Do you get checked for stds when pregnant
STD Facts - STDs & Pregnancy
If you are pregnant, you can become infected with the same sexually transmitted diseases (STDs) as women who are not pregnant. Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.
I’m pregnant. Can I get an STD?
Yes, you can. Women who are pregnant can become infected with the same STDs as women who are not pregnant. Pregnancy does not provide women or their babies any additional protection against STDs. Many STDs are ‘silent,’ or have no symptoms, so you may not know if you are infected. If you are pregnant, you should be tested for STDs, including HIV (the virus that causes AIDS), as a part of your medical care during pregnancy. The results of an STD can be more serious, even life-threatening, for you and your baby if you become infected while pregnant. It is important that you are aware of the harmful effects of STDs and how to protect yourself and your unborn baby against infection. If you are diagnosed with an STD while pregnant, your sex partner(s) should also be tested and treated.
How can STDs affect me and my unborn baby?
STDs can complicate your pregnancy and may have serious effects on both you and your developing baby. Some of these problems may be seen at birth; others may not be discovered until months or years later. In addition, it is well known that infection with an STD can make it easier for a person to get infected with HIV. Most of these problems can be prevented if you receive regular medical care during pregnancy. This includes tests for STDs starting early in pregnancy and repeated close to delivery, as needed.
Should I be tested for STDs during my pregnancy?
Yes. Testing and treating pregnant women for STDs is a vital way to prevent serious health complications to both mother and baby that may otherwise happen with infection. The sooner you begin receiving medical care during pregnancy, the better the health outcomes will be for you and your unborn baby. The Centers for Disease Control and Prevention’s 2015 STD Treatment Guidelines recommend screening pregnant women for STDs. The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
The Centers for Disease Control and Prevention’s 2015 STD Treatment Guidelines recommend screening pregnant women for STDs. The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
Be sure to ask your doctor about getting tested for STDs. It is also important that you have an open, honest conversation with your provider and discuss any symptoms you are experiencing and any high-risk sexual behavior that you engage in, since some doctors do not routinely perform these tests. Even if you have been tested in the past, you should be tested again when you become pregnant.
Can I get treated for an STD while I’m pregnant?
It depends. STDs, such as chlamydia, gonorrhea, syphilis, trichomoniasis and BV can all be treated and cured with antibiotics that are safe to take during pregnancy. STDs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured.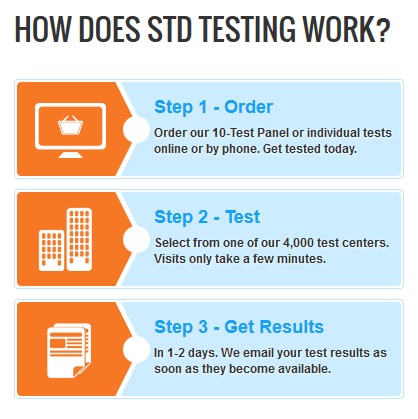 However, in some cases these infections can be treated with antiviral medications or other preventive measures to reduce the risk of passing the infection to your baby. If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
However, in some cases these infections can be treated with antiviral medications or other preventive measures to reduce the risk of passing the infection to your baby. If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
How can I reduce my risk of getting an STD while pregnant?
