How much blood do you lose during a miscarriage
What Does a Miscarriage Look Like? Bleeding, Duration, and More
A miscarriage is a spontaneous pregnancy loss before 20 weeks of gestation. Some 8 to 20 percent known pregnancies end in miscarriage, with the majority happening before the 12th week.
The signs and symptoms of miscarriage vary from person to person. Symptoms may also vary depending on how far along you are. For example, a fetus at 14 weeks will be much larger than a fetus at 5 weeks of gestation, so there may be more bleeding and tissue loss with a later miscarriage.
Miscarriage symptoms may include:
- spotting or bleeding from the vagina
- abdominal cramping or pain in the lower back
- passage of tissue, fluid, or other products from the vagina
Read on to learn more about identifying a miscarriage and what to do if you suspect you’re experiencing one.
Bleeding may start as light spotting, or it could be heavier and appear as a gush of blood. As the cervix dilates to empty, the bleeding becomes heavier.
The heaviest bleeding is generally over within three to five hours from the time heavy bleeding begins. Lighter bleeding may stop and start over one to two weeks before it completely ends.
The color of the blood can range from pink to red to brown. Red blood is fresh blood that leaves the body quickly. Brown blood, on the other hand, is blood that’s been in the uterus a while. You may see discharge the color of coffee grounds, or near black, during a miscarriage.
Exactly how much bleeding you’ll experience depends on a variety of circumstances, including how far along you are and whether or not your miscarriage is progressing naturally.
While you may see a lot of blood, let your doctor know if you fill more than two sanitary pads an hour for two or more hours in a row.
What does a missed miscarriage look like?
You may not experience bleeding or other symptoms with a miscarriage, at least at first.
A missed miscarriage, also referred to as a missed abortion, happens when the fetus has died but the products of conception remain in the uterus. This type of miscarriage is usually diagnosed via ultrasound.
This type of miscarriage is usually diagnosed via ultrasound.
Just as with the amount of blood you’ll see, the duration of a miscarriage will vary from person to person and even from pregnancy to pregnancy.
In many cases, a miscarriage will take around two weeks to pass naturally. Your doctor may prescribe the medication misoprostol (Cytotec) to help a miscarriage pass more quickly. Bleeding may start within two days of beginning the medication. For others, it may take up to two weeks.
Once the miscarriage has started, the tissue and heaviest bleeding should be passed in about three to five hours. After the fetus has passed, you may still experience spotting and mild tissue loss for one to two weeks.
It may be difficult to tell a very early miscarriage from a late period. In fact, many miscarriages happen before a person even knows they’re pregnant.
In general, a miscarriage will cause more intense symptoms than a menstrual period. For example:
- Your menstrual flow may be relatively similar from month to month with heavy days and light days.
 A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to.
A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to. - Bleeding from a miscarriage may also contain large clots and tissue you don’t normally see during your period.
- Cramps can be a part of your normal monthly cycle, but with a miscarriage, they may be particularly painful as the cervix dilates.
- The color of blood during your period can range from pink to red to brown. If you see a color you’re not used to seeing, it may be a sign of miscarriage.
Always contact your doctor if you’re pregnant and experience bleeding. While a miscarriage can’t be stopped once it starts, you doctor can run tests to help determine if you’re experiencing the loss of your pregnancy or something else.
To diagnose a miscarriage, your doctor will likely perform an ultrasound to look for the baby’s heartbeat, if you’re far enough along to see a heartbeat. Your doctor may also order a blood test to check human chorionic gonadotropin (hcG) levels to see if they’re rising or falling.
If a miscarriage is confirmed, your doctor may suggest “expectant management” or waiting for the miscarriage to pass naturally. This generally happens within two weeks.
Incomplete miscarriage
The miscarriage may be incomplete if:
- your bleeding is particularly heavy
- you have a fever
- an ultrasound reveals there’s still tissue in your uterus
If this is the case, your doctor may suggest a dilation and curettage (D and C), which is a surgical procedure done to remove remaining tissue. The procedure is done under general or regional anesthesia, and is considered safe. D and C doesn’t usually lead to long-term complications.
