How much is fever in a child
Fevers (for Parents) - Nemours KidsHealth
All kids get a fever from time to time. A fever itself usually causes no harm and can actually be a good thing — it's often a sign that the body is fighting an infection.
But when your child wakes in the middle of the night flushed, hot, and sweaty, it's easy to be unsure of what to do next. Should you get out the thermometer? Call the doctor?
Here's more about fevers, including when to contact your doctor.
What Is a Fever?
Fever happens when the body's internal "thermostat" raises the body temperature above its normal level. This thermostat is found in a part of the brain called the hypothalamus. The hypothalamus knows what temperature your body should be (usually around 98.6°F/37°C) and will send messages to your body to keep it that way.
Most people's body temperatures change a little bit during the course of the day: It's usually a little lower in the morning and a little higher in the evening and can vary as kids run around, play, and exercise.
Sometimes, though, the hypothalamus will "reset" the body to a higher temperature in response to an infection, illness, or some other cause. Why? Researchers believe that turning up the heat is a way for the body to fight the germs that cause infections, making it a less comfortable place for them.
What Causes Fevers?
It's important to remember that fever by itself is not an illness — it's usually a sign or symptom of another problem.
Fevers can be caused by a few things, including:
Infection: Most fevers are caused by infection or other illness. A fever helps the body fight infections by stimulating natural defense mechanisms.
Overdressing: Infants, especially newborns, may get fevers if they're overbundled or in a hot environment because they don't regulate their body temperature as well as older kids. But because fevers in newborns can indicate a serious infection, even infants who are overdressed must be checked by a doctor if they have a fever.
Immunizations: Babies and kids sometimes get a low-grade fever after getting vaccinated.
Although teething may cause a slight rise in body temperature, it's probably not the cause if a child's temperature is higher than 100°F (37.8°C).
When Is a Fever a Sign of Something Serious?
In healthy kids, not all fevers need to be treated. High fever, though, can make a child uncomfortable and make problems (such as dehydration) worse.
Doctors decide on whether to treat a fever by considering both the temperature and a child's overall condition.
Kids whose temperatures are lower than 102°F (38.9°C) often don't need medicine unless they're uncomfortable. There's one important exception: If an infant 3 months or younger has a rectal temperature of 100.4°F (38°C) or higher, call your doctor or go to the emergency department immediately. Even a slight fever can be a sign of a potentially serious infection in very young babies.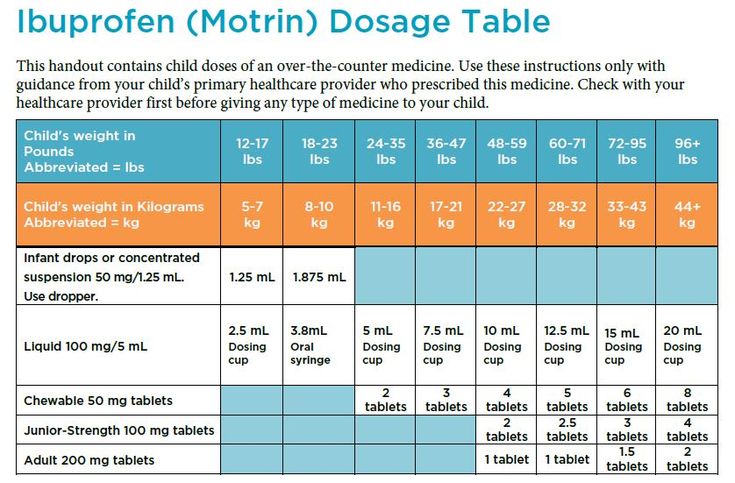
If your child is between 3 months and 3 years old and has a fever of 102.2°F (39°C) or higher, call to see if your doctor needs to see your child. For older kids, take behavior and activity level into account. Watching how your child behaves will give you a pretty good idea of whether a minor illness is the cause or if your child should be seen by a doctor.
The illness is probably not serious if your child:
- is still interested in playing
- is eating and drinking well
- is alert and smiling at you
- has a normal skin color
- looks well when his or her temperature comes down
And don't worry too much about a child with a fever who doesn't want to eat. This is very common with infections that cause fever. For kids who still drink and urinate (pee) normally, not eating as much as usual is OK.
Is it a Fever?
A gentle kiss on the forehead or a hand placed lightly on the skin is often enough to give you a hint that your child has a fever. However, this method of taking a temperature (called tactile temperature) won't give an accurate measurement.
