Passing of tissue in early pregnancy
Signs of Early Miscarriage | Obstetrics & Gynecology
Skip to main content
Department of Obstetrics and Gynecology
News | Careers | Giving | UC Davis Health
- UC Davis Health
- Obstetrics and Gynecology
- Miscarriage Management
- Signs of Early Miscarriage
Early miscarriage refers to loss of a pregnancy in the first trimester. The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
Miscarriage is more common than many people realize. About 10 to 20% of women who learn they are pregnant will have an early miscarriage. The rates of early miscarriage are even higher when women are checking home pregnancy tests very close to the time of their period and are finding a positive test VERY early. By chance alone, 1% to 4% of women will have two miscarriages in a row. However, it is very rare to have 3 or more miscarriages in a row, which is recurrent miscarriage.
In medical terms, early miscarriage is called an early pregnancy failure. This means that the pregnancy failed to develop. Almost all early miscarriages are due to circumstances beyond anyone’s control, and were destined to happen before the woman even knows she is pregnant.
What are the symptoms of early miscarriage?
- Bleeding – light bleeding early in pregnancy is fairly common, and does not mean you will have a miscarriage.
- Brown discharge: This may look like coffee grounds. This “discharge” is actually old blood that has been in the uterus for a while and is just coming out slowly.
- Spotting, bright red bleeding or clots
- Passage of tissue through the vagina
- A gush of clear or pink vaginal fluid
- Abdominal pain or cramping
- Pregnancy symptoms, such as breast tenderness and nausea, begin to go away
- Dizziness, lightheadedness, or feeling faint
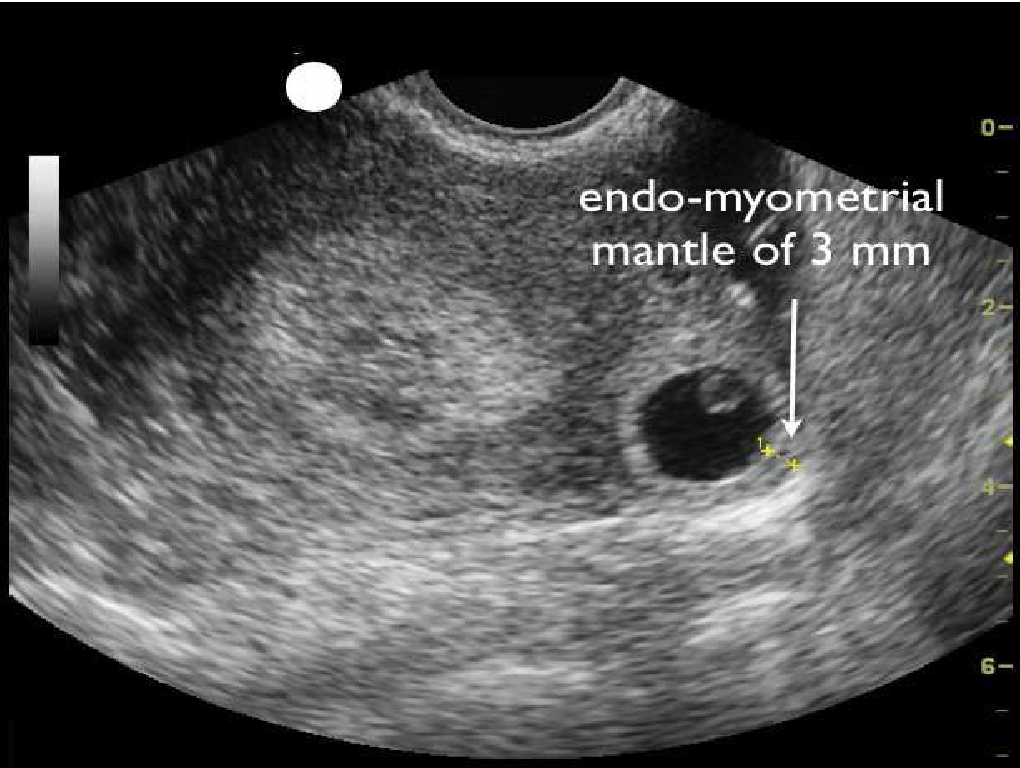
If you have any symptoms of a miscarriage, you should contact a doctor right away to have an evaluation. It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage. Even if you think you passed the entire pregnancy and are feeling better, you should see a doctor. Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage. Even if you think you passed the entire pregnancy and are feeling better, you should see a doctor. Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Types of early miscarriage
Early miscarriage is a non-medical term for lots of different types of events that might or might not actually result in pregnancy loss. The types of miscarriage include the following:
Spotting or bleeding in the first trimester in which the patient and the doctor are not yet sure if the pregnancy will miscarry or not. About 1/3 of all women will bleed in the first trimester, but only about half of those women will have a miscarriage.
The entire pregnancy is passed from the uterus, most commonly with bleeding and cramping, and no additional treatment or observation is needed.
The pregnancy is definitely miscarrying, but only some of the pregnancy tissue has passed. The tissue that is still in the uterus will eventually pass on its own. Some women may need emergency treatment if there is also heavy vaginal bleeding. Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
With this type of miscarriage, the pregnancy implanted but the embryonic tissue (the part of the pregnancy that will develop into a fetus) never developed, or started to develop and then stopped.
With this type of miscarriage, the early embryo (or fetus once 10 weeks pregnant) stops developing and growing.
This is an uncommon type of miscarriage today. With a missed abortion, the pregnancy stops developing but the pregnancy tissue does not pass out of the uterus for at least 4 weeks. Sometimes, dark brown spotting or bleeding occurs, but there is no heavy bleeding.