Threatened miscarriage
It’s important to report any bleeding or pain you experience in your pregnancy to your doctor. In some cases, you may have what’s called a threatened miscarriage, and there may be certain treatments that can help. These include:
- hormone supplements if the bleeding is caused by low progesterone
- a cerclage (stitch in the cervix) if the issue is with the cervix opening prematurely
Speak with your healthcare provider if you’re looking to get pregnant again after a miscarriage. While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
The reason for loss isn’t always known, but around half of miscarriages are caused by issues with the baby’s chromosomes.
Other possible causes include:
- uterine issues
- hormonal imbalances
- other health conditions, such as diabetes, autoimmune disorders, or polycystic ovary syndrome
After a miscarriage, you may have hcG in your blood for one to two months, which could lead to a false positive pregnancy test. In most cases, your period will return within four to six weeks, though you may start ovulating almost immediately following a miscarriage.
Speak with your doctor about birth control options if you don’t wish to become pregnant after a miscarriage.
Will I miscarry again?
Having one miscarriage doesn’t necessarily increases your chances of having another.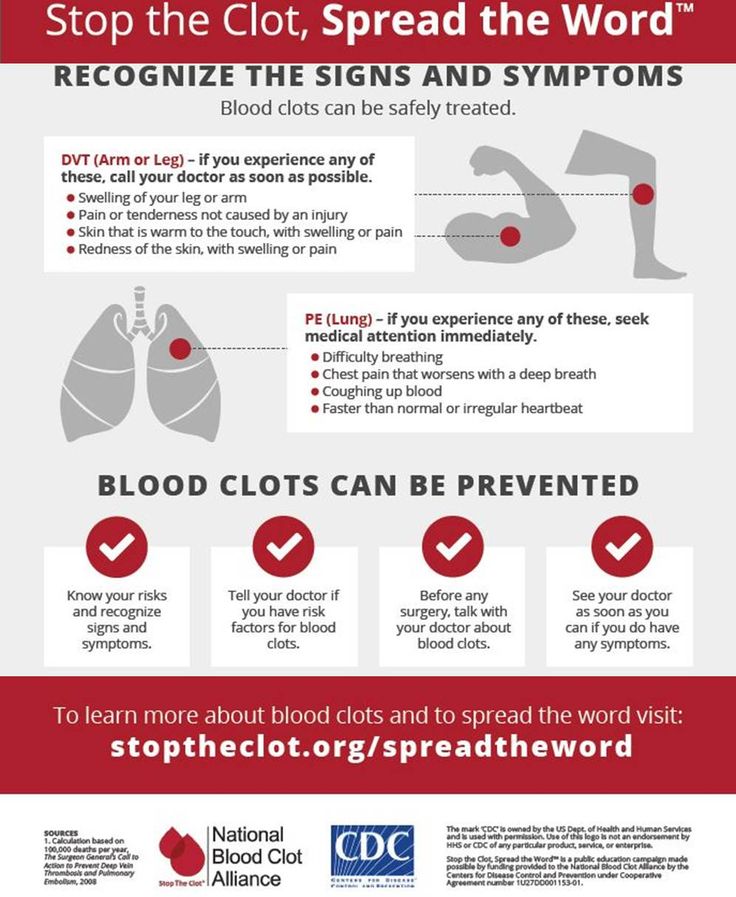 The risk remains around 20 percent.
The risk remains around 20 percent.
Two or more miscarriages is referred to as recurrent pregnancy loss (RPL). The risk of miscarriage after two losses is 28 percent. After three consecutive losses, it increases to 43 percent.
Only 1 percent of people experience three or more miscarriages. About 65 percent of those with unexplained RPL go on to have successful pregnancies.
Activities like exercise, work, morning sickness, and sex don’t cause miscarriages. Even things like smoking or drinking alcohol or caffeine, which can lead to other complications, are also unlikely to lead to early pregnancy loss.
A miscarriage can be physically painful, and it may also cause a variety of emotions. While your body may recover in a few weeks, be sure to take time to process your feelings, grieve, and reach out for help when you need it.
