How many days child born
Baby due date - Better Health Channel
Summary
Read the full fact sheet- The unborn baby spends around 38 weeks in the uterus, but the average length of pregnancy, or gestation, is counted at 40 weeks.
- Pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later.
- Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a baby is considered full term if its birth falls between 37 to 42 weeks of the estimated last menstruation date.
The unborn baby spends around 37 weeks in the uterus (womb), but the average length of pregnancy, or gestation, is calculated as 40 weeks. This is because pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later, followed by five to seven days before it settles in the uterus. Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a pregnancy is considered full term if birth falls between 37 to 42 weeks of the estimated last menstruation date.
A baby born prior to week 37 is considered premature, while a baby that still hasn’t been born by week 42 is said to be overdue. In many cases, labour will be induced in the case of an overdue baby.
The average length of human gestation is 280 days, or 40 weeks, from the first day of the woman’s last menstrual period. The medical term for the due date is estimated date of confinement (EDC). However, only about four per cent of women actually give birth on their EDC. There are many online pregnancy calculators (see Baby due date calculator that can tell you when your baby is due, if you type in the date of the first day of your last period.
A simple method to calculate the due date is to add seven days to the date of the first day of your last period, then add nine months. For example, if the first day of your last period was 1 February, add seven days (8 February) then add nine months, for a due date of 8 November.
For example, if the first day of your last period was 1 February, add seven days (8 February) then add nine months, for a due date of 8 November.
Determining baby due date
Irregular menstrual cycles can mean that some women aren’t sure of when they conceived. Some clues to the length of gestation include:
- Ultrasound examination (especially when performed between six and 12 weeks)
- Size of uterus on vaginal or abdominal examination
- The time fetal movements are first felt (an approximate guide only).
Pregnancy ultrasound
A pregnancy ultrasound is a non-invasive test that scans the unborn baby and the mother’s reproductive organs using high frequency sound waves. The general procedure for a pregnancy ultrasound includes:
- The woman lies on a table.
- A small amount of a clear, conductive jelly is smeared on the woman’s abdomen.
- The operator places the small hand-held instrument called a transducer onto the woman’s abdomen.

- The transducer is moved across the abdomen. The sound waves bounce off internal structures (including the baby) and are transmitted back to the transducer. The sound waves are then translated into a two-dimensional picture on a monitor. The mother doesn’t feel or hear the transmission of the sound waves.
- By measuring the baby’s body parts, such as head circumference and the length of long bones, the operator can estimate its gestational age.
The diagnostic uses of pregnancy ultrasound
Apart from helping to pinpoint the unborn baby’s due date, pregnancy ultrasounds are used to diagnose a number of conditions including:
- Multiple fetuses
- Health problems with the baby
- Ectopic pregnancy (the embryo lodges in the fallopian tube instead of the uterus)
- Abnormalities of the placenta such as placenta praevia, where the placenta is positioned over the neck of the womb (cervix)
- The health of the mother’s reproductive organs.

Premature babies
A baby born prior to week 37 is considered premature. The odds of survival depend on the baby’s degree of prematurity. The closer to term (estimated date of confinement, or EDC) the baby is born, the higher its chances of survival - after 34 weeks gestation with good paediatric care almost all babies will survive.
Premature babies are often afflicted by various health problems, caused by immature internal organs. Respiratory difficulties and an increased susceptibility to infection are common.
Often there is no known cause for a premature labour; however, some of the maternal risk factors may include:
- Drinking alcohol or smoking during pregnancy
- Low body weight prior to pregnancy
- Inadequate weight gain during pregnancy
- No prenatal care
- Emotional stress
- Placenta problems such as placenta praevia
- Various diseases such as diabetes and congestive heart failure
- Infections such as syphilis.

Overdue babies
Around five out of every 100 babies will be overdue, or more than 42 weeks gestation. If you have gone one week past your due date without any signs of impending labour, your doctor will want to closely monitor your condition. Tests include:
- Monitoring the fetal heart rate
- Using a cardiotocograph machine
- Performing ultrasound scans.