Some miscarriages occur with an infection in the uterus.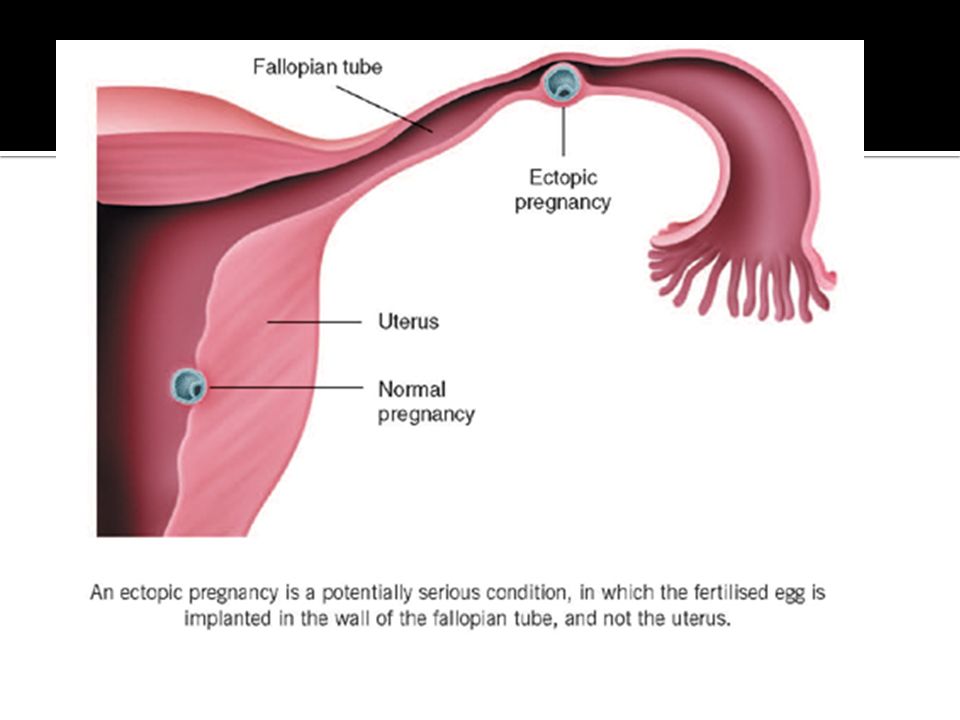 This is a serious condition that requires urgent treatment to prevent shock and death. With septic miscarriage, the patient usually develops fever and abdominal pain and may have bleeding and discharge with a foul odor. Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
This is a serious condition that requires urgent treatment to prevent shock and death. With septic miscarriage, the patient usually develops fever and abdominal pain and may have bleeding and discharge with a foul odor. Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
What causes early miscarriage?
Almost nothing you can do will cause an early miscarriage. Avoiding sex or heavy work will not impact an early pregnancy. There are a lot of changes that need to occur with the cells and genes in a developing pregnancy, and sometimes those changes do not happen perfectly. There are some health conditions or habits that can increase the chance that an early miscarriage will occur, including:
- Heavy smoking
- Use of illicit drugs, especially cocaine
- Poorly controlled diabetes
- Hyperthyroidism or hypothyroidism
- Physical problems with the uterus, including fibroids or abnormalities of development of the uterus
Why see our specialists at UC Davis Health?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately.
Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately.
If we do confirm you have a miscarriage, we can discuss expectant management or treatment options with you immediately. Should you need blood testing to evaluate the pregnancy, the laboratory is in the same building as our office.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Treatment of early miscarriage
Not all miscarriages “need” treatment. The choice of whether to wait for the pregnancy to completely pass without any treatment is up to you. Our doctors are committed to providing options for all patients, including the pros and cons of all available options when miscarriage is diagnosed. All patients with Rh-negative blood, regardless of which option they choose, need treatment with Rh-immune globulin, an injection that prevents a woman from forming substances in her blood that may attack the baby during a future pregnancy.
When a diagnosis of miscarriage is made, options include:
This means that you will not receive any treatment; just continued follow-up. In an early miscarriage, with time, most women will pass the pregnancy completely. The main issue is time – there is no way to predict exactly when this will occur. You will typically have heavy bleeding and severe abdominal cramping when the pregnancy does pass. Should you want this option, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications can be used once the pregnancy begins to pass from the uterus.
This treatment uses medicines to cause the pregnancy tissue to pass from the uterus. The medicines cause cramping and bleeding, just like what will occur with natural passing of the pregnancy tissue. Using the medicines is like expectant management, except that you know when the pregnancy is going to pass. Most women will pass the pregnancy within 24 hours of taking the medication. Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
- This brief procedure can be done in the office or the operating room. The following steps occur regardless of the location:
- The woman is in the same position as during a regular pelvic exam, like when a Pap test is done.
- A speculum is placed in the vagina
- A cleansing antibacterial solution is applied to the cervix and vagina
- Numbing medicine is applied to the cervix to decrease cramping
- The cervix is dilated (opened) with thin rods; with early miscarriage, the cervix does not need to be opened much to complete the procedure
- A thin straw-like tube is placed through the open cervixThe pregnancy is removed using a mechanical suction pump attached to the tube
- Everything is removed from the vagina when the procedure is done
You may choose to have the procedure in the office or operating room based on your preferences – different women have different needs.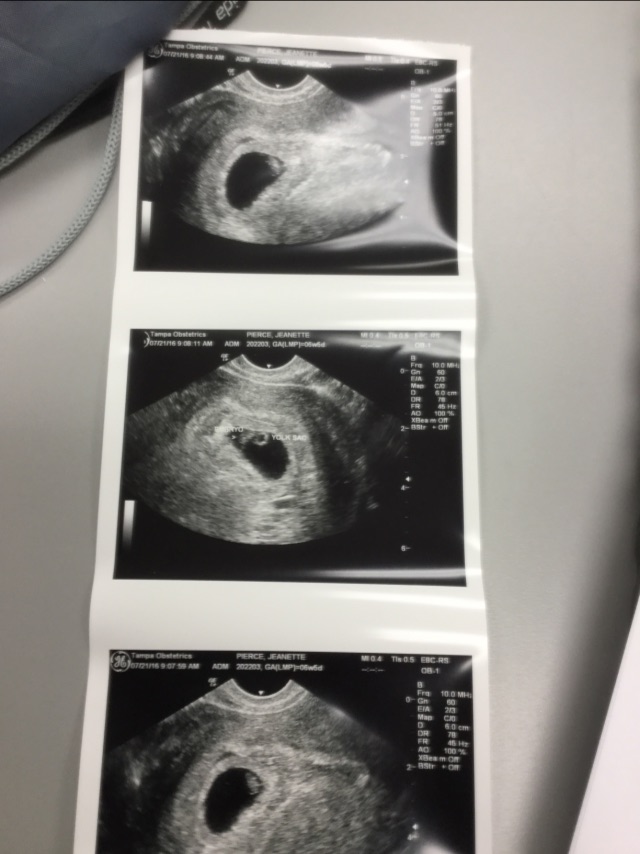
Office procedure:
- A spouse, partner, friend or relative can be in the room with you
- If desired, oral medications can be taken before the procedure to help you feel more relaxed
- You can eat or drink anything you want before the procedure
- The suction used in the office is most commonly a syringe that creates the suction so no noisy machine is used
- You will usually goes home 15-30 minutes after the procedure and can resume relatively normal activities
- Operating room procedure
- The procedure is done in an outpatient operating suite or in the main hospital
- You will be asleep during the procedure
- You cannot eat or drink anything after midnight on the night before the procedure because you will be receiving anesthesia
- You will feel sleepy for the whole day after the procedure and will need someone to be able to drive you home and be with you for the whole day after the procedure
- The operating room is more appropriate for women with certain medical conditions
After treatment for a miscarriage
Bleeding may continue for several weeks after a miscarriage but tends to be much lighter with a suction aspiration. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Frequently asked questions about miscarriage
Having one miscarriage does not increase your chances of having another. If you have had only one prior miscarriage, the rate of miscarriage in the next pregnancy is similar to the overall rate in the general population.
