How to know if my child has bronchitis
Bronchitis (for Parents) - Nemours KidsHealth
What Is Bronchitis?
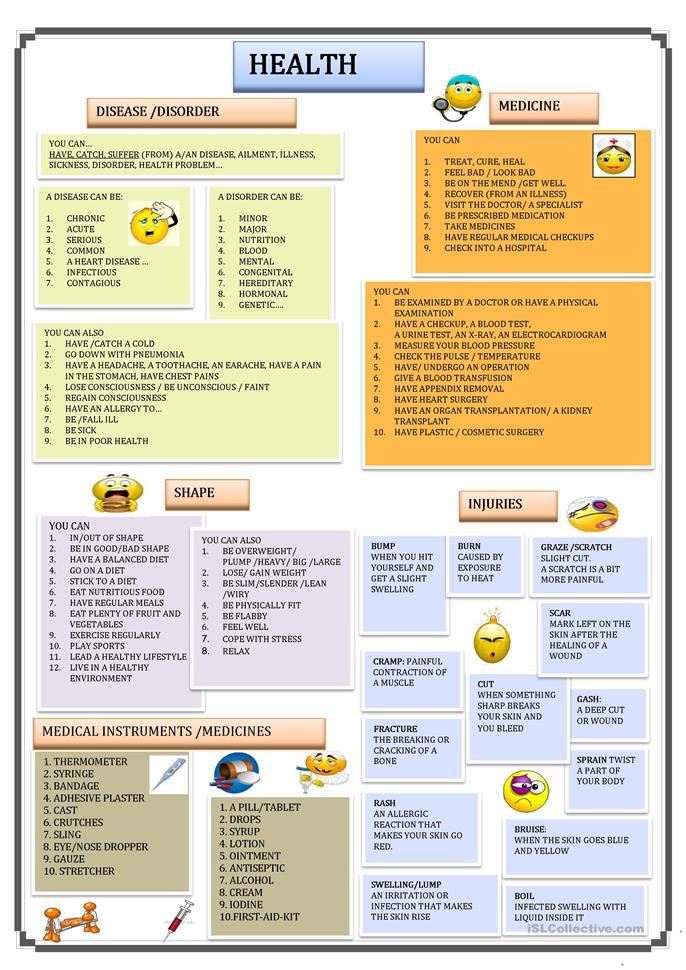
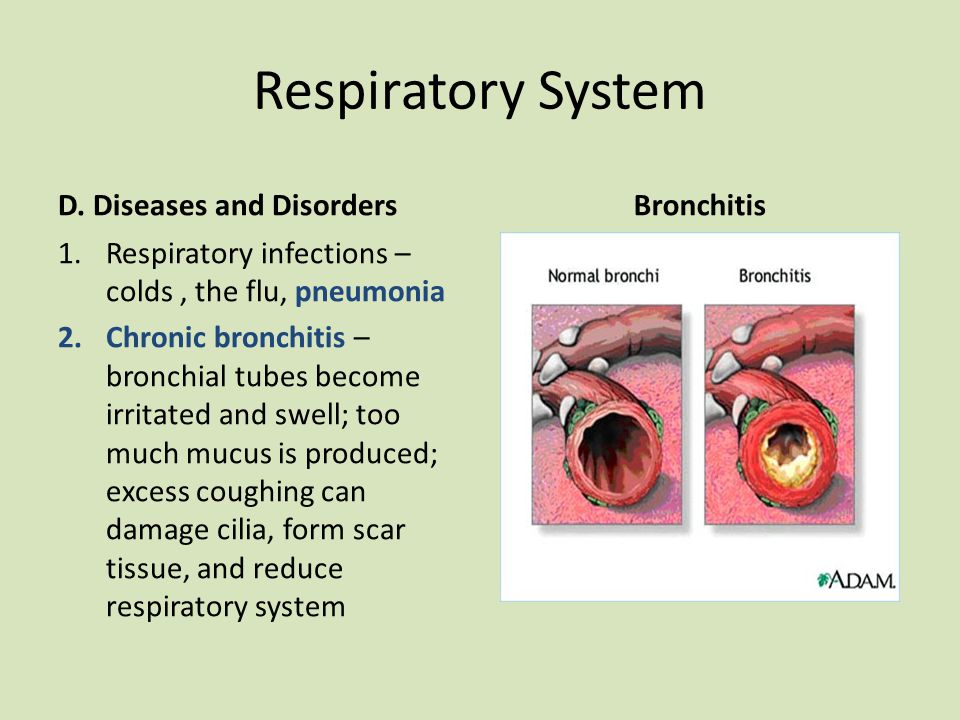
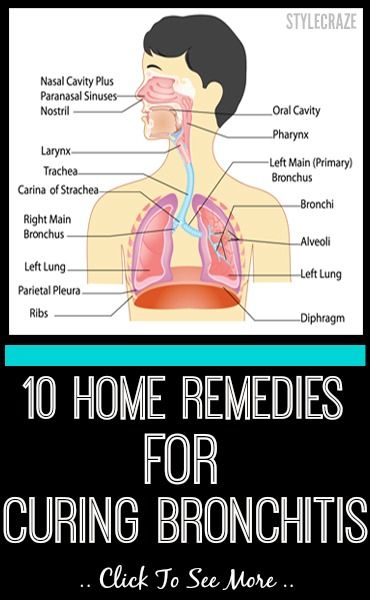
Bronchitis is when the lining of the large breathing tubes get inflamed (swollen and red). These airways, called the bronchial tubes, connect the windpipe to the lungs. Their delicate lining makes mucus, and covers and protects the organs and tissues involved in breathing.
Bronchitis (brong-KYE-tis) can:
- Make it hard for air to pass in and out of the lungs.
- Irritate the tissues of the bronchial tube lining. Then, they make too much mucus.
The most common symptom of bronchitis is a lasting cough.
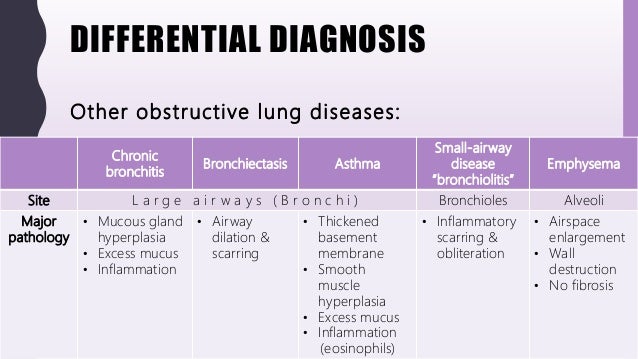
What Are the Types of Bronchitis?
Bronchitis can be acute or chronic:
Acute bronchitis comes on quickly and can cause severe symptoms. But it lasts no more than a few weeks. Viruses cause most cases of bronchitis. Many different viruses can infect the respiratory tract and attack the bronchial tubes. Infection by some bacteria can also cause acute bronchitis. Most people have acute bronchitis at some point in their lives.
Chronic bronchitis is rare in children. It can be mild to severe and lasts longer (from several months to years). The most common cause of chronic bronchitis is smoking. The bronchial tubes stay inflamed and irritated, and make lots of mucus over time. People who have chronic bronchitis have a higher risk of bacterial infections of the airway and lungs, like pneumonia.
What Are the Signs & Symptoms of Bronchitis?
Acute bronchitis often starts with a dry, annoying cough triggered by the
inflammationof the lining of the bronchial tubes.
Other symptoms may include:
- coughing that brings up thick white, yellow, or greenish mucus
- feeling short of breath
- soreness or a feeling of tightness in the chest
- wheezing (a whistling or hissing sound with breathing)
- headache
- generally feeling ill
- fever
- chills
For people with chronic bronchitis:
- It can take longer than usual to recover from colds and other common respiratory illnesses.
- Wheezing, feeling short of breath, and coughing can happen every day.
- Breathing can get harder and harder.
What Causes Bronchitis?
Acute bronchitis is usually caused by a virus. It may happen along with or after a cold or other respiratory infection. Viruses can spread:
- when someone with bronchitis coughs and sends infected droplets into the air
- when someone touches their mouth, eyes, or nose after contact with respiratory fluids from an infected person
Things that put people at risk for chronic bronchitis include:
- smoking, even for a short time
- being around tobacco smoke
- exposure to chemical fumes and other air pollutants for long periods
How Is Bronchitis Diagnosed?
When doctors suspect bronchitis, they will do an exam and listen to a child's chest with a stethoscope to check for wheezing and congestion.
No tests are needed to diagnose bronchitis. But the doctor may order a chest X-ray to rule out a condition like pneumonia. Sometimes doctors do a breathing test (called spirometry) to check for asthma. Some kids who seem to get bronchitis a lot — with coughing, wheezing, and shortness of breath — may have asthma instead.
But the doctor may order a chest X-ray to rule out a condition like pneumonia. Sometimes doctors do a breathing test (called spirometry) to check for asthma. Some kids who seem to get bronchitis a lot — with coughing, wheezing, and shortness of breath — may have asthma instead.
How Is Bronchitis Treated?
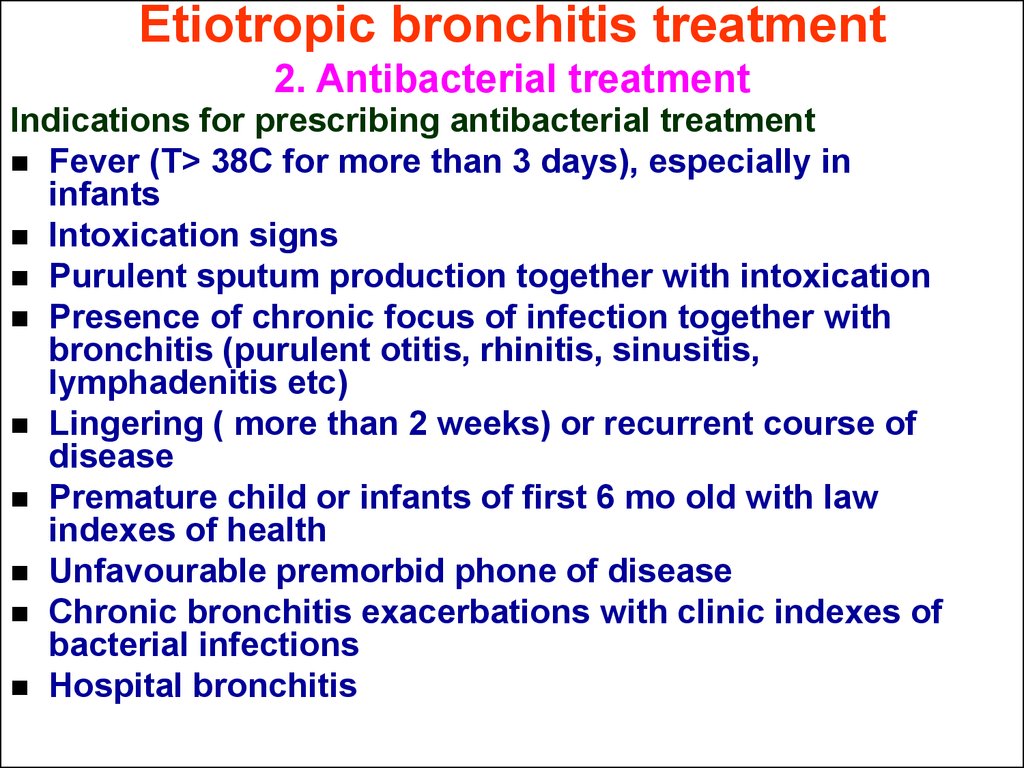
Doctors won't prescribe an antibiotic for bronchitis caused by a virus. Antibiotics work only against bacteria, not viruses.
