How long do you bleed after child birth
What's Normal, What's Not, Causes, Treatment
Written by Paige Fowler
Medically Reviewed by Traci C. Johnson, MD on December 03, 2021
In this Article
- What's Normal
- When to Call Your Doctor
- What Causes It?
- How It's Treated
If you have a vaginal delivery or Cesarean section, you’ll have vaginal bleeding and discharge after birth. This is known as lochia. It’s how your body gets rid of the extra blood and tissue in your uterus that helped your baby grow.
Bleeding is heaviest the first few days after your baby is born. But if heavy bleeding continues after that, you may need to call your doctor.
What's Normal
Your blood will be bright red, and you may see some clots for the first few days after you give birth. They shouldn’t be bigger than a quarter. You’ll have to wear a hospital-grade pad at first. But you should be able to go back to a regular pad later.
You might bleed a little more when you bring your baby home. This may be because you’re moving around a lot. If this happens, try to stay off your feet and rest a little.
It’s also normal to sometimes feel a gush of blood when you stand. This is because of the way your vagina is shaped. The blood collects in a cup-like area while you’re sitting or lying down. When you stand, it comes out.
After about 10 days, you should see less blood. You may have light bleeding or spotting for up to 6 weeks after delivery. You can only use sanitary pads during this time. Tampons could lead to an infection.
When to Call Your Doctor
Heavy bleeding after giving birth is called postpartum hemorrhage. It affects up to 5% of women who give birth. It’s most likely to happen the first 24 hours after delivery. But it can happen anytime within the first 12 weeks after your baby is born.
Postpartum hemorrhage is serious. It can cause a big drop in your blood pressure. If the pressure gets too low, your organs won’t get enough blood. This is shock, and it can cause death.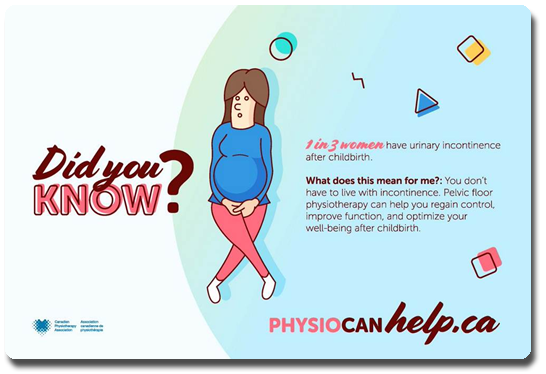 That’s why it’s important to get medical help right away.
That’s why it’s important to get medical help right away.
Tell your doctor or call 911 if you have any of these symptoms or signs:
- Bright red bleeding beyond the third day after birth
- Blood clots bigger than a plum
- Bleeding that soaks more than one sanitary pad an hour and doesn’t slow down or stop
- Blurred vision
- Chills
- Clammy skin
- Rapid heartbeat
- Dizziness
- Weakness
- Nausea
- Faint feeling
What Causes It?
Certain things can raise your chance of postpartum hemorrhage. You’re at higher risk if you’ve had it before. For unknown reasons, Asian and Hispanic women are more likely to have it.
The most common cause of postpartum hemorrhage is something called uterine atony. Normally, the uterus squeezes after delivery to stop bleeding where the placenta was. The placenta is an organ that grows in your uterus during pregnancy and nourishes your baby. With uterine atony, the uterus doesn’t contract as well as it should.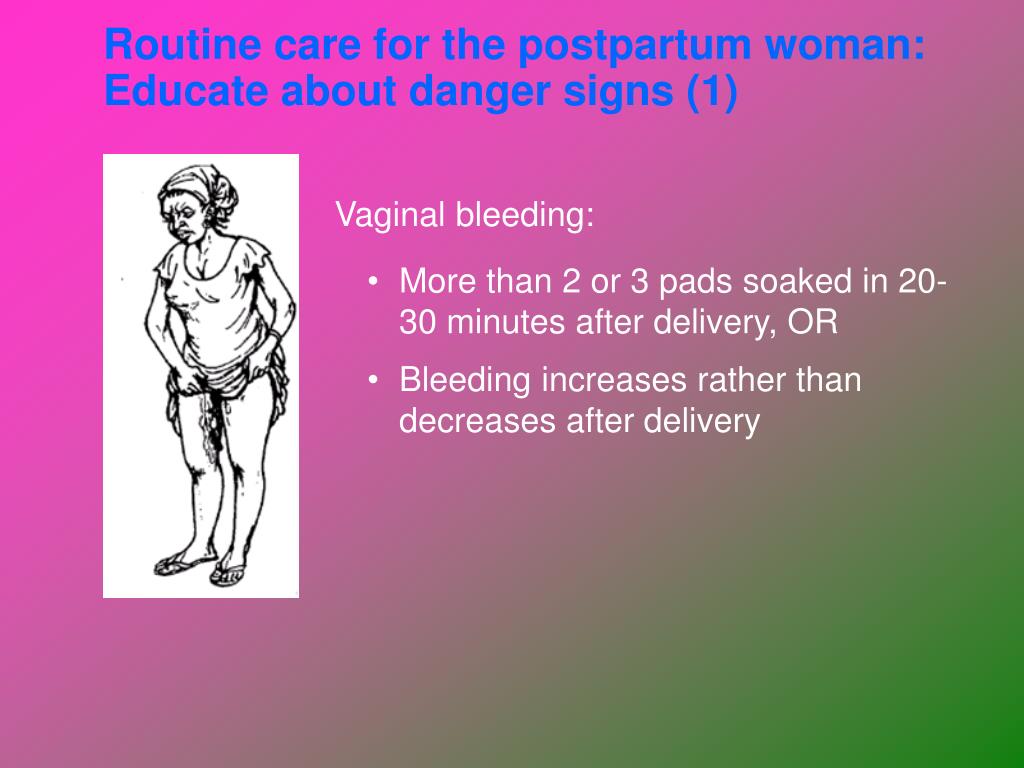 This can cause heavy bleeding after you give birth.