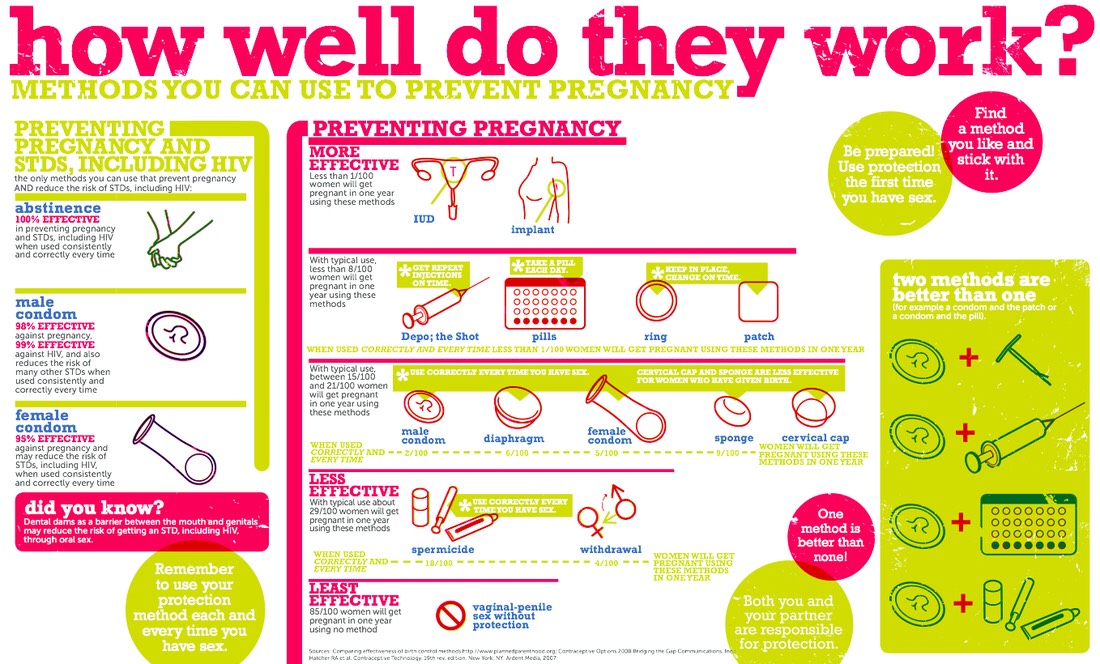
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
You can add this content to your website by syndicating.
STDs during Pregnancy - CDC Detailed Fact Sheet
Detailed fact sheets are intended for physicians and individuals with specific questions about sexually transmitted diseases. Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
5 Tests You Need When You're Pregnant
Dr. Giles talking to an obstetrics patient about tests needed during pregnancyCongratulations! You’re pregnant! It’s exciting and nerve-wracking all at the same time. What can you do to ensure your pregnancy is a healthy one? How will your obstetrician make sure your pregnancy is proceeding normally? There are all kinds of tests we do for exactly those reasons. These include physical exams, blood tests, and ultrasounds – many of which are done at your first visit with your obstetrician, while others are done throughout your pregnancy. Let’s talk about the most common tests you’ll encounter along the way.
1. Pap Smear and STD Testing
Your first visit to your obstetrician, usually around 8-10 weeks into your pregnancy, includes screening for cervical cancer and STDs (sexually trasmitted diseases) to determine any risk to your baby. Screening for sexually transmitted infections is required by the Commonwealth of Virginia at the onset of prenatal care. If you are due for a Pap smear (cervical cancer screening), you’ll also receive this test at your first visit.
Screening for sexually transmitted infections is required by the Commonwealth of Virginia at the onset of prenatal care. If you are due for a Pap smear (cervical cancer screening), you’ll also receive this test at your first visit.
The Pap smear and STD testing require a pelvic exam just like you’d normally have at your annual visit to the gynecologist. STD testing also requires a blood test for hepatitis, syphilis, and HIV. It is important to note that Virginia is an opt-out state when it comes to HIV testing. This means that your physician is required to let you know that HIV testing is recommended for pregnant women and included in the blood work, unless you decide you don’t want to be tested for it. Your doctor will discuss the results of these tests and any implications for you and your baby.
2. Additional Blood Work
The blood work done at your first visit will also determine your blood type and your immunity to rubella (a virus that causes flu-like symptoms and is dangerous for a developing fetus). Depending on your obstetrical history and any medical conditions, your obstetrician may order other blood tests, including thyroid function tests, early gestational diabetes testing, or liver and kidney function tests if you have high blood pressure or did in a previous pregnancy.