No. Working, exercise and sexual activity do not increase the risk of miscarriage.
Patients were told years ago to wait one or two menstrual cycles to wait to get pregnant. We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
Since most early miscarriages are caused by problems specific to that fertilized egg, and miscarriage overall is relatively common, most experts do not recommend special testing until you have had three early miscarriages (or two miscarriages in women 40 years and older). At that point it is termed "recurrent" miscarriage and further testing may be needed. Studies have shown that even after a woman has experienced three consecutive miscarriages, her chance of the next pregnancy being normal is still about 70%. All women who have a pregnancy loss later in pregnancy should have further testing.
Tips to help support parents after pregnancy loss
UC Davis Health social worker Brenna Rizan, who works within the Department of Obstetrics/Gynecology provides supportive tips and advice for grieving parents, family and friends after pregnancy loss.
Related stories
Miscarriages are more common than people think - KCRA (Interview with Brenna Rizan)
Facebook Live: Discussing miscarriages with Dr. Mitch Creinin
UC Davis Early Pregnancy and Miscarriage Center
What does a miscarriage look like? Symptoms and seeking help
Miscarriage, or pregnancy loss, can look and feel different for each person. Common symptoms include bleeding and cramping.
It is important to note that bleeding is common during pregnancy — especially in early pregnancy. It does not necessarily mean that anything is wrong.
The only way to accurately identify a pregnancy loss is to test pregnancy hormone levels and have an ultrasound of the uterus.
Read on to learn more about what pregnancy loss can look and feel like.
According to a 2016 study, not all pregnancy losses involve bleeding. Overall, they do not follow a single pattern. This is why it is crucial to seek medical care for bleeding and any unusual symptoms during pregnancy.
Pregnancy loss during the first trimester may involve:
- heavy bleeding
- bleeding that starts light and gets heavier
- passing blood clots or tissue
- cramping, which may come in waves
- a gush of fluid from the vagina
If a person takes a pregnancy test after experiencing a pregnancy loss during the first trimester, the result may be negative, or the test may have a positive line that gets fainter.
Experiencing pregnancy loss later in the first trimester and beyond will involve passing more tissue.
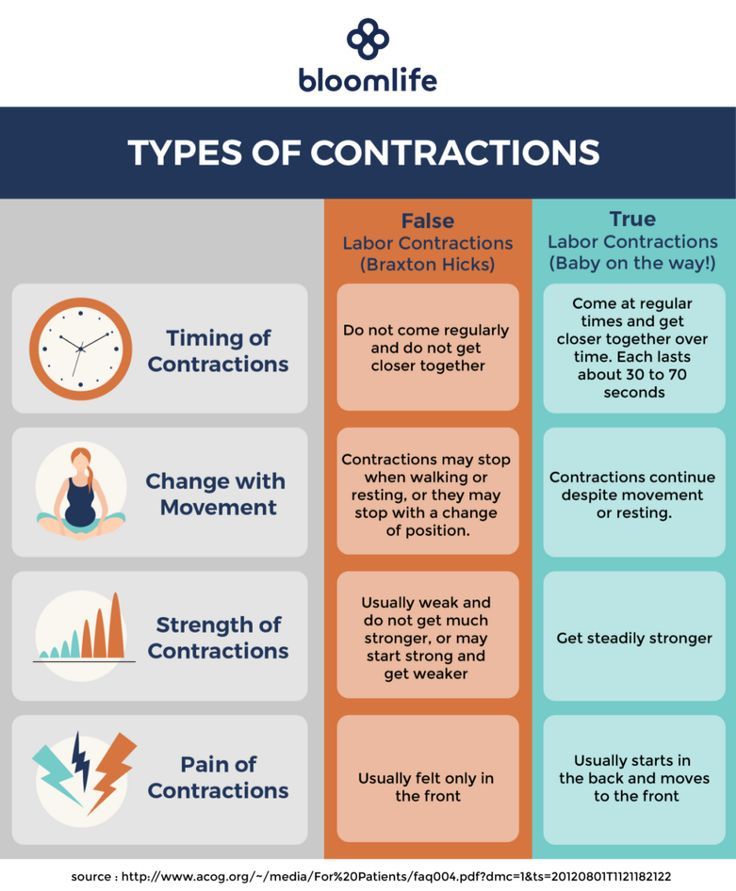
Second-trimester pregnancy loss can also cause intense cramping and sometimes even contractions.
In addition to bleeding and cramping, some people may notice larger blood clots.
According to a 2019 meta-analysis, one-quarter of pregnant women experience bleeding during the first trimester. Another study from 2016 puts that percentage higher, at closer to 20–40%.
A large-scale 2010 study found that about 12% of pregnant women experienced pregnancy loss, and about two-thirds of that group reported bleeding during their pregnancy.
Some differences between bleeding due to a pregnancy loss and other types of bleeding during pregnancy include:
- Amount of blood: Heavy bleeding is more likely to signal a pregnancy loss.
- Bleeding pattern: Bleeding that gets progressively heavier may indicate a pregnancy loss.
- Pain: Cramping, especially when it occurs in a clear pattern, is more likely to signal a pregnancy loss.
- Passing tissue: Some — not all — people who experience a pregnancy loss pass large blood clots or tissue.
For people who do experience bleeding during a pregnancy loss, the duration tends to depend on how far the pregnancy has progressed.