This can cause heavy bleeding after you give birth.
You may be more likely to have this if you:
- Give birth to more than one child at a time (twins, for example)
- Have a baby bigger than 8 pounds 13 ounces
- Are in labor for a long time
- Have given birth several times before
Other conditions can raise your risk for postpartum hemorrhage. These include:
- Uterine rupture -- when the uterus tears during labor
- Cesarean section -- your risk for postpartum hemorrhage is higher compared with a vaginal delivery
- Tears in the vagina or cervix during delivery
- General anesthesia -- this may be used if you have a Cesarean section
- Oxytocin (Pitocin) -- a medicine that makes you go into labor
- Preeclampsia -- high blood pressure and protein in your urine that develops during pregnancy
- Obesity
- Issues that affect the placenta
How It's Treated
There are many different treatments for postpartum hemorrhage. The cause of your bleeding will help your doctor decide what may be best for you.
The cause of your bleeding will help your doctor decide what may be best for you.
They could:
- Give you medicine to help your uterus contract
- Massage your uterus
- Remove pieces of the placenta still in your uterus
- Perform a laparotomy -- surgery to open your abdomen to find out the cause of bleeding and stop it
- Give you a blood transfusion -- blood is given to you through a tube that goes in a vein to help replace blood you've lost
- Perform a hysterectomy -- surgical removal of the uterus
- Give you a shot of a special medicine to stop the bleeding
- Have a radiologist do what's called a uterine artery embolization, which limits blood flow to your uterus
- Use something called a Bakri balloon that's inflated inside your uterus and adds pressure to help slow the bleeding
Bleeding after birth: 10 things you need to know | Life as a parent articles & support
It may be one of the few things you haven’t discussed with friends. Here’s an honest, clear account of what you can expect with bleeding after birth.
Here’s an honest, clear account of what you can expect with bleeding after birth.
1. Every woman bleeds after they give birth
You will have vaginal bleeding after you’ve given birth(NHS, 2021). This bleeding is known as lochia. The lochia is a combination of mucous, tissue and blood that your womb sheds as it replaces its lining after you’ve given birth (UHS NHS Foundation Trust, 2020).
2. Bleeding after birth may last for a while
Bleeding often lasts for around for four to six weeks, but could last up to 12 weeks after your baby's born (RCOG, 2016). If you’re worried, you can talk to a health professional.
Bleeding will start off heavy and red to browny red. It will become lighter in colour and flow over time (NHS, 2021).
Here’s what you can expect:
- Day 1: Fresh red to brownish-red blood. Heavy flow that probably soaks one maternity pad every few hours, with one or two clots or several smaller ones.
- Day 2 to 6: Darker brown or pinkish red blood.
 Moderate flow with 7 cm to 12 cm stains on your maternity pads and smaller blood clots.
Moderate flow with 7 cm to 12 cm stains on your maternity pads and smaller blood clots. - Day 7 to 10: Darker brown or pinkish red blood, becoming lighter. Variable but lighter flow, with less than a 7 cm stain on your pads.
- Days 11 to 14: Darker brown or pinkish red blood, becoming lighter. Lighter flow, you may have some sanitary towels that are hardly stained.
- Week 3 to 4: Paler, possibly a creamy white blood loss. Lighter flow.
- Week 5 to 6: Brown, pinkish red, or creamy yellow stains, possibly for several weeks, and possibly only on some days (UHS NHS Foundation Trust, 2020).
3. Don’t keep quiet about clots
They’re common. Discuss any clots with your midwife as she’ll want to keep track of what’s happening. Save your maternity pads to show your midwife if possible. Passing a lot of large clots can flag up something more serious (NHS, 2021).
4. If you pass a lot of large blood clots or more than a pint of blood in the first 24 hours, talk to a health professional immediately
Passing lots of large blood clots or more than a pint of blood in the first 24 hours after birth are symptoms of primary postpartum haemorrhage (RCOG, 2016).
Severe postnatal blood loss can make you feel even more exhausted than is normal after giving birth but it can also be life threatening. Getting quick treatment is essential before it becomes a major haemorrhage.
Treatment normally involves helping your uterus to contract through massaging the belly, an injection to contract the uterus, and a catheter into your bladder. The doctors will check to make sure all of the placenta has come out, and may have to do this under general anaesthetic. You will also have a drip in your arm and blood taken for tests.
