How does a cleft lip form
Facts about Cleft Lip and Cleft Palate
Cleft lip and cleft palate are birth defects that occur when a baby’s lip or mouth do not form properly during pregnancy. Together, these birth defects commonly are called “orofacial clefts”.
Click here to view a larger image
Click here to view a larger image
What is Cleft Lip?
The lip forms between the fourth and seventh weeks of pregnancy. As a baby develops during pregnancy, body tissue and special cells from each side of the head grow toward the center of the face and join together to make the face. This joining of tissue forms the facial features, like the lips and mouth. A cleft lip happens if the tissue that makes up the lip does not join completely before birth. This results in an opening in the upper lip. The opening in the lip can be a small slit or it can be a large opening that goes through the lip into the nose. A cleft lip can be on one or both sides of the lip or in the middle of the lip, which occurs very rarely. Children with a cleft lip also can have a cleft palate.
What is Cleft Palate?
The roof of the mouth (palate) is formed between the sixth and ninth weeks of pregnancy. A cleft palate happens if the tissue that makes up the roof of the mouth does not join together completely during pregnancy. For some babies, both the front and back parts of the palate are open. For other babies, only part of the palate is open.
Other Problems
Children with a cleft lip with or without a cleft palate or a cleft palate alone often have problems with feeding and speaking clearly and can have ear infections. They also might have hearing problems and problems with their teeth.
How Many Babies are Born with Cleft Lip/Cleft Palate?
- About 1 in every 1,600 babies is born with cleft lip with cleft palate in the United States.
- About 1 in every 2,800 babies is born with cleft lip without cleft palate in the United States.
- About 1 in every 1,700 babies is born with cleft palate in the United States.
 1
1
Causes and Risk Factors
The causes of orofacial clefts among most infants are unknown. Some children have a cleft lip or cleft palate because of changes in their genes. Cleft lip and cleft palate are thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Like the many families of children with birth defects, CDC wants to find out what causes them. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011) and the Birth Defects Study To Evaluate Pregnancy exposureS (BD-STEPS; began with births in 2014), to understand the causes of and risks for birth defects, including orofacial clefts.
Recently, CDC reported on important findings from research studies about some factors that increase the chance of having a baby with an orofacial cleft:
- Smoking―Women who smoke during pregnancy are more likely to have a baby with an orofacial cleft than women who do not smoke.2-3
- Diabetes―Women with diabetes diagnosed before pregnancy have an increased risk of having a child with a cleft lip with or without cleft palate, compared to women who did not have diabetes.5
- Use of certain medicines―Women who used certain medicines to treat epilepsy, such as topiramate or valproic acid, during the first trimester (the first 3 months) of pregnancy have an increased risk of having a baby with cleft lip with or without cleft palate, compared to women who didn’t take these medicines.6-7
CDC continues to study birth defects, such as cleft lip and cleft palate, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.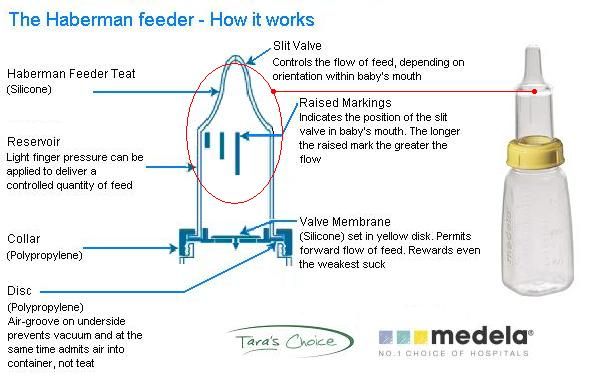
Diagnosis
Orofacial clefts, especially cleft lip with or without cleft palate, can be diagnosed during pregnancy by a routine ultrasound. They can also be diagnosed after the baby is born, especially cleft palate. However, sometimes certain types of cleft palate (for example, submucous cleft palate and bifid uvula) might not be diagnosed until later in life.
Management and Treatment
Services and treatment for children with orofacial clefts can vary depending on the severity of the cleft; the child’s age and needs; and the presence of associated syndromes or other birth defects, or both.
Surgery to repair a cleft lip usually occurs in the first few months of life and is recommended within the first 12 months of life. Surgery to repair a cleft palate is recommended within the first 18 months of life or earlier if possible.8 Many children will need additional surgical procedures as they get older. Surgical repair can improve the look and appearance of a child’s face and might also improve breathing, hearing, and speech and language development.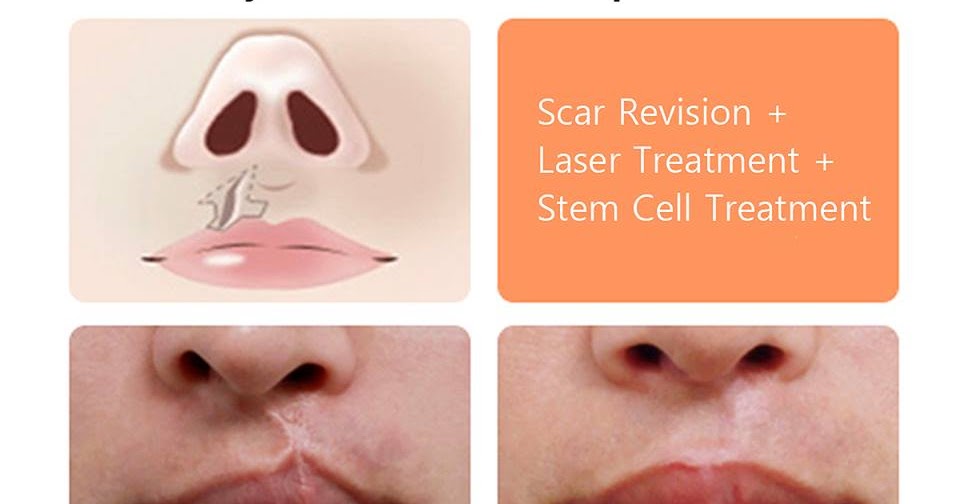 Children born with orofacial clefts might need other types of treatments and services, such as special dental or orthodontic care or speech therapy.4,8
Children born with orofacial clefts might need other types of treatments and services, such as special dental or orthodontic care or speech therapy.4,8
With treatment, most children with orofacial clefts do well and lead a healthy life. Some children with orofacial clefts may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups can prove to be useful for families of babies with birth defects of the head and face, such as orofacial clefts.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
- Little J, Cardy A, Munger RG. Tobacco smoking and oral clefts: a meta-analysis. Bull World Health Organ. 2004;82:213-18.
- Honein MA, Rasmussen SA, Reefhuis J, Romitti P, Lammer EJ, Sun L, Correa A.
 Maternal smoking, environmental tobacco smoke, and the risk of oral clefts. Epidemiology 2007;18:226–33.
Maternal smoking, environmental tobacco smoke, and the risk of oral clefts. Epidemiology 2007;18:226–33. - Yazdy MM, Autry AR, Honein MA, Frias JL. Use of special education services by children with orofacial clefts. Birth Defects Research (Part A): Clinical and Molecular Teratology 2008;82:147-54.
- Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, Cleves MA, Riehle-Colarusso TJ, Waller DK, Reece EA. Diabetes mellitus and birth defects. American Journal of Obstetrics and Gynecology 2008;199:237.e1-9.
- Margulis AV, Mitchell AA, Gilboa SM, Werler MM, Glynn RJ, Hernandez-Diaz S, National Birth Defects Prevention Study. Use of topiramate in pregnancy and risk of oral clefts. American Journal of Obstetrics and Gynecology 2012;207:405.e1-e7.
- Werler MM, Ahrens KA, Bosco JL, Michell AA, Anderka MT, Gilboa SM, Holmes LB, National Birth Defects Prevention Study. Use of antiepileptic medications in pregnancy in relation to risks of birth defects. Annals of Epidemiology 2011;21:842-50.