Pregnancy losses that occur in the first weeks of pregnancy tend to cause bleeding that lasts a few days. Those that occur later may cause bleeding that lasts for as long as 4 weeks.
Sometimes, the bleeding stops and starts again. Over time, it should get lighter.
A very early pregnancy loss is sometimes called a chemical pregnancy. These pregnancies are lost shortly after the embryo implants, usually within a few days or weeks.
A chemical pregnancy may be detectable by a pregnancy test, but it would likely not be seen on an ultrasound.
In many cases, early pregnancy losses can happen before a person knows they are pregnant.
In fact, around 80% of early pregnancy losses occur in the first trimester, or in weeks 0–13. The end of these early pregnancies may be mistaken for a period because the symptoms are similar.
For example, both a period and an early pregnancy loss can involve bleeding and cramping. Pregnancy tissue that passes out of the vagina may look like typical blood clots that occur during a period.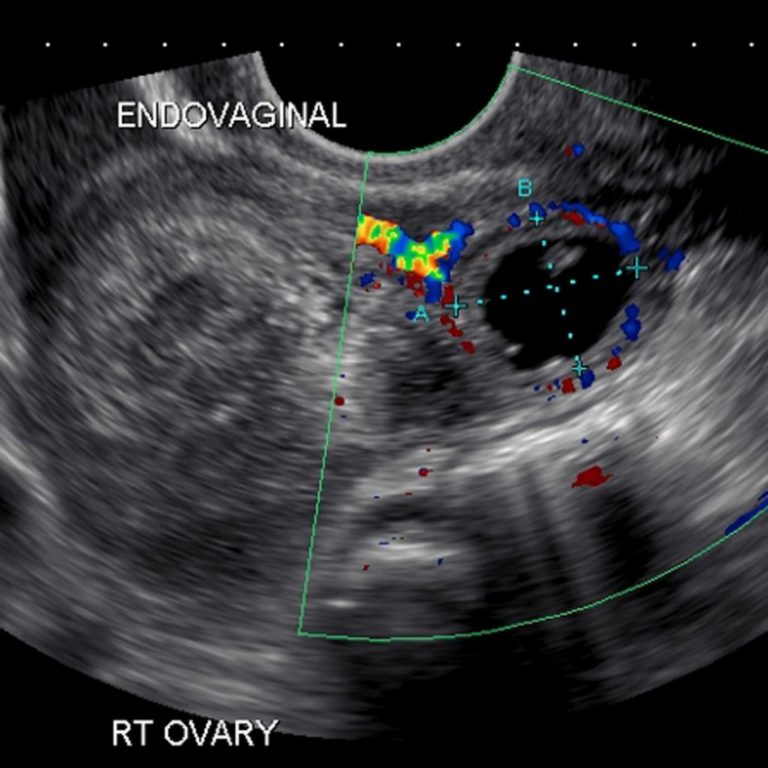
It is possible that a person will not realize they have missed a period. Instead, they may mistake the symptoms of a pregnancy loss for those of a menstrual period.
Pregnancy losses and periods can both cause:
- vaginal bleeding
- passing blood clots or tissue
- abdominal pain
However, a pregnancy loss will often cause additional symptoms that set it apart from a period, especially if the pregnancy loss occurs several weeks into the pregnancy. These symptoms include:
- larger clots or pregnancy loss tissue
- more clots than typical periods
- lower abdominal cramping
- back pain
- passing a significant amount of clear or pinkish fluid
- sudden heavy bleeding, or heavier bleeding than a typical period
- longer bleeding
- sudden easing of some early pregnancy symptoms, such as nausea and breast tenderness
It is important to remember that bleeding during the first weeks of a pregnancy is not uncommon, and it is not always a sign of pregnancy loss or a problem with a pregnancy.
However, if a person experiences other symptoms of pregnancy loss, they should seek care from a doctor.
A “missed miscarriage” refers to a delay between the loss of the pregnancy and any bleeding or passing of tissue.
During a missed miscarriage, an embryo dies but does not leave the uterus for several weeks. In fact, a pregnant person may not realize the pregnancy has ended until an ultrasound finds no heartbeat.
When the embryo does leave the uterus, the blood, tissue, and clots may be dark brown. The tissue has had time to deteriorate, so bright red blood or heavy bleeding may not occur. The bleeding may last several days to several weeks.
A doctor may prescribe medication to help the person who has had the pregnancy loss bleed and pass the tissue. Surgery may also be necessary.
It is not possible for healthcare professionals to stop a pregnancy loss once it starts.
Call a doctor and schedule an appointment within 24 hours if any of the following occur:
- vaginal bleeding
- a fever
- intense pain or cramping
- bleeding that stops and starts again
- any other changes in the pattern of bleeding, even if a doctor has already addressed the cause
- bleeding that lasts for longer than 7 days, even if a doctor has already confirmed pregnancy loss
Pregnant people should receive emergency medical attention if they:
- experience heavy bleeding during the second trimester and cannot reach their doctor
- bleed heavily enough to soak through more than one pad per hour for more than 2 hours
- feel faint, lightheaded, or confused
- experience contractions, amniotic fluid leakage, the water breaking, or other signs of premature labor
Most pregnancy losses pass on their own.
In some cases, the fetus dies without causing any bleeding. When this happens, the person carrying the fetus may want to wait for the pregnancy to pass on its own or want it to be over as quickly as possible.
If a person wants to expedite a pregnancy loss, a doctor can supply medication that helps with passing the pregnancy at home. This approach is safest during early pregnancy.
A healthcare professional can also perform surgery to remove the remains of the embryo or fetus.
Sometimes a pregnancy loss is incomplete, leaving behind tissue that can lead to infection or other health problems. When this happens, a doctor may recommend medication or surgery.
Doctors used to advise couples to wait 1 month, or sometimes much longer, before trying to conceive again after a pregnancy loss.
However, research now shows that there is no medical justification for this recommendation. If a couple feels ready, it is safe to begin trying to conceive again right away.
A 2017 study indicates that fertility may even be slightly higher immediately following a pregnancy loss.
Sometimes, however, it takes a while for a menstruating person’s cycle to resume following a pregnancy loss.
This can make it difficult to time sexual intercourse for conception and to accurately date a pregnancy — especially if a person becomes pregnant before the first menstrual period after a pregnancy loss.