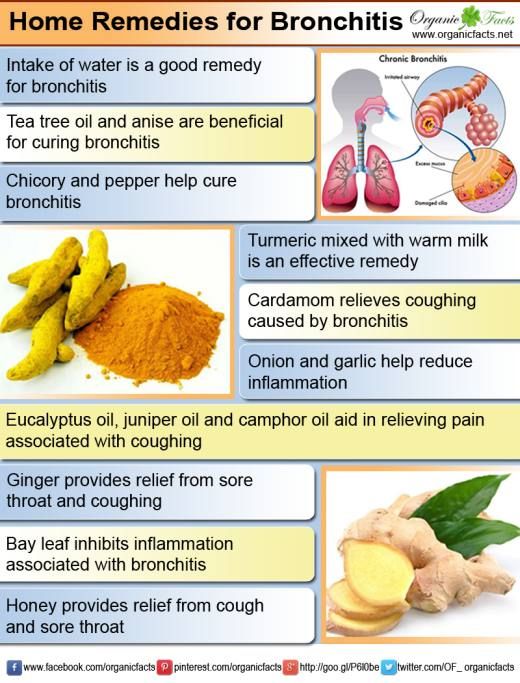
Home care helps most kids with bronchitis feel better. The doctor will recommend that kids and teens:
- drink lots of liquids
- get plenty of rest
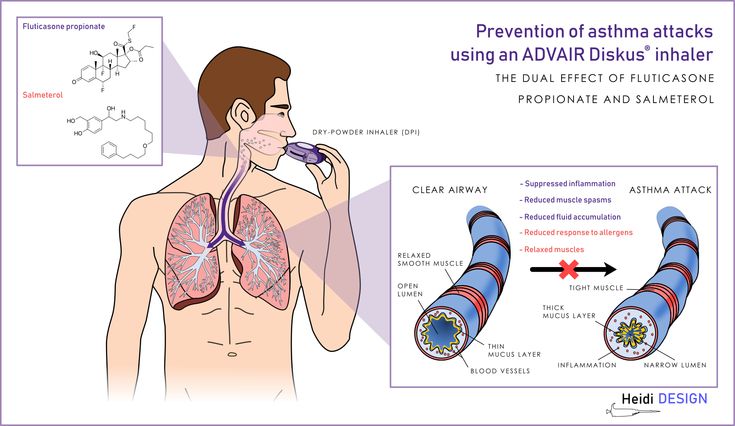
For some older kids or teens, doctors might say it's OK to give an over-the-counter or prescription cough medicine to ease coughing. They also sometimes prescribe a bronchodilator (brong-ko-DY-lay-ter) or other medicines that treat asthma. These help relax and open the bronchial tubes and clear mucus so it's easier to breathe. Kids usually get these medicines through inhalers or nebulizer machines.
A child or teen with chronic bronchitis should avoid being near whatever irritates their bronchial tubes. For people who smoke, that means quitting. Tobacco smoke causes more than 80% of all cases of chronic bronchitis. Smokers also take longer to recover from acute bronchitis and other respiratory infections.
Can Bronchitis Be Prevented?
Washing hands well and often can help prevent the spread of many of the germs that cause bronchitis, especially during cold and flu season.
Encourage anyone in your family who smokes to quit. Protect kids — with or without bronchitis — from secondhand smoke. It can put them at risk for viral infections and increased congestion in their airways.
Reviewed by: Kate M. Cronan, MD
Date reviewed: August 2019
Acute Bronchitis in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is acute bronchitis in children?
Bronchitis is an inflammation of the large breathing tubes (bronchi) in the lungs.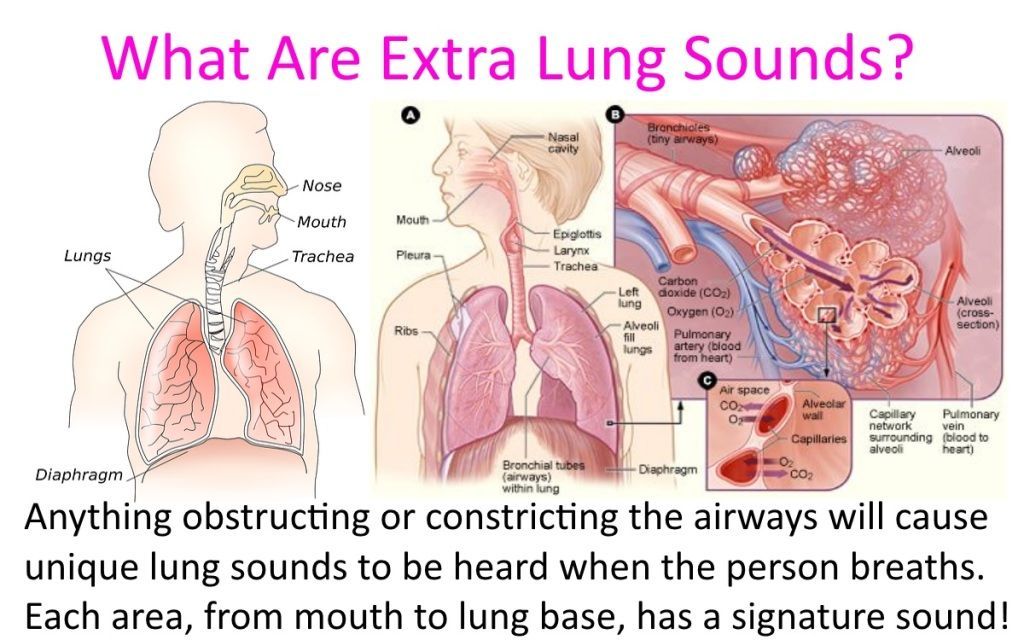 The illness can be short-term (acute) or long-term (chronic). Acute bronchitis means that the symptoms often develop quickly and don’t last long. Most cases are mild.
The illness can be short-term (acute) or long-term (chronic). Acute bronchitis means that the symptoms often develop quickly and don’t last long. Most cases are mild.
What causes acute bronchitis in a child?
Acute bronchitis is most often caused by a viral infection. It may also be caused by bacteria or things such as dust, allergens, strong fumes, or tobacco smoke.
In children, the most common cause of acute bronchitis is a virus. The illness may develop after a cold or other viral infection in the nose, mouth, or throat (upper respiratory tract). Such illnesses can spread easily from direct contact with a person who is sick.
Which children are at risk for acute bronchitis?
Children who have a higher chance of developing acute bronchitis are those who have:
- Chronic sinusitis
- Allergies
- Asthma
- Enlarged tonsils and adenoids
- Exposure to secondhand smoke
What are the symptoms of acute bronchitis in a child?
These are the most common symptoms:
- Dry or mucus-filled cough
- Vomiting or gagging
- Runny nose, often before a cough starts
- Chest congestion or pain
- An overall body discomfort or not feeling well
- Chills
- Slight fever
- Back and muscle pain
- Wheezing
- Sore throat
These symptoms often last 7 to 14 days. But the cough may continue for 3 to 4 weeks. These symptoms may look like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
But the cough may continue for 3 to 4 weeks. These symptoms may look like other health problems. Make sure your child sees his or her healthcare provider for a diagnosis.
How is acute bronchitis diagnosed in a child?
Your child’s healthcare provider can often diagnose acute bronchitis with a health history and physical exam. In some cases, your child may need tests to rule out other health problems, such as pneumonia or asthma. These tests may include:
- Chest X-rays. This test makes images of internal tissues, bones, and organs.
- Pulse oximetry. An oximeter is a small device that measures the amount of oxygen in the blood. For this test, the healthcare provider puts a small sensor (like a clip) on your child's finger or toe. When the device is on, a small red light can be seen in the sensor. The sensor is painless and the red light does not get hot.

- Sputum and nasal discharge samples. These tests can find the germ causing an infection.
How is acute bronchitis treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
In nearly all cases, antibiotics should not be used to treat acute bronchitis. That’s because most of the infections are caused by viruses. Even children who have been coughing for longer than 8 to 10 days often don't need antibiotics.
The goal of treatment is to help ease symptoms. Treatment may include:
- Plenty of rest
- Acetaminophen or ibuprofen for fever and mild pain
- Cough medicine for children over 4 years old
- More fluids
- Cool-mist humidifier in your child’s room
Talk with your child’s healthcare provider before giving over-the-counter cough and cold medicine to your child. The American Academy of Pediatrics does not recommend giving these medicines to children younger than 4 years old because they may cause harmful side effects. For children between ages 4 and 6, only use over-the-counter products when recommended by your child's healthcare provider. In most cases, also don’t give antihistamines. They can dry up the secretions. That can make the cough worse.
The American Academy of Pediatrics does not recommend giving these medicines to children younger than 4 years old because they may cause harmful side effects. For children between ages 4 and 6, only use over-the-counter products when recommended by your child's healthcare provider. In most cases, also don’t give antihistamines. They can dry up the secretions. That can make the cough worse.
Don’t give aspirin or medicine that contains aspirin to a child younger than age 19 unless directed by your child’s provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver.
.
What are possible complications of acute bronchitis in a child?
Most children who have acute bronchitis will get better without any problems. But the illness can lead to pneumonia.
How can I help prevent acute bronchitis in my child?
You can help prevent acute bronchitis by stopping the spread of viruses that may lead to it.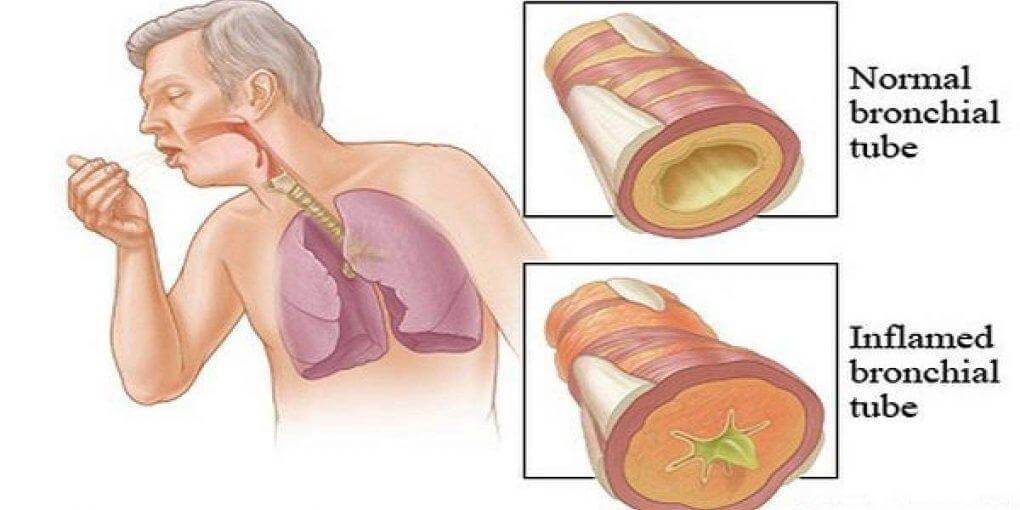 Take these steps:
Take these steps:
- Teach your child to cover their nose and mouth when coughing or sneezing.