- American Cleft Palate-Craniofacial Association. Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Revised edition, Nov 2009. Chapel Hill, NC. P. 1-34. https://acpa-cpf.org/wp-content/uploads/2017/06/Parameters_Rev_2009_9_.pdf
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
Cleft Lip and Cleft Palate: Causes, Diagnosis & Treatment
Overview
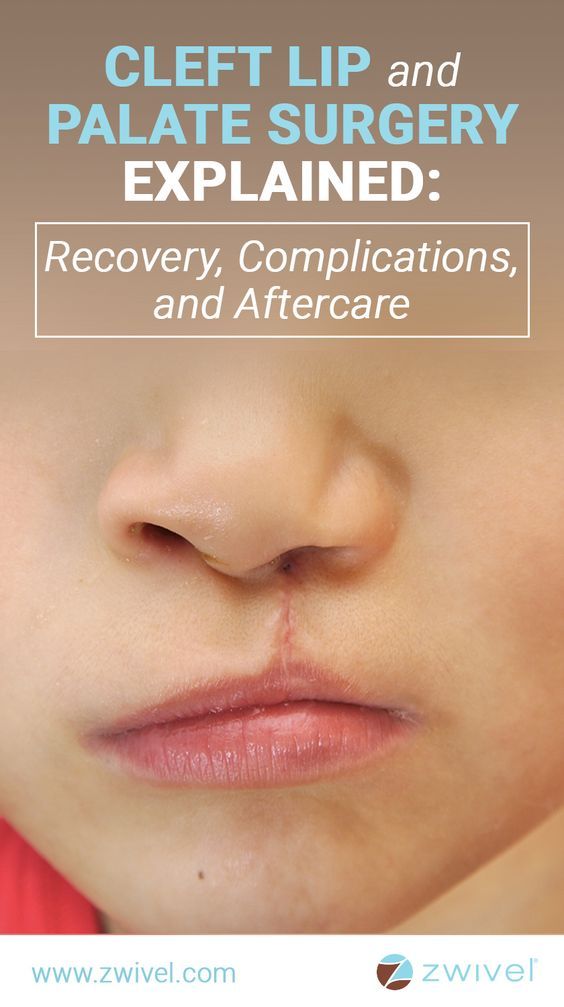
Before and after images of a young boy after surgeries to treat a unilateral cleft lip.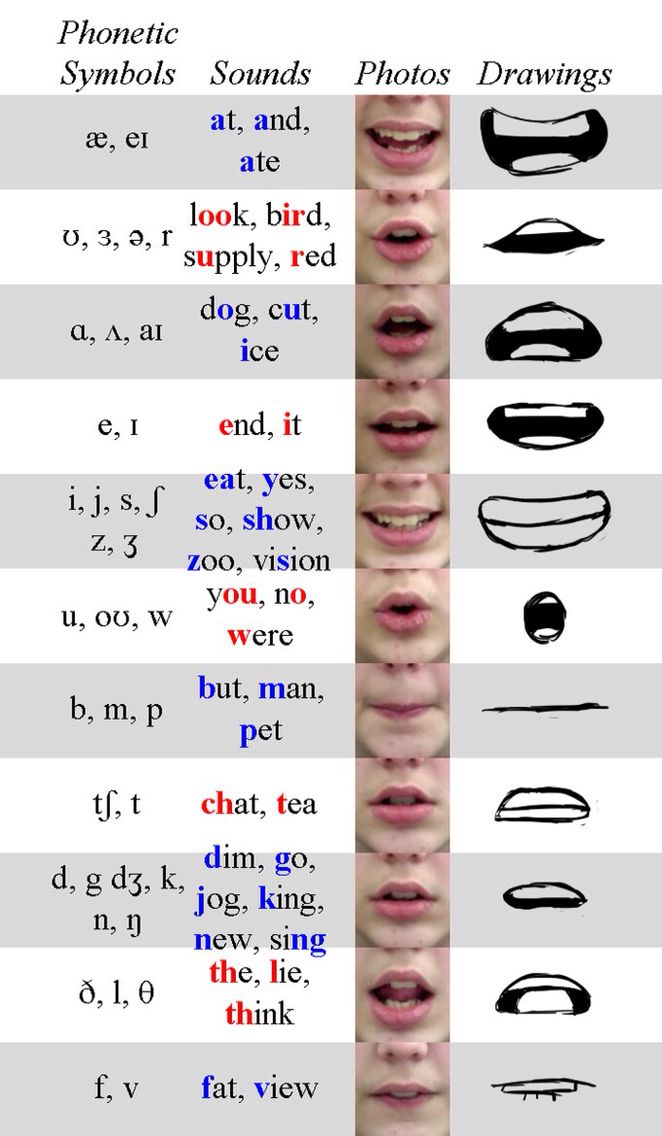 A cleft lip is an opening or split in the upper lip that occurs during fetal development.
A cleft lip is an opening or split in the upper lip that occurs during fetal development.What are cleft lip and cleft palate?
A cleft lip and cleft palate are openings in a baby's upper lip or roof of the mouth (palate). They're congenital abnormalities (birth defects) that form while a fetus develops in the uterus. Cleft lips and cleft palates happen when tissues of the upper lip and roof of the mouth don't join together properly during fetal development. Surgery is required to repair cleft lip and cleft palate.
What is cleft lip?
Our lips form between four and seven weeks of pregnancy. Tissues from each side of our head join together at the center of the face to make our lips and mouth. A cleft lip happens when the tissues that make the lips don't join completely. As a result, an opening or gap forms between the two sides of the upper lip. The cleft can range from a small indentation to a large gap that reaches the nose. This separation can include the gums or the palate (roof of the mouth).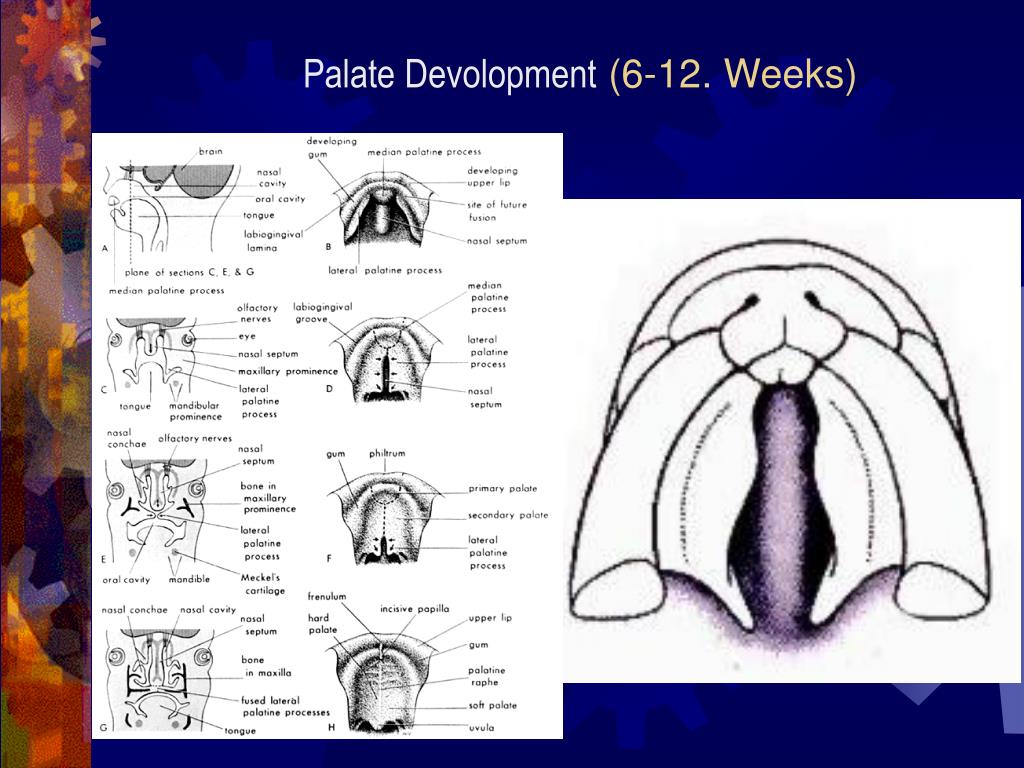
What is cleft palate?
The roof of your mouth (palate) forms between six and nine weeks of pregnancy. A cleft palate is a split or opening in the roof of your mouth that forms during fetal development. A cleft palate can include the hard palate (the bony front portion of the roof of the mouth) or the soft palate (the soft back portion of the roof of the mouth).
Cleft lip and cleft palate can occur on one or both sides of the mouth. Because the lip and the palate develop separately, it's possible to have a:
- Cleft lip without a cleft palate.
- Cleft palate without a cleft lip.
- Both a cleft lip and cleft palate (the most frequently occurring disorder).
Who gets cleft lip and cleft palate?
Cleft lip and cleft palate are the 4th most common congenital disorder in the United States:
- About 1 in every 1,600 babies is born with cleft lip with cleft palate in the U.S.
- About 1 in every 2,800 babies is born with cleft lip without cleft palate in the U.
 S.
S. - About 1 in every 1,700 babies is born with cleft palate in the U.S.
Cleft lips (either with or without a cleft palate) are more common in boy babies. Cleft palate (without a cleft lip) is more common in girl babies.
How will a cleft lip or cleft palate affect my baby?
Babies born with a cleft lip or cleft palate may have difficulties eating (both from the breast and a bottle). They may also have trouble speaking, and they often have fluid behind their eardrum that can affect hearing. Depending on the case, some also have issues with their teeth.
Symptoms and Causes
What causes a cleft lip and cleft palate?
In most cases, there is no cause of cleft lip or cleft palate, and parents can't prevent it. Most scientists believe clefts are caused by a combination of genetic (inherited) and environmental (related to the natural world) factors. There seems to be a greater chance of a newborn having a cleft if a sibling, parent or other relative has one.
Another cause of a cleft lip or cleft palate may be related to medication the birthing parent took during pregnancy. This includes antiseizure medications, acne treatment medications containing Accutane®, or methotrexate, a drug commonly used for treating cancer, arthritis and psoriasis.
Other factors that can contribute to the development of a cleft include:
- Vitamin deficiency (folic acid).
- Having obesity.
- Smoking or tobacco use during pregnancy.
- Substance abuse.
- Birth disorders like DiGeorge syndrome or Pierre Robin syndrome.
The condition may also occur due to exposure to viruses or chemicals while the fetus develops in the uterus.
Diagnosis and Tests
How are cleft lip and cleft palate diagnosed?
