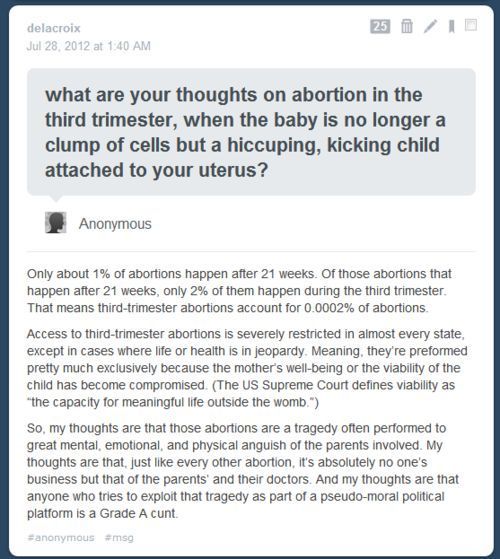
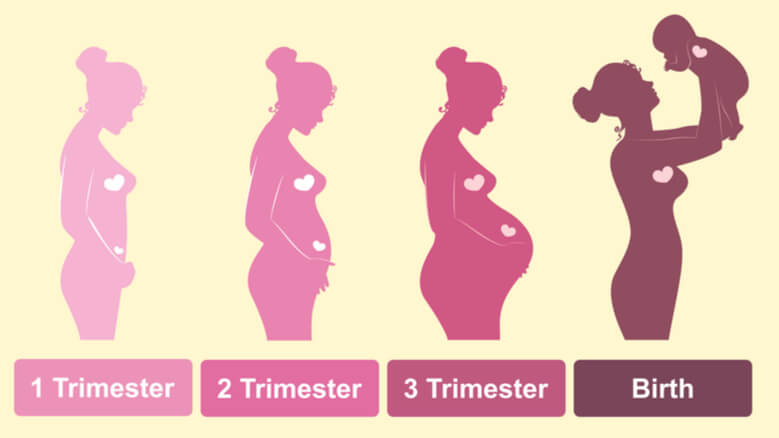
When does the 3 trimester start
28 Weeks Pregnant | Pregnancy
Welcome to the 3rd trimester! Pregnancy is divided into 3 stages, known as trimesters…. and you're now in the 3rd stage. Over the next few weeks, you will probably start to feel a bit more uncomfortable and tired.
What's happening in my body?
You may be getting a bit of heartburn and indigestion. That's down to your growing baby and hormones affecting your digestive system.
Your back will also be under strain, due to the extra weight you're carrying around. Your joints and ligaments will also be looser than usual.
Your ankles, feet and face could be puffing out a bit, particularly when it's hot. This is probably due to water retention, but get it checked out, just in case it's pre-eclampsia. This is a condition where you may feel perfectly well, but then your blood pressure can get dangerously high, very quickly.
Rest can help with a lot of your symptoms, so make sure you get lots of it. But if you are worried about anything at all, talk to your midwife or doctor, or call NHS 111.
3 ways to bust germs
Make sure you know about some of the harmful infections in pregnancy, so that you can do your best to avoid them.
Here are 3 ways you can protect your unborn baby…
-
Wash your hands regularly with soap and water for at least 20 seconds, particularly if you're in contact with children or nappies, as they could carry a virus called CMV (cytomegalovirus).
-
If you have a cat - wear gloves when emptying the cat litter tray, or ask someone else to deal with it. That's because cat poo can contain a bug that causes the dangerous toxoplasmosis infection. You should also wear gloves when gardening, in case you come into contact with animal poo.
-
If you have not had chickenpox let your doctor or midwife know if you come into contact with anyone who could be infectious. The disease can be spread up to 2 days before spots appear, until 5 days afterwards. It's safest for you when there are no new blisters or moist crusts on the spots.
If you're worried about coronavirus, have a look at the guidance from Royal College of Obstetricians and Gynaecologists on coronavirus and pregnancy.
Nosebleeds
Nosebleeds are common in pregnancy, due to hormonal changes, and can even strike when you're asleep. Here's what you can do:
- sit or stand up - don't lie down
- pinch your nose just above your nostrils for 10 to 15 minutes
- lean forward and breathe through your mouth
- put an icepack (or a bag of frozen peas wrapped in a tea towel) at the top of your nose
Read more tips for stopping nosebleeds.
3rd trimester pregnancy symptoms (at 28 weeks)
You may start getting new symptoms now, such as nosebleeds and indigestion.
Your signs of pregnancy could also include:
- sleeping problems (week 19 has information about feeling tired)
- stretch marks (read about stretch marks on week 17's page)
- swollen and bleeding gums (week 13 has information about gum health during pregnancy)
- pains on the side of your baby bump, caused by your expanding womb ("round ligament pains")
- piles (read about piles on week 22's page)
- headaches
- backache
- nosebleeds
- indigestion and heartburn (week 25 talks about digestive problems)
- bloating and constipation (read about bloating on week 16's page)
- leg cramps (week 20 explains how to deal with cramp)
- feeling hot
- dizziness
- swollen hands and feet
- urine infections
- vaginal infections (see week 15 for vaginal health)
- darkened skin on your face or brown patches – this is known as chloasma or the "mask of pregnancy"
- greasier, spotty skin
- thicker and shinier hair
You may also experience symptoms from earlier weeks, such as:
- mood swings (week 8's page has information on mood swings)
- morning sickness (read about dealing with morning sickness on week 6's page)
- weird pregnancy cravings (read about pregnancy cravings on week 5's page)
- a heightened sense of smell
- sore or leaky breasts (read about breast pain on week 14's page) - a white milky pregnancy discharge from your vagina and light spotting (seek medical advice for any bleeding)
Read Tommy's guide to common pregnancy symptoms.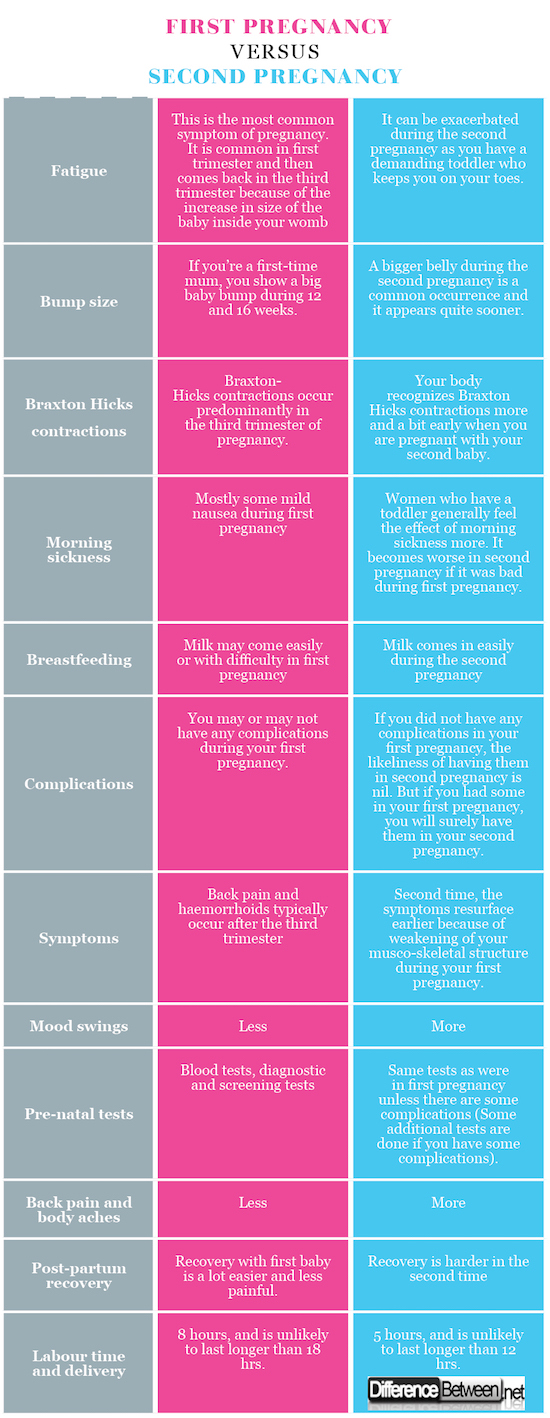
What does my baby look like?