The placenta starts to deteriorate after 38 weeks or so, which means an overdue baby may not get enough oxygen. An overdue baby could also grow too large for vaginal delivery. Generally, an overdue baby will be induced once it is two weeks past its expected date. Some of the methods of induction include:
- Vaginal prostaglandin gel - to help dilate the cervix
- Amniotomy - breaking the waters, sometimes called an artificial rupture of membranes (ARM)
- Oxytocin - a synthetic form of this hormone is given intravenously to stimulate uterine contractions.

Where to get help
- Your doctor
- Your obstetrician
- Midwife or childbirth educator
Things to remember
- The unborn baby spends around 38 weeks in the uterus, but the average length of pregnancy, or gestation, is counted at 40 weeks.
- Pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later.
- Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a baby is considered full term if its birth falls between 37 to 42 weeks of its estimated due date.
- Common concerns and discomforts: overdue baby, Mother’s Bliss, UK.
- Going Overdue, 2001, Centre for Reproduction and Minimally Invasive Surgery.
- Premmie-L FAQ and advice sheets, Parents of Premature Babies Inc.(Preemie-L). More information here.
- Pregnancy: what to expect when it’s past your due date, Family Doctor, USA.
- Ultrasound, Women Health Information, Royal Women’s Hospital, Melbourne. More information here.
This page has been produced in consultation with and approved by:
Baby due date - Better Health Channel
Summary
Read the full fact sheet- The unborn baby spends around 38 weeks in the uterus, but the average length of pregnancy, or gestation, is counted at 40 weeks.
- Pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later.
- Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a baby is considered full term if its birth falls between 37 to 42 weeks of the estimated last menstruation date.
The unborn baby spends around 37 weeks in the uterus (womb), but the average length of pregnancy, or gestation, is calculated as 40 weeks. This is because pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later, followed by five to seven days before it settles in the uterus. Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a pregnancy is considered full term if birth falls between 37 to 42 weeks of the estimated last menstruation date.
This is because pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later, followed by five to seven days before it settles in the uterus. Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a pregnancy is considered full term if birth falls between 37 to 42 weeks of the estimated last menstruation date.
A baby born prior to week 37 is considered premature, while a baby that still hasn’t been born by week 42 is said to be overdue. In many cases, labour will be induced in the case of an overdue baby.
The average length of human gestation is 280 days, or 40 weeks, from the first day of the woman’s last menstrual period. The medical term for the due date is estimated date of confinement (EDC). However, only about four per cent of women actually give birth on their EDC. There are many online pregnancy calculators (see Baby due date calculator that can tell you when your baby is due, if you type in the date of the first day of your last period.
A simple method to calculate the due date is to add seven days to the date of the first day of your last period, then add nine months. For example, if the first day of your last period was 1 February, add seven days (8 February) then add nine months, for a due date of 8 November.
Determining baby due date
Irregular menstrual cycles can mean that some women aren’t sure of when they conceived. Some clues to the length of gestation include:
- Ultrasound examination (especially when performed between six and 12 weeks)
- Size of uterus on vaginal or abdominal examination
- The time fetal movements are first felt (an approximate guide only).
Pregnancy ultrasound
A pregnancy ultrasound is a non-invasive test that scans the unborn baby and the mother’s reproductive organs using high frequency sound waves. The general procedure for a pregnancy ultrasound includes:
- The woman lies on a table.
- A small amount of a clear, conductive jelly is smeared on the woman’s abdomen.
- The operator places the small hand-held instrument called a transducer onto the woman’s abdomen.
- The transducer is moved across the abdomen. The sound waves bounce off internal structures (including the baby) and are transmitted back to the transducer. The sound waves are then translated into a two-dimensional picture on a monitor. The mother doesn’t feel or hear the transmission of the sound waves.
- By measuring the baby’s body parts, such as head circumference and the length of long bones, the operator can estimate its gestational age.
