Dark colored skin
Skin - abnormally dark or light Information | Mount Sinai
Hyperpigmentation; Hypopigmentation; Skin - abnormally light or dark
Abnormally dark or light skin is skin that has turned darker or lighter than normal.
The white spots on this person's face have resulted from drug-induced vitiligo. Loss of melanin, the primary skin pigment, occasionally occurs as a result of medicines, as is the case with this individual. The typical vitiligo lesion is flat and depigmented, but maintains the normal skin texture.
This is a picture of vitiligo on the face. Complete loss of melanin, the primary skin pigment, occurs for unknown reasons. The resulting lesions are white in comparison to the surrounding skin. Vitiligo may occur in the same areas on both sides of the face -- symmetrically -- or it may be patchy -- asymmetrical. The typical vitiligo lesion is flat and depigmented, but maintains the normal skin texture. The dark areas around the eyes are this person's normal skin color.
Incontinentia pigmenti produces darkly-pigmented swirling marks on the skin. It occurs more frequently in females. The skin lesions are divided into three stages blisters (vesicles and bullae) are present at birth or within the first 6 to 7 weeks, followed by a rough wart-like (verrucous) stage, and lastly, swirled and bizarre patterns of dark pigmentation (hyperpigmentation) appear.
Incontinentia pigmenti produces darkly-pigmented swirling marks on the skin. It occurs more frequently in females. The skin lesions are divided into three stages blisters (vesicles and bullae) are present at birth or within the first 6 to 7 weeks, followed by a rough wart-like (verrucous) stage, and lastly, swirled and bizarre patterns of dark pigmentation (hyperpigmentation) appear.
It occurs more frequently in females. The skin lesions are divided into three stages blisters (vesicles and bullae) are present at birth or within the first 6 to 7 weeks, followed by a rough wart-like (verrucous) stage, and lastly, swirled and bizarre patterns of dark pigmentation (hyperpigmentation) appear.
Hyperpigmentation refers to skin that has turned darker than normal where the change that has occurred is unrelated to sun exposure. Cells called melanocytes located in the skin, produce melanin. Melanin gives the skin its color. In certain conditions melanocytes can become abnormal and cause an excessive amount of darkening in the color of the skin.
Hyperpigmented concentric rings over the tibia are secondary to prior inflammation. Residual hemosiderin from broken down red blood cells in macrophages, left behind after inlammation pigments the skin.
Generalized hyperpigmentation, in addition to localized areas of even deeper pigmentation is sometimes found in patients with malignancy. Etiology of these pigmentary changes is varied.
Etiology of these pigmentary changes is varied.
Post-inflammatory hyperpigmentation is seen here in a mottled pattern, over the posterior shoulder. Hemosiderin, left behind by degraded RBC's, creates the discoloration.
Considerations
Normal skin contains cells called melanocytes. These cells produce melanin, the substance that gives skin its color.
Skin with too much melanin is called hyperpigmented skin.
Skin with too little melanin is called hypopigmented. Skin with no melanin at all is called depigmented.
Pale skin areas are due to too little melanin or underactive melanocytes. Darker areas of skin (or an area that tans more easily) occurs when you have more melanin or overactive melanocytes.
Bronzing of the skin may sometimes be mistaken for a suntan. This skin discoloration often develops slowly, starting at the elbows, knuckles, and knees and spreading from there. Bronzing may also be seen on the soles of the feet and the palms of the hands. The bronze color can range from light to dark (in fair-skinned people) with the degree of darkness due to the underlying cause.
Bronzing may also be seen on the soles of the feet and the palms of the hands. The bronze color can range from light to dark (in fair-skinned people) with the degree of darkness due to the underlying cause.