However, this method of taking a temperature (called tactile temperature) won't give an accurate measurement.
Use a reliable digital thermometer to confirm a fever. It's a fever when a child's temperature is at or above one of these levels:
- measured orally (in the mouth): 100°F (37.8°C)
- measured rectally (in the bottom): 100.4°F (38°C)
- measured in an axillary position (under the arm): 99°F (37.2°C)
But how high a fever is doesn't tell you much about how sick your child is. A simple cold or other viral infection can sometimes cause a rather high fever (in the 102°–104°F/38.9°–40°C range), but this doesn't usually mean there's a serious problem. In fact, a serious infection, especially in infants, might cause no fever or even a low body temperature (below 97°F or 36.1°C).
Because fevers can rise and fall, a child might have chills as the body's temperature begins to rise. The child may sweat to release extra heat as the temperature starts to drop.
The child may sweat to release extra heat as the temperature starts to drop.
Sometimes kids with a fever breathe faster than usual and may have a faster heart rate. Call the doctor if your child has trouble breathing, is breathing faster than normal, or is still breathing fast after the fever comes down.
p
How Can I Help My Child Feel Better?
Again, not all fevers need to be treated. In most cases, a fever should be treated only if it's causing a child discomfort.
Here are ways to ease symptoms that often accompany a fever:
Medicines
If your child is fussy or uncomfortable, you can give acetaminophen or ibuprofen based on the package recommendations for age or weight. (Unless instructed by a doctor, never give aspirin to a child due to its association with Reye syndrome, a rare but potentially fatal disease.) If you don't know the recommended dose or your child is younger than 2 years old, call the doctor to find out how much to give.
Infants younger than 2 months old should not be given any medicine for fever without being checked by a doctor. If your child has any medical problems, check with the doctor to see which medicine is best to use. Remember that fever medicine can temporarily bring a temperature down, but usually won't return it to normal — and it won't treat the underlying reason for the fever.
If your child has any medical problems, check with the doctor to see which medicine is best to use. Remember that fever medicine can temporarily bring a temperature down, but usually won't return it to normal — and it won't treat the underlying reason for the fever.
Home Comfort Measures
Dress your child in lightweight clothing and cover with a light sheet or blanket. Overdressing and overbundling can prevent body heat from escaping and can cause the temperature to rise.
Make sure your child's bedroom is a comfortable temperature — not too hot or too cold.
While some parents use lukewarm sponge baths to lower fever, this method only helps temporarily, if at all. In fact, sponge baths can make kids uncomfortable. Never use rubbing alcohol (it can cause poisoning when absorbed through the skin) or ice packs/cold baths (they can cause chills that can raise body temperature).
Food and Drinks
Offer plenty of fluids to avoid dehydration because fevers make kids lose fluids more rapidly than usual.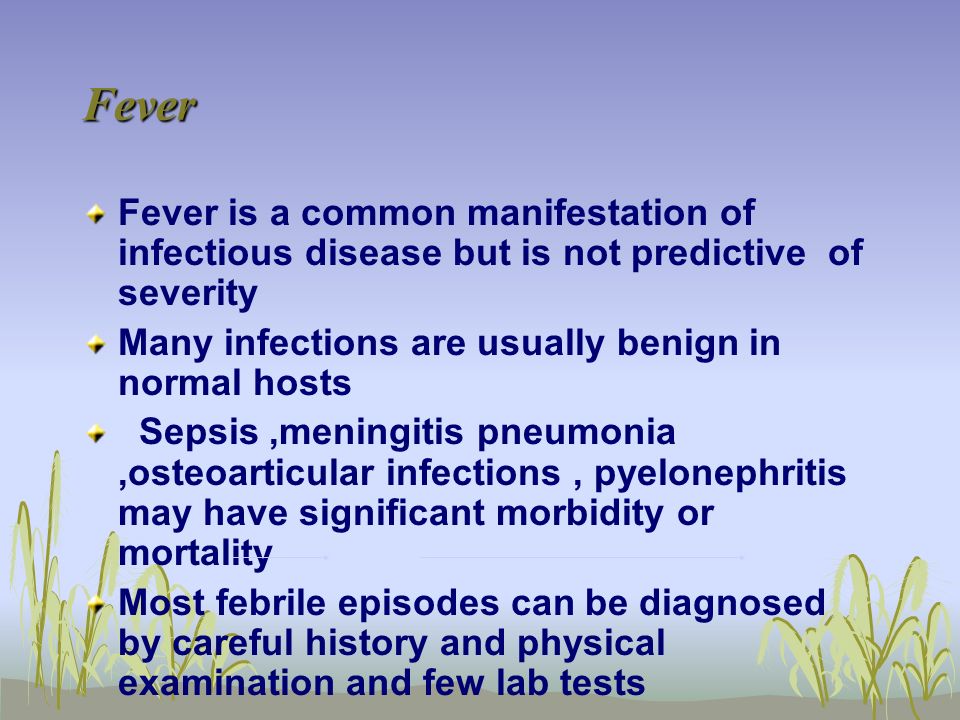 Water, soup, ice pops, and flavored gelatin are all good choices. Avoid drinks with caffeine, including colas and tea, because they can make dehydration worse by increasing urination (peeing).