5. The risk factors for primary postpartum haemorrhage
Before labour, risk factors are:
- Previous postpartum haemorrhages
- A body mass index (BMI) above 35
- A twin or triplet pregnancy
- Low-lying placenta (placenta previa)
- Placenta coming away early (placental abruption)
- Pre-eclampsia or high blood pressure
- Anaemia
- Growths in or around the womb (e.
.jpg) g. fibroids)
g. fibroids) - Taking blood-thinning medication
- Blood clotting problems.
During labour, risk factors are:
- Caesarean section birth
- Induced labour
- Retained placenta
- Episiotomy
- Forceps or vacuum-assisted vaginal delivery (ventouse) birth
- Your labour lasted longer than 12 hours
- Having a baby that weighs more than 4kg (9lbs)
- Having your first baby when you’re over 40 years old
- Having a raised temperature during labour
- Having a general anaesthetic.
(RCOG, 2016)
6. Think about postpartum bleeding when you pack your hospital bag
Pack maternity pads rather than menstrual pads as they’ll be more absorbant and allow the area between the vagina and anus (perineum) to heal with the least irritation. Describing the number of maternity pads you’re using also gives your midwife a clear picture of how much blood loss you’re experiencing.
7. Lots of things can affect the amount of blood loss
Breastfeeding makes your body release oxytocin. This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
Any sort of gentle exercise – even a quick vacuum of the lounge – could also make bleeding heavier. This is especially true in the first two weeks.
Bleeding will tend to be heavier in the morning too. This is because blood pools when you lay down sleeping.
8. It’s important to keep an eye on your blood loss in the weeks after giving birth
It’s possible to get secondary postpartum haemorrhage, which is abnormal or heavy bleeding between 24 hours and 12 weeks after giving birth. It’s often associated with an infection, and sometimes with part of the placenta remaining in the womb (RCOG, 2016).
Symptoms include:
- Feeling shaky, feverish, and generally ill.
- Having lochia with an offensive smell.
- Heavier than expected bleeding, or bleeding that becomes heavier rather than lighter over time. (UHS NHS Foundation Trust, 2015; RCOG, 2016)
If you have any of these symptoms, you should speak to your GP or health visitor immediately (RCOG, 2016).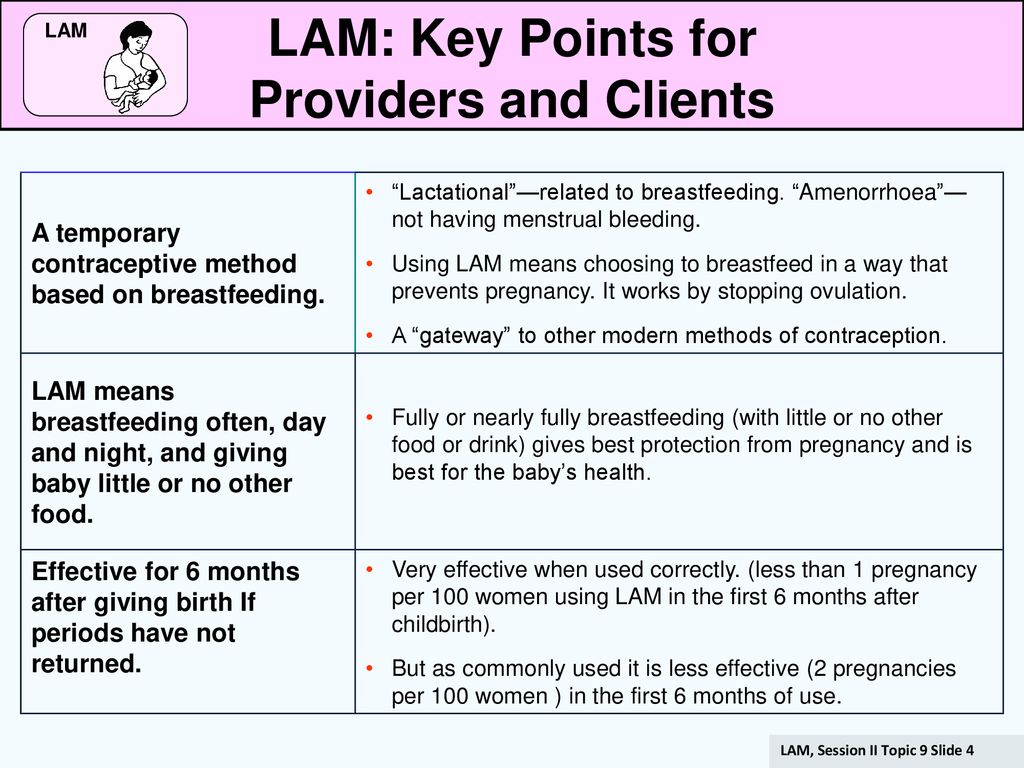 Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Severe pain in the womb in the six weeks after birth could be a sign of a serious infection called sepsis, and should be treated with urgency because it can be life-threatening (RCOG, 2012). Other symptoms of sepsis include a high or low temperature, vomiting, diarrhoea, a rash and offensive discharge (RCOG, 2012). If you are experiencing these symptoms, go straight to the emergency department, say that you have recently given birth, and ask if this could be sepsis.