- Make sure your child washes his or her hands often.
- Check that your child is up-to-date on all vaccines, including the yearly flu shot.
When should I call my child’s healthcare provider?
Call your child’s healthcare provider right away if your child’s symptoms get worse, if new symptoms develop, or if he or she has:
- Trouble breathing
- A high fever
Key points about acute bronchitis in children
- Bronchitis is an inflammation of the large breathing tubes (bronchi) in the lungs. Acute bronchitis means that the symptoms often develop quickly and don’t last long.
- In children, the most common cause of acute bronchitis is a virus.
- A cough, fever, runny nose, and body aches are common symptoms.
- Treatment is aimed at easing symptoms. It may include plenty of rest and fluids. Medicines for fever or cough may also help.
- Antibiotics are not needed, unless the cause is a bacterial infection.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Obstructive bronchitis in children - City Hospital No. 12, Barnaul: articles
Respiratory diseases are sooner or later associated with any child. These include not only SAR, but also laryngitis, bronchitis, pneumonia, bronchitis, etc. It expresses bronchitis, which is a complication of upper respiratory diseases. The blockage is when some of the blood vessels become trapped, constricted, and affect the function of the organs.
Obstructive bronchitis in children is a lung disease that also occurs due to a decrease in the bronchi and convulsions, which leads to the accumulation of mucus, adversely affects the breathing process and complicates breathing.
Outgoing bronchitis has acute and chronic. This disease is mainly characteristic of infants.
What provokes / Causes of Obstructive bronchitis in children:
1. Frequent bronchitis and incomplete bronchitis
2. Congenital forms of bronchial development
3. Low oxygen status during pregnancy and childbirth
5. Initial infection
6. Received a handAcute obstructive bronchitis pediatrics is often caused by influenza virus, respiratory infection virus, adenovirus, type 3 virus, bacteria, akage monkey virus and linovirus. In recurrent obstructive bronchitis, mycoplasma, herpes virus and chlamydial virus are often detected during bronchial lavage.
Dangerous states a-children
- My immunity is decreasing
- With increasing allergic background
- Hit Sars
- Having genetic priority
Starting factors.
- Air pollution (mainly sulfur dioxide)
- Secondhand smoke (when the parent mainly smokes)
- (Particularly when exposed to carbon monoxide in the atmosphere (especially when exposed to air pollution))
- Contact with cadmium and silicon
Pathogenesis (what happens?) during Obstructive bronchitis in children:
In contrast to changes in the thickness of whole bronchi, obstructive bronchitis causes stenosis, edema and bronchial conduction.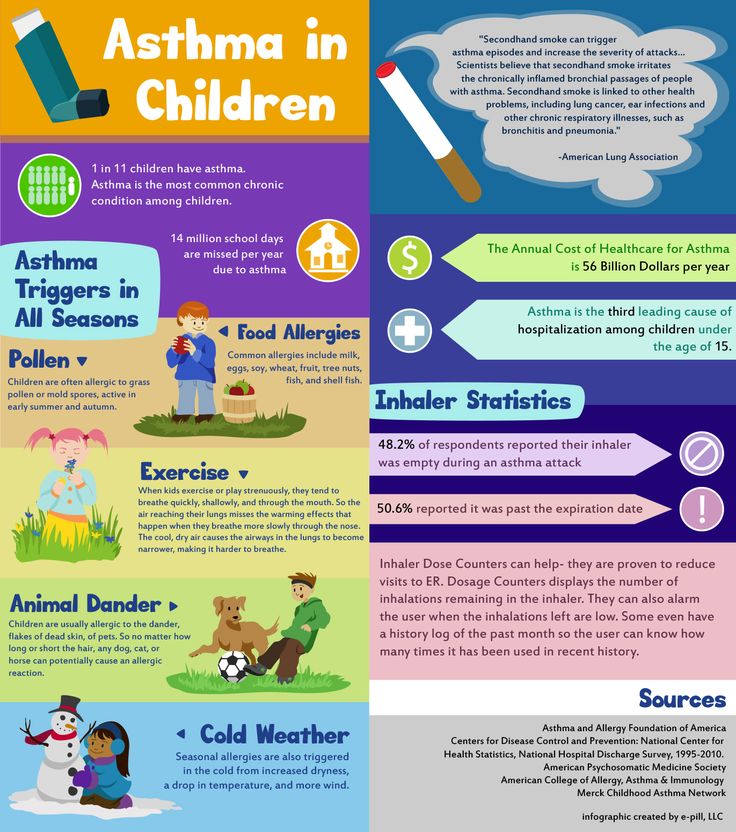
Genetic and environmental influences generate inflammatory processes involving the small tube, middle branch, and tissue around the bronchi. As a result, the movement of epithelial patches is inhibited and transformation occurs later, losing cell cells and increasing the number of n-type Pa cells. In addition, bronchial secretion, mucus composition and blockage of the auxiliary tube supporter, resulting in a balance between ventilation and diffusion.
The content of non-specific local immunity factors also decreases due to bronchial secretions and plays a role in protecting the body from viruses and microorganisms. Such factors include interferon, galactoferrin and raguem. Bronchial secretion has high viscosity and thicker, so the sterilization power is reduced, causing pathogens such as bacteria, viruses and fungi. An important role of the disease relates to the activation of working factors of choline in the autonomic nervous system, causing a bronchodilatory response.
The mechanism described above causes swelling of the bronchial mucosa, excessive mucus indelaism, and smooth muscle spasms. Basically, it's bronchitis.
Symptoms of Obstructive bronchitis in children:
1. Partial picture
2. A large amount of viscous sputum appears
3. Severe sputum
4. Shot in the lips and fingers of Chianose during coughing attack, respiratory failure 9002 9002 9002 In the case of physical labor or severe illness, this tends to be insufficient during rest. Unlike "Heart", shortness of breath is a child who sleeps well and sleeps well and is a child who does not try to sleep while sitting and standing.
Diagnosis of Obstructive bronchitis in children:
Obstructive bronchitis in children is diagnosed with typical symptoms, but such examination is important.
- Doctor
- Endoscope
- functional
- X-Heart
- Laboratory
Obstructive bronchitis in children varies depending on the stage and form. As the disease progresses, a capsule-shaped sound appears on the lungs, the tremor of the voice weakens, and the mobility of the lung of the limb decreases. As a result of listening, a wet pregnancy line was also confirmed during the forced voice, dyspnea and acute phase. After coughing, the amount of wheezing and change in tone.
As the disease progresses, a capsule-shaped sound appears on the lungs, the tremor of the voice weakens, and the mobility of the lung of the limb decreases. As a result of listening, a wet pregnancy line was also confirmed during the forced voice, dyspnea and acute phase. After coughing, the amount of wheezing and change in tone.
X-Ray check performed to rule out local lesions and lung lesions. In this method, it is also possible to identify emerging diseases. Two to three years have passed since the appearance of the fuselage, an increase in the shape of the bronchi and emphysema was detected.
When diagnosing chronic obstructive bronchitis in children, study the functions of external respiration. Spirometry is used, such as inhalation test, Parmono truck test and peak flumetry. Based on the data obtained in these methods, the period of pulmonary ventilation disorders, whether bronchitis is determined by bronchial obstruction, the degree, reversible and chronic obstructive bronchitis.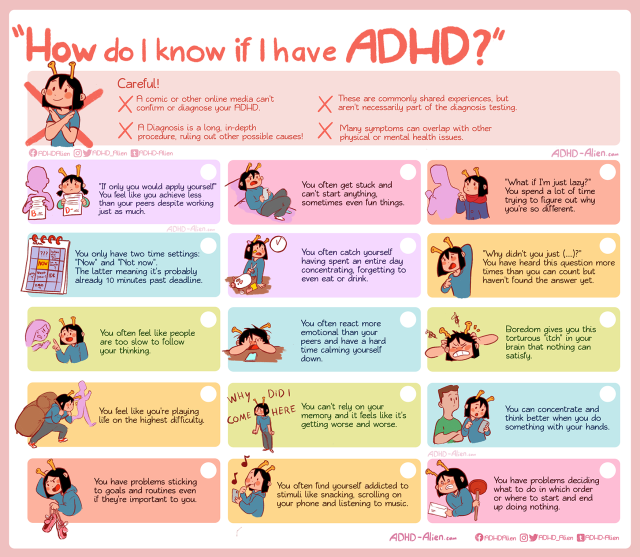
In the case of obstructive bronchitis, bronchoscopy for treatment and diagnosis is performed to check the bronchial mucosa, collect sputum, and clean the bronchodors. Bronchoscopy is performed only in certain cases to rule out bronchodia.
Examination diagnosis.
- Blood biochemical parameters (fibulinogen, total protein and protein division, bilirubin, sil-acid, glucose, aminotransferase, etc.).
- Total blood cells
- General urine test
The degree of respiratory failure in the case of obstructive bronchitis is determined using blood gas composition and CBS. Doctors may order bacterial tests for sputum and cleaning solution and microscopy. For identification with pulmonary tuberculosis, methods such as PCR and AFB are used.
The growth of chronic obstructive bronchitis at diagnosis differs from bronchial asthma, bronchodia, tuberculosis, pneumonia, and childhood lung cancer.
Treatment of obstructive bronchitis in children:
If pediatric occlusive bronchitis develops with influenza, antibiotic treatment is necessary. However, sputum should be removed for culture and antibiotic susceptibility testing. Doctors may prescribe antibiotic tablets. If this is not effective, even if it continues for 4 days, use it in the form of an injection.
However, sputum should be removed for culture and antibiotic susceptibility testing. Doctors may prescribe antibiotic tablets. If this is not effective, even if it continues for 4 days, use it in the form of an injection.
In addition, antifungals and bifidical products are used to protect the respiratory organs from dysentery, which can harm children. The latter cannot be used with antibiotics. The treatment of this disease is carried out with the help of a mucous solution. This is a group of medicines that have phlegm and disturbing phlegm. Not all slime solutions are suitable for children, so don't go overboard. The name and use of the medicine must be instructed by the attending physician.
For dry paraacid cough, doctors may prescribe medicines that act in the cough center of the brain, such as revexin. However, it should not be used if phlegm is involved.
A bronchodilator may be used. These are extensions, for example, eufhillin or broncolitin. Currently there are many side effects so we use it less.
To treat chronic obstructive bronchitis, take antibiotics on a course. Continuous use is very harmful. The immune drug is the first. Topical use of immune formulas derived from plants. To improve sputum production, massage your back regularly.
For sick children, complete food rich in protein and vitamins should be given. Breathing with your child.