Depending on your obstetrical history and any medical conditions, your obstetrician may order other blood tests, including thyroid function tests, early gestational diabetes testing, or liver and kidney function tests if you have high blood pressure or did in a previous pregnancy.
Your doctor will discuss these tests with you during your first visit. All the blood testing will be done at the same time in order to minimize the number of needle sticks.
3. Ultrasounds
Ultrasounds are much more than gender reveals or cute pictures of your unborn baby. They allow your doctor to observe the development of your baby at multiple stages of your pregnancy.
Your first ultrasound is typically conducted at your first visit to your obstetrician. This ultrasound will help your doctor determine your due date, which gives them a better idea of when you’ll reach certain milestones throughout your pregnancy. It might also be the first time you get to hear your baby’s heartbeat, which is truly thrilling.
A second ultrasound can be done at 12-13 weeks, depending on what you and your obsetrician have decided regarding genetic testing.
At 20 weeks, you’ll have a detailed anatomy ultrasound where the baby is carefully examined and measured. Your doctor will look for anatomic abnormalities. You will also be able to find out the sex of your baby during this ultrasound (if you want to know!). If your pregnancy is uncomplicated, this is the last ultrasound you’ll need.
During visits around 24 weeks, your obstetrician will measure your abdomen at each visit to estimate if your baby is growing appropriately. If it appears that the baby is too big or too small based on these measurements, an ultrasound is usually ordered to get a more accurate estimate of the baby’s growth. If you are diagnosed with or have any medical issues, you may need more frequent ultrasounds.
At 36 weeks (almost there!), your obstetrician will examine your belly and check your cervix. If it is difficult to tell if the baby is in the head-down position, an ultrasound will be ordered to determine the baby’s position.
A highly trained ultrasonographer will apply a gel to your skin, then move a transducer around your abdomen to send high frequency sound waves into your uterus that will translate into images on the screen. You may feel pressure, but likely not pain. Don’t empty your bladder before the scan in case having a full bladder will enhance their ability to obtain the images needed. Occasionally during pregnancy, the ultrasound will need to be performed with a transvaginal probe. This probe is not painful. Cell phone use is generally not allowed during ultrasound exams, but you will be provided with a picture of your baby. Your doctor will discuss the results of the scan with you.
4. Genetic Testing
At your first prenatal care visit, your doctor will discuss genetic testing options meant to determine if your baby is at increased risk for a variety of disorders. These disorders include, but are not limited to, cystic fibrosis, certain types of birth defects, and chromosomal disorders such as Down syndrome.
This testing is usually conducted using a combination of ultrasound results and blood tests performed at specific times during your pregnancy. Your doctor will discuss the results with you. If there are abnormal results, you will have the option of meeting with a perinatologist (high risk specialist) to discuss the results, their implications, and any further testing that might be recommended. Our office will help arrange that appointment for you should it be necessary.
5. Glucola Test
You might be wondering, When do I have to drink that sugar drink? The glucola test is routinely given around 28 weeks for all pregnancies. It tests your glucose tolerance to determine if you have gestational diabetes (high blood sugar that develops as a result of hormones produced by the placenta). If you are overweight (BMI is greater than 30) or have other risk factors for developing gestational diabetes, the test is also given earlier in pregnancy, usually at the first or second visit.
There is no need to fast before the glucola test. You will drink a sugary drink and wait for an hour in the waiting room without having anything to eat or drink during the wait time. Then, your blood will be drawn for the test and you might be finished.
Three-hour glucola test – if necessaryIf the results of your hour-long glucola test are abnormally high, you will be scheduled for a 3-hour test where you will drink a larger quantity of the sugary drink. This time, your blood will be tested before you drink the drink and at hourly intervals afterwards. If you need to have the 3-hour sugar test, you will be asked not to eat or drink for 8 hours prior to the test. If the result of the 3-hour test is also abnormal, you will most likely be referred to an endocrinologist and a high-risk pregnancy specialist for management of gestational diabetes.