Prenatal ultrasound can diagnose most clefts of the lip because clefts cause physical changes in the fetus's face. Isolated cleft palate (no cleft lip present) is detected in only 7% of fetuses with the condition during the prenatal ultrasound because it's difficult to see.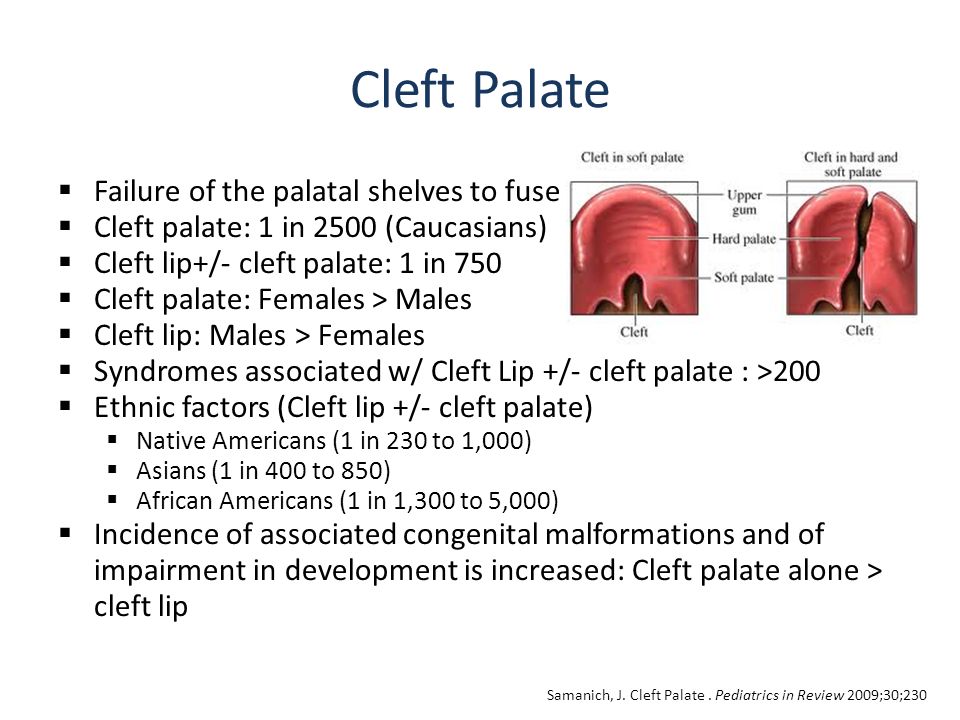
If a cleft has not been detected in an ultrasound before birth, a physical exam of the mouth, nose and palate can diagnose cleft lip or cleft palate after birth.
In some cases, your provider may recommend amniocentesis to check for other genetic conditions. Amniocentesis is a procedure to remove amniotic fluid from the amniotic sac. It helps diagnose other congenital disorders.
When in pregnancy is a cleft lip and cleft palate seen on an ultrasound?
Most healthcare providers detect a cleft lip at your 20-week ultrasound (anatomy scan), which occurs between 18 and 22 weeks of pregnancy. It may be discovered as early as 12 weeks. It's more challenging to detect a cleft palate on an ultrasound.
Management and Treatment
Treatment for cleft lip and cleft palate begins at birth. Surgical treatment begins as early as 3 months and can last until the teen years.What problems are associated with cleft lip and cleft palate?
Problems with eating, hearing and speech are common in children with clefts.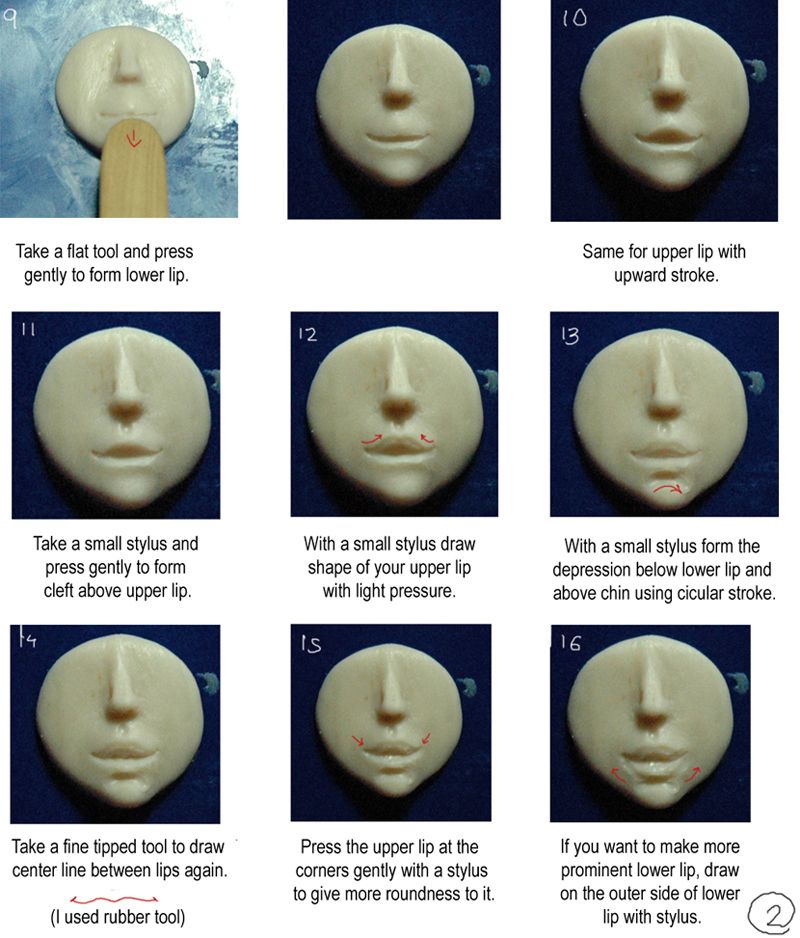 Children may also have issues with their teeth or self-esteem.
Children may also have issues with their teeth or self-esteem.
Eating problems
With a separation or opening in the palate, food and liquids can pass from the mouth back through the nose. Some babies have difficulty breastfeeding (chestfeeding) or taking a bottle because they can't form a good seal around the nipple.
Hearing loss
Children with cleft palate are more prone to fluid buildup in the middle ear (glue ear). If left untreated, this causes hearing loss.
Speech problems
Children with cleft palate may also have trouble speaking. Their voices don't carry well, sound nasally, and the speech may be difficult to understand. Not all children have these problems, and surgery may fix these problems entirely.
Dental problems
Children with clefts are prone to dental problems like cavities and missing, malformed or displaced teeth.
They may be more prone to defects of the alveolar ridge, the bony upper gum that contains the teeth.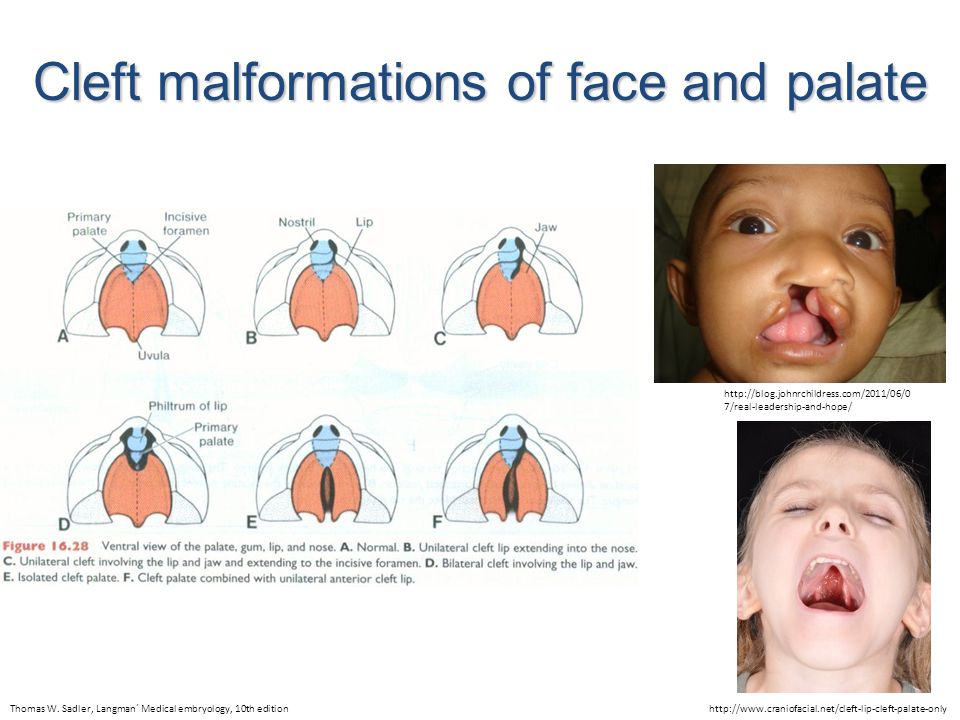 A defect in the alveolus can:
A defect in the alveolus can:
- Displace, tip, or rotate permanent teeth.
- Prevent permanent teeth from appearing.
- Prevent the alveolar ridge from forming.
- Cause premature loss of erupting canine and incisor teeth.
Children with clefts may be self-conscious or embarrassed about their appearance, even at a young age. This can cause emotional, social or behavioral problems at school and lead to issues with their confidence.
Who treats children who have cleft lip and palate?
Healthcare providers work together to develop a care plan because of the number of oral health and medical problems associated with a cleft lip or cleft palate. Treatment usually begins in infancy and often continues through early adulthood.
Members of a cleft lip and palate team may include:
- A cleft surgeon to evaluate and perform necessary surgeries on the lip or palate.
- Your pediatrician.
- An orthodontist to straighten and reposition teeth.
- A dentist or pediatric dentist to perform routine dental care.
- A prosthodontist to make artificial teeth and dental appliances.
- Speech pathologists to assess speech and feeding problems.
- An otolaryngologist (a head and neck surgeon).
- Plastic surgeon.
- Oral surgeon.
- Audiologist (a specialist in hearing disorders) to check and monitor hearing.
- Social worker/psychologist to support the family and note any adjustment problems.
- Genetic counselors help parents and adult patients understand the chances of having more children with a cleft palate or cleft lip.
How do doctors fix a cleft lip and cleft palate?
Treating cleft lip and cleft palate depends on the extent of the cleft, the child's age and other special needs or health conditions. Surgery is performed at a hospital, and the child gets anesthesia so they are asleep during the procedure.