Water, soup, ice pops, and flavored gelatin are all good choices. Avoid drinks with caffeine, including colas and tea, because they can make dehydration worse by increasing urination (peeing).
If your child also is vomiting and/or has diarrhea, ask the doctor if you should give an electrolyte (rehydration) solution made especially for kids. You can find these at drugstores and supermarkets. Don't offer sports drinks — they're not made for younger children and the added sugars can make diarrhea worse. Also, limit your child's intake of fruits and apple juice.
In general, let kids eat what they want (in reasonable amounts), but don't force it if they don't feel like it.
Taking it Easy
Make sure your child gets plenty of rest. Staying in bed all day isn't necessary, but a sick child should take it easy.
It's best to keep a child with a fever home from school or childcare. Most doctors feel that it's safe to return when the temperature has been normal for 24 hours.
When Should I Call the Doctor?
The exact temperature that should trigger a call to the doctor depends on a child's age, the illness, and whether there are other symptoms with the fever.
Call your doctor if you have an:
- infant younger than 3 months old with a rectal temperature of 100.4°F (38°C) or higher
- older child with a temperature of higher than 102.2°F (39°C)
Also call if an older child has a fever of lower than 102.2°F (39°C) but also:
- refuses fluids or seems too ill to drink adequately
- has lasting diarrhea or repeated vomiting
- has any signs of dehydration (peeing less than usual, not having tears when crying, less alert and less active than usual)
- has a specific complaint (like a sore throat or earache)
- still has a fever after 24 hours (in kids younger than 2 years old) or 72 hours (in kids 2 years or older)
- is getting fevers a lot, even if they only last a few hours each night
