How to plan your pregnancy
Planning for Pregnancy | Preconception Care
If you are trying to have a baby or are just thinking about it, it is not too early to start getting ready for pregnancy. Preconception health and health care focus on things you can do before and between pregnancies to increase the chances of having a healthy baby. For some people, getting their bodies ready for pregnancy takes a few months. For other people, it might take longer. Whether this is your first, second, or sixth baby, the following are important steps to help you get ready for the healthiest pregnancy possible.
1. Make a Plan and Take Action
Whether or not you’ve written them down, you’ve probably thought about your goals for having or not having children, and how to achieve those goals. For example, when you didn’t want to have a baby, you used effective birth control methods to achieve your goals. Now that you’re thinking about getting pregnant, it’s really important to take steps to achieve your goal [PDF – 764 KB]—getting pregnant and having a healthy baby!
Preventive health care can help you stay healthier throughout your life.
2. See Your Doctor
Before getting pregnant, talk to your doctor about preconception health care. Your doctor will want to discuss your health history and any medical conditions you currently have that could affect a pregnancy. They may want to discuss any previous pregnancy problems, medicines you currently are taking, vaccinations you might need, and steps you can take before pregnancy to help prevent certain birth defects.
Take a list of talking points so you don’t forget anything. Be sure to talk to your doctor about:
Medical Conditions
If you currently have any medical conditions, be sure they are under control and being treated. Some of these conditions include: sexually transmitted diseases (STDs), diabetes, thyroid disease, high blood pressure, and other chronic diseases.
Lifestyle and Behaviors
Talk with your doctor or another health professional if you smoke, drink alcohol, or use certain drugs; live in a stressful or abusive environment; or work with or live around toxic substances. Health care professionals can help you with counseling, treatment, and other support services.
Health care professionals can help you with counseling, treatment, and other support services.
Medications
Almost every pregnant person will face a decision about taking medicines before and during pregnancy. Talk to your healthcare providers before starting or stopping any medicines. Be sure to discuss the following with your healthcare providers:
- All medicines you take, including prescriptions, over-the-counter medicines, herbal and dietary supplements, and vitamins
- Best ways to keep any health conditions you have under control
- Your personal goals and preferences for the health of you and your baby
Vaccinations (shots)
Some vaccinations are recommended before you become pregnant, during pregnancy, or right after delivery. Having the right vaccinations at the right time can help keep you healthy and help keep your baby from getting very sick or having lifelong health problems.
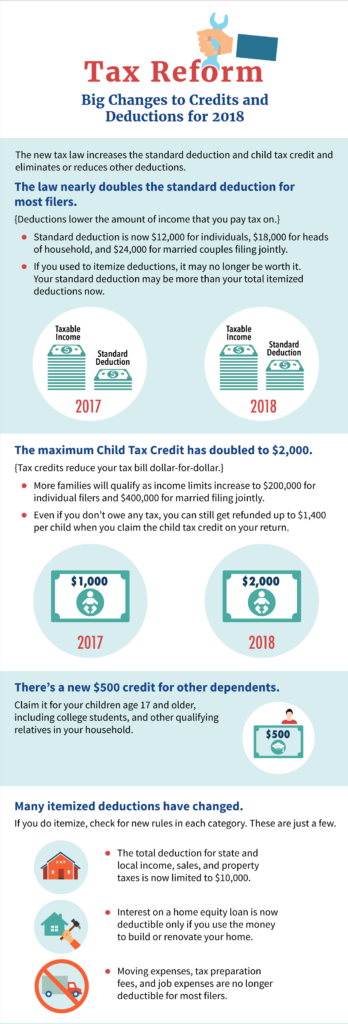
3. Take 400 Micrograms of Folic Acid Every Day
Folic acid is a B vitamin. CDC urges all people who can become pregnant to take 400 micrograms (mcg) of folic acid each day, in addition to consuming food with folate from a varied diet, to help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida).
CDC urges all people who can become pregnant to take 400 micrograms (mcg) of folic acid each day, in addition to consuming food with folate from a varied diet, to help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida).
Learn more about folic acid »
4. Stop Drinking Alcohol, Smoking, and Using Certain Drugs
Smoking, drinking alcohol, and using certain drugs can cause many problems during pregnancy, such as premature birth, birth defects, and infant death.