Testing Needs Vary
While the tests listed above are the most common, we have only scratched the surface of the types of testing done during pregnancy. Each pregnancy is individual, and testing will vary from mom to mom. You and your obstetrician are a team, and together you will determine the most appropriate tests to perform to ensure a happy, healthy pregnancy.
Each pregnancy is individual, and testing will vary from mom to mom. You and your obstetrician are a team, and together you will determine the most appropriate tests to perform to ensure a happy, healthy pregnancy.
To schedule an appointment with a VPFW provider, you can call us at 804-897-2100 or set an appointment online.
STIs and pregnancy - KVD №2
- home
- Articles
- STIs and pregnancy
The presence of an STI in a pregnant woman can cause serious harm to the fetus. Untreated infections can lead to miscarriage, premature birth, stillbirth, underweight babies, blindness, hearing loss, chronic respiratory disease, mental retardation, and other serious developmental problems. Untreated syphilis can lead to the birth of a child with congenital syphilis. Activation of STIs during pregnancy is manifested by symptoms of intrauterine infection, leading to miscarriage and intrauterine lesions of the fetus up to its death. Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis.
Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis.
Untreated gonococcal infection often results in ectopic pregnancy or pelvic inflammatory disease. Chronic gonorrhea may worsen immediately after childbirth. At the same time, the risk of gonococcal sepsis is high. Women who become infected in the last 20 weeks of pregnancy or after childbirth are at high risk of gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth.
Infection of the fetus with gonorrhea occurs in utero or during childbirth. Intrauterine infection is manifested by gonococcal sepsis in the newborn and chorioamnionitis. Infection during childbirth can lead to gonococcal conjunctivitis, otitis externa, and vulvovaginitis. The most common complication in children born to gonorrhea mothers is a highly contagious eye disease (newborn ophthalmia) which, if left untreated, can lead to blindness. Rare complications in children born to gonorrhea mothers are childhood meningitis and arthritis.
The most common complication in children born to gonorrhea mothers is a highly contagious eye disease (newborn ophthalmia) which, if left untreated, can lead to blindness. Rare complications in children born to gonorrhea mothers are childhood meningitis and arthritis.
Most doctors test women for gonorrhea at their first pregnancy visit, and many do another test in the third trimester. If your doctor has not given you the results of the tests, ask him what disease you were tested for.
Trichomoniasis, according to most doctors, does not belong to those diseases that can have a fatal effect on the fetus, but, of course, trichomoniasis during pregnancy is an extremely undesirable condition.
Trichomoniasis in a pregnant woman increases the risk of preterm labor and premature rupture of amniotic fluid.
Chlamydial infection in 80% of pregnant women is latent. The frequency of occurrence of urogenital chlamydia among pregnant women, according to various sources, is 6. 0 - 8.0%. The most common consequences of untreated genital chlamydia during pregnancy are:
0 - 8.0%. The most common consequences of untreated genital chlamydia during pregnancy are:
- missed pregnancy,
- spontaneous miscarriages,
- premature or delayed birth,
- untimely outpouring of waters,
- blood loss more than 300 ml,
- puerperal fever,
- endometritis,
- intrauterine infection of the fetus.
Transmission of the pathogen to the child is possible both in the presence and in the absence of obvious clinical manifestations of infection in the mother (the probability of its transmission is 50-70%). The fetus is infected both by direct contact with the mother's birth canal, and in utero: by ingestion or aspiration of amniotic fluid.
Conjunctivitis (inflammation of the mucous membrane of the eyes) is the most common manifestation of congenital chlamydial infection in infants, pneumonia develops in 10% of infected newborns, and otitis media is somewhat less common. In some children born to infected mothers, these microbes are isolated from the oropharynx, nasopharynx, and rectum. The total percentage of newborns infected with chlamydia reaches 9.eight%.