9. It’s important to reduce your risk of infection
Wash your hands thoroughly before and after using the toilet and changing your maternity pad (NICE, 2021).
10. Always speak to your GP or health visitor if anything doesn’t feel right
In the end, trust your judgement. If you have any worries about your bleeding after you give birth, talk to a health professional.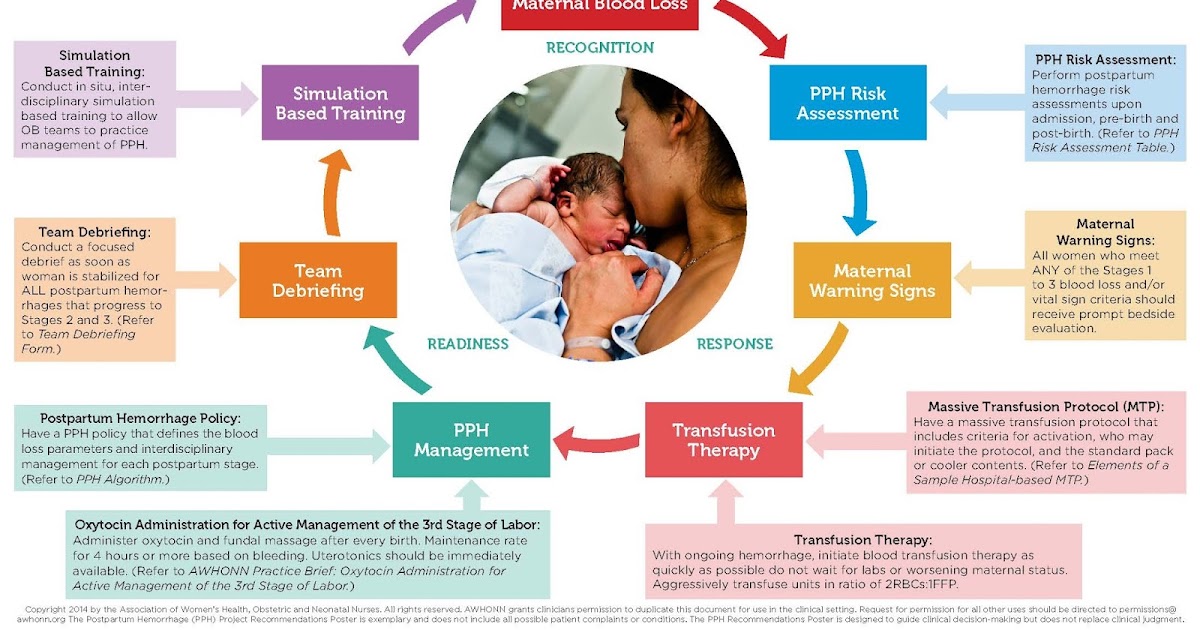 They’re there to help.
They’re there to help.
This page was last reviewed in November 2021
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
You might find attending one of our Early Days groups helpful as they give you the opportunity to explore different approaches to important parenting issues with a qualified group leader and other new parents in your area.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.
Discharge after childbirth - what is lochia and how long does it last
Discharge does not stop after discharge from the hospital
The birth of a child is always a lot of changes: in the end, a new person has appeared, and he needs care! For 9 whole months, you adjusted to each other, both physically and emotionally.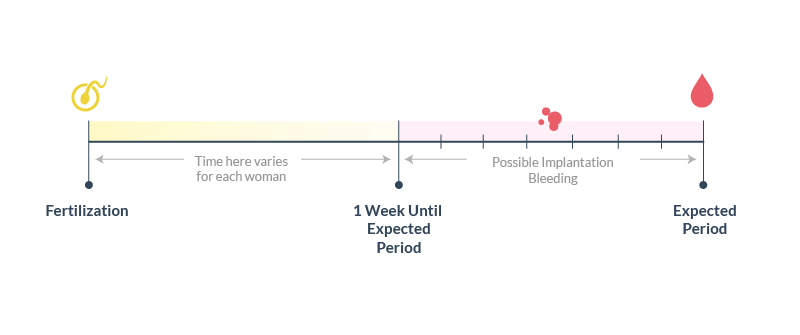 And these changes do not stop immediately after childbirth. Your body continues to change and adapt.
And these changes do not stop immediately after childbirth. Your body continues to change and adapt.
In order to recover and return to his normal shape, he will have to get rid of excess blood and tissue that helped support the growth of the baby (or babies) in the womb. Read on to learn all about postpartum discharge.
Lochia - what is it?
During childbirth, your vagina, like the rest of your body, went through a lot, and it is not surprising that something is secreted from it: this is how your body gets rid of the uterine lining that was necessary during pregnancy, and now begins to regenerate . Such discharge after childbirth is called lochia.
They are like menstrual blood so you have a good idea of what to expect. Their duration is up to six weeks after the birth of the baby.