- has a chronic medical problem, such as heart disease, cancer, lupus, or sickle cell disease
- has a rash
- has pain while peeing
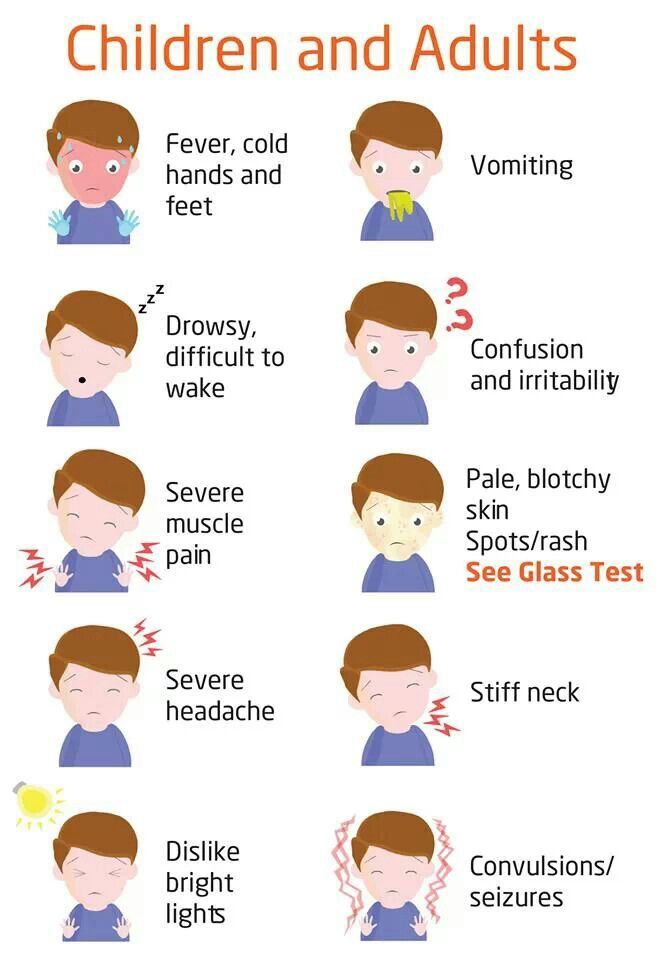
Get emergency care if your child shows any of these signs:
- crying that won't stop
- extreme irritability or fussiness
- sluggishness and trouble waking up
- a rash or purple spots that look like bruises on the skin (that were not there before your child got sick)
- blue lips, tongue, or nails
- infant's soft spot on the head seems to be bulging out or sunken in
- stiff neck
- severe headache
- limpness or refusal to move
- trouble breathing that doesn't get better when the nose is cleared
- leaning forward and drooling
- seizure
- moderate to severe belly pain
Also, ask if your doctor has specific guidelines on when to call about a fever.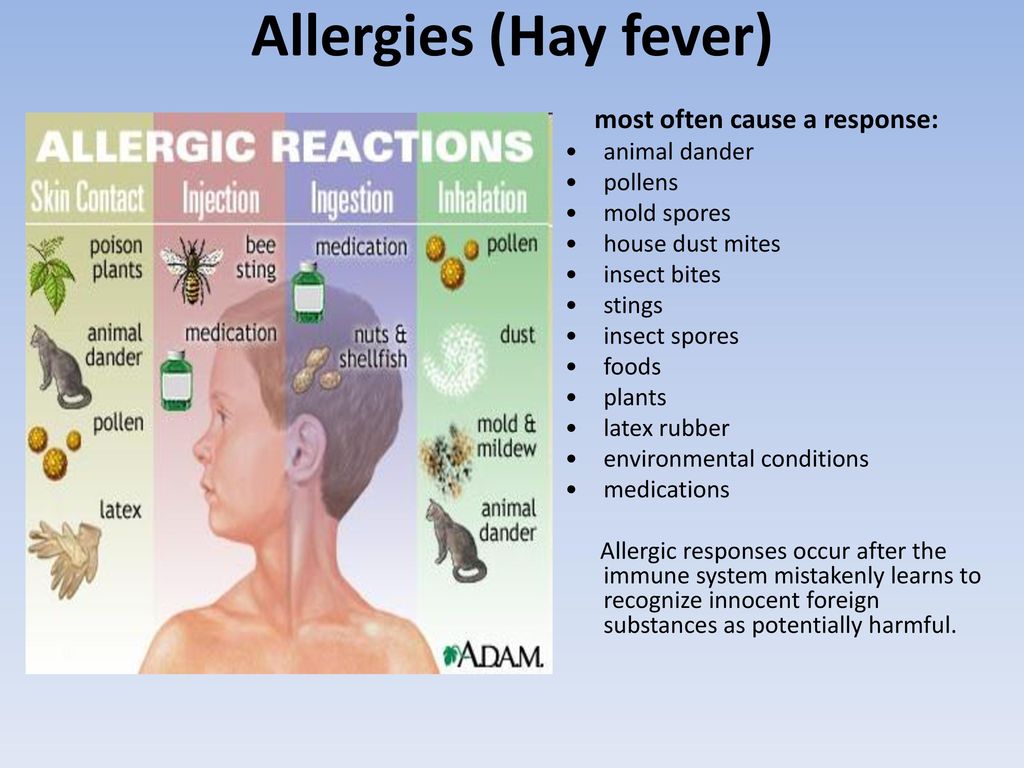
What Else Should I Know?
All kids get fevers, and in most cases they're completely back to normal within a few days. For older babies and kids, the way they act can be more important than the reading on your thermometer. Everyone gets a little cranky when they have a fever. This is normal and should be expected.
But if you're ever in doubt about what to do or what a fever might mean, or if your child is acting ill in a way that concerns you even if there's no fever, always call your doctor for advice.
Reviewed by: Joanne Murren-Boezem, MD
Date reviewed: September 2018
Seizures (for Parents) - Nemours KidsHealth
What Is a Seizure?
A seizure (SEE-zhur) is unusual electrical activity in the brain that can cause changes in behavior, movement, or feelings. Normally, electrical activity in the brain involves neurons (nerve cells) in different areas sending signals at different times. During a seizure, many neurons fire all at once.
Not all kids who have had one seizure will have another. Epilepsy is when someone has repeated seizures. Some kids will outgrow seizures.
What Happens in a Seizure?