If you are trying to get pregnant and cannot stop drinking, smoking, or using drugs, contact your healthcare provider, local Alcoholics Anonymous, or local alcohol treatment center.
Alcohol and Drug Resources
Substance Abuse Treatment Facility Locator
The Substance Abuse and Mental Health Services Administration (SAMHSA) has a treatment facility locator. This locator helps people find drug and alcohol treatment programs in their area.
Alcoholics Anonymous (A. A.)
A.)
Alcoholics Anonymous® is a fellowship of men and women who share their experiences, strengths, and hopes with each other so that they can solve their common problem and help others to recover from alcoholism. Locate an A.A. program near you.
Learn more about alcohol and pregnancy »
Smoking Resources
1-800-QUIT-NOW (1-800-784-8669)
Learn more about smoking during pregnancy »
5. Avoid Toxic Substances and Environmental Contaminants
Avoid harmful chemicals, environmental contaminants, and other toxic substances such as synthetic chemicals, metals, fertilizer, bug spray, and cat or rodent feces around the home and in the workplace. These substances can hurt the reproductive systems of men and women. They can make it more difficult to get pregnant. Exposure to even small amounts during pregnancy, infancy, childhood, or puberty can lead to diseases. Learn how to protect yourself and your loved ones from toxic substances at work and at home.
Learn about the effects of toxic substances on reproductive health »
Learn how CDC tracks Children’s Environmental Health »
6.
 Reach and Maintain a Healthy Weight
Reach and Maintain a Healthy WeightPeople who are overweight or obese have a higher risk for many serious conditions, including complications during pregnancy, heart disease, type 2 diabetes, and certain cancers (endometrial, breast, and colon).1 People who are underweight are also at risk for serious health problems.2
The key to achieving and maintaining a healthy weight isn’t about short-term dietary changes. It’s about a lifestyle that includes healthy eating and regular physical activity.
If you are underweight, overweight, or obese, talk with your doctor about ways to reach and maintain a healthy weight before you get pregnant.
Learn more about healthy weight »
7. Learn Your Family History
Collecting your family’s health history can be important for your child’s health. You might not realize that your sister’s heart defect or your cousin’s sickle cell disease could affect your child, but sharing this family history information with your doctor can be important.
Other reasons people go for genetic counseling include having had several miscarriages, infant deaths, trouble getting pregnant (infertility), or a genetic condition or birth defect that occurred during a previous pregnancy.
Learn more about family history »
Learn more about genetic counseling »
8. Get Mentally Healthy
Mental health is how we think, feel, and act as we cope with life. To be at your best, you need to feel good about your life and value yourself. Everyone feels worried, anxious, sad, or stressed sometimes. However, if these feelings do not go away and they interfere with your daily life, get help. Talk with your doctor or another health professional about your feelings and treatment options.
Learn about mental health »
Learn about depression »
References
- NIH, NHLBI Obesity Education Initiative. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Available online:
http://www. nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf (PDF-1.25Mb)
nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf (PDF-1.25Mb) - Moos, Merry-K, et al. Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age. AJOG Volume 199, Issue 6, Supplement B , Pages S280-S289, December 2008.
Planning your pregnancy - NHS
You can improve your chances of getting pregnant and having a healthy pregnancy by following the steps on this page.
Take a folic acid supplement
It's recommended that you should take a daily supplement of folic acid when you're pregnant, or there's a chance you might get pregnant.
You should take a 400 microgram supplement of folic acid every day before you get pregnant, and every day afterwards, up until you're 12 weeks pregnant.
A microgram is 1,000 times smaller than a milligram (mg). The word microgram is sometimes written with the Greek symbol μ followed by the letter g (μg).
Folic acid reduces the risk of your baby having a neural tube defect, such as spina bifida.
A neural tube defect is when the foetus's spinal cord (part of the body's nervous system) does not form normally.
You might be advised to take a higher dose supplement of 5 milligram (5mg) every day.
You may need to take a 5mg supplement of folic acid if:
- you or the baby's other biological parent have a neural tube defect
- you previously had a pregnancy affected by a neural tube defect
- you or the baby's other biological parent have a family history of neural tube defects
- you have diabetes
- you take anti-epilepsy medicine
Talk to a GP if you think you need a 5mg dose of folic acid, as they can prescribe a higher dose.
You can get folic acid tablets at pharmacies, or talk to a GP about getting a prescription.