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.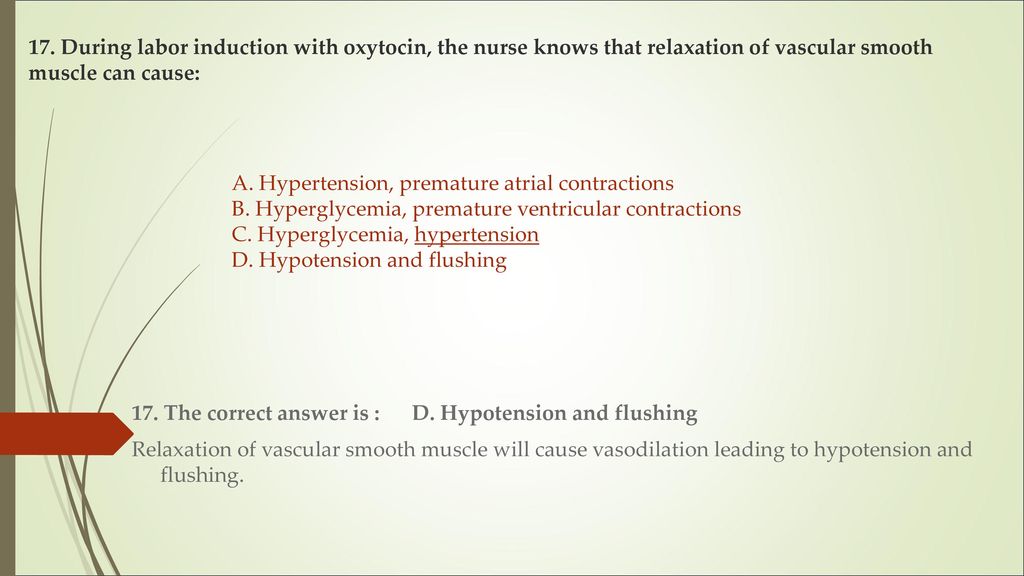
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress. If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining.
 This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week.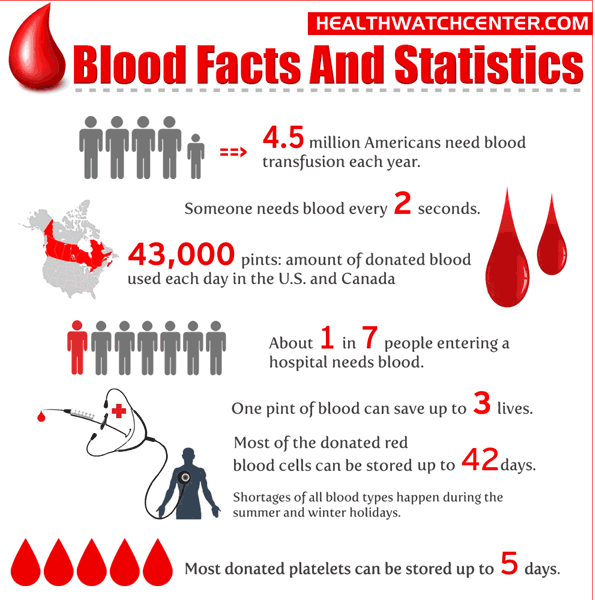 It will take about four to eight weeks for your regular period to return.
It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
Miscarriage, symptoms - Health Clinic 365 Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