Causes
Causes of hyperpigmentation include:
- Skin inflammation (post-inflammatory hyperpigmentation)
- Use of certain drugs (such as minocycline, certain cancer chemotherapies, and birth control pills)
- Hormone system diseases such as Addison disease
- Hemochromatosis (iron overload)
- Sun exposure
- Pregnancy (melasma, or mask of pregnancy)
- Certain birthmarks
Causes of hypopigmentation include:
- Skin inflammation
- Certain fungal infections (such as tinea versicolor)
- Pityriasis alba
- Vitiligo
- Certain medicines
- Skin condition called idiopathic guttate hypomelanosis in sun exposed areas such as the arms
- Certain birthmarks
Home Care
Over-the-counter and prescription creams are available for lightening the skin. Hydroquinone combined with tretinoin is an effective combination. If you use these creams, follow instructions carefully, and don't use one for more than 3 weeks at a time. Darker skin requires greater care when using these preparations. Cosmetics may also help mask a discoloration.
Hydroquinone combined with tretinoin is an effective combination. If you use these creams, follow instructions carefully, and don't use one for more than 3 weeks at a time. Darker skin requires greater care when using these preparations. Cosmetics may also help mask a discoloration.
Avoid too much sun exposure. Always use sunscreen with an SPF of 30 or higher.
Abnormally dark skin may continue even after treatment.
When to Contact a Medical Professional
Call your health care provider for an appointment if you have:
- Skin discoloration that causes significant concern
- Persistent, unexplained darkening or lightening of the skin
- Any skin sore or lesion that changes shape, size, or color may be a sign of skin cancer
What to Expect at Your Office Visit
Your provider will perform a physical exam and ask about your symptoms, including:
- When did the discoloration develop?
- Did it develop suddenly?
- Is it getting worse? How fast?
- Has it spread to other parts of the body?
- What medicines do you take?
- Has anyone else in your family had a similar problem?
- How often are you in the sun? Do you use a sun lamp or go to tanning salons?
- What is your diet like?
- What other symptoms do you have? For example, are there any rashes or skin lesions?
Tests that may be done include:
- Adrenocorticotrophin hormone stimulation test
- Skin biopsy
- Thyroid function studies
- Wood lamp test
- KOH test
Your provider may recommend creams, ointments, surgery, or phototherapy, depending on the type of skin condition you have. Bleaching creams can help lighten dark areas of skin.
Bleaching creams can help lighten dark areas of skin.
Some skin color changes may return to normal without treatment.
Chang MW. Disorders of hyperpigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 67.
Passeron T, Ortonne JP. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 66.
Last reviewed on: 6/19/2021
Reviewed by: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Abnormally dark or light skin: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus. gov/ency/article/003242.htm
gov/ency/article/003242.htm
To use the sharing features on this page, please enable JavaScript.
Abnormally dark or light skin is skin that has turned darker or lighter than normal.
Normal skin contains cells called melanocytes. These cells produce melanin, the substance that gives skin its color.
Skin with too much melanin is called hyperpigmented skin.
Skin with too little melanin is called hypopigmented. Skin with no melanin at all is called depigmented.
Pale skin areas are due to too little melanin or underactive melanocytes. Darker areas of skin (or an area that tans more easily) occurs when you have more melanin or overactive melanocytes.
Bronzing of the skin may sometimes be mistaken for a suntan. This skin discoloration often develops slowly, starting at the elbows, knuckles, and knees and spreading from there. Bronzing may also be seen on the soles of the feet and the palms of the hands. The bronze color can range from light to dark (in fair-skinned people) with the degree of darkness due to the underlying cause.
The bronze color can range from light to dark (in fair-skinned people) with the degree of darkness due to the underlying cause.
Causes of hyperpigmentation include:
- Skin inflammation (post-inflammatory hyperpigmentation)
- Use of certain drugs (such as minocycline, certain cancer chemotherapies, and birth control pills)
- Hormone system diseases such as Addison disease
- Hemochromatosis (iron overload)
- Sun exposure
- Pregnancy (melasma, or mask of pregnancy)
- Certain birthmarks
Causes of hypopigmentation include:
- Skin inflammation
- Certain fungal infections (such as tinea versicolor)
- Pityriasis alba
- Vitiligo
- Certain medicines
- Skin condition called idiopathic guttate hypomelanosis in sun exposed areas such as the arms
- Certain birthmarks
Over-the-counter and prescription creams are available for lightening the skin. Hydroquinone combined with tretinoin is an effective combination. If you use these creams, follow instructions carefully, and don't use one for more than 3 weeks at a time. Darker skin requires greater care when using these preparations. Cosmetics may also help mask a discoloration.