Your baby, or foetus, is around 37.6cm long from head to heel, and weighs about 1kg. That's approximately the size of a pineapple, and the weight of a big bag of brown sugar.
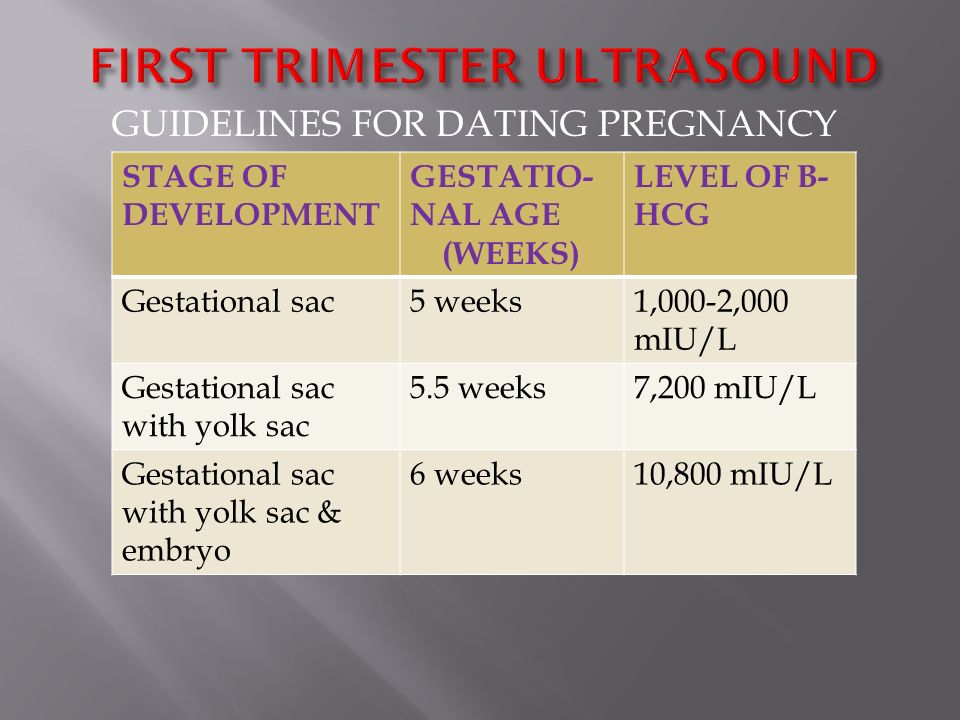
Your baby's heart rate is changing all the time. Around week 5 or 6, when it was first detectable, it was around 110 beats per minute (bpm). Then it soared to around 170 bpm in week 9 and 10. Now, it's slowed down to around 140 bpm and it will be around 130 bpm at birth.
That's still a lot faster than your heart rate, which will be around 80 to 85 beats per minute. This is partly because babies' hearts are so small that they can't pump much blood, but they can make up for this by going faster. It also helps to keep them warm.
Your baby's heart can be heard through a stethoscope. Someone else might be able to hear it by putting an ear to your pregnant belly – give it a go, but it's tricky finding the right spot.
Action stations
It's time to work out where your baby will sleep, and it's best to do this sooner, rather than later, before you start running out of energy. Your baby will spend a lot of time in a cot, so make sure it's safe. If you're buying a new cot, look for the British Standard mark BS EN 716-1. Read more about what you need for your baby.
Your baby will spend a lot of time in a cot, so make sure it's safe. If you're buying a new cot, look for the British Standard mark BS EN 716-1. Read more about what you need for your baby.
This week you could also...
You have maternity rights. You can ask for a risk assessment of your work place to ensure that you're working in a safe environment. You should not be lifting heavy things and you may need extra breaks and somewhere to sit. You can also attend antenatal appointments during paid work time.
It's a good time to tone up your pelvic floor muscles. Gentle exercises can help to prevent leakage when you laugh, sneeze or cough. Get the muscles going by pretending that you're having a wee and then stopping midflow. Visit Tommy’s for more ideas about pelvic floor exercises.
Ask your midwife or doctor about online antenatal classes – they start around now. The charity Tommy's has lots of useful information on antenatal classes and preparing you for birth.
Even if you've had children before, they're still worth going to as you can meet other parents-to-be.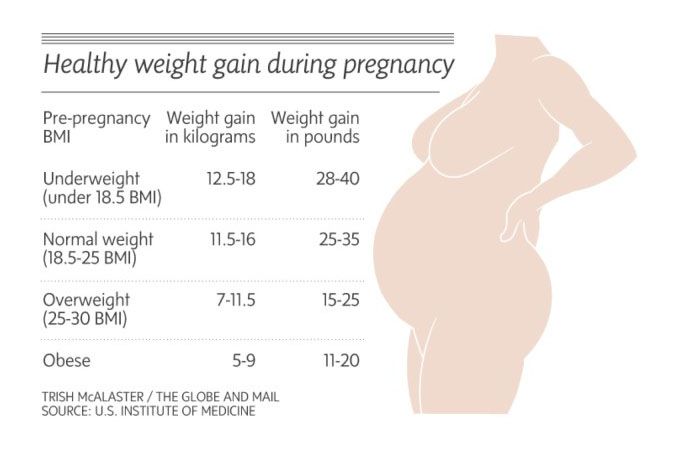 The NCT offers online antenatal classes with small groups of people that live locally to you.
The NCT offers online antenatal classes with small groups of people that live locally to you.
To keep bones and muscles healthy, we need vitamin D. From late March/early April to the end of September, most people make enough vitamin D from sunlight on their skin. However, between October and early March, you should consider taking a daily vitamin D supplement because we cannot make enough from sunlight.
Some people should take a vitamin D supplement all year round, find out if this applies to you on the NHS website. You just need 10 micrograms (it's the same for grown-ups and kids). Check if you're entitled to free vitamins.
It's recommended that you do 150 minutes of exercise a week while pregnant. You could start off with just 10 minutes of daily exercise - perhaps take a brisk walk outside. Check out Sport England's #StayInWorkOut online exercises (scroll to the pregnancy section). Listen to your body and do what feels right for you.