According to statistics, 10 to 20% of all pregnancies end in miscarriage.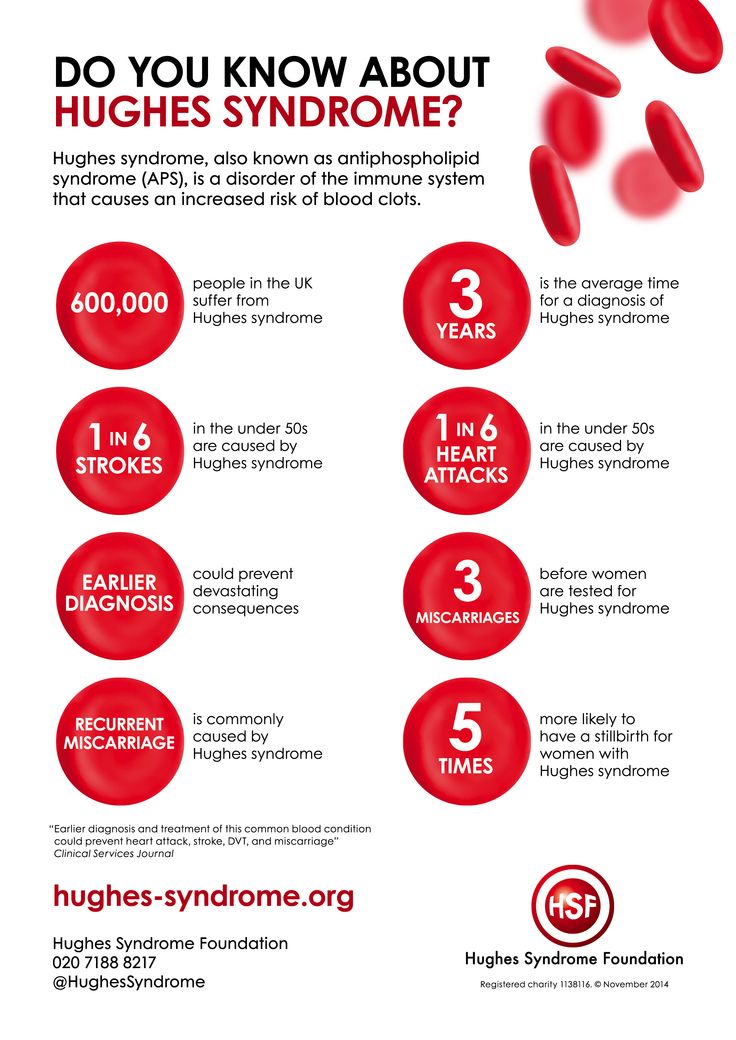 However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Miscarriage symptoms .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common.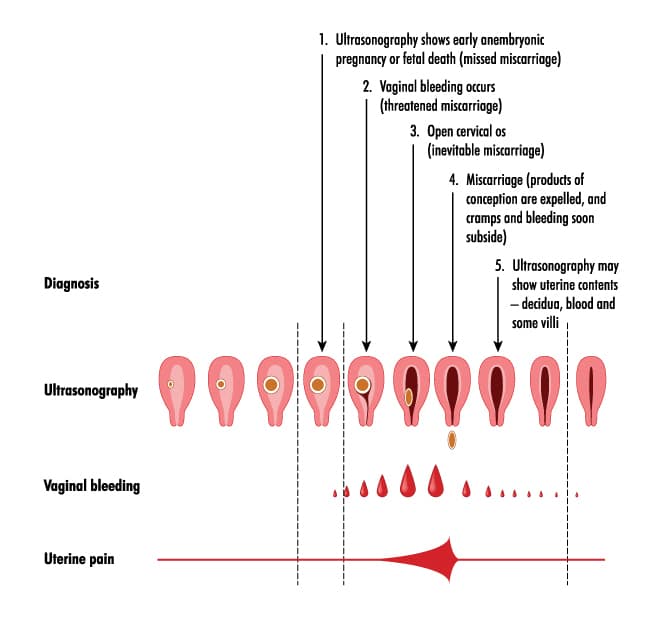 In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Call your doctor if:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can put a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.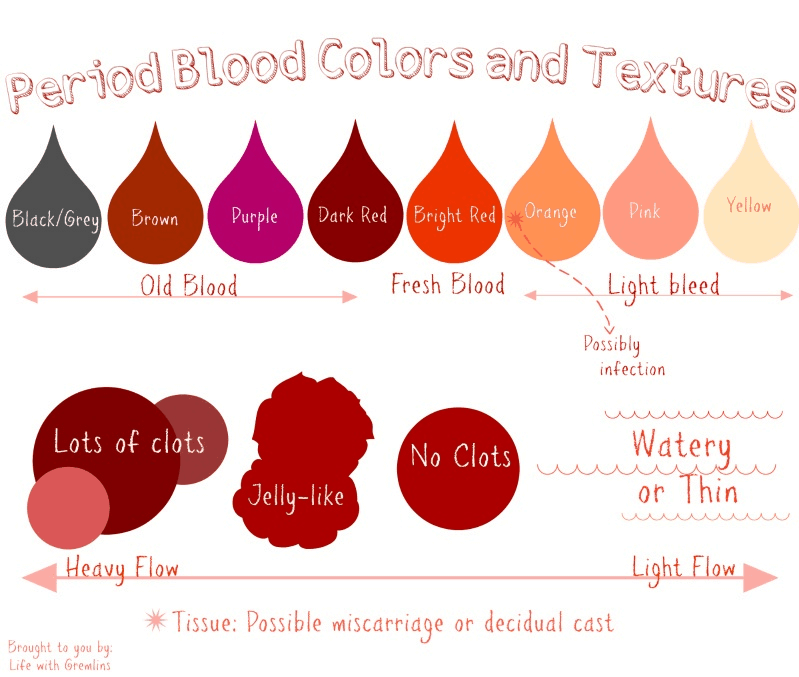
You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg.