Do not worry if you get pregnant unexpectedly and were not taking a folic acid supplement at the time. Start taking them as soon as you find out, until you're past the first 12 weeks of pregnancy.
Stop smoking
Smoking during pregnancy has been linked to a variety of health problems, including:
- premature birth
- low birth weight
- sudden infant death syndrome (SIDS), also known as cot death
- miscarriage
- breathing problems or wheezing in the first 6 months of life
Quitting can be hard, no matter how much you want to, but support is available.
NHS Smokefree offers free help, support and advice on stopping smoking, including when you're pregnant, and can give you details of local support services.
Smoke from other people's cigarettes can damage your baby, so ask your partner, friends and family not to smoke near you.
Cut out alcohol
Do not drink alcohol if you're pregnant or trying to get pregnant. Alcohol can be passed to your unborn baby.
Drinking in pregnancy can lead to long-term harm to your baby, and the more you drink, the greater the risk.
Find out about alcohol and pregnancy, alcohol units and tips for cutting down.
Keep to a healthy weight
If you're overweight, you may have problems getting pregnant and fertility treatment is less likely to work.
Being overweight (having a BMI over 25) or obese (having a BMI over 30) also raises the risk of some pregnancy problems, such as high blood pressure, deep vein thrombosis, miscarriage and gestational diabetes.
Before you get pregnant you can use the BMI healthy weight calculator to find out your BMI. But this may not be accurate once you're pregnant, so consult your midwife or doctor.
Having a healthy diet and doing moderate exercise are advised in pregnancy, and it's important not to gain too much weight.
You can keep to a healthy weight by having a balanced diet and doing regular exercise.
Know which medicines you can take
Not all medicines are safe to take when you're pregnant or planning a pregnancy, whether they're on prescription or medicines you can buy in a pharmacy or shop.
Information:
If you take prescribed medicine and you're planning to get pregnant, talk to a doctor.
Do not stop taking your medicine without talking to a doctor.
Find out about medicines in pregnancy.
Vaccinations and infections
Some infections, such as rubella (German measles), can harm your baby if you catch them during pregnancy.
Most people in the UK are immune to rubella, thanks to the uptake of the measles, mumps and rubella (MMR) vaccination.
If you have not had 2 doses of the MMR vaccine, or you're not sure if you have, ask your GP surgery to check your vaccination history.
If you have not had both doses or there's no record available, you can have the vaccinations at your GP surgery.
You should avoid getting pregnant for 1 month after having the MMR vaccination, which means you'll need a reliable method of contraception.
Talk to a doctor if you have a long-term condition
If you have a long-term condition, such as epilepsy or diabetes, it could affect the decisions you make about your pregnancy – for example, where you might want to give birth.
Before you get pregnant, have a discussion with your specialist or a GP about getting pregnant.
If you're taking medicine for a condition, do not stop taking it without talking to a doctor.
Testing for sickle cell and thalassaemia
Sickle cell disease (SCD) and thalassaemia are inherited blood disorders that mainly affect people whose ancestors come from Africa, the Caribbean, the Mediterranean, India, Pakistan, south and Southeast Asia, and the Middle East.
If you are pregnant and live in England you will be offered screening tests for these disorders, but you do not have to wait until you're pregnant before you have a test.
If you or your partner are concerned you may be a carrier for 1 of these disorders, perhaps because someone in your family has a blood disorder or is a carrier, it's a good idea to get tested before starting a family.
You can ask for a free blood test from either a GP or a local sickle cell and thalassaemia centre.
Find out more about screening for sickle cell and thalassaemia in pregnancy
where to start and what you need to know
Table of contents:
- Consider your age
- Stop smoking
- Adjust physical activity
- Get tested
- Start using vitamin-mineral complexes
- Maintain a healthy lifestyle
As a rule, a couple starts planning a new addition to the family a year or two before the birth of a child, but is this period enough? The lifestyle and habits you adopt now can have a big impact on conception, pregnancy, and the health of your baby in the long run. Where should you start and what do you need to know now?
Consider your age
Doctors agree that the optimal age for the first pregnancy is 20-29 years, and after 30-35 years is a good time for a second pregnancy. This is the official opinion, however, the age limits today are rather arbitrary. With a high level of modern medicine, a woman can safely endure and give birth to a child at the age of 40, and even later, although control by a doctor will be strengthened.