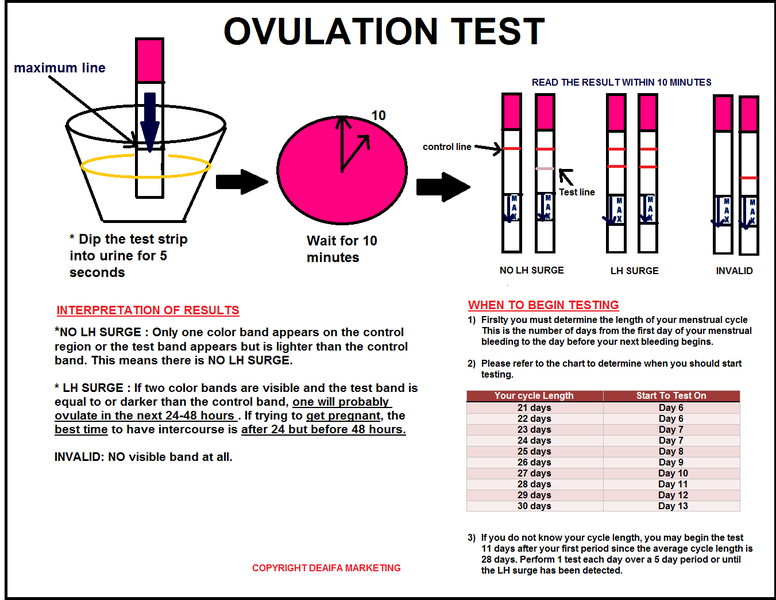
To improve accuracy, it can be helpful to:
- monitor basal body temperature
- use ovulation tests
- try other ways to predict fertility
Early pregnancy losses can sometimes result from chromosomal irregularities. This means that the developing embryo or fetus has an irregular number of chromosomes.
These irregularities usually occur at random, meaning they are unlikely to reoccur. In other words, experiencing one pregnancy loss does not increase the likelihood of experiencing another.
A 2017 study finds that 15. 7% of women with a previous pregnancy loss had another during the 2-year study period.
7% of women with a previous pregnancy loss had another during the 2-year study period.
Meanwhile, a 2016 study finds that women were more likely to become pregnant in the 3 months following a pregnancy loss.
Many people become pregnant again shortly after a pregnancy loss, and a smaller number experience multiple losses in a row.
The risk of repeat pregnancy losses increases with age, according to a 2019 study. The risk is also higher among people with a history of:
- preterm labor
- gestational diabetes
- stillbirth
- cesarean delivery
A 2017 study found that 15.7% of participants whose most recent pregnancy ended in a pregnancy loss went on to have a second pregnancy loss.
A 2018 study focused on women who had three or more pregnancy losses. This study found that 64.5% of those women had a live birth within 5 years. Some of these participants may have received fertility treatments.
Pregnancy loss is one of the less common causes of bleeding during pregnancy, especially when the bleeding occurs early on.
But bleeding in early pregnancy is not always a sign of pregnancy loss.
Some other signs of pregnancy loss include cramping and passing blood clots or tissue.
Only a healthcare professional can accurately identify a pregnancy loss. For this reason, it is important to consult a doctor or nurse midwife about any bleeding during pregnancy.
What does an early miscarriage look like?
Bleeding is common in the early weeks of pregnancy. That is why bleeding alone should not be seen as an indication of an early pregnancy loss.
In addition to bleeding, an early pregnancy loss may cause a person to experience:
- a gush of clear or pale pink fluid from the vagina
- passing blood clots or tissue
- a sudden decrease in pregnancy symptoms (such as nausea and morning sickness)
- a negative result on a pregnancy test, or a positive sign that is very faint
How do I know if I’m miscarrying?
The signs and symptoms of a pregnancy loss will remain largely the same, no matter the week. But the further along a person is, the greater the amount of tissue loss during the miscarriage.
But the further along a person is, the greater the amount of tissue loss during the miscarriage.
Symptoms of pregnancy loss include:
- sudden bleeding, sometimes heavy
- a gush of clear or pink fluid from the vagina
- mild to severe back pain and abdominal cramping
- contraction-like pain
What does miscarriage tissue look like?
The clots and tissue passed during a pregnancy loss may look like typical period clots, or they may be larger.
Pregnancy loss tissue includes:
- the fetus or embryo
- gestational sac
- placenta
When a pregnancy is more advanced (after 6 to 8 weeks), the gestational sac may be noticeable. Before that, it may be too small to see.
The tissue passed during a pregnancy loss may be:
- brown
- black
- dark red
- bright red or pink
- white or gray, in some cases
If the pregnancy began to deteriorate before the start of bleeding, the clots may be smaller and darker. This is common with a missed miscarriage.
This is common with a missed miscarriage.
What does miscarriage tissue vs. a blood clot look like?
It is not always easy to tell the difference between pregnancy loss tissue and a blood clot. Both may look like typical period clots, though it is not uncommon for them to be larger than normal.
Actual pregnancy tissue may not be discernible until after the eighth week. Then, the tissue may look like pink, white, or gray tissue. A person may also be able to see a fluid-filled sac in the passed tissue.
Save at all costs: reasons for abortion
January 17, 2017 Articles on gynecology
According to Wikipedia, 15-20% of clinically diagnosed pregnancies end in spontaneous abortion. These numbers are a lower estimate, as many miscarriages occur in the early stages, before the woman knows she is pregnant. After all, often the clinical signs of a miscarriage are mistaken for heavy periods or for their delay.
What are the reasons for termination of pregnancy at different stages? How to prepare for pregnancy after a bad experience that ended in a miscarriage? These questions were answered by an obstetrician-gynecologist of the highest category at Bullfinch Medical Center ALEXANDER GIL.
- Alexander Vadimovich, most miscarriages happen at the beginning of pregnancy, and many women are perplexed: why could this happen?
- The main cause of miscarriages before 6 weeks is natural selection. There is a laying of pregnancy with congenital malformations of the embryo, which is no longer viable - thus, natural selection is carried out, in which we cannot interfere.
You will never know the exact cause of a miscarriage at this time, even if after abrasion (curettage of the uterine mucosa), the contents are sent for research. As a rule, the answer comes: “short-term pregnancy” and nothing more.
There is another reason for termination of pregnancy, especially if it is not the first one - Rh-conflict (when a woman has Rh-negative blood, and men - Rh-positive). But in our country, effective prevention of the Rh conflict is used, so that troubles can be avoided at the stage of pregnancy planning.