Prices
Gynecologist, initial appointment
2300 i
How much blood can you lose before death, shock, death and more
content
Is there an exact amount?
You can lose quite a lot of blood without experiencing any side effects or complications. The exact amount depends on your size, age and general health.
It helps to think of losses as percentages rather than totals. Men have grown to have more blood on average than most adult women. This means that they usually have a little more to lose before experiencing adverse effects. Children, on the other hand, have much less blood than adults, and even a small amount of blood loss can negatively affect a child.
Common causes of blood loss—office blood sampling, menstruation, nosebleeds—do not usually cause complications.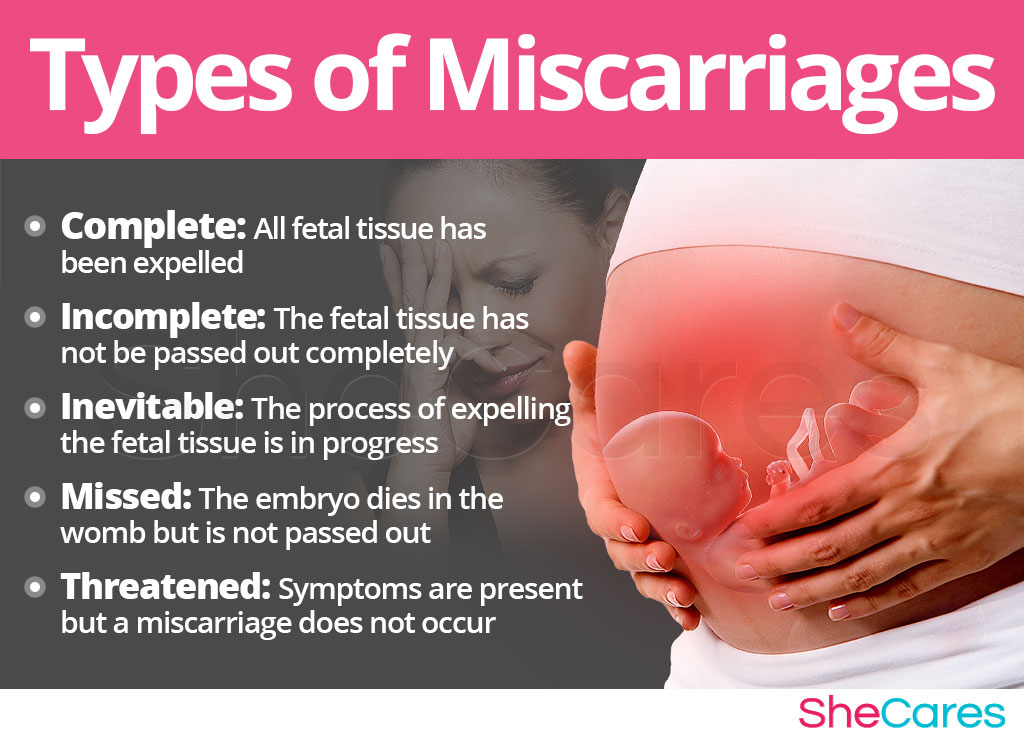 But if he retains an injury or undergoes surgery, it can cause severe bleeding and require a red blood cell transfusion.
But if he retains an injury or undergoes surgery, it can cause severe bleeding and require a red blood cell transfusion.
Read on to find out how much blood is lost in these situations and how much you can lose before nausea, fainting or other complications occur.
How much blood can you lose without side effects?
