a decrease in symptoms during pregnancy, 54% remained unchanged, and 26% worsened the course of the disease [12]. The detection of depression in pregnant women is difficult. Many symptoms, such as emotional lability, increased fatigue, changes in appetite and cognitive decline, are often found in physiologically normal pregnancy. Under stress, the hormones of the adrenal glands of the mother release catecholamines (stress hormones) into the blood, and during the experience of positive emotions (joy, calm, etc. ), the hypothalamic structures produce endorphins, which, penetrating through the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
), the hypothalamic structures produce endorphins, which, penetrating through the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
According to the literature [2,5,11,15], a significant effect of anxiety disorders on the course of pregnancy and perinatal outcomes has been noted: the frequency of placental insufficiency, fetal growth retardation, premature birth, the birth of children with low body weight, which subsequently affects negatively on long-term forecast for them.
Thus, emotional swings are dangerous not only for the woman herself, but also for her unborn child. When a pregnant woman experiences stress, her body produces more of the hormone cortisol, the main “stress hormone”. Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Stress during pregnancy is dangerous for a variety of reasons. Chronic stress experienced for several weeks can slow down the development of the cells of the body of the embryo, the growth of the fetus. This increases the risk of miscarriage or spontaneous abortion or premature birth. Elevated levels of stress hormones can damage the brain of an unborn baby and lead to parenting problems later on.
Psychological stress in the perinatal period brings with it a whole range of problems that require serious attention to the psychological sphere of a pregnant woman in order to avoid obstetric and other complications. However, diagnostic criteria for the transition of the stress syndrome from the link of adaptation to the link of pathogenesis of various diseases have not yet been found [2,4,15].
Emotional control is necessary to maintain normal emotional balance during pregnancy. A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
There are several basic rules that will help to cope with emotional imbalance:
• You must come to terms with the fact that physical and emotional changes are an inevitable part of the pregnancy period. You need to understand that this is a temporary stage that will last only a few months and end a maximum of 1-2 months after the birth of the child.
• Each trimester of pregnancy brings new changes, both in the body and in the emotional state. The main source of information about pregnancy is special literature and the experience of women who have recently given birth, who can share their feelings and experiences.
• A pregnant woman is responsible for the emergence of a new life. Taking care of yourself means taking care of your child. Proper nutrition, rest and self-indulgence are essential.
• A pregnant woman should be open to dialogue and not be afraid to discuss her problems with a gynecologist, partner or friends - anyone who can provide emotional support. You should not keep fears and worries in yourself - this will only aggravate internal tension.
You should not keep fears and worries in yourself - this will only aggravate internal tension.
• Changes associated with pregnancy can lead to low energy and, as a result, rapid fatigue. You need to slow down, re-prioritize your work, and give yourself a break.
• Emotional tension and negative emotions can be overcome by being distracted by pleasant activities or hobbies. When emotions overwhelm you, try to analyze what is bothering you, and then find an adequate solution.
• Engaging in certain physical activities designed specifically for expectant mothers will help improve both physical and emotional health.
• The main components of emotional health during pregnancy are rest and comfort.
However, unfortunately, during pregnancy, a woman cannot always cope with nervous tension, irritability, anxiety, excitement and other symptoms of stress on her own. Therefore, in some situations, she needs medical help.
The relative risk of using drugs during pregnancy makes it difficult to choose therapy, therefore, for the correction of psycho-emotional disorders that occur during pregnancy, herbal drugs that have practically no side effects can be considered as highly safe therapy.
The basis of anti-anxiety complex herbal remedies is valerian. It has been used in traditional medicine for many years for its hypnotic and sedative effects and remains a highly sought after remedy to this day. The mild hypnotic effect of valerian makes it possible to use it for the relief of shallow insomnia caused by anxiety. In addition, the vegetotropic effect of valerian is well known, its ability to have a uniform effect on both mental and somatic (vegetative) symptoms of anxiety. Valerian preparations also have anxiolytic and neuroprotective effects. The spectrum of side effects of valerian is very narrow and practically limited only to allergic reactions. Although valerian extract is metabolized by the cytochrome P450 system, it has virtually no effect on the metabolism of other drugs, and thus unwanted drug interactions are excluded.
Among the phytopreparations used by clinicians for the treatment of psycho-emotional disorders, Persen, a modern combined sedative preparation of plant origin, is widely used to relieve stress symptoms (anxiety, irritability and emotional stress) without causing drowsiness. Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
The advantages of Persen over other sedatives are:
• the preparation contains only natural ingredients;
• the effectiveness and safety of herbal ingredients Persena are well studied;
• does not contain alcohol and bromine;
• can be combined with any psychotropic drugs, including antidepressants;
• effective as a fast-acting symptomatic remedy when it is necessary to stop the symptoms of anxiety, agitation, and during a course of treatment for stress conditions, anxiety and phobic disorders.
Due to the natural components of plant origin that are part of Persen, this drug can be used during pregnancy. In each case, the doctor must evaluate the benefits and risks of taking Persen and other drugs, depending on the severity of the symptoms of the disease.
Thus, to prevent possible development, as well as to treat psycho-emotional disorders in pregnant women, it is advisable to use sedatives, the effect of which softens the damaging effects of psychogenic factors.
Literature
1. Abramchenko V.V., Kovalenko N.P. Perinatal psychology: Theory, methodology, experience. Petrozavodsk, 2004. 350s.
2. Avedisova A.S. Anxiety disorders // Alexandrovsky Yu.A. "Mental disorders in general medical practice and their treatment". M: GEOTAR-MED. 2004, pp. 66–73.