Prevention of Obstructive Bronchitis in Children:
1. Instructions for a handwashing program, especially from winter to autumn, especially from winter to autumn.
2. If handwashing is not possible, keep antibacterial sanitizer close to the child. Pharmacies and supermarkets sell products from various price ranges.
3. Limit contact with the sick person.
4. Avoid smoking around your child, especially in the apartment. Even if there is no smoke in the children's room, there is a chance that there is smoke there, which can adversely affect the respiratory system of your son and daughter.
5. Do not take your child to a smoking facility.
6. Please consult your pediatrician about how to get vaccinated. Inoculation of influenza and pneumonia vaccines may reduce the possibility of bronchitis, which is a complication of these diseases.
Which doctors should you contact if you have Obstructive bronchitis in children:
Is this something worrying? Click here if you want to know more about the cause, symptoms, treatments, preventive methods, and food for children with obstructive bronchitis. Or do you need an overview? You can make a booking for a consultation.
Obstructive bronchitis develops in children on the background of bronchial inflammation. Inflammation occurs in the mucous membrane inside the bronchi. As a result of edema, the internal cavity narrows. The process of inflammation covers the entire network of the bronchus, which leads to epithelial dysfunction.
The condition is accompanied by an obstruction and the exercise of the bronchi is disturbed.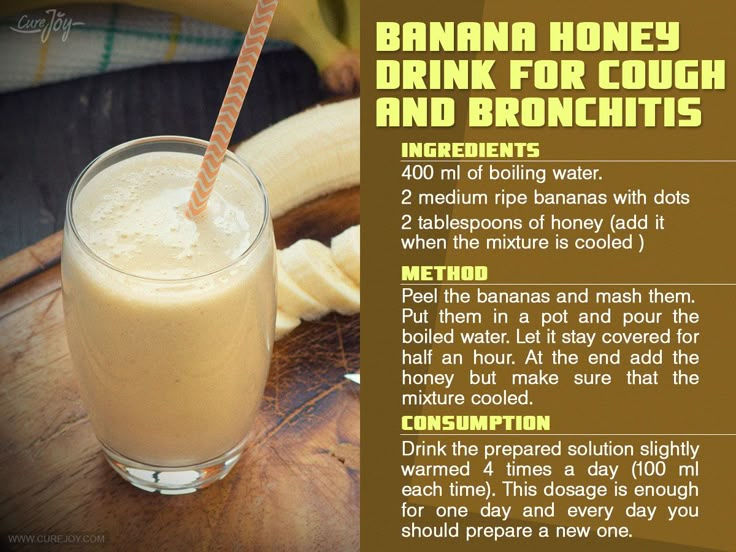 Obstructive bronchitis is characterized by an unproductive cough, meanwhile wheezing, faster and noisier breathing. This occurs regardless of age, but many children under the age of 5, those with allergies, those who have reduced immunity, and children with a primary genetic.
Obstructive bronchitis is characterized by an unproductive cough, meanwhile wheezing, faster and noisier breathing. This occurs regardless of age, but many children under the age of 5, those with allergies, those who have reduced immunity, and children with a primary genetic.
Causes of childhood obstructive bronchitis
Children under three years of age often develop obstructive bronchitis due to a viral infection. Various respiratory viruses can cause lesions.
- Influenza ;;
- Respiratory synchronous?
- Adenovirus?
- Adenovirus
Bacterial preparations and infectious diseases (chlamydia, mycoplasma) can cause obstruction. Allergic factors play an important role in the beginning. Children with atopic dermatitis and food allergies are said to be susceptible to pathological effects. The danger factors are as follows.
- Physiological and anatomical characteristics: narrow airways, low immune activity, weak respiratory muscles and very viscous bronchus.
- Pregnant pathology: advanced anesthetics, risk of miscarriage, toxicosis and internal infections.
- Bad habits during pregnancy: smoking and drinking.
- I have a complicated history of allergies.
- Abnormal growth of the bronchi.
- Premature baby. A baby who was born between 22 and 30 weeks and does not have vitamin D.
- History of respiratory infection up to 6 months.
- Disposal: exudation or lymph.
The onset of sinusitis, caries and tonsillitis recurs when insects appear. The condition may worsen the association.
- Hypothermia
- Hypothermia; overwork; hypothermia; hypertrophol; hypertensive heat disease; hypothermia
- Emotional exercises
- bad weather
- Reduced body protection function
- vitamin
The onset of obstructive bronchitis in children may be associated with passive smoking and exposure to high concentrations of dust.
Pathogenesis of the disease
In the lesions of the bronchial mucosa, leukocytes also appear due to the invasion of viruses and bacterial infections. The inflammatory mediator is activated and histamine, cytokine and prostaglandin are released. The bronchial wall is swollen.
The smooth muscle of the bronchial muscles decreases, contributing to the occurrence of bronchial convulsions. As a result of pancreatic cells, bronchial secretions were found. High viscosity and interferes with the normal function of the epithelium for the body of the hair. As a result, mucosal dysfunction occurs, preventing the discharge of sputum.
As a result, the respiratory tract is covered with a secret. An environment for the spread of pathogenic microorganisms is formed. The process of inflammation is applied to the lower mucous membrane and bronchial muscles.
Classification and stages
Experts distinguish obstructive bronchitis into several types.
- Bronch stones.

- Bronchitis; bronchial hypertension; acute obstructive pulmonary disease.
- Recurrent obstructive bronchitis.
Recurrent obstructive bronchitis, recurrent bronchitis, chronic obstruction, recurrent bronchitis, recurrent bronchitis in many cases develops in response to linovirus and respiratory systemic infection. In the previous Arvey stage, it can be mild and foregoing. With the deterioration of the whole body of children, there is a risk of heart failure and respiratory failure. With bronchitis, you may hear a wet loneliness that is wet during consumption and exhalation.
3-5 year old child affected by viruses, influenza and adenovirus appears to be acute obstructive bronchitis. It is a disease that characterizes the symptoms of SARS that rise rapidly. This can aggravate to respiratory failure. By involving the muscles of the neck and shoulders, this causes severe shortness of breath. The exhalation is long, heavy and looks like a whistle.
Symptoms of obstructive bronchitis in children
Relapse of blockage occurs regardless of age. It is affected by viruses such as herpes, site megalovirus, Epstein Rose, and mycoplasma. Obstructive symptoms gradually progress. Body temperature is normal or slightly elevated. There is rarely a cough, rarely an obsessive nose. There is difficulty in the middle breathing.
As a clinical presentation of obstructive bronchitis, body temperature rises (between 37 and 390 °C), silly nose, runny nose and rarely cough. Infants under three years of age have been found to have gastrointestinal disorders (Binging, diarrhea). These symptoms last from one to three days.
In some cases, obstructive bronchitis occurs suddenly. Symptoms often appear from evening to night. It is difficult for the child to wake up with a rough cough, make noise during breathing and exhalation. After 1-3 days, shortness of breath appears, and during breathing, the shoulder, throat and diaphragm hurt.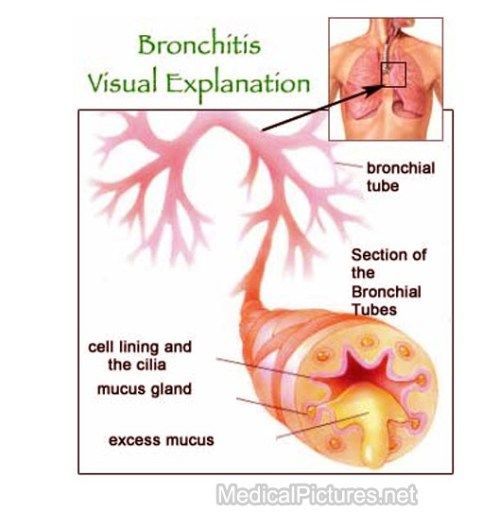 Children can be calm and excited. The skin becomes pale, the triangle on the face is bluish, and the skin becomes marbled.
Children can be calm and excited. The skin becomes pale, the triangle on the face is bluish, and the skin becomes marbled.
This often appears at the onset of the disease rather than the symptoms of SARS. OB stays many times a day and appears in characteristic symptoms.
- Rapid breathing (about 60 times per minute).
- Take 60 times per hour (60 times in 60 minutes per minute, 60 times in 1 minute).
- Noise during breathing and whistling sound.
- Noise and voice of noise; noise voice noise and noise voice noise and trousers; noise and voice air noise and voice noise and states voice
- Involved in respiration of parasympathetic nerves
- Breast augmentation
- Cough and paroxysmology with little sputum.
- Skinfu Coop
- Blue and Olofachi Shark Riangle
- Inflammation of the cervical lymph node
Obstructive symptoms occur within one week. After the inflammation intensifies, it will gradually subside.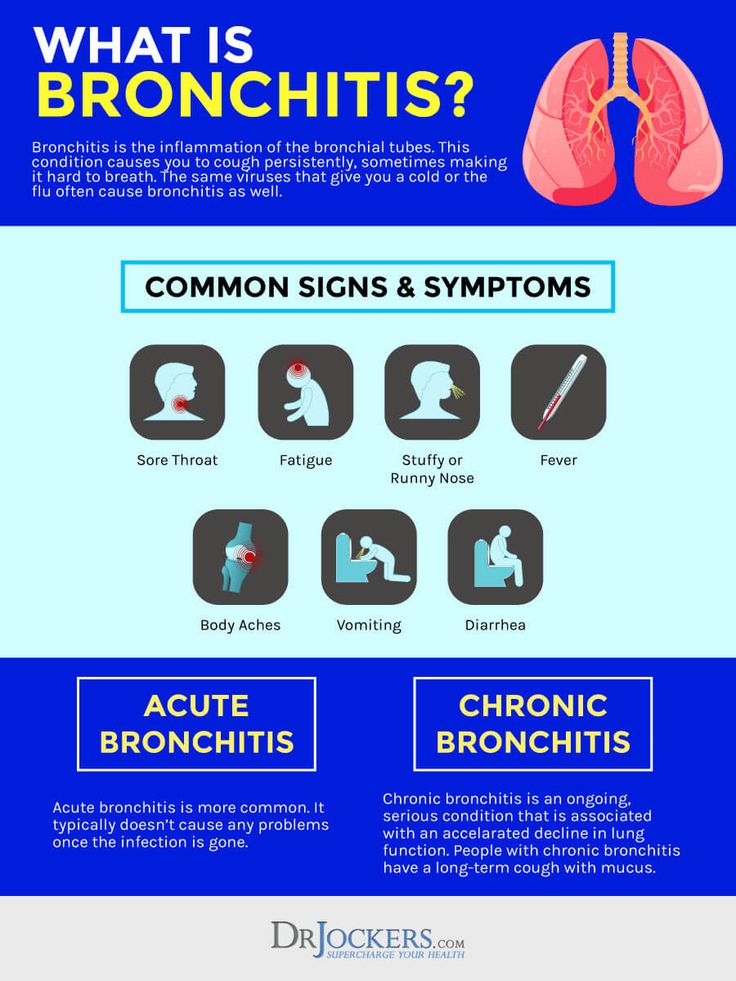 Acute bronchitis, especially in children under six months of age, causes severe respiratory distress.