Cleft lip repair
A cleft lip repair may require one or two surgeries.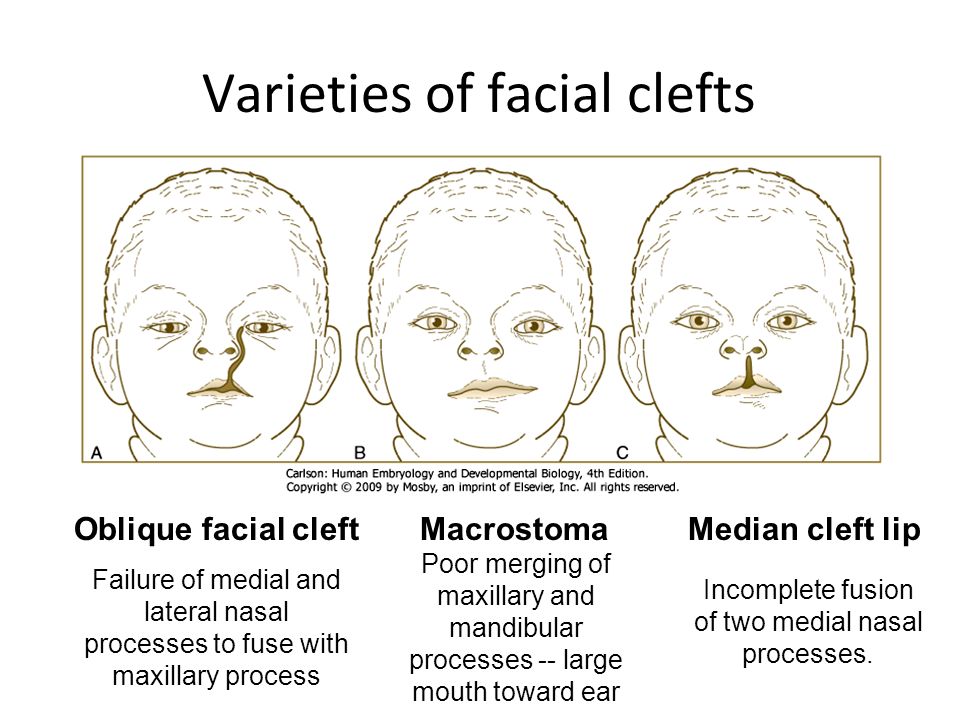 The first surgery usually occurs when the baby is between 3 and 6 months old. This surgery closes the infant's lip. The second surgery, if necessary, is usually done when the child is 6 months old.
The first surgery usually occurs when the baby is between 3 and 6 months old. This surgery closes the infant's lip. The second surgery, if necessary, is usually done when the child is 6 months old.
Several techniques can improve the outcomes of cleft lip and palate repairs when used appropriately before surgery. They are non-invasive and dramatically change the shape of the baby's lip, nose and mouth:
- A lip-taping regimen can narrow the gap in the child's cleft lip.
- A nasal elevator helps form the correct shape of the baby's nose.
- A nasal-alveolar molding (NAM) device may be used to help mold the lip tissues into a more favorable position in preparation for lip repair.
Cleft palate repair
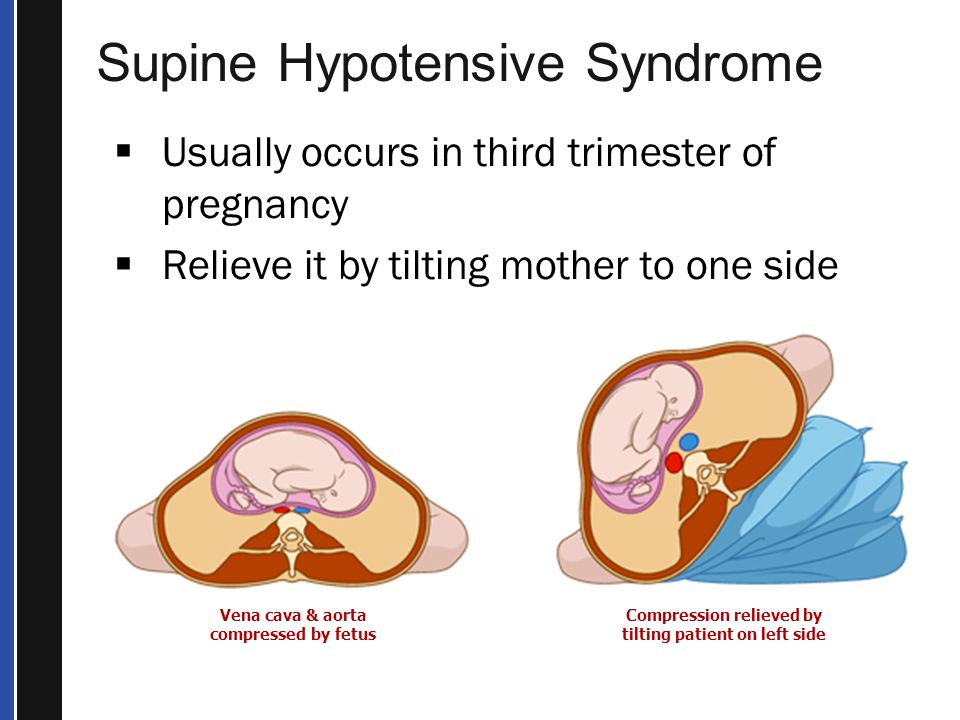
A cleft palate repair is performed at 12 months and creates a working palate and reduces the chances that fluid will develop in the middle ears. To prevent fluid buildup in the middle ear, children with cleft palate usually need special tubes placed in the eardrums to aid fluid drainage, and their hearing needs checked once a year.
Up to 40% of children with a cleft palate need further surgeries to help improve their speech. A speech pathologist assesses speech between ages 4 and 5. They may use a nasopharyngeal scope to check the movement of the palate and throat. If surgery is needed to improve speech, this surgery is usually performed around age 5.
Children with a cleft involving the gum line may also need a bone graft when they are between 6 and 10 to fill in the upper gum line so that it can support permanent teeth and stabilize the upper jaw. Once the permanent teeth grow in, a child will often need braces to straighten the teeth and a palate expander to widen the palate.
Additional surgeries could include surgery to:
- Improve the appearance of the lip and nose.
- Close openings between the mouth and nose.
- Help to breathe.
- Stabilize and straighten the jaw.
Possible risks to surgery include bleeding, infection and damage to nerves, tissues or other structures. Surgery is usually successful, and risks are low. Cleft lip surgery leaves a small pink scar that should shade over time and become less noticeable as the child grows.
Surgery is usually successful, and risks are low. Cleft lip surgery leaves a small pink scar that should shade over time and become less noticeable as the child grows.
At what age are cleft lip and palate repairs done?
Most surgeries to repair a cleft lip happen within the 12 months of an infant's life. Surgery to repair a cleft palate typically occurs within the first 18 months. Some children need additional surgeries to make cosmetic repairs to the areas or fix breathing, hearing, or speech issues.
What nonsurgical treatments help cleft lip and cleft palate?
Children often need treatment beyond surgery for cleft lip or palate. Some other treatments their healthcare providers may use are speech therapy and orthodontic treatment.
Prevention
How do you prevent cleft lips or palates in babies?
Having a baby born with congenital anomalies like cleft lip or cleft palate is unpreventable. However, you can do things to reduce your risk, like avoiding using cigarettes, alcohol, and certain medications. Talk to your healthcare provider if you are concerned about cleft lip or cleft palate.
Talk to your healthcare provider if you are concerned about cleft lip or cleft palate.
Outlook / Prognosis
What's the outlook for children who have cleft lip or cleft palate?
Although treatment may take many years and require several surgeries, most children affected by these conditions have a normal childhood. Treatment helps improve speech and feeding issues. Some people may be self-conscious about the shape of their lips or scarring.
Do cleft lips or palates go away?
No, cleft lips and palates don't go away without treatment.
Living With
How should the dental care needs of children with cleft lips or palates be met?
Generally, the dental care needs of children who have clefts are the same as other children. However, children with cleft lip and palate may have missing, misshapen or poorly positioned teeth. Some recommendations include:
- Early dental care: Like other children, children with cleft lip and cleft palate require proper cleaning, good nutrition and fluoride treatment to have healthy teeth.
 Appropriate cleaning with a small, soft-bristled toothbrush should begin as soon as teeth appear. If a soft children's toothbrush doesn't adequately clean the teeth because of the different shape of the mouth and teeth, the dentist may recommend a soft, mouthwash-containing sponge on a handle to swab the child's teeth. Many dentists recommend that the first dental visit be scheduled at age 1 or earlier if there are problems. Routine dental care can begin around 3.
Appropriate cleaning with a small, soft-bristled toothbrush should begin as soon as teeth appear. If a soft children's toothbrush doesn't adequately clean the teeth because of the different shape of the mouth and teeth, the dentist may recommend a soft, mouthwash-containing sponge on a handle to swab the child's teeth. Many dentists recommend that the first dental visit be scheduled at age 1 or earlier if there are problems. Routine dental care can begin around 3. - Orthodontic care: After permanent teeth appear, an orthodontist can further evaluate a child's short and long-term dental needs. Most children with a cleft palate will require palatal expansion around age 6 or 7. After all the permanent teeth erupt, an orthodontist can align the teeth with braces. Orthodontic care is also required in preparation for jaw surgery (orthognathic surgery).
- Prosthodontic care: A prosthodontist may make a dental bridge to replace missing teeth, or special appliances called "speech bulbs" or "palatal lifts" to help close the nose from the mouth so that speech sounds more normal.
 The prosthodontist coordinates treatment with the oral or plastic surgeon and the speech pathologist.
The prosthodontist coordinates treatment with the oral or plastic surgeon and the speech pathologist.
Frequently Asked Questions
Is a cleft palate genetic?
Some studies suggest cleft lips and cleft palates have a genetic component. If you or your partner were born with a cleft lip or palate, your chance of having a baby with a cleft is around 2% to 8%. If you've already had a child with a cleft lip or palate, your chances of having another child with the condition are slightly higher.