The diagnostic uses of pregnancy ultrasound
Apart from helping to pinpoint the unborn baby’s due date, pregnancy ultrasounds are used to diagnose a number of conditions including:
- Multiple fetuses
- Health problems with the baby
- Ectopic pregnancy (the embryo lodges in the fallopian tube instead of the uterus)
- Abnormalities of the placenta such as placenta praevia, where the placenta is positioned over the neck of the womb (cervix)
- The health of the mother’s reproductive organs.

Premature babies
A baby born prior to week 37 is considered premature. The odds of survival depend on the baby’s degree of prematurity. The closer to term (estimated date of confinement, or EDC) the baby is born, the higher its chances of survival - after 34 weeks gestation with good paediatric care almost all babies will survive.
Premature babies are often afflicted by various health problems, caused by immature internal organs. Respiratory difficulties and an increased susceptibility to infection are common.
Often there is no known cause for a premature labour; however, some of the maternal risk factors may include:
- Drinking alcohol or smoking during pregnancy
- Low body weight prior to pregnancy
- Inadequate weight gain during pregnancy
- No prenatal care
- Emotional stress
- Placenta problems such as placenta praevia
- Various diseases such as diabetes and congestive heart failure
- Infections such as syphilis.
Overdue babies
Around five out of every 100 babies will be overdue, or more than 42 weeks gestation. If you have gone one week past your due date without any signs of impending labour, your doctor will want to closely monitor your condition. Tests include:
- Monitoring the fetal heart rate
- Using a cardiotocograph machine
- Performing ultrasound scans.
The placenta starts to deteriorate after 38 weeks or so, which means an overdue baby may not get enough oxygen. An overdue baby could also grow too large for vaginal delivery. Generally, an overdue baby will be induced once it is two weeks past its expected date. Some of the methods of induction include:
- Vaginal prostaglandin gel - to help dilate the cervix
- Amniotomy - breaking the waters, sometimes called an artificial rupture of membranes (ARM)
- Oxytocin - a synthetic form of this hormone is given intravenously to stimulate uterine contractions.
Where to get help
- Your doctor
- Your obstetrician
- Midwife or childbirth educator
Things to remember
- The unborn baby spends around 38 weeks in the uterus, but the average length of pregnancy, or gestation, is counted at 40 weeks.
- Pregnancy is counted from the first day of the woman’s last period, not the date of conception which generally occurs two weeks later.
- Since some women are unsure of the date of their last menstruation (perhaps due to period irregularities), a baby is considered full term if its birth falls between 37 to 42 weeks of its estimated due date.
- Common concerns and discomforts: overdue baby, Mother’s Bliss, UK.
- Going Overdue, 2001, Centre for Reproduction and Minimally Invasive Surgery.
- Premmie-L FAQ and advice sheets, Parents of Premature Babies Inc.(Preemie-L). More information here.
- Pregnancy: what to expect when it’s past your due date, Family Doctor, USA.

- Ultrasound, Women Health Information, Royal Women’s Hospital, Melbourne. More information here.
This page has been produced in consultation with and approved by:
Your baby was born prematurely | Regional Perinatal Center
Premature babies
If your baby is born too early, the joy of having a baby can be overshadowed by health concerns and thoughts about the possible consequences.
Instead of returning home with the baby, holding him and caressing him, you will have to stay in the department, learn to cope with the fear of touching the baby, realize the need for treatment and various manipulations, get used to the complex equipment that surrounds him.
In this situation, not only your baby needs help, you need it too! The best assistants are your loved ones, their love and care, as well as professional advice and recommendations from doctors and psychologists. This section of articles will help you improve your knowledge of preterm infant care, development and nutrition.
Your help for the baby
Previously, parents were often not allowed into the neonatal unit and, especially, into the intensive care unit because of the fear of infection of the baby, but now the contact of the parent with the child is recognized as desirable and is prohibited only in exceptional cases (for example, if parents have acute infections)
Close communication between you and your baby is very important from the first days of his life. Even very immature premature babies recognize the voices and feel the touch of their parents.