This is the official opinion, however, the age limits today are rather arbitrary. With a high level of modern medicine, a woman can safely endure and give birth to a child at the age of 40, and even later, although control by a doctor will be strengthened.
From a psychological point of view, one of the main difficulties of late pregnancy is the obsessive desire of the expectant mother to make this time and childbirth ideal. But with good intentions, she drives herself into real stress: constant excitement, overload in numerous classes, fears, restructuring to a new mode of life do not benefit the child. Advance pregnancy planning will help you avoid difficulties in carrying a baby at any age, adjust your lifestyle in advance and prevent possible complications during childbirth.
Quit smoking
The dangers of smoking are not empty words. Women who smoke have been shown to go through menopause earlier, are more likely to have estrogen deficiency, and, in addition, smoking has a negative effect on metabolism. If you are still prone to this destructive habit, remember that between the last cigarette and conception should be at least a year. In the event that pregnancy has become a pleasant surprise for you, smoking should be stopped immediately - every cigarette smoked prevents the proper development of the embryo. For example, toxic nicotine and tar interfere with blood circulation in the placenta, which means that oxygen enters the baby's body in insufficient quantities. In addition to oxygen starvation, children are deficient in many nutrients and trace elements. Not surprisingly, babies are often born underweight 1 . Let the prospect of becoming a mother be a good motivation to quit smoking right now or think seriously about the need for this step.
If you are still prone to this destructive habit, remember that between the last cigarette and conception should be at least a year. In the event that pregnancy has become a pleasant surprise for you, smoking should be stopped immediately - every cigarette smoked prevents the proper development of the embryo. For example, toxic nicotine and tar interfere with blood circulation in the placenta, which means that oxygen enters the baby's body in insufficient quantities. In addition to oxygen starvation, children are deficient in many nutrients and trace elements. Not surprisingly, babies are often born underweight 1 . Let the prospect of becoming a mother be a good motivation to quit smoking right now or think seriously about the need for this step.
Correct physical activity
The main brain center - the hypothalamus - was formed in the prehistoric era, and this explains some of the vicissitudes of its work. According to experts, the hypothalamus may perceive fast running as a way to escape from danger, and regard a lack of vitamins as hunger. The center transmits disturbing information to the reproductive system, and as a result, the body “thinks” that it is not the best time for reproduction. That is why, instead of active sports, when planning a pregnancy, it is better to do recreational physical education. So, long walks in the fresh air during daylight hours are useful: you enjoy communication or music, the body is saturated with oxygen and vitamin D, and the muscles receive a moderate load.
The center transmits disturbing information to the reproductive system, and as a result, the body “thinks” that it is not the best time for reproduction. That is why, instead of active sports, when planning a pregnancy, it is better to do recreational physical education. So, long walks in the fresh air during daylight hours are useful: you enjoy communication or music, the body is saturated with oxygen and vitamin D, and the muscles receive a moderate load.
Get tested
As a preventive measure, a woman under 25 should be screened for chlamydia trachomatis and mycoplasma genitalium at least once a year, other tests can be ordered by a gynecologist only if alarming symptoms are detected.
Testing for the presence of antibodies in the blood and timely vaccination against rubella will protect against unwanted risks. For the unborn child, diseases and not at all of a gynecological nature can pose a danger. When planning a pregnancy, the first thing to do is to find out if you have had rubella: the virus that enters the mother's body during pregnancy is instantly transmitted to the child and can lead to serious consequences for his health (cataracts, deafness, heart disease and other defects).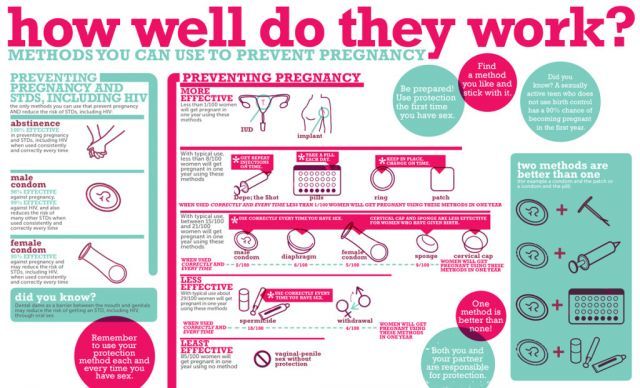 Testing for the presence of antibodies in the blood and timely vaccination against rubella will protect against unwanted risks 2 . For the health of the baby, those diseases acquired during the life of the mother that can negatively affect hormonal homeostasis and disrupt the secretion of hormones in the placenta are also important. First of all, we are talking about diseases of the thyroid gland, diabetes and others. Of course, they should not become an obstacle to conception, but you should assess the risks and consult a doctor in advance in order to properly adjust your lifestyle and, if necessary, start timely treatment.