A note from Cleveland Clinic
You may feel concerned when you find out your baby has a cleft lip or cleft palate. In most cases, your baby is healthy, and surgery can help fix the clefts' appearance. Treating children with cleft lips or palates involves fixing the lip and mouth so that they can function correctly. Treatment may also include dental work, orthodontia and speech therapy. If your child is diagnosed with a cleft lip or cleft palate, talk to your healthcare provider about the treatment plan and what to expect.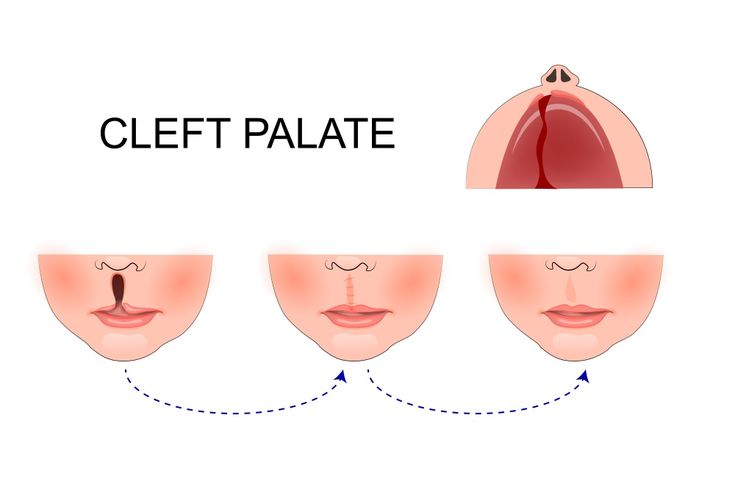 And remember, most children with cleft lip or cleft palate go on to live happy and healthy childhoods.
And remember, most children with cleft lip or cleft palate go on to live happy and healthy childhoods.
Cleft lip. Part 1. Introduction. Indications. Anatomy. Contraindications
History
Chinese doctors were the first to be able to describe in detail the facial reconstruction procedure for cleft lip disease. Early techniques were limited to cutting a flat gap and stitching it piece by piece. In the middle of the 17th century, the evolution of surgical technique made it possible to use special plates for the treatment of such diseases. The use of this method in the early stages of a child's life is the basis of reconstructive interventions even now. nine0005
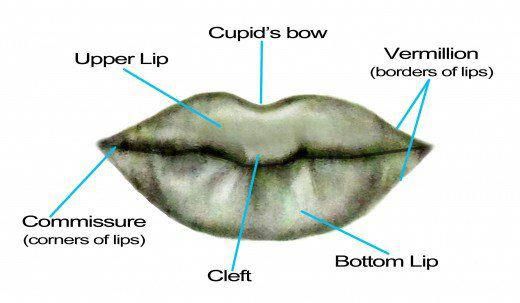
Tennyson introduced the method of triangular leather flaps, which, as a result of surgical intervention on the upper lip, forms the bow of Cupid. The geometry of this technique was described in the works of Randall, who considered it the most popular at that time. Millard introduced the surgical technique of moving the medial lip towards the lateral plate while retaining the shape of Cupid's bow in the form of a deep groove.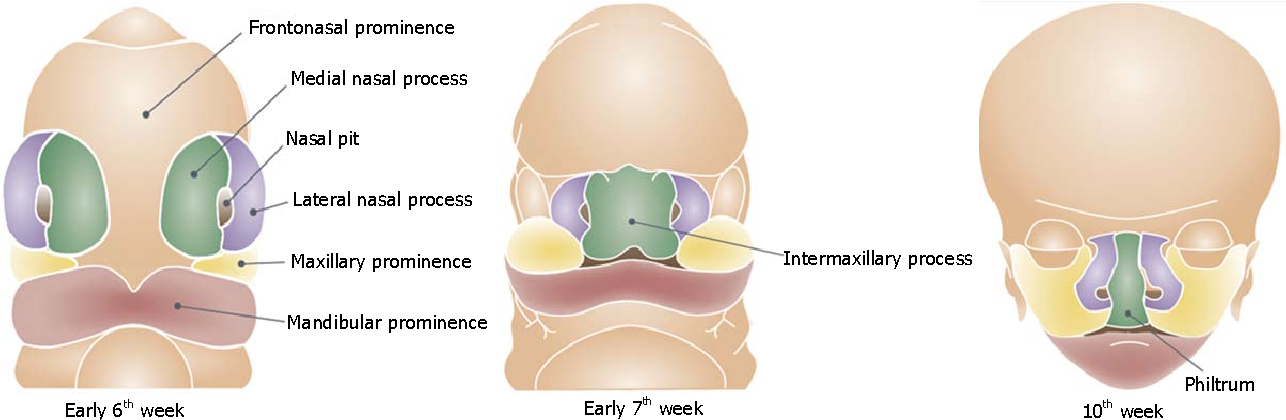 His theory improved the results of 90,007 plastic surgeries for cleft lip .
His theory improved the results of 90,007 plastic surgeries for cleft lip .
Issues
Cleft lip is one of the most common congenital pathologies. This condition is caused by insufficient development of mesenchymal cells during the initial formation of the palate. This occurs from the fourth to the seventh week of intrauterine development of the fetus. The consequence of this development is the distortion of the upper lip and nose. Also, cleft lip can be one of the interrelated syndromes, such as facial underdevelopment, dental anomalies, and speech impairment (if there is a cleft palate). Such children very often in later life have difficulties in communication associated with their psychological state. nine0005
Distribution
Among the fair-skinned population, only one child is born with this pathology in 1000 newborns. Cleft lip is twice as common in Asia. The Negroid race is characterized by the presence of this disease in half of the population.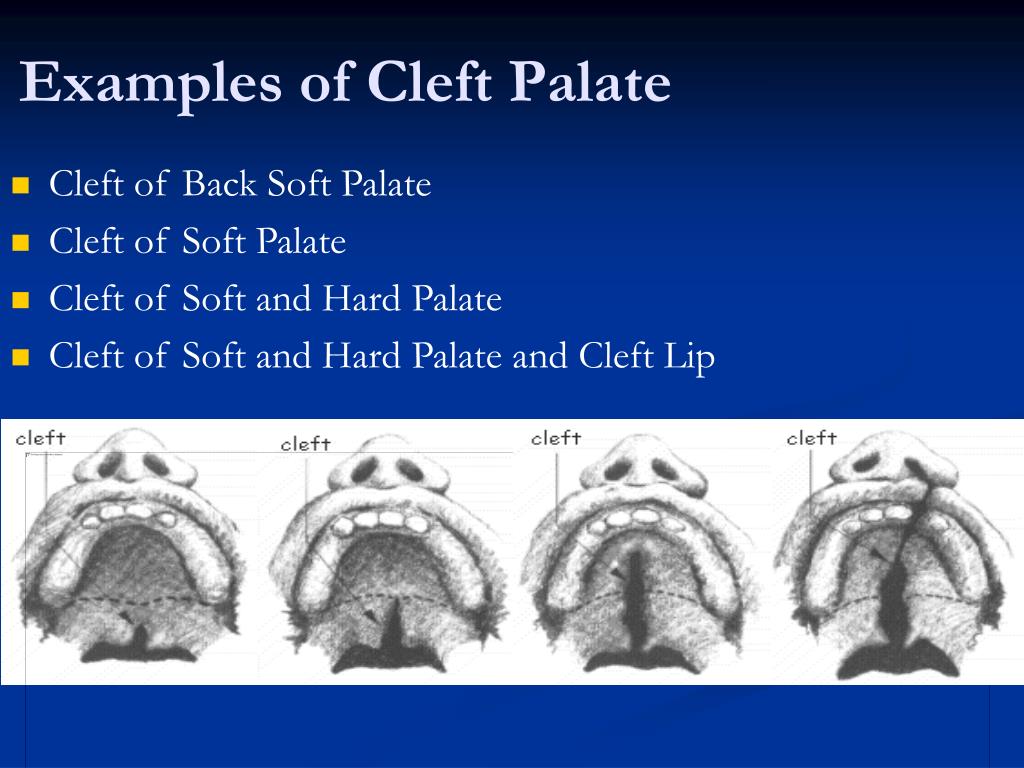 Most often, cleft lip occurs in boys. Isolated clefts on the right side are twice as rare as those on the left side, which in turn can be found 9 times more often than with bilateral cracks. Of the total number of children suffering from this disease, 50% are carriers of combined cleft (lip and palate), 30% - isolated (only palate), and 20% of the alveoli and cleft lips. Less than 10% of the dispersed are bilateral cracks. nine0005
Most often, cleft lip occurs in boys. Isolated clefts on the right side are twice as rare as those on the left side, which in turn can be found 9 times more often than with bilateral cracks. Of the total number of children suffering from this disease, 50% are carriers of combined cleft (lip and palate), 30% - isolated (only palate), and 20% of the alveoli and cleft lips. Less than 10% of the dispersed are bilateral cracks. nine0005
The risk of developing a congenital pathology in the next generation, if one of the parents has a combined cleft, is 4%. In the presence of a cleft lip in two parents at once, the possibility of inheriting the disease increases by 9%.