There's no need to eat for 2.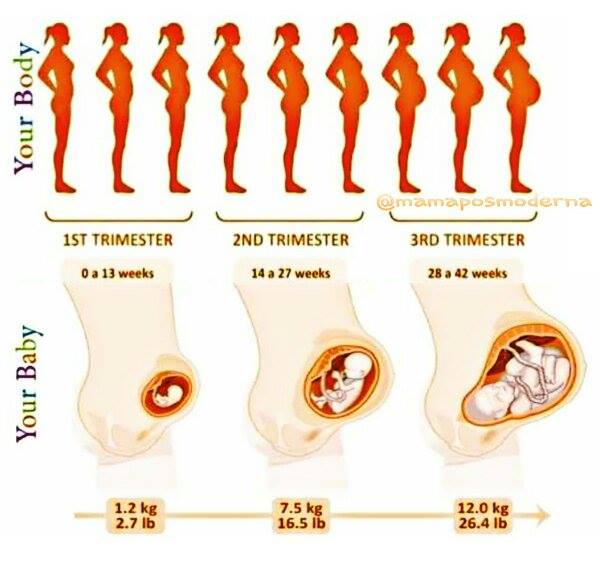 Now you're in the 3rd trimester, you may need an extra 200 calories a day, but that's not much. It's about the same as 2 slices of wholemeal toast and margarine.
Now you're in the 3rd trimester, you may need an extra 200 calories a day, but that's not much. It's about the same as 2 slices of wholemeal toast and margarine.
Try and eat healthily with plenty of fresh fruit and veg, and avoid processed, fatty and salty foods. You may be able to get free milk, fruit and veg through the Healthy Start scheme.
How are you today? If you're feeling anxious or low, then talk to your midwife or doctor who can point you in the right direction to get all the support that you need. You could also discuss your worries with your partner, friends and family.
You may be worried about your relationship, or money, or having somewhere permanent to live. Don't keep it to yourself. It's important that you ask for help if you need it.
Getting pregnant again is probably the last thing on your mind. However now is a good time to start planning what type of contraception you would like to use after your baby is born. Getting pregnant again could happen sooner than you realise and too short a gap between babies is known to cause problems.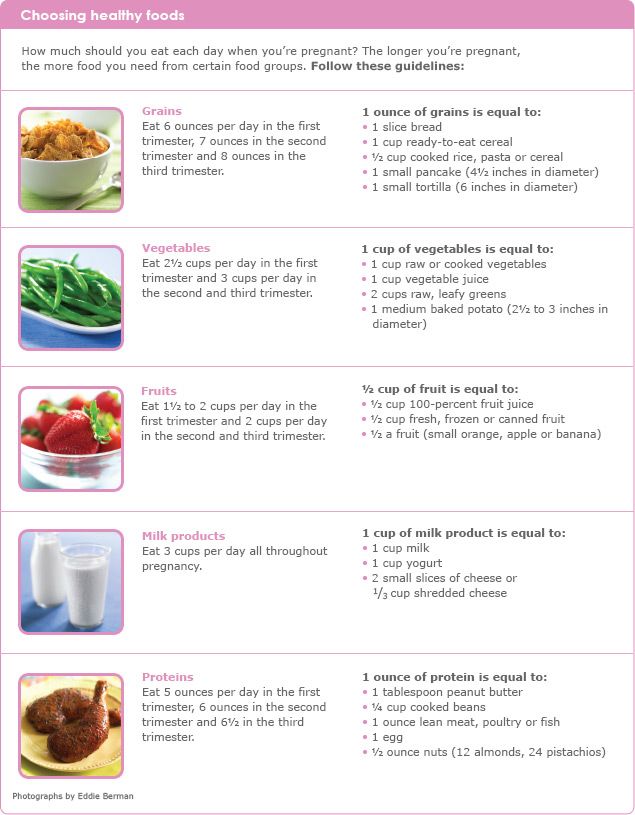 Talk to your GP or midwife to help you decide.
Talk to your GP or midwife to help you decide.
You will be offered newborn screening tests for your baby soon after they are born. These screening tests are recommended by the NHS. This is because these tests can make sure that your baby is given appropriate treatment as quickly as possible. Your decisions about whether or not you want this tests will be respected, and health care professionals will support you. Ask your midwife or doctor for more information about newborn screening.
You and your family should follow the government and NHS guidance on coronavirus (COVID-19):
To find out about about COVID-19 and pregnancy, childbirth and breastfeeding, have a look at advice on the:
Third Trimester of Pregnancy: Fetal Development
The third trimester of pregnancy starts in week 28 of your pregnancy and lasts until you give birth, which is around the 40th week. The third trimester can be tiring and more uncomfortable as your baby takes up more room and you experience:
The third trimester can be tiring and more uncomfortable as your baby takes up more room and you experience:
Backaches: Pregnancy hormones relax the connective tissue that holds your bones in place, especially in the pelvic area. These changes can cause backaches and other discomfort during the third trimester. When you sit, choose chairs with good back support. Get regular exercise. Wear flat or low-heeled shoes with good arch support. Our sponsor, Slumbar has a great pregnancy pillow to help you sleep, sit and be more comfortable.
Shortness of breath: You might get winded easily. Good posture will give your lungs more room to expand.
Heartburn. Pregnancy hormones relaxing the valve between your stomach and esophagus can allow stomach acid to reflux into your esophagus, causing heartburn. To prevent heartburn, eat small, frequent meals and avoid fried foods, citrus fruits, chocolate, and spicy or fried foods. Our sponsor Nightfood’s Nighttime Ice Cream is specially formulated to be easier to digest and uses not artificial sweeteners or erythritol, and contains ingredients that research indicates are effective against heartburn.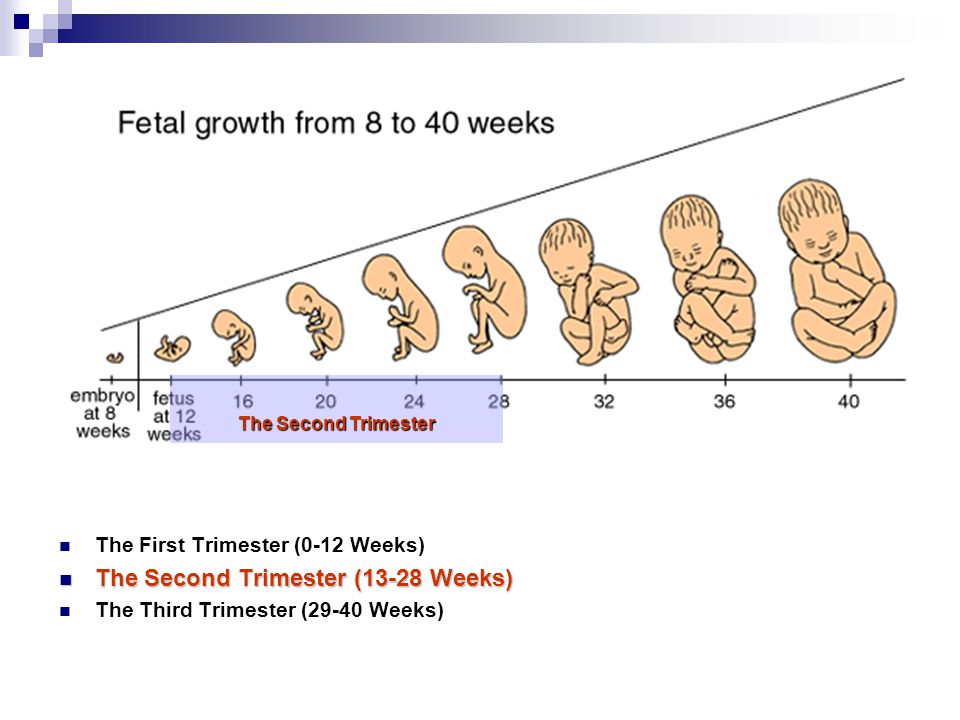
Spider veins, varicose veins and hemorrhoids: Increased blood circulation might cause tiny red-purplish veins (spider veins) to appear on your face, neck and arms. You might also experience swollen veins (varicose veins) on your legs, and hemorrhoids. To ease swelling, exercise and elevate your legs frequently, include plenty of fiber in your diet and drink lots of fluids. For hemorrhoid relief, soak in a warm tub or apply witch hazel pads to the area.