Like menses, lochia is not just blood, but a combination of blood, mucus, white blood cells, placental debris, and bits of uterine lining.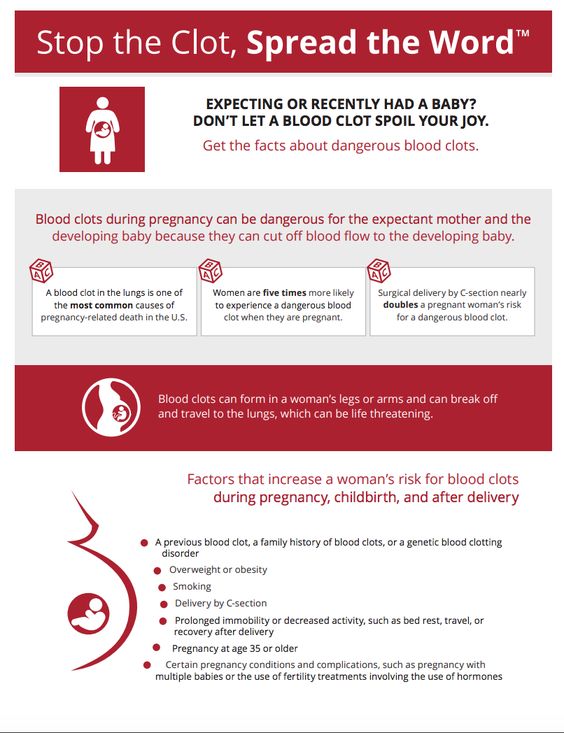 Their consistency changes over time. At first, the discharge after childbirth is bloody, and after a few weeks - more mucous.
Their consistency changes over time. At first, the discharge after childbirth is bloody, and after a few weeks - more mucous.
Lochia after natural childbirth
Immediately after childbirth, the discharge will be mostly bloody - bright red or dark red, with a characteristic smell of menstrual blood. They can contain clumps the size of grapes or even prunes, and sometimes more.
Four to seven days after delivery, the discharge will become pinkish or brownish in color and the clots will likely decrease or even disappear completely.
At the end of the first week, the color of the discharge will become more white or yellow. The profusion will decrease until the discharge after childbirth finally stops - after about 3-6 weeks.
Lochia after caesarean section
If delivery is by caesarean section, there may be less lochia. This is because during a caesarean section, the doctor manually cleans the uterine cavity with a swab or sponge, removing the placenta, blood clots, and remnants of cell membranes that would have left the body in the form of lochia on their own during natural childbirth [1].
Although not as abundant, lochia will still stand out: be prepared for this. Their color will gradually change from red to brown, and then finally to yellow or transparent. The good news is that eventually, postpartum discharge will stop and your menstrual cycle will return.
Is it possible to avoid discharge after childbirth?
Postpartum discharge is an inevitable, natural part of childbirth, it's just rarely talked about. It may seem like a lot because you need to take care of a newborn, but with the support of loved ones and the right hygiene products, the situation can be quite under control.
Most importantly, remember to change your pads frequently to prevent infection and stay away from tampons until your doctor says you can use them again. In the hospital, you can use large postpartum pads. They will help to cope with the initial heavy bleeding. Then, in the first few days after giving birth, our absorbent pads, such as Maxi Extra Long Pads, come to the rescue.
Some women prefer to use disposable panties to keep their pads in place so you don't get nasty surprises like stains on your favorite underwear.
When the post-partum discharge is less heavy, you can return to your favorite pads, such as our Ultra Normal. And in a few weeks there will be enough daily, for example, Libresse Normal Plus.
When to see a doctor about postpartum discharge
Every woman experiences lochia differently. Postpartum discharge can be erratic and unexpected - it's just that your body recovers at its own pace and is usually nothing to worry about. However, there are signs to look out for - they may indicate that you need medical attention.
Seek medical attention if a pad fills up completely in less than an hour, or if the amount of bleeding does not decrease a few days after delivery. If the clots are very large or there are a lot of them, this may mean that there is a problem with the uterus shrinking to its original size.
Some other symptoms to look out for:
• Pungent smell of discharge;
• High fever or chills;
• Perspiration;
• Profuse or bright red spotting in the second week after delivery;
• Tenderness on one or both sides of the abdomen;
• Dizziness or weakness;
• Rapid, irregular heartbeat.
When it comes to postpartum discharge, all you can do is be patient and let your body and mind recover. Take care of yourself, because your health is now a priority, if necessary, ask for help from loved ones. And remember: there's nothing a super absorbent pad can't handle!
If you want to know more about what can happen after childbirth, read our articles on how the vagina changes during this period and when to expect the first period after the baby is born.