Acute bronchitis, especially in children under six months of age, causes severe respiratory distress.
Complications
When disease occurs, there is a risk of recurrent acute obstructive bronchitis and secondary bronchodism. The recurrent type results from passive smoking, overheating, low body temperature, frequent acute respiratory viral infections, and incomplete treatment.
Children under 3 years of age may have pneumonia. This is due to the fact that viscous sputum is difficult to turn over, blocks the internal cavity and disrupts ventilation of the lungs. Includes bacterial infection, causes inflammation.
Diagnosis
Diagnosis includes tests, medical history, functional tests, clinical tests and organ tests. Diagnosis - pediatric respiratory doctor.
Clinical blood tests can check for signs of inflammation. If you repeat the lockdown, you may need an allergy test. When checking x-ray, you can evaluate the transparency of the lungs, the position of the ribs and the dome of the diaphragm. This test is performed when the onset of pneumonia and the presence of foreign substances are suspected.
This test is performed when the onset of pneumonia and the presence of foreign substances are suspected.
Treatment of obstructive bronchitis in children
The need for hospitalization arises in case of severe illness in children. Addiction treatment requires technology.
- Antiviral agent
- Includes antibiotics.
- Inhaled steroid.
- Selective bronchodilator.
Use of the drug appears to relieve symptoms.
- ;
- Anti-inflammatory agent
- Ant i-fever; antiframing agent.
- For thinning sputum.
- Immunity booster
During the recovery period, physiotherapist treatment, breathing exercises and massages are carried out.
Mucous
- Used for the treatment of acute and chronic respiratory diseases.
- This is a mixture of polysaccharides of parachute herb drug.
- It has a whitening effect.
There are contraindications. Please read the instructions carefully before use or consult your doctor.
Please read the instructions carefully before use or consult your doctor.
Prognosis
About 50% of children suffering from occlusive bronchitis are said to relapse within one year. In the recurring type, there is a risk of bronchial asthma. This disease must strictly adhere to timely treatment and doctor's prescription. The prognosis is good, taking medications according to the system, testing and correcting the treatment according to the treatment plan. If you are treated in your own way, you will be more likely to relapse bronchitis.
Prophylaxis
Prophylactic measures mainly to improve immunity and eliminate dangerous factors such as hypothermia and contact with sick people.
Children's meals should be full of meat, eggs, fish, vegetables, fruits and fermented dairy products. It is necessary to limit the use of products that cause allergies. In addition, preventive measures include hardware, exercise, recovery, and vaccinations.
Bronchitis is limited to the bronchi, and it is an inflammation of the respiratory organs that does not extend to lung tissue 5. Depending on the progress, bronchitis in children is 1:
Depending on the progress, bronchitis in children is 1:
Relapse 2-3 times a year, developing in children under the age of 4-5 years 2. In this type, there are no irreversible changes in the bronchi 2.
Chronic - lasts more than 2 years, with symptoms lasting more than 3 months a year. The chronic form is characterized by bilateral changes, i.e. structural remodeling in different parts of the bronchial tree 1.6.
Later we will tell you about when a child gets bronchitis, the symptoms of bronchitis in children and how to deal with the initial symptoms of the disease.
Causes of bronchitis in children
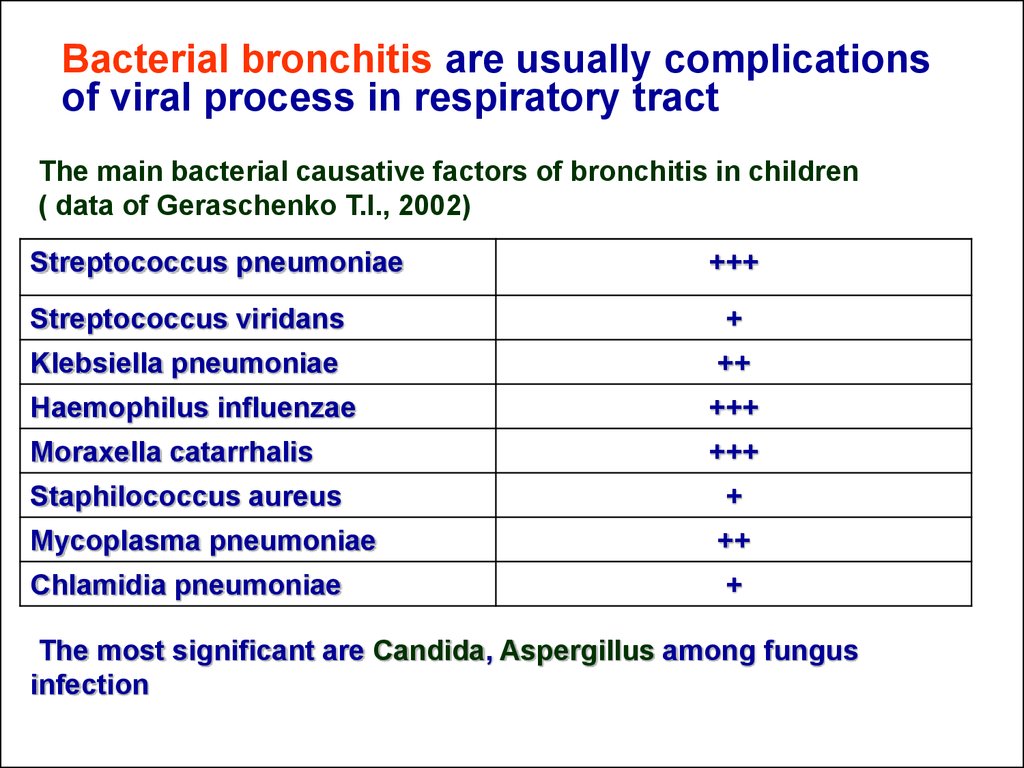
5. Acute inflammation of the bronchi is usually associated with infection. To date, more than 200 viruses and more than 50 bacteria are known to cause acute bronchitis in children aged 6 years and exacerbations of recurrent type 2.
respiratory viral infection (ARVI) 5:.
Early childhood up to 3 years - usually paraviruses (type 3), respiratory tract viruses, rhinoviruses 6.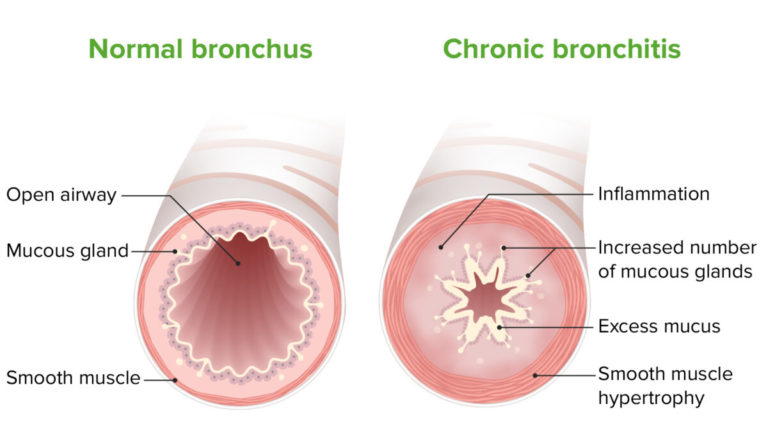
The influenza virus can cause bronchitis at any age6. Less commonly, the bronchi are attacked by bacteria (eosinophilic rods, moracers, streptococci, pneumococci) and other pathogens. And sometimes infections are associated with the action of viral and bacterial coalitions6.
The following factors also contribute to the development of bronchial inflammation 1:
Allergens (plant pollen, household dust, small particles of cleaning / detergents, pet hair) 6.
Prolonged exposure to viruses and aggressive external factors causes chronic inflammation of the bronchi. It uses bacteria and begins to multiply on the mucous membranes and can cause bronchitis.
Normally, the airways are covered with microvilli 10 that protect the cells of the mucous membrane (epithelium) from the adverse effects of destructive agents. On top of the shell is a thin layer of bronchial secretions (mucus). The cilia perform rhythmic vibrational movements, clearing the bronchial lumen from foreign bodies 1 10 . However, viruses, bacteria and allergens that enter the epithelium damage these cilia, causing them to lose their mobility 10 . Inflammation also makes it difficult to physically clear the airways, as the mucus that covers the shell becomes larger, less fluid, and more viscous 6 .
However, viruses, bacteria and allergens that enter the epithelium damage these cilia, causing them to lose their mobility 10 . Inflammation also makes it difficult to physically clear the airways, as the mucus that covers the shell becomes larger, less fluid, and more viscous 6 .
Causes of obstructive bronchitis in children
Obstructive bronchitis is when the lumen of the bronchi narrows or closes completely. Reasons for blockage include 2:
- bronchospasm
- thickening of the walls of the bronchi.
- Thickening of mucous membranes
- Highly viscous sputum accumulates.
Some experts believe that obstruction occurs to protect the lungs from bacteria from the upper respiratory tract6.
Children with weak immune systems or who are prone to allergic reactions have an obstructive predisposition.
Symptoms of bronchitis in a child
Cough is an obligatory symptom in bronchitis 6. It uses protective reactions to remove pathogens and dead cells from the bronchial tree 11 . In this case, coughing can be different.
In this case, coughing can be different.
Dry (unproductive) - in the first days of the disease, when sputum is not separated 16 or with signs of obstruction with spasm of the bronchial walls 6. mucus by bronchial glands 11.
Unproductive - superthorn, dryness, low sputum volume. Such a cough occurs with viscous sputum and impaired patency of the bronchial loop 3.
Pediatric sputum includes clear, white (mucous), yellow, yellow-green and brown (mucus and purulent) depending on the pathogen.
Blont may take a long time to recover after the body has been treated with the virus, so he may continue to cough for one or two weeks. 5. You may worry even if all the symptoms of another bronchitis disappear.
This can be seen with bronchitis.
Generate heat. Body temperature usually rises slightly and does not exceed 38 ° C, but bronchitis often occurs without an increase in body temperature. 3. The fever usually does not last long, the body temperature does not reach a high value, and it returns to normal after a few days.
Pant voice. The breath is dry and wet, and its strength and nature change with coughing. With blocking, the whistle is similar to a whistle and sounds best when exhaled. The situation is that the air passes through the narrow bronchi and is filled with sputum that is difficult to separate with high viscosity.
As a principle of dyspnea, it is observed in children with obstructive bronchitis. The child detects expiration, and the accessory muscle connects the respiratory act to assist his mediastinal and pectoral muscles. 6.
If you have a significant increase in body temperature, you may experience complications, especially pneumonia. If you have 3 days or more of fever, anorexia, drowsiness, headache, and shortness of breath, you should consult your pediatrician to rule out the possibility of pneumonia.
Diagnosis of bronchitis in children
You need to contact a pediatrician or pediatrician to determine the diagnosis. This is gradually being discovered by doctors. Experts take the following five considerations.
Experts take the following five considerations.
If you suspect complaints, tell your doctor about the onset of the disease, the presence or absence of contact with the disease, regardless of whether the body temperature (numbers), cough and change in personality.