Normally, electrical activity in the brain involves neurons (nerve cells) in different areas sending signals at different times. During a seizure, many neurons fire all at once.
What Are the Different Types of Seizures?
Some seizures affect both sides of the brain, while others involve only one side.
Generalized seizures affect both sides of the brain. Generalized seizure types include:
- generalized tonic-clonic seizures
- absence seizures
- atonic seizures
- tonic seizures
- myoclonic seizures
Focal seizures affect a single area in one side of the brain. Focal seizures types include:
- focal aware seizures
- focal impaired awareness seizures
- focal to bilateral generalized tonic-clonic seizures
Some people have both focal and generalized seizures.
What Are the Signs & Symptoms of a Seizure?
Signs and symptoms of seizures depend on what kind of seizure someone has. They may stare into space or have jerking movements in part of their body or the whole body. Some people may show no signs at all.
What Happens After a Seizure?
After a seizure, the person may feel confused, tired, have a headache, or have other symptoms. This is called the postictal (post-IK-tul) phase. It usually lasts just a few minutes, but can be longer.
What Causes Seizures?
The most common type of seizure in children is from a fever (called a febrile seizure). Other causes include infections, low blood sodium, medicines, drug use (amphetamines or cocaine), brain injury or a tumor, and genetic changes. Sometimes, a seizure's cause is never found.
How Are Seizures Diagnosed?
If a child has a seizure, doctors will look for a cause. Kids who’ve had a seizure might need to see a pediatric neurologist (a doctor who specializes in brain, spine, and nervous system problems). Tests done can include:
Tests done can include:
- blood tests and urine (pee) tests to look for infections or illnesses
- EEG to measure brain wave activity
- VEEG, or video electroencephalography (EEG with video recording)
- CAT scan, MRI, and PET/MRI scans to get very detailed images of the brain
How Are Seizures Treated?
How doctors treat seizures depends on their cause (if known) and the type of seizure. Some won’t need any treatment.
Medicines can help with many types of seizures. If medicine doesn’t work, other treatments are available.
How Can Parents Help?
If your child had a seizure, talk to the doctor about:
- any medicines your child should take
- any “triggers” (such as fever, flashing lights, hunger, lack of sleep, or medicines) that can make a seizure more likely
- any precautions your child should take while swimming or bathing
- whether your child should wear a medical ID bracelet
- whether your child needs to see a neurologist
- if it’s OK for your teen to drive
- how to keep your child safe during a seizure.
 Share this information with caregivers, coaches, and staff at your child’s school.
Share this information with caregivers, coaches, and staff at your child’s school.
If your child has another seizure, keep a record of:
- when it happened
- how long it lasted
- what happened right before the seizure
- what happened during and after the seizure
This information will help the doctor find what’s causing the seizures and decide on the best treatment.
What Else Should I Know?
If your child has seizures, reassure them that they’re not alone. Your doctor and the care team can answer questions and offer support. They also might be able to recommend a local support group. Online organizations can help too, such as:
- Epilepsy Foundation
- CDC – Managing Epilepsy
Clinical guidelines SARS
Clinical guidelines:
"Acute respiratory viral infection (ARVI) in children. ICD 10: J00 / J02.9/ J04.0/ J04.1/J04.2/J06.0/J06.9
Year of approval (revision frequency): 2018 (revision every 3 years)
Professional associations: Russian Union of Pediatricians
Approved by: Russian Union of Pediatricians
Appendix B. Patient Information
Patient Information
ARVI (acute respiratory viral infection) is the most common disease in children.
The cause of the disease is a variety of viruses. The disease often develops in autumn, winter and early spring.
How they become infected with an infection that causes ARVI: most often by getting on the nasal mucosa or conjunctiva from hands contaminated by contact with the patient (for example, through a handshake) or with virus-infected surfaces (rhinovirus persists on them for up to a day).
Another way - airborne - by inhalation of saliva particles released when sneezing, coughing or in close contact with the patient.
Period from infection to onset of illness: in most cases 2 to 7 days. Isolation of viruses by patients (infectiousness for others) is maximum on the 3rd day after infection, sharply decreases by the 5th day; mild shedding of the virus can persist for up to 2 weeks.
Signs of ARVI: the most common manifestation of ARVI in children is nasal congestion, as well as nasal discharge: transparent and / or white and / or yellow and / or green (the appearance of discharge from the nose of yellow or green color is not a sign of a bacterial infection !). An increase in temperature often lasts no more than 3 days, then the body temperature decreases. In some infections (influenza and adenovirus infection), the temperature above 38ºC persists for a longer time (up to 5-7 days).