Medical disclaimer
The medical information contained in this article is for reference only and should not be used for any diagnostic or therapeutic purposes.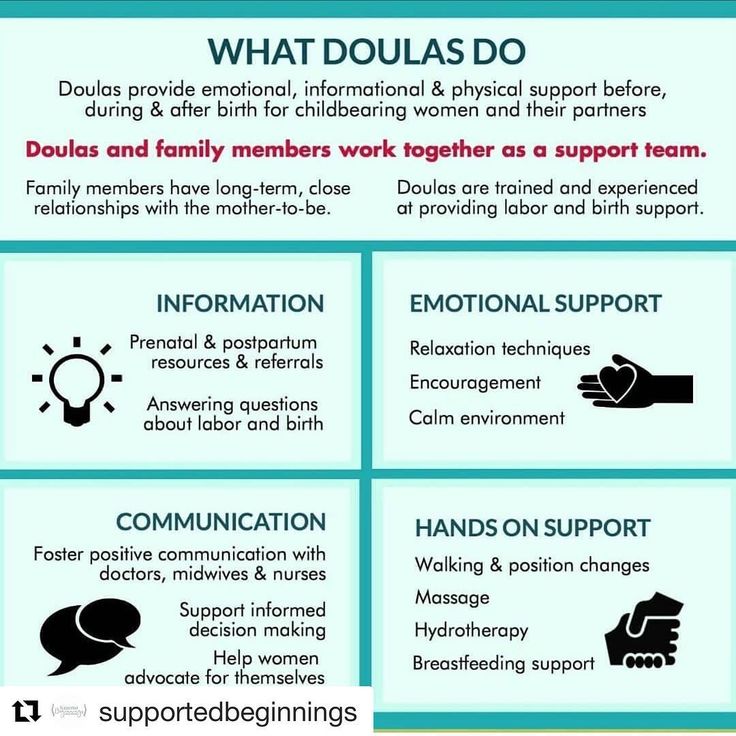 Consult your doctor about a specific medical condition.
Consult your doctor about a specific medical condition.
Links:
note-1 [1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6363334/
Postpartum - recovery, nutrition, sex after childbirth
Yulia Novitsyuk, an obstetrician-gynecologist at the ISIDA clinic, talks about the basic rules of behavior in the postpartum period.
The postpartum period is divided into two parts: the early postpartum period (lasts about two hours from the moment the baby is born) and the late postpartum period (up to 8 weeks after birth).
In the early postpartum period, women in childbirth are in the delivery room, the baby is laid out on the mother's stomach, he is first applied to the breast. The condition of the woman is being closely monitored.
The condition of the woman is being closely monitored.
Two hours later, the mother and child are transferred to the postpartum department, the late postpartum period begins, during which the woman's body is restored. What does it mean?
Restoration of physiological functions. Approximately four hours after delivery, the patient is asked to empty her bladder. Difficulties can arise with this, which can be overcome by trying to relax while sitting on the toilet. You can open the water, its murmur helps to empty the bladder. If this does not work, the doctor, having assessed the fullness of the bladder, may suggest the use of a catheter.
On the second day you need to empty the intestines. There can also be difficulties with this, since the intestines are compressed during childbirth, and after childbirth it changes its location in the abdominal cavity. But it is very important to start the work of the intestines in the first few days after childbirth.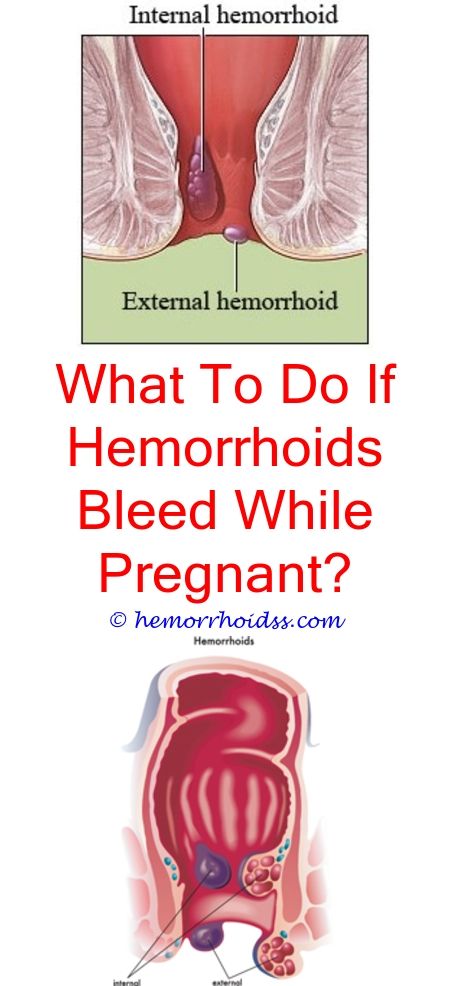 For this purpose, the correct diet is drawn up (foods high in pectins - apples, bananas, etc.). If the rhythmic work of the intestines is not restored, the doctor recommends resorting to microclysters. These are small tubes of medicine that are injected into the rectum and cause a bowel movement.
For this purpose, the correct diet is drawn up (foods high in pectins - apples, bananas, etc.). If the rhythmic work of the intestines is not restored, the doctor recommends resorting to microclysters. These are small tubes of medicine that are injected into the rectum and cause a bowel movement.
Lactation. Milk usually arrives on the third day. In ISIDA, already on the first day after childbirth, a breastfeeding specialist comes to the patients and tells in great detail and in a popular way how to apply the baby to the breast. Proper attachment to the breast is 90% of the success of breastfeeding.