For example, it is prescribed by a pediatrician according to adaptation, if it is necessary to find out the pathogens of clinical testing.
Organic research. Lutino is not implemented. If pneumonia is suspected, an x-ray chest test is required.
If bronchitis is common, it may be necessary to consult immunology or allergy experts. 4.
Treating bronchitis in children
I cannot cure myself. How to cure bronchitis, the pediatrician decides. He is the only one who can choose the best combination of drugs, decide how to administer it, and consider all the exciting elements. This is a treatment to remove the cause of bronchitis and relieve symptoms.
A doctor may be appointed as part of a complex treatment.
To relieve cough, which is the main symptom of bronchitis, children can take the following 17 medicines for children.
Drugs
action
Easy to divide sputum and 16
Increase the number of bronchodula 17
Act on the natural mechanism of clearing the bronchi and improve sputum 17
Adjust the secretion of bronchial mucus 90 90
2 Suppression of cough reflex 11
It must be remembered that bronchitis does not always adapt, but only with a dry and painful non-productive cough 5.11.16. In some cases, antipsychotics may interfere with the effects of sputum, and the risk of bacterial complications may increase by 5.
For sputum that is very viscous and difficult to separate, using a herbal preparation such as cough syrup and Doctor Mom® can be completely effective. Contains 10 kinds of medicinal herbs, a combination of anti-inflation effects, bronchial expansion, mucus dissolution and atonement. Doctor Mama® cough syrup has the effect of promoting mucus discharge and clearing the bronchi.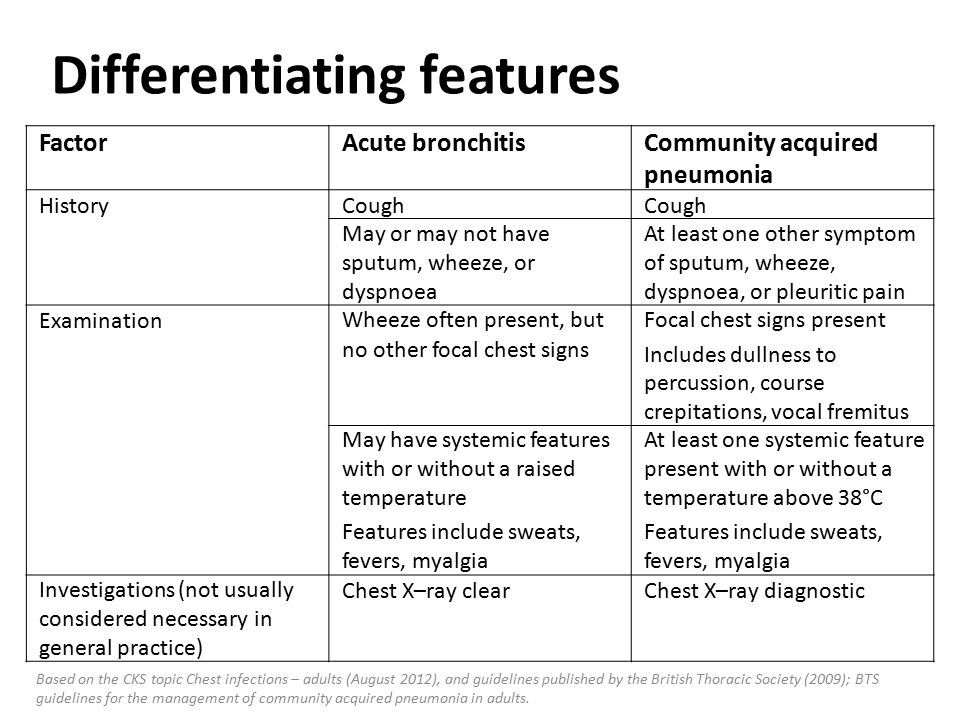 At the same time, fight the "18" inflammation that causes the cough.
At the same time, fight the "18" inflammation that causes the cough.
For acute bronchitis, don't forget that you need rest in bed, nutritious meals and plenty of drinks 6.14. Give very warm water as a guide 14.
For children who are worried about other cold symptoms such as headache, muscle pain and stuffy nose, you can use Dr. Mom® Fito externally. It combines three types of essential oils, Thymol, Levomenol and Campor, which show local anesthesia, antiseptic, local anesthesia and anti-inflation effects. If you have a cold and apply the ointment to the wings of your nose, if you are worried about your nose or a mocking nose, with a whiskey head, muscles or waist, apply the ointment to the painful place.
During the recovery period, it is recommended to perform respiratory exercises and chest drainage to stimulate sputum 14.
Prevention of bronchitis
Most children are caused by viruses, so it cannot be protected. Children are exposed to many sources daily, but to compete with it, increase immunity and keep the precautions. 1.4.6. The latter has the following:
1.4.6. The latter has the following:
Bronchitis is a disease commonly seen in children with a cold, and all parents meet at least once. However, a doctor's consultation is necessary to accurately determine the diagnosis. Do not move, trying to fight only the symptoms of the disease. If the first signs of bronchitis appear, consult a specialist. If your cough lasts more than 10-14 days, breathing is difficult, and the fever does not drop by 14, be sure to contact your pediatrician at home or make a pediatrician booking. Doctors will find out the cause of the disease, especially if it gets worse, and prescribe treatment to manage both the cause of the bronchitis and its symptoms.
The information in this article is for reference only and not for specialized medical advice. For diagnosis and treatment, consult a qualified expert.
References:
- Method development for pediatric teachers/http: //stgmu.ru/userfiles/depts/face_pediatrics/metodicheskie_razrabo.
 (Release date: 20/07/2021).
(Release date: 20/07/2021). - Zakirov I. I., Safina A. I., Shagiakhmeta D. S. Diagnosis of recurrent bronchitis. Vestn Perinatol and Pediatrician 2016 have grown. 61:5:141-148. DOI: 10.21508/1027-4065-2016-61-5-141-148.
- Samsygina G.A. Chronic bronchitis in children: a modern vision of the problem. Consilium Medicum. Pediatrics (app.). 2016? 3:55-59.
- Clinical recommendation of the federal government (2015) for the care of children with acute bronchitis.
- Clinical recommendation (draft). Bronchitis Russian Federation of Pediatrics, Regional Clinical Microbiology and Antibacterial Chemotherapy (MCAM).
- This is a guide to bronchitis for children. This is a guide. Guidelines for students, internships, pediatricians, general practitioners, advanced training and re-registration of students of 4-6 courses of all faculties of higher medical educational institutions / AI Zaryankin, A. Kozlovsky.
- Yulish E.I. Selection of bronchitis and treatment confrontation in children // Zr.
 2015.2 (61). URL: https: //cyberleninka.ru/n/rticle/ronhity-dety-vybor-protivokashle. (Release date: July 20, 2021).
2015.2 (61). URL: https: //cyberleninka.ru/n/rticle/ronhity-dety-vybor-protivokashle. (Release date: July 20, 2021). - Vladimirov S.N. Influence of Moscow on the health indicators of citizens // Bulletin of science and practice. 2016. No. 5(6). S. 34-39.
- Ilchenko S.I., Duka E.Y., Zhukova L.A. Microorgasmic syndrome in pediatric practice: current features and role in the formation of broncho-structural syndrome // Zr. 2016. No. 7 (75) (Release date: July 20, 2021).
- Astashonok A.N., Poresk N.N., Rubanic L.V., Boblofnicchee V.I. Respiratory organs in pediatric diseases of the upper and lower respiratory tract: ultrafin structures and nanoscopic analysis. News of the Belarusian National Scientific Academy. Medical Sciences Series. 2021-18(1): 69-79.
- FSTY FIERWA G.YU., True Sova O.Yu., Danilova E.I., Sumenko V.V. Clinical effective medical consultation on porridge in pediatrics 2019; 2:194-198.
- Delyagin v.m. Cough for children d-need for treatment? 2018-(2): 82-85.

- Zaitsev A.A. Cough. International recommendation // Effective page of drug therapy. 2019.t. 15. No. 27, pp. 38-48.
- Clinical recommendations Acute bronchitis in children. Russian pediatrician Federation. 2016
- Acute respiratory viral infection (SARS) in children. Russian Pediatric Association. 2018
- Diagnosis of bronchitis in children, treatment, prevention [text] / a. Girina, n. Koroid, A. Sulskov // Doctor. -2014. -No.1. -Pp.74-78. -Pp.74-78.
- 1. Recorded by S.V., Maryushkina V.S., Sukhanov D.S., Selizarova N.O. "Pharmaceutical Approach for Rational Selection of Complicated Drugs from Strange Drugs" visited Doctor, 12, 2020, 41-45 pages.
MAMA® Pharmaceutical Physician Guidelines for using MAMABLE for Pitot Moblement // Reg. P number N016277/01 // Russian Federation GRL. —
Bronchitis is a disease in the upper respiratory tract that often occurs in childhood and is characterized by inflammation of the bronchi. This condition can be easily confirmed by a dry cough that is worse during talking and laughing. A few days later, a non-productive cough is reshaped, mucus and has a large amount of sputum.
This condition can be easily confirmed by a dry cough that is worse during talking and laughing. A few days later, a non-productive cough is reshaped, mucus and has a large amount of sputum.
Childhood bronchitis is most likely caused by infectious diseases. In many cases, it is caused by the influenza virus, which is the causative agent of SAR. Often bacterial infections and damage to the bronchi and due to viruses are relevant, in which case the disease receives a virus and a bacterial course.
Bronchitis is as seasonal as many other respiratory diseases and peaks during the cold season (autumn to winter). Answer important questions about how to prevent complications and illnesses and treat your child's bronchitis to protect your loved ones.
Classification of bronchitis in children
Children's bronchitis is very common. By accurately classifying the disease in each case, the most effective treatment can be prescribed.
By origin, primary and secondary diseases are distinguished. In the first case, the pathology begins in the bronchi and affects only them. Secondary lesions develop against the background of inflammation in other parts of the respiratory system.
In the first case, the pathology begins in the bronchi and affects only them. Secondary lesions develop against the background of inflammation in other parts of the respiratory system.
According to the characteristics of inflammation, the following types of childhood bronchitis can be distinguished:
- catarrhal
- purulent?
- fibrous; fibrous; fibrous?
- hemorrhagic?
- Ulcerative?
- necrotic?
- is a mixture of
Depending on the course of the disease, bronchitis in children can be divided into acute, chronic and recurrent. This disease can be contracted for a number of reasons.
- virus
- with bacteria.
- viral-bacterial?
- toxicity?
- Allergic
- The disease may also be obstructive or non-obstructive. Bronchitis is a disease in which the small branches of the bronchi are most noticeably inflamed.
Symptoms of bronchitis in children largely depend on the form and course of the disease. The acute phase is characterized by rapid progression of the disease. The beginning and end of the disease are clearly defined. The greatest feature of this disease is its reversibility, in which the symptoms completely disappear during the period of convalescence.
The acute phase is characterized by rapid progression of the disease. The beginning and end of the disease are clearly defined. The greatest feature of this disease is its reversibility, in which the symptoms completely disappear during the period of convalescence.