The newborn needs this contact. Studies have shown that it greatly contributes to the faster adaptation of an immature child to new conditions and the stabilization of his condition. The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
By constantly and attentively observing the baby, parents can notice the smallest changes in his condition before others. In addition, communication in the hospital is a good practice that will undoubtedly come in handy after discharge. For parents, early physical contact with the baby is very valuable, because it allows them to feel him, despite the incubator and other obstacles, and show him their love.
Treatment in the neonatal intensive care unit requires parents to have full confidence in all medical staff.
Nursing premature babies in the hospital
Many premature babies cannot breathe, suckle and regulate their body temperature sufficiently after birth. Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems.
Fluid loss due to the immaturity of the skin of premature babies and the insufficiency of thermoregulation processes require constant attention. Modern approaches focused on nursing premature babies help to cope with these problems.
Modern approaches focused on nursing premature babies help to cope with these problems.
Heat regulation incubator
Premature babies are very susceptible to temperature fluctuations. At the same time, clothing can interfere with the monitoring of the baby's condition and its treatment. That is why an incubator is used to provide the conditions necessary for premature babies. It maintains a certain temperature and humidity, which change as the child grows. When the body weight of a premature infant reaches 1500-1700 g, he can be transferred to a heated bed, and after reaching a weight of 2000, most premature babies can do without this support. There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.
In incubators, very young premature babies are placed in special "nests" - soft hemispheres in which the baby feels comfortable and assumes a position close to intrauterine. It must be protected from bright lights and loud noises. For this purpose, special screens and coatings are used.
It must be protected from bright lights and loud noises. For this purpose, special screens and coatings are used.
Critical treatments during the first days of life of premature babies with low and very low birth weight:
Use of an incubator or heated bed.
Oxygen supply for respiratory support.
If necessary, artificial ventilation of the lungs or breathing using the CPAP system.
Intravenous administration of various drugs and fluids.
Carrying out parenteral nutrition with solutions of amino acids, glucose and fat emulsions.
Don't worry: not all premature babies need such extensive treatment!
Mechanical ventilation and CPAP for respiratory support
When it comes to nursing, oxygen supply is of the utmost importance for premature babies. In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
This new method made it possible for the majority of even very immature children to do without mechanical ventilation. The need for intubation of children has disappeared: during treatment with CPAP, oxygen is supplied through short tubes - cannulas that are inserted into the nasal passages. CPAP or mechanical ventilation is continued until the lungs can function at full capacity on their own.
In order for the lungs to expand and remain in such a state in the future, a surfactant is needed - a substance that lines the alveoli from the inside and reduces surface tension. Surfactant is produced in sufficient quantities starting from the 34-35th week of pregnancy. Basically, it is by this time that the formation of the lungs is completed. If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
Parenteral nutrition - administering nutrient solutions by vein
Premature babies, especially those born weighing less than 1500 g, are not able to get and absorb enough nutrients, even when fed through a tube. For the rapid growth of the baby, a large amount of nutrition is needed, and the size of the stomach is still very small, and the activity of digestive enzymes is also reduced. Therefore, such children are given parenteral nutrition.
Special nutrients are injected into a vein using infusion pumps that deliver solutions slowly at a predetermined rate. In this case, amino acids necessary for building proteins, fat emulsions and glucose, which are sources of energy, are used. These substances are also used for the synthesis of a number of hormones, enzymes and other biologically active substances. Additionally, minerals and vitamins are introduced.
Gradually, the volume of enteral nutrition increases, and parenteral nutrition decreases until it is completely canceled.
Premature infants with gastrointestinal disease require parenteral nutrition for a longer period of time.
By the time your grown baby is discharged from the hospital, everything should be well prepared at home. And this applies not only to the environment, clothes and means of caring for the child.
All family members must be ready to receive the baby. Of course, the main care will fall on the shoulders of the parents. Although you have already gained some experience in the hospital, it is important to feel the support of others, especially in the early days.