Testing for the presence of antibodies in the blood and timely vaccination against rubella will protect against unwanted risks 2 . For the health of the baby, those diseases acquired during the life of the mother that can negatively affect hormonal homeostasis and disrupt the secretion of hormones in the placenta are also important. First of all, we are talking about diseases of the thyroid gland, diabetes and others. Of course, they should not become an obstacle to conception, but you should assess the risks and consult a doctor in advance in order to properly adjust your lifestyle and, if necessary, start timely treatment.
If you are unable to conceive, do not rush to conclusions: infertility is a clinical diagnosis made by a doctor to a healthy couple of reproductive age who have had a regular sexual life for a year and are not able to conceive a child. Experts explain that regular sex life is unprotected sexual intercourse, repeated 2-3 times a week, regardless of the woman's menstrual cycle. Only a doctor can determine infertility, prescribe an examination, suggest methods of treatment or alternative options for conceiving a child.
Only a doctor can determine infertility, prescribe an examination, suggest methods of treatment or alternative options for conceiving a child.
Start taking vitamin-mineral complexes
Folic acid is one of the key vitamins that a woman should regularly take in, especially during pregnancy planning. With its deficiency at the time of fetal formation, the risk of neural tube defects in a child, which is formed during the first 28 days after conception, is significantly increased. In addition, with a lack of folic acid, other malformations may develop, the risk of miscarriage and termination of pregnancy increases. Of course, not only folic acid is important, but also a whole complex of related vitamins.
It has been proven that the protective properties of folic acid are better manifested in combination with other vitamins: groups B, C, PP. It has been proven that the protective properties of folic acid are better manifested in combination with other vitamins: gr.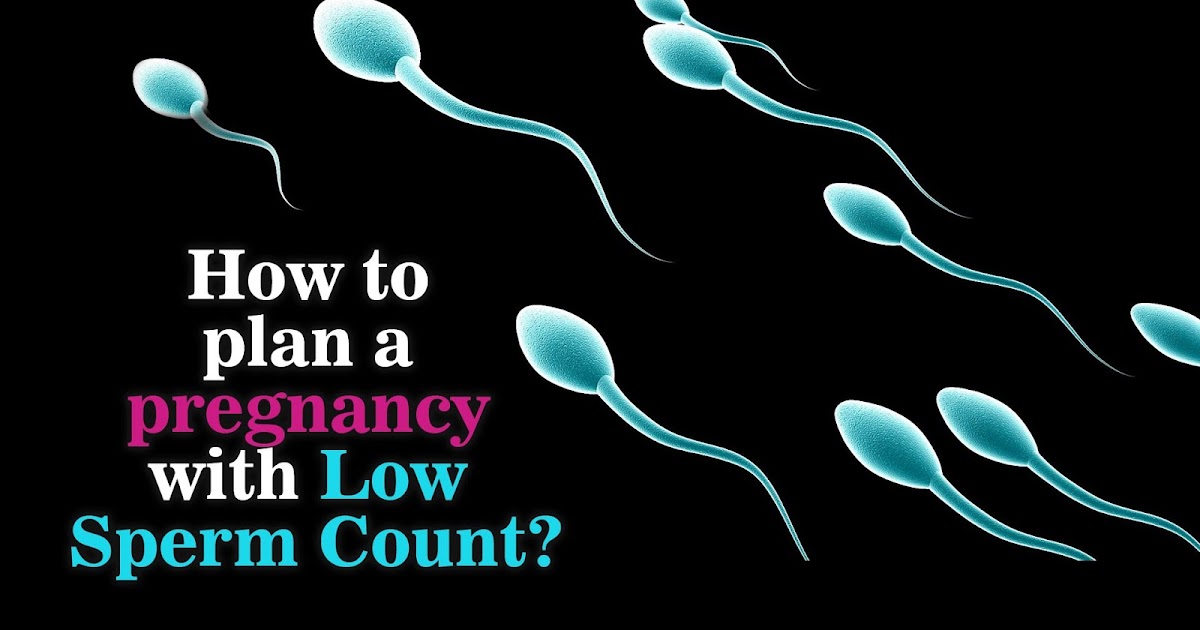 B, C, PP 3 . The role of vitamins A, C, E, D, as well as calcium, magnesium, zinc and many other trace elements cannot be underestimated. It is no secret that during pregnancy the body must produce more blood than usual: part of it is spent on the formation of the placenta, and part is transferred to the child. Iron plays a key role in the processes of hematopoiesis. If before pregnancy the required daily dose of iron for a woman is 18 mg, then with the onset of pregnancy, the “norm” rises to 33 mg 4 . Where do you get these "building materials" for your body?