Etiology
The fact that teratogenic agents influence the appearance of isolated cleft in a child is not well understood. An exception is the anticonvulsant drug phenytoin. Its use during pregnancy has been associated with a tenfold increase in cleft lip births. A child with a characteristic pathology is born to a non-smoking mother two times less often than to a smoking woman.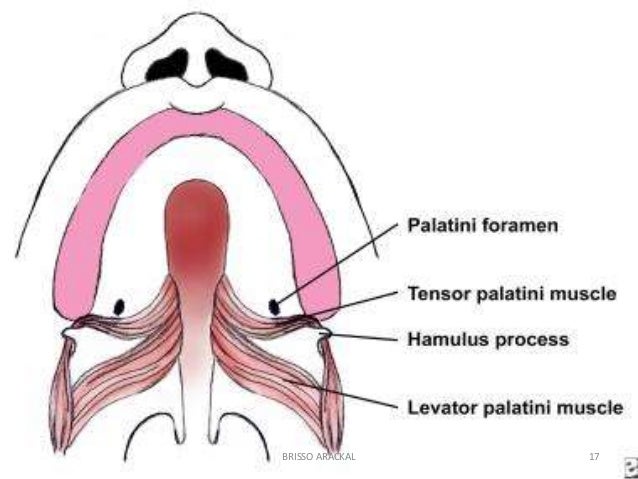 The presence of dispersed is associated with disruptions in the work of other organs in 5-14%. nine0005
The presence of dispersed is associated with disruptions in the work of other organs in 5-14%. nine0005
Vanderwood's syndrome is the most common cleft palate and lip. This autosomal dominant disorder is characterized by cleft lip (palate) and paranasal sinus, or pitting in the lower lip. A cleft palate is more commonly associated with the syndrome than an isolated cleft lip or combined cleft lip. In most cases, a cleft lip is considered the result of many factors or a change in a gene on the chromosome, but not a sign of Vanderwood. nine0005
Pathophysiology
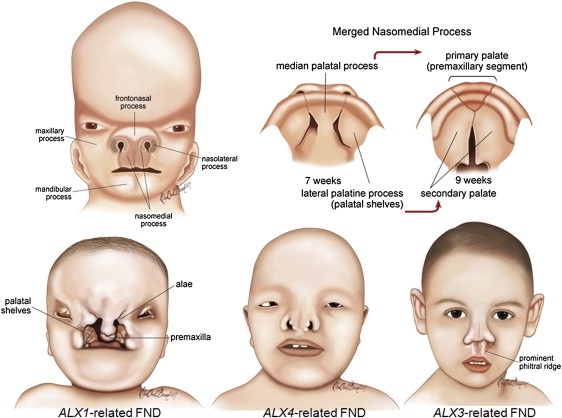
The development of the upper lip in humans is characterized by the fusion of the maxillary sinuses with the lateral and medial wall of the nose. The beginning of this process is associated with the fourth week of pregnancy, and the end with the seventh. The failure of mesenchymal cells to unite one (or both) maxillary sinuses with the medial wall results in unilateral (bilateral) cleft lip.
Classification
There is no generally accepted classification for cleft lip and palate.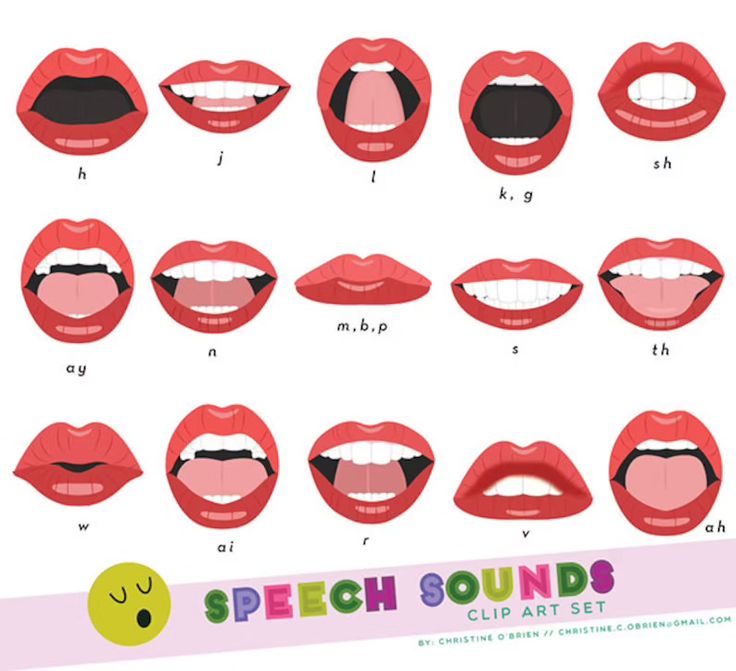 However, 4 groups are pronounced:
However, 4 groups are pronounced:
- Cleft palate only
- Clefts of soft and hard palate
- Complete unilateral cleft lip and palate
- Complete bilateral cleft lip and palate
This group does not include isolated dispersed lips and incomplete cracks. Kernahan's classification makes it possible to separate cleft lip, palate and alveoli. The boundary between the clefts of the primary and secondary palate is determined in it by sharply pronounced holes. nine0005
Presentation
Cleft lips appear as microforms (complete and incomplete cracks). They are characterized by a vertical groove and a scarlet notch with varying degrees of lip reduction. An incomplete unilateral cleft lip of varying degrees is manifested by a violation of the base of the nose, covering the range from the edge of the lip to the nostril. Complete cleft lip, in addition to the features already listed, is characterized by an alveolus.
Bilateral splits are almost always associated with the sky. 86% of patients with this pathology are owners of a palate fissure. Unilateral cleft lip is associated with palatal disorders in 68% of cases. Ejection of food through the nasal cavity during meals indicates the presence of a cleft palate. Children with cleft lip are required to undergo a complete examination of the head, neck and palate to the very tip of the tongue. The presence of a bifurcated uvula, which is a translucent palatine curtain in the central part and a noticeable gap at the posterior border of the hard palate, indicates a submucosal palatal cleft. nine0005
All newborns with cleft lip suffer from chronic otitis media or middle ear effusion, which is inextricably linked to the palatal cleft and requires constant care. To solve this problem, otolaryngologists resort to the procedure of myringotomy, which can be performed before the treatment of Vanderwood syndrome or immediately after it.
In most cases, cleft lip is not a death sentence. Parents of such children should understand that their situation is not critical. At the first visit to the doctor, they can learn detailed information about feeding methods for cleft lip. For a child with this pathology, the ability to suck milk is difficult. However, with an isolated cleft lip and alveoli, breastfeeding is quite possible. Special bottles and nipples have been created for feeding children with a crack in the sky. Transverse soft nipples help premature babies with cleft palate. nine0005
Parents of such children should understand that their situation is not critical. At the first visit to the doctor, they can learn detailed information about feeding methods for cleft lip. For a child with this pathology, the ability to suck milk is difficult. However, with an isolated cleft lip and alveoli, breastfeeding is quite possible. Special bottles and nipples have been created for feeding children with a crack in the sky. Transverse soft nipples help premature babies with cleft palate. nine0005
Indications
Treatment of cleft lip is usually carried out in early childhood. The best time for such an operation is 2-3 months of age. The rule of 10 is considered a safe indication for this. Its essence boils down to the fact that a child over the age of 10 weeks for every 10 pounds of weight should account for up to 10 g/dal of hemoglobin.
Functional Anatomy
A complete unilateral cleft lip is the result of a typical deformity of the soft tissue underlying the bone and cartilage structures. The imbalance of muscle tissue affects the maxilla by rotating the medial incisal and posterolateral parts. nine0005
The lower edge of the anterior nasal septum is displaced from the vomer gap into the intact nostril and rests on the side of the gap. The columella, which lies above, does not reach the sides of the occlusion and is distorted due to the displacement of the caudal septum. At the tip of the nose, the axillary cartilage is deformed, the medial leg goes back. The arch is separated from the intact side, and the lateral pedicle flattens and extends through the gap. The nasal axis from the side of the cleft is located in a horizontal plane. On the opposite side, the nostril axis is different and placed in the normal vertical plane. nine0005
Muscular tissue of a rounded shape is not located transversely, as in normal lips, but goes up at an angle parallel to the edge of the cleft of the axillary base on the lateral side, settled towards the base of the medial columella. The septum on the side of the cleft is very short and the supposed top of Cupid's bow is higher. The presence of a bright red hue indicates an incomplete cleft from the side of the medial part.
The presence of a bright red hue indicates an incomplete cleft from the side of the medial part.
Complete bilateral cleft lip occurs as a result of incisal failure and fusion with the posterior segment of the jaw. The subsequent growth of the incisor bone raises the vomer even higher, bringing the protrusion beyond the lateral part. In an isolated lip border with vertically shortened skin, the white roll is not sufficiently developed, and the cinnabar is not bright enough. The central projection of the upper lip lacks muscle tissue, as well as the philtrum and dimple. Cupid's bow is missing. Bilateral nasal cleft deformity is characterized by a prominent pterygoid base and a wide division of the dome of the axillary cartilage. Columella is significantly shortened, so it becomes the cause of the drooping of the tip of the nose. nine0005
Contraindications
Anything that can lead to heart problems, bleeding disorders, infection or malnutrition is a contraindication for surgery.
Cleft lip in children: photo, causes, symptoms, treatment
Congenital pathology of the lip, in which soft tissues do not grow together, is usually called "hare lip" in colloquial speech. This name is given because in hares the upper lip consists of two halves that are not fused together. nine0005
The nature of the defect is the same as that of the "cleft palate". But in the case of the latter, not only soft tissues do not fuse, but also the bones of the palate. In half of the cases, facial tissues are not affected, and there is no cosmetic defect. In this case, it will only be a "wolf mouth".
Cleft palate and lips are scientifically called cheiloschisis. This congenital pathology occurs in the womb, usually in the first trimester of pregnancy. Under the influence of harmful factors, the development of the lip, palate and alveolar process is disrupted. nine0005
Children with cleft lip can have not only external defects, but also a serious deformity of the skull bones.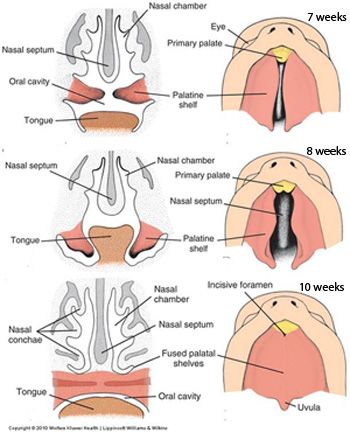 Because of this, there are difficulties with nutrition, speech. But pathology causes only physical problems - the intellect and psyche of such babies are in perfect order.