An increase in temperature often lasts no more than 3 days, then the body temperature decreases. In some infections (influenza and adenovirus infection), the temperature above 38ºC persists for a longer time (up to 5-7 days).
SARS may also cause: sore throat, cough, red eyes, sneezing.
Examinations: in most cases, additional examinations are not required for a child with SARS.
Treatment: ARVI is mostly benign, resolves within 10 days, and does not always require medication.
Decrease in temperature: a feverish child should be opened, wiped with water T° 25-30°C. In order to reduce the temperature in children, it is permissible to use only 2 drugs - paracetamol or ibuprofen. Antipyretic drugs in healthy children ≥3 months are justified at temperatures above 39- 39.5°C. With a less pronounced fever (38-38.5 ° C), fever-reducing agents are indicated for children under 3 months old, patients with chronic pathology, as well as temperature-related discomfort. Regular (course) intake of antipyretics is undesirable, a second dose is administered only after a new increase in temperature.
Regular (course) intake of antipyretics is undesirable, a second dose is administered only after a new increase in temperature.
The alternation of these two drugs or their use in combination does not lead to an increase in the antipyretic effect.
Do not use acetylsalicylic acid and nimesulide for antipyretic purposes in children. It is highly undesirable to use metamizole in children due to the high risk of developing agranulocytosis. In many countries of the world, metamizole has been banned for use for over 50 years.
Antibiotics - do not work on viruses (the main cause of SARS). Antibiotics are considered if a bacterial infection is suspected. Antibiotics must be prescribed by a doctor. Uncontrolled use of antibiotics can promote the development of resistant microbes and cause complications.
How to prevent the development of SARS:
A sick child should be left at home (not taken to kindergarten or school). Of paramount importance are measures to prevent the spread of viruses: thorough hand washing after contact with the sick.
It is also important to wear masks, wash surfaces around the patient, and observe the ventilation regimen. Annual influenza vaccination from age 6 months reduces the risk of this infection. It has also been proven that vaccination of children against influenza and pneumococcal infections reduces the likelihood of developing acute otitis media in children and the complicated course of SARS. There is no reliable evidence of a decrease in respiratory morbidity under the influence of various immunomodulators. The preventive effectiveness of herbal preparations and vitamin C, homeopathic preparations has not been proven either.
Consult a specialist if:
- the child refuses to drink for a long time - you see changes in behavior: irritability, unusual drowsiness with a decrease in reaction to attempts to contact the child
- the child has difficulty breathing, noisy breathing, rapid breathing, retraction of the intercostal spaces, jugular fossa (a place located in front between the neck and chest)
- the child has convulsions on the background of high temperature - the child has delirium on the background of high temperature
- increased body temperature (more than 38. 4-38.5ºC) persists for more than 3 days
4-38.5ºC) persists for more than 3 days
- nasal congestion persists without improvement for more than 10-14 days, especially if at the same time you see a "second wave" of fever and / or worsening of the child's condition
- the child has ear pain and/or discharge from the ear - the child has a cough that lasts more than 10-14 days without improvement
Child's temperature
If a child has a high temperature, what should parents do?
The question is answered by the head of the pediatric department of the MBU "SSMP named after V.F. Kapinos", an emergency doctor of the highest category, pediatrician Vlada Butakova:
against the background of SARS or influenza, the body temperature rises sharply. This can be with other childhood infections, including pneumonia and tonsillitis.
It is important to remember that any fever is a defensive reaction of the body, with which it fights infection.
In the first three days after the onset of SARS, fever should not cause panic in parents. Of course, a doctor should always deal with treatment (and it’s good if the doctor has already examined the patient and made his appointments since the onset of the disease). And if the fever lasts more than 3 days, then the child must be additionally shown to the pediatrician.
What can competent parents do in case of fever in the first days of illness?
From what level should the temperature be lowered?
There are general rules:
- for children under 3 months the temperature should be reduced from 38C
- for children under 4 years the temperature should be reduced from 38.5C 38.5-39C
There are also individual characteristics:
- elevated temperature should be reduced even at lower numbers if the child does not tolerate it well. That is, if it is inhibited or overly excited, if earlier there were convulsions with an increase in temperature;
- if the child has serious congenital diseases of the cardiovascular or nervous system.