Nutrition during breastfeeding. Nutrition after childbirth should be varied and balanced. The diet of a nursing woman should include meat, fish, vegetables, fruits, cereals, dairy products. During the first 10 days, it is necessary to start the rhythmic work of the mother's intestines, so the basis of the diet should be foods high in pectin. On the table of a nursing woman should be baked apples, bananas, cereals, vegetable soups, dried fruit soups, birch sap.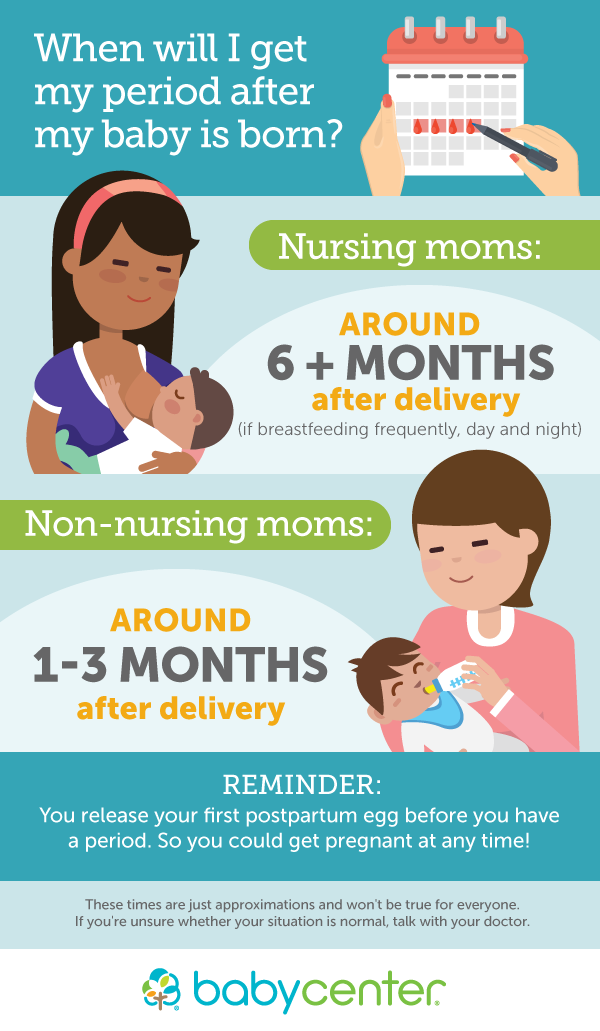
New products should be introduced carefully. You can eat stewed vegetables - broccoli, cauliflower, carrots, beets, onions, zucchini, pumpkin. For snacks, you can use prunes, dried apricots, biscuit cookies, bagels, croutons without raisins. Butter - no more than 15 g per day, chicken, pork are not recommended. Eat rabbit, turkey. 10 days after birth, fermented milk products, boiled fish, black bread, boiled or baked potatoes, pasta from durum wheat are introduced. A little later, you can introduce hard cheese, but its fat content should not exceed 45%.
During breastfeeding, you should not eat raisins, mayonnaise, semi-finished products, sausages, sausages, smoked meats, fast food is unacceptable, alcohol is strictly prohibited. Also exclude sweet carbonated drinks, everything fatty and fried, strong broth is unacceptable. It is also not recommended to eat raw tomatoes, white cabbage - this can cause bloating in both you and the baby. If you can’t wake up without coffee, allow yourself one (maximum two) cups of a weak drink with milk.
It is necessary to monitor the condition of the baby's skin, it is advisable to keep a food diary.
Drinking regimen during breastfeeding. Do not force yourself to drink through force. The amount of milk does not depend on the amount of liquid drunk, lactation is a hormone-dependent process. Drink as thirst arises, excess fluid is an extra burden on the kidneys and nothing more.
"Care" of the abdomen. Women giving birth for the first time usually cherish the dream that the belly will disappear once after childbirth. Unfortunately, they are disappointed. The abdomen cannot immediately decrease, because immediately after childbirth, the uterus weighs 800-1000 g. But already seven days after childbirth, the uterus weighs 400-500 g. And every day until the 12th day after childbirth, the height of the fundus of the uterus decreases by 2 cm. In the future, it decreases less intensively, but by about 6-8 weeks after birth, the uterus has its prenatal weight, which is 50-60 g. It should be noted that the active contraction of the uterus stimulates the frequent attachment of the baby to the breast.
It should be noted that the active contraction of the uterus stimulates the frequent attachment of the baby to the breast.
Postpartum discharge - lochia. Frequent application of the child to the breast also contributes to the expulsion of the postpartum secret from the uterus - lochia. A few days after childbirth, the discharge is abundant, often with clots, and may have a specific smell. By day 5-6, their number decreases, and the appearance also changes: a mucous component is added. After a few more days, the blood in the discharge becomes even less, the discharge becomes brownish, then yellowish, and finally - mucous. As a rule, by 6-8 weeks after birth, lochia disappear.
An important point: if within two weeks the discharge is abundant, but suddenly decreases or disappears sharply, you should consult a doctor. This is a very dangerous symptom!
Episiotomy . An episiotomy is a surgical incision in the perineum along the back wall of the vagina in order to prevent deep vaginal tears and also protect the baby from traumatic brain injury.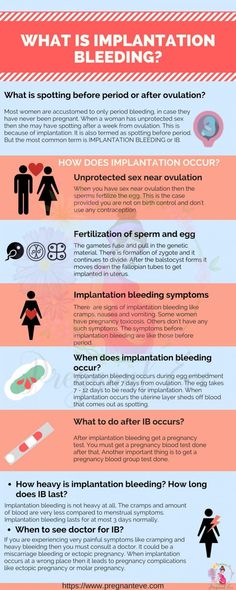 This manipulation is usually resorted to in rapid labor, childbirth with a large fetus, labor with pelvic diligence, or preterm labor.