Older children can also help. The discharge of your baby is a great joy that you want to share with all your relatives.
While you are getting used to your new role, it is important that nothing distracts you from communicating with your child. Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Preparing for discharge from the hospital
Before discharge, you must make sure that:
- Prepared the crib, bath for bathing and a place for changing clothes, preferably a changing table. A crib should be placed in the parents' bedroom, the child should not be left alone even at night. A stroller is also required. you have baby milk that was recommended by the doctor before discharge (if the child is on mixed or artificial feeding). As a rule, this is a specialized medical product. You need a certain number of small bottles and teats of the appropriate size, as well as a sterilizer. All premature babies will need pacifiers.
- You have fully mastered breastfeeding or bottle feeding.
- If your baby is not suckling all the required amount of milk from the breast and is supplementing from a bottle, you have purchased a breast pump that you have learned to use; you may also need it if you have a lot of breast milk.
- You have asked your doctor how often your child's weight should be monitored.
- If your baby still needs medication, you have the required amount at home. And you know exactly how and when to give them to your child.
- You know which warning signs to look out for.
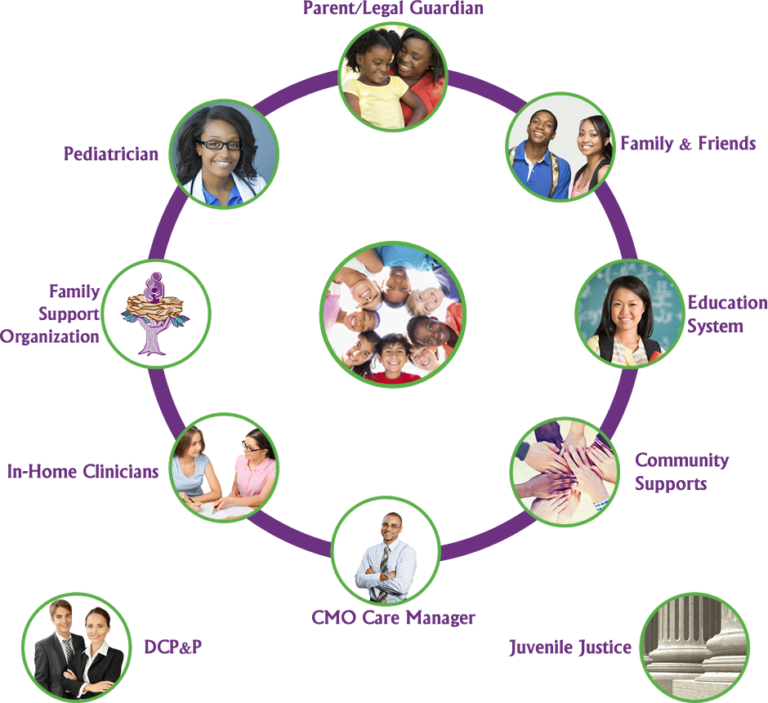
- After the baby is discharged, a pediatrician and a neonatologist will look after the baby, to whom you will give the discharge summary from the hospital.
- You know how the hospital from which your child is being discharged will provide follow-up care after discharge.
- You know which specialists and how often should examine your baby (oculist, neuropathologist, etc.).
- All the emergency phone numbers you need are at your fingertips.
When can a child go home
This question is very difficult to answer because all children are different. The stay in the hospital can last from 6 days to 6 months, depending on the degree of prematurity of the child, the severity of his condition, as well as the presence of certain complications.
Of course, all parents look forward to the moment when the baby can be brought home. Long-term nursing of a premature baby is often a difficult test for you. But we must not forget that safety comes first, and the baby can be discharged home only when the doctors are confident in the stability of his condition. It is certainly in your interest as well.