But even in these cases, the temperature should be reduced not to 36.6C, but to 37-37.5C.
Medicines to reduce fever in children
These are medicines based on paracetamol and nurofen. The main thing here is to observe age dosages (do not overestimate or underestimate them) and in no case give children aspirin (it can cause serious bleeding).
The effect after taking an antipyretic drug should be expected within 40-50 minutes. If the chill continues, then there may not be a decrease in temperature or it will occur later.
If all the drugs have already been used, and the fever does not subside, then the ambulance on calls uses the lytic mixture for injections in the form of intramuscular injections. It is absolutely impossible for children to do these injections on their own!
Pale fever and rose fever features
"Pale fever", when, due to vascular spasm, the child has pale skin with a marbled pattern and chills continue, this is an alarming sign, and it is important not to make mistakes here.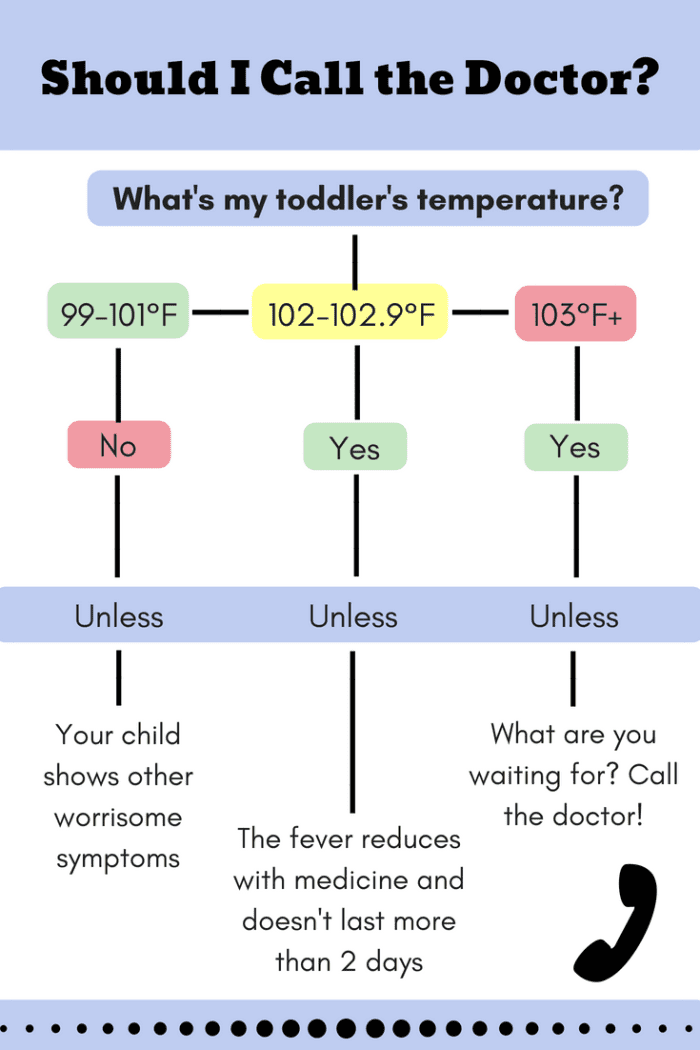
With pale fever:
- the child does not need to undress and wrap up very tightly. It must be warmed - that is, covered with a blanket, but only until the chill stops. Then the blanket can be replaced with a light blanket or sheet;
- do not wipe the child with cold water for chills and "pale fever". The only exception is the forehead of a child, on which, in case of any fever, a cool compress can be applied;
- for pale fever and chills, the child can be given an antispasmodic to dilate blood vessels. It can be a quarter of a no-shpa tablet or a candle with papaverine. This is necessary in order to expand the surface vessels and increase heat transfer.
"Rose fever" - is a "benign" course of hyperthermia. With it, a bright pink or even red skin tone in a child indicates that small vessels are dilated, heat transfer is not disturbed.