Symptoms of bronchitis in children
Symptoms of acute bronchitis in children include:
severe paroxysmal cough
- Pain behind the sternum.
- Presence of wheezing when breathing.
- increased body temperature, increased urine pressure, dyspnea, dyspnea on breathing, dyspnea on breathing, dyspnea on breathing
- Noise and voice of noise; noise voice noise and noise voice noise and trousers; noise and voice air noise and voice noise and states voice
- chills and body aches
- Chronic bronchitis in children is characterized by a long course with repeated exacerbations and remissions. In this form, the bronchial mucosa is always edematous, which causes symptoms such as shortness of breath and lack of air.
 It is also characterized by a cough that does not go away for several months. Symptoms worsen during cold and flu season.
It is also characterized by a cough that does not go away for several months. Symptoms worsen during cold and flu season. - Obstructive bronchitis
The obstructive form is the most dangerous form and is characterized by persistent respiratory failure. As a rule, it develops at the age of 2 to 3 years and older and is accompanied by severe bronchoconstriction. Accompanied by wheezing, painful paroxysmal cough, prolongation of expiration. In severe cases, respiratory failure and heart failure may occur. If children show signs of obstructive bronchitis, they need immediate medical attention.
Tracheobronchitis
Bronchitis causes inflammation of the large bronchi and trachea. It is a dry paroxysmal cough with little sputum. Coughing fits can be triggered by certain factors, such as crying, stress, sudden changes in temperature, or heavy breathing. Dull or burning pain in the sternum may also occur during or after an attack.
bronchitis
Bronchitis is characterized by inflammation of the bronchi (bronchi at the junction with lung tissue). This disease is most common in children of the first year of life. The main symptom of bronchitis is shortness of breath. Initially, shortness of breath occurs in children during physical exertion, but over time it can also appear at rest. The child wheezes, has a characteristic hoarse voice when inhaling, expansion of the wings of the nose, fever up to 38-39°C. Constant cough with incessant barking and soreness in the chest.
This disease is most common in children of the first year of life. The main symptom of bronchitis is shortness of breath. Initially, shortness of breath occurs in children during physical exertion, but over time it can also appear at rest. The child wheezes, has a characteristic hoarse voice when inhaling, expansion of the wings of the nose, fever up to 38-39°C. Constant cough with incessant barking and soreness in the chest.
Infectious bronchitis
The infectious nature of bronchitis is characterized by the following symptoms:
After coughing, sputum comes out well on the 3rd or 4th day.
A hoarse sound may be heard when breathing.
- Pain is often felt in the sternum.
- Body temperature rises significantly, causing weakness and pain.
- allergic bronchitis
- Symptoms of allergic bronchitis in children are easily distinguished from other forms of the disease. Allergic bronchitis develops under the influence of allergens (specific irritants that cause allergic reactions in children), and not infections in the body.

The main feature of the disease is that clinical symptoms appear only upon contact with the allergen. Dry cough without phlegm and without fever.
Immediate treatment is required, as the risk of transition to bronchial asthma is high.
Toxic bronchitis
Toxic (chemical) bronchitis occurs as a result of constant exposure of the child's body to toxic substances in the surrounding air. This is a disease that often develops due to air pollution, dust, harmful gases, etc. It is characterized by shortness of breath, dry cough, wheezing, slightly elevated body temperature, hypoxemia (low oxygen in the blood) and pallor of the skin.
Children are said to be more susceptible to bronchitis than adults due to the structure of their respiratory system. Their narrow airways, weak breathing muscles, and low lung capacity make them vulnerable to infections that spread quickly.
There are two main causes of acute bronchitis in children: infectious and non-infectious.
Causes of bronchitis in children
due to infection
Infectious bronchitis is caused by invasion of the bronchi by pathogenic microflora (bacteria, viruses, rarely fungi or their combination). A weakened immune system in children is the main cause of infectious bronchitis. A healthy body can deal with infections on its own. Infections only occur when the defenses of the immune system fail. This happens due to certain factors that weaken the immunity of the child.
hypothermia
malnutrition
- hypothermia
- Insufficient body nutrients Insufficient body nutrients Insufficient body nutrients Insufficient body nutrients
- Mental or physical overwork (eg use of antibiotics, antibiotics, medicines such as antibiotics to treat disease, etc.).
- stressful
- Viral infections are caused by inhalation of influenza virus, parainfluenza virus, adenovirus, enterovirus, respiratory syncytial virus and rhinovirus.
 Viral bronchitis often develops against the background of untreated ARVI. The bacterial forms are caused by bacterial infections such as Streptococcus pneumoniae, Staphylococcus, Streptococcus, Haemophilus influenzae, Pertussis, Mycoplasma, and Chlamydia. Less commonly, bronchitis can be caused by a fungal infection. Fungi of the genus Candida albicans are the most common fungal pathogens.
Viral bronchitis often develops against the background of untreated ARVI. The bacterial forms are caused by bacterial infections such as Streptococcus pneumoniae, Staphylococcus, Streptococcus, Haemophilus influenzae, Pertussis, Mycoplasma, and Chlamydia. Less commonly, bronchitis can be caused by a fungal infection. Fungi of the genus Candida albicans are the most common fungal pathogens. - Transmitted by airborne droplets and household contact. It can be transmitted by close contact with a sick child or by sharing toys, utensils, towels, etc.
non-infectious causes
Non-infectious bronchitis includes allergic bronchitis and toxic bronchitis.
Allergic bronchitis occurs when there is a reaction to certain allergens. As a rule, it is caused by such allergens as pollen from certain plants, pet hair, chemicals and dust that enter the body. Atopic diseases include atopic dermatitis and food allergies as allergic causes of frequent bronchitis in children.

Toxic bronchitis develops when the body is exposed to adverse external conditions. Develops after frequent contact with smoky rooms, atmospheric air, household chemicals, construction dust, etc. treatment.
At the first visit, the specialist examines the child, listens to his complaints, determines whether the little patient and his parents have any factors contributing to the development of the disease, such as contact with sick people, a tendency to catch a cold, the presence or absence of allergies. Tests include chest palpation and acoustic testing (listening for wheezing and breathing sounds). After the doctor makes a preliminary diagnosis, the patient is sent for a laboratory or organ study to confirm the clinical case.
Diagnosis of bronchitis
Methods for diagnosing bronchitis include:
— It is necessary to check for signs of infection in the body. - Ability to identify pathogens of infectious diseases. - A mandatory test for doctors to visually confirm the pathology of the respiratory system.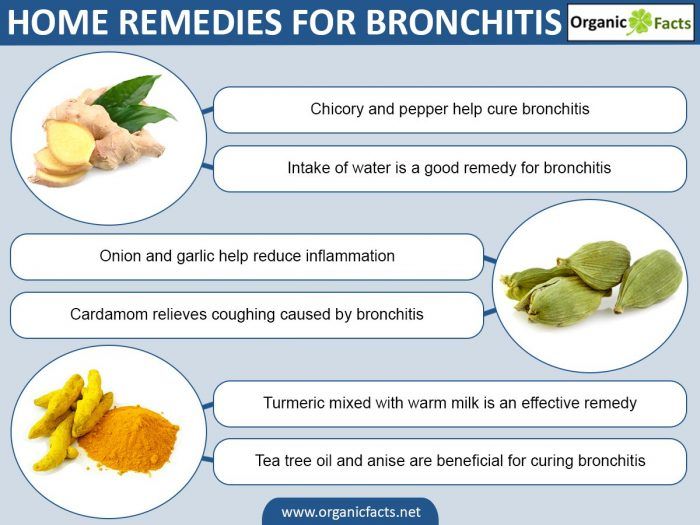 - You can determine the lung function status. Or computed tomography - allows you to examine the lungs and bronchi of the child in more detail. - A device called a bronchoscope helps specialists visualize the state of the mucous membranes of the trachea and bronchi from the inside.
- You can determine the lung function status. Or computed tomography - allows you to examine the lungs and bronchi of the child in more detail. - A device called a bronchoscope helps specialists visualize the state of the mucous membranes of the trachea and bronchi from the inside.
Research results vary on how to treat bronchitis in children.
- Treatment of bronchitis in children should be under the supervision of a qualified specialist. Self-medication can cause irreparable damage to the health of the child.
General recommendations
Treatment of bronchitis in children
To prevent the transition of chronic bronchitis to an acute form, it is necessary to create favorable conditions for the recovery of the child.
Take care of bed rest - the baby needs to gain strength to fight the disease.
Give plenty of warm fluids to reduce the viscosity of the sputum and make it easier to expectorate.
- Humidification, maintaining the room temperature (below 23°C), daily wet cleaning, ventilation, etc.
 make the children's room comfortable.
make the children's room comfortable. - If you don't have children, don't force your appetite to eat! Eliminate coarse, spicy, salty, spicy and other throat stimulants from your diet.
- drug therapy
- Drug treatment is aimed not only at fighting pathogens, but also at stopping unpleasant symptoms and alleviating the general condition of the child. Antibiotics are the basis for the treatment of acute and chronic bacterial bronchitis in children, antiviral drugs are prescribed for viral infections, and antifungal drugs for fungal infections. In case of allergic and toxic diseases, it is necessary to take antihistamines and isolate the baby from external stimuli.
Poor sputum separation from the bronchi may require the administration of mucolytic agents. When the temperature rises (more than 38 ° C), antipyretics should be used. For severe pain, you can give painkillers in the form of lozenges, sprays and syrups (depending on age).
physiotherapy treatment
The following physiotherapy methods are well known for the treatment of bronchitis:
inhale.
UHF, UHF, UHF, UHF, UHF, UHF, etc.
- To prevent bronchitis, you need to spend more time outdoors with your child, adjust your diet, limit contact with sick people, eliminate any symptoms of respiratory diseases as soon as possible.
- If your child has symptoms of bronchitis, sign up for diagnosis and treatment at the SM-Doctor clinic in Moscow. An experienced doctor will conduct the necessary tests, prescribe medications and physiotherapy exercises, and will monitor the baby until complete recovery.
- Bronchitis in children is a very common disease. This is especially dangerous for babies in the first year of life. In order not to waste precious time, it is important that parents do not make medicines on their own and do not follow traditional medicine recipes. If you have young children in your home, it may be helpful to have a nebulizer at home, a device for inhaling medicines. Medicines can be "delivered" directly to the inflamed area, significantly accelerating healing.

Prevention of bronchitis
Is it true that expectorants are harmful to small children?
Yes, sputum aspirators can aggravate the course of the disease, as babies are not yet able to cough properly. The use of such drugs is allowed only as prescribed by a doctor.
Expert opinion
Is it possible to inhale steam with bronchitis?
Q&A
Trying to seat your baby on a pot of hot potatoes or herbal tea can injure you. For inhalation, use a special device (nebulizer) and follow the doctor's instructions.