B, C, PP 3 . The role of vitamins A, C, E, D, as well as calcium, magnesium, zinc and many other trace elements cannot be underestimated. It is no secret that during pregnancy the body must produce more blood than usual: part of it is spent on the formation of the placenta, and part is transferred to the child. Iron plays a key role in the processes of hematopoiesis. If before pregnancy the required daily dose of iron for a woman is 18 mg, then with the onset of pregnancy, the “norm” rises to 33 mg 4 . Where do you get these "building materials" for your body?
Yes, many vitamins and nutrients enter the body with food, but not all and not in the optimal need - heat treatment of food simply “kills” some of the vitamins, in addition, some foods are not always present in our diet in the right amount (for example , seafood, fresh herbs).
Lead a healthy lifestyle
It turns out that inactivity, unbalanced nutrition and stress have a bad effect on a woman’s fertility 5 . You should start to lead a healthy lifestyle as early as possible, because otherwise pregnancy may not occur at all. In order to prolong the reproductive period, pay attention to your diet, use vitamin complexes, try to spend more time outdoors, have active rest, stop smoking and reduce alcohol consumption 6 . Sleep is an equally important component of a healthy lifestyle. According to doctors, a person should sleep at least 7 and preferably no more than 9hours per day. It is not so important when you fall asleep and get up - just do it at the same time. It is necessary to start developing the rules of the daily routine before the onset of pregnancy, so that in a difficult period the body does not experience additional stress when getting used to them, but accepts them with ease, at the level of biorhythms. Before going to bed, perform your own ritual: take a bath, drink a glass of milk, brush your teeth. Over time, you will begin to yawn during these actions. The mode for the body is equal to calmness and stability, and these are the best conditions for conceiving offspring.
You should start to lead a healthy lifestyle as early as possible, because otherwise pregnancy may not occur at all. In order to prolong the reproductive period, pay attention to your diet, use vitamin complexes, try to spend more time outdoors, have active rest, stop smoking and reduce alcohol consumption 6 . Sleep is an equally important component of a healthy lifestyle. According to doctors, a person should sleep at least 7 and preferably no more than 9hours per day. It is not so important when you fall asleep and get up - just do it at the same time. It is necessary to start developing the rules of the daily routine before the onset of pregnancy, so that in a difficult period the body does not experience additional stress when getting used to them, but accepts them with ease, at the level of biorhythms. Before going to bed, perform your own ritual: take a bath, drink a glass of milk, brush your teeth. Over time, you will begin to yawn during these actions. The mode for the body is equal to calmness and stability, and these are the best conditions for conceiving offspring.
How to prepare for conception?
Pregnancy planning is really necessary, especially in our time, when a healthy woman is the exception rather than the rule. Not to mention the fact that pregnancy is a serious test for the body of even a perfectly healthy woman.
It can be said that entering into pregnancy without preliminary preparation for it is the same as flying on an airplane that has not been checked in advance: maybe it will cost, or maybe not. Of course, aircraft are tested before each flight. So why does a woman, ready to give birth to a new human being, not always conduct a similar check of her body? After all, the price of her neglect of herself and her health can be the life of the unborn child.
The process of preparing for pregnancy is quite complex and includes several stages. It is worth starting planning a few months (at least three) before the time when the couple intends to conceive a baby.