If you use these creams, follow instructions carefully, and don't use one for more than 3 weeks at a time. Darker skin requires greater care when using these preparations. Cosmetics may also help mask a discoloration.
Avoid too much sun exposure. Always use sunscreen with an SPF of 30 or higher.
Abnormally dark skin may continue even after treatment.
Call your health care provider for an appointment if you have:
- Skin discoloration that causes significant concern
- Persistent, unexplained darkening or lightening of the skin
- Any skin sore or lesion that changes shape, size, or color may be a sign of skin cancer
Your provider will perform a physical exam and ask about your symptoms, including:
- When did the discoloration develop?
- Did it develop suddenly?
- Is it getting worse? How fast?
- Has it spread to other parts of the body?
- What medicines do you take?
- Has anyone else in your family had a similar problem?
- How often are you in the sun? Do you use a sun lamp or go to tanning salons?
- What is your diet like?
- What other symptoms do you have? For example, are there any rashes or skin lesions?
Tests that may be done include:
- Adrenocorticotrophin hormone stimulation test
- Skin biopsy
- Thyroid function studies
- Wood lamp test
- KOH test
Your provider may recommend creams, ointments, surgery, or phototherapy, depending on the type of skin condition you have. Bleaching creams can help lighten dark areas of skin.
Bleaching creams can help lighten dark areas of skin.
Some skin color changes may return to normal without treatment.
Hyperpigmentation; Hypopigmentation; Skin - abnormally light or dark
- Vitiligo - drug induced
- Vitiligo on the face
- Incontinentia pigmenti on the leg
- Incontinentia pigmenti on the leg
- Hyperpigmentation 2
- Post-inflammatory hyperpigmentation - calf
- Hyperpigmentation w/malignancy
- Post-inflammatory hyperpigmentation 2
Chang MW. Disorders of hyperpigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 67.
Passeron T, Ortonne JP. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 66.
Updated by: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Why does the skin darken in intimate places / Laser Doctor St. Petersburg
Edited by a doctor
February 17, 2021
Valentina Aleksandrovna Chernykh
Leading dermatovenereologist, cosmetologist
Clinic: Silver Boulevard, 17
For the most part, questions of aesthetic appearance are of interest to girls and women, since they are more inclined to take care of themselves. And this applies not only to open areas of the face and body, but also to such a hidden area as the bikini area. One of the most common cosmetic problems in this part of the body is the appearance of pigmentation. In our new article, we will tell you why the skin in intimate places darkens, and also with the help of what procedure it will be possible to effectively get rid of the manifestation of pigmentation.
Dark spots in the intimate area
As a rule, a change in the color of the epidermis in a delicate area causes only aesthetic discomfort, without posing a threat to human health (unless, of course, it is a sign of any disease). However, even in this case, darkening can cause various complexes and self-doubt. Sometimes a person even has to give up visiting the beach, and even from an intimate life. Moreover, dark spots in the intimate area sometimes appear at a fairly young age: for example, at 20-25 years old.
Causes of pigmentation
There are many reasons for this phenomenon. Most often they are associated with external factors. However, there are also those that are caused by poor health.
Dark spots and diseases
Of course, the first step is to check the causes of pigmentation in a delicate area that are related to health. There are a number of failures and ailments, due to which darkening of the skin in the bikini area is possible.
1. Hormonal disruptions. Often this occurs during puberty, menopause, and also during pregnancy. In addition, oral contraceptives can lead to disruptions in the hormonal background.
2. Fungal diseases. Considered one of the most common causes of dark spots in the intimate area. Unless, of course, we talk about the reasons associated with human health. However, fungal diseases, as a rule, are not limited to pigmentation alone: additional symptoms include skin peeling, itching, rashes, and a feeling of discomfort.