But in our country, effective prevention of the Rh conflict is used, so that troubles can be avoided at the stage of pregnancy planning.
In the structure of early termination of pregnancy, no one excludes infections and problems associated with hormones. At a period of 6-8 weeks, promising pregnancies are often interrupted due to a lack of hormones. During normal pregnancy, a woman has a so-called corpus luteum in one of the ovaries, which produces endogenous progesterone.
Unfortunately, the functioning of the corpus luteum ends by about 7 weeks of pregnancy, and if initially there was not enough endogenous progesterone, the pregnancy stops developing: the fetal egg detaches and the so-called missed pregnancy occurs.
In some cases, with detachment of the fetal egg, pregnancy can be saved, the main thing is to contact a specialist in time. If, based on the results of ultrasound studies, the doctor sees that the embryo is still alive, pregnant women are prescribed exogenous progesterone in tablets or suppositories. This hormone also exists in the form of injections - it is used to saturate the body faster and prevent miscarriage.
This hormone also exists in the form of injections - it is used to saturate the body faster and prevent miscarriage.
- Agree, when a woman becomes pregnant, she cannot suspect that she does not have enough progesterone in her body. What should be her concern? What signs indicate this?
- Any discharge from scanty dark brown to more profuse bloody is a bad sign. You should not hesitate to contact a gynecologist.
If spotting appears, an ultrasound examination, a blood test for progesterone is indicated.
I want to say that lack of progesterone can cause miscarriage up to 15 weeks. At 15-16 weeks, the placenta is finally formed, which will secrete (produce) this hormone.
- Alexander Vadimovich, what problems can arise with the placenta during pregnancy?
- In the early stages, the chorion (unformed placenta) can block the internal os, maybe its marginal location - this is a big risk of abortion. In this case, the woman is admitted to the hospital and observed for up to 16 weeks - by this time, the chorion, as a rule, rises. But there remains a percentage of pregnant women in whom the placenta overlaps the cervix of the uterus - this is called the "central location of the placenta." To maintain pregnancy, such women, as a rule, must be in the clinic and under observation all the time.
In this case, the woman is admitted to the hospital and observed for up to 16 weeks - by this time, the chorion, as a rule, rises. But there remains a percentage of pregnant women in whom the placenta overlaps the cervix of the uterus - this is called the "central location of the placenta." To maintain pregnancy, such women, as a rule, must be in the clinic and under observation all the time.
— What is the treatment for infections that appear during pregnancy?
- Infections can occur even in women who were carefully examined before pregnancy. Often this problem occurs due to spotting - this is a favorable environment for the development of infections.
Ectopia (erosion) of the cervix is also an infection that is a clear threat to pregnancy. Therefore, it is so important to undergo a colposcopy before conception and be treated for ectopia, if it is detected.
Infection by the ascending route can penetrate in utero and adversely affect the health of the fetus.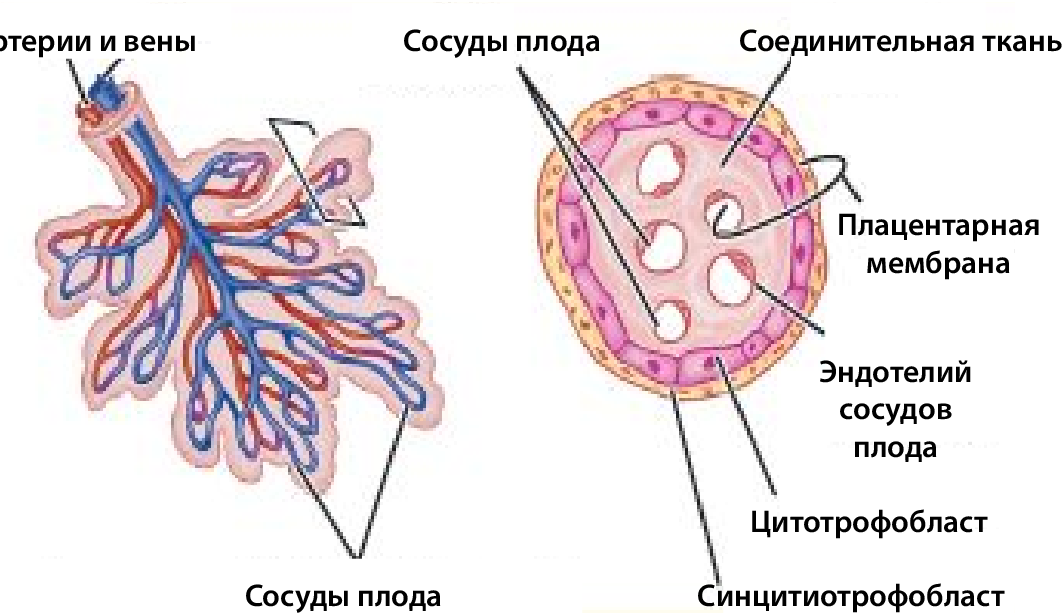 There is such a complication as intrauterine fetal pneumonia, which is treated very poorly and occupies a large percentage in the structure of infant mortality.
There is such a complication as intrauterine fetal pneumonia, which is treated very poorly and occupies a large percentage in the structure of infant mortality.
And we treat infections whenever possible in any way that is prescribed in the protocol. There is such a tactic, which is to take antibiotics. There is no need to be afraid of them, as the doctor will prescribe only medicines approved for pregnant women. Sometimes you have to use those drugs, the benefits of which are greater than the risk of adverse reactions.
— What threats can affect a mid-term pregnancy?
— Among the many causes that lead to spontaneous miscarriages is isthmic-cervical insufficiency. This is a condition in which the isthmus and cervix cannot cope with the increasing load (growing fetus, amniotic fluid), begin to open - and the baby is born prematurely.
There are indications for the prevention of this condition - the imposition of a circular submucosal suture on the cervix. The best time is 16-17 weeks. You can do this procedure after 20 weeks, but the effect will be less.
The best time is 16-17 weeks. You can do this procedure after 20 weeks, but the effect will be less.
In the middle of pregnancy, a placental abruption can occur in a woman. In some cases, pregnancy can be saved with the help of drugs that affect blood clotting. But often doctors are forced to resort to a small caesarean section. As a rule, childbirth before 22 weeks ends in the death of the fetus, and here we are already talking about saving the life of the mother.