And at the stage of pregnancy planning , it is necessary to understand that the bearing and birth of a baby is not a woman's business, but a married couple's.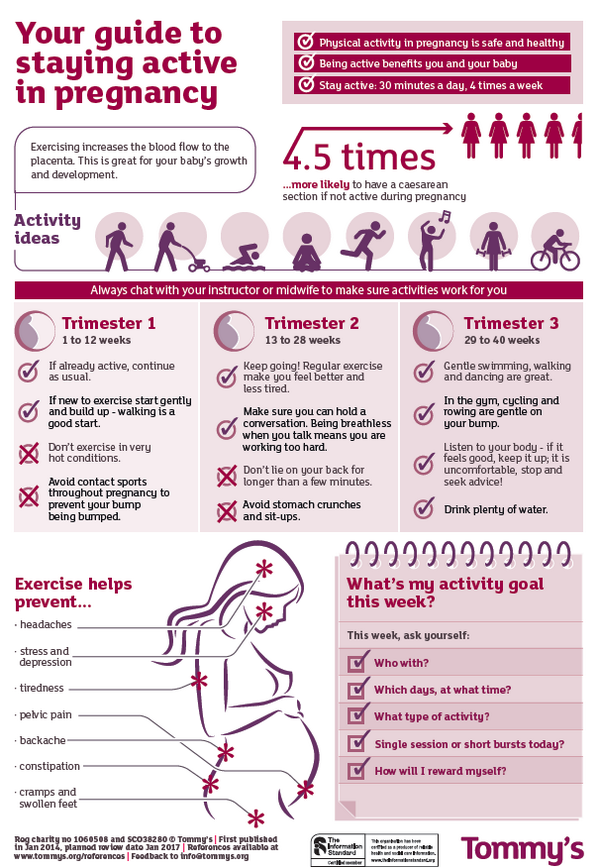 Therefore, the active participation of the father in planning pregnancy is extremely necessary and important for himself, and for his wife, and for the unborn baby.
Therefore, the active participation of the father in planning pregnancy is extremely necessary and important for himself, and for his wife, and for the unborn baby.
Without the help of doctors, it will not be possible to manage even at this stage. A visit to the gynecologist will allow you to identify possible diseases and treat them in a timely manner. After the first appeal, future parents undergo several examinations and pass certain tests in order to find out how ready their bodies are for conceiving a baby, as well as to prevent possible problems when carrying a child. The gynecologist will tell you what to do if, before planning a pregnancy, a woman was protected with hormonal contraceptives. It is necessary to stop taking hormonal contraceptives 3 months before the planned pregnancy.
It is important for a future mother to understand that only a healthy woman can bear and give birth to a healthy baby. In this regard, you need to start taking care of your own health long before conception. Good physical shape, the absence of diseases, proper nutrition and the rejection of bad habits, hygiene and a measured lifestyle - all this has a beneficial effect on the female body and subsequently makes it easier to endure pregnancy. However, not all vitamins can be obtained from food. For example, the body can only obtain folic acid in an artificial form, since its counterpart (folate), found in green vegetables, beans, asparagus, and citrus fruits, is much less absorbed. Folic acid is very important for the development of the baby to take place correctly, and the need for its intake exists throughout pregnancy. If the mother's body during the bearing of the child receives a sufficient amount of this substance, then the risk of pathology from the nervous system is minimized.
Good physical shape, the absence of diseases, proper nutrition and the rejection of bad habits, hygiene and a measured lifestyle - all this has a beneficial effect on the female body and subsequently makes it easier to endure pregnancy. However, not all vitamins can be obtained from food. For example, the body can only obtain folic acid in an artificial form, since its counterpart (folate), found in green vegetables, beans, asparagus, and citrus fruits, is much less absorbed. Folic acid is very important for the development of the baby to take place correctly, and the need for its intake exists throughout pregnancy. If the mother's body during the bearing of the child receives a sufficient amount of this substance, then the risk of pathology from the nervous system is minimized.
What tests should a married couple undergo
before planning a pregnancy?
- Gynecological examination, colposcopy for women.
- Blood type, Rh factor for both spouses.
 If a woman has a positive Rh factor, there is no problem. If a woman has a negative Rh factor - antibodies to the Rh factor (even if a man is also negative). If they are positive, pregnancy is not currently possible and needs to be corrected. If negative - repeat this analysis once a month, starting from 8 weeks of pregnancy. If a woman has 1 group, and a man has any other group, incompatibility by blood types is possible. An analysis for group antibodies, as well as an analysis for antibodies to the Rh factor, is carried out once a month, starting from 8 weeks of pregnancy.