3. Diseases of the gallbladder or liver. Such ailments are accompanied not only by darkening of the skin in intimate places, but also by poor health, impaired functioning of the digestive system, and a feeling of heaviness in the right hypochondrium.
4. Varicose veins. The course of this disease is often accompanied by congestion in the tissues of the small pelvis. As a result, the outflow of blood is disturbed, which may cause tissue hyperemia in the intimate area and swelling. All this can affect the manifestation of pigmentation in the bikini area. It is noted that varicose veins are most common in women after thirty years.
All this can affect the manifestation of pigmentation in the bikini area. It is noted that varicose veins are most common in women after thirty years.
5. Addison's disease. During this disease, the adrenal glands do not produce enough hormones. At the same time, the skin darkens not only in the intimate area, but also in the armpits. It is also worth noting that this disease is quite rare.
Remember that you cannot self-diagnose yourself, even if most of the symptoms match. Only a specialist with a higher medical education will be able to determine exactly why the skin darkens in intimate places, the reasons for which will tell you after all the necessary tests have been carried out. Remember, you can not self-medicate! The best thing to do if you suspect a particular disease is to make an appointment with a doctor.
Causes of pigmentation in the groin area
The most common causes of discoloration of the epidermis in a delicate area are:
1. Removal of excess vegetation. True, in the case of depilation, not all methods are suspect, but only those that one way or another can lead to skin damage. This is mainly shaving, sugaring and waxing. If such damage is regular, then they can lead to a disruption in the production of melanin, the pigment that gives the skin a dark tint.
Removal of excess vegetation. True, in the case of depilation, not all methods are suspect, but only those that one way or another can lead to skin damage. This is mainly shaving, sugaring and waxing. If such damage is regular, then they can lead to a disruption in the production of melanin, the pigment that gives the skin a dark tint.
2. Overweight. If you are overweight, your skin may be constantly chafed. In addition, folds are formed, sweating often increases. The combination of these factors can lead to darkening of the skin in the bikini area.
3. Underwear. Incorrectly selected underwear made of non-natural materials can also constantly rub the skin. In addition, poor-quality underwear can stain the skin in the intimate area with dangerous paint.
4. Abuse of ultraviolet light. If you “register” in a solarium, then this is unlikely to allow you to get a beautiful bronze tan. But problems with skin pigmentation - it can very well be. And the intimate zone in this case is no exception.
5. Natural age-related changes. As a rule, after reaching the age of forty, the skin in the intimate area becomes darker in almost all people: about three out of four. Usually this is again associated with hormonal changes.
6. Care procedures. Age spots in a delicate area can appear due to improper care or the use of inappropriate cosmetics, and sometimes due to a combination of these factors.
7. Long period of taking antibiotics.
Bikini area pigmentation removal
Many experts believe that today one of the most effective ways to get rid of pigmentation in a delicate area is IPL phototherapy. In our clinic, this procedure is performed using a special Quantum apparatus. However, before signing up for a session, you will need to remove the hair in the intimate area and avoid tanning a couple of weeks before the procedure. In addition, it is necessary to make an appointment with a dermatocosmetologist for the first time. At such an appointment, a specialist will conduct a consultation, interview you and, if necessary, examine you. In some cases, after the examination, the specialist will be able to tell why the skin in the intimate area is dark. Also, the dermatocosmetologist should check you in advance for the presence of restrictions and contraindications to the Quantum procedure.
In some cases, after the examination, the specialist will be able to tell why the skin in the intimate area is dark. Also, the dermatocosmetologist should check you in advance for the presence of restrictions and contraindications to the Quantum procedure.
Quantum: contraindications and limitations
1. Infectious diseases.
2. Acute phase of herpes.
3. Fresh tan.
4. Exacerbation of skin diseases.
5. Pregnancy and lactation period.
6. Malignant neoplasms.
If the patient has no contraindications to Quantum, then the procedure can be performed immediately after the end of the initial appointment.