Childhood diseases: Textbook / Edited by A. A. Baranova — M.: GEOTAR-Media, 2007. Media, 2021
Obstructive bronchitis in children
Causes of obstructive bronchitis in children
Diagnosis of obstructive bronchitis in children
what it is, types of drugs and how to treat it
Of course, if a child has a dry, rough cough and an increase in body temperature, the child's parents will contact the district clinic in order to call a pediatrician.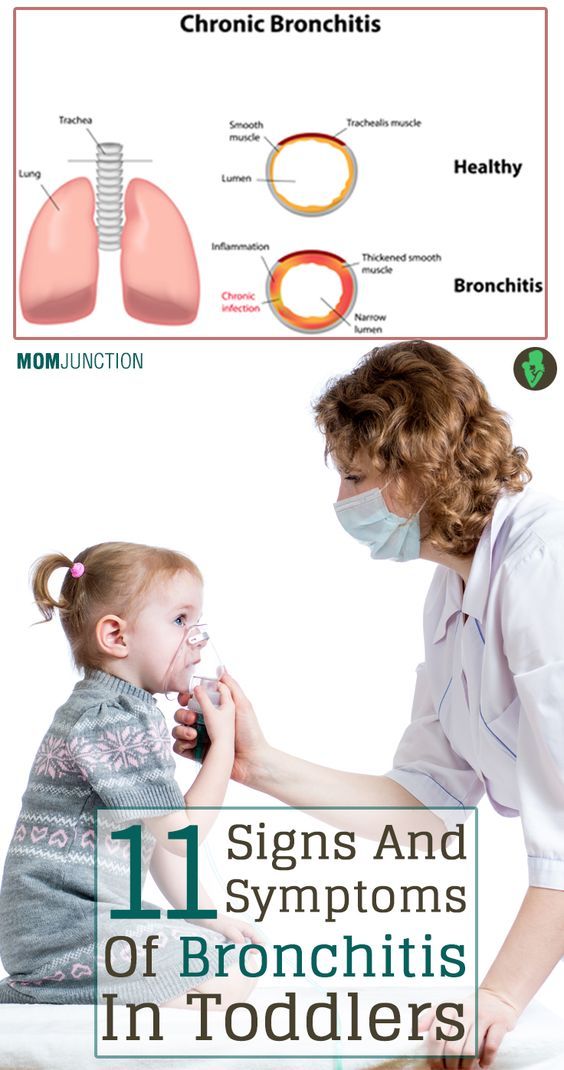 Everything is correct.
Everything is correct.
Usually, the first regimen prescribed by the district pediatrician when a child is diagnosed with bronchitis necessarily includes cough syrup (usually plant-based), or some kind of synthetic mucolytic, that is, a sputum thinning agent. The second item, as a rule, is an antiviral drug, such as viferon or arbidol, and some doctors still prescribe an antihistamine drug for the prevention of allergies, and in general they do it right.
Fortunately, more and more practicing pediatricians prefer not oral forms of antitussive drugs, but a simple and extremely effective way to treat cough (bronchitis, laryngitis, obstructive bronchitis) in children - a nebulizer.
Cough syrups and bronchitis. How do syrups affect the symptoms of bronchitis in a child?
In general, all cough medicines can be divided into three main groups:
- A - drugs of central action, that is, those that suppress the cough reflex in the brain. They do not solve problems, but they create the appearance of improvement.
 Although in some rare cases it is difficult to do without them, for example, when a child has whooping cough;
Although in some rare cases it is difficult to do without them, for example, when a child has whooping cough; - B - herbal preparations (mucaltin, pertussin, sinupret, and many others) mainly stimulate the secretion of the goblet glands of the respiratory tract, that is, they, on the contrary, increase the cough. The effectiveness of these drugs is higher, the older the child, but not earlier than 3 years! But in life there are, pardon the jargon, "nerds" who cannot cough themselves up even at the age of 14-15;
- B - preparations that thin sputum. These are basically all synthetic mucolytics: ACC, carbocysteine, ambroxol, erespal. Although a lot of things are written in the instructions for these drugs, but in the end, when a small child has bronchitis, and the doctor prescribes any syrup from group B or C, the result is always the same: the cough intensifies, but the result of this cough worsens. A small child does not have enough strength to cough up a large amount of sputum.
 This is especially noticeable on babies: while he lies on his back, he yells to the “blue”, they take him in his arms, he begins to cough a little and calm down, he can fall asleep in his arms with a “column”;
This is especially noticeable on babies: while he lies on his back, he yells to the “blue”, they take him in his arms, he begins to cough a little and calm down, he can fall asleep in his arms with a “column”;
It should be clarified that an experienced pediatrician prescribes an antihistamine drug (zyrtec or fenistil) together with cough syrups, since their flavorings often cause allergies in a child, especially if he already had dermatitis on the skin.
Childhood bronchitis and nebulizer treatment
Inhalation with a compressor nebulizer is the best way to cure bronchitis in a child. For infants, competent pediatricians recommend adding 6-8 drops of berodual solution to the inhalation chamber to expand the airways and improve coughing. In addition to the bronchodilator (berodual), a solution for inhalation of lazolvan or ambrobene is added to the inhalation chamber of the nebulizer (for children under one year old - 0.5 ml, over a year old - 1.0 ml), and this cocktail of drugs is diluted with a small amount, about 1.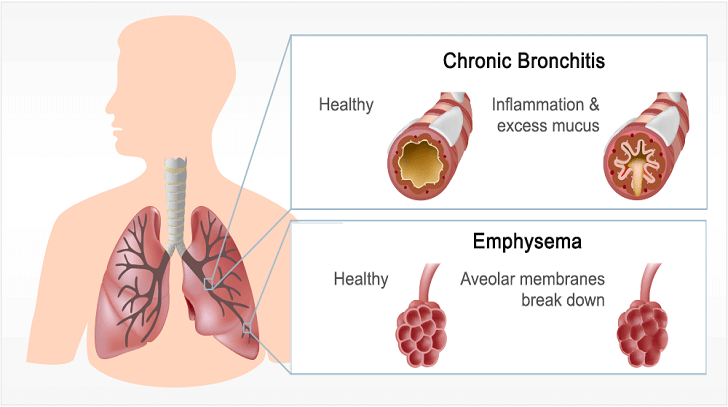 0 ml of saline or children's drinking water. The pediatrician prescribes such inhalations 2-3 times a day for 10 minutes for at least 5 days. But this is still not enough.
0 ml of saline or children's drinking water. The pediatrician prescribes such inhalations 2-3 times a day for 10 minutes for at least 5 days. But this is still not enough.
If you do only one inhalation, and nothing else, then the child's cough and bronchitis can drag on for a long time. After inhalation (not immediately, but after about half an hour - an hour), but before feeding, you need to massage the back with obligatory vibrational techniques (such as tapping with your fingertips, and a child older than a year - with the edge of the palms along the intercostal space), as well as some simple procedures from breathing exercises . A child younger than a year is usually rolled on a fitball (a large massage ball), putting it on his stomach (up to 6-7 months), and at an older age, you can already put the child on the ball, like on a horse. Instead of a fitball, with some experience, you can use your own knees, then you can combine light jumping on your knees with a back massage. Children after 2 - 3 years old, as a rule, already can and love to play with various inflatable tubes or blow bubbles through straws.
Children after 2 - 3 years old, as a rule, already can and love to play with various inflatable tubes or blow bubbles through straws.
In general, inhalations are good because the right medicine is delivered directly to the focus of inflammation itself, and is not “smeared” throughout the body. Plus, mineral water or saline, which we add to the nebulizer, moisturizes the mucous membranes of the trachea and bronchi, which suffer from drying at elevated temperatures and a strong cough in a child.
Recurrent bronchitis in a child
However, in some cases, bronchitis in a child becomes recurrent. In such cases, the outpatient tactics of pediatricians, unfortunately, often comes down to the monthly prescription of antibiotics. I have met parents of children who were given the idea by a certain doctor that their child could not get better without antibiotics. They laughed at the word inhalation and demanded from me another antibiotic for their child, like a dose for a drug addict.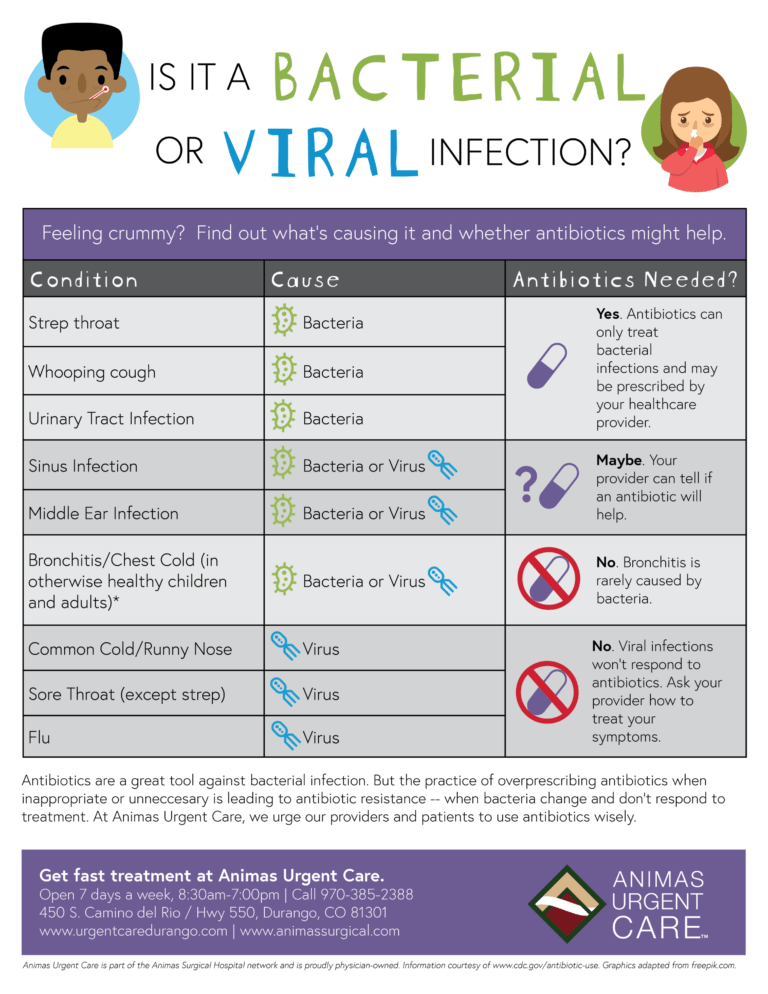
This sad case should alert you if you see that the doctor prefers the easiest, as it seems to him, way of treating bronchitis in your child, especially if this bronchitis is not the first. In this case, you may need to consult an allergist-immunologist, who will have to collect the most thorough history, that is, study the life history of not only the child himself, but also his parents, as well as grandparents at least. Further, it may be necessary to conduct a special allergological examination, since recurrent bronchitis is nothing more than a harbinger of bronchial asthma, already a chronic bronchial disease. I’ll warn you right away that we can’t always carry out the full range of necessary diagnostic procedures in a small child, so sometimes the final diagnosis is postponed by an allergist-immunologist to an older age, but the doctor can still prescribe prophylactic anti-relapse treatment, which should help both times to avoid such a diagnosis in the future. In general, based on clinical practice, I can say that even in a child under three years old, the presence of more than two episodes of obstructive bronchitis is already a reason for consulting an allergist-immunologist.