If a woman has a positive Rh factor, there is no problem. If a woman has a negative Rh factor - antibodies to the Rh factor (even if a man is also negative). If they are positive, pregnancy is not currently possible and needs to be corrected. If negative - repeat this analysis once a month, starting from 8 weeks of pregnancy. If a woman has 1 group, and a man has any other group, incompatibility by blood types is possible. An analysis for group antibodies, as well as an analysis for antibodies to the Rh factor, is carried out once a month, starting from 8 weeks of pregnancy. - Tests for infections: routine smear, PCR for latent infections - both spouses.
- Blood test for TORCH-complex. Antibodies to rubella, toxoplasma, herpes, CMV, chlamydia - quantitative analysis (with titer). The presence of IgG antibodies means immunity to these infections, and is not an obstacle to pregnancy. The presence of IgM means an acute stage, planning in this case must be postponed until recovery.
 If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it.
If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it. - A trip to the dentist, a therapist, chest x-ray is a must for both spouses. By appointment of the therapist - consultation of narrow specialists (ENT doctor, urologist, endocrinologist, cardiologist, gastroenterologist).
- Spermogram. Desirable, but not required. It is done to determine the quality of spermatozoa and identify a hidden inflammatory process (a much more informative analysis than any smears and PCR).
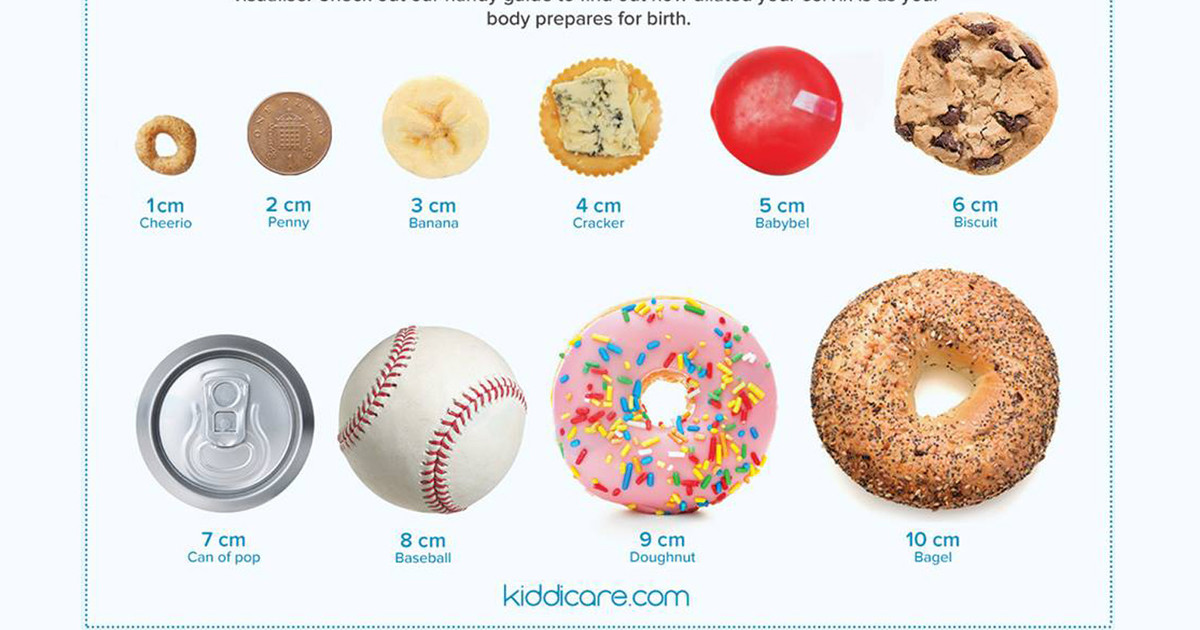
- Ultrasound of the pelvic organs - at least 2 times per cycle: after menstruation and before menstruation. For the first time, the general condition of the pelvic organs is assessed, in the second, the presence of a corpus luteum and endometrial transformation, indicating that ovulation has occurred. Ideally, an intermediate third ultrasound on the eve of the expected ovulation is to detect the dominant follicle.
- Blood test for hormones of the reproductive system, thyroid gland, adrenal glands - according to indications.