Removing pigmentation in delicate areas with Quantum
Before treatment with Quantum, the skin is cleaned and disinfected. A special media gel is also used, which is applied to the epidermis for better penetration of light waves into the skin. The procedure is performed under local anesthesia.
As a result of light exposure, the melanin pigment in the skin is destroyed, after which it is removed from the skin in a natural way. After one or more sessions, the pigmentation gradually becomes lighter and eventually disappears. To completely eliminate pigmentation in the bikini area, one to five sessions are required, which are carried out with an interval of four weeks.
The duration of one session is about half an hour. When it is finished, the doctor will apply a soothing agent to the skin and tell you how the correct recovery period should go.
Quantum: rehabilitation period
It is noted that after exposure to light, the skin may turn red, begin to peel off or become slightly swollen. However, all these manifestations pass quite quickly. Skin care involves the use of soothing, moisturizing and restorative products. In the first four weeks, excessive heat exposure to the skin should be excluded. Therefore, it will be necessary to abandon the bath, steam room, sauna, hot bath. You will also need protection from UV rays. That is, any kind of tanning will also have to be excluded. To avoid unnecessary skin irritation, for the first time, refuse intimate hair removal.
You will also need protection from UV rays. That is, any kind of tanning will also have to be excluded. To avoid unnecessary skin irritation, for the first time, refuse intimate hair removal.
In addition to the above recommendations, the recovery period can be given by a dermatocosmetologist and individual.
Skin pigmentation: what it is, causes, how to get rid of it, doctor's advice
Individual areas of skin of a darker color are in most cases a healthy phenomenon. However, you may not like it aesthetically. In this case, a number of safe measures can be taken.
The author of the article is Margarita Gekht, leading dermatologist at the Butterfly Children charity foundation, lecturer at the online academy of skin problems Skill for Skin
Advertising on RBC www.adv.rbc.ru
Hyperpigmentation, or skin pigmentation, is a condition in which some areas of the skin are darker than others. Hyperpigmentation can appear in small areas, cover large areas or, in rare cases, even the entire body. This is a fairly common skin problem that affects people with all skin types.
Hyperpigmentation can appear in small areas, cover large areas or, in rare cases, even the entire body. This is a fairly common skin problem that affects people with all skin types.
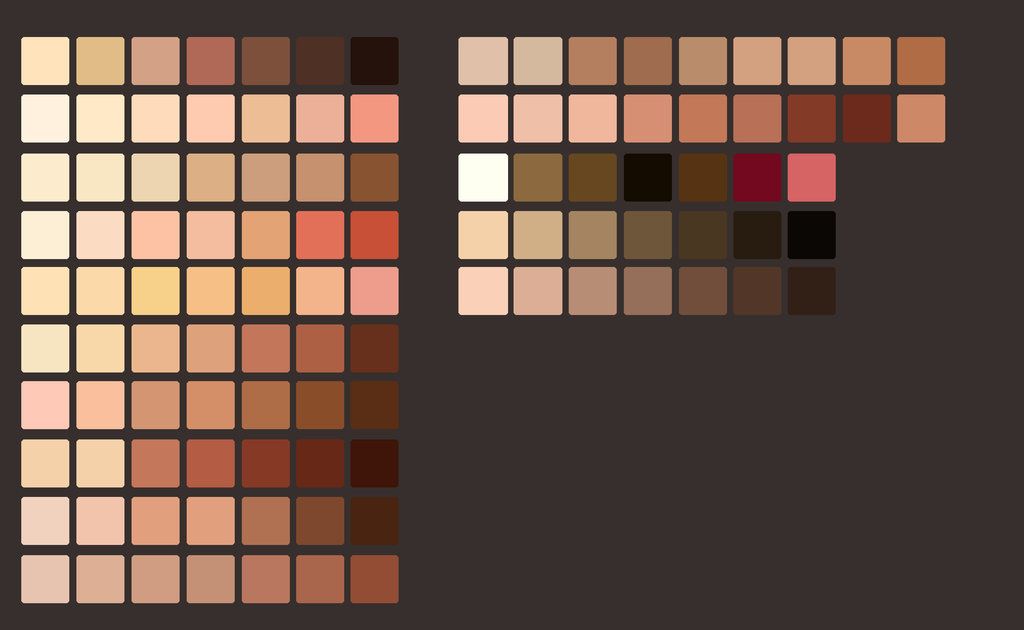
The mechanism of hyperpigmentation is as follows. The color of the skin, hair and eyes is determined by the pigment melanin, which is produced by special cells - melanocytes. Melanin is usually evenly distributed over the skin, but some people may have areas of the skin in which the concentration of melanin is higher or lower than normal. As a result, brown or gray spots appear on the skin.