3. Voznesenskaya T.G., Fedotova A.V., Fokina N.M. Persen-forte in the treatment of anxiety disorders in patients with psychovegetative syndrome // Treatment of nervous diseases. 2002.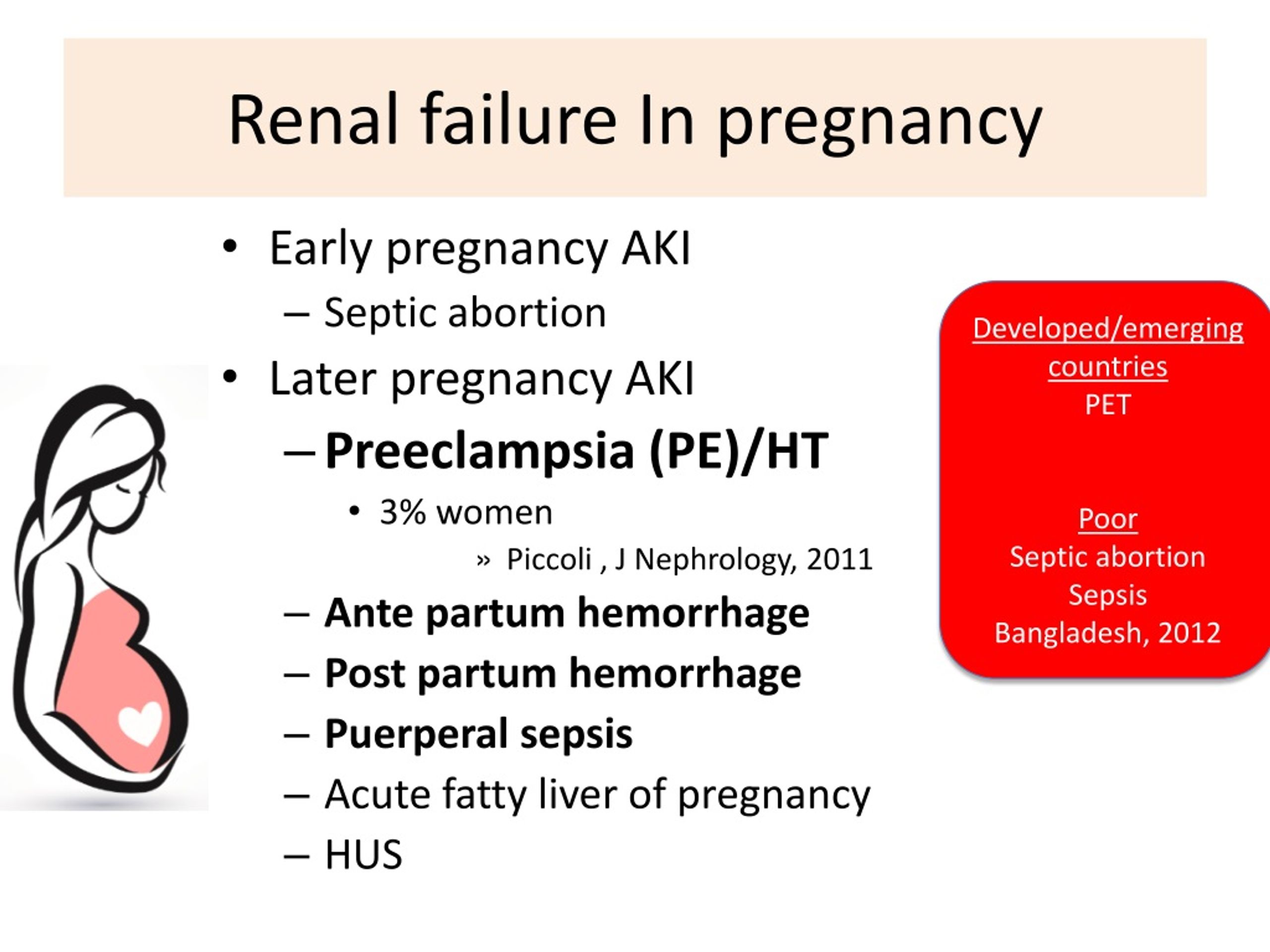 No. 3 (8). pp. 38–41.
No. 3 (8). pp. 38–41.
4. Vorobieva O.V. Psychovegetative syndrome associated with anxiety (issues of diagnosis and therapy) // Russian Medical Journal. 2006. V.14. No. 23. S. 1696–1699.
5. Grandilevskaya I.V. Psychological features of women's response to the identified pathology of pregnancy: Abstract of the thesis. dis. ... cand. psychol. Sciences. SPb., 2004.
6. Kasyanova O.A. Socio-psychological factors in preparing women for pregnancy, childbirth and motherhood: Abstract of the thesis. dis. ... cand. psychol. Sciences. Yaroslavl, 2005.
7. Kovalenko N.P. Psychoprophylaxis and psychocorrection of women during pregnancy and childbirth: Abstract of the thesis. dis. … doc. psychol. Sciences. SPb., 2001.
8. Filippova G.G. Psychological readiness for motherhood // Reader on perinatal psychology: Psychology of pregnancy, childbirth and the postpartum period. M., Izd-vo URAO, 2005. 328 p.
9 Davidson J.R.T. Pharmacotherapy of generalized anxiety // J.