It is somewhat easier to reduce the temperature in rose fever: with the help of antipyretics, undressing (here you do not need a blanket, and doctors advise you to remove the diaper from the baby), wiping with lukewarm water and drinking plenty of water.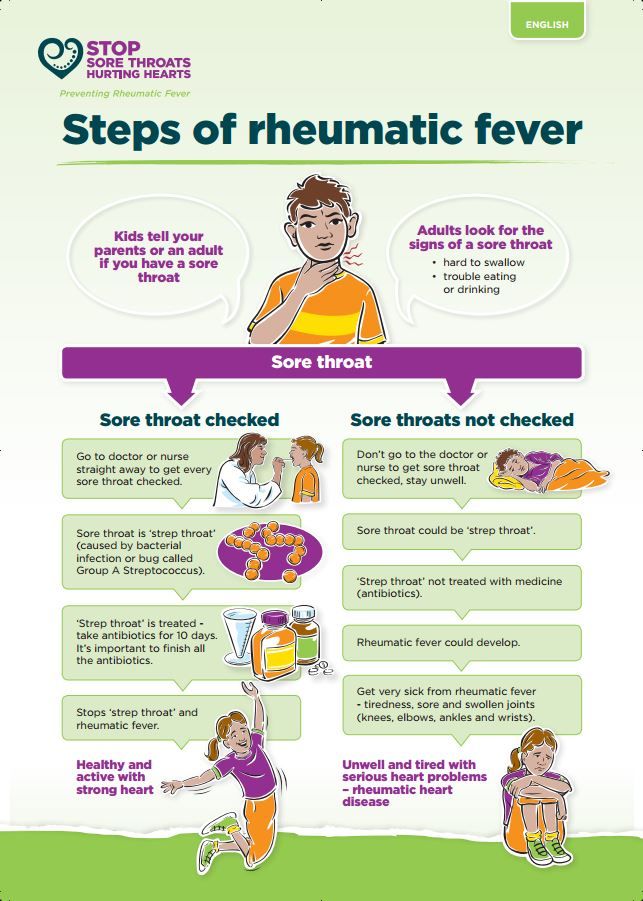
Clarification about wiping
We do not recommend adding vinegar, vodka or alcohol to water. Children's skin is characterized by increased permeability, and at elevated temperatures, all harmful substances from the skin will enter the bloodstream in seconds.
And about drinking
When the child's temperature rises, it is necessary to give water, but it should be given often, little by little (so as not to provoke vomiting) and slightly acidified drinks (for example, non-concentrated fruit drinks).
When and who should be called - an ambulance, an ambulance or an on-call doctor?
Most often, district or duty doctors or an emergency team from a polyclinic come to children's homes for fever. All of them can make a diagnosis, prescribe treatment, if necessary, refer them for additional studies or to a hospital, and issue a sick leave to mom or dad.
Emergency departments are open during the day, 7 days a week.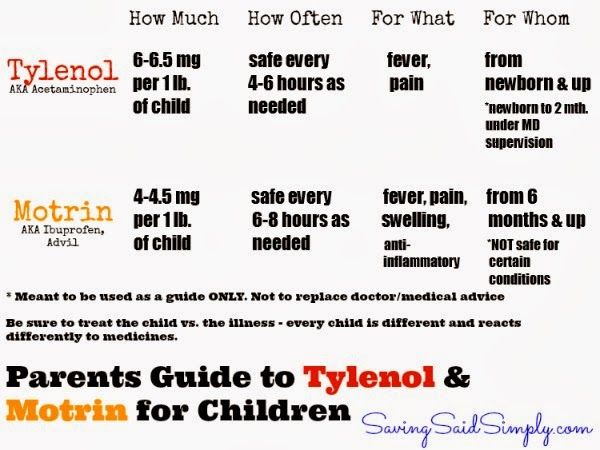 Calls are sent to them by an ambulance or a polyclinic registry. It is better to call the reception in the morning or in the afternoon, so as not to wait too long for the arrival of doctors, because there are a lot of calls in the evenings.
Calls are sent to them by an ambulance or a polyclinic registry. It is better to call the reception in the morning or in the afternoon, so as not to wait too long for the arrival of doctors, because there are a lot of calls in the evenings.
Ambulance needed:
— if the child is unable to cope with “pale fever” and chills in a few hours;
— if there is a disturbance of consciousness and behavior during fever, sharp lethargy and weakness appear;
- if convulsions, hallucinations, rash, vomiting appear together with fever;
- if parents fail to cope with fever in children with serious diseases of the cardiovascular, respiratory or nervous systems (congenital diseases, malformations, bronchial asthma, epilepsy, cerebral palsy).
During the evening "peak" ambulance workload, doctors can come to the child in 2-3 hours. This is not a violation of the law, since the time for servicing emergency calls (they are most calls for fever) is not regulated (for emergency calls, when there is a direct threat to life, the ambulance team must arrive strictly 20 minutes or earlier).