This manipulation is usually resorted to in rapid labor, childbirth with a large fetus, labor with pelvic diligence, or preterm labor.
After the episiotomy, the sutures are sutured with a synthetic thread, which is completely absorbed after one and a half to two months. The seam must be kept clean and dry, treated with an antiseptic (ordinary brilliant green). Sometimes in the area of the seam, and then the scar, there is a violation of sensitivity. This is normal and will pass in 6-9 months.
Delivery by caesarean section. On the first day after the caesarean section, the woman is in intensive care, on the second day she is transferred to the postpartum department. Seam care is normal, that is, brilliant green and air baths. To reduce the load, after a caesarean section, wearing a bandage is recommended. It is strictly forbidden to strain the press, physical education and sports are permissible no earlier than 6 months after childbirth. And it should be moderate physical activity - dancing, Pilates, yoga. Strength training equipment, tennis, active running are not recommended.
Strength training equipment, tennis, active running are not recommended.
The next pregnancy after delivery by caesarean section is recommended no earlier than two years later. In this case, it is necessary to look at the scar on the uterus, if there is a niche there. These niches can be the cause of an inconsistent scar on the uterus - an indication for the next delivery by caesarean section.
Sex after childbirth. The uterus recovers within 6-8 weeks after childbirth, the vaginal mucosa is about the same. Therefore, you should not start an intimate life earlier than 6-8 weeks after childbirth. It is important to note that women often experience a decrease in libido, sometimes vaginal dryness. This is how the hormone estrogen works. His influence will soon decline. To eliminate dryness, you can use candles with hyaluronic acid, lubricants. It improves the quality of sexual life.
A “stretched” vagina after childbirth is another unpleasant moment from the point of view of sexual sensations. Wumbling helps to cope with this (in particular, Kegel exercises, vaginal cones). These classes can begin approximately 2 months after childbirth.
Wumbling helps to cope with this (in particular, Kegel exercises, vaginal cones). These classes can begin approximately 2 months after childbirth.
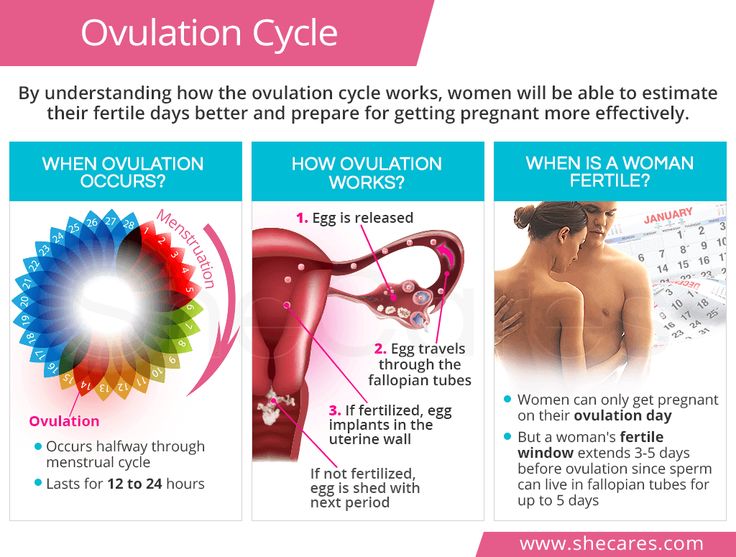
Postpartum contraception is a must! There is a stereotype that if a woman is breastfeeding, then she cannot become pregnant. This is not true. Contraceptives after childbirth are necessary, even if menstruation has not yet recovered.
The easiest method of contraception is condoms. The intrauterine device is very effective. If a woman has not yet menstruated, putting a spiral is more difficult, but possible.
The next method of contraception is hormonal contraceptives, the so-called mini-pills. These are tablets with one hormone that acts at the level of the uterus and does not affect milk in any way. These pills are designed specifically for nursing mothers.
The next method is the use of spermicides - suppositories that are inserted into the vagina. They work well if done right.
The last method is sterilization. In women, this can occur during a caesarean section, with her consent. Sometimes men agree to sterilization.
In women, this can occur during a caesarean section, with her consent. Sometimes men agree to sterilization.
Especially for those who want to know as much as possible about partner births, we have created a selection of materials on this topic. In the Partner Birth Toolkit , you'll find active links to video interviews with doctors, to flyer presentations with the most important logically structured information, and even an interesting celebrity birth interview.
For those who want to know as much as possible about childbirth, we have created a selection of materials on this topic. The Childbirth Resource Kit will answer most of your questions.
You can find out about the conditions of comprehensive pregnancy monitoring programs at the ISIDA clinic on our page Pregnancy management programs.
Are you looking for a clinic whose specialists you can trust with the birth of your baby? Trust the specialists of the ISIDA clinic: sign up for a consultation by calling 0800 60 80 80, +38 (044) 455 88 11.