The total percentage of newborns infected with chlamydia reaches 9.eight%.
Finally, what do you need to know about the impact of STIs on pregnancy, childbearing and breastfeeding?
A pregnant woman can pass on most STIs during pregnancy or childbirth to her children, and some diseases can be passed through breast milk (eg HIV). However, the chance of transmission can be drastically reduced if treatment is started on time.
Once you decide to become pregnant, visit your doctor and make sure that neither you nor your partner have an STI. If you are infected, take a course of treatment and get tested again before pregnancy.
If you are already pregnant, you will need a complete examination. At any time during your pregnancy, be sure to tell your doctor if you notice any symptoms of an STI or suspect you may have contracted it.
Pregnancy screening for STIs
If you are planning a pregnancy, you should know that you need to be screened for sexually transmitted infections before pregnancy. How to correctly pass all the tests, what kind of treatment is needed if the infection is still detected?
How to correctly pass all the tests, what kind of treatment is needed if the infection is still detected?
This article will cover only those infections that are often the subject of controversy - how best to detect them, whether they always need to be treated, what treatment is better to prescribe to a woman. Very often, patients engage in self-deception, completely trusting the results of a single analysis. Five infections will be consecrated - chlamydia, mycoplasma, urepaplasma, herpes, cytomegalovirus.
If you have been diagnosed with chlamydial infection
Chlamydial infection is a sexually transmitted disease during unprotected intercourse. Chlamydia bacteria can be the cause of chlamydia. The likelihood that you will become infected with them in the household way - after sitting on the toilet, swimming in the pool - is very low, since chlamydia quickly die outside the human body.
Symptoms of chlamydial infection
The incubation period is 7 to 30 days. In a woman: white, yellow, clear discharge from the vagina, pain during urination, during sexual intercourse, pain in the lower abdomen, in the lumbar region. In a man: discharge from the urethra - transparent, scanty, pain during urination and coitus.
In a woman: white, yellow, clear discharge from the vagina, pain during urination, during sexual intercourse, pain in the lower abdomen, in the lumbar region. In a man: discharge from the urethra - transparent, scanty, pain during urination and coitus.
Chlamydia is often asymptomatic and can be detected by testing. A chlamydial infection can be a complication. For women, it is fraught with inflammatory diseases of the uterus and appendages, which can lead to infertility. For men, it is fraught with inflammation of the epididymis - epididymitis. In order to identify this infection, you need to pass an analysis for chlamydia using the PCR method - DNA diagnostics. If the doctor detects chlamydia, he will prescribe a course of treatment that must be completed by both partners.
Treatment for chlamydial infection: a 21 day course of antibiotics is prescribed. If chlamydia is detected during pregnancy, then the woman is also prescribed antibiotics that are allowed during pregnancy - a course of 2 weeks, but this can only be done after the 20th week of pregnancy.
Why chlamydial infection is dangerous during pregnancy
Chlamydia increases the risk of miscarriage. If the fetus becomes infected, this will lead to chlamydial pneumonia in the newborn, to the fact that he will develop inflammatory eye diseases. Treatment of chlamydial infection during pregnancy is a must!
If ureaplasma, mycoplasma infection is detected
Ureaplasmas are bacteria that live in the human body, on the mucous membranes of the genital organs, urinary tract. These microorganisms can be classified as conditionally pathogenic, which means that every person has them. If the number of bacteria increases sharply, then it begins to exceed the permissible limits, a person develops painful symptoms. This happens when the immune system is weakened.
Mycoplasmosis and ureaplasmosis are sexually transmitted. Also, another way of transmission is from a child to a mother, while a person may grow up to a certain point without even suspecting that this disease is the cause of a weakened immune system. Symptoms of ureplasmosis: inflammatory diseases of the uterus and appendages, cystitis, pyelonephritis, kidney stones, bacterial vaginosis. In men, these bacteria most often multiply rapidly with urethritis, pyelonephritis, kidney stones.