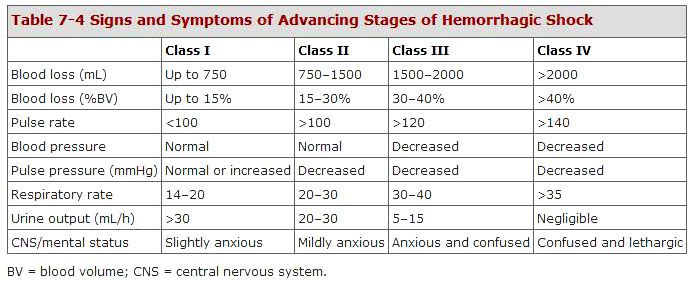
Most adults can lose 14 their blood without noticing any serious side effects or changes in vital signs. Some, on the other hand, may feel dizzy or dizzy if this amount is lost quickly.
You will start to experience mild side effects such as nausea when you experience blood loss. 15 to 30 percent of total blood volume. This loss increases the heart rate and respiration rate. Your urine output and blood pressure will decrease. You may feel anxious or uncomfortable.
Your body begins to compensate for the loss of blood by constricting blood vessels in the limbs and limbs. This is your body's attempt to maintain blood pressure and blood flow.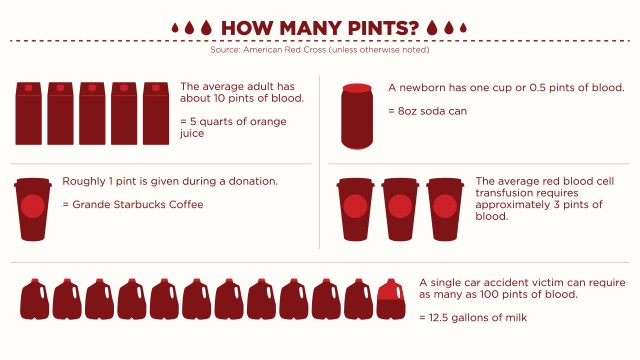 This subsequently reduces the amount of blood your heart pumps out of the center of your body. Your skin may become colder and paler.
This subsequently reduces the amount of blood your heart pumps out of the center of your body. Your skin may become colder and paler.
How much blood can happen before you pass out?
When approaching a blood loss of 30 to 40 percent of your total blood volume, your body will have a traumatic reaction. Your blood pressure will drop even more and your heart rate will increase even more.
You may show signs of obvious confusion or disorientation. Your breathing will become faster and shallower.
As volume loss increases, your body may not be able to maintain proper circulation and blood pressure. At this point, you may lose consciousness. You will need urgent help to prevent further blood loss and serious side effects.
How much blood loss can occur before hemorrhagic shock occurs?
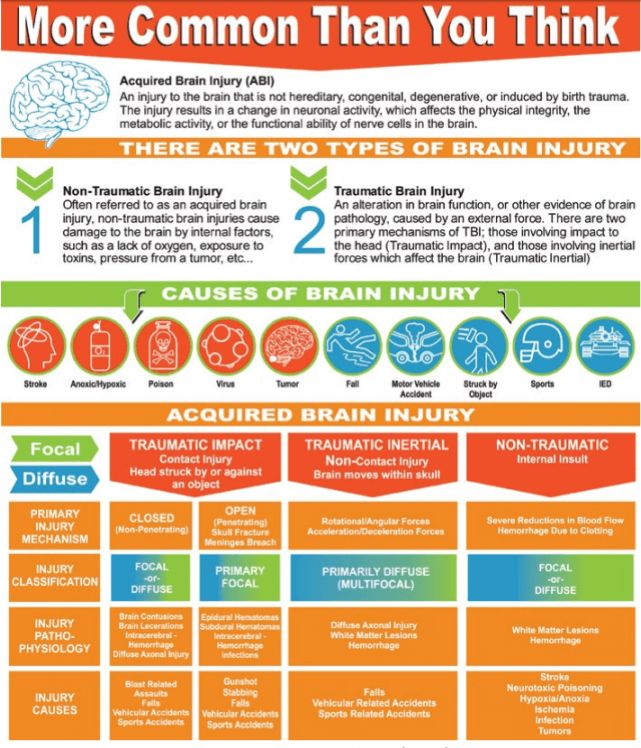
Hemorrhagic or hypovolemic shock occurs when you have lost 20 percent or more of your total blood volume. As blood loss increases, your symptoms will become more severe.