The rate of increase in body weight and length
Weight gain is the main indicator of the growth of the baby and the adequacy of the treatment. The weight of the child, especially in the first days and weeks of life, is influenced by a number of factors: the presence of milk in the stomach (immediately after feeding), the time of bowel movement, the degree of filling of the bladder, the presence of edema. Therefore, if an edematous child does not gain weight for several days, and perhaps even loses it, do not worry. It should be remembered that children grow unevenly and periods of high weight gain alternate with lower ones. It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is currently accepted that in the interval corresponding to 28-34 weeks of pregnancy, the normal weight gain of the child is 16-20 g/kg per day. Then it is reduced to 15 g/kg.
It is also important to take into account the rate of increase in body length. With malnutrition, at first the child gains less weight (or even loses it), and with a more pronounced deficiency of nutrients, his growth is also disturbed.
The weight must not only increase at a certain rate, but must also correspond to the length of the baby. An important parameter characterizing the development of the baby is an increase in the circumference of the head. The brain most actively increases in size during the first 12–18 months of life. But an excessively rapid increase in head circumference, as well as a slowdown in its increase, indicate neurological disorders.
A premature baby can be discharged from the hospital if:
- he is able to independently maintain the required body temperature;
- does not need breathing support and constant monitoring of the work of the respiratory and cardiovascular systems;
- can suck out the required amount of nutrition on its own;
- does not need round-the-clock monitoring and frequent determination of biochemical or other indicators;
- supportive care can be provided at home;
- he will be under the supervision of a local pediatrician and neonatologist at the place of residence.

The decision to discharge home is made for each patient individually. In addition to the state of health of the baby, the degree of preparedness of parents, their ability to provide high-level care for a premature baby is also taken into account.
Feeding a premature baby after discharge
Breastfeeding is the ideal way to feed premature babies.
However, if the baby was born much prematurely and his birth weight did not exceed 1800-2000 g, his high nutritional requirements cannot be met by breastfeeding. The growth rate will be insufficient. Moreover, over time, the content of many nutrients, including protein, in milk decreases. And it is the main material for building organs, and primarily brain tissue. Therefore, proteins must be supplied to the body of a premature infant in the optimal amount.
In addition, premature babies have a significantly increased need for calcium and phosphorus, which are essential for bone formation.
In order for the baby's nutrition to be complete even after being discharged from the hospital, special additives - "enrichers" are introduced into breast milk in a certain amount, already less than in the hospital. They make up for the lack of protein in it, as well as some vitamins and minerals. As a result, the child receives them in the optimal amount. The duration of their use will be determined by your doctor. If there is not enough milk or it does not exist at all, children born prematurely should be transferred to artificial feeding. Complementary feeding of premature babies is carried out with special children's dairy products designed for children with low birth weight. This baby milk is ideally suited to both the ability of immature children to digest and assimilate nutrients, and their needs.
Premature infant milk contains more protein, fat and carbohydrates than term infant milk, resulting in a higher calorie content. In specialized baby milk, the concentration of many minerals is higher, especially iron, zinc, calcium, phosphorus, as well as vitamins, including vitamin D. Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
At present, specialized children's dairy products have been developed and are being used to feed premature babies after discharge from the hospital. In its composition, it occupies an intermediate position between a specialized product for premature babies and regular baby milk. Your baby will be transferred to such baby milk while still in the hospital. You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
Feeding needs for premature babies
Higher caloric intake because they need to gain weight faster than term babies.
More protein as premature babies grow faster.
More calcium and phosphorus for bone building.
More trace elements and vitamins for growth and development.
A premature baby grows faster than a term baby. Nutrition for such children is calculated taking into account body weight at birth, the age of the baby and its growth rate. As a rule, the calorie content of the daily diet is about 120-130 calories per 1 kg of body weight.