Symptoms of ureplasmosis: inflammatory diseases of the uterus and appendages, cystitis, pyelonephritis, kidney stones, bacterial vaginosis. In men, these bacteria most often multiply rapidly with urethritis, pyelonephritis, kidney stones.
Diagnosis of mycoplasma and ureplasma infection
In order to identify myco-, ureplasma infection, it is necessary to take tests using PCR or culture culture.
The culture method shows a more objective picture - the number of bacteria. PCR provides information that these microorganisms are in the genitourinary tract, but does not establish their number. If a woman is found to have mycoplasmas or ureaplasmas in the amount of 10x2 degrees, then treatment is not needed, but if in the amount of 10x4 degrees, then treatment is necessary. Culture can also determine which antibiotic is needed to make treatment more effective. When detecting ureaplasmas and mycoplasmas in a blood test, there are often false positive results.
Treatment of myco-. Ureplasma infections are usually carried out when a woman has health problems - inflammation of the uterus, appendages, cystitis, pyelonephritis. If women do not experience pain, then these infections do not need to be treated. Unmotivated use of antibiotics will only lead to a violation of the microflora of the vagina.
Ureplasma infections are usually carried out when a woman has health problems - inflammation of the uterus, appendages, cystitis, pyelonephritis. If women do not experience pain, then these infections do not need to be treated. Unmotivated use of antibiotics will only lead to a violation of the microflora of the vagina.
If we are talking about planning a pregnancy, then it is necessary to treat it, even if the woman does not have symptoms of the disease. Treatment consists in taking antibiotics - a course of 10 days. In order to start taking, you need to do a seeding for sensitivity to antibiotics in order to determine the choice of the desired drug. Both spouses must complete the course.
If mycoplasma or ureaplasma is detected during pregnancy, then the woman is also prescribed treatment.
What is dangerous ureaplasma and mycoplasma
Ureaplasma and mycoplasma can lead to abortion or premature birth, intrauterine infection of the child. Also, children can develop pathologies of the urinary tract, cystitis, pyelitis.
Also, children can develop pathologies of the urinary tract, cystitis, pyelitis.
If you have found genital herpes
The herpes simplex virus is dangerous for your unborn baby. The genital child is sexually transmitted, may be passed on by the mother to the child. A person lives and does not know that an infection lives in him, and when immunity is weakened, herpes suddenly manifests itself.
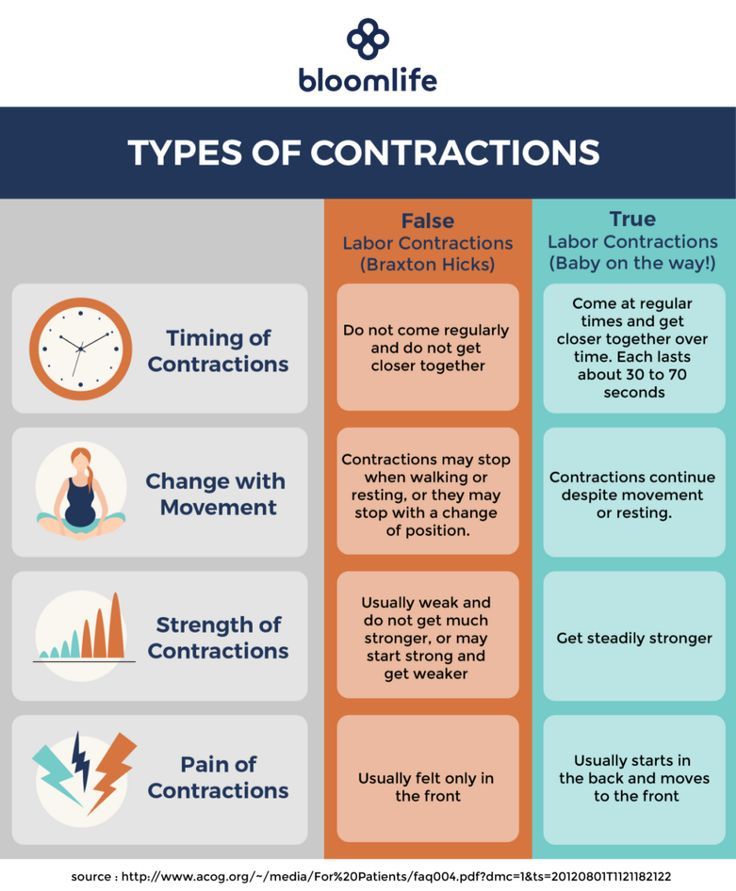
Symptoms of genital herpes - infection with herpes causes pain, burning, swelling in the genital area. These symptoms are accompanied by general malaise, fever, headache. Small bubbles appear on the genitals, which are filled with liquid. The blisters burst and painful red sores form. Heal within two weeks.