Because of this, there are difficulties with nutrition, speech. But pathology causes only physical problems - the intellect and psyche of such babies are in perfect order.
Cleft lip without cleft palate is a milder pathology, since only soft tissues are affected and the bones are not deformed.
What is a cleft lip
Cleft palate and lip appear in a baby in the first months of development. It is then that the jaw and face are formed. Normally, by the 11th week, the bones of the palate in the fetus grow together, and then the soft palate is formed. In the 2nd to 3rd month, the upper lip is also formed, when the processes of the upper jaw and the median nasal process are finally fused. nine0005
The first months of pregnancy are the most important for the formation of the correct anatomy of the child. If during this period negative factors from the outside influence the embryo, a failure in the formation of bones and soft tissues may occur, and a cleft lip occurs.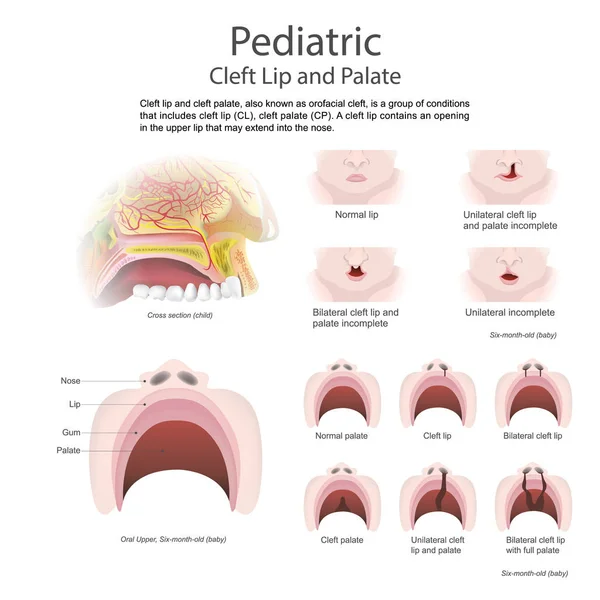 Genetic factors also play a role.
Genetic factors also play a role.
Causes of cleft lip in children
The cleft lip develops under the influence of "internal" and "external" causes. A hereditary factor, inferiority of germ cells, early abortions can affect the development of the fetus. nine0005
No less dangerous infections that a woman suffers in early pregnancy.
Chemicals, radiation, maternal drug use, alcohol or smoking adversely affect fetal development. Poor nutrition, beriberi, cold and heat, abdominal trauma, fetal hypoxia also affect the formation of the fetus.
The causes of pathology are still being studied. The main ones are listed above, but in rare cases, a cleft lip develops after birth. After injuries, infections, removal of tumors, the palate and lips can be damaged. nine0005
Symptoms of cleft lip in children
A cleft lip in a baby is usually detected before birth, on ultrasound after 12 weeks of pregnancy. Unfortunately, even with this early detection, nothing can be done before the baby is born.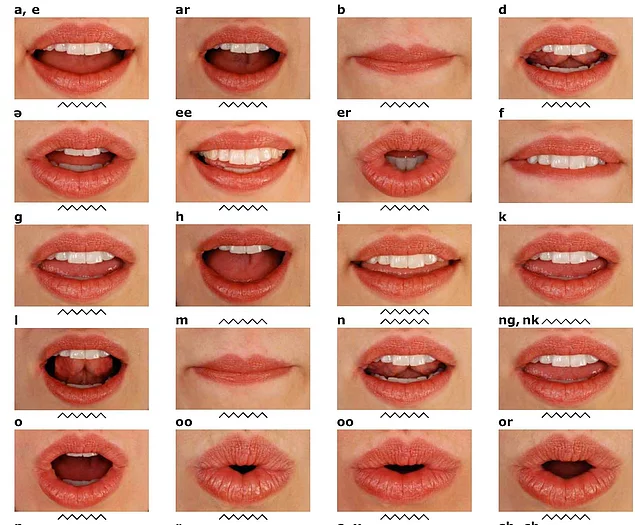
After birth, the baby shows deformed lips, nose, and possibly a cleft palate. The form and degree of pathology are of varying severity - crevices are possible even on both sides. But unilateral cleft palate and lips are more common.
An infant with such a defect takes the breast poorly, often chokes, and breathes shallowly. It is prone to infections of the nasopharynx and ear due to frequent reflux of food through the cleft in this area.
Treatment of cleft lip in children
It is important to understand that cleft lip is often not only a cosmetic problem. She will have to be treated anyway, and at a very early age. Otherwise, the child will not be able to suck, swallow food correctly, sometimes feeding through a tube is even required.
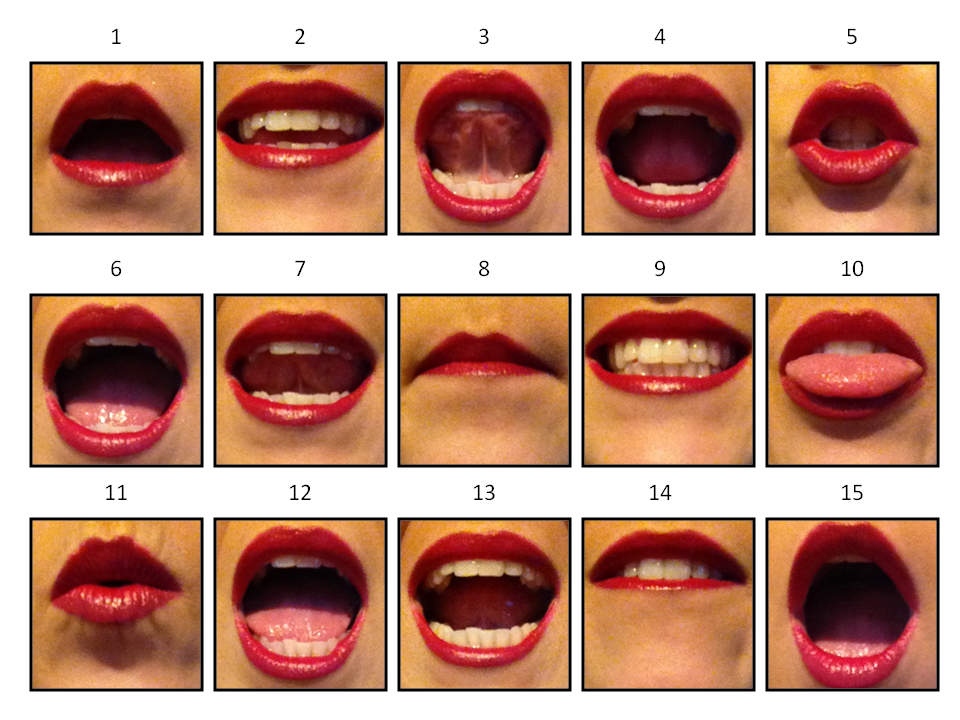
Without treatment of the defect, the bite is formed incorrectly, speech is impaired. The splitting of the palate disrupts the timbre of the voice, children do not pronounce sounds well and speak “through the nose”.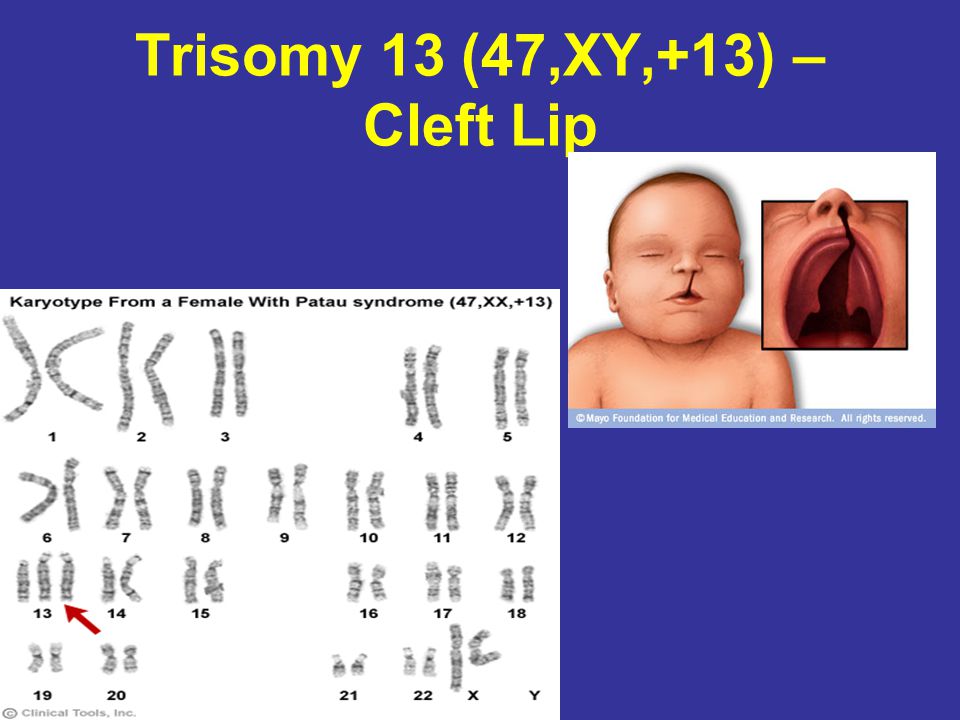 Even a cleft only in the soft tissues will interfere with the production of speech. Frequent inflammation in the nasal cavity and ears due to reflux of food leads to hearing loss. nine0005
Even a cleft only in the soft tissues will interfere with the production of speech. Frequent inflammation in the nasal cavity and ears due to reflux of food leads to hearing loss. nine0005
After the diagnosis is made, a decision is made to perform a surgical operation – there is no other way to help the child. The age at which the baby will be operated on is determined by the doctor. If the defect is too dangerous, the first operation is possible in the first month of life. Usually it is postponed until 5 - 6 months.