I encourage pregnant women to refrain from flying. In my medical practice, there have been several cases where placental abruption in patients occurred during a flight. Who will provide you with qualified assistance in this case? I advise you not to take risks.
In Belarus, as in other European countries, labor begins at 22 weeks, but it is considered premature. Doctors are doing everything possible to save a promising pregnancy by any means. The main thing is to always be under the supervision of a specialist and follow all his recommendations.
- Alexander Vadimovich, unauthorized termination of a desired pregnancy is always a great psychological trauma for a woman. No one wants to experience this again. What are the features of preparing for the next pregnancy after a miscarriage?
— Before thinking about re-pregnancy, it is advisable for women who experience mental anguish to undergo a course of psychotherapy. This is very important, because mental problems can be very serious, especially in women after unsuccessful in vitro fertilization (IVF).
The main rule: do not get pregnant after a miscarriage for 6 months. It is best to protect yourself at this time with oral contraceptives, which the doctor will prescribe. This is necessary in order to restore normal reproductive function.
A set of examinations for women who have had a miscarriage is ordered individually. But the general recommendations are:
1. Diagnosis of sexually transmitted infections: mycoplasmosis, ureaplasmosis, chlamydia, herpes simplex virus, human papillomavirus (HPV).
You should also be screened for infections that may have caused a miscarriage in a previous pregnancy.
2. Test for sex hormones - if prescribed by a doctor.
3. Thyroid hormones (TSH, T4 free, ATPO), ultrasound of the thyroid gland, consultation with an endocrinologist.
4. If necessary, consultation of a therapist and other specialists, a blood test for sugar, syphilis, HIV.
5. Ultrasound of the abdomen and kidneys. During pregnancy, many chronic diseases are exacerbated, incl. and kidney disease. You need to be treated before conception.
6. Colposcopy (examination of the cervix under a microscope).
7. Analysis of the spermogram of the partner.
An examination by a geneticist is indicated if, when planning a pregnancy, a woman is 36 years old, and a man is 45 years old and over. Also, this doctor should be visited by a couple who had two non-developing early pregnancies in a row.
Another tip from practice. Many women, having barely become pregnant, rush to confirm this on an ultrasound. Of course, there is no direct evidence that such research is harmful to the fetus, but there is also no evidence to the contrary that it is absolutely harmless. Since you so desire this pregnancy, it’s not worth the risk, and a competent doctor will definitely warn a woman against doing an early ultrasound without any special indications.
Of course, there is no direct evidence that such research is harmful to the fetus, but there is also no evidence to the contrary that it is absolutely harmless. Since you so desire this pregnancy, it’s not worth the risk, and a competent doctor will definitely warn a woman against doing an early ultrasound without any special indications.
Pregnancy and its prospects can be determined using a blood test for hCG (human chorionic gonadotropin), or, more simply, the pregnancy hormone. It is absolutely harmless for pregnancy. It is advisable to donate blood at the beginning of the delay, a week later - again. If the increase in hCG is normal, then the pregnancy is promising, not ectopic - and there are no indications for ultrasound.
For the first time, a woman should come for ultrasound diagnostics at 11-12 weeks of pregnancy. Alexander Vadimovich Gil
March 29, 2022 Articles on gynecology
Frequency of examinations by a gynecologist
July 20, 2020 Articles on gynecology
MVS in elderly patients
Population aging is one of the global problems. The increase in life expectancy and the decrease in the birth rate in one way or another leads to the aging of nations. In this regard, questions arise regarding improving the quality of life of the elderly and senile people.
The increase in life expectancy and the decrease in the birth rate in one way or another leads to the aging of nations. In this regard, questions arise regarding improving the quality of life of the elderly and senile people.
June 8, 2020 Gynecology articles
5 facts about physical activity to help you get started
Hypodynamia is a problem of the 21st century. Both adults and children suffer from lack of activity. Modern lifestyle, the popularity of the Internet and the prevalence of remote technologies lead to an annual decrease in physical activity in people around the world. It has long been proven that physical inactivity is a risk factor for the development of many diseases. Low activity provokes mental disorders, cancer, reduces the quality and life expectancy!
Premature placental abruption: what expectant mothers need to know and how not to miss its signs | Blog
First, let's talk about what is the placenta?
The placenta is the fetal organ that connects the mother and child.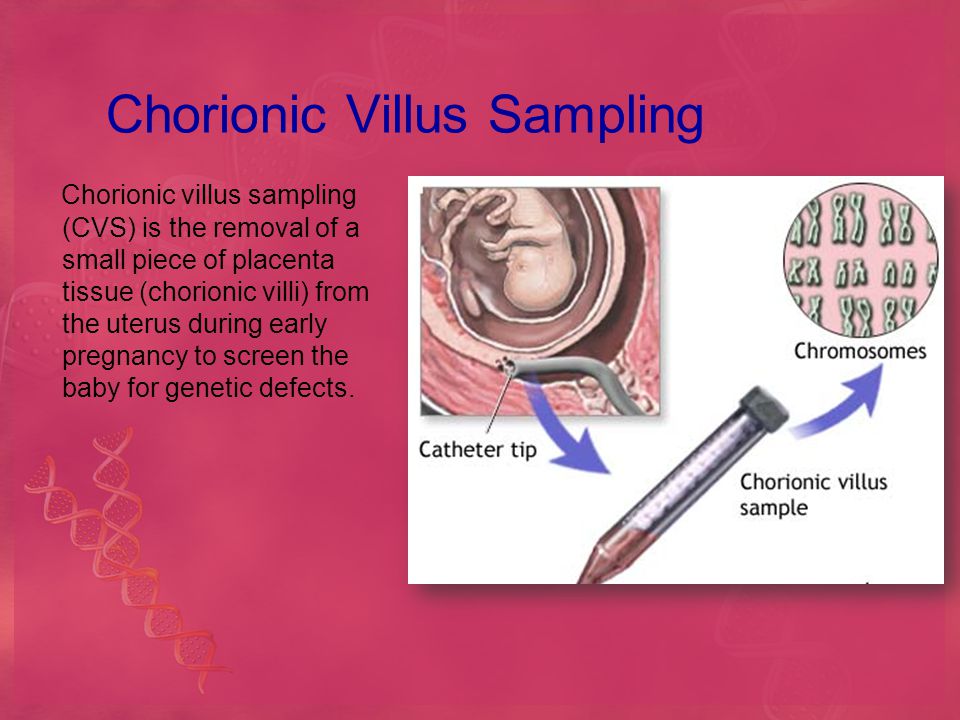 Its uniqueness lies in the fact that it is the only "disposable" organ. The placenta begins to develop from the 2nd week of pregnancy, forms up to 15-16 weeks and reaches full functional maturity by 36 weeks. And after the birth of the fetus (in the third stage of childbirth), it separates and leaves the mother's body, starting the process of lactation at the endocrinological level.