However, people with phototypes 3-6 on the Fitzpatrick phototype scale [1] tend to be more hyperpigmented than people with phototypes 1 and 2. the main ones include sun exposure, hormonal changes, age, injury or inflammation of the skin.
Sun exposure
Excessive exposure to sunlight is the main cause of hyperpigmentation.
Sunlight triggers additional production of melanin, which acts as a natural sunscreen, protecting the skin from harmful UV rays. But excessive sun exposure disrupts this process, leading to hyperpigmentation.
But excessive sun exposure disrupts this process, leading to hyperpigmentation.
In addition, sun exposure makes existing areas of hyperpigmentation - age or sun spots, melasma and post-inflammatory hyperpigmentation spots - even more pronounced.
Diseases and drugs
It has been established that certain diseases and medications can provoke hyperpigmentation. It is also a symptom of certain diseases, such as autoimmune and gastrointestinal diseases, metabolic disorders and vitamin deficiencies.
Hyperpigmentation can also be caused by a number of medications, including chemotherapy drugs, antimalarials, anticonvulsants, and antibiotics.
Hormonal changes
Hormonal changes are the main causes of a special type of hyperpigmentation known as melasma or chloasma. This phenomenon is especially common among women and is believed to occur when the female sex hormones estrogen and progesterone stimulate the overproduction of melanin and the skin is exposed to the sun. This skin condition is typical for pregnant women.
This skin condition is typical for pregnant women.
Melasma occurs in 10-15% of pregnant women and in 10-25% of women taking oral contraceptives. In men, this condition is less common.
Age
Age or liver spots are a common form of hyperpigmentation.
Brown spots occur in people over 40 years of age on the hands, face, or other areas exposed to frequent sun exposure. Doctors call such spots "solar" lentigo.
They arise due to the fact that with age the number of skin cells producing melanin decreases, but the rest of the cells increase and the distribution of melanin becomes less uniform.
Skin lesions and inflammations
Post-inflammatory hyperpigmentation occurs after injury or inflammation of the skin resulting from cuts, burns, chemical exposure, acne, atopic dermatitis or psoriasis. The skin darkens, and after the cause is removed, the areas of pigmentation become discolored.
© Shutterstock
How to Prevent Hyperpigmentation
Daily Broad Spectrum Sunscreen
Sun protection is the most important and essential step to help prevent hyperpigmentation. The sun's rays affect the skin even on cloudy days, so it is recommended to provide the skin with daily sun protection, regardless of the weather.
For the city, the spectrum of action of the cream should be 15-25 SPF, for recreation at sea and in the mountains - 30-50+ SPF.
Limiting skin exposure to the sun will also help reduce hyperpigmentation. The hottest hours are best spent in the shade and, if possible, wear protective clothing, a sun hat and goggles. Before sun exposure, apply and reapply sun protection with the appropriate SPF level for your skin type and condition.
How to reduce existing age spots
Preventing age spots is easier than removing them. But fresh spots can be made less noticeable and prevent their recurrence.
Specialty Pigmentation Products
If you're concerned about hyperpigmentation, check out skin care products that have been formulated to address this problem and are clinically and dermatologically proven to work. In particular, the lines of pharmaceutical products marked "melascreen", "depiderm", "anti-pigment" deserve attention.