If there is a relapse of the disease, then it is accompanied by a rise in temperature, hypothermia, stress can lead to relapses. Genital herpes is asymptomatic, it is possible for a husband to be infected by his wife, or vice versa.
Diagnosis of genital herpes : if you are planning a pregnancy, you need to take a blood test from a vein for IgM and IgG antibodies to herpes simplex viruses.
If, according to the results of the analysis, class G antibodies are detected, the organism has already encountered genital herpes. If antibodies to class M immunoglobulins are present, genital herpes is in an acute stage.
Treatment of genital herpes : treated with antiviral drugs, partner should also be tested - he may not be infected. During pregnancy, antiviral drugs should not be taken, but it is necessary to undergo immunoglobulin therapy.
Why is genital herpes dangerous during pregnancy
Primary herpes infection during pregnancy is the most dangerous. It leads to termination of pregnancy, as well as to serious damage to the fetus. If a pregnant woman becomes infected with this virus shortly before the expected birth of a child, then the doctor refuses to give birth naturally, the woman is given a caesarean section. In natural childbirth, the risk of infection of the child when passing through the mother's birth canal is high. If the disease is in the acute phase, then the child is highly likely to become infected, so you need to treat it in a timely manner.
If the disease is in the acute phase, then the child is highly likely to become infected, so you need to treat it in a timely manner.
If cytomegalovirus is detected
Cytomegalovirus is sexually transmitted, it can also be transmitted from mother to fetus, it is possible to transmit the virus through kissing, through blood.
Cytomegalovirus is asymptomatic, after a month or two a mononucleosis-like syndrome. It is similar to ARVI and flu, accompanied by high fever, chills, a person gets very tired, feels unwell, and has a headache.
If the immune system is weakened, then cytomegalovirus can cause serious diseases - damage to the eyes, lungs, digestive system and brain.
Diagnosis of cytomegalovirus : it can be detected by the results of a blood test from a vein for antibodies of the IgM and IgG classes to cytomegalovirus. If antibodies to class M immunoglobulins are fixed, then the disease is in the acute stage, if antibodies to class G immunoglobulins are detected, then the body has already met with this infection.
Treatment of cytomegalovirus : a woman is prescribed immune preparations, during pregnancy immunotherapy is carried out using approved drugs.
Why cytomegalovirus is dangerous during pregnancy: primary infection with cytomegalovirus during pregnancy is dangerous, it can lead to infection of the fetus, abortion, and fetal malformations. Treatment of cytomegalovirus before pregnancy and during pregnancy is mandatory.
How to get tested for sexually transmitted diseases
Do this before your period, right after it. On such days, the woman's immunity is reduced. 20 days before the test, you need to stop taking antibiotics, stop putting candles, etc. Before visiting the doctor, you do not need to wash yourself, take a shower.
When are tests taken?
First time before pregnancy. If an infection is found, then you need to undergo treatment, then re-take tests. Until the control of cure is carried out, sexual life should be carried out with condoms.