You may experience:
- rapid breathing
- weakness or fatigue
- confusion
- cold, pale skin
- sweaty, damp skin
- anxiety or discomfort
- low urine output
- hangover
- weak
Your body cannot compensate for the loss of blood volume on its own for much longer. above 40 percent At this point, your heart cannot properly maintain blood pressure, pumping, or circulation. Your organs may begin to deteriorate without proper blood and fluids. You will probably pass and go into a coma.
How much blood loss can occur before death?
Without treatment, your body will completely lose its ability to pump blood and maintain oxygen delivery after losing about 50 percent of your blood volume.
Your heart will stop beating, other organs will shut down, and you will probably fall into a coma. Death is likely unless aggressive life-saving measures are taken.
Your body can compensate for most of the blood loss. However, at some point, it eliminates unnecessary components to protect your heart.
However, at some point, it eliminates unnecessary components to protect your heart.
You will probably feel tired moments before falling into a coma. If they are close to death, these feelings may not even be noticed.
How much blood loss can occur before you need a blood transfusion to get well?
The average hemoglobin level is between 13.5 to 17.5 grams per deciliter for men and 12 to 15.5 grams per deciliter for women. Most doctors do not consider a transfusion until the hemoglobin level in the blood reaches 7 or 8 grams per deciliter.
This is not the only parameter included in the approach to managing volume loss in active bleeding. But the level of hemoglobin is important for the decision to transfuse RBCs. Your doctor and care team will use these and other factors to decide if a blood transfusion is needed and if it would be effective for your situation.
Is there a moment when a transfusion has no effect?
Blood loss greater than 40 may be difficult for physicians to correct a transfusion. This is especially true if bleeding is poorly controlled.
This is especially true if bleeding is poorly controlled.
Your doctor will consider several factors when deciding if a blood transfusion is right for you. This includes:
- your additional injuries
- the rate of blood loss
- the location of the blood loss
- your general health
How much blood is lost under normal conditions?
Minor blood loss is not common and not even dangerous. The average adult can lose a significant amount of blood without noticing any symptoms.
Here's how much blood is lost and what to expect from:
Blood donation
Exposure The average person loses one pint of blood when donating. Your body has about 10 pints of blood, so just when you donate blood, you lose about 10 percent of your total blood volume.
Nosebleeds
Nosebleeds may be bloodier than nosebleeds. The amount of blood you normally lose is not enough to cause complications. However, if you wet the gauze or tissue several times five minutes apart, you may need to seek medical attention to stop your nosebleed.
Bleeding hemorrhoids
Bright red blood on toilet paper or underwear can be alarming but rarely serious. Most people lose a small amount of blood due to a bleeding hemorrhoid. This level of blood loss is not usually a cause for concern.
Menstruation
The average person loses 60 milliliters of blood per period. People with heavier periods lose an eye 80 milliliters If you think you are losing more, see your doctor. Explaining how fast you go through pads or tampons will help your doctor determine if bleeding is heavy.
Miscarriage
Abortion bleeding that occurs very early in pregnancy is similar to bleeding during menstruation. However, the later the miscarriage occurs during pregnancy, the greater the blood loss. It can appear very suddenly and be quite severe. Other signs of a miscarriage include severe abdominal pain, back pain, and contractions.
Shipping
The average person loses 500 milliliters of blood during vaginal delivery. It's only half a quarter. Those who have a C-section typically lose 1,000 milliliters. You can lose more if complications arise, but your doctor and delivery team can usually manage the bleeding.
It's only half a quarter. Those who have a C-section typically lose 1,000 milliliters. You can lose more if complications arise, but your doctor and delivery team can usually manage the bleeding.
Laboratory tests
The average bottle of blood is 8.5 milliliters short. You need to take about 88 of these bottles of blood before you start experiencing side effects.
Surgery
Doctors and surgical staff work hard to reduce blood loss during surgery. However, some surgeries result in significant blood loss or occur as a complication of the procedure. Your doctor can give you an idea of how much you might lose during surgery and what you can do if you lose more than expected.
Essence
Your body can cope with blood loss, but how it happens and how much you lose will determine the outcome.
In some cases, blood loss may occur immediately. It is not uncommon to lose a significant amount of blood as a result of injury or accident. It can also happen slowly over a long period of time, which can make recognizing symptoms more tiring.