Its uniqueness lies in the fact that it is the only "disposable" organ. The placenta begins to develop from the 2nd week of pregnancy, forms up to 15-16 weeks and reaches full functional maturity by 36 weeks. And after the birth of the fetus (in the third stage of childbirth), it separates and leaves the mother's body, starting the process of lactation at the endocrinological level.
The placenta performs important functions such as gas exchange, nutrient exchange between the mother and the child, provides immunological protection and works as an endocrine gland, producing hormones necessary for the development of the fetus and the normal course of pregnancy. Every minute, about 500 ml of blood enters the placenta, but at the same time it is a kind of barrier that does not allow the blood of the mother and child to mix, and also prevents many toxic substances from entering the bloodstream of the baby.
In this article we will talk about placental abruption.
This condition is quite rare (up to 1. 5% of all pregnancies), but causes such threatening complications as massive bleeding and hemorrhagic shock, fetal distress, which in some cases can cause death. Normally, the detachment of the placenta from the inner wall of the uterus occurs only after the birth of the fetus. If this happens before the onset of labor, as well as in the first or second stage of labor, this is the premature detachment of a normally located placenta. This condition is a very dangerous pathology that requires immediate diagnosis and decision of further medical tactics in the near future.
5% of all pregnancies), but causes such threatening complications as massive bleeding and hemorrhagic shock, fetal distress, which in some cases can cause death. Normally, the detachment of the placenta from the inner wall of the uterus occurs only after the birth of the fetus. If this happens before the onset of labor, as well as in the first or second stage of labor, this is the premature detachment of a normally located placenta. This condition is a very dangerous pathology that requires immediate diagnosis and decision of further medical tactics in the near future.
Causes of premature placental abruption
The only cause of premature placental abruption, unfortunately, has not been established to date. There are many theories, but in general, the occurrence of this condition is associated with many provoking factors.
Major risk factors include:
- arterial hypertension,
- diabetes mellitus
- pregnant age over 40
- multiple pregnancy
- polyhydramnios
- postterm pregnancy and large fetus
- past uterine surgery
- blood clotting disorder,
- autoimmune diseases
- kidney disease
- bad habits such as smoking and drug use
- inflammatory diseases of the uterus and placenta, anomalies in the development of the uterus.
Causes that can provoke placental abruption: physical trauma of a pregnant woman (accident, fall, blow to the stomach), disruption of the contractile activity of the uterus, stress, gross obstetric manipulations.
Types of placental abruption
There are the following types of placental abruption: partial and complete.
Partial detachment, in turn, can be central and marginal.
Why is this classification so important? And because both the clinical picture and medical tactics depend on the place and volume of the detachment. Partial detachment can be progressive or non-progressive.
Non-progressive detachment has a significantly better prognosis for a pregnant woman, because in this case, conservative treatment is possible with preservation of pregnancy.
Symptoms of placental abruption:
Here is a triad of main symptoms that may be a sign of placental abruption:
- abdominal pain, feeling of increased uterine tone;
- bleeding from the genital tract;
- violation of the fetal heartbeat, indicating fetal distress.
Also, a woman can feel the baby's reaction to a decrease in the amount of oxygen supplied to him due to placental abruption - he begins to move more actively, reacting to hypoxia.
These symptoms do not always appear at the same time! For example, with marginal abruption of the placenta, blood flows into the vagina, which means that the woman sees signs of bleeding. With central detachment, a retroplacental hematoma is formed. Bleeding is internal, which means that a pregnant woman may not notice its signs. The appearance of an accelerated heartbeat in a woman, a decrease in blood pressure, nausea, dizziness, and severe weakness may indicate internal bleeding.
However, with central placental abruption, blood accumulates in front of the placenta and begins to “press” on nearby tissues. As a result, a pronounced pain syndrome occurs.
It must be emphasized that if at least one of the symptoms appears, it is necessary to immediately inform the doctor about this! This condition can be very dangerous for you and your baby, so it is important to diagnose it in a timely manner.
Diagnosis of placental abruption
Diagnosis of placental abruption is based not only on clinical symptoms and gynecological examination. Ultrasound diagnostics is the main method that allows you to accurately assess the location and area of the exfoliated area of the placenta and see the presence or absence of a hematoma. Also, ultrasound can distinguish premature detachment from placenta previa (its abnormal location, in which it overlaps the internal pharynx of the cervix). This condition can have similar symptoms, as it is often accompanied by bleeding. The condition of the fetus and the degree of its hypoxia will be determined using cardiotocography, and Dopplerography, in turn, assesses violations of the uteroplacental circulation. Based on these examination results, the obstetrician-gynecologist, and more often a council of doctors, decides on the type of further medical tactics.
Treatment of placental abruption
Treatment of placental abruption always requires hospitalization of the pregnant woman in the maternity hospital for constant monitoring of her condition. In cases of non-progressive mild placental abruption with a stable state of the mother and fetus, conservative tactics with drug therapy and preservation of pregnancy are possible. Progressive detachment, as well as severe detachment, certainly requires an emergency caesarean section.
In cases of non-progressive mild placental abruption with a stable state of the mother and fetus, conservative tactics with drug therapy and preservation of pregnancy are possible. Progressive detachment, as well as severe detachment, certainly requires an emergency caesarean section.
In the case of complete detachment of the placenta, with the rapid progression of this condition, massive bleeding occurs, which threatens the life of both the pregnant woman and the child. In such a situation, surgeons always prioritize the life of a woman and do everything necessary to save her. Some cases may, unfortunately, require even such radical surgical tactics as removal of the uterus. However, at the current level of development of medicine, more and more technologies are emerging that, with timely assistance, can save not only the life of the mother and child, but also the reproductive functions of a woman. In particular, our obstetrician-gynecologists and anesthesiologists use up-to-date international medical protocols to ensure the safest possible delivery.