Frequent urination. As your baby moves deeper into your pelvis, you’ll feel more pressure on your bladder and the need to urinate more often. This extra pressure might also cause you to leak urine when you laugh, cough, sneeze, bend or lift. If this is a problem, consider using panty liners.
How Your Baby is Developing Now:
Weeks 27 thru 32 – Gestational Age (Fetal Age – Weeks 25 thru 30)
The fetus really fills out over these next few weeks, storing fat on the body, reaching about 15-17 inches long and weighing about 4-4 ½ lbs by the 32nd week. The lungs are not fully mature yet, but some rhythmic breathing movements are occurring. The bones are fully developed but are still soft and pliable. The fetus is storing its own calcium, iron, and phosphorus. The eyelids open after being closed, since the end of the first trimester.
The lungs are not fully mature yet, but some rhythmic breathing movements are occurring. The bones are fully developed but are still soft and pliable. The fetus is storing its own calcium, iron, and phosphorus. The eyelids open after being closed, since the end of the first trimester.
Weeks 33 thru 36 – Gestational Age (Fetal Age – Weeks 31 thru 34)
This is about the time that the fetus will descend into the head-down position preparing for birth. The fetus is beginning to gain weight more rapidly. The lanugo hair will disappear from the skin, and it is becoming less red and wrinkled. The fetus is now 16-19 inches and weighs anywhere from 5 ¾ lbs to 6 ¾ lbs.
Weeks 37 thru 40 – Gestational Age (Fetal Age – Weeks 35 thru 38)
At 38 weeks the fetus is considered full-term and is ready to make its appearance at any time. As your baby becomes bigger, you may notice a change in fetal movement. If you notice a decrease in fetal movement, make sure to talk with your doctor.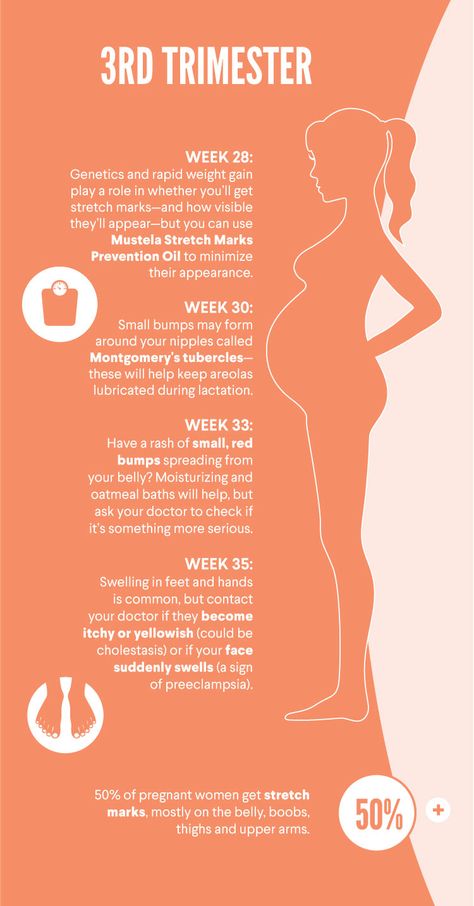 The fingernails have grown long and will need to be cut soon after birth. Small breast buds are present on both sexes. The mother is supplying the fetus with antibodies that will help protect against disease. All organs are developed, with the lungs maturing all the way until the day of delivery. The fetus is about 19 – 21 inches in length and weighs anywhere from 6 ¾ lbs to 10 lbs.
The fingernails have grown long and will need to be cut soon after birth. Small breast buds are present on both sexes. The mother is supplying the fetus with antibodies that will help protect against disease. All organs are developed, with the lungs maturing all the way until the day of delivery. The fetus is about 19 – 21 inches in length and weighs anywhere from 6 ¾ lbs to 10 lbs.
Want to Know More?
- 16 Ways to Bond WIth Your Baby While Pregnant
- Nutrients and Vitamins for Pregnancy
- Creating Your Birth Plan
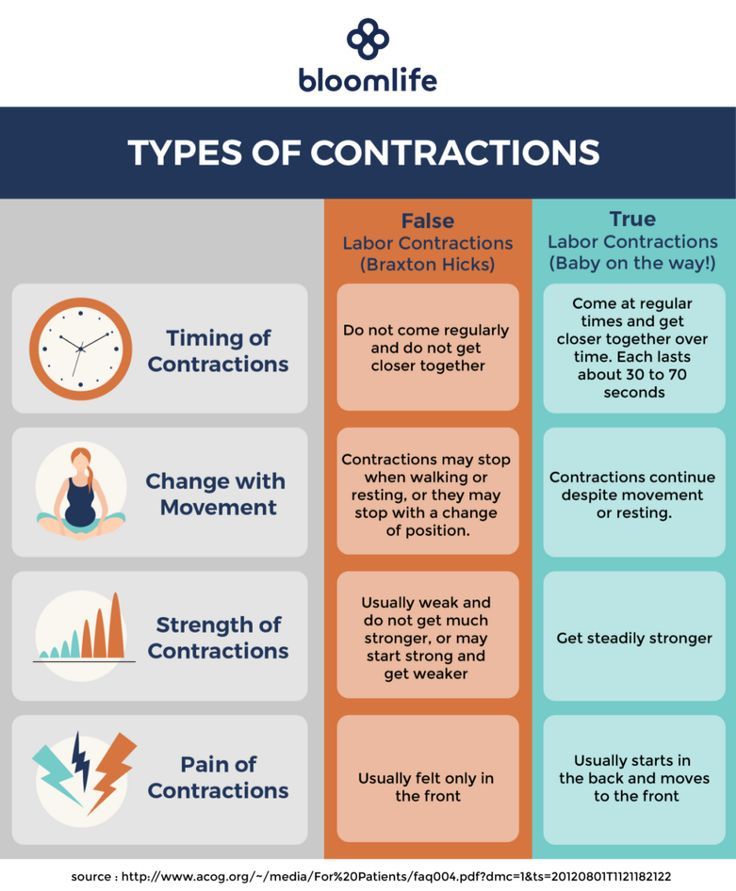
- Signs of Labor
Pregnancy management from the 3rd trimester (Aleksandrov)
Pregnancy management program from the 3rd trimester at Paracelsus Clinic
All doctors and diagnostics in one place . As part of the Paracelsus Medical Center, all narrow specialists are available to you - highly qualified obstetrician-gynecologists with extensive experience in pregnancy management, as well as all the necessary diagnostic and laboratory tests.
Availability every day, Paracelsus Medical Center works seven days a week and without holidays. No queues and convenient clinic opening hours.
Paracelsus Medical Center offers comprehensive pregnancy management programs. The programs were developed by experienced obstetrician-gynecologists based on the recommendations of the Ministry of Health of the Russian Federation for routine examinations of pregnant women. The programs include examinations of all necessary specialists and all necessary laboratory and diagnostic tests.
If a woman is observed at the Paracelsus clinic under the pregnancy management program, the attending obstetrician-gynecologist draws up all the necessary documents for the patient:
- certificate of observation of pregnancy,
- exchange card.
Leave a request for registration of the program, our administrators will advise you.
The primary task of the future mother is increased attention to the psychophysical state throughout the entire period of pregnancy.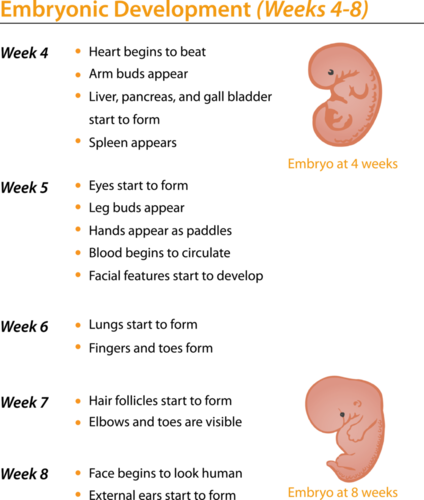 Pregnancy management within the framework of the program is a comprehensive approach that includes accurate diagnostics and consultations of practicing obstetricians and gynecologists and is the key to a successful pregnancy and subsequent childbirth.
Pregnancy management within the framework of the program is a comprehensive approach that includes accurate diagnostics and consultations of practicing obstetricians and gynecologists and is the key to a successful pregnancy and subsequent childbirth.
Benefits of pregnancy management programs at Paracelsus Clinic
Pregnancy management is primarily our responsibility, as a professional medical organization, for your health during the entire period of pregnancy, as well as for the full development of your baby. Comprehensive pregnancy management programs provide you with all the necessary set of consulting and diagnostic measures, you can be completely confident in receiving high-quality medical services.
Documents for obtaining a GENERAL CERTIFICATE:
- Registration of an exchange card to the maternity hospital.
- Issuance of sick leave for pregnancy and childbirth.
A birth certificate is issued to every woman who has a compulsory medical insurance policy at the antenatal clinic at the place of residence, despite the fact that she is observed in a private clinic.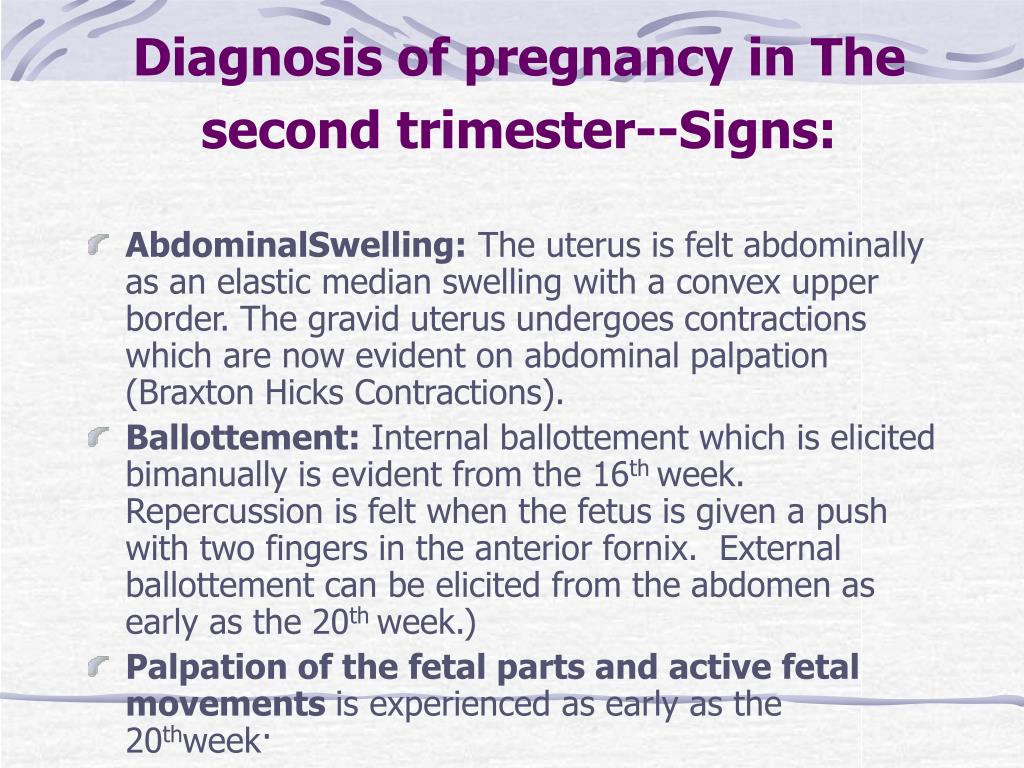
Economy:
- Fixed cost for services during pregnancy.
- By purchasing programs, your SAVINGS can reach up to 10% .
- Up to 60 days after the birth, you get an additional 10% discount on the services of the center.
Compliance with the recommendations of the Ministry of Health of the Russian Federation . The programs include the necessary set of examinations to monitor the health of a pregnant woman and an unborn child, in accordance with the recommendations of the Ministry of Health of the Russian Federation.
Pregnancy management 3rd trimester
Features
The 3rd trimester of pregnancy is the final period of bearing a baby. The beginning of this stage is considered to be the 27th obstetric week. Although in the 3rd trimester a woman is already at the final stage, there is the possibility of facing some health risks. The pregnancy management program from the 3rd trimester, which includes a set of consulting and diagnostic measures to maintain the health of mother and baby, will help to identify and prevent such risks.
Fetal development in the 3rd trimester
By week 27, the weight of the baby is about 1 kg., And the height is 30 cm. The baby is almost completely formed, at this stage, the final development of his organs and vital systems takes place.
In the 3rd trimester of pregnancy, the baby begins to hear and respond to the mother's voice, the muscles of the eyes and eyelids begin to work actively. By the beginning of the third trimester, he actively moves, rolls over, these intervals of movement alternate with a calm state of sleep of the child.
With an increase in the gestational age, the baby begins to lack space for activity, small pushes are already replaced by stronger ones, and when the baby moves and changes position, you can visually distinguish the movement of the mother's abdomen.
For only 3 trimesters of the pregnancy management program, obstetrician-gynecologists conduct a thorough palpation of the pregnant woman's abdomen to determine the position of the fetus in order to diagnose the development of pathology in the mother and child.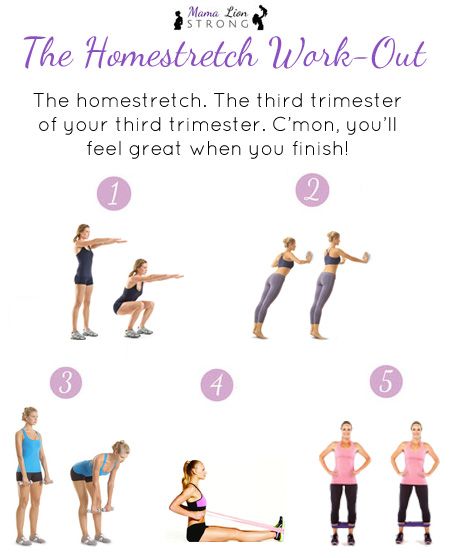
Experienced obstetrician-gynecologists will advise you on possible disorders of the intestines, stomach, liver due to changes in the structure of the uterus, which puts pressure on the internal organs.
3rd trimester diagnostics
The 3rd trimester pregnancy management program includes a mandatory scheduled ultrasound examination. The main task of this diagnosis in the 3rd trimester of pregnancy is the diagnosis and prevention of the development of malformations that appear in the final stages of fetal development, in addition, an assessment is made of the functional state of the baby, his motor and respiratory systems.
Obstetrician-gynecologists in the 3rd trimester of pregnancy determine the localization of the placenta, the degree of maturity of the placenta is established.
Ultrasound diagnosis of the 3rd trimester allows you to identify the entanglement of the baby's umbilical neck, placenta previa, insufficient placentation, etc. Based on the diagnostic and laboratory data obtained during the study, the obstetrician-gynecologist chooses the tactics of childbirth: naturally or childbirth by caesarean section.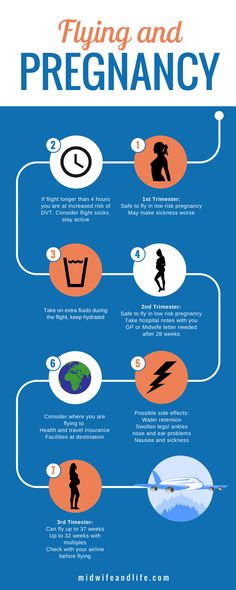
An obstetrician-gynecologist monitors a woman's readiness for childbirth and the condition of the fetus. The specialist measures body weight, blood pressure, measures the height of the uterine fundus in the 3rd trimester, determines the tone, and conducts a thorough palpation of the fetus. The appearance of edema of an explicit or latent nature is analyzed, and preeclampsia is diagnosed.
The program includes all the necessary laboratory tests, such as: a complete blood count, blood for biochemistry, protein, urea, creatinine, etc.
In the third trimester of pregnancy, fetal cardiotocography is prescribed, which allows you to diagnose in advance possible signs of oxygen starvation in the baby.
Doctors of the Medical Center "PARACELS" for 10 years helped more than 7000 patients become happy parents. We help at all stages of this desirable event for every family, from solving the problems of male and female infertility to the birth of your baby.
Leave a request for registration of the program, our administrators will advise you.
Pregnancy by trimesters: 2nd and 3rd trimester
The first trimester is behind us with its anxiety, morning sickness, constant sleepiness and other problems. If you count by weeks, the II trimester starts from the 13th week and is considered the easiest and calmest. The future mother, both psychologically and physically, has already adapted to her status, but it seems that motherhood is not yet close. However, there is also a lot of research to be done.
A full range of laboratory tests is available at DILA: Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy", prenatal screening of the II trimester, prenatal non-invasive screening (NIPT, basic), as well as a number of other screening programs and mono-examinations. All of them are aimed at determining the general state of health, the work of the main systems and organs of a pregnant woman in the second and third trimesters of pregnancy. Regular monitoring will allow early detection of various complications that may arise and provide the necessary treatment. Thus, the chances of a normal pregnancy and the birth of a healthy child are increased.
Regular monitoring will allow early detection of various complications that may arise and provide the necessary treatment. Thus, the chances of a normal pregnancy and the birth of a healthy child are increased.
Second trimester examinations
The second (II) trimester of pregnancy includes the period between 13 and 26 weeks. It is during this time period, closer to the 16th week, that all organs and systems of the fetus are already finally laid down, but all the organs and systems of the fetus continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators of this period reflects not only the state of health of a pregnant woman and the features of the work of the main organs and systems, but also makes it possible to detect diseases and possible complications.
So, Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy" includes the following studies:
- Complete blood count.
 It is aimed at a basic assessment of the general state of health: the hematopoietic system, the presence of inflammatory, infectious (including viral), oncological diseases, as well as allergic processes in the body.
It is aimed at a basic assessment of the general state of health: the hematopoietic system, the presence of inflammatory, infectious (including viral), oncological diseases, as well as allergic processes in the body. - Urinalysis. Allows you to assess the state of the urinary tract and some extrarenal diseases, to identify the presence of preeclampsia.
- Glucose tolerance test, which makes it possible to evaluate carbohydrate metabolism disorders (including latent forms).
- HIV 1/1o/2 to detect HIV infection.
Complete blood count with leukocyte count and ESR (erythrocyte sedimentation rate) and urinalysis should preferably be performed once a month.
Clinical blood test makes it possible to study the qualitative and quantitative composition of blood by key indicators: erythrocytes and their specific indicators, leukocytes and their varieties in absolute and percentage terms, platelets. The detection of deviations in these markers may indicate the presence of pathological processes in the body of a pregnant woman.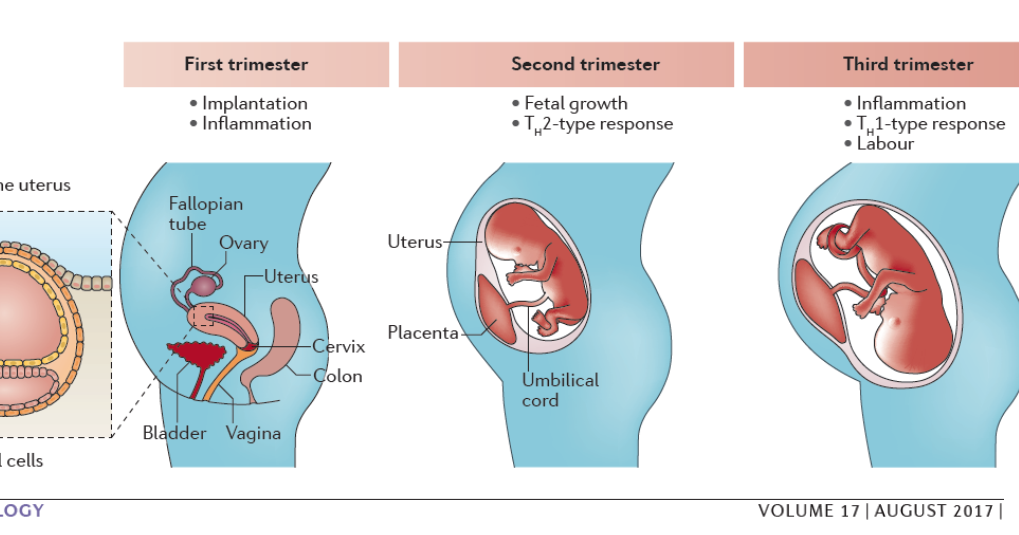 A decrease in the level of erythrocytes and hemoglobin in erythrocytes is a sign of anemia in pregnant women. This can lead to placental insufficiency - the main reason for miscarriage, the birth of small children and fetal death.
A decrease in the level of erythrocytes and hemoglobin in erythrocytes is a sign of anemia in pregnant women. This can lead to placental insufficiency - the main reason for miscarriage, the birth of small children and fetal death.
Changes in the leukocyte formula may indicate a wide range of changes in the body of pregnant women in the 2nd trimester. They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which requires a more extensive additional examination - both instrumental and laboratory. The content of platelets during physiological pregnancy may slightly decrease, but significant changes in this indicator, including developing thrombocytopenia, require special observation, since they may be indirect signs of a violation of the blood coagulation system, as well as DIC (disseminated intravascular coagulation syndrome), which are severe pregnancy complications.
A change in the erythrocyte sedimentation rate (ESR) can be observed in acute and chronic inflammatory pathologies, infectious diseases, as well as oncological and autoimmune processes. At the same time, in pregnant women, the erythrocyte sedimentation rate slightly increases in the norm.
At the same time, in pregnant women, the erythrocyte sedimentation rate slightly increases in the norm.
General analysis of urine allows you to evaluate the general properties of urine, its physico-chemical properties, the presence of metabolic products, to detect the quantitative and qualitative content of certain organic compounds. This study reflects the functional state of the kidneys, urinary tract, allows you to evaluate the overall metabolic processes, suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, "pregnancy diabetes". If protein is found in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks.
The glucose tolerance test detects gestational diabetes (“diabetes in pregnancy”).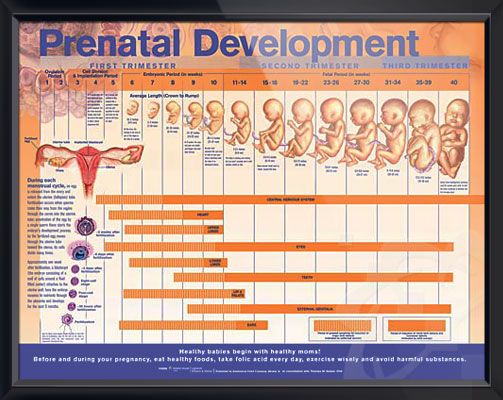 If this deviation is detected, a woman needs to control her sugar levels throughout pregnancy and after childbirth. Early detection of gestational diabetes is very important to prevent a number of undesirable consequences, including the birth of a large fetus and the risk of prenatal complications.
If this deviation is detected, a woman needs to control her sugar levels throughout pregnancy and after childbirth. Early detection of gestational diabetes is very important to prevent a number of undesirable consequences, including the birth of a large fetus and the risk of prenatal complications.
HIV testing . To reduce the risk of infection of the fetus, it is very important to detect the human immunodeficiency virus in a pregnant woman in a timely manner. The detection of HIV infection is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. Without preventive measures, the risks of transmission of HIV infection from mother to fetus are 20-40%, while the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur when the fetus passes through the natural birth canal. In addition, there is a high risk of infection during breastfeeding.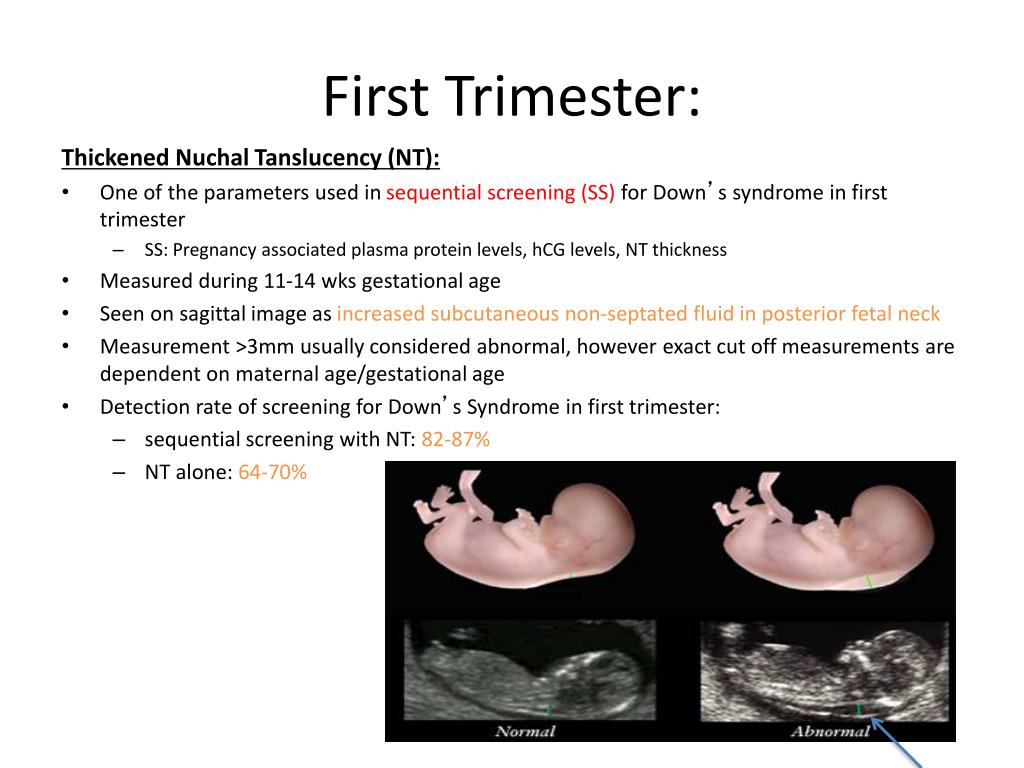
We have only described the possibilities of Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy", but there are a number of other important studies.
2nd trimester prenatal screening is a “triple test” that includes a total unit of beta-hCG, AFP, and unconjugated (free) estriol. It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain fetal chromosomal abnormalities:
- Down syndrome. Violation is accompanied by characteristic features of appearance, mental retardation, defects of internal organs, short stature.
- Edwards syndrome. Most children with this syndrome die before the age of 3 months, only 5-10% survive to a year. The survivors are profoundly mentally retarded.
- Patau Syndrome. Accompanied by severe congenital malformations.
Also, prenatal screening of the second trimester makes it possible to assess the risk of malformations of the neural tube of the fetus.
The test is performed between 14 and 21 weeks, optimally between 16 and 18 weeks of pregnancy. Down, Edwards and Patau syndromes are the most common chromosomal disorders. The ability to detect these disorders in the early stages allows you to timely assess the genetic health of the fetus.
An alternative to biochemical prenatal screening is the NIPT test. It is more accurate than biochemical, and neither the course of pregnancy, nor the drugs taken, nor the woman's somatic diseases affect its results. The difference from biochemical screening is that NIPT is a direct method that allows you to examine the DNA of the fetus, while biochemistry is an indirect method. Biochemical screening has an accuracy of 70-80%, while NIPT has an accuracy of more than 99.9%.
Another important laboratory marker in the 2nd trimester is thyroid-stimulating hormone (TSH). This hormone is produced by the pituitary gland and is responsible for regulating the synthesis of the thyroid hormones thyroxine and triiodothyronine according to the “feedback system”, which allows maintaining a stable concentration of these hormones in the blood. Despite the fact that the thyroid hormone systems of a pregnant woman and the fetus do not depend on each other, her health and, accordingly, the course of the entire pregnancy depend on the normal functioning of the thyroid system of a woman. During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible.
Despite the fact that the thyroid hormone systems of a pregnant woman and the fetus do not depend on each other, her health and, accordingly, the course of the entire pregnancy depend on the normal functioning of the thyroid system of a woman. During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible.
In the second and third trimesters of pregnancy, it is important to assess the risk of one of the most serious pregnancy complications, preeclampsia. Placental growth factor (PLGF), a marker of preeclampsia, has angiogenic properties and is essential for the normal development of the placental vascular system. Normally, the concentration of PlGF gradually increases up to 30 weeks of pregnancy. In the case of preeclampsia, there is a decrease in PLGF. Timely detection of increased risk allows you to predict the optimal tactics of pregnancy and childbirth.
Timely detection of increased risk allows you to predict the optimal tactics of pregnancy and childbirth.
What tests should be done in the third trimester
The third trimester of pregnancy includes the period between 27 and 40 weeks. This period is characterized by the active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, and the maturation of the nervous system. Clinical laboratory diagnostics of the III trimester is aimed at assessing the functioning of the main organs and systems, in particular the liver, kidneys, blood coagulation system, endocrine system of a pregnant woman, as well as infection control during pregnancy.
To check the state of health in the 3rd trimester, complex examinations are available in DILA Program 186 “Examination of a pregnant woman at 28-29 weeks of pregnancy” and Program 187 “Examination of a pregnant woman at 32-35 weeks of pregnancy”, as well as individual programs.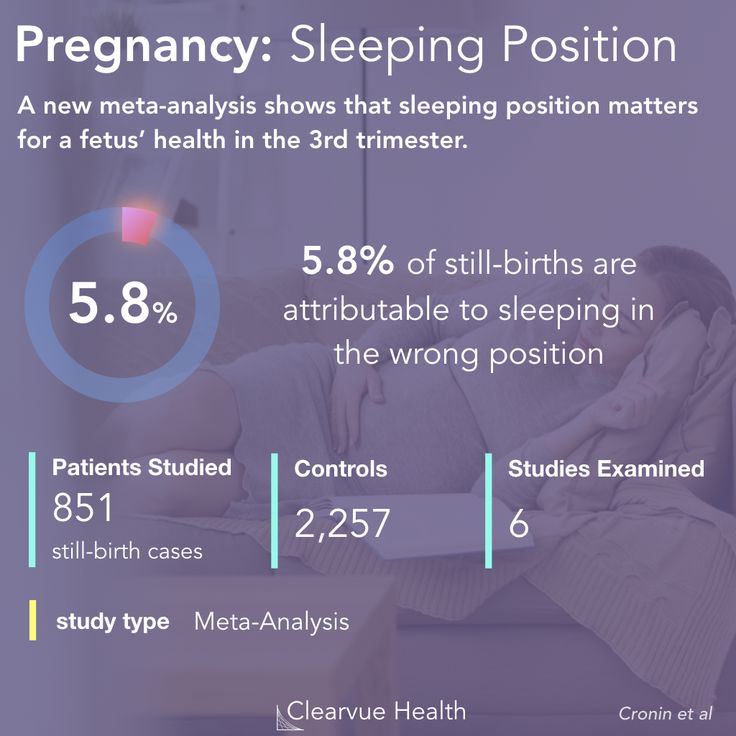
Risk of bleeding . In the third trimester of pregnancy, it is important to monitor the state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic coagulation pathway. The results of the test are the prothrombin time according to Quick and the international normalized ratio. These indicators make it possible to assess the state of the liver, the main pathways of the blood coagulation system and the functional state of its basic components. The determination of these markers has a high diagnostic value for predicting thrombosis during pregnancy, diagnosing DIC, a dangerous complication accompanied by massive blood loss.
Normally, the levels of prothrombin and fibrinogen in the third trimester of pregnancy slightly increase, but a significant increase in these indicators requires close monitoring and the appointment of the necessary treatment. The concentration of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, however, a sharp increase in the concentration of this protein may indicate a large number of blood clots, which is often associated with venous thromboembolism or DIC.
Infections . In the III trimester of pregnancy, it is also recommended to re-examine for:
- hepatitis B;
- hepatitis C;
- HIV infection;
- syphilis - antibodies to Treponema pallidum.
Because the incubation period for some infectious diseases varies greatly, negative test results taken early in pregnancy may change by the 3rd trimester or remain negative as well. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or a planned caesarean section.
Screening for group B streptococcus is now a mandatory test, essential at 36 +0 -37+ 6 weeks of pregnancy.
There is a group of infections that are very dangerous for pregnant women - these are TORCH infections. Their peculiarity lies in the fact that during the primary infection (if the woman has not yet been ill with them) during pregnancy, they can adversely affect all systems and organs of the fetus, especially its central nervous system. Infection with TORCH-group infections increases the likelihood of miscarriage, stillbirth and congenital malformations of the baby, up to disability. Program 134 "Extended screening for TORCH infections" from DILA allows you to assess the immune status (the presence of immune memory) to pathogens that are part of the TORCH complex group. Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period.
Infection with TORCH-group infections increases the likelihood of miscarriage, stillbirth and congenital malformations of the baby, up to disability. Program 134 "Extended screening for TORCH infections" from DILA allows you to assess the immune status (the presence of immune memory) to pathogens that are part of the TORCH complex group. Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period.
Biochemical indicators (alanine aminotransferase, aspartate aminotransferase total bilirubin and direct bilirubin fraction, total protein in serum), which are part of Program 151 "Blood Biochemistry", allow assessing the functional state of the liver. A significant increase in the content of transaminases in the blood may indicate the presence of liver damage, hepatitis, the development of preeclampsia. A decrease in the level of total protein in the blood serum, along with the loss of protein in the urine and with an increase in blood pressure, can also be a sign of developing preeclampsia. To exclude gestational diabetes and the development of complications, in particular diabetic nephropathy, it is important to determine the level of glucose in the blood plasma. To assess the functional state of the kidneys will help determine the concentration of urea and creatinine, as well as assessing the glomerular filtration rate. Importantly, in pregnant women, the amount of creatinine is reduced by almost half due to an increase in blood volume, increased blood flow to the kidneys and, consequently, an increasing degree of filtration. Also, an increase in renal filtration leads to a decrease in the amount of urea in pregnant women.
A decrease in the level of total protein in the blood serum, along with the loss of protein in the urine and with an increase in blood pressure, can also be a sign of developing preeclampsia. To exclude gestational diabetes and the development of complications, in particular diabetic nephropathy, it is important to determine the level of glucose in the blood plasma. To assess the functional state of the kidneys will help determine the concentration of urea and creatinine, as well as assessing the glomerular filtration rate. Importantly, in pregnant women, the amount of creatinine is reduced by almost half due to an increase in blood volume, increased blood flow to the kidneys and, consequently, an increasing degree of filtration. Also, an increase in renal filtration leads to a decrease in the amount of urea in pregnant women.
During the second and third trimesters of pregnancy, a woman still needs to carefully monitor her health and undergo laboratory diagnostics. Screening programs and individual studies from DILA will help the doctor evaluate the functioning of internal organs, timely identify bleeding disorders in a woman, diagnose dangerous infections, detect possible genetic abnormalities of the fetus, and identify the risk of preeclampsia in time.