Dermatological treatments
Dermatological treatments such as chemical peels and laser treatments can help reduce hyperpigmentation.
Chemical peel is one of the effective ways to remove hyperpigmentation and stimulate the appearance of new and evenly pigmented skin. During the procedure, a chemical solution is applied to the face, neck and hands. In the process of such peeling, the skin is exfoliated and the growth of new skin cells is stimulated.
laser treatments provide a similar effect to a chemical peel, but here the treatment can be more targeted as the dermatologist has more control over the intensity of the peel.
They are "irradiation" of the affected areas with high energy light. The softest laser treatments affect only the superficial layer of the skin, while the more intense ones work on the deepest skin layers.
© Shutterstock
Dealing with pigmentation problems
First, the root cause of hyperpigmentation must be addressed. Treating this condition early will help prevent further darkening of the skin.
Some manifestations of hyperpigmentation, such as melasma during pregnancy, may disappear on their own.
Medicines to correct hyperpigmentation
A number of medicines are effective in treating hyperpigmentation. They can be used alone or in combination with each other, which enhances the effect. Some of these treatments require several months.
Hydroquinone
One of the most commonly used drugs for hyperpigmentation. Hydroquinone slows down the action of the enzyme needed to produce melanin. The drug is available in creams, lotions and gels, some of which can be bought without a prescription.
The drug is available in creams, lotions and gels, some of which can be bought without a prescription.
However, hydroquinone does not affect sunspots. Also, it can only be used for a limited time because, like chemical peels and laser treatments, it can irritate the skin and cause post-inflammatory hyperpigmentation, especially in people with phototypes 3-6.
Topical retinoids
These are creams, lotions and gels containing medicines derived from vitamin A. They can be used alone or in combination with other medicines to treat hyperpigmentation.
Azelaic Acid
Azelaic acid gel and cream products slow down the production of tyrosinase, an enzyme needed to make melanin, and also inhibit the growth of abnormal melanocytes, the cells that produce melanin.
Kojic acid
This acid is produced by some fungi during fermentation. It slows down the formation of melanin and can be used in conjunction with hydroquinone and glycolic acid.
It slows down the formation of melanin and can be used in conjunction with hydroquinone and glycolic acid.
Ascorbic acid
Or the well-known vitamin C. In addition to its skin lightening function, it also has an anti-inflammatory effect and helps reduce molecular damage caused by sunlight.
Regardless of the choice of therapy, always use sunscreen before going out.
© Shutterstock
Treating Pigmentation at Home
One of the best ways to reduce the risk of hyperpigmentation is to use sunscreen every day.
People with hyperpigmentation of the skin should also avoid the sun and wear protective clothing, hats and sunglasses. Remember that one day in the sun can negate months of hyperpigmentation treatment.
Secondly, it is important to maintain a balance of free radicals and antioxidants in the body. Free radicals damage healthy skin cells and cells in other body systems. Antioxidants neutralize free radicals and prevent damage to skin cells, helping the skin recover.
Antioxidants neutralize free radicals and prevent damage to skin cells, helping the skin recover.
Antioxidants can be taken orally or used in cosmetic preparations to prevent pigmentation. To do this, you can:
Eat antioxidants with food
Vitamin C and glutathione supplements help neutralize free radicals and prevent oxidative stress. Strengthening the skin is also facilitated by a balanced diet with a sufficient amount of foods rich in "antioxidants" (greens, green vegetables, fruits, green tea).
Use cosmetics with antioxidants
Choose skin care products with antioxidant ingredients such as vitamin C, berry extracts, arbutin, glycolic, kojic, azelaic and ferulic acids, arbutin, retinol and niacinamide. Niacinamide, also known as vitamin B3, is a powerful ingredient that reduces the risk of hyperpigmentation and evens out skin tone. Its effectiveness has been clinically proven.
Topical formulations containing these ingredients inhibit melanin production while increasing cell turnover by removing the top layer of dead skin and thus reducing existing pigmentation.