The treatment consists of several stages, so one surgical intervention will not work. Even before the age of 3, the baby will have to go through 2 to 6 operations. But as a result, only a barely noticeable scar and possibly a slight asymmetry of the lips will remain. All other problems will be behind. nine0005
Diagnosis
The first diagnosis of cleft lip is carried out while still in the womb using ultrasound. After the birth of such a child, the doctor examines the severity of the pathology. It determines how much the defect prevents the baby from eating, whether there are any respiratory disorders.
It determines how much the defect prevents the baby from eating, whether there are any respiratory disorders.
They resort to the help of other specialists: an otolaryngologist, a dentist, an infectious disease specialist. Further, general blood and urine tests, blood biochemistry, x-rays of the maxillofacial region are prescribed. The reaction of the baby to sounds and smells is checked - this is how hearing and smell, facial expressions are evaluated. nine0005 Photo: @mart.production, pexels.com
Modern methods of treatment
Plastic surgery is used to eliminate the defect of the cleft lip. Doctors of various profiles will be involved in multi-stage treatment. Before surgery, the child often wears an obturator - a device that serves as a barrier between the nasal and oral cavities. This prevents the reflux of food, helps to breathe and talk normally.
With a small defect, isolated cheiloplasty is used - the skin, fiber, muscle and mucous layers of the lips are sutured. If the nose is affected, rhinocheiloplasty is performed, correcting the cartilages of the nose. Rhinognatocheiloplasty forms the muscular frame of the mouth area. nine0005
If the nose is affected, rhinocheiloplasty is performed, correcting the cartilages of the nose. Rhinognatocheiloplasty forms the muscular frame of the mouth area. nine0005
Cleft palate is corrected by uranoplasty. Unlike previous operations, it is carried out quite late - by 3 or even 5 years. Early intervention can damage jaw growth.
Additional reconstructive surgeries are needed to remove scars, improve speech and aesthetics.
In addition to surgical treatment, the child needs the help of a speech therapist, since it is more difficult for such children to pronounce sounds correctly than for others. The otolaryngologist makes sure that the baby's hearing is not affected, and the breathing is full. If the teeth do not grow properly, the orthodontist installs braces. nine0005
Chronic oxygen deprivation due to shallow breathing, poor weight gain and frequent infections can lead to sickness, stunted growth.
The help of a psychologist will be equally important, because due to their characteristics, children with a cleft lip experience difficulties in adapting.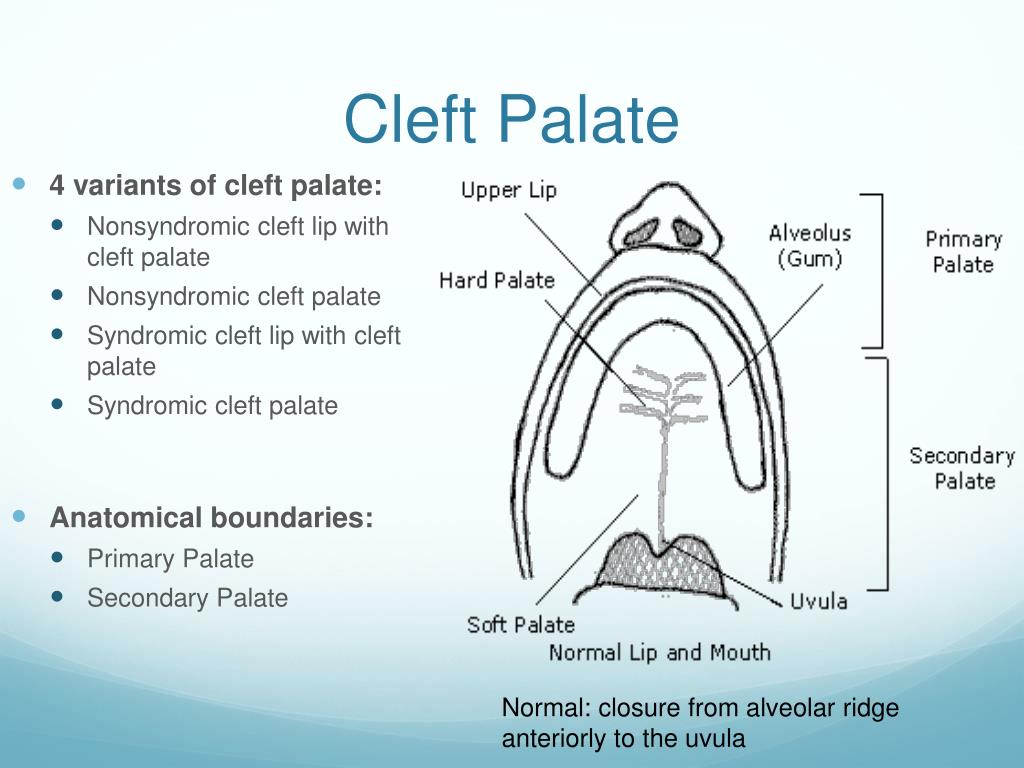 Despite the fact that the mind of such children is in perfect order, they can still lag behind in development. Due to psychological problems, unwillingness to study due to bullying by peers, there are problems in learning. Difficulties in pronunciation of words can also interfere with a fulfilling life. Therefore, it is better to complete all stages of treatment before school age. nine0005
Despite the fact that the mind of such children is in perfect order, they can still lag behind in development. Due to psychological problems, unwillingness to study due to bullying by peers, there are problems in learning. Difficulties in pronunciation of words can also interfere with a fulfilling life. Therefore, it is better to complete all stages of treatment before school age. nine0005
Prevention of cleft lip in children at home
Avoiding such a problem is quite difficult. If such a pathology was observed in the family, you can consult a geneticist to find out the likelihood of having a baby with a cleft lip.
It is important to take special care of yourself in the first weeks of pregnancy - avoid infections, injuries, eat well. As a preventive measure, pregnant women take folic acid.
It is necessary to detect the problem as early as possible, while still in the womb. Since cleft palate and lip can cause additional complications during childbirth, the doctor should be aware.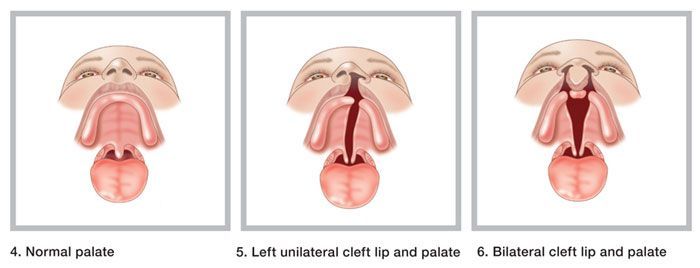 During childbirth, the risk of amniotic fluid entering the baby's respiratory tract increases. nine0005
During childbirth, the risk of amniotic fluid entering the baby's respiratory tract increases. nine0005
After the birth of a child with a cleft lip, it is necessary to carry out a complete diagnosis, consult with specialists and assess the severity of the pathology. If doctors insist on an early operation, then the baby really needs it.
The first months and years of the life of such a child will be difficult, feeding is difficult and parents need to be prepared for this. But do not forget that after all stages of treatment, the child will be completely healthy and the problem will be left behind.
Popular questions and answers
The pediatrician remains the main doctor for a child with cleft lip - he prescribes additional examinations, refers to narrow specialists. pediatrician Daria Schukina will tell you more about this pathology.
What are the complications of cleft lip?
Without treatment, the child's speech will be impaired even if the palate is not affected.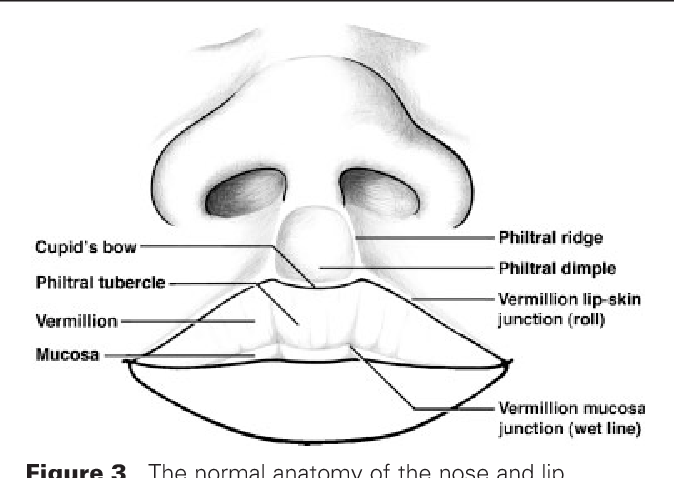 Severe cleft lip will also have difficulty sucking.
Severe cleft lip will also have difficulty sucking.
When to call a doctor at home for cleft lip?
When a child has SARS or similar diseases. In emergency cases, you need to call an ambulance. The treatment of the cleft lip is planned, it is not necessary to call a doctor for such a pathology. Are the cleft palate and cleft lip the same thing? Why then are they called differently? Not exactly. Indeed, both diseases are congenital. The cleft lip is a cleft and defect in the soft tissues of the lip, and the cleft palate is a cleft palate when a message appears between the oral cavity and the nasal cavity. However, they are often combined, and then the child will have both an external defect and an internal one. Moreover, there is a possibility of malformations of other organs and systems. nine0005
At what age should the operation be done so that it is not too late?
There is no consensus on this matter. Optimally - before the formation of speech, but in general - the sooner the better.