It is very important that your baby continues to gain weight quickly and grow in length after discharge. To do this, feeding premature babies must be carried out using a specialized fortified diet prescribed by a doctor.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It's not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth, so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling, or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps you recover after childbirth? This is because oxytocin stimulates uterine contractions.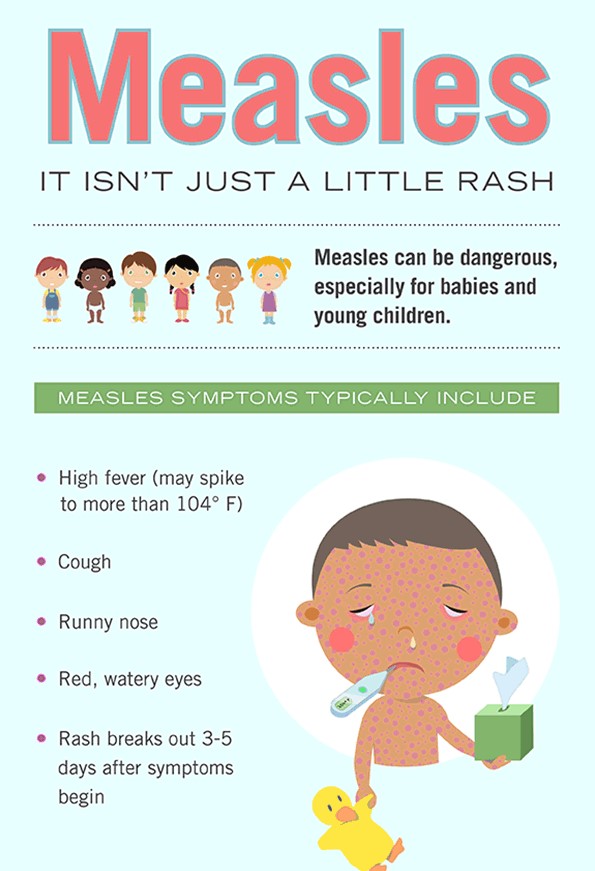 In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What should I do if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding. ”
”
To start milk production, you can express milk manually or use a breast pump, which can be given to you at the maternity hospital. 5 And with expressed precious colostrum, it will be possible to feed a child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby is born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is a prerequisite for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk, and therefore grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When you put your baby to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“If the baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
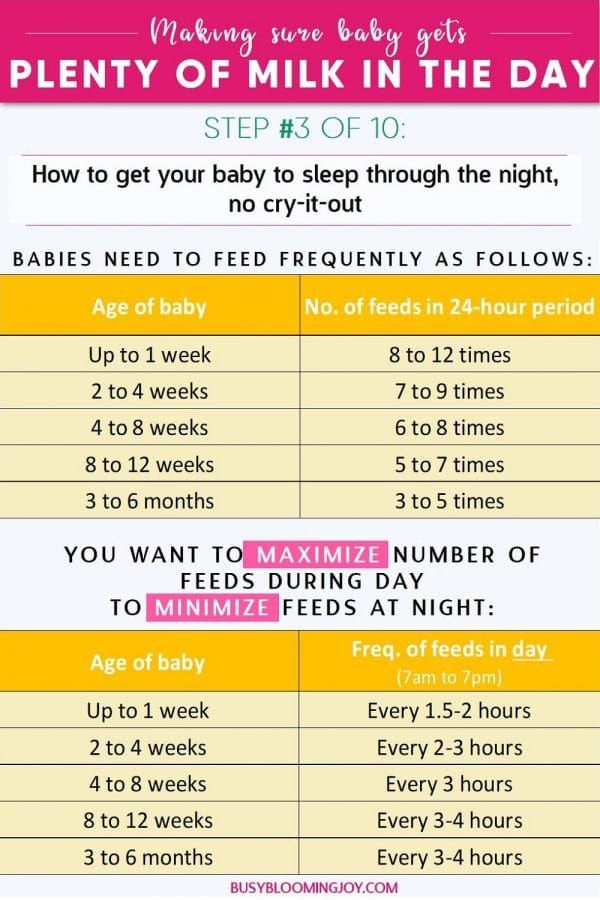
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and produced in smaller quantities, but it provides many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination for effective suckling.
7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination for effective suckling.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in his sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before childbirth. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Second day
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
11
Does the baby get enough breast milk?
Since very little milk is produced at first,
you may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes given above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”recommends Katie.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2): S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2): S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." W Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
- Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM.